Abstract
Study Objective:
Obstructive sleep apnea syndrome (OSAS) has been considered to be an important predisposing factor for cardiovascular disease. This study aims to investigate the impact of OSAS on cardiac function and remodeling in patients without congestive heart failure.
Methods:
A total of 79 patients with sleep disordered breathing, preserved systolic function, and normal pro-brain natriuretic peptide level were enrolled. Sixty-five patients were classified to have moderate to severe OSAS (apnea-hypopnea index [AHI] ≥ 15/h), while the other 14 patients with mild or no OSAS (AHI < 15/h) served as control subjects. Baseline clinical and polysomnographic variables as well as tissue Doppler imaging and three-dimensional echocardiographic parameters were obtained.
Results:
The body mass index, neck circumference, Epworth Sleepiness Scale, desaturation index, arousal index, and snoring index were significantly higher in patients with moderate to severe OSAS than those without (p < 0.05). The left atrial size, mitral A-wave velocity, and left ventricular end-diastolic volume were significantly larger, while E/A ratio was lower in patients with moderate to severe OSAS than those without (p < 0.05). Notably, AHI in REM sleep was significantly correlated with the aortic root size, E/A ratio, left ventricular volume, and stroke volume. In addition, the area under the receiver operator characteristic curve for AHI in REM sleep ≥ 32.3/h was 0.647 (95% CI [0.525, 0.769]) in predicting the development of left ventricular diastolic dysfunction. AHI in REM sleep ≥ 32.3/h was the only independent variant in predicting diastolic dysfunction after adjusting the variables including age, gender, hypertension, and body mass index.
Conclusions:
Patients with moderate to severe OSAS tend to have cardiac dysfunction revealed by echocardiography. High AHI in REM sleep is significantly associated with cardiovascular remodeling and ventricular diastolic dysfunction, and may be a potential variable to predict cardiac dysfunction.
Citation:
Chen YL; Su MC; Liu WH; Wang CC; Lin MC; Chen MC. Influence and predicting variables of obstructive sleep apnea on cardiac function and remodeling in patients without congestive heart failure. J Clin Sleep Med 2014;10(1):57-64.
Keywords: Echocardiography, sleep apnea syndrome, diastolic dysfunction, cardiovascular remodeling
Obstructive sleep apnea syndrome (OSAS) has been reported to correlate closely with systemic hypertension, and possibly atrial fibrillation, myocardial infarction, congestive heart failure, stroke, and probably death.1–16 During sleep, intermittent hypoxemia and arousals from sleep may increase sympathetic activity and induce acute hemodynamic changes in patients with OSAS.17,18 Sustained breathing effort due to pharyngeal collapse yields substantially negative intrathoracic pressure, which increases transmural cardiac pressure, ventricular wall tension, and afterload.19 Furthermore, both increased venous return due to negative intrathoracic pressure and increased pulmonary arterial pressures caused by hypoxemia may elevate right ventricular pressure, resulting in a leftward shift of the interventricular septum.20,21 These hemodynamic changes may cause left ventricular dyssynchrony, and either diastolic or systolic heart failure. On the other hand, a large number of patients with congestive heart failure have been reported to have comorbid OSAS.22,23 Such phenomena suggest cardiovascular disease is also a predisposing factor for OSAS. Therefore, the mechanisms how OSAS induces cardiovascular diseases or the other way around have not yet been fully elucidated.
BRIEF SUMMARY
Current Knowledge/Study Rationale: The frequent coexistence of obstructive sleep apnea syndrome (OSAS) and congestive heart failure in clinical scenarios make it difficult to clearly define the exact impact of OSAS on cardiac remodeling and function, and vice versa. This study aims to investigate the impact of OSAS on cardiac function and remodeling in the patients without congestive heart failure.
Study Impact: Those with OSAS have a higher incidence of cardiovascular remodeling and ventricular diastolic dysfunction than those without, even in patients without congestive heart failure. The higher apnea-hypopnea index (AHI) in REM sleep is significantly associated with cardiovascular remodeling and ventricular diastolic dysfunction and might be a potential variable to predict cardiac dysfunction and remodeling.
Tissue Doppler imaging (TDI), real-time three-dimensional (RT3D) echocardiography, as well as biomarkers such as high-sensitivity C-reactive protein (hs-CRP) and N-terminal pro-brain natriuretic peptide (NT-proBNP) have been well defined techniques to investigate cardiac structural and functional remodeling and to predict patients with a high risk of cardiovascular mortality and morbidity.24–30 In spite of the fact that these tools are widely available and frequently introduced in clinical settings, the cardiac structural and functional remodeling studied by utilizing TDI and RT3D has rarely been conducted in patients with OSAS to evaluate their cardiac function.31–37 In addition, the frequent coexistence of OSAS and congestive heart failure in clinical scenarios make it difficult to clearly define the exact impact of OSAS on cardiac remodeling and function, and vice versa. In order to answer these unresolved issues regarding the impact of OSAS itself on cardiac structure and function, it is crucial to conduct a study enrolling subjects exclusively without clinical symptoms of heart failure.
This study tested the hypothesis that significant OSAS may be associated with enlarged left ventricle and ventricular dysfunction. Accordingly, we measured the echocardiographic parameters by TDI and RT3D echocardiography in sleep disordered breathing patients with preserved systolic function and without significant congestive heart failure (normal NT-proBNP level), and we aimed to identify important parameters in predicting the development of cardiovascular remodeling and ventricular dysfunction in patients with sleep disordered breathing.
METHODS
Patient Population
Patients with symptoms of sleep disordered breathing referred to our sleep center for sleep study between June 2009 and September 2011 were enrolled in this study. The following were exclusion criteria: (1) unwillingness or inability to perform the testing procedures; (2) systolic dysfunction defined as left ventricular ejection fraction < 50% and with marked symptoms or signs of congestive heart failure; (3) cardiac murmur revealed by physical examination or significant valvular stenosis or regurgitation documented by echocardiography; (4) evidence of ischemic heart disease; (5) any documented bradyarrhythmia, tachyarrhythmia, or aborted cardiac death; (6) diabetes mellitus and other metabolic disorders; (7) renal function impairment, defined as serum creatinine > 1.2 mg/ dL; and (8) history of malignancy. Echocardiography measurements and blood tests were routinely performed in all patients before the polysomnographic study to minimize investigation bias. The study protocol was approved by the Institutional Review Committee for Human Research at our institution (98-0769B). Written informed consents were obtained from all subjects prior to the study.
Polysomnography
All patients enrolled in this study underwent an overnight polysomnographic study. Prior to the sleep study, body height, body weight, body mass index (BMI), and neck size were measured. The tendency to fall asleep during various situations, and subjective sleepiness was assessed simultaneously by using a validated questionnaire, the Epworth Sleepiness Scale (ESS).38 The overnight polysomnographic study was conducted using a standardized commercial suite (Sandman Elite, Mallinckrodt Inc., St. Louis, MO) set in our sleep center. Sleep parameters were then recorded and analyzed, and the respiratory events were identified by experienced technicians according to the standard criteria.39 Respiratory events were classified as either obstructive or central on the basis of presence or absence of respiratory effort. Respiratory events were defined as apnea when there was a cessation of oronasal airflow ≥ 10 seconds. Hypopnea was defined as a decrease ≥ 30% in oronasal airflow ≥ 10 seconds, associated with a fall in arterial oxygen saturation (SpO2) > 4% of the baseline level or associated with an arousal. Mean nighttime SpO2, minimum SpO2 (lowest values recorded during sleep), desaturation index, and percentage of time with SpO2 < 90% on oximetry were computed as indexes of nocturnal oxygen saturation. Moderate to severe OSAS was defined as apnea-hypopnea index (AHI) ≥ 15/h with associated symptoms, such as excess daytime sleepiness and witnessed apneas during sleep.
Echocardiography
Transthoracic two-dimensional (2D) echocardiography, TDI, and RT3D echocardiography were performed using a Sonos 7500 (Live 3D Echo; Philips Medical Systems, Andover, MA) with an S3 transducer, and iE-33xMATRIX Echocardiography System (Philips Medical Systems, Andover, MA), following our previous echocardiography protocol.40,41 The left atrial and ventricular dimensions, aortic root size and septal-to-posterior wall motion delay (SPWMD) were determined with conventional M-mode echocardiography. Pulsed-wave Doppler was used for the measurement of myocardial performance index (MPI), an index combining systolic and diastolic myocardial performance,42 and the aortic time-velocity integrals.
Tissue Doppler imaging was conducted using standard apical views for long-axis motion of the ventricle, as previously described.40,41 At least 3 consecutive beats were stored with digital loops for offline analysis using a validated software, QLAB version 8.1 (Philips Medical Systems). Times to peak systolic velocity (Ts) and early diastolic velocity (Te) were determined for each of the 12 non-apical segments. Synchronicity was assessed by calculating the standard deviation of Ts (Ts-SD) and Te (Te-SD) of all 12 non-apical segments.
The details of RT3D measurements have been reported in our previous studies.40,41 In brief, the RT3D echocardiography obtained a pyramidal volume in real time using an X4 matrix transducer. QLAB version 8.1was also used for quantitative analysis. The RT3DE data sets were used for time-volume analysis for the determination of global and segmental left ventricular volumes. The systolic dyssynchrony index was measured; a higher systolic dyssynchrony index indicated increased intraventricular dyssynchrony.
Statistical Analysis
There were two well-trained echocardiologists performing the echocardiogram in our study. Eight study subjects were selected for assessment of inter-rater and intra-rater reliability. The intraclass correlation coefficiency for intraobserver agreement was 0.913, 0.982, and 0.974 for systolic dyssynchrony index, A-wave velocity, and myocardial performance index, respectively. The interclass correlation coefficiency for interobserver agreement was 0.896, 0.937, and 0.963 for systolic dyssynchrony index, A-wave velocity, and myocar-dial performance index, respectively. Data were expressed as mean ± SD unless stated otherwise. Differences in continuous variables were analyzed using Mann-Whitney-Wilcoxon test and categorical variables by χ2 test or Fisher exact test. The correlation between AHI in REM sleep or NREM sleep and all echocardiographic parameters were analyzed with Pearson correlation test. Areas under the receiver operator characteristic curve were constructed for the sensitivity and specificity of AHI to predict the development of left ventricular diastolic dysfunction in patients with sleep disordered breathing. Multiple stepwise logistic regression analysis was utilized for independent predictors of diastolic dysfunction which defined as E/A ratio ≤ 1. Statistical analysis was performed using commercial statistical software (SPSS for Windows, version 13; SPSS Inc., IL, USA). A two-sided p-value < 0.05 was considered statistically significant.
RESULTS
Baseline Characteristics of the Study Patients
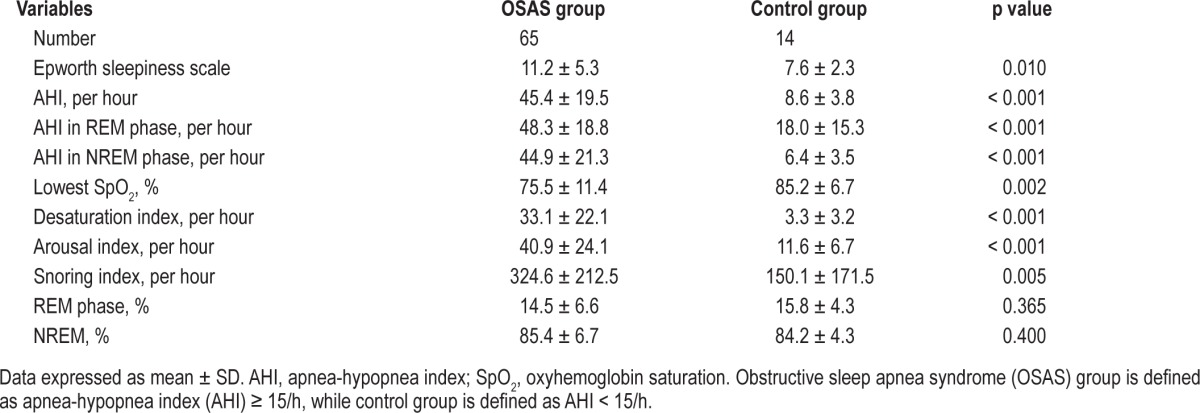
Eighty- four consecutive patients were screened during the study period. Five patients were subsequently excluded due to obvious valvular regurgitation, stenosis, or left ventricular systolic dysfunction. A total of 79 patients thus completed this study. After an overnight polysomnographic study, 65 patients were classified as having moderate-to-severe OSAS (AHI ≥ 15/h), while the other 14 patients with mild or no OSAS (AHI < 15/h) served as control subjects. Table 1 lists the baseline clinical characteristics and laboratory data of the studied patients with and without moderate-to-severe OSAS. There was no significant difference in age, gender, prevalence of hypertension, dyslipidemia, or systolic or diastolic blood pressures between the 2 groups. In addition, serum levels of the hs-CRP, NT-proBNP, creatinine, and sodium, as well as the heart rate, PR interval, QRS duration, and QRS axis measured by 12-lead surface electrocardiography did not differ significantly between the 2 groups. Polysomnographic variables obtained from both groups are shown in Table 2. The BMI, ESS, the lowest oxyhemoglobin saturation, desaturation index, arousal index, and snoring index were significantly higher in patients with moderate-to-severe OSAS than those without (all p < 0.05). There was no significant difference in REM sleep and NREM sleep percentage.
Table 1.
Baseline characteristics and laboratory data of all patients with sleep disordered breathing
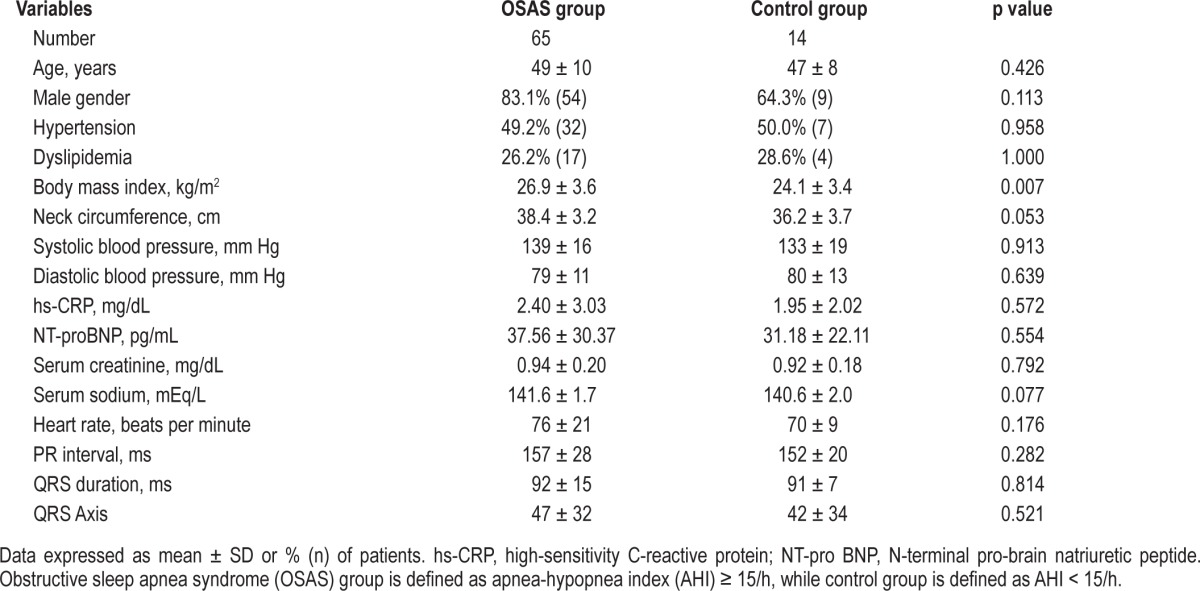
Table 2.
Polysomnographic variables of all patients with sleep disordered breathing
Echocardiographic Parameters of Study Patients
Table 3 shows the echocardiographic parameters of patients with and without moderate to severe OSAS. Between the 2 groups there was no significant difference in the thickness of interventricular septum and left ventricular posterior wall, left ventricular end-diastolic and end-systolic diameters, left ventricular ejection fraction, myocardial performance index, time-velocity integral at left ventricular outflow tract, E-wave velocity, deceleration time, tricuspid regurgitation pressure gradient, left ventricular end-systolic volume, left ventricular stroke volume, and global left ventricular ejection fraction by RT3D echocardiography, as well as mechanical dyssynchrony indices, such as septal-to-posterior wall motion delay by M-mode echocardiography, Ts-SD and Te-SD by TDI, and systolic dyssynchrony index by RT3D echocardiography.
Table 3.
Echocardiographic parameters of all patients with sleep disordered breathing
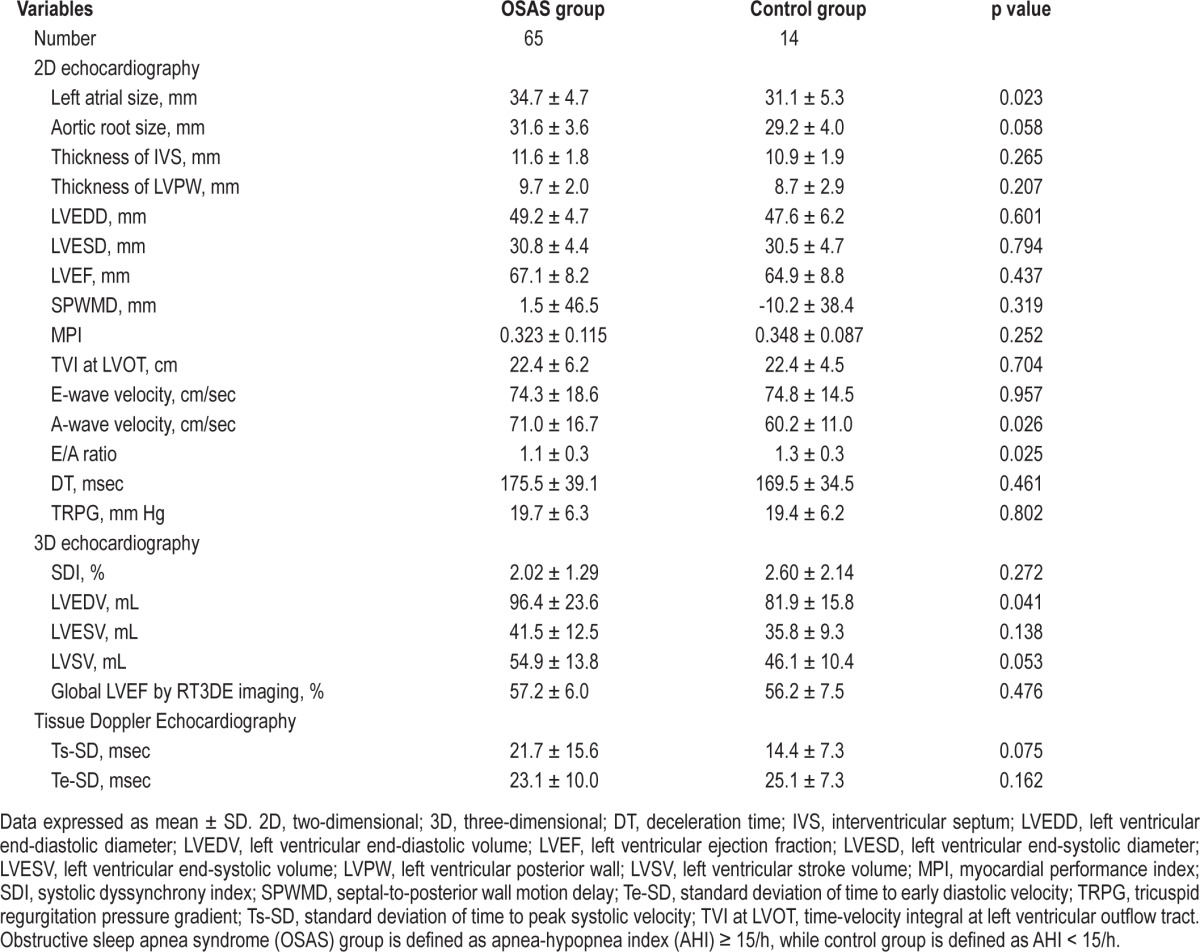
Nevertheless, the left atrial size, mitral A-wave velocity, and left ventricular end-diastolic volume by RT3D echocardiography were significantly larger in patients with moderate to severe OSAS than in patients without (all p < 0.05). The E/A ratio was significantly lower in patients with moderate to severe OSAS than in those without (p < 0.05).
Correlation between AHI and Echocardiographic Parameters
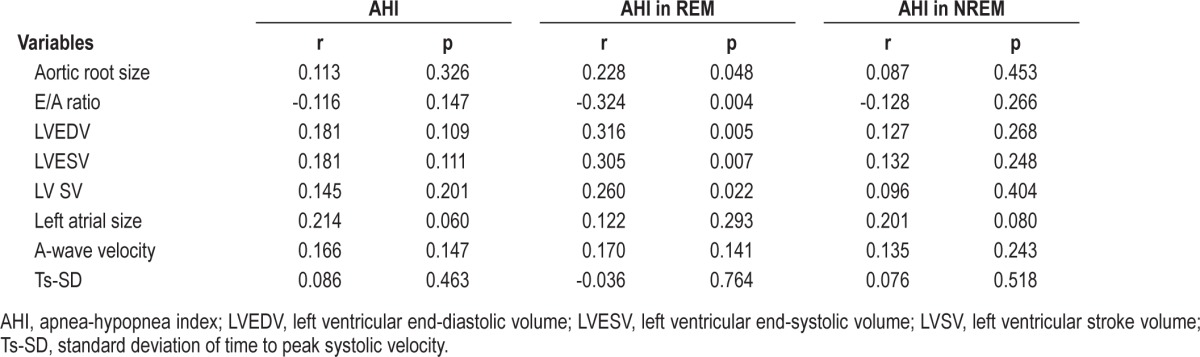
In order to explore the impact of OSAS on cardiac function, the association between AHI (both in REM and NREM sleeps) and all echocardiographic parameters measured by M mode, 2D and RT3D echocardiography and TDI were further analyzed. Notably, only AHI in REM sleep but neither AHI in NREM sleep nor total AHI was significantly associated with the aortic root size, E/A ratio, left ventricular end-diastolic volume, left ventricular end-systolic volume, and left ventricular stroke volume (Table 4).
Table 4.
Correlation between AHI and echocardiographic parameters
Discriminant analysis was performed to identify the AHI in REM sleep in predicting the development of left ventricular diastolic dysfunction (E/A ≤ 1) in patients with sleep disordered breathing. The area under the receiver operator characteristic curve for the cutoff value ≥ 32.3/h was 0.647 (95% CI [0.525, 0.769], p = 0.032; Figure 1).
Figure 1. Receiver operator characteristic curve for the cutoff value of apnea-hypopnea index (AHI) in predicting E/A ratio ≤ 1 (an index of ventricular diastolic dysfunction).
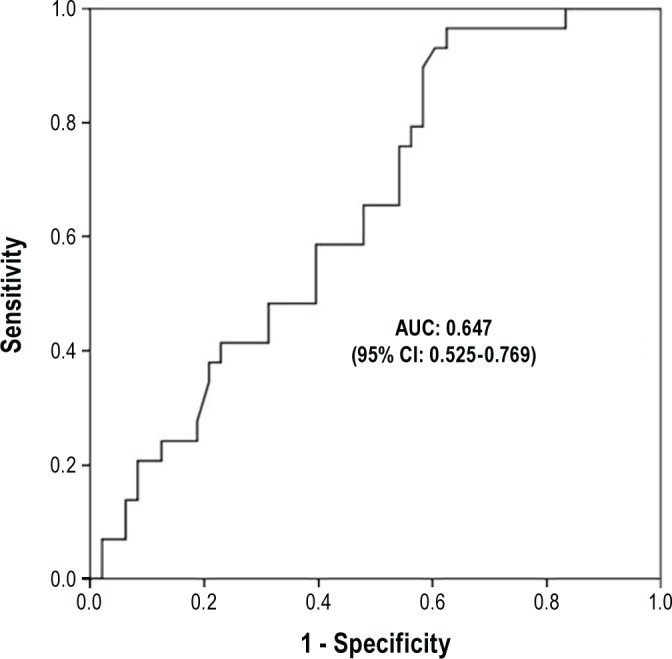
The area under curve (AUC) for the cutoff value of AHI ≥ 32.3/h was 0.647. 95% CI: 0.525, 0.769. p = 0.032.
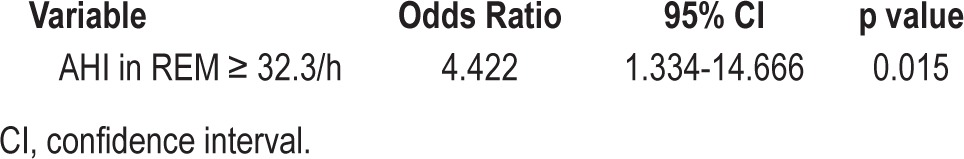
Multivariate Logistic Regression Analysis of Predictors for Left Ventricular Diastolic Dysfunction
Multiple stepwise logistic regression analysis of the variables, including age, gender, hypertension and AHI in REM sleep showed that AHI in REM ≥ 32.3/h was the only independent predictor of left ventricular diastolic dysfunction (E/A ≤ 1; Table 5).
Table 5.
Multivariate logistic regression analysis of predictors for left ventricular diastolic dysfunction
DISCUSSION
In this study we used echocardiographic methods to investigate the impact of marked OSAS on cardiac function and structural remodeling in sleep disordered breathing patients without symptoms of congestive heart failure. We found that patients with moderate to severe OSAS have an increased size of left atrium, larger A-wave velocity and left ventricular enddiastolic volume and lower E/A ratio compared with patients with mild or no OSAS, and this is independent of the presence of hypertension. In addition, the aortic root size, E/A ratio, left ventricular end-diastolic volume, left ventricular end-systolic volume, and left ventricular stroke volume were strongly associated with AHI in REM sleep but not in NREM sleep. This suggests that high AHI in REM sleep could be a potential polysomnographic variable for predicting ventricular dysfunction and cardiovascular structural remodeling in patients with sleep disordered breathing who are without clinical symptoms of congestive heart failure.
OSAS has been reported to cause hypertension1–6 and has been associated with the development of variable cardiovascular disease and probably, congestive heart failure.10 In patients with OSAS, nocturnal intermittent hypoxemia and arousals from sleep increase sympathetic activity and induce acute hemodynamic changes.17,18 Increased negative intrathoracic pressure due to upper airway collapse increases trans-mural cardiac pressure, ventricular wall tension, and afterload.19 Both increased venous return and increased pulmonary arterial pressures caused by hypoxemia may elevate right ventricular pressure, resulting in a leftward shift of the interventricular septum.20,21 Such hemodynamic changes may cause left ventricular dyssynchrony, and either diastolic or systolic heart failure. On the other hand, patients with congestive heart failure have also been reported in association with OSAS, with the reported prevalence up to a range of 11% to 37%.21,22 Upper airway soft tissue edema caused by congestive heart failure, and consequently increased airway resistance, may result in increased inspiratory force and upper airway collapse, which may lead to an increased risk of the development of OSAS. The frequent coexistence of congestive heart failure and OSAS may therefore make it difficult to dichotomize the impact of OSAS on cardiac dysfunction in patients with congestive heart failure.
It has been believed that OSAS has a profound negative effect on the cardiovascular system and induces a high cardiovascular event rate in the long run. Several cardiac biomarkers have been measured and have been shown to be associated with the severity of OSAS. However, the definite mechanisms of how OSAS causes cardiovascular diseases remain incompletely elucidated. Our study showed that patients with moderate-to-severe OSAS and preserved systolic function have cardiac remodeling with dilated left atrial size, decreased E/A ratio, increased A-wave velocity, and enlarged left ventricular end-diastolic volume when compared to those with mild or no OSAS. These changes could be induced by the repetitively and abruptly increased transmural gradients across the atria,43–45 ventricles, and aorta,46–49 caused by the very substantial negative intrathoracic pressure (possibly approaching -65 mm Hg) during pharyngeal collapse.50
This study showed a novel finding in that AHI in REM sleep, but not NREM sleep, was significantly associated with cardiac remodeling (dilated aortic root size by 2D echocardiography, increased left ventricular end-diastolic volume, left ventricular end-systolic volume, and left ventricular stroke volume by 3D echocardiography) and ventricular diastolic dysfunction (high A-wave velocity and low E/A ratio). The severity of OSAS becomes greater during REM sleep, partly due to a decreased respiratory muscle tone.51,52 Sympathetic activity is typically higher with intermittent discharge surges in REM sleep than in NREM sleep, and is further exacerbated with recurrent upper airway obstruction and hypoxemia.53 This increased sympathetic output in REM sleep may underlie the relationship between sleep disordered breathing, insulin resistance, and glucose intolerance.54,55 Moreover, there may be more pronounced neurohormonal perturbations and cytokine release during REM sleep caused by apnea and hypopnea, as compared to NREM sleep.56–59 All these pathophysiological changes may be the underlying mechanisms to explain why the AHI in REM sleep, but not the AHI in NREM sleep, was significantly associated with cardiovascular remodeling and ventricular diastolic dysfunction in this study. It is also possible that muscular compensatory ability decreases significantly in patient with occult cardiac dysfunction. The decreased respiratory muscular compensation along with the decreased muscle tone in REM sleep results in a higher AHI. As a result, higher AHI in REM sleep might serve as a surrogate predicting variable for cardiovascular diseases. By receiver operator characteristic curve, we identify the cutoff value ≥ 32.3/h in AHI during REM sleep in predicting the development of left ventricular diastolic dysfunction in patients with OSAS. This suggests that in patients with severe OSAS, particularly those with an AHI greater than 30/h, their cardiovascular function should be surveyed. Treatment of OSAS might reverse these adverse effects on the cardiovascular system.
Limitations
There are some limitations in the study. Although this study demonstrated the novel finding of high AHI in REM sleep, but not AHI in NREM sleep, being significantly associated with cardiovascular remodeling and ventricular diastolic dysfunction. Further research should investigate the complete mechanisms or pathways regarding OSAS contributing to cardiovascular diseases. In addition, the subject number in the control group was limited and normal non-snoring subjects were not enrolled. Due to our facility shortage and long waiting list, only patients with symptoms of sleep disordered breathing could receive the polysomnographic studies during the study period. Instead, we separated patient groups by their AHI of 15/h, which has been commonly introduced for defining significant OSAS. Furthermore, the effects of OSAS treatment should be investigated in order to further clarify the mechanisms of OSAS influencing cardiac function.
CONCLUSIONS
By using echocardiography, we found that patients with moderate to severe OSAS have a higher incidence of cardiovascular remodeling and ventricular diastolic dysfunction than those without. In addition, high AHI in REM sleep is significantly associated with cardiovascular remodeling and ventricular diastolic dysfunction and might be a potential variable to predict cardiac dysfunction and remodeling. Occult cardiac dysfunction may be present in most patients with significant OSAS, and they thus require further detailed evaluation and management.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by program grants from the Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan (CMRPG880771-880772). The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Yung-Lung Chen, M.D. and Mao-Chang Su, M.D. contributed equally to this paper. Meng-Chih Lin, M.D. and Mien-Cheng Chen, M.D. contributed equally to this paper. The authors thank the Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan for financially supporting this research under Contract number (CMRPG880771-880772).
REFERENCES
- 1.Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359:204–10. doi: 10.1016/S0140-6736(02)07445-7. [DOI] [PubMed] [Google Scholar]
- 2.Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283:1829–36. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- 3.Lavie P, Silverberg D, Oksenberg A, Hoffstein V. Obstructive sleep apnea and hypertension: from correlative to causative relationship. J Clin Hypertens (Greenwich) 2001;3:296–301. doi: 10.1111/j.1524-6175.2001.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks D, Horner RL, Kozar LF, Render-Teixeira CL, Phillipson EA. Obstructive sleep apnea as a cause of systemic hypertension. Evidence from a canine model. J Clin Invest. 1997;99:106–9. doi: 10.1172/JCI119120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ. 2000;320:479–82. doi: 10.1136/bmj.320.7233.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 7.Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–7. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 8.Gami AS, Hodge DO, Herges RM, et al. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49:565–71. doi: 10.1016/j.jacc.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 9.Hung J, Whitford EG, Parsons RW, Hillman DR. Association of sleep apnoea with myocardial infarction in men. Lancet. 1990;336:261–4. doi: 10.1016/0140-6736(90)91799-g. [DOI] [PubMed] [Google Scholar]
- 10.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 11.Arzt M, Young T, Finn L, Skatrud JB, Bradley TD. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172:1447–51. doi: 10.1164/rccm.200505-702OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 13.Janszky I, Ljung R, Rohani M, Hallqvist J. Heavy snoring is a risk factor for case fatality and poor short-term prognosis after a first acute myocardial infarction. Sleep. 2008;31:801–7. doi: 10.1093/sleep/31.6.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahlin C, Sandberg O, Gustafson Y, et al. Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up. Arch Intern Med. 2008;168:297–301. doi: 10.1001/archinternmed.2007.70. [DOI] [PubMed] [Google Scholar]
- 15.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–85. [PMC free article] [PubMed] [Google Scholar]
- 16.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–45. doi: 10.1016/S0140-6736(02)09464-3. [DOI] [PubMed] [Google Scholar]
- 18.Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health) Circulation. 2008;118:1080–111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 19.Fessler HE. Heart-lung interactions: applications in the critically ill. Eur Respir J. 1997;10:226–37. doi: 10.1183/09031936.97.10010226. [DOI] [PubMed] [Google Scholar]
- 20.Jellinek H, Krenn H, Oczenski W, Veit F, Schwarz S, Fitzgerald RD. Influence of positive airway pressure on the pressure gradient for venous return in humans. J Appl Physiol. 2000;88:926–32. doi: 10.1152/jappl.2000.88.3.926. [DOI] [PubMed] [Google Scholar]
- 21.Magder S. More respect for the CVP. Intensive Care Med. 1998;24:651–3. doi: 10.1007/s001340050640. [DOI] [PubMed] [Google Scholar]
- 22.Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160:1101–6. doi: 10.1164/ajrccm.160.4.9903020. [DOI] [PubMed] [Google Scholar]
- 23.Javaheri S, Parker TJ, Liming JD, et al. Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation. 1998;97:2154–9. doi: 10.1161/01.cir.97.21.2154. [DOI] [PubMed] [Google Scholar]
- 24.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347:1557–65. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]
- 25.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–43. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 26.Koenig W, Lowel H, Baumert J, Meisinger C. C-reactive protein modulates risk prediction based on the Framingham Score: implications for future risk assessment: results from a large cohort study in southern Germany. Circulation. 2004;109:1349–53. doi: 10.1161/01.CIR.0000120707.98922.E3. [DOI] [PubMed] [Google Scholar]
- 27.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg J, Schou M, Gustafsson F, Badskjaer J, Hildebrandt P. Prognostic threshold levels of NT-proBNP testing in primary care. Eur Heart J. 2009;30:66–73. doi: 10.1093/eurheartj/ehn525. [DOI] [PubMed] [Google Scholar]
- 29.Kapetanakis S, Kearney MT, Siva A, Gall N, Cooklin M, Monaghan MJ. Real-time three-dimensional echocardiography: a novel technique to quantify global left ventricular mechanical dyssynchrony. Circulation. 2005;112:992–1000. doi: 10.1161/CIRCULATIONAHA.104.474445. [DOI] [PubMed] [Google Scholar]
- 30.Yu CM, Sanderson JE, Marwick TH, Oh JK. Tissue Doppler imaging a new prognosticator for cardiovascular diseases. J Am Coll Cardiol. 2007;49:1903–14. doi: 10.1016/j.jacc.2007.01.078. [DOI] [PubMed] [Google Scholar]
- 31.Chami HA, Devereux RB, Gottdiener JS, et al. Left ventricular morphology and systolic function in sleep-disordered breathing: the Sleep Heart Health Study. Circulation. 2008;117:2599–607. doi: 10.1161/CIRCULATIONAHA.107.717892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koga S, Ikeda S, Nakata T, Yasunaga T, Maemura K. Effects of nasal continuous positive airway pressure on left ventricular concentric hypertrophy in obstructive sleep apnea syndrome. Intern Med. 2012;51:2863–8. doi: 10.2169/internalmedicine.51.8062. [DOI] [PubMed] [Google Scholar]
- 33.Wachter R, Lüthje L, Klemmstein D, et al. Impact of obstructive sleep apnoea on diastolic function. EurRespir J. 2013;41:376–83. doi: 10.1183/09031936.00218211. [DOI] [PubMed] [Google Scholar]
- 34.Oliveira W, Poyares D, Cintra F, et al. Impact of continuous positive airway pressure treatment on right ventricle performance in patients with obstructive sleep apnoea, assessed by three-dimensional echocardiography. Sleep Med. 2012;13:510–6. doi: 10.1016/j.sleep.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 35.Butt M, Dwivedi G, Shantsila A, Khair OA, Lip GY. Left ventricular systolic and diastolic function in obstructive sleep apnea: impact of continuous positive airway pressure therapy. Circ Heart Fail. 2012;5:226–33. doi: 10.1161/CIRCHEARTFAILURE.111.964106. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira W, Campos O, Cintra F, et al. Impact of continuous positive airway pressure treatment on left atrial volume and function in patients with obstructive sleep apnoea assessed by real-time three-dimensional echocardiography. Heart. 2009;95:1872–8. doi: 10.1136/hrt.2009.173625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oliveira W, Campos O, Bezerra Lira-Filho E, et al. Left atrial volume and function in patients with obstructive sleep apnea assessed by real-time three-dimensional echocardiography. J Am Soc Echocardiogr. 2008;21:1355–61. doi: 10.1016/j.echo.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 38.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 39.Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 40.Liu WH, Chen MC, Chen YL, et al. Right ventricular apical pacing acutely impairs left ventricular function and induces mechanical dyssynchrony in patients with sick sinus syndrome: a real-time three-dimensional echocardiographic study. J Am Soc Echocardiogr. 2008;21:224–9. doi: 10.1016/j.echo.2007.08.045. [DOI] [PubMed] [Google Scholar]
- 41.Liu WH, Guo BF, Chen YL, et al. Right ventricular outflow tract pacing causes intraventricular dyssynchrony in patients with sick sinus syndrome: a real-time three-dimensional echocardiographic study. J Am Soc Echocardiogr. 2010;23:599–607. doi: 10.1016/j.echo.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 42.Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function--a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26:357–66. [PubMed] [Google Scholar]
- 43.Otto ME, Belohlavek M, Romero-Corral A, et al. Comparison of cardiac structural and functional changes in obese otherwise healthy adults with versus without obstructive sleep apnea. Am J Cardiol. 2007;99:1298–302. doi: 10.1016/j.amjcard.2006.12.052. [DOI] [PubMed] [Google Scholar]
- 44.Romero-Corral A, Somers VK, Pellikka PA, et al. Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest. 2007;132:1863–70. doi: 10.1378/chest.07-0966. [DOI] [PubMed] [Google Scholar]
- 45.Usui Y, Takata Y, Inoue Y, et al. Severe obstructive sleep apnea impairs left ventricular diastolic function in non-obese men. Sleep Med. 2013;14:155–9. doi: 10.1016/j.sleep.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 46.Buda AJ, Pinsky MR, Ingels NB, Jr., Daughters GT, 2nd, Stinson EB, Alderman EL. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301:453–9. doi: 10.1056/NEJM197908303010901. [DOI] [PubMed] [Google Scholar]
- 47.Sampol G, Romero O, Salas A, et al. Obstructive sleep apnea and thoracic aorta dissection. Am J Respir Crit Care Med. 2003;168:1528–31. doi: 10.1164/rccm.200304-566OC. [DOI] [PubMed] [Google Scholar]
- 48.Arias MA, Garcia-Rio F, Alonso-Fernandez A, Mediano O, Martínez I, Villamor J. Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation. 2005;112:375–83. doi: 10.1161/CIRCULATIONAHA.104.501841. [DOI] [PubMed] [Google Scholar]
- 49.Floras JS, Bradley TD. Treating obstructive sleep apnea: is there more to the story than 2 millimeters of mercury? Hypertension. 2007;50:289–91. doi: 10.1161/HYPERTENSIONAHA.107.092106. [DOI] [PubMed] [Google Scholar]
- 50.Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Fogel RB, Malhotra A, Pillar G, Pittman SD, Dunaif A, White DP. Increased prevalence of obstructive sleep apnea syndrome in obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2001;86:1175–80. doi: 10.1210/jcem.86.3.7316. [DOI] [PubMed] [Google Scholar]
- 52.Tasali E, Van Cauter E, Ehrmann DA. Relationships between sleep disordered breathing and glucose metabolism in polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91:36–42. doi: 10.1210/jc.2005-1084. [DOI] [PubMed] [Google Scholar]
- 53.Fuster V, Kelly BB, Vedanthan R. Promoting global cardiovascular health: moving forward. Circulation. 2011;123:1671–8. doi: 10.1161/CIRCULATIONAHA.110.009522. [DOI] [PubMed] [Google Scholar]
- 54.Mahmood K, Akhter N, Eldeirawi K, et al. Prevalence of type 2 diabetes in patients with obstructive sleep apnea in a multi-ethnic sample. J Clin Sleep Med. 2009;5:215–21. [PMC free article] [PubMed] [Google Scholar]
- 55.Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96:1897–904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Trinder J, Kleiman J, Carrington M, et al. Autonomic activity during human sleep as a function of time and sleep stage. J Sleep Res. 2001;10:253–64. doi: 10.1046/j.1365-2869.2001.00263.x. [DOI] [PubMed] [Google Scholar]
- 57.Redwine L, Hauger RL, Gillin JC, Irwin M. Effects of sleep and sleep deprivation on interleukin-6, growth hormone, cortisol, and melatonin levels in humans. J Clin Endocrinol Metab. 2000;85:3597–603. doi: 10.1210/jcem.85.10.6871. [DOI] [PubMed] [Google Scholar]
- 58.Baharav A, Kotagal S, Gibbons V, et al. Fluctuations in autonomic nervous activity during sleep displayed by power spectrum analysis of heart rate variability. Neurology. 1995;45:1183–7. doi: 10.1212/wnl.45.6.1183. [DOI] [PubMed] [Google Scholar]
- 59.Somers VK, Dyken ME, Mark AL, Abboud FM. Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med. 1993;328:303–7. doi: 10.1056/NEJM199302043280502. [DOI] [PubMed] [Google Scholar]


