Abstract
Background:
Airway patency in both children and adults depends on the tonic and phasic activation of muscles of the tongue and pharynx supplied by the hypoglossal nerve arising at the medullary level
Methods/Patient:
We report a case of a 2-year-old who after resection of fourth ventricle anaplastic ependymoma developed severe sleep disordered breathing and tongue fasciculation.
Results:
Polysomnography showed severe obstructive sleep apnea with oxygen desaturation to 33%. Magnetic resonance imaging of the brain showed post-surgical effacement of the dorsal lateral medulla.
Conclusions:
We postulate that damage to the hypoglossal nerve at the level of the medulla contributed to the patient's severe obstructive sleep apnea. Patient was treated with tracheostomy.
Citation:
DelRosso LM; Hoque R; Gonzalez-Toledo E. Two-year-old with post-surgical hypoglossal nerve injury and obstructive sleep apnea. J Clin Sleep Med 2014;10(1):97-98.
Keywords: Hypoglossal nerve injury, sleep disordered breathing, tracheostomy, pediatric OSA
A 2-year-old girl underwent resection of a fourth ventricle anaplastic ependymoma through a posterior fossa approach at age 1. Prior to the craniotomy, the patient had neither apneas nor snoring. She required postoperative tracheostomy placement, which was removed 2 weeks prior to presentation. After tracheostomy removal the mother reported breathing pauses followed by gasping at night. The patient was admitted for observation and placed on high-flow oxygen. The sleep medicine team was consulted. The patient did not have any other past medical or surgical history.
On physical exam while awake, her blood pressure was 125/88, her heart rate 126, and her respiratory rate 24. Physical exam while awake revealed horizontal nystagmus. Her tongue showed fine fasciculation without atrophy or tongue deviation. Palate elevation was normal bilaterally. Tonsil size was 2+. Breathing was labored with increased oral secretions but no drooling or choking. She appeared to have partial airway obstruction while awake. Flexible laryngoscopy revealed an enlarged adenoid pad, normal vocal cord movements bilaterally, and airway patency. Lung exam was normal with transmitted upper airway sounds. Physical exam while asleep revealed mouth breathing, loud snoring with increased upper airway sounds secondary to secretions, and increased use of accessory breathing muscles with prolonged apneas.
Laboratory work up including comprehensive metabolic panel and complete blood count were normal. A barium swallow X-ray study showed delay in the oral and pharyngeal phase of swallowing. Diagnostic polysomnogram (PSG) was performed without high-flow oxygen at the start of the recording. Without high-flow oxygen the oxygen saturation was > 95% during wakefulness. After sleep onset, sleep disordered breathing emerged and the oxygen saturation dropped to 25% to 30%; high-flow oxygen was resumed early during the study. PSG revealed a total sleep time (TST) of 459 minutes, sleep efficiency of 93%, sleep latency of 12 minutes, and a TST apneahypopnea index of 66 events/h of sleep, all obstructive with no evidence of hypoventilation noted. The minimum oxygen saturation on high-flow oxygen during NREM sleep was 50%, and during REM sleep was 33% (Figure 1A).
Figure 1.
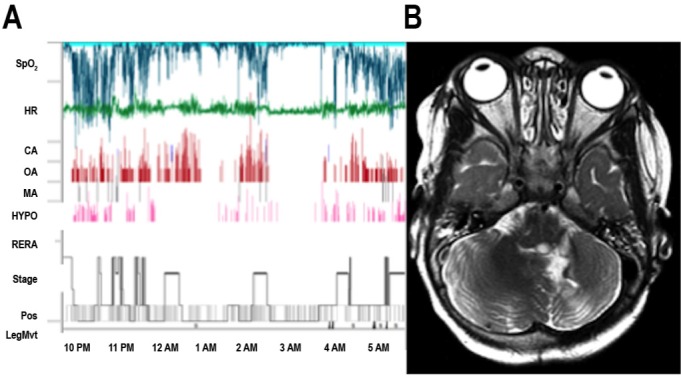
(A) Overnight polysomnography trends. Severe sleep disordered breathing with severe oxygen desaturations were noted across the night. (B) Magnetic resonance imaging of the brain, axial T2-weighted image showing post-surgical changes of the left cerebellar hemisphere associated with deformation of the dorsal-lateral medulla.
The patient underwent tonsillectomy–adenoidectomy. After extubation the patient continued to exhibit severe oxygen desaturation with labored breathing and witnessed apneas during sleep. The patient was re-intubated. Magnetic resonance imaging (MRI) of the brain revealed post-surgical changes of the left cerebellar hemisphere associated with posterior approach to the fourth ventricle and deformation of the dorsal-lateral medulla (Figure 1B).
Tongue fasciculation and severe sleep disordered breathing with difficulty clearing secretions and delayed swallowing phase on barium swallow contributed to decide the best treatment option consisted on repeat tracheostomy. The labored breathing and witnessed apneas resolved with normalization of oxygen saturation.
DISCUSSION
The mechanism of obstructive sleep apnea in children has been almost exclusively linked to peripheral obstruction due to tonsillar or adenoid hypertrophy, however the patency of the airway in both children and adults, depends on the tonic and phasic activation of muscles of the tongue and pharynx supplied by pontomedullary cranial nerves.1
Obstructive sleep apnea (OSA) is common in children with neurologic deficits from cerebral palsy, spina bifida, Chiari malformation, and achondroplasia. Compression of these cranial nerves at the foramen magnum level has been postulated as a contributing mechanism of OSA in patients with Chiari malformation or achondroplasia.2,3
The hypoglossal nerve (HN) arises from the hypoglossal nucleus in the medulla just off the midline, below the floor of the fourth ventricle and exits the medulla between the pyramid and the inferior olive. The HN innervates the genioglossus muscle (GM), considered the main tongue protruder and main pharyngeal dilator.4
HN motor neurons receive serotonergic and noradrenergic activation during wakefulness. This input is decreased at sleep onset and completely withdrawn during REM sleep, contributing to decreased GM activity and airway vulnerability during this sleep stage.5
Nerve conduction studies and electromyography studies have shown hypoglossal mononeuropathy in adult patients with OSA, suggesting that loss of hypoglossal axons may predispose to pharyngeal collapse and OSA.6 In addition, HN stimulation has been shown to improve the severity of OSA.7
In our patient, postoperative medullary insult with hypoglossal nerve (HN) damage may have resulted in centrally mediated severe obstructive sleep apnea with tongue fasciculation, which was not evident while the patient was on chronic tracheostomy. The main criteria for decannulation in patients with chronic tracheostomy are resolution of the initial insult or injury that prompted the tracheostomy; and the patient's ability to maintain a safe and adequate airway without the tracheostomy.8 Polysomnography is useful in the evaluation of these children prior to decannulation. In our patient, pharyngeal muscle weakness, presence of large adenoidal pad and enlarged tonsils could have contributed to worse OSA during REM sleep as seen in the hypnogram.
Management strategies for our patient included tonsillectomy-adenoidectomy, continuous positive airway pressure, or tracheostomy. After tonsillectomy-adenoidectomy, the family opted for tracheostomy. The patient underwent tracheostomy and remains stable.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Adelman S, Dinner DS, Goren H, Little J, Nickerson P. Obstructive sleep apnea in association with posterior fossa neurologic disease. Arch Neurol. 1984;41:509–10. doi: 10.1001/archneur.1984.04050170055017. [DOI] [PubMed] [Google Scholar]
- 2.Khatwa U, Ramgopal S, Mylavarapu A, et al. MRI findings and sleep apnea in children with Chiari I malformation. Pediatr Neurol. 2013;48:299–307. doi: 10.1016/j.pediatrneurol.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 3.DelRosso LM, Gonzalez-Toledo E, Hoque R. A three-month-old achondroplastic baby with both obstructive apneas and central apneas. J Clin Sleep Med. 2013;9:287–9. doi: 10.5664/jcsm.2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dotan Y, Golibroda T, Oliven R, et al. Parameters affecting pharyngeal response to genioglossus stimulation in sleep apnoea. Eur Respir J. 2011;38:338–47. doi: 10.1183/09031936.00125810. [DOI] [PubMed] [Google Scholar]
- 5.Horner RL. Respiratory motor activity: influence of neuromodulators and implications for sleep disordered breathing. Can J Physiol Pharmacol. 2007;85:155–65. doi: 10.1139/y06-089. [DOI] [PubMed] [Google Scholar]
- 6.Ramchandren S, Gruis KL, Chervin RD, et al. Hypoglossal nerve conduction findings in obstructive sleep apnea. Muscle Nerve. 2010;42:257–61. doi: 10.1002/mus.21690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep. 2011;34:1479–86. doi: 10.5665/sleep.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherman JM, Davis S, Albamonte-Petrick S, et al. Care of the child with a chronic tracheostomy. Am J Respir Crit Care Med. 2000;161:297–308. doi: 10.1164/ajrccm.161.1.ats1-00. [DOI] [PubMed] [Google Scholar]


