Abstract
Background:
Different types of data transmission technologies are used in remote monitoring (RM) programs. This study reports on a retrospective analysis of how participants engage, based on the type of data transfer technology used in a blood pressure (BP) RM program, and its potential impact on RM program design and outcomes.
Methods:
Thirty patients, aged 23–84 years (62 ± 14 years), who had completed at least 2 months in the program and were not participating in any other clinical trial were identified from the Remote Monitoring Data Repository. Half of these patients used wireless-based data transfer devices [wireless-based device (WBD)] while the other half used telephone modem-based data transfer devices [modem-based device (MBD)]. Participants were matched by practice and age. Engagement indices, which include frequency of BP measurements, frequency of data uploads, time to first BP measurement, and time to first data upload, were compared in both groups using the Wilcoxon–Mann–Whitney two-sample rank-sum test. Help desk call data were analyzed by Chi square test.
Results:
The frequency of BP measurements and data uploads was significantly higher in the WBD group versus the MBD group [median = 0.66 versus 0.2 measurements/day (p =.01) and 0.46 versus 0.01 uploads/day (p <.001), respectively]. Time to first upload was significantly lower in the WBD group (median = 4 versus 7 days; p =.02), but time to first BP measurement did not differ between the two groups (median = 2 versus 1 day; p =.98).
Conclusion:
Wireless transmission ensures instantaneous transmission of readings, providing clinicians timely data to intervene on. Our findings suggest that mobile-enabled wireless technologies can positively impact patient engagement, outcomes, and operational workflow in RM programs.
Keywords: chronic diseases, mobile, patient engagement, remote monitoring, self-management
Background and Introduction
Globally, the burden of chronic diseases continues to rise and places a huge strain on health systems.1 Many health care systems are now seeking innovative methods to improve the quality of care and curtail costs. In the United States, this has led to the introduction of newer payment models, such as bundled payments, accountable care organizations, and the medical home, which are performance based and more patient centric. To derive maximal benefits from shared savings, health care providers are seeking new ways to engage their patients.2 Patient engagement is important because the management of most chronic diseases requires a lifelong commitment to treatment protocols, and patients are responsible for performing majority of the care activities in the treatment plan.3 Therefore, an important goal for care providers is to implement effective interventions that improve the ability of patients to self-manage their disease.
To achieve best outcomes in chronic disease management, extensive patient education and empowerment to self-manage the disease are important measures to cultivate and sustain positive lifestyle behaviors.4 For many of these diseases, specifically diabetes and hypertension, recommended self-care practices include regular self-monitoring of blood glucose or blood pressure (BP), adhering to medication regimens, lifestyle modification, and regular visits to provider to evaluate treatment success.5 Adherence to these self-care recommendations is very critical in achieving favorable outcomes. Studies have shown that many patients struggle to initiate and sustain these self-care practices, which ultimately impacts outcomes.4–6 This makes it necessary for disease self-management programs to seek innovative methods that promote patient participation and enable patients to perform care activities with minimal effort. These demands correspond with the explosion of innovative delivery strategies facilitated by information technology that has led to the increasing use of remote monitoring (RM) in many disease management programs. Many of these programs seek to increase “connectedness” between patients and their providers by leveraging health-monitoring technologies, and innovations in mobile technologies are increasingly making this possible.7–9
Engaging patients to participate fully in a program, as designed, is critical to the success of the intervention. A complex set of factors influencing patient interactions and success in many disease management programs have been described. These factors include effect of the disease, knowledge of the disease, relationships with care providers, technology, and other program-specific factors.5 The ability to integrate each of these components effectively to function seamlessly is a determinant of the success of the program.5 A number of studies have examined the patterns of patient interaction in RM programs, but those examining the impact of the type of data transmission technology used in RM programs on patient engagement are scarce.
Different types of technology exist today to transmit data from home-based sensors and devices to clinical databases in RM programs. The type of technology is usually determined by cost, type of data to be transferred, and frequency of transmission. Mobile technologies have overtaken wired technology in terms of the timeliness, quality, and volume of data transfer. Today, they are also gaining advantage on affordability and user-friendliness. Standards for wireless data transfer include high-bandwidth Bluetooth, Zigbee, various forms of Wi-Fi, standard mobile phone voice channels, short message service, multimedia messaging service, general packet radio service, universal mobile telecommunications system, satellite, and standard radio.10,11 In this article, we explore the difference between the two most popular forms of data transmission—landline-based transmission and mobile-enabled transmission—and their effect on patient engagement, activation, and help desk support requirements.
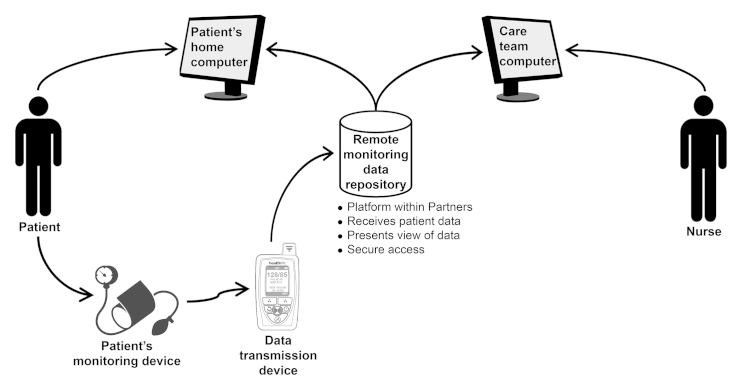
Remote Monitoring Programs at the Center for Connected Health
The Center for Connected Health (CCH) offers RM programs for chronic disease self-management in diabetes [Diabetes Connect, (DC)], hypertension (BP Connect), and heart failure (Connected Cardiac Care). The diabetes and hypertension programs are Web-based home monitoring programs that empower patients to self-manage disease and also facilitate communication between patients and their providers. As part of these “connect programs,” patients are provided commercially available electronic monitoring devices, such as BP or glucose monitors, along with a data transfer device. The data transfer device enables transmission of patients’ data from monitoring devices in their homes to the Remote Monitoring Data Repository (RMDR), a secured database housed within the Partners Healthcare firewall. Data are displayed in a user-friendly manner on a secure Web interface where patients and providers can view the processed data (Figure 1). Two types of data transfer technology are used in the DC and BP Connect programs: modem-based devices (MBDs) and wireless-based devices (WBDs; Figure 2). The transmitted data are processed in the RMDR and displayed on the secure Web portal, where patients can log on to view and monitor trends in their readings. Providers are also able to view these data to monitor patients’ progress and to provide timely feedback based on the objective data captured. This provides both the patient and the provider an opportunity to connect and collaborate on a care plan between office visits. Pelletier and coauthors12 have previously reported on our experience implementing the DC system in different outpatient practices, and patients who engaged in the program achieved an average hemoglobin A1c drop of 1.5% over a 1-year period.13 An evaluation of the BP Connect program also revealed that, overall, systolic BP decreased by 6 mmHg and diastolic BP by 2 mmHg.14 In this article, we describe our experience on how participants engage in the connect programs based on the type of data transfer technology they use and the potential impact on program design and outcomes using data from a subset of patients in the BP Connect program.
Figure 1.
Remote monitoring program.
Figure 2.

(A) Modem-based iMetrikus and (B) wireless-based Medapps.
Methods
Clinicians at different practices were provided with the connected health BP monitoring devices in order to enroll eligible patients. Patients were required to have a functioning telephone land line, Internet connection, ability to read/speak English, and ability to navigate a simple Web site. Patients with significant visual or cognitive defects were excluded. Clinicians enrolled eligible patients with uncontrolled hypertension into the program based on their clinical judgment. Enrolled patients were each given a set of the connected health BP monitoring devices consisting of a commercially available BP device (A&D UA-767PC or 767BT), a data transfer technology [Medapps (WBD) or iMetrikus (MBD); Figure 2], and set-up instructions. Participants were trained in the correct use of the BP monitors and data transfer devices. They were instructed to set up and use the devices as soon as they could, to submit at least two measurements per week, log on the Web site at least once a week, and contact the Connected Health operation support team if they experience problems with setting up or using the devices. By default, a normal range of BP was set for all participants; providers can modify the default parameters at enrollment based on a patient’s needs. Out-of-range measurements are flagged when providers log on to the Web interface. A provider was designated per practice to monitor patients’ measurements and log on the Web site at least once per week. The provider was able to reach out to the patient to provide “just-in-time” teaching or recommend changes to management plans. Patients could not initiate communications via the Web site; they would have to contact their providers through usual communication protocols.
At program inception, only the MBDs were available for use. The WBDs were introduced after the technology became available and were used initially only for patients who did not have landlines at home. However, the MBDs were not removed after the introduction of the WBDs, and both types of devices are still currently used in the program. Therefore, the time of enrollment into the program determined the type of device used by participants. The MBDs are wired and have to be connected to a standard telephone line outlet; the participant’s ability to upload data to the RMDR is restricted based on the length of the telephone cord. The BP devices (A&D UA-767PC or 767BT) are able to store measurements and connect directly to the MBDs to securely transmit data using Health Level Seven standards from the patient’s home to a data repository at Numera, a Health Insurance Portability and Accountability Act-compliant third-party vendor. These data are then relayed to the RMDR at the CCH and displayed on the BP Connect Web portal, where patients and providers can log on to view the processed data. Conversely, the WBD plugs into an electric outlet and needs to be paired with a BP device to transmit BP measurement. The BP monitor must be within the range of the WBD to wirelessly (Bluetooth) transmit data in real time. The data are also transmitted securely to the RMDR via a partial implementation of Health Level Seven standards.
A retrospective review of the RMDR was conducted between May and November 2011 to determine those currently enrolled in the program. Patients participating in pilots or clinical trials (during the review period) and those who had been in the program for less than 2 months were excluded from analysis. Participants using an MBD were matched with participants using a WBD based on practice and age. Data were collected on frequency of measurements, frequency of uploads from monitoring device to the RMDR from the data transfer device, time to first measurement, time to first data upload from data transfer device to the RMDR, and frequency of troubleshooting calls to help desk calls. All data were captured and stored in the RMDR except the help desk call data that were documented by the administrative support personnel managing the program. Demographic data were retrieved from the Partners Healthcare electronic medical records. For statistical analysis, a Wilcoxon–Mann–Whitney two-sample rank-sum test was used for nonparametric data comparison between the two groups and a Chi square test was used to compare the number of help desk calls received in both groups. Statistical significance was set at 0.05, and data were analyzed with Data Analysis and Statistical Software (STATA, version 12).
Results
Participant Characteristics
Entries of 58 participants in the database from May 1, 2011, through November 30, 2011, were reviewed for this study. After excluding patient participants in an ongoing pilot or clinical trial and those who had been in the program for less than two months, 30 participants, drawn from three practices, were selected for this matched-pair analysis. A summary of participant characteristics is included in Table 1. The mean age of the study population was 61.7 years. Program participants were predominantly white and female. Comparison of participant characteristics (Table 1) did not show significant difference between the two groups.
Table 1.
Demographics Data by Type of Device
| All participants, n = 30 | MBD, n = 15 | WBD, n = 15 | |
|---|---|---|---|
| Mean age (years) | 61.7 | 61.6 | 61.9 |
| Female gender (%) | 70 | 60 | 80 |
| White race (%) | 93.3 | 93.3 | 93.3 |
Engagement Measures
Participants who used a WBD engaged more frequently in the program. The number of measurements per day was significantly higher in the WBD group versus the MBD group (median = 0.66 versus 0.2 measurements/day; p = .01). Similarly, the number of uploads per day was significantly higher in the WBD group versus the MBD group (0.46 versus 0.01 uploads/day; p <.001, respectively). Participants who used a WBD engaged earlier in the program compared with the participants who used an MBD. Time to first upload was significantly lower in the WBD group (median = 4 versus 7 days; p = .02). Time to first BP measurement did not differ significantly between the groups (median = 2 versus 1 day; p =.98). There were more help desk calls for troubleshooting from MBD users than WBD users. Seven out of the 15 MBD users called the help desk within the first 30 days of enrollment, while only 2 WBD users called the help desks. At the end of the review period, total number of help desk calls from MBD users had increased significantly to 10 out of 15; in contrast,WBD users recorded 3 help desk calls in total. A summary of these findings is provided in Table 2.
Table 2.
Engagement Indices by Type of Technology
| MBD, n = 15 | WBD, n = 15 | p value | |
|---|---|---|---|
| Median number of BP measurements per day | 0.20 | 0.66 | 0.01 |
| Median number of data uploads per day | 0.01 | 0.46 | <0.001 |
| Median time to first data upload (days) | 7 | 4 | 0.02 |
| Median time to first BP measurement (days) | 2 | 1 | 0.98 |
| Participants who called the help desk within 30 days of enrollment (%) | 46.7 | 13.3 | 0.05 |
| Participants who called the help desk within review period (%) | 66.7 | 20 | 0.01 |
Discussion
This matched-pair analysis provides data to show that data transmission technologies may potentially create barriers to patient engagement in RM programs. Key success factors for wireless transmission through a WBD include ease-of-use (due to fewer steps required to upload data), real-time transmission of data (which makes it available to view online almost immediately), and increased device portability within patients’ homes.
Wireless-enabled transmission devices allowed for automatic, wireless pairing of sensors to their base station. As a result, patients were not required to set it up or push any buttons. This resulted in the significantly fewer help desk calls received, as well as significantly lower time to first upload. Participants were able to use their monitoring devices anywhere within a particular range of the WBD; the data were uploaded immediately and available for viewing by both patients and providers. Real-time data transmission facilitating patient–provider communication coupled with ease of data upload encouraged our patients to measure their BP even more regularly. This led to a significantly higher number of BP measurements. The wired MBD restricts user positioning to upload within the length of the telephone line. Even patients who measure regularly do not upload immediately after taking their readings, as demonstrated by the disproportionate frequencies of BP measurements and data upload by the MBD. This may potentially lead to delays in feedback for the observed measurements. Our findings demonstrate that the less obtrusive the upload process, the better the level of patient engagement. As a program design measure, this is extremely critical, as it provides clinicians timely data to intervene on. We posit that the increased feedback resulting from this instantaneous upload leads to better engagement in the program, as demonstrated by the significantly higher number of measurements in the WBD group. Due to the first-time setup requirement that patients measure their BP during enrollment and initial excitement for the system, it is not surprising that time to first measurement did not differ in both groups. The challenge of our program has always been continuous engagement. Therefore, the goal of effective mobile applications is to be able to sustain this initial interest and to help users continually and consistently engage in the program. We also observed that MBD users were more likely to call the help desk for troubleshooting than WBD users. Many of these calls relate to problems with the telephone line setup and can potentially increase operational burden.
Provider engagement was not measured in this analysis. An evaluation of the DC program revealed that hemoglobin A1c decrease correlated with provider engagement that was measured by frequency of provider logins to the Diabetes Connect Web site.13 These provider logins usually generate feedback based on observed measurements. The feedback factor has been measured extensively in our RM programs in diabetes and heart failure. For many patients, there’s an increased awareness of their health, and knowing that care providers monitor their measurements keeps them motivated and engaged in the program.12,13,15–17 Similarly, a qualitative analysis to understand patients’ experiences with various components of a home BP monitoring program with a focus on technology also suggests that bidirectional conversations between patients and providers facilitate the patient’s increased understanding of the disease and promote patient empowerment, critical factors to the success of a hypertension management program.18
This study is not without limitations, notably, the small sample size and method of subject selection, which has the potential for selection bias. Subjects were selected from three sites that had a sizeable number of people using both types of technologies in order to achieve an even match. Since this analysis was based on a review of a RM database, which was not integrated with the electronic medical records, we had limited baseline information about participants, which may influence the pattern of interactions in the program. Additionally, a prospective randomized controlled trial would have been ideal to test our hypothesis, but the matched-pair design also allowed for potential confounders to be equally distributed across the two groups. Provider engagement, which can also influence patient engagement, was not measured in this study but has been well described in the Diabetes Connect program referenced earlier. Lastly, since this study compares only limited types of data transfer technologies used in patients with hypertension, it limits the generalizability of our findings to only these two forms of data transfer technology. More research is needed to evaluate newer technologies.
Conclusion
Mobile technologies are becoming more affordable and acceptable, especially in low-resource settings,9,10 making it an opportune time to widely adopt mobile technology to better engage patients in the self-management of chronic diseases. Although we understand that the field of mobile technologies for use in RM programs is rapidly changing, with new inventions entering the market on a regular basis, it may be difficult to keep up with the latest technologies. The cost of the new technologies may also be a limiting factor. Despite these challenges, adopting the “right” technology should be a priority, as it could potentially optimize patient engagement. In our experience, wired technology can be difficult for patient monitoring, because it restricts the range of a patient’s health monitoring activities to the location of the transfer technology or the length of connecting wire. This may negatively impact patients’ participation in RM programs. In conclusion, our findings suggest that the type of technology used in RM programs can potentially impact patient engagement, operational workflow processes, and, consequently, program end points. Therefore, as care providers seek to improve outcomes and curtail costs of disease management, we recommend that RM program designers actively look to embrace technologies that promote patient engagement to self-manage chronic diseases.
Acknowledgments
Acknowledgments:
We acknowledge Kurleigh Henry, at the CCH, for his invaluable contribution during the data extraction process.
Glossary
- (BP)
blood pressure
- (CCH)
Center for Connected Health
- (DC)
Diabetes Connect
- (MBD)
modem-based device
- (RM)
remote monitoring
- (RMDR)
Remote Monitoring Data Repository
- (WBD)
wireless-based device
Funding:
This work was supported by the Verizon Foundation.
References:
- 1.World Health Organization . World health statistics 2012. Geneva: World Health Organization; 2012. Non-communicable diseases: a major health challenge of the 21st century; pp. 34–36. [Google Scholar]
- 2.Burns J. Patient engagement. Manag Care. 2012;21(6):16–21. [PubMed] [Google Scholar]
- 3.Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, Hsu J, Martiniuk A, Celletti F, Patel K, Adshead F, McKee M, Evans T, Alwan A, Etienne C. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376(9754):1785–1797. doi: 10.1016/S0140-6736(10)61353-0. [DOI] [PubMed] [Google Scholar]
- 4.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 5.Bosworth HB, Powers BJ, Oddone EZ. Patient self-management support: novel strategies in hypertension and heart disease. Cardiol Clin. 2010;28(4):655–663. doi: 10.1016/j.ccl.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, Haass M. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87(3):235–241. doi: 10.1136/heart.87.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stuckey M, Fulkerson R, Read E, Russell-Minda E, Munoz C, Kleinstiver P, Petrella R. Remote monitoring technologies for the prevention of metabolic syndrome: the diabetes and technology for increased activity (DaTA) study. J Diabetes Sci Technol. 2011;5(4):936–944. doi: 10.1177/193229681100500417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal S, Lau CT. Remote health monitoring using mobile phones and web services. Telemed J E Health. 2010;16(5):603–607. doi: 10.1089/tmj.2009.0165. [DOI] [PubMed] [Google Scholar]
- 9.Boland P. The emerging role of cell phone technology in ambulatory care. J Ambul Care Manage. 2007;30(2):126–133. doi: 10.1097/01.JAC.0000264602.19629.84. [DOI] [PubMed] [Google Scholar]
- 10.Clifford GD, Clifton D. Wireless technology in disease management and medicine. Annu Rev Med. 2012;63:479–492. doi: 10.1146/annurev-med-051210-114650. [DOI] [PubMed] [Google Scholar]
- 11.Nikita KS, Lin JC, Fotiadis DI, Waldmeyer MT. Editorial: special issue on mobile and wireless technologies for healthcare delivery. IEEE Trans Biomed Eng. 2012;59(11):3083–3089. doi: 10.1109/TBME.2012.2212775. [DOI] [PubMed] [Google Scholar]
- 12.Pelletier AC, Jethwani K, Bello H, Kvedar J, Grant RW. Implementing a web-based home monitoring system within an academic health care network: barriers and facilitators to innovation diffusion. J Diabetes Sci Technol. 2011;5(1):32–38. doi: 10.1177/193229681100500105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jethwani K, Ling E, Mohammed M, Myint-U K, Pelletier A, Kvedar JC. Diabetes connect: an evaluation of patient adoption and engagement in a web-based remote glucose monitoring program. J Diabetes Sci Technol. 2012;6(6):1328–1336. doi: 10.1177/193229681200600611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agboola S, Myint-U K, Kvedar J, Jethwani K. 2012 Home blood pressure monitoring program improves management of hypertension Poster presented at: Quality Care and Outcomes Research in Cardiovascular Disease and Stroke 2012 Scientific Sessions, May 9-11, Atlanta, GA. [Google Scholar]
- 15.Watson AJ, Kvedar JC, Rahman B, Pelletier AC, Salber G, Grant RW. Diabetes connected health: a pilot study of a patient- and provider-shared glucose monitoring web application. J Diabetes Sci Technol. 2009;3(2):345–352. doi: 10.1177/193229680900300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kulshreshtha A, Kvedar JC, Goyal A, Halpern EF, Watson AJ. Use of remote monitoring to improve outcomes in patients with heart failure: a pilot trial. Int J Telemed Appl. 2010;2010:870959. doi: 10.1155/2010/870959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watson AJ, Singh K, Myint-U K, Grant RW, Jethwani K, Murachver E, Harris K, Lee TH, Kvedar JC. Evaluating a web-based self-management program for employees with hypertension and prehypertension: a randomized clinical trial. Am Heart J. 2012;164(4):625–631. doi: 10.1016/j.ahj.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 18.Lambert-Kerzner A, Havranek EP, Plomondon ME, Albright K, Moore A, Gryniewicz K, Magid D, Ho PM. Patients’ perspectives of a multi-faceted intervention with a focus on technology: a qualitative analysis. Circ Cardiovasc Qual Outcomes. 2010;3(6):668–674. doi: 10.1161/CIRCOUTCOMES.110.949800. [DOI] [PubMed] [Google Scholar]