Abstract
Background:
Increasingly various technologies are being tested to deliver behavioral health care. Delivering services via videoconferencing shows promise. Given that the patient–provider relationship is a strong predictor of patient adherence to medical regimens, addressing relationship quality when services are not delivered face-to-face is critical. To that end, we compared the therapeutic alliance when behavioral health care was delivered to youth with poorly controlled type 1 diabetes mellitus (T1DM) and their caregivers in-clinic with the same services delivered via Internet-based videoconferencing (i.e., Skype™).
Methods:
Seventy-one adolescents with poorly controlled T1DM (hemoglobin A1c ≥9%) and one of their caregivers received up to 10 sessions of a family-based behavioral health intervention previously shown to improve adherence to diabetes regimens and family functioning; 32 were randomized to the Skype condition. Youth and caregivers completed the working alliance inventory (WAI), a 36-item measure of therapeutic alliance, at the end of treatment. Additionally, the number of behavioral health sessions completed was tracked.
Results:
No significant differences in WAI scores were found for those receiving behavioral health care via Skype versus in-clinic. Youth WAI goal and total scores were significantly associated with the number of sessions completed for those in the clinic group.
Conclusion:
Behavioral health can be delivered to youth with T1DM via Internet-based videoconferencing without significantly impacting the therapeutic relationship. Thus, for those adolescents with T1DM who require specialized behavioral health care that targets T1DM management, Internet-based teleconferencing represents a viable alternative to clinic-based care.
Keywords: adherence, adolescence, behavioral health, telemedicine
Introduction
Research has consistently shown that youth with type 1 diabetes mellitus (T1DM) experience a notable and clinically meaningful decrease in self-management and adherence to the prescribed medical regimen during adolescence,1 which is associated with poor metabolic control. While numerous factors affect this process, parent–adolescent and family functioning variables are important in predicting poor adherence. Specifically, cross-sectional and prospective studies show that family conflict, parent–adolescent communication, and family problem solving relate to adolescents’ diabetes outcomes.2–7
Given the role of family interaction patterns in adherence and metabolic control among adolescents with T1DM, the effectiveness of family-based psychosocial interventions have been evaluated. Behavioral family systems therapy (BFST) is the most researched behavioral intervention for improving adherence among youth with diabetes. Behavioral family systems therapy is a manualized, structured intervention that includes four components: problem solving training, communication skills training, cognitive restructuring, and family systems interventions. Behavioral family systems therapy has been shown to improve family communication and problem solving compared with standard medical care.8–10 Further, a modified version of BFST specifically focused on diabetes care [behavioral family systems therapy for diabetes (BFST-D)] significantly improved glycemic control, treatment adherence, and diabetes-related family conflict among adolescents with T1DM, compared with standard medical care or supportive therapy;11–13 effects were greater for youth in very poor metabolic control.11 A home-based version of BFST-D has also been shown to produce statistically and clinically meaningful improvements in family functioning and hemoglobin A1c (HbA1c) in youth with chronically poor glycemic control.14,15
Unfortunately, patient access to evidence-based behavioral health treatments such as BFST-D is limited by numerous factors (e.g., paucity of well-trained providers, difficulties arranging weekly visits, travel costs, and time);13,16 access to behavioral health care can be even more difficult for those living in rural areas.17 As a result, researchers are increasingly testing the use of technology to deliver mental and behavioral health care, or telemental health care.18
Telemental health can be defined as the use of electronic communications technology to eliminate or reduce geographic barriers to receiving psychiatric and other mental health services. Existing evidence supports the effectiveness of telemental health to improve psychosocial functioning in a variety of domains.19,20 While there is a growing body of research on telemental health services, most studies are preliminary or largely descriptions of feasibility and usage rather than well-controlled randomized clinical trials of effectiveness.20 Further, limited research on telemental health has been completed with youth and/or families,20 and thus much remains unknown regarding the feasibility and effectiveness of this method of delivering mental health services to youth and families.
Data are beginning to emerge regarding the use of Internet-based psychosocial interventions for youth with chronic health conditions, showing positive results.21,22 However, most studies focus on youth with asthma, with published research on youth with diabetes being virtually nonexistent. Studies that have focused on delivering behavioral telehealth for youth with diabetes are beginning to emerge, and thus far, preliminary results have largely been disseminated via professional presentation. Whittemore and coauthors23 demonstrated high consent rates when enrolling youth with T1DM into an Internet-based psycho-educational treatment, though retention rates were lower for ethnic minority and low-income participants. Mulvaney and coauthors24 showed a high participation rate of adolescents with T1DM in an Internet-based multimedia problem solving program and that participation was positively associated with improved diabetes problem solving skills. These preliminary findings support continued emphasis on dissemination of treatments via technology.
An important predictor of psychotherapeutic treatment outcome is the relationship between the patient and therapist, or therapeutic alliance.25,26 In particular, patient-reported therapeutic alliance appears more predictive of treatment outcome than clinician report.27 To date, the patient–provider working relationship appears similar when comparing traditional face-to-face services provided to adults against telemental health psychiatric and psychological services delivered via videoconferencing.28
Scant attention has been paid to the role of therapeutic alliance in pediatric/child and/or family telemental health or behavioral health services. A strong working alliance has been shown when delivering mental health services to child–parent dyads via the telephone.29 Further, overall therapeutic alliance was high in an investigation of videoconferencing-based family counseling for adolescents with epilepsy living in rural areas;30 however, those receiving treatment via home-based videoconferencing reported significantly lower therapeutic alliance than those receiving face-to-face care. To date, no research exists that has evaluated the association between therapeutic alliance and treatment engagement (e.g., attending scheduled sessions) or outcome in pediatric behavioral health care.
In the current study, we report on the working alliance between youth with T1DM and their parents and therapists when delivering BFST-D via freely available Internet-based videoconferencing (i.e., SkypeTM) versus clinic-based care. Specifically, we investigated whether youth- and parent-reported therapeutic alliance differed across experimental conditions. Drawing on literature from telemental health services with adults,28 we hypothesized no difference in therapeutic alliance across experimental conditions.
Further, we tested the association between the number of treatment sessions completed and youth- and parent-reported therapeutic alliance. As predicted, preliminary results from the current trial of BFST-D suggest an association between the number of therapeutic sessions completed and treatment outcome.31 Therefore, understanding the factors associated with continuation in treatment is important. We hypothesized that youth- and parent-reported therapeutic alliance would be positively associated with the number of prescribed BFST-D treatment sessions completed.
Methods
Participants
Seventy-one adolescents with poorly controlled T1DM and one parent/legal guardian who participated in a randomized controlled trial examining the effectiveness BFST-D delivered via Skype versus via clinic-based delivery are included in this analysis; 32 were randomized to the Skype condition. See Figure 1 for the Consolidated Standards of Reporting Trials statement; note the sample in this study included only those for whom data on working alliance were available from post-treatment assessment. The sample of youth included in this analysis was largely Caucasian (n = 63); the remainder were biracial/multiracial (n = 4), Hispanic (n = 2), Native American (n =1), and Hawaiian/Pacific Islander (n = 1). See Table 1 for additional demographic information. No statistically significant differences between experimental groups were found for any demographic variables of interest.
Figure 1.
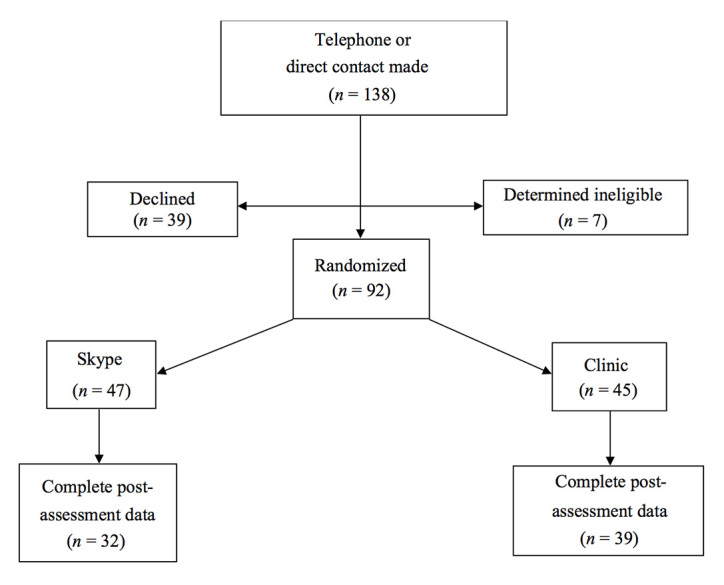
Consolidated Standards of Reporting Trials statement that details youth recruitment.
Table 1.
Demographic Variables of Participants by Experimental Conditiona n
| Clinic | Skype | n | |
|---|---|---|---|
| Age of youth | 15.2 (1.8) | 14.9 (1.9) | −0.034 |
| Sex of youthb | Male = 23 Female = 16 | Male = 19 Female = 13 | 0.001 |
| Hollingshead index of social status | 37.12 (10.7) | 37.37 (11.97) | −0.071 |
| Duration of diabetes | 7.69 (3.67) | 6.36 (3.26) | 1.56 |
| Baseline HbA1c | 10.91 (1.74) | 10.99 (1.63) | −0.202 |
Numbers in parentheses represent standard deviations.
Pearson χ2 test was used to test the difference between groups regarding distribution of sex of youth.
Measures
A demographic information form was used to gather information about patient and family demographic (e.g., youth age, family composition, race/ethnicity) and disease (e.g., date and length of diagnosis) variables of interest. Information needed to calculate the Hollingshead index of social status was also gathered via this form. For this index, scores range from 0–60, with a score of 30 representing lower-middle class; lower scores indicate lower socioeconomic status.
Baseline metabolic control was measured via HbA1c assay taken within 2 weeks of initiating treatment.
Parent–adolescent conflict was assessed using two measures. First, the parent and youth versions of the Conflict Behavior Questionnaire-20 (CBQ-20)32 were used to assess general conflict in the relationship. The CBQ-20, originally a 75-item form, measures perceived communication–conflict behavior at home. The CBQ-20 is now a 20-item version that contains items that maximally discriminate between distressed and nondistressed families by asking respondents to indicate whether statements are true or false over the previous 2 weeks. Higher scores indicate greater conflict. In the current investigation, the CBQ-20 demonstrated excellent internal consistency based on both youth (α = 0.845) and parent (α = 0.873) report.
Second, diabetes-management-specific conflict was measured using complimentary parent and youth versions of the Diabetes Responsibility and Family Conflict Scale (DRFC);33 only the item related to direct management tasks (nine items) were used.34 Higher scores indicate greater conflict during the preceding month. Missing items scores were imputed using the mean score from the remainder of the nine items. In the current investigation, the nine-item DRFC demonstrated excellent internal consistency based on both youth (α = 0.775) and parent (α = 0.764) report.
The Working Alliance Inventory (WAI)35 is a 36-item report form that provides an overall total score (range 36–252) as well as three subscale scores [i.e., task, extent to which a client and therapist agree on how to reach goals (range 12–84); bond, extent to which a client and therapist have established trust, understanding, and confidence (range 12–84); goal, extent to which the client and therapist agree on outcomes and targets of intervention (range 12–84)]; higher scores are indicative of more positive working alliance.35 Missing item responses were imputed using the mean score of items in each specific factor (i.e., task, bond, goal); these scores were also used to calculate the total score. In the current investigation, the WAI demonstrated excellent internal consistency based on both youth (α = 0.927) and parent (α = 0.930) report.
Additionally, the total number of sessions completed was calculated for each participant.
Procedures
All study procedures were approved by the institutional review board at the authors’ institution. Youth between the ages of 12 and 19 years (at enrollment) with T1DM in poor metabolic control (i.e., HbA1c ≥ 9.0%) and at least one parent/legal guardian were recruited (via referral by medical provider, identification by study staff via review of medical chart, or self-referral) from two multidisciplinary, comprehensive hospital-based diabetes care centers located in an urban Pacific Northwest city. Legal guardians provided consent, and all youth provided assent. Upon enrollment, participants were randomized to receive up to 10 sessions lasting 1 to 1.5 h of BFST-D within a 12-week time frame either via Skype or via traditional clinic-based visits; therapists followed the BFST-D manual used in previous trials.36 Therapists included one psychology intern and two doctoral level therapists. All therapists received preparatory training and weekly supervision from Michael A. Harris, who has extensive experience implementing BFST-D. Randomization procedures were used to ensure equivalent distribution of cases (i.e., Skype versus clinic) with each therapist. Pretreatment contact between the therapist and family occurred via telephone only to arrange appointment schedules. During treatment, all participants received a telephone call from the study coordinator reminding them about their scheduled appointments 3–4 days prior. “No show” participants were called weekly to reschedule their missed appointment. They were reminded weekly until they participated or until the 12-week treatment period ended.
Participants completed a variety of measures, including those analyzed in this study, prior to, immediately after, and 3 months following treatment. The WAI was completed after session 5 and at post-treatment. For those in the Skype condition, the WAI was completed at home in hard copy after session 5 and returned to the researchers via a self-addressed stamped envelope; post-treatment WAIs were completed during an in-person assessment that was administered by a research assistant or study investigator (not the therapist) for all participants, regardless of condition. Only the post-treatment WAI scores are used in the current analyses.
Results
Working Alliance Inventory Between-Group Comparisons
To test the hypothesis related to whether therapeutic alliance differed across experimental conditions, WAI task, bond, goal, and total scores based on youth and parent report were compared. Results of an independent sample t-test revealed no significant differences in WAI scores across those receiving BFST-D via Skype versus in-clinic (Table 2).
Table 2.
Comparison of Working Alliance Inventory Subscale and Total Scores Across Conditions
| Clinic | Skype | t | |
|---|---|---|---|
| Youth WAI | |||
| Task | 70.84 | 72.03 | 0.675 |
| Bond | 68.85 | 71.03 | 0.970 |
| Goal | 71.40 | 72.81 | 0.641 |
| Total | 210.78 | 215.88 | 0.834 |
| Parent WAI | |||
| Task | 72.79 | 75.31 | 0.429 |
| Bond | 72.79 | 73.89 | 0.674 |
| Goal | 75.00 | 75.93 | 0.584 |
| Total | 221.62 | 224.84 | 0.528 |
We also explored whether parent and youth reports on the WAI differed, again conducting independent sample t-tests. For all WAI subscale and total scores, youth report was significantly lower than parent report (Table 3).
Table 3.
Comparison of Youth versus Parent Report on the Working Alliance Inventory
| WAI factor | Youth | Parent | t | p |
| Task | 71.21 | 74.49 | −2.28 | 0.024 |
| Bond | 69.83 | 73.15 | −2.28 | 0.024 |
| Goal | 72.04 | 75.42 | −2.45 | 0.015 |
| Total | 213.08 | 223.07 | −2.53 | 0.012 |
Correlation among Pretreatment Demographic, Personal, and Parent–Adolescent Variables and Sessions Completed
Completing treatment sessions can be affected by a number of variables. Therefore, before testing our primary hypo-thesis, we investigated the association between specific personal and demographic variables (i.e., gender, youth age, duration of T1DM, ethnicity), pretreatment metabolic control (i.e., HbA1c), and pretreatment general (CBQ-20) and diabetes-specific (DRFC) parent–adolescent conflict. Only pretreatment HbA1c was significantly associated with the number of sessions completed (r = −0.318, p = .002). Therefore, all analyses investigating the association between WAI and the number of sessions completed were conducted controlling for pretreatment HbA1c.
Correlation between Working Alliance Inventory Scores and Sessions Completed
To test our second hypothesis, we examined the association between reported therapeutic alliance (i.e., WAI subscale and total scores) and the number of BFST-D sessions completed by conducting two-tailed partial correlation controlling for pretreatment HbA1c. First, we tested the association with the entire sample combined; the mean number of sessions completed for all participants was 7.39 (range 1–10). No significant associations between WAI task, bond, goal, or total scores were obtained based on either youth or parent report (all p > .1).
Second, given our interest in whether method of treatment delivery affected outcomes of interest, we investigated whether associations between WAI scores and the number of sessions differed for each experimental group. Those in the Skype group completed a mean of 7.03 sessions (range 1–10). Again using partial correlation controlling for pretreatment HbA1c, no significant associations between number of sessions completed and WAI subscale and total scores were found based on both youth and parent report for those in the Skype group (all p > .2). For the clinic-based group, the mean number of sessions completed was 7.56 (range 1–10). Again, no significant partial correlations were found between sessions completed and parent-reported WAI scores (all p > .2). In contrast, the number of sessions of BFST-D completed and youth WAI goal (r = 0.443, p = .005) and total (r = 0.322, p = .048) scores in the clinic group were significantly positively associated while controlling for pretreatment HbA1c, which represent strong to moderate positive relationships, respectively.
Ancillary Analyses
Post hoc exploratory analyses of possible mediation effects were conducted using criteria outlined by Baron and Kenny.37 Two possible models were hypothesized: (1) working alliance mediates the relationship between number of sessions completed and outcome (HbA1c) and (2) the number of sessions competed mediates the relationship between working alliance and outcome (HbA1c). For the first model, further exploration ceased at step 3 due to a lack of identifying a significant relationship between the proposed mediator (working alliance total or subscale scores) and outcome (HbA1c). For the second model, exploration ceased at step 1 due to the same lack of relationship between working alliance and HbA1c.
Discussion
This study is the first randomized controlled trial to examine therapeutic alliance when delivering BFST-D to youth with poorly controlled T1DM via Skype. Results showed that patient–provider therapeutic alliance was similar to clinic-based care based on both youth and parent report and largely unaffected by the use of videoconferencing technology. Youth randomized to the clinic-based condition who completed more treatment sessions reported a greater agreement with their therapist on therapeutic targets and expected outcomes (WAI goal) and overall more positive working alliance (WAI total). The direction of the relationship is impossible to discern in this study, but it may be that the better alliance contributed to patients completing a larger number of sessions. This finding is in contrast to those in the Skype condition, where the number of sessions completed was not related to the quality of youth-reported working alliance. This difference may have occurred because the in-person interaction created a more personal patient/provider atmosphere that was more directly related to return than during videoconferencing and is consistent with other research demonstrating that working alliance may be more predictive of outcomes when providing face-to-face care.38 However, the relationship was strong across experimental conditions, which is consistent with previous research examining the impact of telehealth on the therapeutic relationship between patients and providers.39–41
Very few telemental health studies have used a randomized controlled design.42 The present study is the first such trial to examine the therapeutic relationship when delivering a family-based intervention (BFST-D) to improve diabetes management. As such, the present study is an important contribution to the extant literature. Findings offer further evidence regarding the ability to establish a positive working relationship while delivering care via technology and support integration of such a treatment delivery approach into clinical care. However, using telehealth to engage in widespread clinical dissemination of evidence-based treatments such as BFST-D across state lines may be premature, because current licensing laws in most states dictate that practice occurs only within the state of licensure; thus treatment delivery cannot legally occur across state lines unless the practitioner is licensed in both jurisdictions.
Much of the existing research on the use and effectiveness of telehealth, including telemental health, via video-conferencing has relied on closed circuit technology. While findings are generally positive, use of this technology greatly hampers treatment dissemination and accessibility, as it requires expensive hardware and staff support not available in many communities. Further, it typically requires designating a centralized location to which people within the distant community must come to receive services; while this is better than traveling (presumably) longer distances to receive care in person, it nonetheless requires designated community resources and significant coordination of care. Internet-based videoconferencing such as that used in the current investigation further diminishes barriers to effective behavioral health care for youth with diabetes.
Fortunately, advances in computer and Internet technology have led to increased access to videoconferencing technology. Personal computers are now typically equipped with video cameras, and if not, aftermarket cost for such products are generally affordable. Further, multiple low-cost or free programs, such as Skype, are available for download that allow consumers to engage in real-time conversations that include both audio and video feeds. Thus, telehealth services need not rely on sophisticated and expensive technology. Further, access to broadband Internet continues to increase in the United States,43 and there is an increase in legislation supporting reimbursement for telehealth services. Together, these changes to the landscape highlight the importance of investigating how technology intersects with the delivery of behavioral health care. Our findings support that not only is it possible to deliver services via freely available videoconferencing technology, but the patient–provider working relationship remains intact when doing so.
There are several limitations to our study. Failure to detect statistically significant differences in outcome does not necessarily indicate equivalence of outcome.44,45 In this study, small differences in WAI scores across groups were found; thus it is possible that insufficient power existed to detect statistically significant differences. Therefore, there is a possibility of type II error. Importantly, while nonsignificant, observed differences in WAI scores were always in the direction of those receiving care via Skype reporting higher working alliance. As a related limitation, we did not test clinical relevance of the differences. Additionally, it may be that questionnaires specific to assessing working alliance when care is provided via videoconferencing are needed to identify factors unique to the intervention delivery method. While versions of the WAI have been used in previous telehealth research,29,38,46 it has yet to be investigated when delivering care via Skype, and thus it may or may not capture important dimensions of the working relationship when care is delivered via this technology.
Conclusions
Despite limitations, our study adds to growing evidence supporting the ability to deliver care via videoconferencing technology, improving and extending the extant literature by testing the delivery of care via freely available Internet videoconferencing. Further, suggestions for future research emerge from this investigation. First, testing the association between working alliance when providing behavioral telehealth for adolescents with poorly controlled T1DM and for associated improvements in adherence and glycemic control is warranted. While working alliance has been shown to strongly predict treatment outcome in traditional face-to-face care,25,26 the association when providing telehealth is mixed, with some research suggesting positive associations46 and others failing to identify such a link.38,47 Whether these differences are due to variations in measures used, treatment delivery methods (e.g., telephone, video-conferencing, online psycho-education), or conditions/outcomes targeted is unclear and warrants further study. Second, future research should address what conditions and which populations of youth with diabetes (e.g., T1DM versus T2DM) could benefit most from behavioral telehealth in improving diabetes management. Finally, there are many videoconferencing platforms (e.g., Skype, FaceTime) and devices supporting videoconferencing (e.g., cell phones, tablets, laptops) currently on the market. Thus future research examining the relative effectiveness and/or usability of behavioral telehealth across various hardware and software platforms would inform clinical practice such that youth with diabetes benefit the most in improved diabetes self-care.
Acknowledgments
The authors acknowledge Bruce Boston’s support of this project; Beth Hirschfield’s efforts for patient recruitment and data collection; and Lisa Shimomaeda, Kevin Shimomaeda, and Jonah Harris for their efforts with data entry.
Glossary
- (BFST)
behavioral family systems therapy
- (BFST-D)
behavioral family systems therapy for diabetes
- (CBQ-20)
conflict behavior questionnaire-20
- (DRFC)
diabetes responsibility and family conflict scale
- (HbA1c)
hemoglobin A1c
- (T1DM)
type 1 diabetes mellitus
- (WAI)
working alliance inventory
Funding
This work was funded by the American Diabetes Association.
References
- 1.Johnson SB, Kelly M, Henretta JC, Cunningham WR, Tomer A, Silverstein JH. A longitudinal analysis of adherence and health status in childhood diabetes. J Pediatr Psychol. 1992;17(5):537–553. doi: 10.1093/jpepsy/17.5.537. [DOI] [PubMed] [Google Scholar]
- 2.Anderson BJ, Miller JP, Auslander WF, Santiago JV. Family characteristics of diabetic adolescents: telationships to metabolic control. Diabetes Care. 1981;4(4):586–594. doi: 10.2337/diacare.4.6.586. [DOI] [PubMed] [Google Scholar]
- 3.Bobrow ES, AvRuskin TW, Siller J. Mother-daughter interaction and adherence to diabetes regimens. Diabetes Care. 1985;8(2):146–151. doi: 10.2337/diacare.8.2.146. [DOI] [PubMed] [Google Scholar]
- 4.Gustafsson PA, Cederblad M, Ludvigsson J, Lundin B. Family interaction and metabolic balance in juvenile diabetes mellitus. A prospective study. Diabetes Res Clin Pract. 1987;4(1):7–14. doi: 10.1016/s0168-8227(87)80027-x. [DOI] [PubMed] [Google Scholar]
- 5.Hauser ST, Jacobson AM, Lavori P, Wolfsdorf JI, Herskowitz RD, Milley JE, Bliss R, Wertlieb D, Stein J. Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up: II. Immediate and long-term linkages with the family milieu. J Pediatr Psychol. 1990;15(4):527–542. doi: 10.1093/jpepsy/15.4.527. [DOI] [PubMed] [Google Scholar]
- 6.Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Lovinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. J Consult Clin Psychol. 1994;62(3):603–610. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- 7.Wysocki T. Associations among teen-parent relationships, metabolic control, and adjustment to diabetes in adolescents. J Pediatr Psychol. 1993;18(4):441–452. doi: 10.1093/jpepsy/18.4.441. [DOI] [PubMed] [Google Scholar]
- 8.Wysocki T, Harris MA, Greco P, Bubb J, Danda CE, Harvey LM, McDonell K, Taylor A, White NH. Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol. 2000;25(1):23–33. doi: 10.1093/jpepsy/25.1.23. [DOI] [PubMed] [Google Scholar]
- 9.Wysocki T, Miller K, Greco P, Harris MA, Harvey LM, Taylor A, Elder-Danda C, McDonell K, White NH. Behavior therapy for families of adolescents with diabetes: effects on directly observed family interactions. Behav Ther. 1999;30:496–515. [Google Scholar]
- 10.Wysocki T, Greco P, Harris MA, Bubb J, White NH. Behavior therapy for families of adolescents with diabetes: maintenance of treatment effects. Diabetes Care. 2001;24(3):441–446. doi: 10.2337/diacare.24.3.441. [DOI] [PubMed] [Google Scholar]
- 11.Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, Mauras N, White NH. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31(9):928–938. doi: 10.1093/jpepsy/jsj098. [DOI] [PubMed] [Google Scholar]
- 12.Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, White NH. Randomized, controlled trial of behavioral family systems therapy for diabetes: maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008;39(1):33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Mauras N, White NH. Randomized trial of behavioral family systems therapy for diabetes: maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30(3):555–560. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]
- 14.Harris MA, Freeman KA, Beers M. Family therapy for adolescents with poorly controlled diabetes: initial test of clinical significance. J Pediatr Psychol. 2009;34(10):1097–1107. doi: 10.1093/jpepsy/jsp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris MA, Mertlich D. Piloting home-based behavioral family systems therapy for adolescents with poorly controlled diabetes. Child Health Care. 2003;32:65–79. [Google Scholar]
- 16.Devineni T, Blanchard EB. A randomized controlled trial of an internet-based treatment for chronic headache. Behav Res Ther. 2005;43(3):277–292. doi: 10.1016/j.brat.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Jerome LW, Zaylor C. Cyberspace: creating a therapeutic environment for telehealth applications. Prof Psychol Res Pract. 2000;31:478–483. [Google Scholar]
- 18.Palermo TM, Wilson AC. eHealth applications in pediatric psychology. In: Roberts MC, Steele RG, editors. Handbook of pediatric psychology. 4th. New York: Guilford; 2009. pp. 227–237. [Google Scholar]
- 19.Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of internet-based psycho-therapeutic interventions. J Technol Hum Serv. 2008;26:109–160. [Google Scholar]
- 20.Hailey D, Roine R, Ohinmaa A. The effectiveness of telemental health applications: a review. Can J Psychiatry. 2008;53(11):769–778. doi: 10.1177/070674370805301109. [DOI] [PubMed] [Google Scholar]
- 21.Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of internet-based self-management interventions for youth with health conditions. J Pediatr Psychol. 2009;34(5):495–510. doi: 10.1093/jpepsy/jsn115. [DOI] [PubMed] [Google Scholar]
- 22.Van Allen J, Davis AM, Lassen S. The use of telemedicine in pediatric psychology: research review and current applications. Child Adolesc Psychiatr Clin N Am. 2011;20(1):55–66. doi: 10.1016/j.chc.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Whittemore R, Grey M, Faulkner M, Jaser S, Deamater A, Murphy K. Recruitment and participation of youth in an internet psycho-educational intervention study. Diabetes. 2009;58(Suppl 1):A486. [Google Scholar]
- 24.Mulvaney SA, Rothman RL, Lybarger C, Wallston KA. Modeling problem solving with an internet-based self-management intervention for adolescents with type 1 diabetes. Diabetes. 2009;58(Suppl 1):A482. [Google Scholar]
- 25.Horvath AO, Del Re AC, Fluckiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy (Chic) 2011;48(1):9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- 26.Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Couns Psychol. 1991;38(2):139–149. [Google Scholar]
- 27.Krupnick JL, Sotsky SM, Simmens S, Moyer J, Elkin I, Watkins J, Pilkonis PA. The role of the therapeutic alliance in psychotherapy and pharmacotherapy outcome: findings in the national institute of mental health treatment of depression collaborative research program. J Consult Clin Psychol. 1996;64(3):532–539. doi: 10.1037//0022-006x.64.3.532. [DOI] [PubMed] [Google Scholar]
- 28.Morgan RD, Patrick AR, Magaletta PR. Does the use of telemental health alter the treatment experience? Inmates’ perceptions of telemental health versus face-to-face treatment modalities. J Consult Clin Psychol. 2008;76(1):158–162. doi: 10.1037/0022-006X.76.1.158. [DOI] [PubMed] [Google Scholar]
- 29.Lingley-Pottie P, McGrath PJ. A paediatric therapeutic alliance occurs with distance intervention. J Telemed Telecare. 2008;14(5):236–240. doi: 10.1258/jtt.2008.080101. [DOI] [PubMed] [Google Scholar]
- 30.Glueckauf RL, Fritz SP, Ecklund-Johnson EP, Liss HJ, Dages P, Carney P. Videoconferencing-based family counseling for rural teenagers with epilepsy: phase 1 findings. Rehab Psychol. 2002;47:49–72. [Google Scholar]
- 31.Duke DC, Freeman KA, Hirschfield B, Boston B, Harris MA. Videoconferencing: more is better? 2012 International Clinical Diabetes Technology Meeting. Los Angeles, CA: 2012. June. [Google Scholar]
- 32.Robin AL, Foster SL. Negotiating parent-adolescent conflict: a behavioral-family systems approach. New York: Guilford; 1989. [Google Scholar]
- 33.Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38(Suppl 2):28A. [Google Scholar]
- 34.Hood KK, Butler DA, Anderson BJ, Laffel LM. Updated and revised Diabetes Family Conflict Scale. Diabetes Care. 2007;30(7):1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. J Counsel Psychol. 1989;36:223–233. [Google Scholar]
- 36. Wysocki T, Harris MA, Greco P, Mertlich D, Buckloh L. Behavioral family systems therapy (BFST) for adolescents with a chronic illness: treatment and implementation manual. Unpublished manual. 2001.
- 37.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 38.Knaevelsrud C, Maercker A. Does the quality of the working alliance predict treatment outcome in online psychotherapy for traumatized patients? J Med Internet Res. 2006;8(4):e31. doi: 10.2196/jmir.8.4.e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cluver JS, Schuyler D, Frueh BC, Brescia F, Arana GW. Remote psychotherapy for terminally ill cancer patients. J Telemed Telecare. 2005;11(3):157–159. doi: 10.1258/1357633053688741. [DOI] [PubMed] [Google Scholar]
- 40.Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, Barrett D, Knowles F, 3rd, Hauser P. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiatry. 2004;161(8):1471–1476. doi: 10.1176/appi.ajp.161.8.1471. [DOI] [PubMed] [Google Scholar]
- 41.Simpson S, Knox J, Mitchell D, Ferguson J, Brebner J, Brebner E. A multidisciplinary approach to the treatment of eating disorders via video-conferencing in north-east Scotland. J Telemed Telecare. 2003;9(Suppl 1):S37–S38. doi: 10.1258/135763303322196286. [DOI] [PubMed] [Google Scholar]
- 42.Richardson LK, Frueh BC, Grubaugh AL, Egede L, Elhai JD. Current directions in videoconferencing tele-mental health research. Clin Psychol (New York) 2009;16(3):323–338. doi: 10.1111/j.1468-2850.2009.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pew Internet. Broadband adoption in 2007. http://www.pewinternet.org/~/media//Files/Reports/2007/PIP_Broadband%202007.pdf. Accessed March 12, 2013.
- 44.Greene CJ, Morland LA, Durkalski VL, Frueh BC. Noninferiority and equivalence designs: issues and implications for mental health research. J Trauma Stress. 2008;21(5):433–439. doi: 10.1002/jts.20367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O’Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007;58(6):836–843. doi: 10.1176/ps.2007.58.6.836. [DOI] [PubMed] [Google Scholar]
- 46.Anderson RE, Spence SH, Donovan CL, March S, Prosser S, Kenardy J. Working alliance in online cognitive behavior therapy for anxiety disorders in youth: comparison with clinic delivery and its role in predicting outcome. J Med Internet Res. 2012;14(3):e88. doi: 10.2196/jmir.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, He Q, Frueh BC. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiatry. 2010;71(7):855–863. doi: 10.4088/JCP.09m05604blu. [DOI] [PubMed] [Google Scholar]


