Abstract
Purpose
To determine whether T category of the American Joint Committee on Cancer (AJCC) TNM staging system for eyelid carcinoma, 7th edition, correlates with lymph node metastasis, distant metastasis, and survival in patients with sebaceous carcinoma of the eyelid.
Design
Retrospective, cohort study.
Participants
Fifty consecutive patients treated by 1 author (BE) for eyelid sebaceous carcinoma between May 1999 and August 2010.
Methods
Each tumor was staged according to the AJCC 7th edition TNM criteria. The Kaplan-Meier method was used to determine associations between disease-specific survival and (1) T category at presentation, (2) lymph node metastasis, and (3) distant metastasis.
Main Outcome Measures
T category at presentation, nodal metastasis, survival.
Results
The study included 37 women and 13 men (median age, 68.5 years; range, 44–86 years). Forty-four patients were white, 5 were Hispanic, and 1 was Asian. TNM designations were TXN0M0, 7 patients; T1N0M0, 4 patients; T2aN0M0, 12 patients; T2bN0M0, 11 patients; T2bN1M0, 2 patients; T2bN1M1, 1 patient; T3aN0M0, 2 patients; T3aN1M0, 5 patients; T3bN0M0, 1 patient; T3bN1M0, 1 patient; T3bN0M1, 2 patients; T4N0M0, 1 patient; and T4N0M1, 1 patient. T category at presentation was significantly associated with lymph node metastasis (P = 0.0079). No tumors with T category better than T2b or smaller than 9 mm in greatest dimension were associated with nodal metastasis. Five patients (10%) died of disease during follow-up. Their TNM designations were T2bN1M1, 1 patient; T3bN0M1, 2 patients; T4N0M0, 1 patient; and T4N0M1, 1 patient. No tumors smaller than 12 mm in greatest dimension were associated with distant metastasis or death. T category was significantly associated with disease-specific survival (P = 0.0009). Disease-specific survival was poorer among patients with T category of T3a or worse (P = 0.035).
Conclusions
T category in the 7th edition of the AJCC TNM staging system for eyelid carcinoma correlates with outcomes in patients with sebaceous carcinoma of eyelid. On the basis of the present findings, it seems reasonable to recommend sentinel lymph node biopsy or at least strict regional lymph node surveillance for patients with eyelid sebaceous carcinoma with tumors of T category T2b or worse or 10 mm or more in greatest dimension.
Sebaceous carcinoma of the eyelid is a rare carcinoma accounting for less than 1% of all eyelid tumors and 4.7% of all malignant epithelial eyelid tumors.1,3,4 It can exhibit aggressive local behavior and can metastasize to regional lymph nodes and distant organs.4
Sebaceous carcinoma of the eyelid is notorious for masquerading as other benign and less malignant lesions and often is misdiagnosed as recurrent blepharoconjunctivitis or chalazion. Thus, diagnosis of sebaceous carcinoma of the eyelid often is delayed, and patients sometimes present with advanced-stage disease. Sebaceous carcinoma of the eyelid also has the tendency to exhibit multicentric origins5 and pagetoid spread, which makes local recurrence a potential problem. In recent years, greater awareness of this neoplasm has resulted in earlier diagnosis, which has provided the opportunity for less aggressive therapies.6,7 The previously published studies on treatment outcomes and biologic behavior of sebaceous carcinoma of the eyelid have not classified the eyelid tumors on the basis of size, thickness, or extent at presentation, and thus it is not known whether tumor size is predictive of metastatic behavior.8-11 To the authors’ knowledge, no reports to date have correlated the American Joint Commission on Cancer (AJCC) T category for primary eyelid tumors with outcomes. The purpose of this study was to determine whether the T category of the AJCC 7th edition TNM classification for eyelid carcinoma correlated with lymph node metastasis, distant metastasis, and survival in a cohort of patients with sebaceous carcinoma of the eyelid treated at a single center. Because tumor size is a major determinant of the T category in the AJCC classification, whether tumor size correlated with lymph node metastasis also was evaluated. Identification of a correlation between tumor size and lymph node metastasis would help with patient selection for sentinel lymph node biopsy, which recently showed promise in identifying early microscopic metastasis associated with sebaceous carcinoma of the eyelid.12,13
Patients and Methods
A search of the database of the Section of Ophthalmology at The University of Texas MD Anderson Cancer Center identified 50 consecutive patients who were treated between May 1999 and August 2010 for sebaceous carcinoma of the eyelid by the principal investigator (B.E.). Institutional review board approval was obtained for this retrospective study. The requirement for informed consent was waived by institutional review board. The work carried out for this study complied with the Health Insurance Portability and Accountability Act. For each patient, the clinical records and the histopathologic data from tumor specimens were reviewed. Demographic and clinical data were recorded, including age, gender, ethnicity, previous history of radiation therapy or immunosuppression, tumor location, and clinical size of the eyelid tumor (greatest dimension of the lesion in millimeters). Histologic features of the eyelid tumor also were recorded, including tumor size based on the surgical specimen, presence of intraepithelial neoplasia, and perineural invasion. For each tumor, a TNM designation was assigned when the patient sought treatment at MD Anderson Cancer Center according to the 7th edition of the AJCC classification for eyelid carcinoma (Table 1).14
Table 1.
Definitions of TNM for Eyelid Carcinoma, AJCC Cancer Staging Manual, Seventh Edition14
| Primary tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Tis | Carcinoma in situ |
| T1 | Tumor ≤5 mm in greatest dimension; not invading the tarsal plate or eyelid margin |
| T2a | Tumor >5 mm, but not >10 mm, in greatest dimension; or, any tumor that invades the tarsal plate or eyelid margin |
| T2b | Tumor >10 mm, but not >20 mm, in greatest dimension; or, involves full thickness eyelid |
| T3a | Tumor >20 mm in greatest dimension; or, any tumor that invades adjacent ocular or orbital structures; any T with perineural tumor invasion |
| T3b | Complete tumor resection requires enucleation, exenteration, or bone resection |
| T4 | Tumor is not resectable because of extensive invasion of ocular, orbital, or craniofacial structures, or brain |
| Regional lymph nodes (N) | |
| NX | Regional lymph nodes cannot be assessed |
| cN0* | No regional lymph node metastasis, based on clinical evaluation or imaging |
| pN0† | No regional lymph node metastasis, based on lymph node biopsy |
| N1 | Regional lymph node metastasis |
| Distant metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
AJCC = American Joint Committee on Cancer.
Clinical N0.
Pathologic N0.
Also recorded was information about surgical treatments, including sentinel lymph node biopsy, and nonsurgical treatments, including adjuvant radiotherapy and topical chemotherapy. Information regarding surveillance for regional lymph nodes and distant metastasis was collected. The primary end points were local recurrence, regional lymph node metastasis, and distant metastasis during the study period and death resulting from sebaceous carcinoma. The relationships between these end points and T category at presentation to the authors’ institution were evaluated. Follow-up time was defined as time in months from presentation to MD Anderson Cancer Center to last contact or death, whichever occurred first.
Statistical Considerations
Simple descriptive statistics, including frequencies, percentages, medians, ranges, means, and standard deviations, are presented for the variables of interest. Associations between 2 categorical variables were determined using the Fisher exact test, and associations between continuous and categorical variables were tested using the Kruskal-Wallis test. Disease-specific survival (DSS) was defined as the time from presentation until last follow-up or death. The Kaplan-Meier method was used to determine associations between DSS and (1) T category at presentation, (2) lymph node metastasis at presentation or during the follow-up period, and (3) distant metastasis at presentation or during the follow-up period. Patients who were alive at the end of follow-up were censored at the time of last follow-up, and those who died of other causes were censored at the time of death. Homogeneity between strata was tested using the log-rank test. All P values were 2-tailed and were considered significant at α<0.05. Analyses were conducted using SAS for Windows version 9.2 (SAS Inc., Cary, NC).
There were 7 patients in whom the size of tumor could not be determined at the time of presentation to MD Anderson Cancer Center, Houston, Texas. These 7 patients were not included in the statistical analysis of DSS as a function of T category. Nodal metastasis did not develop in any of these patients developed, and none died during the study period.
Results
The study included 37 women and 13 men with a median age of 68.5 years (range, 44 – 86 years). Forty-four patients were white, 5 were Hispanic, and 1 was Asian. Tumor location was the upper eyelid in 28 patients, the lower eyelid in 15 patients, and both eyelids in 7 patients. The AJCC 7th edition TNM designations were as follows: TXN0M0, 7 patients; T1N0M0, 4 patients; T2aN0M0, 12 patients; T2bN0M0, 11 patients; T2bN1M0, 2 patients; T2bN1M1, 1 patient; T3aN0M0, 2 patients; T3aN1M0, 5 patients; T3bN0M0, 1 patient; T3bN1M0, 1 patient; T3bN0M1, 2 patients; T4N0M0, 1 patient; and T4N0M1, 1 patient.
Thirteen (26%) of 50 tumors had evidence of intraepithelial neoplasia. Three (6%) of 50 tumors had histologic evidence of perineural invasion. The TNM designation for all 3 tumors with perineural invasion was T3aN1M0. The greatest dimension of tumor in these 3 tumors was 27 mm, 20 mm, and 15 mm.
All 50 patients underwent an imaging study of the head and neck region (either computed tomography or magnetic resonance imaging) at baseline. All 50 patients also underwent ultrasonography of the regional lymph nodes (parotid and submandibular) with fine-needle aspiration of any suspicious nodes at baseline. Fifteen patients underwent sentinel lymph node biopsy as part of an ongoing prospective clinical trial at MD Anderson; 2 of 15 had histologically positive sentinel lymph nodes. Given that there are no previous published reports (before the current study) correlating size of tumor with nodal metastasis for sebaceous carcinoma, at the moment, the selection criteria for inclusion in the sentinel lymph node biopsy trial at the authors’ center does not include size criteria and only requires a confirmed diagnosis of invasive sebaceous carcinoma. The TNM designation for both patients with sebaceous carcinoma with positive sentinel lymph nodes was T3aN1M0. The greatest dimension of the tumors in these 2 patients was 25 mm and 20 mm.
All 50 patients had surgery as the primary method of treatment of eyelid sebaceous carcinoma. The final margins on all patients demonstrated negative results for invasive carcinoma, although in some patients, there was some residual intraepithelial neoplasia that later was treated with adjuvant topical chemotherapy. Two patients had adjuvant radiation therapy, 1 because of perineural invasion and the other because of very close margins at the time of surgery for recurrent disease. Four patients had topical chemotherapy with mitomycin C drops because of intraepithelial neoplasia or clinical suspicion of corneal epithelial involvement.
Of the 9 patients with regional lymph node metastasis, 2 had nodal metastasis identified through sentinel lymph node biopsy, and 7 had nodal metastasis identified on clinical examination and ultrasound-guided fine-needle aspiration of the regional lymph nodes. T category at presentation was associated significantly with lymph node metastasis (P = 0.0079); patients with nodal metastasis all had T category of T2b or worse. No tumors smaller than 9 mm in greatest dimension were associated with nodal metastasis. The tumor size for patients who had nodal metastasis ranged from 9 to 35 mm in greatest dimension (median, 17.5 mm; mean, 19.4 mm).
Four patients (8%) had documented distant metastasis. The size of eyelid tumors in these 4 patients ranged from 12 to 40 mm in greatest dimension (median, 23.4 mm; mean, 26.8 mm). The TNM designation for these 4 patients was T2bN1M1, 1 patient; T3bN0M1, 2 patients; and T4N0M1, 1 patient. Five patients (10%) died of disease during follow-up. The T designations for these 5 patients were as follows: T2b, 1 patient; T3b, 2 patients; and T4, 2 patients. No tumors smaller than 12 mm in greatest dimension were associated with distant metastasis or death.
Forty-two of the 50 patients were alive at the end of follow-up; 41 had no evidence of disease, and 1 was alive with disease. The median length of follow-up among the 41 patients alive without evidence of disease was 36 months (range, 11–96 months). One patient was alive with disease at last follow-up 14 months after presentation to the authors’ center. Of the 8 patients who died during follow-up, 5 died of disease; the median time to death for these 5 patients was 26 months (range, 19 –100 months). Three patients died of other causes; the median time to death in these 3 patients was 18 months (range, 18 –30 months). Overall, the 2-year DSS rate was 93.29% (95% confidence interval, 75.63%–98.29%), and the 5-year DSS rate was 79.27% (95% confidence interval, 48.31%–92.85%).
T category was significantly associated with DSS (P = 0.0009; Fig 1). Disease-specific survival was significantly poorer among patients with a T category of T3b or worse at presentation (P = 0.0137; Fig 2). Disease-specific survival also was poorer among patients with a T category of T3a or worse at presentation (P = 0.035; Fig 3). We did not detect a significant difference in DSS based on lymph node status (P = 0.57; figure not shown).
Figure 1.
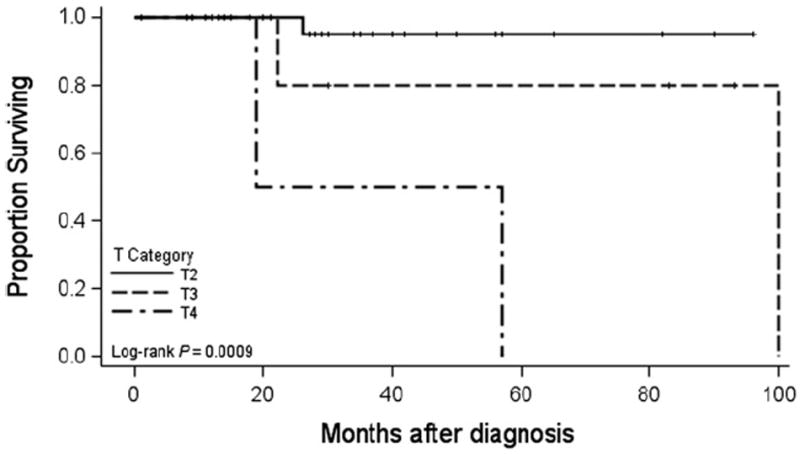
Graph showing disease-specific survival as a function of T category.
Figure 2.
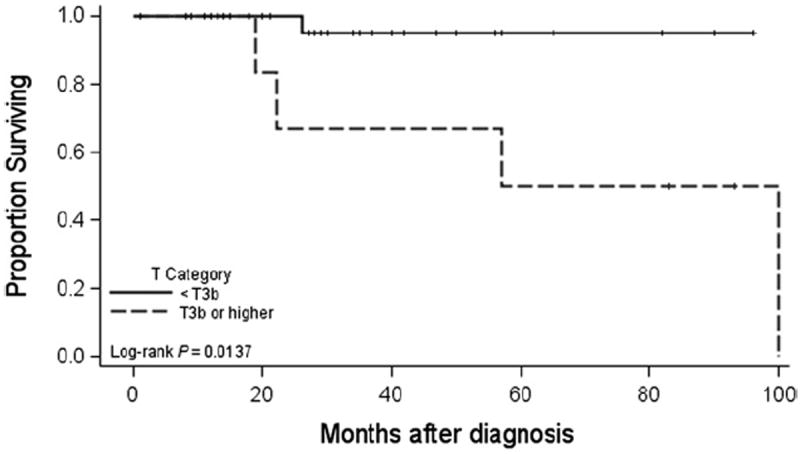
Graph showing disease-specific survival in patients with tumors better than T3b versus T3b or worse.
Figure 3.
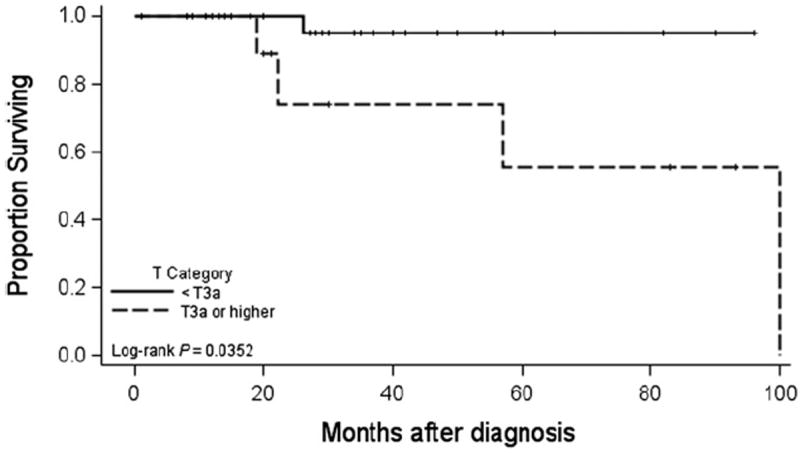
Graph showing disease-specific survival in patients with tumors better than T3a versus T3a or worse.
Discussion
The present findings suggest that the T category of the 7th edition of the AJCC TNM staging system for eyelid carcinoma correlates with lymph node metastasis and DSS in patients with sebaceous carcinoma of the eyelid. In the present cohort of patients, T category of T2b or worse correlated with regional lymph node metastasis, and T category or T3a or worse correlated with distant metastasis and death as a result of disease. Most patients with distant metastasis and death as a result of disease (4 of 5; 80%) had T3b or worse tumors.
Tumor size (greatest dimension of the eyelid tumor in millimeters) is one of the main determinants of T category in the AJCC staging system for eyelid carcinomas, although it is not the only determinant. The present data suggest that an eyelid sebaceous carcinoma of approximately 10 mm or more in greatest dimension correlates with increased risk for regional lymph node metastasis. In this series, no tumors of 9 mm or less in greatest dimension were associated with lymph node metastasis, and no tumors of 12 mm or less in greatest dimension were associated with distant metastasis and death as a result of disease.
The overall rate of nodal metastasis in this series was 18%. This is higher than the 8% rate reported in a series of 60 eyelid sebaceous carcinomas reported by Shields et al.2 However, Shields et al2 did not distinguish between nodal and distant metastasis and reported the same rates of nodal metastasis and distant metastasis. Furthermore, it is not clear what surveillance regimen was used to arrive at the data regarding metastasis. There was no attempt to identify possible correlations between the size of primary tumors and the risk of metastasis.2
The 2-year overall DSS rate was 93%, which was similar to rates in previously published reports. In their report on 60 eyelid sebaceous carcinomas, Shields et al2 reported a 94% survival rate at a median follow-up period of 22 months (mean, 41 months; range, 1–295 months). However, the present 5-year DSS rate of 79% was higher than rates in most previously published reports. Boniuk and Zimmerman15 reported a 70% 5-year survival rate in a series of 88 patients with sebaceous carcinoma of the eyelid. Ni and Kou16 observed a 60% survival rate in their series of 100 patients with eyelid sebaceous carcinoma. In another report, Ni et al17 reported a 71% survival rate at a median follow-up period of 4 years in a series of 82 patients with eyelid sebaceous carcinoma. It is not clear whether the same patients were reported in the 2 articles by the same group of authors.
The present 5-year DSS rate of 79% was similar to the 78% rate reported by Rao et al10 in a series of 104 patients. Two previously published papers reported higher 5-year survival rates: Song et al11 reported a 93.5% 5-year survival rate in a case series of 31 patients, and Muqit et al7 reported a 97% 5-year survival rate in a case series of 32 patients. Both groups of authors attributed early diagnosis and aggressive surgical treatment as the reason for their higher survival rates than those in other reports of eyelid sebaceous carcinoma.
Unless investigators reporting on eyelid sebaceous carcinoma report the size of tumors included in their cohorts according to a uniform system for classifying tumors at presentation, such as the AJCC TNM staging system, comparisons of survival rates within each study and between studies will be difficult. It is important to use 1 uniform standard and agreed-upon way to classify carcinomas of the eyelid so that outcome reporting can be viewed with some level of confidence and reproducibility.
Although the AJCC classification for eyelid carcinoma has been available for decades,14,18 to date, the ophthalmic literature is lacking reports of treatment outcomes for eyelid carcinomas according to the AJCC classification. To the authors’ knowledge, this study is the first attempt to correlate the T category of primary carcinomas of the eyelid with the risk of nodal metastasis and with DSS in patients with sebaceous carcinoma of the eyelid. This report demonstrates the value of using standard criteria for reporting of outcomes for eyelid carcinomas. It helps to define characteristics of the primary tumor at presentation that have important prognostic value in terms of lymph node metastasis and survival.
The current series also represents one of the largest single-center cohorts reported to date of patients with eyelid sebaceous carcinoma in the United States. The Wills Eye Hospital series, one of the largest single-center series published in the last decade, includes 60 patients who were treated over a period of more than 30 years. The present study includes 50 patients who were accrued over 11 years at a single tertiary referral cancer center in the United States. All patients in the current study were under active surveillance by the same practitioner for the duration of the study and had a uniform method of evaluation of their regional lymph nodes and surveillance for distant metastasis. The current series also contains data regarding sentinel lymph node status in 15 of the 50 patients with eyelid sebaceous carcinoma. To the authors’ knowledge, this represents the largest cohort of eyelid sebaceous carcinoma patients for whom information about sentinel lymph node status is available.
On the basis of the findings of an overall risk of regional lymph node metastasis of 18% and a significant correlation between T2b or higher T category and lymph node metastasis, it seems reasonable to recommend sentinel lymph node biopsy or at least strict regional lymph node surveillance for patients with sebaceous carcinoma of the eyelid who have T category of T2b or worse or tumors of 10 mm or more in greatest dimension.
Acknowledgments
Supported in part by the National Institutes of Health, Bethesda, Maryland (MD Anderson Cancer Center Support Grant no.: CA016672). The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Financial Disclosure(s):
The author(s) have no proprietary or commercial interest in any materials discussed in this article.
References
- 1.Shields JA, Demirci H, Marr BP, et al. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005;50:103–22. doi: 10.1016/j.survophthal.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Shields JA, Demirci H, Marr BP, et al. Sebaceous carcinoma of the eyelids: personal experience with 60 cases. Ophthalmology. 2004;111:2151–7. doi: 10.1016/j.ophtha.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Zürcher M, Hintschich CR, Garner A, et al. Sebaceous carcinoma of the eyelid: a clinicopathological study. Br J Ophthalmol. 1998;82:1049–55. doi: 10.1136/bjo.82.9.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Husain A, Blumenschein G, Esmaeli B. Treatment and outcomes for metastatic sebaceous cell carcinoma of the eyelid. Int J Dermatol. 2008;47:276–9. doi: 10.1111/j.1365-4632.2008.03496.x. [DOI] [PubMed] [Google Scholar]
- 5.von Below H, Rose GE, McCartney AC, Wright JE. Multicentric sebaceous gland carcinoma of the lid? Br J Ophthalmol. 1993;77:819–20. doi: 10.1136/bjo.77.12.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chao AN, Shields Cl, Krema H, Shields JA. Outcome of patients with periocular sebaceous gland carcinoma with and without conjunctival intraepithelial invasion. Ophthalmology. 2001;108:1877–83. doi: 10.1016/s0161-6420(01)00719-9. [DOI] [PubMed] [Google Scholar]
- 7.Muqit MM, Roberts F, Lee WR, Kemp E. Improved survival rates in sebaceous carcinoma of the eyelid. Eye (Lond) 2004;18:49–53. doi: 10.1038/sj.eye.6700523. [DOI] [PubMed] [Google Scholar]
- 8.Pereira PR, Odashiro AN, Rodrigues-Reyes AA, et al. Histopathological review of sebaceous carcinoma of the eyelid. J Cutan Pathol. 2005;32:496–501. doi: 10.1111/j.0303-6987.2005.00371.x. [DOI] [PubMed] [Google Scholar]
- 9.Doxanas MT, Green WR. Sebaceous gland carcinoma: review of 40 cases. Arch Ophthalmol. 1984;102:245–9. doi: 10.1001/archopht.1984.01040030195025. [DOI] [PubMed] [Google Scholar]
- 10.Rao NA, Hidayat AA, McLean IW, Zimmerman LE. Sebaceous carcinomas of the ocular adnexa: a clinicopathologic study of 104 cases, with five-year follow-up data. Hum Pathol. 1982;13:113–22. doi: 10.1016/s0046-8177(82)80115-9. [DOI] [PubMed] [Google Scholar]
- 11.Song A, Carter KD, Syed NA, et al. Sebaceous cell carcinoma of the ocular adnexa: clinical presentations, histopathology, and outcomes. Ophthal Plast Reconstr Surg. 2008;24:194–200. doi: 10.1097/IOP.0b013e31816d925f. [DOI] [PubMed] [Google Scholar]
- 12.Ho VH, Ross MI, Prieto VG, et al. Sentinel lymph node biopsy for sebaceous cell carcinoma and melanoma of the ocular adnexa. Arch Otolaryngol Head Neck Surg. 2007;133:820–6. doi: 10.1001/archotol.133.8.820. [DOI] [PubMed] [Google Scholar]
- 13.Savar A, Oellers P, Myers J, et al. Positive sentinel node in sebaceous carcinoma of eyelid. Ophthal Plast Reconstr Surg. 2011;27:4–6. doi: 10.1097/IOP.0b013e3181ef7450. report online. [DOI] [PubMed] [Google Scholar]
- 14.Edge SB, Byrd DR, Compton CC, et al., editors. AJCC Cancer Staging Manual. 7. New York: Springer; 2009. Carcinoma of the eyelid; pp. 523–30. [Google Scholar]
- 15.Boniuk M, Zimmerman LE. Sebaceous carcinoma of the eyelid, eyebrow, caruncle, and orbit. Trans Am Acad Ophthalmol Otolaryngol. 1968;72:619–42. [PubMed] [Google Scholar]
- 16.Ni C, Kou PK. Meibomian gland carcinoma: a clinicopatho-logical study of 156 cases with long-period follow-up of 100 cases. Jpn J Ophthalmol. 1979;23:388–401. [Google Scholar]
- 17.Ni C, Searl SS, Kuo PK, et al. Sebaceous cell carcinomas of the ocular adnexa. Int Ophthalmol Clin. 1982 Spring;22:23–61. doi: 10.1097/00004397-198202210-00006. [DOI] [PubMed] [Google Scholar]
- 18.Ainbinder DJ, Esmaeli B, Groo SC, et al. Introduction of the 7th edition eyelid carcinoma classification system from the American Joint Committee on Cancer-International Union Against Cancer staging manual. Arch Pathol Lab Med. 2009;133:1256–61. doi: 10.5858/133.8.1256. [DOI] [PubMed] [Google Scholar]


