Abstract
Objective
To examine the potential impact of a policy of selective referral to high-volume knee replacement hospitals on patient-hospital travel distance and access to care for patients seeking total knee replacement (TKR) in urban and rural settings.
Methods
The travel distance required for patients to reach their hospital and the additional travel distance required to reach the nearest high-volume hospital were analyzed using a 100% sample of Medicare fee-for-service patients undergoing TKR in 2001.
Results
Of the 183,174 TKR performed in the US during 2001, 95% of patients selected underwent TKR at a hospital that was located within 50 miles of their residence. There were 11,550 patients who had their TKR performed at a low-volume hospital (LVH) where there was no nearer high-volume hospital. The impact of a policy that would direct patients to high-volume hospitals varied by region. In urban areas, the nearest high-volume hospital was a median 3.8 miles further than LVH of service. Patient factors, race and poverty, were associated with selection of LVHs in urban areas. In rural areas, 1,506 patients would have had to travel more than 50 miles and 259 patients would have had to travel more than 100 miles to reach a high-volume hospital.
Conclusions
A policy to direct patients away from LVHs could increase patient-hospital travel time in rural areas and restrict access of minority and low-income patients in urban areas. Any implementation of selective referral to high-volume centers should address access to hospitals for rural patients, urban minority and poor patients.
Introduction
Several studies have shown that hospitals with higher surgical volumes are associated with lower complication rates following a variety of surgical procedures, including coronary artery bypass grafting, colon cancer resection, prostatectomy and aortic aneurysm repair (1–12). These findings have led some organizations to advocate selective referral to high-volume hospitals in order to improve the quality of care for certain high-risk procedures such as cardiac surgery (13). A similar relationship of hospital volume to outcomes following total knee replacement (TKR) has been documented, with decreased rates of mortality, pulmonary embolism and infection at high-volume hospitals compared to low-volume hospitals (LVHs) (6;7;10;11). Higher TKR surgical volumes have also been associated with greater cost-effectiveness (15). These relationships persist after correcting for patient characteristics such as age, gender, comorbidity, race/ethnicity, and insurance type.
Medicare restricts care for certain procedures (eg. carotid artery stenting, bariatric surgery, lung volume reduction surgery) to Centers of Excellence (16). If Medicare or other insurers adopted such a policy to knee replacement surgery it may lead to reduced utilization at low-volume hospitals.
While referral to high-volume hospitals has theoretical benefits, there may be unanticipated consequences. Prior studies have shown that a large proportion of patients receive care at LVHs. (10;11;16) Among hip replacement patients, Losina and colleagues reported that rural and suburban patients had longer travel distances when selecting high-volume centers over LVH (18) and postulated that travel distance might deter patients from undergoing elective surgery (19).
The purpose of this study is to examine the potential impact that a policy of selective referral to high-volume hospitals might have on increased travel distance for patients living in urban and rural settings seeking TKR. The travel distance required for patients to reach their hospital of service and the additional travel distance required to reach the nearest high-volume hospital were analyzed using the 100% sample of Medicare fee-for-service patients undergoing TKR in 2001.
Methods
Data source
From the Medicare Provider Analysis and Review (MEDPAR) administrative records, all joint replacement surgeries identified by DRG 207 or 471 were requested for the for 100% fee for service sample of patients residing in the 48 contiguous states (excluding Alaska and Hawaii) and the District of Columbia. ICD-9 codes 81.54 or 81.55 were subsequently selected to identify TKR patients. Matching denominator file data were requested. Data files from 2001 were used for study analyses. Data files from 1996 to 2000 were used to define LVH as described below.
Outcomes
Determination of Hospital Volume
Based upon prior literature (14), a LVH was defined to be any hospital that performed fewer than 25 Medicare TKR per year for at least 3 of the preceding 5 years (between 1996 and 2000).
Patient to hospital travel distance
For patients undergoing TKR in 2001, patient residence was approximated using the centroid location of the patient’s residential 9-digit zip code. The 9-digit zip code locates residences to city blocks or high density apartment buildings. When the 9-digit zip code was not available (7% of residences), the centroid of the 5-digit zip code was used as an approximation of the patient residence.
For hospitals conducting at least 1 TKR in 2001, their address was identified from their corresponding cost report.
All patient and hospital locations were geocoded using ArcView 9.0 software (19). Illustrative maps for urban and rural regions were prepared identifying LVH, non-LVH along with patient residence. The travel distance between the patient residence and their hospital of service and the travel distance between patients and the nearest high-volume hospital was calculated using the ArcView network extension.
All patient addresses were subsequently defined to be located in an urbanized area, urban cluster or rural area using US 2000 census definitions (19). Urban regions are defined as census blocks or groups that have a population density of at least 1,000 people per square mile and surrounding blocks have at least 500 people per square mile. Urban areas have at least 50,000 people while urban clusters have at least 2,500 people but less than 50,000 people. Rural areas are all other areas that are not specified as above. All these areas are identified in the ArcView spatial analyst (21).
Statistical analyses
The number of TKR hospitals and number of TKR performed during 2001 were tallied by hospital volume for the 48 contiguous states, and also stratified by rural and urban residence. For patients undergoing TKR at a LVH who did not have a high-volume hospital located closer than the hospital of service, the travel distance to the LVH of service and median, 75th, 90th, 95th percentile and maximum travel distances to the nearest high-volume hospitals were calculated for the nation, state and urban/rural region.
Covariates
Patient demographic factors included age at the time of surgery, gender and race (Caucasian, African-American and other). We used socio-economic indicators including patient receipt of state aid and median income for each 5-digit zip code from the 2000 US Census.
Patient medical characteristics included the original reason for Medicare entitlement categorized as aged, disabled, end-stage renal disease, or disabled and end-stage renal disease. Medical comorbidities were identified from the 10 MEDPAR diagnostic codes and categorized into 17 hierarchical categories using the Charlson comorbidity index. (22) Type of surgery was categorized as primary vs. revision and unilateral vs. bilateral.
Multivariate analyses
To compare patient characteristics at high vs. low-volume hospitals, logistic regression models were used. For national analyses, models were stratified by region. To evaluate for significant difference across regions, a single national logistic model was also calculated interacting region with each of the other independent variables. All multivariate analyses accounted for clustering of results within hospital.
Results
During 2001, 3,214 hospitals performed 183,174 TKRs on Medicare patients in the 48 contiguous states and District of Columbia (Table 1). There were 1,390 hospitals that met our definition for a low-volume of TKR (43% of all TKR hospitals). These LVH performed 17,484 TKR (9.5% of all TKR performed). A total of 5,934 patients travelled past a high-volume hospital to receive TKR at their LVH of service. A policy to reduce utilization of LVH would not affect travel distance for these patients, and they were therefore dropped from subsequent distance analyses. Of the remaining 11,550 receiving care at a LVH, the median travel distance to the hospital of service was 4.2 miles. The median travel distance patients would need to travel to reach the nearest high-volume hospital would be 23.6 miles (Table 1). Ten percent of patients would have to travel 55 miles or more to the nearest high-volume hospital. (See Table A-1 in Appendix.)
Table 1.
Count of patients by type of hospital volume and distance from patient to nearest High Volume Hospital
| Number and proportion of TKR patients | Median Travel distance (miles) (TKR patients discharged from LVH where no nearer high-volume hospital) | |||||||
|---|---|---|---|---|---|---|---|---|
| All TKR patients (000) * | TKR patients discharged from LVH† | …where no nearer high-volume hospital | To LVH of service | To nearest high volume hospital‡ | Additional distance | |||
| US | 183.2 | 17,484 | 9.5% | 11,550 | 66.1% | 4.2 | 23.6 | 14.3 |
| Urban Area | 98.3 | 6,843 | 7.0% | 3,313 | 48.4% | 2.7 | 7.5 | 3.8 |
| Urban Cluster | 26.7 | 3,867 | 14.5% | 3,219 | 83.2% | 1.9 | 29.3 | 24.4 |
| Rural | 58.2 | 6,774 | 11.6% | 5,018 | 74.1% | 10.9 | 31.1 | 17.8 |
| STATE | ||||||||
| FL | 13.1 | 1,062 | 8.1% | 571 | 53.8% | 3.7 | 12.9 | 7.8 |
| TX | 12.3 | 1,476 | 12.0% | 964 | 65.3% | 5.3 | 27.9 | 15.9 |
| CA | 10.0 | 1,855 | 18.5% | 1,045 | 56.3% | 5.4 | 7.5 | 1.1 |
| PA | 9.7 | 722 | 7.5% | 435 | 60.2% | 3.0 | 15.7 | 8.8 |
| OH | 9.1 | 578 | 6.3% | 359 | 62.1% | 4.1 | 15.9 | 8.9 |
| MI | 8.5 | 489 | 5.8% | 326 | 66.7% | 4.4 | 19.3 | 11.2 |
| IL | 8.4 | 566 | 6.7% | 247 | 43.6% | 3.0 | 20.8 | 13.8 |
| NY | 8.2 | 804 | 9.8% | 524 | 65.2% | 3.7 | 16.8 | 8.2 |
| AZ | 3.0 | 291 | 9.7% | 161 | 55.3% | 3.3 | 42.2 | 38.3 |
| CO | 2.1 | 201 | 9.7% | 167 | 83.1% | 4.1 | 46.3 | 33.6 |
| Other large TKR states§ | 69.8 | 6755 | 9.7% | 4,701 | 69.6% | 7.9 | 22.5 | 8.7 |
| MT | 1.0 | 128 | 12.9% | 128 | 89.1% | 2.8 | 65.5 | 60.9 |
| ND | 1.0 | 82 | 8.5% | 82 | 54.9% | 20.8 | 98.7 | 88.7 |
| SD | 1.2 | 73 | 6.3% | 36 | 49.4% | 6.3 | 50.3 | 44.9 |
| NV | 0.9 | 162 | 17.7% | 162 | 77.2% | 2.4 | 51.0 | 44.0 |
| NM | 0.6 | 35 | 5.6% | 13 | 37.1% | 6.3 | 84.2 | 64.8 |
| WY | 0.4 | 90 | 24.5% | 63 | 70.0% | 1.8 | 104.6 | 76.2 |
| Other small TKR states** | 24.0 | 2,115 | 8.8% | 1,653 | 78.1% | 7.6 | 21.5 | 11.5 |
States sorted by number of TKR performed.
States where proportion of LVH discharges was > 10% emboldened and proportion of patients that did not drive-by a high volume hospital > 70% emboldened.
States where nearest high volume hospital median travel distance or the median additional travel distance is greater than 50 miles is emboldened.
Other large TKR states: IN, MO, GA, VA, TN, MN, IA, MD, WA, AL, NJ, SC, MA, KS, KY, LA, OK, AR, NE, MS
Other small TKR states: CT, UT, OR, WV, NC, WI, ME, ID, NH, DE, RI, VT, DC
The travel distance for patients to reach the nearest high-volume hospital varied significantly by region. Specifically, when stratifying LVH by region, urban clusters and rural areas differed from urban areas. Rural or urban cluster regions had higher proportions of LVH and higher proportions of patients cared for at a LVH than did urban areas. In addition, rural and urban cluster regions had fewer patients who bypassed closer high-volume hospitals to reach their LVH of service. In these regions, the distance to the nearest high-volume hospital was approximately 30 miles (Table 1). For patients in urban clusters or rural areas the additional median travel distance required for a patient that had TKR in a LVH to have it in a high-volume hospital instead was 24.4 and 17.8 miles (Table 1) with the top 10th percentile of patients (823 patients) driving over 60 miles and the top 5th percentile (416 patients) over 80 miles (Table A-1). In contrast, in urban areas, the additional median travel distance to nearest high-volume hospital was only 3.8 miles.
For the 11,550 patients served at a LVH that was closer than any high-volume center, 10,044 (87%) had the closest high-volume hospitals located within 50 miles of their residence (Table 2a). For the remaining 1,506 patients, we divided travel distances into tiers of 50–74 miles, 75–100 miles, and more than 100 miles. Patient travel distances increased to a higher tier (as defined above) for all but 55 patients. In total, 259 patients would have to travel more than 100 miles, and 261 patients would require travel between 75 and 100 miles. For patients whose LVH was within 50 miles of their home, the nearest high-volume hospitals was increased to the next tier of 50–74 miles away for 943 patients, 75–100 miles for 221 patients and more than 100 miles for 207 patients.
Table 2a.
Distribution of distance to hospital of service and distance to closest high volume hospital for all US Medicare beneficiaries that had TKR in low volume hospital and had no nearer high volume hospital, 2001.
| Distance to Hospital of Service | Distance to closest high-volume hospitals | Total | |||
|---|---|---|---|---|---|
| Less than 50 miles | 50 – 74 miles | 75 – 100 miles | More than 100 miles | ||
| Less than 50 miles | 10,044 | 943 | 221 | 207 | 11,415 |
| 50 – 74 miles | 43 | 33 | 20 | 96 | |
| 75 – 99 miles | 7 | 27 | 34 | ||
| More than 100 miles | 5 | 5 | |||
| Total | 10,044 | 986 | 261 | 259 | 11,550 |
Breaking this analysis down further by type of region, 6,731 of 8,237 patients from either urban clusters or rural regions had a high-volume hospital within 50 miles of their home. For the remaining 1,506 who did not have nearby high-volume hospital, 986 would have to travel 50–74 miles, 261, 75–100 miles and 259 more than 100 miles. (Table 2b)
Table 2b.
Distribution of distance to hospital of service and distance to closest high volume hospital for beneficiaries in residing in Rural Area or Urban Cluster that had TKR in low volume hospital and had no nearer high volume hospital, 2001.
| Distance to Hospital of Service | Distance to closest high-volume hospitals | Total | |||
|---|---|---|---|---|---|
| Less than 50 miles | 50 – 74 miles | 75 – 100 miles | More than 100 miles | ||
| Less than 50 miles | 6,731 | 943 | 221 | 207 | 8,102 |
| 50 – 74 miles | 43 | 33 | 20 | 96 | |
| 75 – 99 miles | 7 | 27 | 34 | ||
| More than 100 miles | 5 | 5 | |||
| Total | 6,731 | 986 | 261 | 259 | 8,237 |
Small area analyses
Patient-high-volume hospitals travel distance varied widely by state (Table 1). In the 8 states with the most TKR patients (FL, TX, CA, PA, OH, MI, IL, NY), the large majority of patients had travel distances that did not exceed 50 miles. For geographically larger states, travel distances for the 90th and 95th percentiles could exceed 90 miles. For example, Arizona and Colorado are two large states with travel distances greater than 100 miles at the 90th percentile (Table A-1).
For the smaller, more rural states patient travel distances were also large with median additional travel distances often exceeding 50 miles. However, given the small number of TKR performed in these states, the absolute number of patients who would need to travel these distances is few.
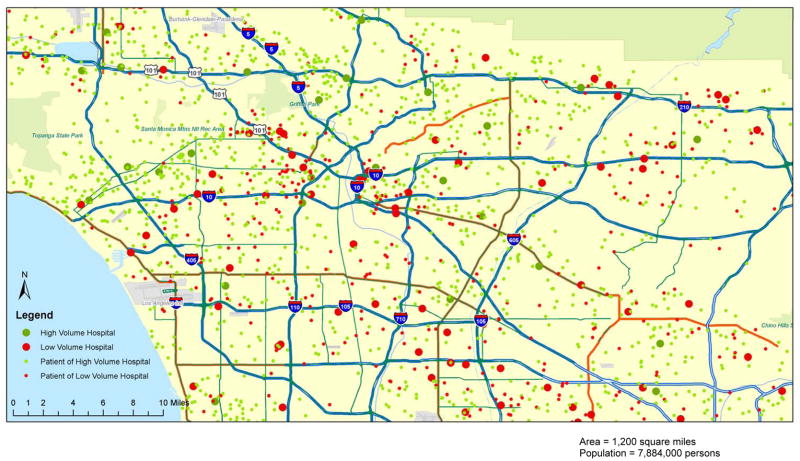
Figure 1 illustrates the locations of LVH, high-volume hospitals and the TKR patient residences for the densely populated Los Angeles region. The majority of this 1,200 square mile region is classified as an urban area and has 65 LVHs represented by large red circles (67% of the total 96 TKR hospitals) providing 390 (22% of the 1,808) TKR performed (small red circles). Of the 390 patients treated at a LVH for TKR, 250 patients (64%) had a high-volume hospital closer than the LVH of service. For the remaining 140 patients, the median distance for patients to travel to the nearest high-volume hospitals was 4.3 miles with the maximum being only 8.6 miles. (Table A of Figure 1) Combining these findings with those noted above for urban areas, a policy of selective referral to high-volume hospitals in urban settings would not significantly impact patient to hospital travel distance.
Figure 1. Los Angeles Region 2001 TKR Patient Residence, Low and High Volume Hospital Locations.
Table A.
| Number of TKR patients | TKR patients discharged from LVH …and no nearer high- volume hospitals |
Distance from patient residence to | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LVH Hospital of service | nearest High Volume TKR Hospital | ||||||||||
| All patients | 1808 | Mean | Median | Mean | Median | P75 | P90 | P95 | Max | ||
| LVH patients | 390 | 7.3 | 4.7 | ||||||||
| … and no nearer HVH | 140 | 2.3 | 2.2 | 4.5 | 4.3 | 5.7 | 6.6 | 7.7 | 8.6 | ||
Table B.
| High Volume Hospital (n = 1,418) | Low Volume Hospital (n = 390) | Odds Ratio of LVH selection | |
|---|---|---|---|
| Age mean (s.d.) in years | 74.2 (8.1) | 72.2 (8.9) | 1.00 |
| Female (%) | 71.5 | 73.5 | 1.12 |
| Race/Ethnicity (%) | |||
| Caucasian | 76.8 | 50.3 | (Referent) |
| African-American | 9.0 | 15.3 | 1.59* |
| Asian | 3.7 | 11.7 | 3.27*** |
| Hispanic | 8.0 | 17.9 | 1.82*** |
| Other | 2.6 | 4.9 | 2.01*** |
| Original reason for Medicare eligibility† (%) | |||
| Aged | 84.6 | 75.8 | (Referent) |
| Disabled | 15.3 | 23.7 | 1.26 |
| State aid recipient (%) | 32.1 | 60.2 | 1.79*** |
| Median Income, Mean (s.d) in $000 | 46.7 (16.9) | 41.3 (15.1) | 0.99*** |
| Revision (vs. Primary) TKR | 8.4% | 7.4% | 0.74 |
| Charlson mean number of comorbidities (s.d) | 0.65 (1.0) | 0.73 (1.1) | 1.01 |
Notably, the map also shows that LVHs and patients receiving care at LVH are clustered. Patients receiving care at LVH were more likely to reside in poorer zipcodes than patients receiving care at high-volume hospitals (small green circles), p < 0.05. Patients receiving care at LVH were also more likely to be non-Caucasian (50% vs. 24%, p < 0.05), have disability as their original eligibility for Medicare (24% vs. 15%, p = NS) and be a recipient of state aid (60% vs. 32%, p < 0.05). (Table B associated with Figure 1).
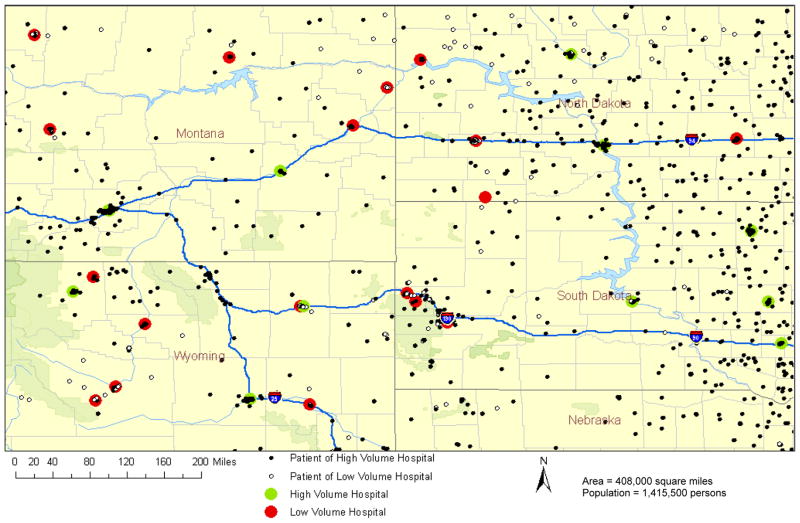
In contrast to the densely populated LA region, in a rural setting, depicted in Figure 2, patient to hospital travel distances were much greater. For the much larger area covering 408,000 square miles (scale is 340 times greater while population captured is only twice as great as Figure 1) the majority of the area shown is rural with small urban areas and clusters centered on the larger cities (not well visualized owing to the scale of the map). For the area depicted in Figure 2, there were 34 TKR hospitals performing 1930 TKR. Of these hospitals, there were 19 LVH (56% of TKR hospitals) that performed 240 TKR (13% of the total TKR performed). There were 154 patients who had their TKR performed at a LVH and for whom there was no closer high-volume hospital. The median patient to the LV hospital of service for these patients was 1.8 miles while their median patient travel to the nearest high-volume TKR hospital travel distance would have been 99.6 miles. (Table A of Figure 2)
Figure 2. Rural state 2001 TKR Patient Residence, Low and High Volume Hospital Locations.
Table A.
| Number of TKR patients | TKR patients discharged from LVH …and no nearer high- volume hospitals | Distance from patient residence to | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LVH Hospital of service | nearest High Volume TKR Hospital | ||||||||||
| All patients | 1,930 | Mean | Median | Mean | Median | P75 | P90 | P95 | Max | ||
| LVH patients | 240 | 34.2 | 6.6 | ||||||||
| …and no nearer HVH | 154 | 20.1 | 1.8 | 93.5 | 99.6 | 120.5 | 138.7 | 156.0 | 218.5 | ||
Table B.
| Distance to Hospital of Service | Distance to closest high-volume hospitals | Total | |||
|---|---|---|---|---|---|
| Less than 50 miles | 50 – 74 miles | 75 – 99 miles | More than 100 miles | ||
| Less than 50 miles | 22 | 17 | 27 | 60 | 126 |
| 50 – 74 miles | 7 | 2 | 6 | 15 | |
| 75 – 99 miles | 3 | 8 | 11 | ||
| More than 100 miles | 2 | 2 | |||
| Total | 23 | 25 | 32 | 76 | 154 |
Table C.
| High Volume Hospital (n = 1690) | Low Volume Hospital (n = 240) | Odds Ratio of LVH selection | |
|---|---|---|---|
| Age mean (s.d.) in years | 73.2 (7.1) | 73.2 (7.5) | 1.00 |
| Female (%) | 63.9 | 63.9 | 0.98 |
| Caucasian (%) | 98.1 | 98.4 | 1.05 |
| Original reason for Medicare eligibility* (%) | |||
| Aged | 88.2 | 88.5 | (Referent) |
| Disabled | 11.8 | 11.5 | 1.08 |
| State aid recipient (%) | 6.4 | 4.5 | 0.65 |
| Median Income, Mean (s.d) in $000 | 32.5 (4.9) | 31.9 (5.3) | 0.99 |
| Revision (vs. Primary) TKR (%) | 8.9 | 3.7 | 0.41† |
| Charlson mean number of comorbidities (s.d.) | 0.74 (1.0) | 0.80 (1.2) | 1.05 |
Stratifying travel distance by tier (Table B of Figure 2), patient travel distances increased to the next tier for all but 34 of these 154 patients if they were to be redirected to the nearest high-volume hospital. For the remaining 126 patients whose LVH was within 50 miles of their residence, the nearest high-volume hospitals increased the tier to 50–74 miles away for 17 patients, 75–99 miles for 27 patients and more than 100 miles for 60 patients.
Patient travel distance was the primary factor associated with selection of LVH in this rural area as there were few differences in patient characteristics by type of hospital with the exception of more patients undergoing revision surgery at high-volume hospitals. (Table C associated with Figure 2.)
To evaluate if the above associations were similar across other regions of the US, we stratified the total TKR population by urban and rural regions (Table 3). The associations noted in the Los Angeles area were observed in other urban areas. Urban African-American and other non-Caucasian patients were 1.5 and 2.3 times more likely to receive their care at a LVH than Caucasian patients (p < 0.0001 for both). Urban patients receiving state aid were 2.2 times more likely to receive their care at a LVH than urban patients not receiving state aid. Association between patient characteristics and type of hospital in urban clusters and rural areas was less prominent with the exception of patients undergoing revision surgery which had significantly stronger association with high-volume hospital.
Table 3.
Descriptors of patients at High and Low Volume Hospital by Type of Region
| Type of Region | Urban Area (n = 98.3K) | Urban Cluster (n = 26.7K) | Rural (n = 58.2K) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Type of Hospital | High Volume Hospital | Low Volume Hospital | Odds Ratio | High Volume Hospital | Low Volume Hospital | Odds Ratio | High Volume Hospital | Low Volume Hospital | Odds Ratio |
| Number of TKR (000) (Proportion by type of hospital within that region) | 91.5 (93.0) | 6.8 (7.0) | 22.8 (85.5) | 3.9 (14.5) | 52.4 (88.2) | 7.0 (11.8) | |||
| Mean Age (s.d.) in years§§ | 72.8 (7.6) | 71.8 (8.4) | 1.00 | 72.5 (7.7) | 72.7 (8.0) | 1.01 | 71.7 (7.6) | 71.8 (7.9) | 1.01†† |
| Female proportion | 66.9 | 71.3 | 0.93 | 67.7 | 69.2 | 1.01 | 61.3 | 63.4 | 0.97 |
| Race | |||||||||
| Caucasian | 89.4 | 77.9 | REF | 94.0 | 91.0 | REF | 94.0 | 91.7 | REF |
| African-American§§ | 7.8 | 13.6 | 1.55* | 4.5 | 6.6 | 1.28 | 3.9 | 5.1 | 1.07 |
| Other§§ | 2.8 | 8.5 | 2.27†† | 1.5 | 2.4 | 1.27 | 2.0 | 3.1 | 1.26 |
| Original reason for Medicare eligibility† | |||||||||
| Aged | 86.4 | 80.5 | REF | 84.1 | 83.2 | REF | 83.3 | 81.0 | REF |
| Disabled | 13.4 | 19.2 | 1.11 | 15.8 | 16.8 | 1.02 | 16.6 | 18.9 | 1.18†† |
| State aid recipient§§ | 9.4 | 23.3 | 2.23†† | 11.3 | 17.5 | 1.65†† | 9.4 | 15.2 | 1.63†† |
| Median Income§§ Mean (s.d) in $000 |
37.4 (12.6) | 35.3 (11.5) | 1.00 | 35.4 (10.5) | 34.4 (10.3) | 0.99 | 46.3 (18.4) | 45.0 (17.8) | 0.99†† |
| Revision (vs. Primary) TKR‡ | 9.0 | 7.4 | 0.77†† | 9.2 | 4.7 | 0.49†† | 9.0 | 5.1 | 0.53†† |
| Charlson mean number of comorbidities (s.d.) | 0.70 (1.00) | 0.69 (0.99) | 0.97 | 0.68 (1.00) | 0.61 (0.93) | 0.92†† | 0.65 (0.97) | 0.61 (0.94) | 0.94†† |
p < 0.0001 for Odds Ratio using stratified logistic model
Does not sum to 100% (Renal Disease not shown)
p < 0.0001 for interaction effect between region and variable tested for multivariate model on entire sample
Discussion
Given the freedom to choose which hospital to receive their care, 95% of patients chose a hospital that was within 50 miles of their residence. The primary factors associated with selection of high and low-volume hospitals differ between rural and urban regions. Travel distance is the predominant factor in remote rural regions whereas race and socio-economic status are the strongest correlates in urban areas.
One approach proposed for improving the overall quality of care for other high-risk surgical procedures is the selective referral of patients to higher-volume hospitals. The Leapfrog group has advocated volume standards for certain high-risk surgical procedures including TKR.(13;16) However, for TKR, there is limited data on optimal strategies for improving the quality of care for patients treated at low-volume institutions. (23)
If such a policy (selective referral to high-volume hospitals) were implemented it is not clear how it would impact patient care. Except in rural areas, for most patients selective referral to high-volume care would not result in unmanageable travel distances. However, in rural regions some patients would be required to travel distances of greater than 50 or 100 miles, though the absolute numbers of patients affected would be small. Patients with longer travel distances might be dissuaded from considering TKR.(18) The lost benefits in patient quality of life from forgone surgeries might outweigh any potential benefits from shifting care to high-volume hospitals. To understand this utility tradeoff more clearly, better understanding about the willingness to consider surgery as a function of distance and the marginal benefits of receiving surgery at a high volume center are needed.
In urban areas, patient travel distance to high-volume hospital is not an issue. However, as reported by other authors (16;24;25), it is clear that socio-economic factors are associated with selection of low-volume hospitals. As all patients studied were Medicare fee-for-service, the associations observed could be mediated through other pathways such as patients’ primary care or orthopedic physician hospital affiliation. Therefore, it is possible that selective referral to high-volume hospitals where poorer patients may not have access to physicians with affiliation to high-volume hospitals could lead to reduced access where switching hospitals (or doctors) might not be an option.
The findings and interpretation are limited by the potential inaccuracies of administrative data. Though patient addresses are updated annually, there may be inaccuracies in residence at the time of surgery attributable to change of address or multiple residences. While 6.8% of residences had only 5-digit zipcodes (missing 9-digit zipcode), a greater proportion of these (60%) came from rural areas (which represent only 32% of TKR cases). To perform sensitivity analyses, we re-ran the analysis excluding residences with missing 9-digit zipcodes. The resulting patient to hospital median distances for rural residents changed by less than 0.3 miles. Other limitations of the administrative data include the lack of data available on patient marital status, driving preferences, or ability to utilize nearby family or other social support to facilitate care.
The findings of this study quantify how the elimination of TKR at low-volume hospitals would increase the travel distance for a significant number of patients in rural areas and may decrease access for poorer and minority patients in urban areas. Restricting access to a highly effective procedure (even if outcomes are slightly poorer at LVH) may not be optimal policy if it discourages utilization. Any implementation of selective referral to high-volume centers should explicitly address issues of access for rural, minority and lower socio-economic status populations. An alternative approach to improving quality of care may be to identify and disseminate the processes of care that lead to better outcomes at high-volume centers. (26)
Supplementary Material
Summary points.
Better patient outcomes have been associated with higher surgical volumes.
Urban minority and poor are more likely to receive care at low-volume hospitals.
Selective referral to high-volume hospitals would increase patient-hospital travel distances for select rural patients.
Rural patients, minority and poor urban patients could be adversely affected by a policy to reduce utilization of low-volume hospitals.
Acknowledgments
Jeffrey Katz is partly supported by NIH P60 AR 47782.
Elena Losina is partly supported NIH P50 AR 47782 and NIH K24 AR 057827
Contributor Information
John D. FitzGerald, Department of Medicine, Division of Rheumatology, University of California, Los Angeles.
Nelson F. SooHoo, Department of Orthopaedic Surgery, University of California, Los Angeles.
Elena Losina, Division of Rheumatology, Immunology and Allergy and Department of Orthopedic Surgery, Brigham and Women’s Hospital, Harvard Medical School and Department of Biostatistics, Boston University School of Public Health, Boston.
Jeffrey N. Katz, Division of Rheumatology, Immunology and Allergy and Department of Orthopedic Surgery, Brigham and Women’s Hospital, Harvard Medical School and Department of Epidemiology, Harvard School of Public Health, Boston.
Reference List
- 1.Begg CB, Riedel ER, Bach PB, Kattan MW, Schrag D, Warren JL, et al. Variations in morbidity after radical prostatectomy. N Engl J Med. 2002;346(15):1138–1144. doi: 10.1056/NEJMsa011788. [DOI] [PubMed] [Google Scholar]
- 2.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 3.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. Jama. 2000;283(9):1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 4.Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2003;85-A(12):2318–2324. doi: 10.2106/00004623-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider Volume of Total Knee Arthroplasties and Patient Outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg Am. 2003;85-A(9):1775–1783. doi: 10.2106/00004623-200309000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86-A(9):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am JID - 0014030. 2001;83-A(11):1622–1629. doi: 10.2106/00004623-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ko CY, Chang JT, Chaudhry S, Kominski G. Are high-volume surgeons and hospitals the most important predictors of in-hospital outcome for colon cancer resection? Surgery. 2002;132(2):268–273. doi: 10.1067/msy.2002.125721. [DOI] [PubMed] [Google Scholar]
- 9.Kreder HJ, Deyo RA, Koepsell T, Swiontkowski MF, Kreuter W. Relationship between the volume of total hip replacements performed by providers and the rates of postoperative complications in the state of Washington. J Bone Joint Surg Am. 1997;79(4):485–494. doi: 10.2106/00004623-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 10.SooHoo NF, Zingmond DS, Lieberman JR, Ko CY. Primary total knee arthroplasty in California 1991 to 2001: does hospital volume affect outcomes? J Arthroplasty. 2006;21(2):199–205. doi: 10.1016/j.arth.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 11.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88(3):480–485. doi: 10.2106/JBJS.E.00629. [DOI] [PubMed] [Google Scholar]
- 12.Steinbrook R. Disparities in health care--from politics to policy. N Engl J Med. 2004;350(15):1486–1488. doi: 10.1056/NEJMp048060. [DOI] [PubMed] [Google Scholar]
- 13.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130(3):415–422. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 14.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB. Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am JID - 0014030. 2001;83-A(12):1856–1864. doi: 10.2106/00004623-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, et al. Cost-effectiveness of Total Knee Arthroplasty in the United States Patient Risk and Hospital Volume. Archives of Internal Medicine. 2009;169(12):1113–1121. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medicare Approved Facilities/Trials/Registries. https://www.cms.gov/MedicareApprovedFacilitie/
- 17.Liu JH, Zingmond DS, McGory ML, SooHoo NF, Ettner SL, Brook RH, et al. Disparities in the utilization of high-volume hospitals for complex surgery. Jama. 2006;296(16):1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 18.Losina E, Barrett J, Baron JA, Levy M, Phillips CB, Katz JN. Utilization of low-volume hospitals for total hip replacement. Arthritis Rheum. 2004;51(5):836–842. doi: 10.1002/art.20700. [DOI] [PubMed] [Google Scholar]
- 19.Losina E, Kessler CL, Wright EA, Creel AH, Barrett JA, Fossel AH, Katz JN. Geographic diversity of low-volume hospitals in total knee replacement: implications for regionalization policies. Med Care. 2006 Jul;44(7):637–45. doi: 10.1097/01.mlr.0000223457.92978.34. [DOI] [PubMed] [Google Scholar]
- 20.United States Census 2000. United States Census Bureau; Census 2000 Urban and Rural Classification. http://www.census.gov/geo/www/ua/ua_2k.html. [Google Scholar]
- 21.ArcGIS. Redlands, CA: ESRI; 2007. [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 23.Solomon DH, Chibnik LB, Losina E, Huang J, Fossel AH, Husni E, et al. Development of a preliminary index that predicts adverse events after total knee replacement. Arthritis Rheum. 2006;54(5):1536–1542. doi: 10.1002/art.21772. [DOI] [PubMed] [Google Scholar]
- 24.SooHoo NF, Zingmond DS, Ko CY. Disparities in the utilization of high-volume hospitals for total knee replacement. J Natl Med Assoc. 2008;100(5):559–564. doi: 10.1016/s0027-9684(15)31303-1. [DOI] [PubMed] [Google Scholar]
- 25.Losina E, Wright EA, Kessler CL, Barrett JA, Fossel AH, Creel AH, et al. Neighborhoods matter: use of hospitals with worse outcomes following total knee replacement by patients from vulnerable populations. Arch Intern Med. 2007;167(2):182–187. doi: 10.1001/archinte.167.2.182. [DOI] [PubMed] [Google Scholar]
- 26.Finlayson SR. Delivering quality to patients. Jama. 2006;296(16):2026–2027. doi: 10.1001/jama.296.16.2026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.