Abstract
Background and Purpose: We sought to examine a large nationwide (United States) sample of emergency department (ED) visits to determine data related to utilization and costs of care for urolithiasis in this setting.
Methods: Nationwide Emergency Department Sample was analyzed from 2006 to 2009. All patients presenting to the ED with a diagnosis of upper tract urolithiasis were analyzed. Admission rates and total cost were compared by region, hospital type, and payer type. Numbers are weighted estimates that are designed to approximate the total national rate.
Results: An average of 1.2 million patients per year were identified with the diagnosis of urolithiasis out of 120 million visits to the ED annually. Overall average rate of admission was 19.21%. Admission rates were highest in the Northeast (24.88%), among teaching hospitals (22.27%), and among Medicare patients (42.04%). The lowest admission rates were noted for self-pay patients (9.76%) and nonmetropolitan hospitals (13.49%). The smallest increases in costs over time were noted in the Northeast. Total costs were least in nonmetropolitan hospitals; however, more patients were transferred to other hospitals. When assessing hospital ownership status, private for-profit hospitals had similar admission rates compared with private not-for-profit hospitals (16.6% vs 15.9%); however, costs were 64% and 48% higher for ED and inpatient admission costs, respectively.
Conclusions: Presentation of urolithiasis to the ED is common, and is associated with significant costs to the medical system, which are increasing over time. Costs and rates of admission differ by region, payer type, and hospital type, which may allow us to identify the causes for cost discrepancies and areas to improve efficiency of care delivery.
Introduction
Urolithiasis is a common cause of emergency department (ED) visits, with a lifetime development risk of 12% in men and 6% in women in the United States.1,2 Urolithiasis treatment represents a significant economic burden, costing an estimated $2 billion a year as of 2000 and increasing.3
However common urolithiasis may be, there is a wide range of variability in its management and associated costs. Factors such as payer type, hospital characteristics, and geographic region are believed to play a significant role in this variability. Due to such a large prevalence of urolithiasis, it is important to assess patterns of admission rates and treatment costs in order to elucidate areas for potential improvements on a nationwide level.
The Nationwide Emergency Department Sample (NEDS) is the largest all-payer ED database in the United States. It provides a wide range of information about ED visits, including key demographics, costs, and methods of treatment.4 By examining the NEDS from 2006 to 2009, we aimed at identifying the factors affecting admission rates and costs relative to the emergent presentation of urolithiasis.
Materials and Methods
The study examined ED visits for upper tract urolithiasis using discharge data from NEDS, HCUP, Agency for Healthcare Research and Quality.4 All presentations with diagnosis of ureteral or renal stone were identified by querying the NEDS database from 2006 to 2009.
The NEDS is the largest all-payer ED database publically available in the United States, and it was created to facilitate analyses of ED utilization patterns. At the time of this analysis, the NEDS included data from 2006 through 2009, containing between 26 and 29 million ED records per year from more than 950 hospital-based EDs across 24–29 states, representing a 20% stratified sample of U.S. hospital EDs. Hospitals are selected annually based on sampling of hospital characteristics, including geographic region (Northeast, Midwest, South, and West), trauma center designation, location (urban vs rural, and metropolitan size), teaching status, and hospital ownership type (public, for profit, and not for profit). Total ED charges were reported in the sample based on revenue codes or a separate charge field for the entire recorded event. Charge data were not reported from five to six states each year of data collection, representing ∼19% of the sample. To account for the missing data, summary of charges utilized the product of the number of estimated cases times the average charge. Supplemental files included total inpatient charges for a proportion of those events that resulted in admission. These charges did not include professional fees and noncovered charges. Once again, the product of the estimated number of cases and the average charge was used to estimate the total summary of charges. Hospital-based weights are provided in the sample to allow for national estimates of ED utilization pertaining to ∼125 million ED visits estimated annually in the United States.
Upper tract urolithiasis encounters were identified by International Classification of Diseases 9 (ICD-9) diagnosis code 592.0, 592.1, or 592.9. No distinction was made between codes for renal and ureteral stones given previous studies noting a high level of incongruity between ICD-9 code and imaging for determination of stone location.5 Each encounter was further analyzed for patient and hospital characteristics and hospital charges. Established weighting in the sample, as described earlier, was used to calculate nationwide estimates of urolithiasis presentation to the ED.
A multivariate regression model was used to estimate odds of admission given specific patient demographics. Variables included in the model included presence of diabetes, pregnancy, sepsis, and urinary tract infection (UTI). All statistical analysis was performed using IBM SPSS® v19. Since the data are public and de-identified, this study qualifies for institutional review board exempt status (title 45 of the Code of Federal Regulations, section 46.102).
Results
An average of 1.2 million patients per year were identified with the diagnosis of stones out of roughly 120 million visits to the ED yearly from 2006 to 2009. ED visits due to stones increased from 1,136,882 to 1,308,759 over this period, an increase of 15% over 4 years.
There were no significant trends in admission rates from 2006 to 2009; however, there were significant variations between regions, hospital types, and payer types (Table 1). Admission rates were highest in the Northeast, among teaching hospitals, and among Medicare patients. The lowest admission rates were noted for self-pay patients and nonmetropolitan hospitals. Mean age of patients admitted to the hospital was 54.8 years vs 49.1 years for those discharged from ED (p<0.001). A number of patient factors were also noted to be predictive of admission. On multivariate analysis, UTI, pregnancy, diabetes, and a diagnosis of sepsis were the largest predictors for admission from the ED (Table 2).
Table 1.
Number of Patients Seen and Disposition Rates from ED Stratified by Payer, Region, and Hospital Type
| |
|
|
Disposition (%) |
|||
|---|---|---|---|---|---|---|
| Patients per year | % of total ED visits for category | Home | Transfer | Admit | Died in ED | |
| Total |
1,231,355 |
0.99 |
79.65 |
1.13 |
19.21 |
0.005 |
| Payer | ||||||
| Medicare |
20,268 |
0.08 |
56.20 |
1.72 |
42.04 |
0.017 |
| Medicaid |
133,048 |
0.47 |
76.57 |
1.12 |
22.29 |
0.004 |
| Private |
639,871 |
1.50 |
84.47 |
1.06 |
14.45 |
0.003 |
| Self pay |
198,816 |
0.91 |
89.55 |
0.67 |
9.76 |
0.002 |
| Region | ||||||
| West |
212,923 |
0.96 |
80.12 |
0.99 |
18.89 |
0.004 |
| Midwest |
295,348 |
1.02 |
79.00 |
2.34 |
18.65 |
0.008 |
| South |
521,026 |
1.07 |
81.83 |
0.70 |
17.46 |
0.005 |
| Northeast |
202,058 |
0.83 |
74.49 |
0.62 |
24.88 |
0.002 |
| Hospital type | ||||||
| Metropolitan teaching |
412,937 |
0.86 |
76.92 |
0.79 |
22.27 |
0.006 |
| Metropolitan nonteaching |
590,260 |
1.12 |
79.81 |
0.90 |
19.29 |
0.005 |
| Nonmetropolitan | 228,158 | 0.97 | 84.18 | 2.33 | 13.49 | 0.002 |
ED=emergency department.
Table 2.
Multivariate Analysis of Presenting Variables and Odds Ratios for Admission
| Admit (%) | Odds ratio (95% CI) | |
|---|---|---|
| Sex | ||
| Female |
21.11 |
1.34 (1.32–1.36) |
| Male |
14.83 |
|
| Age | ||
| >18 |
17.60 |
1.04 (1.04–1.04) |
| <18 |
10.28 |
|
| Urinary tract infection | ||
| Yes |
33.46 |
2.50 (2.46–2.54) |
| No |
14.69 |
|
| Pyelonephritis/sepsis | ||
| Yes |
75.91 |
15.99 (15.55–16.46) |
| No |
14.80 |
|
| Pregnant | ||
| Yes |
40.83 |
2.07 (2.04–2.11) |
| No |
21.11 |
|
| Diabetes | ||
| Yes |
41.20 |
2.42 (2.38–2.47) |
| No | 15.17 | |
CI=confidence interval.
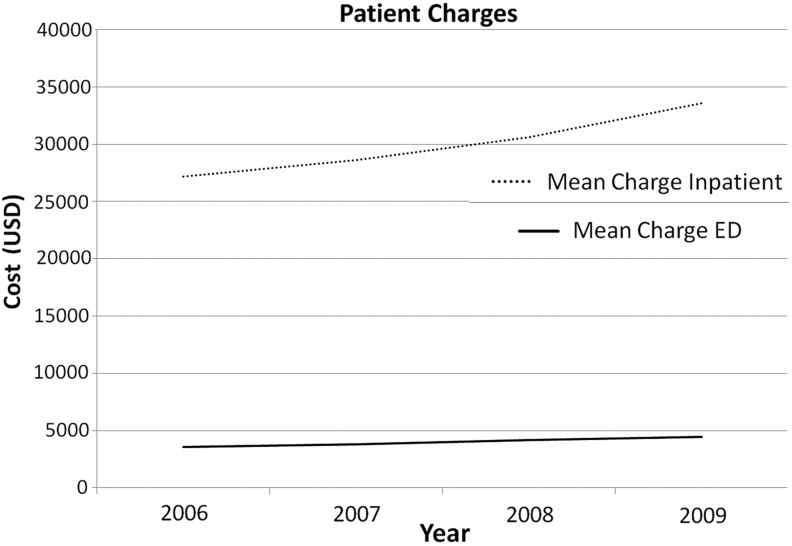
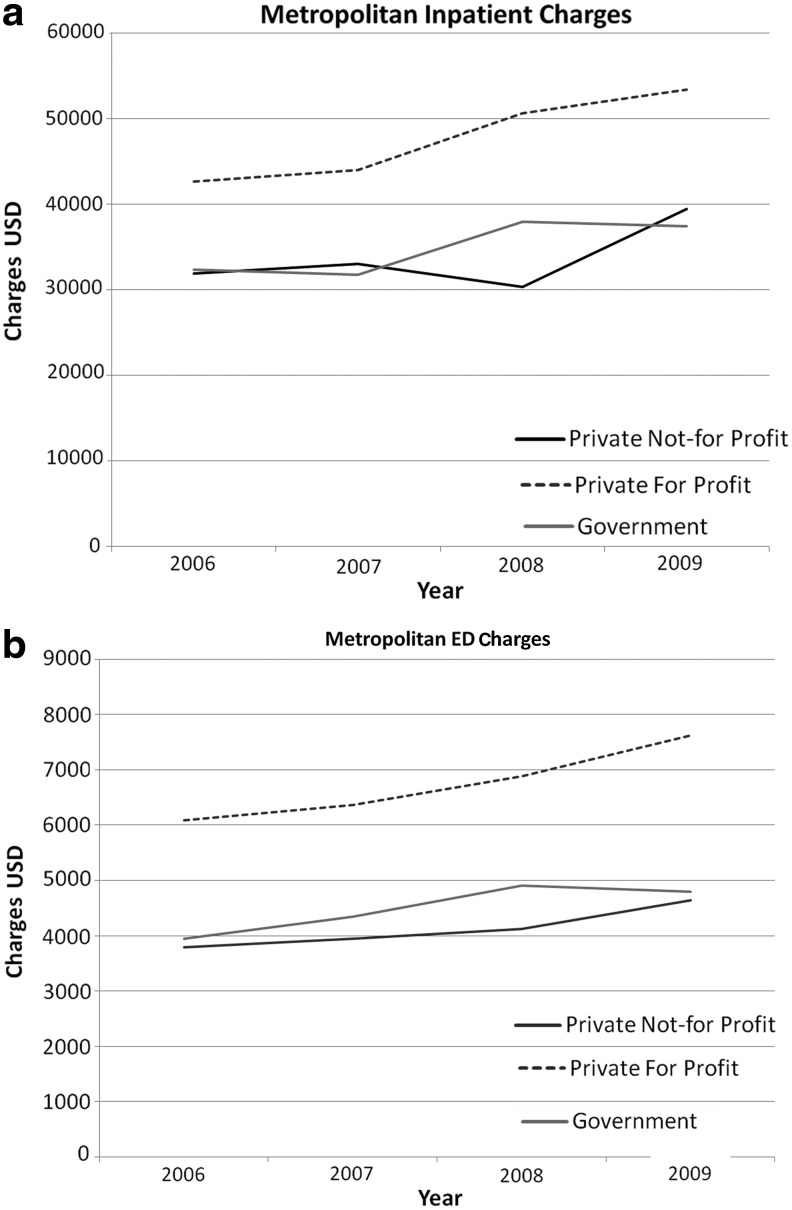
Costs increased for both ED visits and admissions over time (Fig. 1). Total costs were least in nonmetropolitan hospitals; however, more patients were transferred to other hospitals. The smallest increases in costs over time were noted in the Northeast (Table 3). When looking at hospital ownership, significant differences in costs were noted for both patients discharged from the ED and costs of admission (Fig. 2a, b) for those metropolitan facilities in which hospital control was disclosed. Patterns for metropolitan and nonmetropolitan private for profit hospitals were similar, although overall costs for nonmetropolitan hospitals were less (data not shown). Private for-profit hospitals were noted to have similar admission rates to private not-for-profit hospitals; however, costs were markedly higher than both government and private not-for-profit hospitals for all data points examined.
FIG. 1.
Mean costs for emergency department (ED) alone and ED+Inpatient (for patients admitted) for all patients by year.
Table 3.
Average Cost and Cost Increases Over Time Stratified by Payer, Region, and Hospital Type
| Average ED cost | Increase 2006–2009 | Percent per year | Average inpatient cost | Increase 2006–2009 | Percent per year | |
|---|---|---|---|---|---|---|
| Total |
4014 |
913 |
8.57 |
26,103 |
5488 |
7.74 |
| Payer | ||||||
| Medicare |
3560 |
895 |
7.12 |
32,200 |
6246 |
5.32 |
| Medicaid |
3703 |
908 |
6.89 |
26,213 |
3810 |
3.83 |
| Private |
4098 |
948 |
6.48 |
21,207 |
4630 |
6.00 |
| Self pay |
4165 |
919 |
6.23 |
21,942 |
3224 |
3.88 |
| Region | ||||||
| West |
3724 |
914 |
9.20 |
38,741 |
9798 |
7.37 |
| Midwest |
4075 |
894 |
6.16 |
19,303 |
5599 |
8.38 |
| South |
4200 |
1189 |
8.22 |
25,688 |
6163 |
6.80 |
| Northeast |
3391 |
236 |
1.75 |
26,108 |
757 |
0.71 |
| Hospital type | ||||||
| Metropolitan teaching |
4101 |
856 |
7.85 |
27,471 |
5011 |
4.97 |
| Metropolitan nonteaching |
4262 |
893 |
5.82 |
27,880 |
5821 |
5.71 |
| Nonmetropolitan | 3151 | 1087 | 10.59 | 15,117 | 5420 | 10.89 |
FIG. 2.
Charges segregated by hospital control. (a) Metropolitan hospital charges for patients admitted. (b) Metropolitan hospital charges for patients discharged from emergency department (ED).
Discussion
Emergency management of kidney stones represents a large and increasingly costly burden, representing a significant fraction of ED visits with increasing costs and numbers of visits. In the Urologic Diseases in America Project, total costs associated with treatment of stone disease in the United States were estimated to be more than 2 billion dollars in 2000, a figure that has likely increased substantially since that time.6 In addition, this study found that an increasing percentage of stone cases and costs were attributed to the ED, increasing from 14.9% of total costs in 1994 to 23.7% of total costs in 2000. Overall stone prevalence has increased since that time, with recently estimated prevalence of 10% in men, and 7% in women, representing an absolute increase of 4% and 3%, respectively, since 1994.7
In the current cost-conscious environment, identifying factors that may influence costs of care, as well as admission rates for management of stones may enable changes to streamline management of stones, and, ultimately, reduce the costs associated with stone management. We attempted to identify factors that may influence differences in costs among patients presenting to the ED with stones.
In assessing patient factors, we found infection, diabetes, and presence of pregnancy to be highly predictive of need for admission on multivariate analysis. In addition, patients with Medicare, followed by Medicaid, were noted to have higher rates of admission than those with private insurance. In the setting of Medicare and Medicaid, this is likely a result of higher levels of co-morbidities in this population. Interestingly, for patients who were self-pay, they had the lowest rate of admission. While the causes for this are unknown, it is likely that financial concerns in this population lead to decreased desire for inpatient management.
Unsurprisingly, the South region was noted to have nearly a two-fold higher number of stone presentations to the ED; however, it also had the lowest admission rate of any region. Interestingly, the South region also had the highest costs associated with ED visits. Whether this represents more efficient handling of stone presentations, that is, by performing more management in the ED before admission, or simply is related to differences in ED utilization rates between the regions is not clearly ascertainable from these data, and may represent an area of further investigation. Costs of admission were lowest within the Midwest region; however, cost increases over the years examined were lowest within the Northeast. While absolute costs between regions may be based on a number of factors, an analysis of the reasons behind discrepancies in cost changes may identify areas of cost containment that could be more widely implemented.
There were lower costs and admission rates associated with nonmetropolitan hospitals, although this was also associated with a greater than twofold higher rate of transfer to other facilities. This likely indicates that sicker and more complex patients are being referred to other (presumably metropolitan/teaching) medical centers, which may be a large factor in these cost differences.
While an analysis of this large database has provided for a broad assessment in trends for admission and cost associated with management of stones presenting to ED, and certain clear patient factors predicting admission were noted, the database is somewhat limited in determining causes for differences in cost and admission between the categories examined. Due to lack of standardized reporting tools to compare patient populations, such as Charlson Comorbidity Index, there is no straightforward way to correct for illness severity or baseline comorbidities between the groups examined, although the size of the database should average out significant outliers. In addition, reliance on coding data as opposed to individual chart review may result in certain errors in diagnosis and assessments, although there is no indication that this would be responsible for the differences noted within the study.
Conclusions
Upper tract urolithiasis represents a large and costly burden on the US health care system, and it represents a significant portion of ED visits. Certain factors, such as pregnancy, diabetes, and presence of infection, seem to indicate a higher likelihood of admission from the ED, leading to greater costs. Substantial differences in costs exist within the system, potentially exposing further paths of inquiry to attempt to control costs associated with the management of urolithiasis.
Abbreviations Used
- ED
emergency department
- HCUP
Healthcare Cost and Utilization Project
- ICD-9
International Classification of Diseases 9
- NEDS
Nationwide Emergency Department Sample
- UTI
urinary tract infection
Author Disclosure Statement
No competing financial interests exit.
References
- 1.Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med 2004;350:684–693 [DOI] [PubMed] [Google Scholar]
- 2.Graham A, Luber S, Wolfson AB. Urolithiasis in the emergency department. Emerg Med Clin North Am 2011;29:519–538 [DOI] [PubMed] [Google Scholar]
- 3.Pearle MS, Calhoun EA, Curhan GC, Urologic Diseases of America P. Urolithiasis Vol NIH Publication No. 07-5512-5 US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Washington, DC: US GovernmentPrinting Office, 2007. Available at http://kidney.niddk.nih.gov/statistics/uda/Urolithiasis-Chapter08.pdf (Accessed: March4, 2012) [Google Scholar]
- 4.HCUP Nationwide Emergency Department Sample (NEDS), Rockville, MD: Agency for Healthcare Research and Quality; Available at www.hcup-us.ahrq.gov/nedsoverview.jsp (Accessed: March4, 2012) [Google Scholar]
- 5.Semins MJ, Trock BJ, Matlaga BR. Validity of administrative coding in identifying patients with upper urinary tract calculi. J Urol 2010;184:190–192 [DOI] [PubMed] [Google Scholar]
- 6.Pearle MS, Calhoun EA, Curhan GC, Urologic Diseases of America P. Urologic diseases in America project: urolithiasis. J Urol 2005;173:848–857 [DOI] [PubMed] [Google Scholar]
- 7.Scales CD, Jr, Smith AC, Hanley JM, Saigal CS, Urologic Diseases in America P. Prevalence of kidney stones in the United States. Eur Urol 2012;62:160–165 [DOI] [PMC free article] [PubMed] [Google Scholar]