Abstract
Purpose
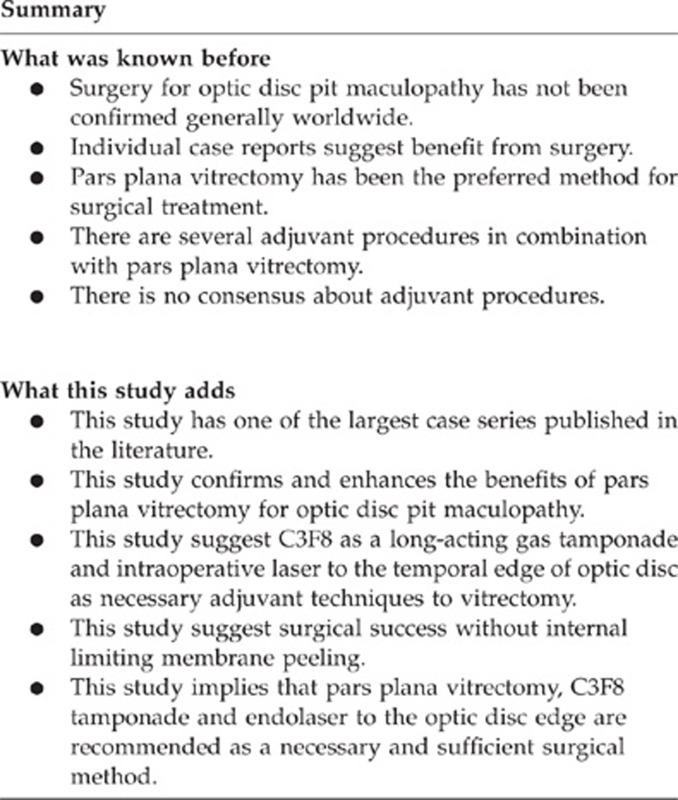
To evaluate the results of surgical treatment of maculopathy secondary to congenital optic pit anomaly with pars plana vitrectomy (PPV), endolaser to the temporal edge of the optic disc and C3F8 tamponade without internal limiting membrane (ILM) peeling.
Patients and methods
Thirteen eyes of 12 patients with serous macular detachment and/or macular retinoschisis secondary to congenital optic disc pit (ODP) were included in the study. All eyes underwent PPV, posterior hyaloid removal, endolaser photocoagulation on the temporal margin of the optic disc and 12% C3F8 gas tamponade. Anatomic success and functional outcome determined retrospectively by optical coherence tomography and measurement of best corrected visual acuity (BCVA), respectively were the main outcome parameters.
Results
Two lines or more improvement in BCVA was obtained in 11 eyes and 6 of these eyes had 20/40 or better BCVA at the final visit. Subretinal or intraretinal fluid was completely resorbed postoperatively in 12 eyes but a little intraretinal fluid persisted in one eye at the 16-month follow-up. Better visual improvement was observed in patients treated by earlier surgical intervention.
Conclusion
PPV, C3F8 gas tamponade and endolaser to the optic disc margin without ILM peeling may yield favourable results in the treatment of ODP maculopathy.
Keywords: internal gas tamponade, laser endophotocoagulation, optical coherence tomography, optic disc pit maculopathy, pars plana vitrectomy
Introduction
Congenital pits of the optic nerve head are a rare clinical entity affecting <1 in 10 000 persons.1, 2 Congenital optic disc pits (ODP) are bilateral in 10–15% of patients. Serous macular detachment associated with ODP develops within the second to fourth decades of life in 25–75% of cases.3, 4, 5, 6
Most authors thought that macular elevation associated with ODP represented serous retinal detachment even before the era of optical coherence tomography (OCT). The typical pattern of macular schisis seen on OCT helps us to differentiate this pathology from other macular elevations. This situation is observed not only due to serous macular detachment but also due to separation within the inner layers of the retina.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19
Treatment of ODP associated maculopathy is somewhat controversial because there is no consensus regarding the indications for surgical intervention, or the methods and techniques of surgery. Although there are several treatment options for this pathology, none of them has been generally accepted as a choice of treatment method that is shown to be superior to the other treatment methods.7, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40 Macular buckle surgery and optic nerve sheath fenestration were employed in the past.4, 11, 29, 30, 31, 32 Although pars plana vitrectomy (PPV) and gas tamponade was performed at least twenty years ago, this procedure with or without inner limiting membrane (ILM) peeling has become more widespread in recent years.28, 33, 34, 35, 36, 37, 41, 42, 43, 44, 45, 46, 47 Endolaser photocoagulation to the temporal edge of optic disc is controversial and not applied by all authors.20, 22, 36 Recently, intraretinal or subretinal fluid drainage has been reported as an additional procedure.29, 30, 42
The results of PPV, the removal of the posterior hyaloid, peripapillary argon laser photocoagulation on the temporal edge and C3F8 gas tamponade without ILM peeling for the treatment of ODP maculopathy in 13 eyes of 12 consecutive patients are reported in this study.
Patients and methods
ODP were identified as grey to white/yellow round or oval excavations in the optic nerve head. Maculopathy was diagnosed clinically by elevation of macula and confirmed by typical OCT findings in all eyes. Thirteen eyes of 12 consecutive patients diagnosed as ODP maculopathy between April 2007 and October 2011 were included in the study. Patients' records were retrospectively analysed. All patients were operated and included consequently in the study. Long-term outcomes of all patients were subsequently given in the results. Best corrected visual acuity (BCVA), data from full ophthalmological examination and OCT data before the surgery and at each follow-up were recorded.
Patients with complaints of visual acuity loss due to ODP maculopathy were offered surgery. The surgery was done in each patient after the nature of the disease and possible consequences of the surgery were explained. The study was performed with the agreement of the local ethics committee. Written and signed informed consent was obtained from each patient before inclusion in the study. Data from each patient were collected from hospital files and OCT archives. This retrospectively conducted case series study adhered to the tenets of the Declaration of Helsinki.
One patient had been previously treated at the same centre and had suffered recurrence before being included in the study. This patient had undergone PPV, posterior hyaloid separation and gas tamponade without laser photocoagulation at the temporal side of the optic disc in which postoperative visual acuity had increased and subretinal fluid resolved until she developed vision loss due to recurrent maculopathy at month 4. This patient was then included into this series and underwent PPV and C3F8 gas tamponade together with peripapillary laser photocoagulation. The other patients included in this series had not been treated previously for ODP maculopathy and underwent primary vitrectomy first time. None of the patients had any known systemic or ocular disease history. Clinical characteristics and OCT data of all cases are summarized in Table 1.
Table 1. Clinical characteristics and OCT findings of the patients with ODP and associated maculopathy.
| Patient | Age (years) | G | Eye | Pit location | Preoperative BCVA | *Duration of symptoms |
Type of macular elevation |
Duration until macular attachment* | Final BCVA | Follow-up* | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Double layer retinal detachment | Intraretinal separation | Serous macular detachment | ILM detachment | Outer layer hole | ||||||||||
| 1 | 60 | M | L | Temporal | 20/400 | 16 | − | + | − | − | − | 3 | 20/125 | 15 |
| 2 | 31 | F | R | Inferotemporal | 20/800 | 9 | + | + | + | − | − | 4 | 20/400 | 37 |
| 3 | 23 | F | L | Temporal | 20/125 | 36 | + | + | + | − | − | 3 | 20/40 | 9 |
| 4 | 27 | M | L | Temporal | 20/400 | 4 | + | + | + | − | − | 2 | 20/125 | 33 |
| 5 | 48 | F | R | Temporal | 20/800 | 3 | + | + | + | + | + | 2 | 20/63 | 14 |
| 6 | 23 | F | R | Temporal | 20/400 | 1 | + | + | + | − | − | 5 | 20/25 | 44 |
| 7 | 40 | M | L | Temporal | 20/200 | 1 | + | + | + | − | + | 3 | 20/25 | 9 |
| 8 | 28 | F | L | Temporal | 20/63 | 1 | + | + | + | − | − | 1 | 20/40 | 13 |
| 9 | 24 | F | L | Superotemporal | 20/100 | 1 | − | − | + | − | − | 14 | 20/32 | 18 |
| 10 | 68 | F | R | Inferotemporal | 20/125 | 8 | + | + | + | − | + | Incomplete | 20/50 | 16 |
| 11 | 49 | F | L | Inferotemporal | 20/2000 | 12 | + | + | + | − | − | 12 | 20/400 | 26 |
| 12 | 18 | M | R | Inside in coloboma | 20/125 | 1 | + | + | + | − | − | 1 | 20/20 | 54 |
| L | Inferotemporal | 20/200 | 1 | + | + | + | − | − | 1 | 20/20 | 50 | |||
Patient order in the table was given due to patient names on their files and not represents subsequent order of operations.
Abbreviations: BCVA, best corrected visual acuity; F, female; G, Gender; ILM, internal limiting membrane; L, left; M, male; ODP, optic disc pit; R, right;
+, present; −, absent; *, month.
All patients underwent the same surgical technique performed by the same surgeon (RA). A 3-port and 23-gauge small incision transconjunctival PPV was employed in all cases. Posterior hyaloid removal was attained by separation of the posterior hyaloid at the nasal edge of the optic disc with a vitrectomy probe applying active aspiration. Intraoperative triamcinolone acetone was used in all eyes to verify complete removal of vitreous at the posterior pole. Single line and 180° endolaser photocoagulation at mild to moderate intensity of 200 ms was applied to the retina in the temporal margin of the optic disc before the fluid air exchange. The tip of the laser probe was held as close to the retina as possible to induce smaller laser spots. Peeling of ILM was not attempted in any of the cases. Twelve percent of C3F8 gas was given as internal tamponade to produce a long-acting tamponade effect. Patients were instructed to adhere to facedown positioning for 10 days.
Spectral OCT (RTVue FD-OCT system, Optovue, Inc. Fremont, CA, USA) was used preoperatively and postoperatively in each follow-up to monitor the status of the maculopathy. Visual field investigation was used with Dicon LD 400 autoperimeter (Paradigm Medical Industries, Inc., San Diego, CA, USA) in one patient who developed enlarged laser scars.
ETDRS BCVAs were transformed into a logarithmic scale (LogMAR) before the statistical analysis was done. Statistical analysis was carried out with SPSS 18.0 for Windows. The results were analysed with nonparametric statistical methods. The relationship between preoperative and final BCVAs was calculated using the Wilcoxon signed rank test. To reveal the correlation between the postoperative functional and anatomical results and other parameters, the Spearman rank correlation test was used. Descriptive statistics were given as mean±SD. A P-value <0.05 was considered to be statistically significant.
Results
Clinical characteristics
The patients were four males and eight females with a mean age at presentation of 35.15±16.38 years (range, 18–68 years, median 28 years). ODP and associated maculopathy was bilateral in one patient. All pits except one were located on the temporal side of the disc. Four pits had an inferotemporal location, one pit was superotemporal and one pit was inside the disc coloboma. Seven of the 11 affected cases with a unilateral pit were left eyes. The duration of the complaints of visual loss ranged between 1 month and 36 months (mean 7.23±9.97 months, median 3 months). Preoperative BCVA was between logMAR 2.0 (20/2000) and logMAR 0.5 (20/63) (mean 20/440 (mean logMAR BCVA 1.13±0.43)). Median BCVA was 20/200 (LogMAR 1.0) preoperatively and 20/40 (LogMAR 0.3) at the final follow-up.
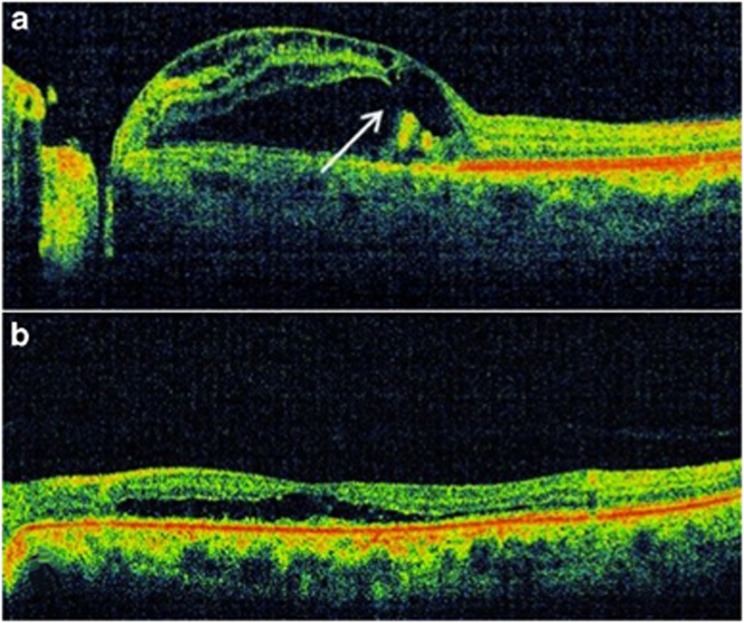
Preoperative OCT findings showed intraretinal separation and serous macular detachment (double layer detachment) in 11 eyes (Figure 1a), intraretinal separation alone in one eye (Figure 1b) and serous macular detachment alone in one eye (Figure 2a). In addition, a hole in the external layer was present in three eyes (Figure 1a). Posterior vitreous detachment was not observed in any of the eyes intraoperatively. Firm attachment of the posterior hyaloid was observed especially in the peripapillar region rather than the macula in eight eyes. Mean and median follow-up for all patients was 26.00±15.89 (9–54) months and 18 months, respectively.
Figure 1.
Preoperative OCT showing (a) double layer detachment and outer layer hole (arrow) in patient 7 in the table (preoperative VA was 20/200) and (b) intraretinal separation at the external layers of the retina and schisis cavity in patient 1 (preoperative VA was 20/400).
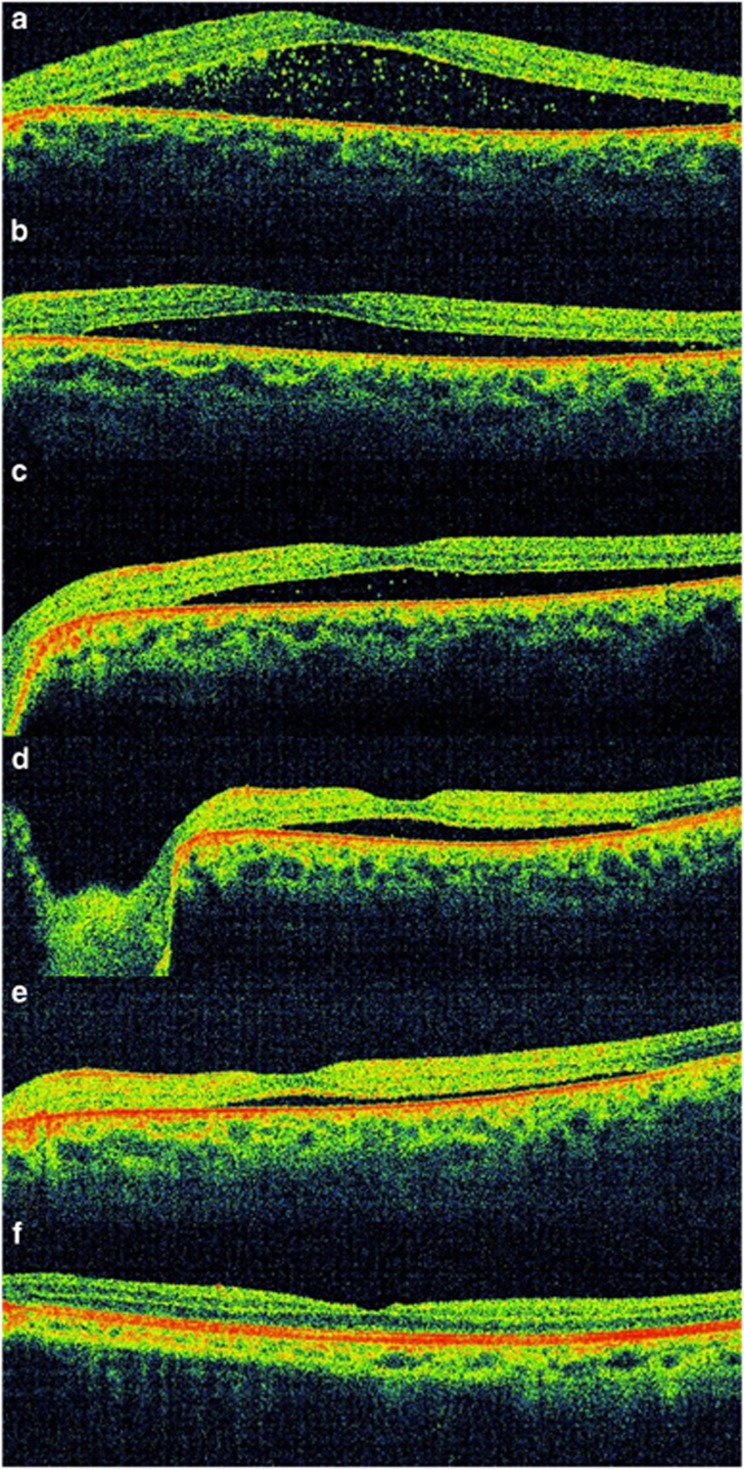
Figure 2.
Preoperative serous macular detachment in patient 9 (preoperative VA was 20/100 (a), gradual resolving of subretinal fluid at month 1 (20/80) (b), month 3 (20/63) (c), month 6 (20/40) (d), month 9 (20/40) (e) and month 14 (20/32) (f).
Anatomic results
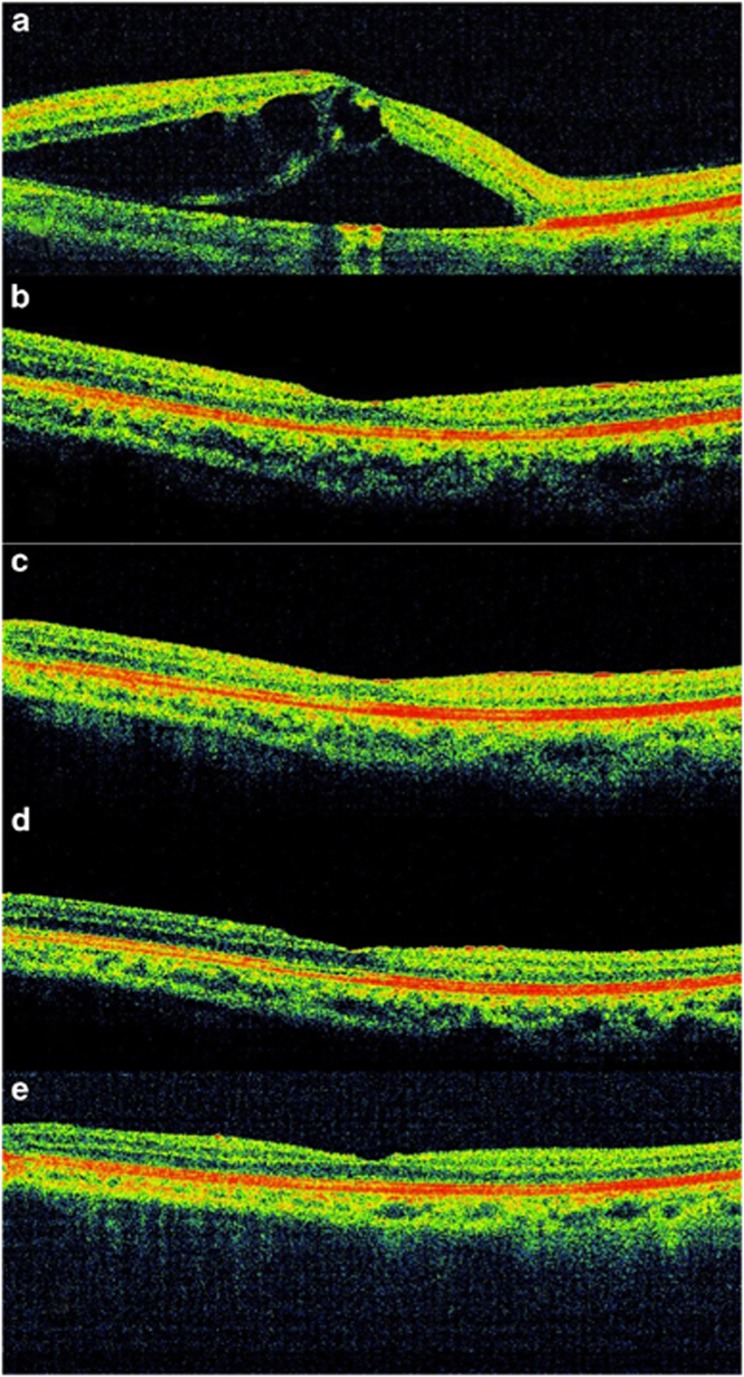
Postoperative complete anatomic improvement by OCT evaluation was detected in 12 eyes. The mean duration of morphological improvement was 4.25±4.29 months (range: 1–14 months, median 3 months) (Figures 2 and 3). Mean preoperative and final postoperative macular thickness was 611.8±249.1 and 254.6±29.6 μm, respectively (P:0.001). Complete macular reattachment was obtained during the first 3 months in eight cases (61.5%). Eleven eyes reached complete fluid reabsorption by month 12 (84.6%). All eyes except one reattached at month 14 (92.3%). Complete anatomic attachment could not be obtained in one eye during the 16-month follow-up period in spite of a decrease in fluid related to macular elevation and an increase in visual acuity.
Figure 3.
Preoperative serous macular detachment and large schisis cavity in the left eye of patient 12. Preoperative VA was 20/200 (a) macular detachment is seen to subside completely at postoperative month 1. VA at this point was 20/40. (b) Anatomic stabilization persisted at months 6 and 12 (VA was 20/25) (c,d) and month 24 (VA was 20/20) (e).
Visual acuity results
At the time of the final examination, BCVA had increased in all eyes (P<0.001). BCVA ranged between 20/400 and 20/20 (mean 20/105 and median 20/40). Mean and median BCVA was logMAR 0.47±0.45, (range: 1.3–0) and LogMAR 0.3, respectively at the final follow-up. An increase of two or more ETDRS lines in visual acuity was present in 11 eyes, of which 6 eyes had been operated within 1 month after the initial symptoms of vision loss and had visual acuity better than 20/50 (0.4 logMAR) at the final visit. Eighty-five percent of the patients gained two or more ETDRS lines of vision. Fifty-four percent of the patients obtained 20/40 or better postoperative BCVA at the final examination.
When noncomparative correlation by Spearman's bivariate analysis was computed to investigate a relationship between the patient characteristics and the results, some statistically significant outcomes were observed. The patient's age at presentation and duration of visual acuity loss were negatively correlated with the final BCVA (P=0.007, r=0.70 and P=0.003, r=0.76, respectively). The time from the onset of decrease in BCVA was also correlated positively with postoperative final macular thickness (P=0.038, r=0.60). Although the initial BCVA was correlated with the final BCVA (P=0.043, r=0.57), it showed no correlation with the final macular thickness. Negative correlation between the duration of symptoms (decline in VA) and the preoperative BCVA did not reach statistical significance. However, postoperative BCVA at months 3, 6, 9 and at the final follow-up was negatively correlated with the duration of symptoms at presentation (P=0.003, r=0.76 for final examination). Negative correlation between the preoperative or final BCVA and OCT values for macular thickness did not show any statistical significance. It seems that visual acuity is affected by the degenerative process rather than macular thickness itself in these patients. The duration of anatomic resolution was correlated with postoperative BCVA and macular thickness in the early period, but this correlation had disappeared at the final follow-up.
Complications
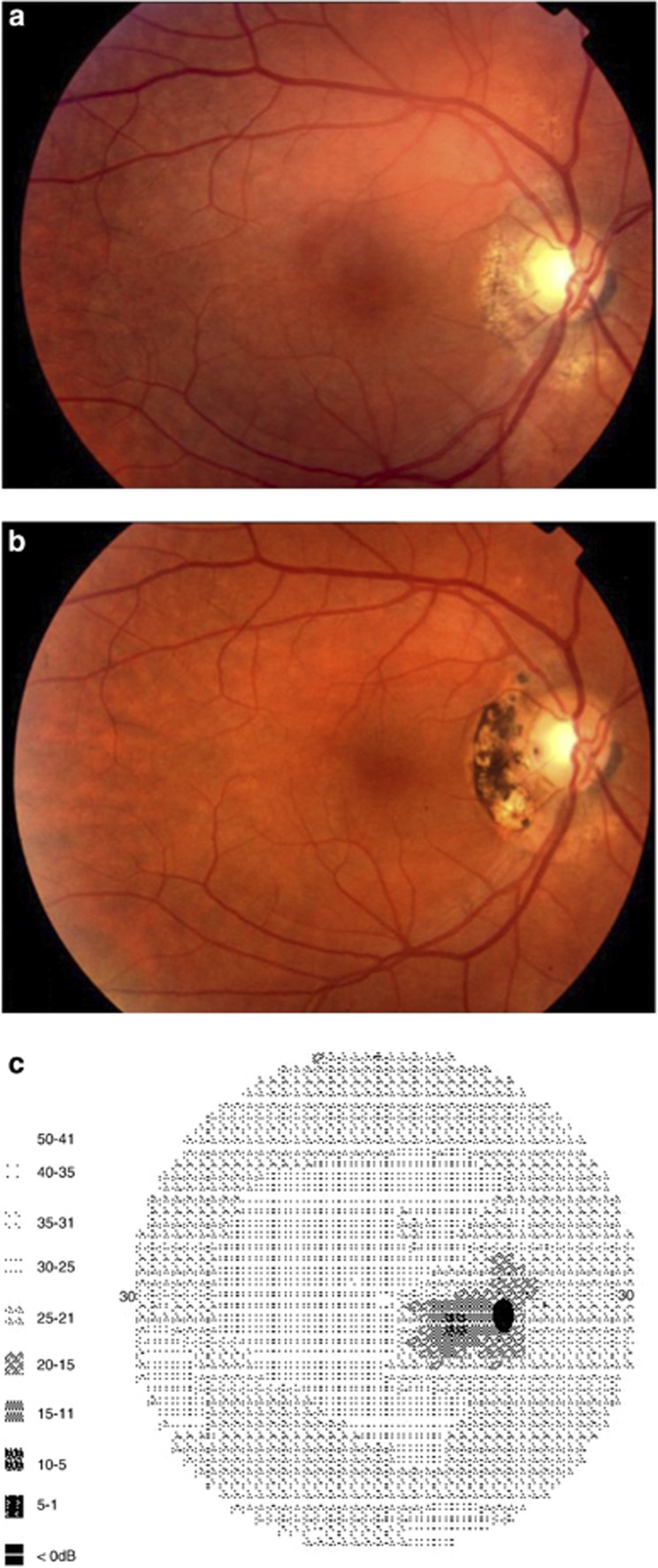
No intraoperative complications were observed during the surgery in any eyes. Cataract surgery was performed in two eyes (patients 1 and 5) due to progression of cataract during the postoperative follow-up period. An enlargement of peripapillary laser scars was observed in one patient who had been operated on previously and had developed recurrent maculopathy before inclusion in the study. Peripapillary scotoma in the visual field was detected in this patient although she had maintained improved visual acuity at the 3-year follow-up (Figures 4a–c). None of the other cases developed any enlargement in laser scars. Recurrence did not develop during the course of the follow-up in any of the patients after complete resolution had been observed.
Figure 4.
(a) Appearance of laser scars at the temporal edge of the optic disc of patient 6 at postoperative month 6 (preoperative VA was 20/400 and 20/200 at month 6), (b) enlargement of laser scars and (c) peripapillary scotoma in visual field testing of the same patient at postoperative year 3 (VA was 20/25).
Discussion
The surgical treatment of the ODP maculopathy provided high rates of anatomical and visual success in our series. An enlargement in laser scars in the papillomacular bundle adjacent to the temporal side of the optic disc was observed to develop in only one eye, which caused peripapillary scotoma without affecting central visual acuity. Resolution of maculopathy lasted 1–14 months with a mean 4-month duration in our series. This duration is probably due to the configuration of maculopathy related to the fluid coming from the optic pit. ODP maculopathy has been suggested to initiate with inner retinal splitting such as schisis, then return to serous macular detachment after development of a hole in the external retinal layers through which the intraretinal fluid passes to the subretinal space.12, 13, 14, 15, 16, 17, 18, 19 It has been reported that detachment of external retinal layers occurred secondarily in a group of patients in whom 10 out of 11 eyes had double layer detachment and 7 had a hole in external retinal layers.22 However, it was shown in a high resolution OCT study that a hole in the external retinal layers was not a common finding and that the fluid could pass through the optic pit directly into all layers of the sensorial retina, especially to beneath the internal limiting membrane, ganglion cell layer, and inner and outer nuclear layers in addition to the subretinal space.16, 17 In our study, 11 out of 13 eyes had fluid within the sensorial retina spreading into different layers in addition to the subretinal space; therefore, double layer detachment displayed on OCT was found in these eyes. This OCT finding was the most common configuration as observed in other reports published previously.12, 13, 14, 15, 16, 17, 18, 19 We found a hole in the outer retinal layers in only three eyes. We also detected only intraretinal schisis in one eye and only serous macular detachment in one eye by OCT evaluation. Our OCT finding of only subretinal fluid in one eye (Figure 2a) in which symptoms were reported to have begun 1 month before presentation may suggest that fluid rarely spreads through the optic pit directly to the subretinal space without disturbing the sensorial retinal layers.
Spontaneous resolution with visual improvement has been reported in 25% of cases with ODP maculopathy in which no treatment was selected except observation. However, development of macular hole causing permanent visual loss, foveolar cystic changes and degenerative retinal pigment epithelial changes can be observed during the resolution period in this group of patients.2, 4, 7, 10, 12, 33, 34 The poor final visual outcome in the natural course of spontaneously resolved maculopathy may lead to a surgical approach being the preferred modality of treatment at the time of diagnosis.24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 Therefore, we also opted to offer surgical treatment to all patients after diagnosis of ODP maculopathy. Patients with ODP maculopathy usually present with visual acuity worse than 20/70 and 80% of these eyes will progress to visual acuity worse than 20/200, when observed in their natural course. Better visual outcome has been reported in cases with ODP maculopathy undergoing surgical treatment.24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 In our study, visual acuity had improved at the final visit in all patients compared with preoperative levels. Six patients in our series were operated on within a 1-month period after the initiation of visual symptoms, and 20/40 or better visual acuity was obtained at the final follow-up in all of these patients. Favourable results from cases undergoing early surgery have suggested that the surgical option in the short term after the onset of visual symptoms may provide better visual prognosis. Therefore, earlier surgical intervention after the diagnosis of ODP maculopathy may be a better approach than the expectation of spontaneous resolution during the natural course.
Although various surgical techniques with different success rates have been reported in literature,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 PPV with gas endotamponade seems to be the preferred procedure when surgery is selected. Differences in techniques result from the selection of adjuvant procedures such as short or long-acting gas tamponade, ILM peeling, endolaser photocoagulation in the peripapillary area and drainage of subretinal fluid.27, 28, 29, 30, 33, 35, 36, 37, 40, 41, 42, 43, 44, 45, 46, 47
Hirakata et al22 reported favourable results in 10 out of 11 patients treated with vitrectomy and gas exchange without endolaser photocoagulation. Hirakata et al36 have also recently reported good surgical outcomes with vitrectomy but without laser treatment or gas tamponade for macular detachment with an optic disc pit.36 Georgalas et al40 reported successful results in two cases with vitrectomy, ILM peeling and gas tamponade without endolaser. They reported that laser photocoagulation was not performed to avoid any side effect of the laser treatment in the papillomacular region and also proposed that the rationale for the effect of laser photocoagulation on the prevention of fluid transportation to the inner retinal layers of the macula would be weak. On the other hand, Ghosh et al27 performed additional endolaser photocoagulation to the temporal side of the optic disc during surgery and reported that they could not see any side effects attributable to endolaser that was applied with low intensity. Brockhurst38 reported a series of six patients with congenital pits of the optic disc and serous macular detachment treated by xenon and argon laser photocoagulation. He reported that the cases with initial failure showed inadherent retina at some o'clock positions through which fluid passed into the retina and attached completely after additional photocoagulation applications were placed at these points. Bakri and Beer41 performed 360° peripapillary endophotocoagulation during vitrectomy and reported excellent visual acuity and anatomic reattachment in two cases.
The anatomical success rate of our series was 92.3% (12 out of 13 eyes) in which intraoperative endolaser was combined with vitrectomy and gas exchange. We suggest that laser photocoagulation at the temporal disc margin could increase surgical success by preventing fluid ingress into the retina with a barrier effect of chorioretinal scar formation. We consider that effects on the nerve fibre layer may not be so evident as to cause clinically important side effects such as central visual acuity loss. In addition, we did not observe any severe complications due to endolaser application to the temporal side of the optic disc in our series. We detected only blind spot enlargement in the visual field due to enlargement of laser scars in an asymptomatic patient with a longer follow-up. The enlargement of peripapillary laser scars did not affect central visual acuity. This patient had been included in the study after recurrence of ODP maculopathy following previous surgery without an endolaser and had maintained reattachment of the macula after successful resolution of maculopathy with the same surgical procedure containing an additional endolaser. Enlargement of laser scars has been found to occur in patients with diabetic retinopathy undergoing laser photocoagulation and has been observed with at least 4 years duration in 1.2% of laser scars, which developed after low-wavelength argon laser.48 We consider that endolaser photocoagulation to the temporal edge of the optic disc should be performed with mild to moderate laser power settings owing to the greater tendency for enlargement in laser scars arising from heavier laser burns, especially in the posterior pole.
Another controversial issue involving surgical technique in the treatment of ODP maculopathy is ILM peeling. Georgalas et al40 performed ILM peeling after the induction of PVD in order to completely eliminate any vitreoretinal traction in the macular area and facilitate the absorption of intraretinal and subretinal fluid. The same authors also reported a 5-year-old boy with ODP maculopathy treated with vitrectomy and ILM peeling without complete removal of the posterior hyaloid.45 Ishikawa et al46 also performed vitrectomy and induction of PVD followed by ILM peeling after intraoperative observation of very taut, dome-shaped ILM and a tangential tractional force on the retina in a child with ODP maculopathy. However, very thin internal layers of the retina with cystic structure and schisis cavity in ODP maculopathy can make it prone to develop macular hole while attempting ILM peeling during the surgery.35 The beneficial contribution of ILM peeling in addition to standard surgical procedure to better improve surgical and functional success is already controversial and remains to be established in future studies with larger series.
In conclusion, PPV, long-acting gas endotamponade and endolaser to the temporal side of the optic disc without ILM peeling may be a favoured option in the surgical management of ODP maculopathy with a good surgical outcome including both anatomical and functional improvement.
The authors declare no conflict of interest.
Footnotes
This study was presented in the XXVIIIth Meeting of the Club Jules Gonin, Reykjavik, Iceland, 20-23 June 2012.
References
- Kranenburg EW. Crater-like holes in the optic disc and central serous retinopathy. Arch Ophthalmol. 1960;64:912–924. doi: 10.1001/archopht.1960.01840010914013. [DOI] [PubMed] [Google Scholar]
- Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249:1113–1122. doi: 10.1007/s00417-011-1698-5. [DOI] [PubMed] [Google Scholar]
- Akiba J, Kakehashi A, Hikichi T, Trempe CL. Vitreous findings in cases of optic nerve pits and serous macular detachment. Am J Ophthalmol. 1993;116:38–41. doi: 10.1016/s0002-9394(14)71741-6. [DOI] [PubMed] [Google Scholar]
- Gass JD. Serous detachment of the macula secondary to congenital pit of the optic nerve head. Am J Ophthalmol. 1969;67:821–849. doi: 10.1016/0002-9394(69)90075-0. [DOI] [PubMed] [Google Scholar]
- Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980;87:51–65. doi: 10.1016/s0161-6420(80)35278-0. [DOI] [PubMed] [Google Scholar]
- Sugar HS. Congenital pits in the optic disc and their equivalents (congenital colobomas and colobomalike excavations) associated with submacular fluid. Am J Ophthalmol. 1967;63:298–307. [PubMed] [Google Scholar]
- Brodsky MC. Congenital optic disc anomalies. Surv Ophthalmol. 1994;39:89–112. doi: 10.1016/0039-6257(94)90155-4. [DOI] [PubMed] [Google Scholar]
- Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology. 1997;11:1539–1542. doi: 10.1016/s0161-6420(90)32380-1. [DOI] [PubMed] [Google Scholar]
- Polunina AA, Todorova MG, Palmowski-Wolfe AM. Function and morphology in macular retinoschisis associated with optic disc pit in a child before and after its spontaneous resolution. Doc Ophthalmol. 2012;124:149–155. doi: 10.1007/s10633-012-9314-5. [DOI] [PubMed] [Google Scholar]
- Ferry AP. Macular detachment associated with congenital pit of the optic nerve head. Pathologic findings in two cases simulating malignant melanoma of the choroid. Arch Ophthalmol. 1963;70:346–357. doi: 10.1001/archopht.1963.00960050348014. [DOI] [PubMed] [Google Scholar]
- Irvine AR, Crawford JB, Sullivan JH. The pathogenesis of retinal detachment with morning glory disc and optic pit. Retina. 1986;6:146–150. doi: 10.1097/00006982-198600630-00002. [DOI] [PubMed] [Google Scholar]
- Krivoy D, Gentile R, Liebmann JM, Stegman Z, Rosen R, Walsh JB, et al. Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996;114:165–170. doi: 10.1001/archopht.1996.01100130159008. [DOI] [PubMed] [Google Scholar]
- Brasil OF, Brasil MV, Brasil OM. Different presentations of intraretinal fluid collections in optic disc pits: OCT study of 3 cases. Arq Bras Oftalmol. 2006;69:745–747. doi: 10.1590/s0004-27492006000500024. [DOI] [PubMed] [Google Scholar]
- Imamura Y, Zweifel SA, Fujiwara T, Freund KB, Spaide RF. High-resolution optical coherence tomography findings in optic pit maculopathy. Retina. 2010;30:1104–1112. doi: 10.1097/IAE.0b013e3181d87ecb. [DOI] [PubMed] [Google Scholar]
- Rutledge BK, Puliafito CA, Duker JS, Hee MR, Cox MS. Optical coherence tomography of macular lesions associated with optic nerve head pits. Ophthalmology. 1996;103:1047–1053. doi: 10.1016/s0161-6420(96)30568-x. [DOI] [PubMed] [Google Scholar]
- Moon SK, Kim JE, Spaide RF. Optic pit maculopathy without inner retinal schisis cavity. Retina. 2006;26:113–116. doi: 10.1097/00006982-200601000-00023. [DOI] [PubMed] [Google Scholar]
- Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106:61–67. doi: 10.1001/archopht.1988.01060130067030. [DOI] [PubMed] [Google Scholar]
- McDonald HR, Schatz H, Johnson RN. Treatment of retinal detachment associated with optic pits. Int Ophthalmol Clin. 1992;32:35–42. doi: 10.1097/00004397-199203220-00005. [DOI] [PubMed] [Google Scholar]
- Schatz H, McDonald HR, Johnson RN. Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology. 1988;95:178–186. doi: 10.1016/s0161-6420(88)33197-0. [DOI] [PubMed] [Google Scholar]
- Theodossiadis G. Evolution of congenital pit of the optic disc with macular detachment in photocoagulated and nonphotocoagulated eyes. Am J Ophthalmol. 1977;84:620–631. doi: 10.1016/0002-9394(77)90375-0. [DOI] [PubMed] [Google Scholar]
- Yuen CH, Kaye SB. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: a case report. J AAPOS. 2002;6:330–331. doi: 10.1067/mpa.2002.127921. [DOI] [PubMed] [Google Scholar]
- Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005;112:1430–1435. doi: 10.1016/j.ophtha.2005.02.013. [DOI] [PubMed] [Google Scholar]
- Lincoff H, Kreissig I. Optical coherence tomography of pneumatic displacement of optic disc pit maculopathy. Br J Ophthalmol. 1998;82:367–372. doi: 10.1136/bjo.82.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annesley W, Brown G, Bolling J, Goldberg R, Fischer D. Treatment of retinal detachment with congenital optic pit by krypton laser photocoagulation. Graefes Arch Clin Exp Ophthalmol. 1987;225:311–314. doi: 10.1007/BF02153395. [DOI] [PubMed] [Google Scholar]
- Sandali O, Barale PO, Bui Quoc E, Belghiti A, Borderie V, Laroche L, et al. Long-term results of the treatment of optic disc pit associated with serous macular detachment: a review of 20 cases. J Fr Ophtalmol. 2011;34:532–538. doi: 10.1016/j.jfo.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Taiel-Sartral M, Mimoun G, Glacet-Bernard A, Delayre T, Coscas G. Vitrectomy-laser-gas for treating optic disc pits complicated by serous macular detachment. J Fr Ophtalmol. 1996;19:603–609. [PubMed] [Google Scholar]
- Ghosh YK, Banerjee S, Konstantinidis A, Athanasiadis I, Kirkby GR, Tyagi AK. Surgical management of optic disc pit associated maculopathy. Eur J Ophthalmol. 2008;18:142–146. doi: 10.1177/112067210801800126. [DOI] [PubMed] [Google Scholar]
- Dai S, Polkinghorne P. Peeling the internal limiting membrane in serous macular detachment associated with congenital optic disc pit. Clin Exp Ophthalmol. 2003;31:272–275. doi: 10.1046/j.1442-9071.2003.00652.x. [DOI] [PubMed] [Google Scholar]
- Spaide RF, Fisher Y, Ober M, Stoller G. Surgical hypothesis: inner retinal fenestration as a treatment for optic disc pit maculopathy. Retina. 2006;26:89–91. doi: 10.1097/00006982-200601000-00014. [DOI] [PubMed] [Google Scholar]
- Jalil A, Stavrakas P, Dhawahir-Scala FE, Patton N. Drainage of subretinal fluid in optic disc pit maculopathy using subretinal 42-gauge cannula: a new surgical approach. Graefes Arch Clin Exp Ophthalmol. 2010;248:751–753. doi: 10.1007/s00417-010-1321-1. [DOI] [PubMed] [Google Scholar]
- Theodossiadis GP. Treatment of maculopathy associated with optic disc pit by sponge explant. Am J Ophthalmol. 1996;121:630–637. doi: 10.1016/s0002-9394(14)70628-2. [DOI] [PubMed] [Google Scholar]
- Theodossiadis GP, Theodossiadis PG. The macular buckling technique in the treatment of optic disc pit maculopathy. Semin Ophthalmol. 2000;15:108–115. doi: 10.3109/08820530009040001. [DOI] [PubMed] [Google Scholar]
- Snead MP, James N, Jacobs PM. Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol. 1991;75:381–382. doi: 10.1136/bjo.75.6.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postel EA, Pulido JS, McNamara JA, Johnson MW. The etiology and treatment of macular detachment associated with optic nerve pits and related anomalies. Trans Am Ophthalmolol Soc. 1998;96:73–88. [PMC free article] [PubMed] [Google Scholar]
- Shukla D, Kalliath J, Tandon M, Vijayakumar B. Vitrectomy for optic disc pit with macular schisis and outer retinal dehiscence. Retina. 2012;32:1337–1342. doi: 10.1097/IAE.0b013e318235d8fc. [DOI] [PubMed] [Google Scholar]
- Hirakata A, Inoue M, Hiraoka T, Mccuen BW., 2nd Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012;119:810–818. doi: 10.1016/j.ophtha.2011.09.026. [DOI] [PubMed] [Google Scholar]
- Garcia-Arumi J, Guraya BC, Espax AB, Castillo VM, Ramsay LS, Motta RM. Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefe's Arch Clin Exp Ophthalmol. 2004;242:819–826. doi: 10.1007/s00417-004-0897-8. [DOI] [PubMed] [Google Scholar]
- Brockhurst RJ. Optic pits and posterior retinal detachment. Trans Am Ophthalmol Soc. 1975;73:264–291. [PMC free article] [PubMed] [Google Scholar]
- Lincoff H, Yannuzzi L, Singerman L, Kreissig I, Fisher Y. Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol. 1993;111:1071–1079. doi: 10.1001/archopht.1993.01090080067020. [DOI] [PubMed] [Google Scholar]
- Georgalas I, Petrou P, Koutsandrea C, Papaconstadinou D, Ladas I, Gotzaridis E. Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: a report of two cases. Eur J Ophthalmol. 2009;19:324–326. doi: 10.1177/112067210901900230. [DOI] [PubMed] [Google Scholar]
- Bakri SJ, Beer PM. Vitreoretinal surgery for optic pit associated serous macular detachment: a discussion of two cases. Int Ophthalmol. 2004;25:143–146. doi: 10.1007/s10792-004-5197-0. [DOI] [PubMed] [Google Scholar]
- Ehlers JP, Kernstine K, Farsiu S, Sarin N, Maldonado R, Toth CA. Analysis of pars plana vitrectomy for optic pit-related maculopathy with intraoperative optical coherence tomography: a possible connection with the vitreous cavity. Arch Ophthalmol. 2011;129:1483–1486. doi: 10.1001/archophthalmol.2011.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziahosseini K, Sanghvi C, Muzaffar W, Stanga PE. Successful surgical treatment of optic disc pit maculopathy. Eye. 2009;23:1477–1479. doi: 10.1038/eye.2008.211. [DOI] [PubMed] [Google Scholar]
- Konno S, Akiba J, Sato E, Kuriyama S, Yoshida A. OCT in successful surgery of retinal detachment associated with optic nerve head pit. Ophthalmic Surg Lasers. 2000;31:236–239. [PubMed] [Google Scholar]
- Georgalas I, Kouri A, Ladas I, Gotzaridis E. Optic disc maculopathy treated with vitrectomy, internal limiting membrane peeling, and air in a 5-year-old boy. Can J Ophthalmol. 2010;45:189–191. doi: 10.3129/i09-215. [DOI] [PubMed] [Google Scholar]
- Ishikawa K, Terasaski H, Mori M, Sugita K, Miyake Y. Optical coherence tomography before and after vitrectomy with internal limiting membrane removal in a child with optic disc pit maculopathy. Jpn J Ophthalmol. 2005;49:411–413. doi: 10.1007/s10384-004-0225-1. [DOI] [PubMed] [Google Scholar]
- Cox MS, Witherspoon CD, Morris RE, Flynn HW. Evolving techniques in the treatment of macular detachment caused by optic nerve pits. Ophthalmology. 1988;95:889–896. doi: 10.1016/s0161-6420(88)33078-2. [DOI] [PubMed] [Google Scholar]
- Maeshima K, Utsugi-Sutoh N, Otani T, Kishi S. Progressive enlargement of scattered photocoagulation scars in diabetic retinopathy. Retina. 2004;24:507–511. doi: 10.1097/00006982-200408000-00002. [DOI] [PubMed] [Google Scholar]