Abstract
Objective
Mindfulness-based interventions have enjoyed a marked increase in support within biomedical and psychological research and practice in the past two decades. Despite the widespread application of these treatments for a range of psychological and medical conditions, there remains a lack of consensus regarding mechanisms through which these interventions effect change. One plausible yet underexplored mechanism is the therapeutic alliance between participants and mindfulness instructors.
Methods
In this report, data are presented on therapeutic alliance from the mindfulness arm (n = 37) of a randomized controlled trial of a mindfulness-based smoking cessation treatment.
Results
Results suggest that client-reported therapeutic alliance measured mid-treatment did not significantly predict primary smoking outcomes. Alliance did predict improvement in post-treatment scores on several outcome variables linked to mindfulness practice, including emotion regulation (β =−.24, p = .042), mindfulness (β = .33, p = .007), negative affect (β = −.33, p = .040), as well as treatment compliance (β = .39, p = .011).
Conclusion
Implications of these relationships and the possible role of therapeutic alliance in mindfulness treatments are explored.
Keywords: mindfulness, therapeutic alliance, mechanisms, smoking cessation, addiction, group treatment
Introduction
Mindfulness has been defined as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally” (Kabat-Zinn, 1994, p. 4), and mindfulness practices have been hypothesized to improve moment-to-moment awareness, acceptance and non-reactivity to thoughts, sensations, and emotions (Baer, 2003; Bishop et al., 2004). Therapies that utilize training in mindfulness practices have enjoyed increasing support in the past two decades. Interest has “quietly exploded” (Brown, Ryan & Creswell, 2007, p. 211), with the number of publications on mindfulness climbing from 80 in 1990 to over 600 in 2006. With origins in Buddhist practices, the theoretical foundations of mindfulness have been imported into a Western biomedical framework through the work of practitioners and researchers in medicine and psychology (Grossman, Niemann, Schmidt & Walach, 2004). This process has been fruitful, such that today there are an expanding number of mindfulness-based approaches to a variety of psychological and medical conditions and a growing research base to support their dissemination (for a review, see Hofmann, Sawyer, Witt, & Oh, 2010; Mars & Abbey, 2010).
Recently, mindfulness researchers have been encouraged to implement more rigorous research designs for testing the efficacy and mechanisms of various treatments (Baer, 2003; Coelho, Canter, & Ernst, 2007). This shift has included an increased emphasis on randomized controlled trials for assessing the unique therapeutic contributions that mindfulness approaches may provide. Along similar lines, researchers are now attempting to determine what processes mediate the observed treatment effects of mindfulness training. Potential mediators of interest include changes in attention regulation, body awareness, emotion regulation, and view of the self (Hölzel et al., 2011).
Modern mindfulness therapies commonly occur in a group setting and are lead by a mindfulness instructor. As in all group-structured therapies, some degree of therapeutic alliance is assumed to occur as a result of participant-instructor interactions (Yalom & Leszcz, 2005). Therapeutic alliance may be defined as the affective bond between client and therapist as well as mutual agreement between client and therapist on the goals and tasks of psychological intervention (Bordin, 1979; Horvath & Greenberg, 1989). Therapeutic alliance is seen by many researchers as playing a central role in outcomes across a range of psychotherapies (Horvath & Symonds, 1991; Horvath, Del Re, Fluckiger & Symonds, 2011; Martin, Garske & Davis, 2000), although it has remained essentially unstudied in mindfulness-based interventions.
A substantial literature within counseling and clinical psychology has long recognized the importance of therapeutic alliance. Meta-analytic evidence supports therapeutic alliance as an important factor in psychotherapy outcomes, with treatment outcomes correlating r = .28 with therapeutic alliance measured during treatment (Horvath et al., 2011). In addition, meta-analytic evidence suggests that the relationship between therapeutic alliance and therapeutic outcome persists across treatment types (e.g., behavioral, cognitive), raters (i.e., client, therapist, observer), time of alliance assessment (i.e., early in treatment, late in treatment), and outcome measure (Fluckiger, Del Re, Wampold, Symonds, & Horvath, 2012; Horvath et al., 2011; Martin, Garske, & Davis, 2000).
To our knowledge, Imel, Baldwin, Bonus and MacCoon (2008) conducted the only study that has explored the role of “non-mindfulness” pathways, such as group-effects, within a mindfulness-based treatment. Imel et al. re-analyzed archived data from 59 Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990) groups using multi-level modeling. This analysis found that 7% of variance in psychological symptom outcomes was accounted for by the group. Although Imel et al. made an important first step in showing that group appears to impact outcomes in mindfulness treatments, the report was not designed to address the underlying question of what caused this variability. Variation in therapeutic alliance, related in part to group and therapist effects, has been proposed as one such proximal mechanism (Wampold, 2001).
Although extant literature suggests that therapeutic alliance would significantly predict outcome in mindfulness treatments as well (given that it predicts outcome across other treatment types), to our knowledge no published research has yet demonstrated this relationship. Much of the literature on the mechanisms of change in mindfulness interventions to date has emphasized mindfulness-specific factors such as the development of different ways of paying attention and relating to one’s moment-to-moment experience, emotion regulatory skills, and body awareness (Brown & Ryan, 2003; Carmody, Baer, Lykins, & Olendzki, 2009; Hölzel et al., 2011) and intervention-specific factors such as duration and quality of mindfulness practice (Del Re, Fluckiger, Goldberg, & Hoyt, 2012; Vettese, Toneatoo, Stea, Nguyen, & Wang; 2009). Given the introspective nature of mindfulness practice, it is theoretically plausible that alliance with one’s mindfulness instructor is simply less important than in other forms of therapy. It is also theoretically plausible, however, that the alliance would matter a great deal in mindfulness interventions due to the role of the instructor in creating a context of emotional safety necessary for participants look directly into their moment-to-moment experience (Kabat-Zinn, 2011) and to allow for instructor modeling of mindful behavior (Wilson & Sandoz, 2008). As participant and mindfulness instructor practice together, it would be hypothesized that some degree of alliance would likely form and that this alliance might predict the acquisition of mindfulness skills or other treatment outcomes.
The current study sought to examine the relation between therapeutic alliance and treatment outcomes in the context of a mindfulness-based smoking cessation intervention—Mindfulness Training for Smokers (MTS; Davis et al., in press). Principal study hypotheses proposed that therapeutic alliance would predict the following outcomes:
| H1: | Therapeutic alliance would predict changes in psychological functioning and mindfulness. |
| H2: | Therapeutic alliance would predict participant compliance with the MTS course requirements. |
| H3: | Therapeutic alliance would predict smoking cessation outcomes. |
Methods
Intervention
Participants received a mindfulness-based smoking cessation intervention in a group format (MTS; Davis et al., in press), based substantively on MBSR (Kabat-Zinn, 1990) but providing mindfulness skills training targeted to the management of smoking relapse challenges. The course consisted of ten group meetings over the span of 8-weeks: a 7-hour initial introductory day, four weekly 3-hour pre-quit mindfulness class meetings, a 7-hour quit-day retreat, and four weekly 1.5-hour post-quit mindfulness group meetings. Three mindfulness instructors were recruited to provide the intervention and were additionally trained through a 2-day manualized training course by the MTS program developer. The instructors had all previously received training in various meditation traditions including mindfulness-based Vipassana meditation and concentration practices. The three instructors had practiced meditation for 41, 38, and 15 years respectively (M = 31.3) and taught meditation for 38, 36, and 8 years respectively (M = 27.3). Each of the 8 waves of participants was assigned one of the three instructors.
The MTS instructors, with use of the MTS Instructional DVD, taught general mindfulness practices such as mindfulness meditation, mindful walking, and mindful eating. Targeted instruction was also provided on how to use mindfulness skills to overcome specific relapse challenges such as smoking triggers, urges, addictive thoughts and negative emotions. During each class instructors would provide 20 minutes of standardized instruction through the MTS DVD. The DVD provided instruction by addiction experts, mindfulness instructors, physicians and past participants. After playing each section of the DVD, MTS instructors would teach mindfulness practices, and address questions related to the DVD. The quit-day retreat was comprised of 7-hours of instructor-guided mindfulness practice and was conducted mostly in silence. The four post-quit mindfulness group meeting included formal mindfulness practice and time for group discussion.
Throughout the MTS intervention participants were asked to practice 30 minutes of guided meditation per day at home with a 30-minute guided meditation CD. The CD provided guidance in mindfulness skills specifically targeted for managing relapse challenges and included exercises in mindful attention to physical sensation, emotion, and thoughts. Participants received a copy of the MTS Manual, which provided an expanded version of the concepts and exercises available on the DVD. Participants were provided with access to all materials through the MTS website www.sittoquit.com.
Participants received four weeks of 21 mg nicotine patches and access to the Wisconsin Tobacco Quit Line, a national telephonic smoking cessation service that provides behavioral strategies and brief phone counseling.
Participants were recruited through newspaper, television advertisements, and flyers posted in a medium-sized Midwestern city. Materials advertised a “Quit Smoking Study” that provided training in mindfulness meditation, free medication, and $90 for study completion. Inclusion criteria included that participants had to be at least 18 years old and smoke at least five cigarettes per day. Participants were excluded prior to randomization if they reported the use of tobacco products other than cigarettes (e.g., chewing tobacco, snuff), the consumption of four or more alcoholic drinks on four or more nights per week, or major depression or suicidality.
Participants were grouped in treatment waves (n = 8) over the course of approximately one year. An initial baseline study visit occurred prior to the beginning of treatment, typically within two weeks of the first mindfulness class. Therapeutic alliance measures were completed five weeks into the intervention during the quit day. Post-test measures were completed approximately one-month following the quit day. The larger randomized controlled trial also included a six-month post-quit follow-up study visit and has been reported elsewhere (Davis et al., in press).
Participants
The analysis sample (n = 37) included all mindfulness group participants who completed alliance measures (assessed at the quit day) and attended the 4-week post-quit study visit. The alliance study sample was drawn from the larger sample of n = 196 participants recruited to participate in a randomized controlled mindfulness-based smoking cessation intervention. Within this larger sample, n = 105 participants were randomized to the mindfulness condition with the remaining participants (n = 91) offered only the Quit Line and nicotine patches (Davis et al., in press). Of the subsample randomized to the mindfulness condition, 57.1% (n = 60) attended the first mindfulness class, with 41.0% (n = 43) attending the quit day, 41.9% (n = 44) attending the post-quit study visit, with 35.2% (n = 37) completing the alliance measure. This high level of attrition is not inconsistent with that found in other mindfulness-based substance use treatments (for a review, see Zgierska et al., 2009) or other smoking cessation interventions targeted at more recalcitrant smoking populations (Prochaska, Delucchi, & Hall, 2004).
The study sample was almost entirely Caucasian with an even distribution of males and females (Table 1). The highest degree earned by participants included: high school diploma = 11, associates degree = 10, bachelors degree = 13, masters degree = 3. The modal participant reported smoking 18.1 cigarettes per day for the past 24.2 years with 10.9 previous quit attempts and reported a 4.5 on the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, et al., 1991) suggesting medium-level nicotine dependence. Independent t-tests conducted comparing the analysis sample with those randomized to the mindfulness condition showed the analysis sample included participants with higher levels of education (t(99) = 2.64, p = .010), a lower percentage of racial/ethnic minority individuals (t(99) = −2.22, p = .029), and more cigarettes smoked per day (t(99) = 2.19, p = .031). Groups did not differ on other baseline demographic and smoking history characteristics including levels of nicotine dependence (FTND).
Table 1.
Baseline demographic and smoking-related characteristics.
| Variable | n | Mean (SD) | % |
|---|---|---|---|
| Age | 42.1 (12.3) | ||
| Gender (Female) | 20 | 54.1 | |
| Racial/Ethnic Minority | 2 | 5.4 | |
| Bachelors degree or higher | 16 | 43.2 | |
| Years Smoked | 24.2 (12.5) | ||
| Cigarettes Smoked Per Day | 18.1 (9.3) | ||
| Previous Quit Attempts | 10.9 (21.9) | ||
| Longest Period Abstinent (months) | 24.4 (39.77) | ||
| FTND Score | 4.5 (2.5) |
Note: Total n = 37; FTND = Fagerstrom Test for Nicotine Dependence, α = .74 in the current sample.
Measures
Baseline Demographic Questionnaire
A questionnaire was completed by all participants at the baseline study visit assessing demographic characteristics and smoking history.
Smoking Behavior
Two metrics were used to assess post-quit day smoking behavior: a self-report “time-line follow-back” smoking calendar (Sobell, Sobell, Leo, & Cancilla, 1988) and biomedical testing via carbon monoxide (CO) breath testing. Participants were asked to log cigarette consumption each day throughout the intervention. Calendar data for smoking in the two weeks following the quit day served as a continuous variable for smoking abstinence. The use of the number of days smoked in the first two weeks post-quit is a contemporary measure of smoking abstinence that correlates highly with measures of long-term (six-month) abstinence, provides more statistical power than dichotomous outcomes, and generally has less missing data than long-term abstinence measures (Baker et al., 2011).
Biochemically-confirmed seven-day point prevalence abstinence was assessed one-month post-quit and served as a dichotomous measure of smoking behavior. In order to be considered abstinent, participants had to both self-report no cigarette consumption in the seven days prior to the post-quit study visit as well as obtain a reading below 7.0 ppm via expired CO breath test. A 7.0 ppm cut-off has been used elsewhere and found to be a satisfactory balance between sensitivity and selectivity (Middleton & Morice, 2000).
Nicotine Dependence
The Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) was administered at baseline to assess smoking addiction severity. The FTND is a six-item measure intended to determine to what extent an individual has developed a biological dependence on nicotine, with higher scores indicating greater dependence. The FTND was included to assess the severity of nicotine dependence in the sample and improve generalizability of findings. The measure possesses fair internal consistency (α= .61) and correlates well with biological indices of heaviness of smoking (Heatherton et al, 1991). Items assess indicators of nicotine dependence such as, “How soon after you wake up do you smoke your first cigarette?” and “How many cigarettes do you smoke per day?”
Treatment Compliance
Self-reported daily minutes meditated was used to assess treatment compliance. This was assessed via telephone calls made to participants during which they were asked how many minutes they had practiced meditation in the past 24 hours. Calls were made once a day for five days prior to the beginning of treatment and once a day for five days after the quit day. Reported minutes meditated was averaged across all five calls in each time period, yielding an average number of minutes pre-intervention and post-quit day.
Psychological Functioning
Psychological functioning was assessed using two self-report measures.
The Depression, Anxiety and Stress Scales (DASS; Lovibond & Lovibond, 1995) were used to assess psychological symptoms and involved the report of negative affect and somatic symptoms over the past week. The DASS were included to assess negative affect, a known cause of relapse (Kenford et al., 2002) and one hypothesized mechanism by which MTS may work. This 42-item scale has been used extensively and has good psychometric qualities, with the depression, anxiety and stress subscales possessing internal consistencies of α = 0.91, 0.84, and 0.90, respectively. In addition, the depression and anxiety subscales correlate strongly with the Beck Depression Inventory (r = 0.74; Beck, Steer, & Brown, 1996) and Beck Anxiety Inventory (r = 0.81; Beck, Epstein, Brown, & Steer, 1988). Items from the three subscales include symptoms related to anxiety (e.g. “I felt scared without any good reason”), depression (e.g. “I felt that life wasn’t worthwhile”), and stress (e.g. “I found it hard to wind down”). In order to decrease Type I error rates by running multiple tests with a relatively small sample, a total score was used in analyses, with higher scores indicating more negative affect.
The Difficulty in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was used to look at both emotional arousal and reaction to emotional arousal in terms of awareness, understanding and acceptance of emotions as well as behavioral concomitants. The DERS was included to assess predictors of relapse by which MTS may assist smokers attempting to quit. The scale is 41 items and has high internal consistency (α= .93), with higher scores indicating more difficulty in emotion regulation. Although the measure yields six subscales, a single total score was used for all analyses in order to decrease Type I error rates. The DERS possesses adequate construct validity as assessed by its correlation (r = −.69) with the Negative Mood Regulation scale (NMR; Catanzaro & Mearns, 1990), a commonly used measure of emotional regulation. The DERS total score has demonstrated strong predictive ability for behavioral outcomes relevant to emotion regulation, predicting frequency of deliberate self-harm for both men and women (r = .26 and .20, respectively) and frequency of intimate partner abuse for men (r = .34). The DERS has shown good test-retest reliability (α = .88; Gratz & Roemer, 2004). Items ask respondents to indicate how often various statements apply to them, such as “I experience my emotions as overwhelming and out of control” or “I pay attention to how I feel.”
Mindfulness
A widely used self-report instrument served as the primary measure of mindfulness. The Five Facet Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) has been shown to possess adequate psychometric properties including good construct and predictive validity (Baer et al., 2008) as well as adequate internal reliability for all five subscales (αs = .75 to .91; Baer et al., 2006). The 39-item1 scale was designed to measure dispositional tendencies individuals may possess or learn through mindfulness training to be attentive and accepting in daily life, with higher scores indicating higher levels of these tendencies. The FFMQ was included to measure the impact of the MTS intervention on participant levels of mindfulness. Sample items for each of the five factors include “When I’m walking, I deliberately notice the sensations of my body moving” (observe), “I’m good at finding words to describe my feelings” (describe), “When I do things, my mind wanders off and I’m easily distracted” (acting with awareness), “I perceive my feelings and emotions without having to react to them” (non-reactivity), and “I criticize myself for having irrational or inappropriate emotions” (non-judgmental). While the FFMQ includes five subscales, a total score was used for all analyses to reduce Type I error rate and avoid over-interpretation of artifactual differences between subscales. Although there has been some debate regarding whether or not the FFMQ total score is psychometrically sound (e.g., Van Dam, Hobkirk, Danoff-Burg, & Earleywine, 2012), the FFMQ total score has been used in previous research (e.g., Greason & Cashwell, 2009; Lykins & Baer, 2009; Roberts & Danoff-Burg, 2010; Vollestad, Sivertesen, & Nielsen, 2011) as well as specifically in research on mindfulness and substance use (e.g., Brewer et al., 2009; Garland, Boettiger, Gaylord, Chanon, & Howard, 2011).
Working Alliance Inventory – Group Version
The Working Alliance Inventory Group Version (WAI-G; Hoyt & Goldberg, 2012) is a 20-item self-report measure that was used to assess the strength of therapeutic alliance between participants and mindfulness instructors. This instrument is based closely on Horvath and Greenberg’s Working Alliance Inventory (WAI; 1989) but was adapted for use in group counseling settings, with the instrument shortened from the original 36-item form. The original WAI has been shown to possess adequate internal consistency (α =.93; Horvath & Greenberg, 1989). WAI composite scores assessed early in treatment have been shown to predict client-reported satisfaction with psychotherapy (r = .50) as well as client-reported change in psychotherapy (r = .33; Horvath & Greenberg, 1989). The WAI is composed of three subscales—bond, task, and goal—which correspond to aspects of Bordin’s (1979) conceptualization of therapeutic alliance.
In a validation study of the WAI-G based on n = 254 undergraduates involved in interpersonal process groups, the measure showed acceptable test-retest reliability at three- and six-week intervals (rs = .79 and .70, respectively; Hoyt & Goldberg, 2012). The measure also demonstrated acceptable internal consistency reliability (α = .94).
The WAI-G also contains items corresponding to the three aspects of therapeutic alliance. Sample items include: “The instructor and I understand one another” (bond), “I am clear as to what the instructor wants me to do in these meetings” (task), and “The instructor perceives accurately what my goals are” (goal). For the current study, a single composite score was computed including all 20 items in lieu of individual subscales, with higher scores indicating stronger working alliance. This decision was based on previous research demonstrating high subscale inter-correlations (rs = .69 to .92; Horvath & Greenberg, 1989) and a good fitting hierarchical factor model for the full WAI (Tracey & Kokotovic, 1989). Internal reliability computed for this composite score based on data collected in the present study demonstrated adequate internal consistency (α = .89).
Results
Paired samples t-tests were conducted examining pre-post changes (Table 2). Significant improvements were found in mindfulness and emotion regulation. Cohen’s (1988) d effect sizes for these changes would be considered medium-sized in magnitude for mindfulness (d = .58) and small for emotional regulation (d = .30). No changes were found in negative affect. Internal reliability coefficients computed on study sample pre-test data are all within the acceptable range and are also displayed in Tables 1 and 2.
Table 2.
Pre- and post-treatment means, standard deviations, paired t-tests, and reliability coefficients.
| Measure | Pre-test | Post-test | t | p-value | Cohen's d | α |
|---|---|---|---|---|---|---|
| Negative Affect (DASS) | 0.61 (0.39) | 0.63 (0.46) | 0.31 | .757 | −0.05 | 0.95 |
| Emotion Regulation (DERS) | 2.08 (0.53) | 1.92 (0.50) | −2.47 | .018** | 0.30 | 0.93 |
| Mindfulness (FFMQ) | 3.33 (0.50) | 3.62 (0.54) | 4.29 | < .001*** | 0.58 | 0.92 |
Note: n = 37 and degrees of freedom = 36 for all tests; DASS = Depression, Anxiety, and Stress Scales; DERS = Difficulty in Emotion Regulation Scale, a higher score indicates greater difficulty in emotion regulation; FFMQ = Five-Facet Mindfulness Questionnaire, total score computed using all items; α = Cronbach’s internal reliability coefficient computed from pre-test data. Cohen’s d computed using mean difference scores divided by pre-test standard deviation, with directions changed so that a larger d reflects improvement on given variable.
p <.05;
p < .01;
p < .001
Overall, the sample reported a high level of therapeutic alliance (M = 6.13 out of 7, SD = 0.75). A random effects one-way ANOVA was conducted to see if alliance ratings varied significantly by instructor. There was not significant variation in ratings of alliance between the three instructors (F(2, 34) = 2.34, p = .112). Further, the intraclass correlation coefficient (ICC) assessing the relative degree of similarity between ratings made of a given instructor was small (ICC = .10). As this primary test did not yield significant between-instructor variation in alliance, and as more instructors (i.e., level two units) would be necessary for an adequately powered hierarchical linear model (Snijders & Bosker, 2012), instructor variables were not included in subsequent analyses. A series of bivariate and multiple regression analyses were conducted examining the association between mid-treatment client reported alliance and outcomes (Table 3). For variables that lacked a meaningful baseline comparison (i.e., number of days smoked, smoking abstinence), these coefficients represent bivariate associations. For all other analyses, baseline levels were controlled for in multiple regression models and the coefficients reported are thus partial regression coefficients.
Table 3.
Therapeutic alliance as predictor of change in cognitive, affective, and behavioral outcomes.
| Outcome | β [95% CI] | t | p-value |
|---|---|---|---|
| Days Smoked | −0.25 [−.58, .08] | −1.54 | 0.133 |
| Smoking Abstinence | −0.20 [−.52, .14] | −1.17 | 0.248 |
| Negative Affect (DASS)a | −0.33 [−0.64, −0.02] | −2.13 | 0.040* |
| Emotion Regulation (DERS)a | −0.24 [−0.47, −0.01] | −2.11 | 0.042* |
| Mindfulness (FFMQ)a | 0.33 [0.09, 0.57] | 2.88 | 0.007** |
| Minutes Meditateda | 0.39 [0.09, 0.68] | 2.69 | 0.011* |
Note: n = 37 for all models; β = standardized regression coefficients for therapeutic alliance predicting outcomes,
β represents partial regression coefficient with pre-test scores simultaneously controlled; 95% confidence intervals are reported;
t = t-statistic from regression analyses; therapeutic alliance measured by Working Alliance Inventory Group Format.
p <.05;
p < .01
p < .001
Contrary to study hypothesis (H3), alliance did not significantly predict smoking abstinence or number of days smoked, although the associations were in the expected direction. As predicted (H1and H2), alliance predicted several psychological outcomes as well as participant compliance with the MTS course requirements. Specifically, mid-treatment alliance predicted post-treatment negative affect, emotion regulation, mindfulness, and treatment compliance (i.e., minutes meditated), all in the expected direction2. As these analyses controlled for pre-treatment level, they imply that alliance was significantly associated with changes in these variables. The magnitude of these relationships would be considered medium-sized by Cohen’s (1988) standards.
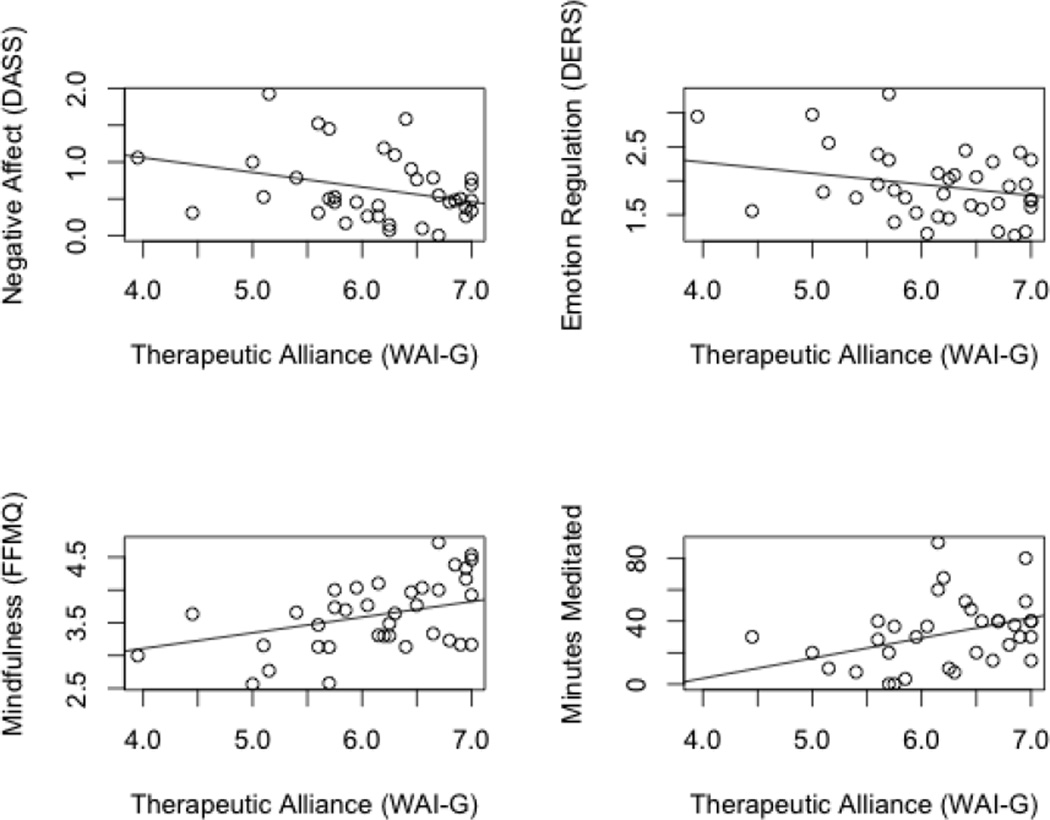
Scatterplots of the significant associations are displayed in Figure 1. These plots display the bivariate association between alliance and post-treatment outcome with a regression line drawn based on the partial regression coefficients. Inspection of these plots suggests that the observed relationships, although based on a relatively small sample, is not being driven by statistical outliers.
Figure 1.
Scatterplots of associations between post-test measures and alliance. Plots display bivariate associations with regression lines added from multiple regression models controlling for baseline levels of given variable. All associations are statistically significant and in the expected direction. DASS = Depression, Anxiety, and Stress Scales; DERS = Difficulty in Emotion Regulation; FFMQ = Five-Facet Mindfulness Questionnaire; WAI-G = Working Alliance Inventory Group Version.
Discussion
This study presents data on pre-post changes and the associations between therapeutic alliance and post-treatment outcomes. Despite a relatively small sample and associated low statistical power, these data suggest a number of tentative conclusions. First, the significant pre-post changes observed on several measures suggest that MTS was an effective intervention for the development of mindfulness and emotional regulation. This is important, given that MTS is a smoking cessation intervention in addition to a mindfulness training course. The significant improvements in self-reported mindfulness support the generalizability of the current findings related to therapeutic alliance to other mindfulness-based interventions not designed to treat smokers.
It is important to acknowledge that in addition to the MTS course all participants received four weeks of nicotine patches and had access to the Wisconsin Quit Line, and that these resources may have contributed in some way to the observed pre-post psychological effects. Most participants (89.2%) did start nicotine patches on the Quit Day. In contrast, the Wisconsin Tobacco Quit Line was used less extensively, with MTS participants making on average only 1.35 calls (SD = 1.59), including one call that was required during study orientation and was made from the study center. For those participants who did make additional calls, it is worth noting that the Wisconsin Tobacco Quit Line is designed principally to provide smoking cessation tips and does not offer mindfulness training or psychological counseling (Fiore et al., 2008). In addition, while it could be expected that nicotine patches might attenuate post-treatment difficulties in emotion regulation associated with nicotine withdrawal (Piper & Curtin, 2006), it is unlikely that patches would lead to higher post-treatment versus pre-treatment emotion regulation as was seen in our sample.
It is also notable that the negative affect composite scores, comprised of depression, anxiety and stress subscales, did not decrease during the course of the intervention. Despite its close relation to MBSR, a stress reduction program, MTS did not appear to lead to a decrease in self-reported post-treatment versus pre-treatment stress. This finding is not surprising in light of the significant body of literature documenting increases in negative affect during nicotine withdrawal (Piper & Curtin, 2006; Kenford et al., 2002). Immediate post-treatment effects of MTS are measured during nicotine withdrawal and a reasonable goal for such an intervention would be to attenuate the expected stress and negative affect of smoking cessation. Comparisons between MTS participants and controls on the relative attenuation of withdrawal-related negative affect have been reported elsewhere (Davis et al., in press).
As was hypothesized, mid-treatment therapeutic alliance was significantly associated with changes in several key measures of interest including mindfulness, negative affect, and emotion regulation. The significant partial regression coefficients for therapeutic alliance predicting post-test scores while controlling for baseline levels, indicate that individuals endorsing higher levels of therapeutic alliance at the quit day also reported increased mindfulness, decreased negative affect, and decreased difficulty in emotion regulation at post-test.
As expected, in addition to predicting changes in several psychological outcomes, therapeutic alliance also significantly predicted treatment adherence indexed by minutes meditated. This may be a meaningful finding in that it suggests that therapeutic alliance may not only predict changes on self-report questionnaires, but may in fact influence participants’ willingness to engage in key aspects of the treatment, namely the meditation practice.
Contrary to our hypothesis, therapeutic alliance did not significantly predict smoking outcomes. It may be worth noting that associations between therapeutic alliance and both measures of post-quit smoking behavior were in the expected direction (βs = −.25 and −.20, for days smoked and abstinence, respectively). It is possible that the lack of statistical significance in these analyses may be related to low statistical power to detect associations. Relatedly, a ceiling effect may have been observed on our measure of alliance. This restriction of range may have further attenuated our ability to detect associations between alliance and some outcomes (Cohen, Cohen, West, & Aiken, 2003). It may also be that participants’ success in quitting smoking through the MTS intervention was influenced by factors unrelated to therapeutic alliance, such as pre-intervention motivation to quit (Garvey, Bliss, Hitchcock, Heinold, & Rosner, 1992) or the occurrence of stressful life events external to the treatment (Cohen & Lichtenstein, 1990).
Although other smoking cessation studies have found an association between alliance and outcome (Gifford et al., 2011), the current study was not the first study to find a lack of association between alliance and substance use. Indeed, a recent literature review failed to find a consistent association between alliance and substance use outcomes in substance abuse treatments (Meier, Barrowclough, & Donmall, 2005). Meier et al. (2005) suggest instead that alliance may be an important predictor for how clients progress in treatment rather than as a predictor of post-treatment outcomes.
Taken together, these findings suggest that participant-instructor alliance, may play a role in mindfulness interventions. In addition, these findings suggest that alliance may be less important for substance use outcomes than for psychological and treatment compliance outcomes. Interestingly, the magnitude of association between alliance with psychological and compliance outcomes in the current sample is similar in magnitude to that found in previous meta-analyses of the alliance-outcome relationship (e.g., Horvath et al., 2011), perhaps supporting the case that alliance is operating with a similar strength in mindfulness treatments as in other treatment types.
It is worth considering here the importance of alliance as an additional variable that predicts outcomes, such as emotion regulation and negative affect that did not show large pre-post effects. For one, the pre-post effect sizes reported above include all participants who reported a range of strengths of alliance, thus it is conceivable (and likely given the multiple regression analyses) that participants forming higher alliances would have larger pre-post effect sizes for variables in which the alliance predicted changes (i.e., mindfulness, negative affect, and emotion regulation). In addition, alliance did predict changes in self-reported mindfulness, a variable that showed medium sized pre-post effects and with obvious importance in this intervention and other mindfulness-based treatments.
A broader issue concerns the meaning of therapeutic alliance as a measure of agreement on the tasks and goals in the context of a mindfulness-based intervention. While smoking cessation provided a clear goal, the practice of mindfulness by definition involves a shift from striving for goals (i.e., non-striving, non-doing; Kabat-Zinn, 1994). While the items included on the WAI-G may seem somewhat at odds with the objective (or perhaps more accurately non-objectives) of mindfulness training, this apparent contradiction was likely less problematic in the specific context of MTS. This was largely due to the fact that the mindfulness practices offered in MTS were explicitly framed as cognitive skills that would be helpful for the explicit goal of smoking cessation (Davis et al., in press). Thus mindfulness, although fundamentally non-goal oriented (i.e., non-doing; Kabat-Zinn, 1994), became something participants did work to practice and learn in MTS, allowing goal items on the WAI-G to remain relevant. Additionally, of the items on the WAI-G, half were related to the therapeutic bond, with only three related to task and seven related to goal.
Conclusion
Therapeutic alliance, the relational bond between a therapist and client, which involves positive personal attachment and agreement on the tasks and goals of a given psychotherapeutic intervention, has been shown to play an integral role across a variety of treatments (Horvath et al., 2011). Despite the fact that it is understood to play a central role in psychotherapy, therapeutic alliance has not yet been reported in the context of mindfulness-based interventions. This study explores the role of therapeutic alliance in predicting outcomes in a mindfulness-based treatment for smoking cessation. The results support the position that the therapeutic alliance created between mindfulness instructor and participant is playing a role in the salutary effects associated with mindfulness training such as the acquisition of mindfulness skills and changes in emotion regulation and negative affect, but not in regards to quitting smoking.
Although an exploratory study, these results may have implications for both the provision of mindfulness-based treatments and future research in this area. The findings should encourage mindfulness instructors to recognize that the alliance they form with participants may be an influential aspect of the therapy provided, at least for certain outcomes. This may require a widening in perspective for those clinicians or researchers who hold closely to the view that it is the specific techniques or practices of their intervention that drive beneficial effects (Baer, 2003; Carmody et al., 2009; Shapiro, Carlson, Astin, & Freedman; Wampold, 2001). Further research could help clarify the extent to which alliance influences outcomes in other mindfulness interventions such as MBSR and how alliance interacts with other mechanisms in these multifaceted treatments.
These results do not suggest that the mindfulness skills in MTS are not important predictors of the observed outcomes—indeed, the significant improvements in self-reported mindfulness suggest that mindfulness skills are being learned. Rather, these results suggest that therapeutic alliance may influence the extent to which individuals are able to develop mindfulness skills within a mindfulness intervention. This study provides evidence to suggest that therapeutic alliance plays a role in particular positive outcomes associated with a mindfulness-based intervention and suggests that researchers and clinicians may benefit from considering therapeutic alliance as an underexplored aspect of mindfulness treatments.
Limitations
A small sample size was used with consequent low power to detect associations and especially to test more complex relationships such as moderation or mediation (Hoyt, Imel, & Chan, 2008). Relatedly, the sample included in this study was largely racially and ethnically homogeneous and differed from the intent-to-treat sample on several demographic variables. This limits the generalizability of findings to racial and ethnic minority populations and may have implications for the acceptability of the treatment to some groups. The high-level attrition in the present study, although not unlike attrition found in other mindfulness-based substance use treatment (Zgierska et al., 2009) or other smoking cessation studies (Prochaska et al. 2004), may put the clients who remained in the sample at greater risk for the halo effect discussed below and thus limit the generalizability of findings to those who did not complete treatment.
A second limitation of this study was the use of a novel mindfulness intervention, rather than the use of a more widely available treatment (e.g., MBSR). While MTS appears to be an effective smoking cessation intervention (Davis, Fleming, Bonus, Baker, 2007; Davis et al., in press) and has been shown to increase participant mindfulness, it may be that patterns observed between therapeutic alliance and post-test outcomes are somehow idiosyncratic to this intervention and may not, therefore, generalize to other mindfulness-based interventions. The addition of the Wisconsin Tobacco Quit Line and nicotine patches to mindfulness training also introduces variables that may have influenced the pre-post changes observed.
An additional limitation of this current study is the exclusive use of self-report measures (with the exception of biochemically-confirmed abstinence). Reliance on a single measurement method is more at risk for the halo effect, in which systematic response biases, such as social desirability, are compounded through the inclusion and inter-correlation of a single measurement method (Heppner, Wampold, & Kivligan, 2008). Ideally, future research could include a wider range of measurement types (eg., observer- and instructor-rated measures of alliance, objective measures of outcomes especially mindfulness-related constructs, qualitative data on the process of therapeutic alliance in mindfulness interventions). It may be worthwhile to examine the mindfulness instructor’s understanding of the alliance, either through instructor-ratings of alliance or qualitative analysis.
One broader criticism and potential limitation of these findings is that the association between alliance and outcomes may not be causally related. To address this concern, it is important to acknowledge two potential confounding explanations for the observed relationship. These alternative explanations include the halo effect and reverse directionality. The halo effect is a methodological concern commonly raised when examining process-outcome data drawn from a single rater (i.e., only the participant). Simply put, if a client experiences therapy as positive, the client is more likely to rate both the process (e.g., therapeutic alliance) and outcome (e.g., mindfulness) more favorably (Hoyt, 2000). While theoretically this is a valid concern, associations between alliance and outcome have been shown not to differ in magnitude when ratings are from the same source or different sources (rs = .29 and .25 for same source and different source, respectively; Horvath et al., 2011).
A second confound is the potential bi- or reverse directionality between process and outcome variables. Given that our data are correlational, it is conceivable that the direction of effect is reversed, with positive outcomes such as symptom change, especially early in treatment, causing higher levels of therapeutic alliance (DeRubeis & Feeley, 1990; Feeley, DeRubeis, & Gelfand, 1999). Several sources of evidence against this argument have been offered, including significant associations between early alliance and outcome (Fluckiger et al., 2012) and associations between alliance and outcome even when controlling for early symptom change (Fluckiger, Holtforth, Znoj, Caspar, & Wampold, 2012).
Lastly, the Hawthorne effect may be at play in the current study (Adair, 1984). It is possible that the observed relationship between alliance and some outcomes was related to the participants’ knowledge that they were in a research study and may thus not generalize to treatments occurring in different contexts (Adair, 1984). While it is impossible to rule out this potential confound, alliance ratings were collected as part of a battery of questions that may have obscured study hypotheses from participants.
Footnotes
Due to a clerical error, only items 1 – 30 of the FFMQ’s 39 items were administered to n = 22 participants at the post-treatment study visit. The entire scale was administered at baseline to all participants. An analysis conducted using baseline FFMQ data found a large (r = .91, p < .001) correlation between the mean of the missing 9 items and the remaining 30 items. A similarly large correlation was found between a total score computed using 30 items with a total score computed using 39 items (r = .99, p < .001). Means were computed for the 30 and 9 items, in order to assess differences in elevation between administered and non-administered items (i.e., although correlated, perhaps one set of items yielded overall lower or higher scores). The mean for the 30 items was 3.32 (SD = .50) and for the 9 items 3.38 (SD = .55) yielding a mean difference of .06, or .12 standard deviations. A Welch two sample t-test indicated that this difference was not significant (t(71.37) = −.50, p = .620). In instances where the short version was administered, the total score was computed using the administered items only.
Post-hoc analyses were conducted in order to determine if pre-treatment smoking behavior impacted any of the reported associations between alliance and outcome. Nicotine dependence assessed via Fagerstrom Test for Nicotine Dependence (FTND; Heatherton et al., 1991) served as this control variable since it was arguably the most reliable indicator of baseline smoking addiction severity included in the study. Multiple regression analyses reported in Table 3 were repeated with FTND added as an additional predictor variable. Alliance remained a significant predictor of change (p < .05) in all of the same outcomes (i.e., emotion regulation, negative affect, mindfulness, minutes meditated).
Contributor Information
Simon B. Goldberg, Department of Counseling Psychology, University of Wisconsin, 335 Education Building - 1000 Bascom Mall, Madison, WI, 53706, Telephone: 608-262-4807, Fax: 608-265-3347, sbgolberg@wisc.edu.
James M. Davis, Department of Medicine, University of Wisconsin School of Medicine and Public Health, Center for Tobacco Research and Intervention, 1930 Monroe St., Suite 300, Madison, WI, 53711, Telephone: 608-217-9405, Fax: 608-265-3102, jjamesdavis@hotmail.com.
William T. Hoyt, Department of Counseling Psychology, University of Wisconsin, 335 Education Building - 1000 Bascom Mall, Madison, WI, 53706, Telephone: 608-262-0462, Fax: 608-265-3347, wthoyt@education.wisc.edu.
References
- Adair J. The Hawthorne Effect: A reconsideration of the methodological artifact. Journal of Applied Psychology. 1984;69(2):334–345. [Google Scholar]
- Baer R. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10(2):125–143. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer R, Smith G, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Baker TB, Mermelstein R, Collins LM, Piper ME, Jorenby DE, Smith SS, Fiore MC. New methods for tobacco dependence treatment research. Annals of Behavioral Medicine. 2011;41(2):192–207. doi: 10.1007/s12160-010-9252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown GK, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 2nd ed. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research and Practice. 1979;16(3):252–260. [Google Scholar]
- Brewer J, Sinha R, Chen J, Michalsen R, Babuscio T, Nich C, Rounsaville BJ. Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled Stage I pilot study. Substance Abuse. 2009;30:306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K, Ryan R. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown K, Ryan R, Creswell J. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18(4):211. [Google Scholar]
- Carmody J, Baer R, Lykins E, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2009;65(6):613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Catanzaro S, Mearns J. Measuring generalized expectancies for negative mood regulation: Initial scale development and implications. Journal of Personality Assessment. 1990;54(3&4):546–563. doi: 10.1080/00223891.1990.9674019. [DOI] [PubMed] [Google Scholar]
- Coelho H, Canter P, Ernst E. Mindfulness-based cognitive therapy: Evaluating current evidence and informing future research. Journal of Consulting and Clinical Psychology. 2007;75(6):1000–1005. doi: 10.1037/0022-006X.75.6.1000. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression / correlation analysis for the behavioral sciences. 3rd edition. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc.; 2003. [Google Scholar]
- Cohen S, Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology. 1990;9(4):466–478. doi: 10.1037//0278-6133.9.4.466. [DOI] [PubMed] [Google Scholar]
- Davis JM, Fleming M, Bonus K, Baker T. A pilot study on mindfulness based stress reduction for smokers. BMC Completementary and Alternative Medicine. 2007;7(2) doi: 10.1186/1472-6882-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial to evaluate the addition of mindfulness training to a usual-care smoking cessation intervention. Substance Use and Misuse. (In Press) [Google Scholar]
- Del Re AC, Fluckiger C, Goldberg SB, Hoyt WT. Monitoring mindfulness practice quality: An important consideration in mindfulness practice. Psychotherapy Research. 2012 doi: 10.1080/10503307.2012.729275. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14:469–482. [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578–582. doi: 10.1037//0022-006x.67.4.578. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update-clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- Fluckiger C, Del Re AC, Wampold BE, Symonds D, Horvath AO. How central is the alliance in psychotherapy? A multilevel longitudinal meta-analysis. Journal of Counseling Psychology. 2012;59(1):10–17. doi: 10.1037/a0025749. [DOI] [PubMed] [Google Scholar]
- Fluckiger C, Holtforth MG, Znoj HJ, Caspar F, Wampold BE. Is the relation between early post-session reports and treatment outcome an epiphenomenon of intake distress and early response? A multi-predictor analysis in outpatient psychotherapy. Psychotherapy Research, 2012 doi: 10.1080/10503307.2012.693773. [DOI] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Gaylord S, Chanon VW, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. Cognitive Therapy and Research. 2011;36:441–450. doi: 10.1007/s10608-011-9378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey AJ, Bliss RE, Hitchcock JL, Heinold JW, Rosner B. Predictors of smoking relapse among self-quitters: A report from the normative aging study. Addictive Behaviors. 1992;17:367–377. doi: 10.1016/0306-4603(92)90042-t. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, Palm KM. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? A randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behavior Therapy. 2011;42:700–715. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Greason PB, Cashwell CS. Mindfulness and counseling self-efficacy: The mediating role of attention and empathy. Counselor Education and Supervision. 2009;49:2–19. [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Heatherton T, Kozlowski L, Frecker R, Fagerstrom K. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heppner PP, Wampold BE, Kivlighan DM., Jr . Research design in counseling. 3rd ed. Belmont, CA: Brooks/Cole; 2008. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Del Re AC, Fluckiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48(1):9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg L. Development and validation of the working alliance inventory. Journal of Counseling Psychology. 1989;36(2):223–233. [Google Scholar]
- Horvath AO, Symonds B. Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology. 1991;38(2):139–149. [Google Scholar]
- Hoyt WT. Rater bias in psychological research: When is it a problem and what can we do about it? Psychological Methods. 2000;5(1):64–86. doi: 10.1037/1082-989x.5.1.64. [DOI] [PubMed] [Google Scholar]
- Hoyt WT, Goldberg SB. Unpublished manuscript, Department of Counseling Psychology, University of Wisconsin, Madison, Wisconsin. 2012. Initial validation of the Working Alliance Inventory – Group Version. [Google Scholar]
- Hoyt WT, Imel ZE, Chan F. Multiple regression and correlation techniques: Recent controversies and best practices. Rehabilitation Psychology. 2008;53(3):321–339. [Google Scholar]
- Imel Z, Baldwin S, Bonus K, MacCoon D. Beyond the individual: Group effects in mindfulness-based stress reduction. Psychotherapy Research. 2008;18(6):735–742. doi: 10.1080/10503300802326038. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go there you are: Mindfulness meditation in everyday life. New York: Hyperion; 1994. [Google Scholar]
- Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemporary Buddhism: An Interdisciplinary Journal. 2011;12(1):281–306. [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: Contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology. 2002;70(1):216. [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd. Ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- Lykins E, Baer R. Psychological functioning in a sample of long-term practitioners of mindfulness meditation. Journal of Cognitive Psychotherapy. 2009;23(3):226–241. [Google Scholar]
- Mars T, Abbey H. Mindfulness meditation practise as a healthcare intervention: A systematic review. International Journal of Osteopathic Medicine. 2010;13(2):56–66. [Google Scholar]
- Martin D, Garske J, Davis M. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438–450. [PubMed] [Google Scholar]
- Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: A critical review of the literature. Addiction. 2005;100:304–316. doi: 10.1111/j.1360-0443.2004.00935.x. [DOI] [PubMed] [Google Scholar]
- Middleton E, Morice A. Breath carbon monoxide as an indication of smoking habit. Chest. 2000;117:758–763. doi: 10.1378/chest.117.3.758. [DOI] [PubMed] [Google Scholar]
- Prochaska J, Delucchi K, Hall S. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of Consulting and Clinical Psychology. 2004;72(6):1144–1156. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- Piper M, Curtin J. Tobacco withdrawal and negative affect: An analysis of initial emotional response intensity and voluntary emotion regulation. Journal of Abnormal Psychology. 2006;115(1):96. doi: 10.1037/0021-843X.115.1.96. [DOI] [PubMed] [Google Scholar]
- Roberts KC, Danoff-Burg S. Mindfulness and health behaviors: Is paying attention good for you? Journal of American College Health. 2010;59(3):165–173. doi: 10.1080/07448481.2010.484452. [DOI] [PubMed] [Google Scholar]
- Shapiro S, Carlson L, Astin J, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83(4):393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Snijders TA, Bosker RJ. Multilevel analysis: An introduction to basic and advance multilevel modeling. 2nd ed. London: Sage; 2012. [Google Scholar]
- Tracey T, Kokotovic A. Factor structure of the working alliance inventory. Psychological Assessment. 1989;1(3):207–210. [Google Scholar]
- Vettese L, Toneatoo T, Stea J, Nguyen L, Wang J. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy: An International Quarterly. 2009;23(3):198–225. [Google Scholar]
- Wampold B. The great psychotherapy debate: Models, methods, and findings. New York: Routledge; 2001. [Google Scholar]
- Wilson K, Sandoz E. Mindfulness, values, and therapeutic relationship in acceptance and commitment therapy. In: Hick S, Bein T, editors. Mindfulness and the therapeutic relationship. New York: Guilford Press; 2008. [Google Scholar]
- Van Dam NT, Hobkirk AL, Danoff-Burg S, Earleywine M. Mind your words: Positive and negative items create method effects on the Five Facet Mindfulness Questionnaire. Assessment. 2012;19(2):198–204. doi: 10.1177/1073191112438743. [DOI] [PubMed] [Google Scholar]
- Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behavior Research and Therapy. 2011;49:281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Yalom I, Leszcz M. The theory and practice of group psychotherapy. 5th ed. New York: Basic Books; 2005. [Google Scholar]
- Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt A. Mindfulness meditation for substance use disorders: A systematic review. Substance Abuse. 2009;30(4):266–294. doi: 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]