Abstract
Patient: Male, 22
Final Diagnosis: Cardiomyopathy
Symptoms: Shortness of breath • dispnoea • chest discomfort
Medication: —
Clinical Procedure: Echocardiogram • cardiac MRI
Specialty: Cardiology
Objective:
Challenging differential diagnosis
Background:
Non-compaction cardiomyopathy (NCM) is a rare congenital cardiomyopathy characterized by increased trabeculation in one or more segments of the ventricle. The left ventricle is most commonly affected. However, biventricular involvement or right ventricle predominance has also been described. Clinical features of NCM are non-specific and can range from being asymptomatic to symptoms of congestive heart failure, arrhythmia, and systemic thromboembolism.
Case Report:
22-year-old Hispanic male presented with two month history of chest discomfort. Laboratory workup revealed an elevated brain-natriuretic-peptide of 1768 pg/ml. ECG and chest x-ray was nonspecific. Transthoracic echocardiogram revealed prominent trabeculae and spongiform appearance of the left ventricle (LV) with an ejection-fraction of 15–20%; 5 of 9 segments of the LV were trabeculated with deep intertrabecular recesses also involving the right ventricle (RV) with demonstrated blood flow in these recesses on color-doppler. The biventricular spongiform appearance was morphologically suggestive for NCM with involvement of the RV. Confirmatory cardiac MRI was performed, demonstrating excessive trabeculation of the left-ventricular apex and mid-ventricular segments. Hypertrabecularion was exhibited at the apical and lateral wall of the RV. Cardiac catheterization showed an intact cardiac vessel system. The patient was discharged on heart failure treatment and was placed on the heart transplantation list.
Conclusions:
NCM is a unique disorder resulting in serious and severe complications. The majority of the reported cases describe the involvement of the left ventricle. However, the right ventricle should be taken into careful consideration. The early diagnosis may help to increase the event-free survival.
Keywords: trabeculation, dilated cardiomyopathy, biventricular noncompaction
Background
Non-compaction cardiomyopathy (NCM) of the ventricular myocardium is a rare congenital cardiomyopathy characterized by increased trabeculation in one or more segments of the ventricle, which in turn is caused by the cessation of compaction during intrauterine development. Noncompaction is a genetic disorder and can be found alone or together with other congenital heart diseases. This genetic cardiomyopathy is due to abnormal arrest in endomyocardial embryogenesis between fetal 5th and 8th week [1].
This arrest in the endomyocardial morphogenesis occurs during the compaction of myocardial fibers, resulting in excessive multiple trabeculation of the myocardial tissue [2]. NCM cardiomyopathy was first identified and described by Engberding and Benber in 1984 [3]. The term “non-compaction” was first used in 1990 to describe an embryogenic spongy myocardium without other cardiac abnormalities [2,3].
The left ventricle is the most affected site of non-compaction, but biventricular involvement has also been described. In contrast, the predominance of the right ventricle has been observed in almost 50 percent. An isolated right ventricle involvement has been reported in some cases [4,5]. Clinical features of NCM are non-specific and can range from being asymptomatic to presenting with congestive heart failure, arrhythmia, and systemic thromboembolism [6]. We present a case report of a 22-year-old Hispanic male patient with biventricular non-compaction that predominantly involved the right ventricle.
Case Report
22-year-old Hispanic male present to our care without any significant past medical history He complained of a two-month history of intermittent chest discomfort. Before this admission he was mistakenly being treated gastritis. He reported progressive decrease in his exercise tolerance and mild shortness of breath. Social history was remarkable for a 20 pack-year of smoking but he denied alcohol abuse and illegal drugs. Family history was not significant.
Initial vital signs were within normal limits. Cardiovascular examination was remarkable for an early aortic diastolic murmur of grade 3/6 over the 2nd intercostal area without radiation to the carotids and a pansystolic murmur of grade 4/6 at the apex with radiation to the mid-axillary line the neck examination showed a jugular venous distention of about 8 cm. The chest examination demonstrated reduced breath sounds over both lung bases with basal crackles. Bilateral pitting pedal edema of grade 1 was noted. Laboratory workup was unremarkable except for an elevated brain natriuretic peptide (BNP) of 1768 pg/ml.
The electrocardiogram was remarkable for sinus tachycardia with occasional premature ventricular complexes, left atrial enlargement and non-specific ST-T wave changes. Chest X-ray demonstrated features of pulmonary edema. Transthoracic echocardiogram revealed prominent trabeculae and spongi-form appearance of the left ventricle, moderately dilated left ventricle of 65 mm with severely reduced systolic function and an ejection fraction of 20% (Video sequences 1–4 – see web sites). In addition there was right atrial enlargement, moderate to severe mitral regurgitation, moderate aortic regurgitation and severe pulmonary hypertension (peak systolic pulmonary artery pressure 37 mmHg) (Figure 1). Five of nine left ventricle segments were trabeculated and deep intertrabecular recesses predominantly involving the right ventricle were noticed. A color Doppler echocardiographic examination demonstrated the presence of blood flow in the deep intertrabecular recesses. Transmitral blood flow revealed the restrictive pattern of diastolic dysfunction. The right ventricular papillary muscles and chordae structure were hypertrophic and thick. There was no associated congenital cardiac anomaly. The spongiform appearance of the both ventricles was morphologically suggestive for non-compaction cardiomyopathy with notable involvement of the right ventricle.
Figure 1.
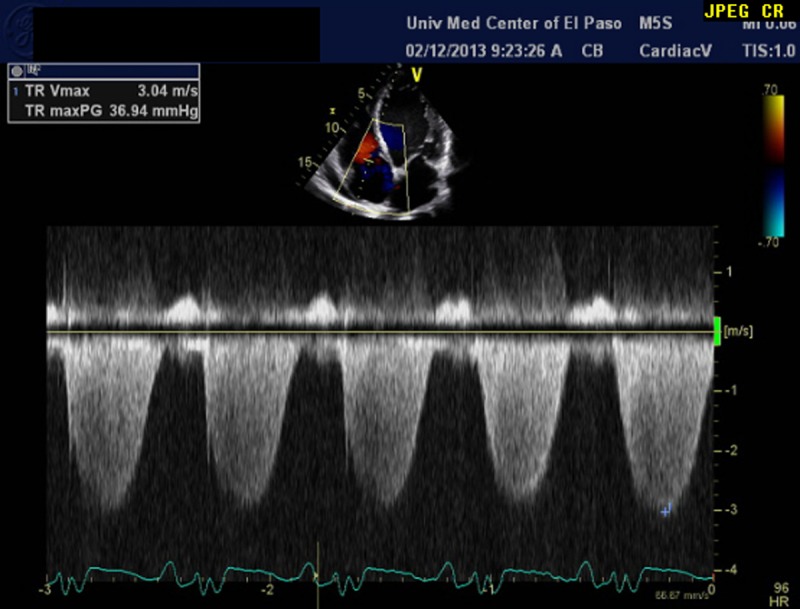
Echocardiographic CW-Doppler demonstrates the increased pulmonary artery systolic pressure of 36.9 mmHg.
Cardiac MRI was performed and demonstrated the global dilation and diffuse hypokinesia (Figure 2A). The right ventricle was dilated and showed exhibited trabeculations as well as prominent intramycocardial recesses, which confirmed the echocardiographic findings (Figure 2B).
Figure 2.
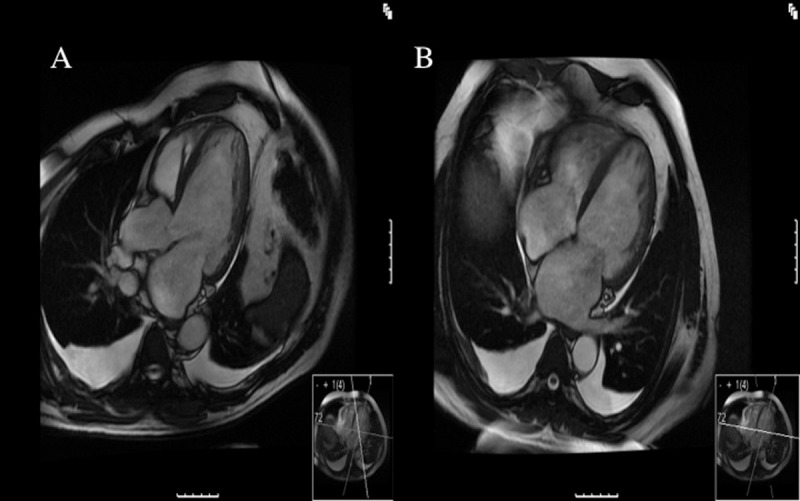
(A) Three-chamber view of the cardiac MRI shows trabeculation of the left ventricular apex and mid ventricular segments. (B) Four chamber view of the cardiac MRI demonstrates global biventricular dilation with prominent intramyocardial recesses in communication with the ventricular cavities.
Further laboratory workup (leukocyte alpha-galactosidase-A activity) was performed to exclude metabolic and storage disorders.
Left heart catheterization demonstrated normal coronary arteries and elevated left ventricular end diastolic pressure. A right heart catheterization revealed pulmonary hypertension (peak pulmonary artery systolic pressure 43 mmHg) that was higher than the measured pulmonary artery systolic pressure in the echocardiography; the right ventricular end-diastolic pressure was elevated as well.
The patient had no significant cardiac family history. An echocardiogram for the first-degree relatives was performed to rule out a familial variant; these results were normal. He was started on an ACE-inhibitor (lisinopril 10 mg daily), diuretic agent (torsemide 5 mg daily) and spironolactone 25 mg daily.
A follow up in the cardiologic outpatient clinic was performed 3 months after the discharge; the EF did not improve and was documented with 15–20%, β-blocker was added. The patient was placed on the heart transplantation list. Further follow-ups are scheduled.
Discussion
Noncompaction cardiomyopathy (NCM) is a congenital cardiomyopathy defined by the presence of prominent ventricular myocard trabeculations and deep intertrabecular recesses [7]. NCM occurs secondary to interruption of the normal myocardial morphogenesis. It occurs more frequently in males, and its prevalence varies from 0.06 to 0.24% of the general population [8]. Left ventricular NCM is the most common affected site, however right ventricle involvement has been reported in a few cases [5,6]. Familial or sporadic cases of CNM [9] and genetic association with a mutation in the G 4.5 gene and to chromosome Xq28 have been described [10]. Genetic studies in familial cases are needed to localize the causative genes.
Clinical presentations are often nonspecific; nevertheless clinical features represent heart failure, dyspnea and arrhythmia. At the time of recognized first onset the clinical symptoms are often advanced resembling NYHA class III/IV. A sudden cardiac death is responsible for half of the deaths in patients with noncompaction [11]. Thromembolic events are also known to occur as a complication associated with NCM. They occur in 21–38% of the cases involving lungs, mesenteric organs and the brain [11].
Compared with other common types of cardiomyopathy NCM, is underreported and remains unrecognized. The echocardiography is the key method delivering specific characteristics for NCM that include, in the absence of any coexisting lesions, regional thickening of the myocardial wall consisting of 2 layers namely an outer epicardial layer, which is usually thin and an extremely thick layer that includes at least four prominent trabeculations and deep recesses. This wall appearance delivers significant information in the first assessment of the abnormal myocardial configuration. A maximum end-systolic ratio of the noncompacted endocardial layer to the compacted myocardium of >2 are characteristic. Color Doppler can be helpful and is a significant feature of the diagnosis; it is usually remarkable for deeply perfused intertrabecular recesses [12].
Magnet-Resonance Imaging (MRI) is helpful addition in the diagnostic of ventricular noncompaction. MRI detects advantageous the septal resolution at the lateral and apical wall of the left ventricle [13]. Even though echocardiography may establish the diagnosis, but cardiac MRI should be considered in a patient presenting with ventricular arrhythmias and systolic dysfunction prior to ICD implantation.
There are no specific diagnostic criteria for the right ventricle noncompaction, however some authors suggest that the left ventricle diagnostic criteria apply to the right ventricle as well [14]. The irregular geometric shape of the RV makes a clear visualization limited, which makes the diagnosis of the RV-noncompaction more difficult.
To our knowledge biventricular noncompaction with significant pulmonary hypertension has been described in the literature in a single case report [15]. Managment of biventricular noncompaction includes similar therapy as for CHF, thromboembolic complications and arrhythmias. However currently there is clear pharmacological treatment for biventricular noncompaction. Heart transplantation is an option for patients with refractory symptoms. A long-term anticoagulation may be considered and is a recommended choice [11].
The benefit of Implantable Cardiac Defibrillators (ICD) has been mentioned in the literature; ICD can be used in cases of significant hemodynamical impairment [16]. ICD improves outcomes in left ventricular noncompaction cardiomyopathy when implanted for the prevention of sudden cardiac death in those with ejection fraction less than 35% of in those with history of sustained ventricular tachycardia or ventricular fibrillation.
Familial screening of first-degree relatives is recommended [17]. In general the prognosis is associated with the stage of heart failure and other comorbidities. Familial inheritance is a common feature of NCM an echocardiographic screening of the 1st degree relatives is recommended.
Conclusions
NCM is a unique disorder resulting in serious and severe complication. The majority of the reported cases describe an involvement of the left ventricle. However the right ventricle should always be taken into careful consideration when NCM is suspected. The early diagnosis may help to increase the event-free survival.
References:
- 1.Ranganathan A, Ganesan G, Sangaredd V, et al. Isolated noncompaction of right ventricle – a case report. European Heart Journal. 2010;31:806–14. [Google Scholar]
- 2.Chin TK, Perloff JK, Williams RG, et al. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation. 1990;82:507–13. doi: 10.1161/01.cir.82.2.507. [DOI] [PubMed] [Google Scholar]
- 3.Engberding R, Bender F. Identification of a rare congenital anomaly of the myocardium by two-dimensional echocardiography: Persistence of isolated myocardial sinusoids. Am J Cardiol. 1984;53(11):1733–34. doi: 10.1016/0002-9149(84)90618-0. [DOI] [PubMed] [Google Scholar]
- 4.Ritter M, Oechslin E, Sutsch G, et al. Isolated noncompaction of the myocardium in adults. Mayo Clin Proc. 1997;72:26–31. doi: 10.4065/72.1.26. [DOI] [PubMed] [Google Scholar]
- 5.Sato Y, Matsumoto N, Matsuo S, et al. Right ventricular involvement in a patient with isolated noncompaction of the ventricular myocardium. Cardiovasc Revasc Med. 2007;8:275–77. doi: 10.1016/j.carrev.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Gomathi SB, Makadia N, Ajit SM. An unusual case of isolated noncompacted right ventricular myocardium. Eur J Echocardiogr. 2008;9:424–25. doi: 10.1093/ejechocard/jen016. [DOI] [PubMed] [Google Scholar]
- 7.Erer B, Nurkalem Z, Orhan AL, et al. Isolated biventricular noncompaction; case report. Chin Med J. 2010;123(7):969–71. [PubMed] [Google Scholar]
- 8.Sandhu R, Finkelhor RS, Gunawardena DR, et al. Prevalence and characteristics of left ventricular noncompaction in a community hospital cohort of patients with systolic dysfunction. Echocardiography. 2008;25:8–12. doi: 10.1111/j.1540-8175.2007.00560.x. [DOI] [PubMed] [Google Scholar]
- 9.Ichida F, Hamamichi Y, Miyawaki T, et al. Clinical features of isolated noncompaction of the ventricular myocardium. Long-term clinical course, hemodynamic properties, and genetic background. J Am Coll Cardiol. 1999;34:233–40. doi: 10.1016/s0735-1097(99)00170-9. [DOI] [PubMed] [Google Scholar]
- 10.Chen R, Tsuji T, Ichida F, et al. Mutation analysis of the G4.5 gene in patients with isolated left ventricular noncompaction. Mol Genet Metab. 2002;77:319–25. doi: 10.1016/s1096-7192(02)00195-6. [DOI] [PubMed] [Google Scholar]
- 11.Oechslin EN, Attenhofer Jost CH, Rojas JR, et al. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36:493–500. doi: 10.1016/s0735-1097(00)00755-5. [DOI] [PubMed] [Google Scholar]
- 12.Jenni R, Oechslin E, Schneider J, et al. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: A step towards classification as a distinct cardiomyopathy. Heart. 2001;86:666–71. doi: 10.1136/heart.86.6.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohli SK, Pantazis AA, Shah JS, et al. Diagnosis of left-ventricular non-compaction in patients with left-ventricular systolic dysfunction: Time for a reappraisal of diagnostic criteria. Eur Heart J. 2008;29:89–95. doi: 10.1093/eurheartj/ehm481. [DOI] [PubMed] [Google Scholar]
- 14.Ulusoy RE, Kucukarslan N, Kirilmaz A, Demiralp E. Noncompaction of ventricular myocardium involving both ventricles. Eur J Echocardiogr. 2006;7:457–77. doi: 10.1016/j.euje.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Ciurzynski M, Lichodziejewska B, Tomaszewski A. Bibentricular noncompaction associated with left ventricular systolic and diastolic dysfuntion and severe pulmonary hypertension in a young man. Circ J. 2009;73:2163–65. doi: 10.1253/circj.cj-08-0857. [DOI] [PubMed] [Google Scholar]
- 16.Kobza R, Jenni R, Erne P, et al. Implantable cardioverterdefibrillators in patients with left ventricular noncompaction. Pacing Clin Electrophysiol. 2008;31:461–67. doi: 10.1111/j.1540-8159.2008.01015.x. [DOI] [PubMed] [Google Scholar]
- 17.Murphy RT, Thaman R, Blanes JG, et al. Natural history and familial characteristics of isolated left ventricular noncompaction. Eur Heart J. 2005;26:187–92. doi: 10.1093/eurheartj/ehi025. [DOI] [PubMed] [Google Scholar]


