Abstract
Background
The purpose of this study is to use mixed (qualitative/quantitative) methods to determine 1) the feasibility and acceptability of using online social networking to facilitate HIV-related discussions, and 2) the relationship between HIV-related online discussions and requests for a home-based HIV testing kit, among men who have sex with men (MSM).
Methods
Participants, primarily African American and Latino, were invited to join a “secret” group on the social networking website, Facebook. Peer leaders, trained in HIV prevention, posted HIV-related content. Participants were not obligated to respond to discussions or remain within the group. Participant public group conversations were qualitatively and thematically analyzed. Quantitative methods tested associations between qualitative data, participants’ demographic information, and likelihood of requesting a home-based HIV testing kit.
Results
Latino and African-American participants (N=57) voluntarily used Facebook to discuss the following HIV-related topics (N=485 conversations): Prevention and Testing; Knowledge; Stigma; and Advocacy. Older participants more frequently discussed Prevention and Testing, Stigma, and Advocacy, though younger participants more frequently discussed HIV Knowledge-related conversations. As the study progressed, the proportion of messages related to Prevention and Testing and HIV Stigma increased. Multivariate analysis showed that participants posting about HIV Prevention and Testing (compared to those who did not) were significantly more likely to request an HIV testing kit (OR 11.14, p = 0.001).
Conclusions
Facebook can serve as an innovative forum to increase both HIV prevention discussions and HIV testing requests among at-risk groups.
Keywords: HIV prevention, social networking technologies, peer leader models, MSM
Social networking technologies, such as Facebook.com, have grown rapidly, providing researchers with an innovative tool for HIV and STD prevention. Social networking sites are online platforms designed for multi-media communication and sharing, such as with pictures, messages, and Website links. (1) Over 750 million people used social networking technologies worldwide in 2010, and this number is expected to increase to 1.5 billion by 2015. (2) Due to their ability to reach people in almost all populations and locations, HIV prevention researchers have recommended using social networking technologies for HIV prevention. (3–5)
Social networking technologies might be especially well-suited for facilitating HIV prevention conversations by using community-based HIV prevention, such as peer leader “diffusion of innovations” models. Peer leader HIV prevention studies recruit peer leaders who have been trained in HIV fundamentals and send them to community venues to spread HIV prevention knowledge and increase HIV prevention conversations among at-risk individuals. (6) Peer leader models have been successfully used in offline studies to increase HIV-related discussions and HIV prevention behaviors. (7, 8) Because social networking technologies were designed for social engagement and communication, they might be acceptable and useful platforms for peer-delivered HIV prevention methods. Further, social networking group conversations can be analyzed for topics and themes, and compared with behavioral data to see whether HIV-related conversations predict actual behavior change. However, no research has tested whether participants would be willing to communicate about HIV prevention over social networking groups, whether these data could be qualitatively analyzed, or whether group participants’ HIV prevention discussions might be associated with HIV prevention behaviors.
This study is designed to assess the feasibility and acceptability of using social networking for mixed methods (qualitative and quantitative) HIV prevention research. Specifically, we seek to determine 1) whether participants are willing to use peer-led HIV prevention social networking groups for HIV prevention communication, 2) participants’ conversation topics and whether these topics change over time, and 3) the influence of these HIV-related conversations on subsequent requests for HIV testing.
METHODS
Participant populations and recruitment
The HOPE UCLA study is a 12-week intervention designed to test whether participants receiving peer-led HIV prevention information via online social networking (Facebook) groups will be more willing to engage in HIV–related discussions and HIV prevention behaviors, compared to a group receiving peer-led general health information over Facebook. The University of California, Los Angeles internal review board approved this study. The present methods adhere to current recommendations for conducting HIV research using social networking technologies. (9)
In total, 118 men who have sex with men (MSM) were recruited over 5 months (from August 2010-January 2011) to an HIV prevention or general health (control) group. Six participants completed only the initial survey items and were dropped from the analysis. Four participants completed duplicate surveys. The second of their responses were included, leaving 112 valid responses. This analysis is based on HIV prevention-themed conversations and therefore only includes participants from the HIV intervention groups (n= 57), as the control group (n=55) did not engage in any HIV prevention-related discussions. However, recruitment methods for the overall sample are included to provide full sampling methods. Additional study information has been previously described. (10)
Participants were recruited online, as well as from Los Angeles venues (e.g., bars, schools, gyms, and community organizations), and participant referrals.
Participants were recruited online using the following methods: 1) paid targeted banner ads on social networking sites such as Facebook and Myspace, 2) a Facebook fan page with study information, and 3) Website banner advertisements or posts on Craigslist. For offline recruitment, venue staff members distributed study fliers to relevant potential participants. Participants were directed to the study Website for study information to determine eligibility. Participants were also able to refer other interested participants.
Interested participants were screened for eligibility online (male, 18 years of age or older, living in Los Angeles, has a Facebook account, and has had sex with a man in the past 12 months). Because the study was designed for African American and Latino MSM, we first recruited 70% of the sample from these populations and then allowed participation from other MSM populations to bring diversity to the social network groups.
Facebook Connect was used to verify that participants were uniquely registered Facebook users and reduce duplicate survey respondents. Once participants passed the eligibility screening, they were asked to input their Facebook username into Facebook Connect to verify their unique participant status. After Facebook verified the new participant, he was sent a notification thank you email stating that he would be contacted once the study was ready to begin.
Once 112 participants had been enrolled, they were randomly assigned to an HIV intervention or control group and completed a baseline survey. Participants were paid $30 to complete the survey.
Peer leaders
Eighteen African American and Latino MSM peer leaders were recruited from organizations that provide services to African American and Latino MSM. Organization staff provided study fliers to potential peer leaders (i.e., sociable and well-respected African American and/or Latino MSM who were 18 years of age or older, had had sex with a man in the past 12 months, had a Facebook account or willing to set one up, and interested in educating others about health).
Qualified peer leaders were randomly assigned to either an HIV or general health group. Peer leaders attended 3 training sessions (3 hours each) at UCLA, where they learned about HIV education and prevention (or general health education), ways of presenting stigmatized information, and ways of using Facebook for delivering health behavior change education. Additional information about the peer training sessions is available. (11) Two peer leaders (1 in the general health group and 1 in the HIV group) did not complete training, leaving 16 trained and qualified peer leaders (8 control; 8 HIV intervention group).
Intervention
Facebook was used to create secret (unable to be accessed or searched for by non-group members) HIV prevention and general health groups. Participants were randomly assigned to either a general health or HIV prevention secret group. During each of the 12 weeks, peer leaders attempted to communicate with their group participants through Facebook chat, messages, and group wall posts approximately 2–3 times per week. HIV group peer leaders were instructed to communicate about HIV prevention, while control group peer leaders communicated general health behaviors such as exercise, nutrition and stress control. Peer leaders were paid each week for their participation.
Participants could connect with other group participants and peer leaders by expressing thoughts, experiences, or friendly conversations. Participants were told to use Facebook as they normally would. They did not receive participation-based incentives and had no obligation to respond to or engage with peer leaders or other group participants, or to remain part of the Facebook groups. Participants could request one free home-based HIV testing kit during the intervention.
Measures
Participation
Participant conversations on the Facebook groups were collected.
HIV testing requests
Requests for home-based HIV tests were recorded. Home Access Health (the testing kit manufacturer) provided a pin number on each kit associated with the participant ID and recorded before sending. Participants testing positive were routed to a Home Access counselor for post-test counseling services.
Statistical Analysis
This analysis includes qualitative (topics and themes discussed by group participants) as well as quantitative data (participant demographic information and requests for a home-based HIV testing kit). For qualitative data, Facebook has a feature known as the “Wall” that allows participants to communicate in an open forum group members. Participants can post text, reply to posts, and “Like” comments. In addition, links to photos, videos and websites can be added. Posts are placed in reverse chronological order on the group page, with a time stamp. This provides an opportunity to evaluate content of participant conversations. We used grounded theory to code participant conversations and elicit key themes.
After twelve weeks, screen captures of the group Facebook Wall were coded and analyzed using Dedoose Software (SocioCultural Research Consultants, CA, USA). Prior to analysis, participant names were replaced by anonymous IDs, and profile photos removed, to maintain the participant privacy while blinding the researchers.
The following codes were applied to the Facebook Wall in the HIV group: HIV and Knowledge, HIV and Stigma, HIV and Culture, HIV Advocacy, Promoting or Discussing HIV-STI Prevention and Testing, MSM Culture, and Friendly Conversation. HIV and Knowledge was defined as a conversation related to facts about HIV/AIDS including methods of transmission, epidemiology, and treatment. HIV and Stigma was coded if the discussion related to stigma associated with HIV positive individuals, and/or barriers to test or reveal HIV status because of stigma. HIV and Culture was identified if the conversation related to the sociocultural barriers to HIV/AIDS prevention, such as related to race, religion, and community. Promoting and Discussing HIV-STI Prevention and Testing was used if participants discussed topics around the prevention and testing of HIV and other STIs, or promoted HIV testing to other participants. MSM culture was defined if the discussion was about topics specific to the MSM community, including community events, advocacy and challenges facing MSM. Friendly Conversation was defined as all other conversation not related to the above topics. There was a 0.91 Kappa statistic between two independent coders, demonstrating a strong agreement regarding the conversation themes.
Participation in the given theme was defined if a person initiated, responded or “Liked” a post related to that topic. Posts could represent more than one topic and be tagged with multiple codes. Excerpts were also classified by study period, (i.e., first, second or third 4-week period of the study), as determined by the time stamp.
Qualitative excerpts were stratified by participants’ (quantitative) survey responses about their age (older or younger than 31.2 years, the mean age) and race. Excerpts were also divided by study period to evaluate the change in excerpt type over each 4-week period. Values are expressed in frequency and percentage of excerpts by subgroup. Simple and multiple logistic regression (controlling for age and race) on Stata Software version 12.1 (StataCorp, College Station, TX, USA) was used to determine the relationship between HIV testing requests and conversation themes.
RESULTS
Table 1 presents demographic information about HIV group study participants. Participants were on average 31 years old, with almost 60% Latino and almost 30% African American.
Table 1.
Demographic Characteristics by participants in HIV prevention Facebook group (n=57)
| Characteristics: n (%) | Group participants) |
|---|---|
| Age (mean, SD) | 31.2 (10.6) |
| Race | |
| African American | 17 (29.8%) |
| Latino | 34 (59.7%) |
| White | 5 (8.8%) |
| Asian | 1 (1.8%) |
| Highest Education | |
| Less than high school | 3 (5.3%) |
| High School | 14 (24.6%) |
| GED | 3 (5.3%) |
| Associates | 14 (24.6%) |
| Bachelors | 16 (28.1%) |
| Graduate school | 7 (12.3%) |
| Monthly Income | |
| $1000 or less | 31 (54.4%) |
| $1001 – $2000 | 9 (15.8%) |
| $2001 – $3000 | 11 (19.3%) |
| > $3000 | 6 (10.5%) |
| Birthplace | |
| Northern USA | 7 (12.3%) |
| Southern USA | 7 (12.3%) |
| Eastern USA | 3 (5.3%) |
| Western USA | 38 (66.7%) |
| Latin America/Caribbean | 2 (1.8%) |
| Self-described sexual orientation | |
| Homosexual | 42 (73.7%) |
| Bisexual | 10 (17.5%) |
| Heterosexual/questioning/don’t kno | 5 (8.8%) |
| Current marital status | |
| Single | 42 (75.0%) |
| Married | 2 (3.6%) |
| Partnered | 8 (14.3%) |
| Divorced | 4 (7.1%) |
| Have a computer at home | 52 (91.2%) |
Participants engaged in 485 conversations over the group Wall. We identified five major HIV-related themes: HIV-STI prevention and testing, HIV and Knowledge, HIV and Culture, HIV and Stigma and HIV Advocacy (Table 2). Participants were comfortable initiating and sharing information about HIV, including experiences with stigma and discrimination, fears about HIV testing, and desire to change HIV policies. Twenty-nine percent (29%) of total discussion by participants was related to these topics, with the remaining conversations related to MSM culture (12%), and friendly conversation (59%).
Table 2.
Topics discussed among MSM on Facebook HIV prevention groups (485 conversations)
| Topic (% of overall conversations) | Example quote |
|---|---|
| HIV-STI prevention/testing (15%) | I tend to feel that despite it all, being apart of the group would inspire each of us to get tested. I agree it is a personal responsibility but on some level I feel it is a social one as well. Despite what ever your reasoning, it will remain a private matter unless you chose to divulge it with the group. But, for all of those who haven’t; knowing is worth it in the end. Let’s just do it! |
| HIV and Knowledge (6%) | (in response to a Website link that a group member posted on the scale of the universe) HIV is 90 nanometers in size… almost as big as a pit on a CD… and it affects the red and white blood cells… |
| HIV/AIDS and culture (.2%) | I am a Gay Black man who is not in jail, alive & healthy and HIV free. Despite all of it, I am a man who continues to be and be a better man daily. So, in the end; I remain most humble. |
| HIV and stigma (4%) | Despite 30 years of livng with HIV within the gay community there is still MAJOR stigma attached to being poz from neg guys…It also further harkens back to a deep underlying pathology within this community…Welcome to the Scarlet “H”. |
| HIV advocacy (3%) | I doubt there will be a cure or vaccine for HIV/AIDS because spending money on a lifelong treatment is better than one treatment and you’re set. The Pharmaceutical Companies are in business for profits not remedies. |
| LGBT/MSM Culture (12%) | Hi Everyone, Every year we host an event at Disneyland in October called Gay Days. It is a chance for the community to come to the park, meet new people and show your pride by wearing red shirts. |
| Friendly conversation (59%) | Hope everybody had a ‘safe’ weekend!!! Whats up with this weather??? |
Figure 1 displays the breakdown of topics by each 4-week period. Initially, topics focused on friendly conversation, MSM culture, and sharing HIV knowledge, with HIV prevention and testing taking up approximately 5% of conversations. By the final 4 weeks, friendly conversation had decreased, as approximately 35% of conversations focused on HIV prevention and testing, with approximately 15% focused on HIV and stigma.
Figure 1.
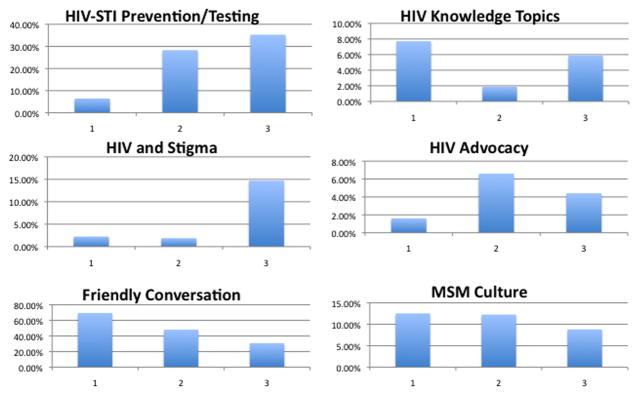
Percent of total excerpts related to a given topic, by time period
Table 3 shows the topics discussed by demographics and request for home-based HIV testing kit. African American and Latino MSM actively used the groups for each of the conversation topics. Older participants contributed more frequently to HIV-related conversations while younger participants contributed friendly conversations more frequently. Those who requested HIV testing kits contributed more to HIV-related topics. Non-HIV-related conversations did not appear to differ based on HIV testing kit request.
Table 3.
Topics discussed among participants based on demographics
| HIV-STI Prevention/Testing | HIV Knowledge | HIV and Culture | HIV and Stigma | HIV Advocacy | Friendly Conversation | MSM Culture | |
|---|---|---|---|---|---|---|---|
| Race | |||||||
| Latino (%) | 33 (44.6) | 27 (90) | 0 | 7 (36.8) | 5 (33.3) | 192 (66.7) | 37 (63.8) |
| African American (%) | 28 (37.8) | 2 (6.7) | 1 (100) | 10 (52.6) | 10 (66.7) | 75 (26) | 14 (24.1) |
| Other (%) | 13 (17.6) | 1 (3.3) | 0 | 2 (10.5) | 0 | 21 (7.3) | 7 (12.1) |
| Age | |||||||
| ≤31.2 years | 27 (36.5) | 19 (63.3) | 0 | 1 (5.3) | 4 (26.7) | 169 (58.7) | 39 (67.2) |
| > 31.2 years | 47 (63.5) | 11 (36.7) | 1 (100) | 18 (94.7) | 11 (73.3) | 119 (41.3) | 19 (32.8) |
| HIV Testing Kit Requested | |||||||
| Yes (42.11%) | 67 (90.5) | 18 (60) | 1 (100) | 14 (73.7) | 13 (86.7) | 141 (49) | 27 (46.6) |
| No (57.89%) | 7 (9.5) | 12 (40) | 0 | 5 (26.3) | 2 (13.3) | 147 (51) | 31 (53.4) |
Table 4 displays results of a logistic regression with conversation topics as independent variables and requests for HIV testing kits as the dependent variable. Compared to participants who did not discuss HIV prevention, those who discussed HIV prevention with other group members had over 9 times the odds of requesting an HIV test. When adjusted for age and race, these effects remained significant.
Table 4.
Topics discussed among participants based on HIV testing requests
| Univariate | Multivariate+ | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Requested HIV Test Kit N (%) | Didn’t Request | OR | 95% CI | P value | OR | 95% CI | P value | |
| Posted on the Wall about HIV-STI Prevention/Testing | 15 (62.5) | 5 (15.15) | 9.33 | 2.65–32.91 | 0.001** | 11.14 | 2.52–49.31 | 0.001** |
| Knowledge | 6 (25) | 4 (12.12) | 2.42 | 0.6–9.75 | 0.22 | 1.99 | 0.46–8.58 | 0.36 |
| Stigma | 7 (29.17) | 3 (9.09) | 4.12 | 0.94–18.05 | 0.06 | 6.56 | 0.96–45.01 | 0.06 |
| Culture | 1 (4.17) | 0 | - | - | - | - | - | - |
| Friendly Conversation | 12 (50) | 17 (51.52) | 0.94 | 0.33–2.69 | 0.91 | 1.05 | 0.3–3.59 | 0.94 |
| MSM Culture | 9 (37.5) | 7 (21.21) | 2.23 | 0.69–7.21 | 0.18 | 3.36 | 0.88–12.88 | 0.08 |
Significant at the p < .01 level
Controlling for age and race
DISCUSSION
While the dynamic and large Facebook community could be an important tool for HIV and STD prevention, it is not currently known whether at-risk individuals would actually use it for this purpose, or whether participation would be associated with health promoting behaviors such as requesting an HIV test kit. Results from this mixed method analysis suggest that social networking technologies are a feasible platform for engaging HIV and STD prevention conversations among African American and Latino MSM, and that participants’ online HIV/STD testing conversations are associated with actual requests to receive a home-based testing kit. While African American and Latino MSM peer leaders established the initial social norms to promote HIV-related communication, group participants quickly accepted this norm and used the social networking group to initiate their own HIV-related conversations with other group members. As the study progressed, overall discussions declined, but the fraction related to HIV-STI Prevention and Testing and HIV and Stigma increased, demonstrating the acceptability of using the technology for HIV-related conversations. Finally, we found that HIV prevention-related conversations are associated with HIV-related behaviors, such as HIV testing.
Results demonstrate the utility and acceptability of using social networking technologies for HIV prevention, especially among minority populations. In the initial days of the Internet there was a large socioeconomic “digital divide.” However, this divide has narrowed, in large part due to social networking usage among minority populations. In fact, English-speaking Latinos and African Americans are almost 1.5 times more likely to use social networking sites compared to the general adult population (33% of African Americans, 36% of English-speaking Latinos, and 23% of adults in the general population). (12)
It is important to note the differences in topics discussed among the sample, as well as the fact that individual participants varied in the amount of information they shared with the groups. For example, older participants more frequently discussed HIV Prevention and Testing, Stigma, and Advocacy topics, though younger participants participated more in conversations about HIV Knowledge, MSM culture, and overall friendly conversation. It might be that younger participants were interested in friendly conversations and general learning about HIV, but discussed stigma and testing experiences less frequently due to being younger and less experienced with these topics. Additionally, only one participant engaged in a conversation around the theme of HIV and culture. Because HIV and culture may be a personal conversation topic (for example, discussing the difficulty of revealing one’s HIV status within a religious family), it is possible that these conversations were discussed in more private forums (such as private messages and chats). In fact, peer leaders’ personal reports suggest that participants were more likely to discuss personal experiences such as HIV and culture through private messages and chats. While social networking technologies have changed social norms to make public “sharing” of information widely accepted, it is still important to understand that certain topics are best discussed through more private online or offline communication methods.
A limitation of these findings is that peer leaders initiated initial conversations about HIV/AIDS, making it important to emphasize that simply inviting at-risk participants to social networking groups might not increase HIV-related communications. In fact, the absence of HIV-related conversations among general health group participants suggests that it is doubtful that participants will generate HIV prevention conversations without guidance. However, the study does demonstrate that peer leaders can initiate discussion of HIV-related content, and that at-risk participants will respond and initiate their own HIV-related conversations with other group members. Additionally, this paper focuses on topics discussed over the Facebook group Wall (public for all members of the group). It is possible that these conversation themes would not occur in private settings on social networks, such as private message and chat. While we found similar discussion rates among private messages and chats, those statistics are not reported here as they were self-reported by peer leaders and could not be verified with a time stamp. Nevertheless, peer leader reports corroborate our findings and suggest that participants were also discussing HIV-prevention topics through private chats and messages. It is also unknown whether these results will generalize to testing of STD’s other than HIV. However, as participants conversation topics focused on not just HIV but also other STD’s, we believe these results will generalize to prevention of testing of other STD’s such as Chlamydia and Gonorrhea. Future research can explore this question. Finally, while these results are based on a 3-month intervention, it is unknown whether the present results would be sustainable over a longer time period. Future results of this longitudinal intervention will help address that question.
CONCLUSION
This study demonstrates that social networking technologies are a feasible and acceptable platform for increasing HIV and STD-related communication among African American and Latino MSM. Participants frequently and willingly used social networking groups to initiate HIV-related conversations, and HIV/STD prevention-related conversations were associated with actual increased requests for a home-based HIV test. As social networking usage continues to grow among at-risk populations, it becomes important to understand how to use these innovative and engaging social technologies for population-focused STD prevention.
Summary.
A mixed-methods study found that African American and Latino MSM were willing to use social networking technologies to discuss HIV-prevention topics, and that their discussions were associated with increased requests for home-based HIV testing.
Acknowledgments
This work has been generously supported by the help of the National Institutes of Mental Health (NIMH).
Footnotes
There are no conflicts of interest.
References
- 1.Eysenbach G. Medicine 2.0: social networking, collaboration, participation, apomediation, and openness. J Med Internet Res. 2008;10(3):e22. doi: 10.2196/jmir.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radicati S. Social networking report. Palo Alto, CA, USA: The Radicati Group, Inc; 2010. pp. 1–5. [Google Scholar]
- 3.Young SD, Rice E. Online Social Networking Technologies and HIV Knowledge, Sexual Risk Behaviors, and Testing for Sexually Transmitted Infections. AIDS and Behavior. 2011;15(2):253–60. doi: 10.1007/s10461-010-9810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan PS, Khosropour CM, Luisi N, Amsden M, Coggia T, Wingood GM, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13(2):e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gold J, Pedrana AE, Sacks-Davis R, Hellard ME, Chang S, Howard S, et al. A systematic examination of the use of online social networking sites for sexual health promotion. BMC. 2011;11:583. doi: 10.1186/1471-2458-11-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers E. Diffusion of innovations. 4. New York: Free Press; 1995. [Google Scholar]
- 7.Maiorana A, Kegeles S, Fernandez P, Salazar X, Caceres C, Sandoval C, et al. Implementation and evaluation of an HIV/STD intervention in Peru. Eval Program Plann. 2007 Feb;30(1):82–93. doi: 10.1016/j.evalprogplan.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly J, Murphy D, Sikkema K. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Lancet. 1997;350:1500–05. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 9.Young S. Recommended Guidelines on Using Social Networking Technologies for HIV Prevention Research. Aids and Behavior. 2012;16(7):1743–5. doi: 10.1007/s10461-012-0251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jaganath D, Gill HK, Cohen AC, Young SD. Harnessing Online Peer Education (HOPE): integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care. 2011;24(5):593–600. doi: 10.1080/09540121.2011.630355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young SD, Harrell L, Jaganath D, Cohen AC, Shoptaw S. Feasibility of recruiting peer educators for an online social networking-based health intervention. Health Education Journal. 2012 Apr 13; doi: 10.1177/0017896912440768. Published online before print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith A Project PIAL, editor. Technology trends among people of color. 2010. Commentary: Race and Ethnicity, Digital Divide. [Google Scholar]


