Abstract
Background
Total transposition of the superior and inferior rectus muscle laterally, with augmentation sutures, may be complicated by induction of an undesirable vertical deviation. Induced vertical misalignment may be associated with changes in torsion. We have developed a simple method to monitor intraoperative torsion that may reduce the incidence of vertical deviations.
Methods
We reviewed consecutive cases of total abducens palsy or esotropic Duane syndrome treated with augmented lateral transposition of the superior and inferior rectus muscles, where the 12 o’clock and 6 o’clock intraoperative positions were initially marked with a dot at the limbus using a surgical pen. The location of the marks was monitored during tying of the augmentation sutures; changes in torsion were monitored intraoperatively.
Results
Records of 9 cases of augmented vertical rectus transposition were reviewed. Based on intraoperative assessment of torsion by observing the position of the preplaced limbal dots, the inferior rectus augmentation suture was tied less tightly than the superior rectus suture, leaving a gap of 1–3 mm between the inferior and lateral rectus muscles in 8 of 9 cases. The augmentation suture was totally removed in 1 case. Following these intraoperative adjustments, there was no induced intraoperative torsion, whereas further tightening of the inferior suture induced extorsion. Six weeks postoperatively, 8 of 9 patients did not experience a symptomatic vertical deviation.
Conclusions
When performing augmented transposition procedures, intraoperative monitoring of torsion may reduce the incidence of inadvertent vertical deviations and torsion. This technique may also be useful in other cases where correction or avoidance of torsion is needed.
In 1997 Scott Foster described augmenting a total lateral transposition of the superior and inferior rectus muscles using polyester (Mersilene, Ethicon, Inc, Somerville, NJ) sutures placed 8 mm behind the superior and inferior poles of the lateral rectus muscle insertion.1 This procedure was designed to enhance the effect of the transposition and to allow surgery on only the superior rectus muscle and inferior rectus muscle in many cases of total sixth (abducens) nerve palsy or esotropic Duane syndrome.1 One reported complication of the procedure is induction of an undesirable vertical deviation.2 Having also encountered this complication, we developed a simple method of intraoperative monitoring that may reduce its incidence. The method is based on a possible association between changes in torsion and changes in vertical deviation when performing vertical muscle transposition. We report this technique of intraoperative monitoring of torsion to reduce the risk of inadvertent vertical deviations.
Patients and Methods
Approval of the Mayo Clinic Institutional Review Board was obtained and all data were collected in a manner compliant with the Health Insurance Portability and Accountability Act. The surgical database of one surgeon (JMH) was searched for all cases of augmented full-tendon transpositions performed for total abducens nerve palsy or Duane syndrome, where intraoperative monitoring of torsion was performed using the technique described. Cases were excluded from this case series if previous transpositions had been performed elsewhere or if simultaneous vertical surgery was performed. Simultaneous horizontal surgery was allowed.
Surgical Technique
At the start of the procedure, after induction of general anesthesia and before any intraoperative rotation of the eye, the 12 o’clock and 6 o’clock positions at the limbus were marked with a blue skin marking pen (Figure 1A). A 180-degree conjunctival perimetry was performed, and 6-0 polyester fiber suture (Mersilene; Ethicon, Inc, Somerville, NJ) augmentation sutures were placed taking 3 mm scleral bites 8 mm back from the superior and inferior poles of the lateral rectus muscle, just above and below the belly of the muscle, in the manner described by Foster.1 The superior and inferior rectus muscles were imbricated with a 6-0 polyglactin 910 suture (Vicryl; Ethicon, Inc, Somerville, NJ) after carefully cleaning the attachments to the upper and lower lids, detached from the sclera and reattached to the sclera laterally along the spiral of Tillaux, so that the lateral pole of the superior rectus muscle was apposed to the superior pole of the lateral rectus muscle and the lateral pole of the inferior rectus muscle was apposed to the inferior pole of the lateral rectus muscle. The superior 6-0 polyester fiber augmentation suture was then passed through the lateral third of the superior rectus muscle, 8 mm back from its insertion, so that the lateral edge of the superior rectus muscle belly was apposed to the superior edge of the lateral rectus muscle belly.
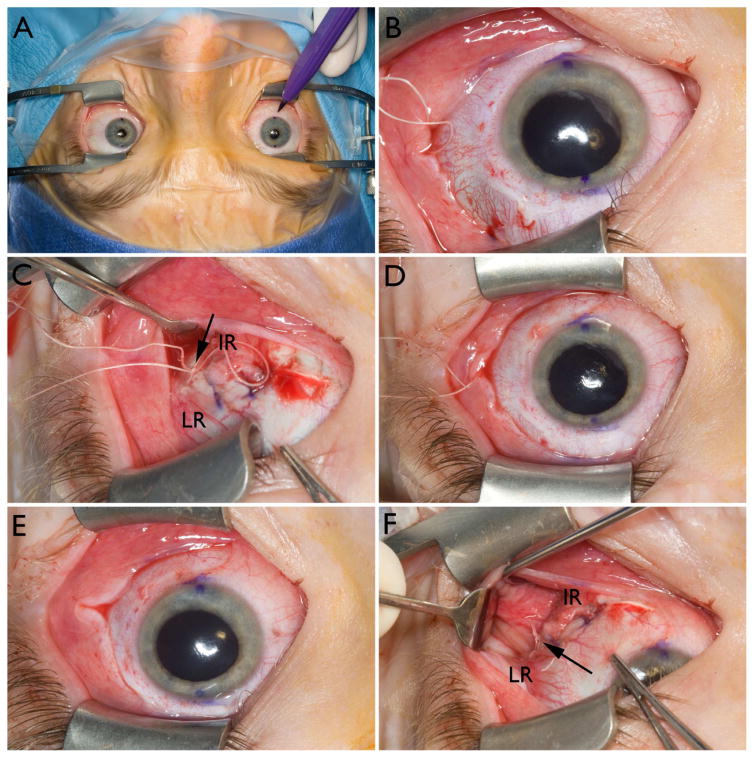
FIG 1.
Using blue dots at the limbus to monitor intraoperative torsion during augmented vertical muscle transposition. A, Marking 12 o’clock and 6 o’clock at each limbus at the start of the case, following induction of anesthetic, using a sterile skin marking pen. B, Intorsion of left eye (surgeon’s view) after both superior rectus muscle and inferior rectus muscle have been transposed laterally and after tying only the superior augmentation suture. C, Inferior augmentation suture is bow tied, setting the inferior rectus muscle belly approximately 3 mm from the lateral rectus (LR) muscle belly (arrow in C). D, Eye is then noted to be still slightly intorted. E, The inferior augmentation suture is untied and the inferior rectus (IR) muscle belly pulled up 1 mm more until there is no residual torsion. F, The inferior augmentation suture is then permanently tied, leaving the inferior rectus muscle belly, in this case, 2 mm from the lateral rectus muscle belly (arrow).
At this stage of the procedure the eye consistently became intorted (Figure 1B) due to the unbalanced effect of augmenting only the superior rectus muscle transposition. The inferior 6-0 polyester fiber augmentation suture was then passed through the lateral third of the inferior rectus muscle, 8 mm back from its insertion, and temporarily tied in a bow when the lateral edge of the inferior rectus muscle was 2 mm from the inferior edge of the lateral rectus muscle. Our unpublished previous experience of induced hypotropia following transposition had lead to the conclusion that if the inferior augmentation suture was tied to appose the inferior rectus muscle belly to the inferior aspect of the lateral rectus muscle belly, the inferior rectus muscle might be relatively too tight, increasing the risk of extorsion and hypotropia. The preplaced blue dots at 12 o’clock and 6 o’clock on the limbus were then carefully monitored. During intraoperative adjustment of the position of the inferior rectus muscle, the augmentation suture was bow tied and the positions of the preplaced limbal blue dots were inspected. If extorsion was noted, the inferior augmentation suture was untied and the inferior rectus muscle belly was allowed to return toward its original position, resulting in less extorsion. The suture was then retied in a bow tie and the limbal dots reinspected. Similarly, if the eye was intorted, the inferior rectus muscle augmentation suture could be untied and tightened, pulling the inferior rectus muscle belly closer to the lateral rectus muscle belly. The desired endpoint was no extorsion or intorsion based on the position of the preplaced limbal blue dots (Figure 1C), as assessed by the surgeon who was positioned at the head of the bed. In this position, the inferior polyester fiber augmentation suture was tied.
After the patient awoke from anesthesia, any adjustment was limited to medial rectus muscle recession, which would not be expected to influence the vertical or torsional alignment. Postoperative status was assessed at a 6-week visit (range, 3–10 weeks).
Results
We identified 9 cases of augmented full-tendon transposition with intraoperative monitoring of torsion. Six patients had unilateral total abducens nerve palsy, 1 bilateral total abducens nerve palsy, and 2 Duane syndrome. Ages ranged from 11 to 83 years. Two of the unilateral abducens nerve palsies and both Duane syndrome cases were children aged 11, 12, 14, and 15 years respectively. Preoperatively, primary position distance esotropia, measured using simultaneous prism and cover test ranged from 35Δ – to 50Δ in the 6 unilateral abducens nerve palsy cases, 20Δ in both cases with Duane syndrome and >50Δ in the case with bilateral sixth nerve palsy. None of the cases had a preoperative vertical deviation measurable by simultaneous prism and cover test, but 2 of the unilateral cases had 1Δ and 4Δ hypertropia, respectively, by prism and alternative cover test and the bilateral case had 6Δ hypertropia by prism and alternate cover test. Preoperative torsion, measured using double Maddox rods, ranged from 3 degrees intorsion to 5 degrees extorsion (2 of the children were not tested).
Based on intraoperative assessment of torsion by observing the position of the preplaced limbal dots, the inferior rectus augmentation suture was adjusted to leave the final position of the inferior rectus muscle belly from 1 mm to 3 mm from the lateral rectus muscle belly in 8 of the 9 cases: 2 mm from the lateral rectus muscle belly in 6 cases (both eyes in the bilateral case) and 1 mm in one case and 3 mm in one case. In 1 case of Duane syndrome, we needed to completely remove the inferior rectus muscle augmentation suture in order to eliminate extorsion.
Six weeks postoperatively (range, 3–10 weeks), distance esotropia in forced primary position had improved in all cases to between 4Δ exotropia and 12Δ esotropia by simultaneous prism and cover test. Three cases had a postoperative hypotropia in forced primary position by simultaneous prism and cover test: in 1 patient the hypotropia was minimal, measuring 2Δ and in one it measured 4Δ, but could be fused with a small face turn without diplopia. The third patient (with Duane syndrome) developed a 14Δ hypotropia with diplopia, despite completely removing the inferior rectus muscle augmentation suture intraoperatively. Of the 8 unilateral cases, 7 reported single vision in primary position or with a small head turn to compensate for any tiny residual esotropia in primary position. The 1 unilateral case with symptomatic vertical diplopia subsequently required recession of the inferior rectus muscle combined with contralateral superior rectus muscle recession. The bilateral case, measuring 95Δ of esotropia (by prism and alternate cover test preoperatively) had persistent horizontal diplopia but the residual angle only measured 12Δ esotropia.
We specifically asked each patient about torsional diplopia symptoms: none of the 9 patients complained of symptomatic torsion. Pre- and postoperative torsion measurements, using double Maddox rods, were available in 6 of the 9 cases. The change in torsion from before surgery to 6 weeks after surgery ranged from 4° of intorsion to 5° of extorsion.
Discussion
We have described a surgical technique that may help surgeons avoid unintended vertical deviations and unintended torsion when performing augmented full-tendon transpositions of the superior and inferior rectus muscles for total abducens nerve palsy and Duane syndrome. The technique involves marking the limbus at 12 o’clock and 6 o’clock, observing the position of the dots when temporarily tying the inferior augmentation suture, and if necessary, adjusting the tension of the augmentation suture to optimally position the inferior rectus muscle belly before permanently tying the suture. Using this technique, 8 of the 9 patients did not experience a symptomatic postoperative vertical deviation.
The reported incidence of unintended vertical deviations when performing augmented full-tendon transpositions for total abducens nerve palsy and Duane syndrome is not high, estimated in one study as 19% (4 of 21 cases)1 and in another as 8.5% (7 of 82 cases).2 Ruth and colleagues2 also mention “other cases” in their series where the operating surgeon made changes in the position of the vertical rectus muscle or tightness of the augmentation suture to avoid a subsequent vertical deviation, commenting that there is a learning curve to successfully performing this procedure without complication. We suggest that our technique may help both the novice and experienced surgeon avoid inadvertent vertical deviations when performing augmented transpositions.
Our technique makes assumptions about the relationship between vertical and torsional alignment in transposed muscles. Prior to developing our technique, we had noted that some cases of postaugmented transposition had a hypotropia associated with marked extorsion. Previous authors have also described induced hypotropia more often than induced hypertropia, following both augmented2 and nonaugmented transposition.3 We reasoned that an unintended vertical/torsional deviation was due to a relatively tight inferior rectus muscle, despite surgery being performed with care to assure symmetry of inferior and superior rectus muscles. We hypothesized that perfect symmetry between inferior and superior rectus muscles during an augmented transposition may therefore be undesirable. It is unclear exactly why symmetric augmentation of transposed vertical rectus muscles might result in induced vertical deviation. Anatomical differences between the superior and inferior rectus muscles may play a role, and mechanical factors, connective tissue, or attachments to the eyelid may affect the force of the transposed muscle. Alternatively, as discussed by Laby and colleagues,3 it may be that differences in tension between nasal and temporal portions of the new insertion results in vertical misalignment.
Little has been published on changes in torsional and vertical alignment with vertical muscle transposition surgery. In the present study, intraoperative changes in torsion were noted when both the augmentation sutures were tied—intorsion when the superior suture was tied and extorsion when the inferior suture was tied. Nevertheless, in a recent study by Mehendale and colleagues4 of augmented superior rectus muscle transposition alone (with adjustable medial rectus recession), there were surprisingly no cases of surgically induced torsion or vertical deviation. It is possible that the discrepancy between our study and theirs4 is due to our taking one-third of the muscle width in the augmentation suture versus their one-quarter of the muscle width. As discussed by Mehendale and colleagues,4 enhanced modeling of the forces operating within the orbit may be needed to explain the absence of intorsion and hypertropia with their method.
As an interim step in the development of our described technique, several cases were performed with monitoring of fundus torsion using an indirect ophthalmoscope. Although this was effective and led to the approach of initially tying the augmentation suture to set the inferior rectus muscle belly 2 mm away from the lateral rectus muscle belly, monitoring fundus torsion was somewhat time consuming and inconvenient. Therefore the method of marking the limbus at 12 o’clock and 6 o’clock was developed.
Other methods of avoiding inadvertent vertical and torsional deviations during augmented transpositions have been described. Rosenbaum’s group2 has stressed performing vertical forced ductions at the end of the surgical procedure to ensure there are no vertical restrictions. They have also pointed out that because hypotony develops during strabismus surgery, forced duction testing at the termination of the surgical case may provide a false-negative result. Based on their report,2 it would appear that the forced-duction method alone at the conclusion of the procedure does not eliminate inadvertent vertical and torsional deviations.
It is possible that recently described modifications of augmented transpositions such as those described by Struck and colleagues5 might have a lower incidence of vertical and torsional complications than the original procedure described by Foster. Nevertheless, Struck does report the development of postoperative vertical deviation5 in 1 of 10 cases and therefore monitoring of intraoperative torsion may also be beneficial when using Struck’s modification. Other recently described transposition techniques include the crossed adjustable transposition for use in nonaugmented transposition surgery, described by Phamonvaechavan and colleagues.6 Nevertheless, the rate of induced vertical deviations ranged from 17% (conventional transposition) to 26% (crossed adjustable transposition).6
We had 1 patient with Duane syndrome who underwent augmented transposition with an unusual course. Intraoperatively the inferior augmentation suture had to be completely slack to avoid extorsion and so was removed during surgery. Nevertheless, the patient still developed a 4Δ hypotropia the day following surgery which by 8 weeks postoperatively had increased to 14Δ by simultaneous prism cover test, requiring subsequent recession of the inferior rectus muscle combined with contralateral superior rectus muscle recession. We attribute this unusual outcome to abnormal innervation of the inferior rectus muscle due to Duane syndrome in this case. We speculate that our technique of monitoring torsion may not be universally successful in preventing induced vertical deviations in Duane syndrome, due to abnormal innervation.
The main weakness of our study is the small number of cases. The 95% confidence intervals of 1 of 9 cases (11%) are 0% and 48%. A very large series would be needed to conclude that the true rate of induced vertical deviation was very close to zero. Additional weaknesses are unknown measurement error and unknown minimum detectable torsional changes using our method. Although more rigorous studies are warranted to confirm our findings, we believe that this technique provides at least one method of potentially reducing the incidence of unintended vertical and torsional deviations when performing augmented full-tendon transpositions for total abducens nerve palsy and Duane syndrome.
We have subsequently found that this technique of monitoring intraoperative torsion is very useful in a spectrum of cases, from addressing torsional diplopia in superior oblique muscle dysfunction to cases of Graves disease, where recessing tight vertical muscles can have differential effects on torsion.
Acknowledgments
Supported by National Institutes of Health Grants EY015799 and EY018810 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Footnotes
Presented in part at a workshop during the 36th Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, Orlando, Florida, April 14–18, 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997;1:20–30. doi: 10.1016/s1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 2.Ruth AL, Velez FG, Rosenbaum AL. Management of vertical deviations after vertical rectus transposition surgery. J AAPOS. 2009;13:16–9. doi: 10.1016/j.jaapos.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Laby DM, Rosenbaum AL. Adjustable vertical rectus muscle transposition surgery. J Pediatr Ophthalmol Strabismus. 1994;31:75–8. doi: 10.3928/0191-3913-19940301-03. [DOI] [PubMed] [Google Scholar]
- 4.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition combined with medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130 doi: 10.1001/archophthalmol.2011.384. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Struck MC. Augmented vertical rectus transposition surgery with single posterior fixation suture: Modification of Foster technique. J AAPOS. 2009;13:343–9. doi: 10.1016/j.jaapos.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Phamonvaechavan P, Anwar D, Guyton DL. Adjustable suture technique for enhanced transposition surgery for extraocular muscles. J AAPOS. 2010;14:399–405. doi: 10.1016/j.jaapos.2010.08.004. [DOI] [PubMed] [Google Scholar]