Abstract
Objective
This study aimed to explore how well Victorian pharmacists perceived they understood pharmacogenetics, their perceived capacity to counsel a patient about such testing, how they believed pharmacogenetics would impact upon their profession, and to investigate the ways in which Victorian pharmacists would like to be educated about pharmacogenetics.
Methods
A cross-sectional survey was dispatched to 800 Victorian pharmacists. The participants were randomly selected and the survey was anonymous. The survey contained questions about where the pharmacists worked, the pharmacists’ perceived knowledge of pharmacogenetics, how well they believed they would be able to counsel patients about pharmacogenetic testing, how they thought pharmacists should be educated on the topic and how they believed pharmacogenetics would impact upon their profession.
Results
291 surveys were returned (36% response rate). Results suggest that Victorian pharmacists generally perceived they had a poor understanding of pharmacogenetics and that those who have more recently graduated from tertiary education had a better perceived understanding than those who have been in the workforce for longer. Most pharmacists indicated that they did not believe that they could counsel a patient adequately about the results of a pharmacogenetic test. Regarding education about pharmacogenetics, participants suggested that this would be best delivered during tertiary studies, and as seminars and workshops forming part of their continuing professional development. Although some pharmacists were unsure how pharmacogenetics would affect their profession, many believed it would have a major impact upon their role as a pharmacist and lead to improved patient care. Some concerns about the implementation of pharmacogenetics were noted, including economic and ethical issues.
Conclusions
This study highlights the need for further research across the pharmacy profession in Australia on the issue of preparedness for the putative incorporation of pharmacogenetics into the healthcare system and everyday practice.
Keywords: Pharmacogenetics; Pharmacists; Health Knowledge, Attitudes, Practice; Australia
Introduction
Pharmacogenetics refers to the influence that an individual’s genetics has on drug response.1,2,3,4 To be able to screen for and identify specific genes that may be involved in adverse drug reactions would be of immense benefit to patients. Understanding these technologies will allow health professionals, including pharmacists, to play a role in the implementation of ‘personalised medicine’ in the prevention and treatment of certain conditions.1,2,3 This personalised medicine may help reduce the incidence of adverse drug reactions, which present a major health problem worldwide, and lead to many patient hospitalisations and deaths every year.4,5 Therefore, by identifying the specific genes which may contribute to adverse drug reactions, health professionals may eventually be able to tailor medication regimes to suit the genetic makeup of patients, leading to increased efficacy, safety and adherence.2,5,6,7,8,9,10,11,12,13
The term ‘pharmacogenetics’ was first developed in the 1950’s to describe clinical observations of inherited differences in response to medicines.14 Since the completion of the Human Genome Project (HGP) in 2001, pharmacogenetics has expanded into an innovative, broad and rapidly growing research area.2,15,16 The HGP was able to identify many protein-coding genes that function as drug metabolising enzymes, receptors and transporters within the body, variations of which result in differing responses to drugs.2,10,17,18 At present, there is information about the influence of genetic differences in the metabolism of over 280 drugs.19 Accordingly, the U.S. Food and Drug Administration has altered the labels of more than a dozen medicines to include pharmacogenetic information.20 It is therefore essential that health professionals and in particular pharmacists understand the concept of pharmacogenetics, are properly educated in the area, and understand how to implement pharmacogenetics into everyday practice.21
Several studies have focused on the implementation of pharmacogenetics into health care and more specifically, pharmacy practice.2,3,6,16,22,23 It is generally accepted that pharmacists will have a role in shaping the way these technologies are incorporated into healthcare. It is likely that they will have a role in the interpretation of pharmacogenetic tests, counseling patients about the pharmacogenetic testing and the influence of these results on their medication regimes.2,3,18 However, given that these screens are relatively new, with most yet to be incorporated into clinical practice, there is a need to develop and implement a systematic method of educating pharmacists about the knowledge and skills which will be required in order to incorporate pharmacogenetics into everyday practice so as to provide optimal pharmaceutical care to patients.2,15,16,23 At present, the perceptions and level of knowledge of pharmacogenetics amongst Australian pharmacists is largely unknown.2,16 Studies that have demonstrated the need to educate pharmacists21,23 have focused on the type of information which should be conveyed.3,16,18,22,24 Yet there has been very little research on Australian pharmacists’ perceptions of pharmacogenetics, their current knowledge regarding pharmacogenetics, and how they would prefer to be educated about this area.
This descriptive exploratory study aims to explore the level of knowledge of pharmacogenetics that pharmacists in Victoria, Australia, perceive they have, how they believe pharmacogenetics will impact upon their profession, and the ways in which they would like to be educated about pharmacogenetics.
Methods
A cross-sectional survey was employed to achieve the aims this study. The survey contained eight questions, with the type of questions being multiple choice, numeric open-ended, text open ended and rating scales. It is estimated that the survey would have taken less than 5-10 minutes to complete. The use of a cross-sectional survey enabled information regarding pharmacists’ perceptions and knowledge about pharmacogenetics to be collected across a large geographical area at one point in time.25 The questions in the survey enabled data to be gathered on a) where the pharmacists worked, b) the pharmacists’ perceived knowledge of pharmacogenetics, c) the perceived ability of the pharmacists to counsel patients about pharmacogenetic testing, d) how pharmacists should be educated on the topic and e) how they believed that pharmacogenetics will affect their careers in the future. The questions used in this study were modelled on findings from previous studies regarding the incorporation of pharmacogenetics into pharmacy.2,3,22,23
For inclusion in this study, participants were required to be registered pharmacists practicing in Victoria. 800 Victorian pharmacists from 400 randomly selected community and hospital pharmacies were asked to participate in this study. The pharmacies, including both community and hospital pharmacies, were randomly selected from an online directory. A survey pack containing a cover letter, a participant information sheet, the survey and a reply paid envelope were dispatched to the pharmacists. Pharmacists were asked to complete the surveys and return them in the reply paid envelope.
Both quantitative and qualitative data was obtained during this study. Quantitative data was analysed using SPSS® version 17.0 for Windows® to generate simple descriptive statistics in order to address the key objectives of this study. Confidence intervals were calculated and the correlation between the number of years the pharmacists had been practicing and their perceived level of knowledge about pharmacogenetics was explored. Qualitative data was interpreted and analysed thematically in order to identify the major areas that pharmacists believe pharmacogenetics will impact upon them.
In order to maintain anonymity of the subjects and confidentiality of this study, the survey did not ask for any identifying information. The return of a completed survey was considered as consent to participate in the study. This was conveyed to the pharmacist in the participant information sheet. Ethical approval for this project was granted by the La Trobe University, Faculty of Science Technology and Engineering Human Research Ethics Committee (Approval # FHEC09/R74).
Results
Of the 800 surveys that were dispatched, 291 (36%) were completed and returned. 77.4% of the participants practiced in a community pharmacy setting, 18.9% practiced in hospitals, 2.2% practiced in both hospital and community pharmacy whilst 1.5% were involved in government or industry work. Of the respondents 31.3% practiced in a rural area, 27.6% in a regional area, 40.7% in a metropolitan area and 0.4% practiced in both regional and metropolitan areas. In terms of the experience of the pharmacists who completed the survey, the majority (43.6%) had been practicing from one month to nine years, 15.5% from 10 to 19 years, 22.6% from 20 to 29 years, 11.7% from 30 to 39 years and 6.6% had been practicing for 40-49 years.
To determine the perceived level of knowledge regarding pharmacogenetics amongst Victorian pharmacists, respondents were asked to rate their understanding of pharmacogenetics on a scale from 1 to 10 (with 1 being the least and 10 being the highest ranking). Of the 291 respondents 78% indicated their understanding to be five or less on the scale. Only 6.5% of respondents rated their understanding of pharmacogenetics to be eight or greater on the scale (Figure 1).
Figure 1.

Figure 1 shows the respondents’ perceived understanding of pharmacogenetics. The respondents had to rate their understanding on a scale from 1 to 10 with 1 being the least ranking and 10 being the highest ranking. The results show that the majority of pharmacists perceived they have a limited understanding of pharmacogenetics.
The relationship between a pharmacist’s experience and their perceived understanding of pharmacogenetics was explored. There was a negative correlation between a pharmacist’s experience and how well they perceived they understood pharmacogenetics (Spearman coefficient= -0.289; P<0.001). Therefore, it appears that pharmacists who had more recently graduated from university have a better perceived understanding of pharmacogenetics than those who had graduated longer ago (Figure 2).
Figure 2.
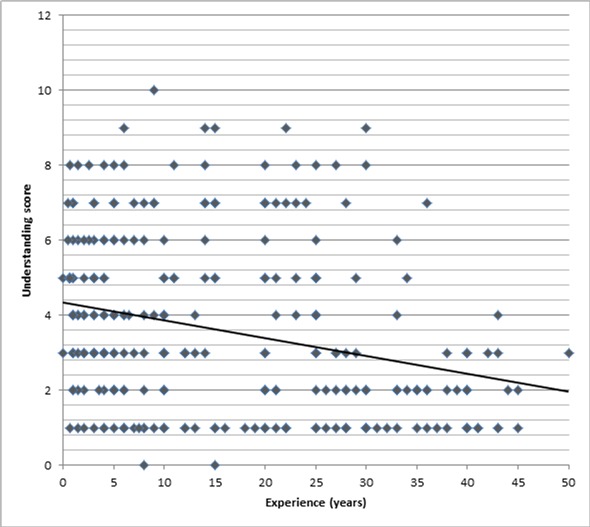
Figure 2 shows the correlation between a pharmacist’s experience and their perceived understanding of pharmacogenetics. The respondents had to rate their perceived understanding on a scale from 1 to 10, with 1 being the least ranking and 10 being the highest ranking. The results show a negative correlation between a pharmacist’s experience and their perceived understanding of pharmacogenetics (Spearman coefficient= -0.289; P<0.001).
When asked how well the pharmacists believed they would be able to counsel a patient about the results of a pharmacogenetic test 1% of respondents believed they could counsel very well, 4.9% indicated that they could counsel well, 24.3% believed they could counsel reasonably well, 37.2% indicated that they would counsel poorly and 32.3% stated they would counsel very poorly (Figure 3).
Figure 3.
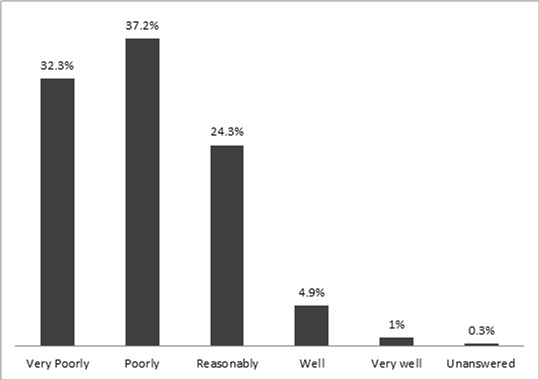
Figure 3 illustrates the pharmacists’ perceived ability to counsel a patient about the results of a pharmacogenetic test. As shown in the figure, the vast majority of respondents believed that they would counsel a patient poorly or very poorly about the results of a pharmacogenetic test.
The survey also asked how the pharmacists had learnt about pharmacogenetics (Table 1). Of the 291 respondents, 31.6% had learnt about pharmacogenetics during their tertiary education, 11.6% had learnt about pharmacogenetics by attending various seminars or lectures, 23.7% had learnt about pharmacogenetics by reading about the subject while 33.1% of respondents indicated that had not learnt about pharmacogenetics at all.
Table 1.
How the pharmacists had learnt about pharmacogenetics
| At university | 31.6% of respondents |
| Self directed learning/reading | 23.7% of respondents |
| Structured seminars or lectures | 11.6% of respondents |
| Had not learnt about the topic at all | 33.1% of respondents |
In order to define optimal ways to educate pharmacists about pharmacogenetics, participants were asked which mode of education they preferred to learn about this topic (Table 2). Pharmacists were able to select more than one option. The majority of respondents believed the best setting to educate pharmacists was at university during a Bachelor of Pharmacy degree (66.7%) and after registration, as workshops and seminars which contribute to pharmacists’ continuing education program (79%). The least popular choices included educating pharmacists during the intern (pre-registration) year (13.1%) and as directed learning which pharmacists undertake on their own (19.2%). Education via information packages and internet based learning activities were preferred by 28.5% and 37.8% of respondents respectively.
Table 1.
Pharmacists’ preferred mode of learning about pharmacogenetics
| At workshops and seminars | 79% of respondents |
| At university | 66.7% of respondents |
| Internet based learning activities | 37.8% of respondents |
| Information packages | 28.5% of respondents |
| Self directed learning | 19.2% of respondents |
| During intern year | 13.1% of respondents |
When the participants were asked how they believed pharmacogenetics would affect their career as a pharmacist, six themes that were frequently cited included the impact on the pharmacy profession, impact on counselling, impact on medicine use, impact on patient, economic consequences of pharmacogenetic testing and education. These major themes (reported below) include quotes taken directly from the respondents.
-
a) Impact on pharmacy profession:
Although many pharmacists were unsure about the impact that pharmacogenetics would have on pharmacy and some believed that it would be minimal, many of the respondents suggested that it would have a very large impact on the future of the pharmacy profession. In particular,
Pharmacogenetics would be a positive challenge that would be embraced enthusiastically and provide another potential avenue for specialisation
Pharmacogenetics would present an opportunity to make the pharmacy profession “more relevant and health orientated”, reinforce their important role as healthcare experts, and enhance communication with doctors and other health care professionals
Pharmacists would be at the forefront of monitoring patients with respect to pharmacogenetic testing
Pharmacogenetics represented the “future of pharmacy”
-
b) Impact on counselling:
Many pharmacists said that counselling was one of the areas of pharmacy practice that pharmacogenetics would have the most impact upon. A summary of the some of the views include:
Pharmacogenetics would result in an increased need for counselling and may require a longer time to be spent with each patient
While making counselling even more complex, pharmacogenetics would improve pharmacists’ ability to counsel patients
Pharmacogenetic information would help tailor treatment and advice for individual patients
The impact of pharmacogenetics on the pharmacy profession would be dependent upon accessibility of test results and willingness of patients to divulge details of their genetic profile.
-
c) Education:
The need to educate pharmacists about pharmacogenetics was a major theme identified by the respondents. Issues raised included:
That the application of the knowledge of pharmacogenetics would become a routine aspect of a pharmacist’s daily activities
That pharmacogenetics and learning about pharmacogenetics would be embraced enthusiastically by pharmacists
That a sound knowledge of pharmacogenetics would be required, as pharmacists may have a role in providing information to doctors and other health professionals about this area
-
d) Impact on medication use:
The perceived impact upon medication use was another major theme in this study. Some of the thoughts of pharmacists included:
That pharmacogenetics would affect all aspects of a patient’s treatment
That pharmacogenetics would result in improved efficacy of the chosen drug and more appropriate dosing, thus enabling the tailoring of medications to individual patients’ requirements
Following on from this, pharmacogenetic testing would result in fewer adverse drug reactions, improved medication safety and management and quality use of medicines.
Polypharmacy would be reduced, leading to better patient compliance
-
e) Impact on patients:
Overall, it was thought that pharmacogenetics would result in:
more time delays for the patient
better patient outcomes
increase in a patient’s confidence in treatment
increase in the number of services available, and value to the patient
-
f) Economic consequences:
The economic consequence of implementing pharmacogenetic testing was an issue addressed by participants. Some pharmacists suggested:
The impact of pharmacogenetics on the profession may be dependent on economic factors such as the cost to the patient, cost to the government and cost/benefit analysis
Pharmacogenetics would lead to an overall reduction in government expenditure and community costs, with consequent improved pharmacoeconomics
Pharmacogenetics would reduce the number of medications taken by patients, which may reduce the income and viability of small community pharmacies
Because pharmacists would need to spend more time counselling patients about pharmacogenetics, staffing levels would need to be increased
Discussion
This study provided novel insights into Victorian pharmacists’ perceptions about pharmacogenetics. Specifically, it explored the perceived level of knowledge regarding pharmacogenetics, how Victorian pharmacists believed pharmacogenetics would impact upon their profession, and the ways in which Victorian pharmacists would like to be educated about pharmacogenetics. These were all areas where literature was lacking.
Pharmacogenetics is a rapidly evolving scientific field, yet the knowledge and experience of pharmacogenetics amongst pharmacists generally, and particularly in Australia, is limited.13,16,24 This study has shown that the perceived level of understanding of pharmacogenetics is poor. This study also suggests that the pharmacists who have more recently graduated from university perceive that they have a more sound understanding of pharmacogenetics compared to those who have been working as pharmacists for longer. While this correlation was not strong due to a limited response rate and the impact of outliers on the data, it was statistically significant. This would suggest that pharmacists who have been practicing for longer require more education on the topic and may need education that is targeted at them specifically. Approximately 25% of respondents had learnt about pharmacogenetics by reading around the topic. Together with the qualitative data gathered, this demonstrates that pharmacists are interested in pharmacogenetics and may embrace education on the topic. However, while self-directed learning demonstrates initiative on behalf of the pharmacists, it may result in differing levels of knowledge and uneven standards of practice amongst pharmacists regarding pharmacogenetics. Therefore, guidelines and competency standards will need to be drafted and implemented to ensure that there is a consistent standard of practice among Australian pharmacists.
As illustrated by the results of this study and the conclusions of many others, pharmacists will need a sound understanding of pharmacogenetics in order to counsel appropriately and provide optimal pharmaceutical care to their patients.2,15,18,22,26,27 Previous studies have recommended that more targeted pharmacogenetics education initiatives be developed.22 The participants in this study generally agreed that this education should be delivered as part of a Bachelor of Pharmacy degree at university. Education directed at pharmacists who are already registered should be delivered via seminars and conferences which contribute to the pharmacist’s continuing education programs. As previously mentioned, education which is specifically tailored to a pharmacist’s experience and level of knowledge may need to be delivered. Therefore, pharmacists who have recently graduated from university may need less education on the scientific principles behind pharmacogenetics and may benefit from more intensive education about different pharmacogenetic tests and the clinical applications of these results. On the other hand, pharmacists who have been practicing for longer may require more education about the key principles behind the science of pharmacogenetics, as well as education about tests and clinical implications of these. As suggested elsewhere, teaching health professionals about the key principles of the science behind pharmacogenetics could help instil an appreciation of the future clinical importance of genomics, so that these pharmacists and doctors could be more motivated to lifelong learning of genetics and how it affects people’s health.23
Patient counselling was cited as one of the most important aspects of a pharmacist’s role which may be impacted upon by pharmacogenetics. However, when asked how well the respondents believed they could counsel a patient about a pharmacogenetic test result, the majority indicated that they would counsel poorly or very poorly. The importance of counselling and the provision of appropriate information to patients about pharmacogenetics have been noted as important aspects in the implementation of pharmacogenetics into healthcare.10 To ensure a suitably high standard of counselling and pharmaceutical care, a thorough education and understanding of pharmacogenetics by clinicians and pharmacists would be required.10
The impact of pharmacogenetics on the pharmacy profession, counselling, medicine use, the patient, education of pharmacists, as well as economic and ethical implications were identified as major themes through thematic analysis of the qualitative data gathered. Generally the respondents were positive about the impact of pharmacogenetics on pharmacy practice and the topics mentioned above. While the potential impact of pharmacogenetics on a pharmacist’s role has been discussed in international studies3,16,18,22,24,26,27, scant research had been conducted in Australia to determine pharmacists’ views on how pharmacogenetics may affect their roles. The views expressed in this study reflect those of overseas studies, namely that pharmacogenetics will impact upon pharmacy in specific ways. These include the potential for increased specialisation of and broadening of the skills base for pharmacy, the requirement for pharmacists to interpret pharmacogenetic test results, the need for increased counselling of patients in defined areas of genetic testing, the optimisation of medication regimes and doses, and the need and capacity to educate other health professionals.2,18,22 Some concerns were noted by pharmacists in this study, and these included the economic ramifications of pharmacogenetics on pharmacy, specifically, whether there would be the need to employ more staff given the greater time required by the pharmacist to counsel on and assess test results. There were suggestions also that the potential for reduced medicine use by patients could negatively affect the viability of some pharmacies. Privacy and ethical issues were noted, including whether pharmacists would have access to a patient’s pharmacogenetic test results or would need to depend on the patient disclosing the results. These concerns were similar to those raised in studies overseas1,2,3,8,13,27, and describe issues that will need to be addressed prior to the implementation of pharmacogenetic testing in Australia to ensure pharmacists are comfortable and positive about their potential new roles.
Conclusions
This study provided novel insights into Victorian pharmacists’ perceptions of pharmacogenetics. It explored the perceptions of these participants regarding their knowledge of pharmacogenetics, how competent they perceived themselves to be in counselling patients about pharmacogenetic testing, how they believed pharmacogenetics would impact upon their profession, and the ways in which pharmacists would prefer to be educated about pharmacogenetics. The survey revealed that very few perceived that they had a good understanding of the concept of pharmacogenetics and the majority of participants indicated that if the need to counsel a patient about the results of a pharmacogenetic test arose, they would counsel poorly. Those pharmacists who had more recently graduated from tertiary studies perceived that they had a greater understanding of pharmacogenetics than those who had been working in the profession for longer. This study demonstrated the need for governing bodies of pharmacy, continuing professional education providers and universities to educate pharmacists and students about this important topic. Seminars and workshops which contribute to the pharmacist’s continuing education were identified as the preferred method of educating registered pharmacists about this topic. Education should include information on the drugs and conditions upon which pharmacogenetics may impact, the types of tests which may be undertaken, clinical implications of pharmacogenetic testing as well as the ways which pharmacogenetics may be incorporated into everyday practice. Guidelines should be introduced which ensure that pharmacists are knowledgeable and competent in counselling patients about pharmacogenetics. Pharmacists’ concerns regarding economic consequences of pharmacogenetic testing, ethical issues and the accessibility of pharmacogenetic results should be investigated further prior to the implementation of pharmacogenetics into pharmacy practice. Finally, this research needs to be extended to include pharmacists from across Australia. Such studies would assist in developing an educational tool that could enable the setting of competency standards for the profession in preparedness for the putative incorporation of pharmacogenetics into the healthcare system and everyday practice.
Acknowledgments
The authors wish to thank Dr. Jon Willis and Dr. Virigina Dickson-Swift for their time and assistance as well as the pharmacists who kindly gave up their time to participate in this study.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Competing interests: There was no conflict of interest for any author during the preparation of this manuscript.
Contributor Information
Teresa McMahon, School of Pharmacy & Applied Science, La Trobe University. Bendigo, Victoria (Australia)..
Joseph Tucci, School of Pharmacy & Applied Science, La Trobe University. Bendigo, Victoria (Australia)..
References
- 1.Cook J, Hunter G, Vernon JA. The Future Costs, Risks and Rewards of Drug Development; The Economics of Pharmacogenomics. Pharmacoeconomics. 2009;27:355–363. doi: 10.2165/00019053-200927050-00001. [DOI] [PubMed] [Google Scholar]
- 2.Clemerson JP, Payne J, Bissell P, Anderson C. Pharmacogenetics, the next challenge for pharmacy? Pharm World Sci. 2006;28:126–130. doi: 10.1007/s11096-006-9029-3. [DOI] [PubMed] [Google Scholar]
- 3.El-Ibiary SY, Cheng C, Alldredge B. Potential roles for pharmacists in pharmacogenetics. J Am Pharm Assoc. 2003;48:21–29. doi: 10.1331/JAPhA.2008.07050. [DOI] [PubMed] [Google Scholar]
- 4.Runciman WB, Roughead EE, Semple SJ, Adams RJ. Adverse drug events and medication errors in Australia. Int J Qual Health Care. 2003;15:149–159. doi: 10.1093/intqhc/mzg085. [DOI] [PubMed] [Google Scholar]
- 5.Nelson MR, Bacanu SA, Mosteller M, Bowman CE, Roses AD, Lai EH, Ehm MG. Genome-wide approaches to identify pharmacogenetic contributions to adverse drug reactions. Pharmacogenomics J. 2009;9:23–33. doi: 10.1038/tpj.2008.4. [DOI] [PubMed] [Google Scholar]
- 6.Shih T. Pharmacogenetics: From bench science to the bedside. Drug Inf J. 2008;42:503–513. [Google Scholar]
- 7.Anderson Jl, Horne BD, Stevens SM, Grove AS, Barton S, Nicholas ZP, Kahn SF, May HT, Samuelson KN, Muhlestein JM, Carlquist JF. Randomized Trial of Genotype-Guided Versus Standard Warfarin Dosing in Patients Initiating Oral Anticoagulation. Circulation. 2007;166:2563–2570. doi: 10.1161/CIRCULATIONAHA.107.737312. [DOI] [PubMed] [Google Scholar]
- 8.Hiratsuka M, Sasaki T, Mizugaki M. Genetic testing for pharmacogenetics and its clinical application in drug therapy. Clinica Chimica Acta. 2006;363:177–186. doi: 10.1016/j.cccn.2005.05.047. [DOI] [PubMed] [Google Scholar]
- 9.Bukaveckas B. Adding Pharmacogenetics to the Clinical Laboratory: Narrow Therapeutic Index Medications as a Place to Start. Arch Pathol Lab Med. 2004;128:1330. doi: 10.5858/2004-128-1330-APTTCL. [DOI] [PubMed] [Google Scholar]
- 10.Haddy CA, Ward HM, Angley MT, McKinnon RA. Consumers' views of pharmacogenetics-A qualitative study. Res Social Adm Pharm. 2010;6:221–231. doi: 10.1016/j.sapharm.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Brien JAE. Pharmacogenetics and the future of clinical pharmacy practice. Pharm J. 2008;38:7. [Google Scholar]
- 12.Flowers CR, Veenstra D. The role of cost-effectiveness analysis in the era of pharmacogenomics. Pharmacoeconomics. 2004;22:481–493. doi: 10.2165/00019053-200422080-00001. [DOI] [PubMed] [Google Scholar]
- 13.Corkindale D, Ward H, McKinnon R. Low adoption of pharmacogenetic testing: an exploration and explanation of the reasons in Australia. Per Med. 2007;4:191–199. doi: 10.2217/17410541.4.2.191. [DOI] [PubMed] [Google Scholar]
- 14.Evans WE, McLeod HE. Pharmacogenomics - Drug disposition, drug targets, and side effects. N Engl J Med. 2003;348:538–549. doi: 10.1056/NEJMra020526. [DOI] [PubMed] [Google Scholar]
- 15.Latif DA, McKay AB. Pharmacogenetics and pharmacogenomics instruction in colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2005;69:152–156. [Google Scholar]
- 16.Shin J, Kayser SR, Langaee TY. Pharmacogenetics: from discovery to patient care. Am J Health Syst Pharm. 66:2009. 625–637. doi: 10.2146/ajhp080170. [DOI] [PubMed] [Google Scholar]
- 17.Venter J. The sequence of the human genome. Science. 2001;291:1304–1351. doi: 10.1126/science.1058040. [DOI] [PubMed] [Google Scholar]
- 18.Clemerson J, Payne K. Pharmacogenetics- Background and future potential. Hosp Pharm. 2008;15:159–164. [Google Scholar]
- 19.US Department of Health & Human Services and Stanford University PharmGKB; Pharmacogenetics Knowledge Base [online] 2010; www.pharmgkb.org/index.jsp (accessed 7thOctober2010).
- 20.U.S. Food and Drug Administration Table of Pharmacogenomic Biomarkers in Drug Labels [online] 2010; http://www.fda.gov.htm (accessed 7thOctober2010).
- 21.National Institute of General Medical Sciences From genes to personalised medicines [online] 2010; www.nigms.nih.gov/Initiatives/PGRN/Background/FactSheet.htm (accessed 7thOctober2010).
- 22.Newton R. How will pharmacogenetics impact on pharmacy practice? Pharmacists' views and educational priorities. Birmingham: NHS National Genetics Education and Development Centre; 2007. [Google Scholar]
- 23.Guttmacher AE, Porteous ME, McInernay JD. Educating health-care professionals about genetics and genomics. Nat Rev Genet. 2007;8:151–157. doi: 10.1038/nrg2007. [DOI] [PubMed] [Google Scholar]
- 24.Sansgiry SS, Kulkarni AS. The human genome project: Assessing confidence in knowledge and training requirements for community pharmacists. J Manag Care Pharm. 2002;8:525. doi: 10.18553/jmcp.2002.8.6.525. [DOI] [PubMed] [Google Scholar]
- 25.Liamputtong P, editor. Research methods in health : foundations for evidence-based practice. South Melbourne: Oxford University Press; 2010. [Google Scholar]
- 26.Shin J, Kayser SR. Clinical pharmacy consultation for pharmacogenetic testing. Per Med. 2009;6:183–192. doi: 10.2217/17410541.6.2.183. [DOI] [PubMed] [Google Scholar]
- 27.Brock TP, Valgus JM, Smith SR, Summers KM. Pharmacogenomics: implications and considerations for pharmacists. Pharmacogenomics. 2003;4:321–330. doi: 10.1517/phgs.4.3.321.22698. [DOI] [PubMed] [Google Scholar]


