SUMMARY
The retromolar trigone is a challenging transoral surgical site due to the difficulty of visualization. Our aim is to report a new technique of transoral robotic resection of retromolar trigone tumours. We present three patients with retromolar trigone tumours with pathological diagnosis of squamous cell carcinoma who underwent successful transoral robotic resection. Robotic retromolar trigone resection and concurrent supraomohyoid neck dissections were performed in all patients without any complication. In conclusion, transoral robotic surgery is a safe and feasible technique for resection of malignant retromolar trigone tumours with minimal complications and favourable outcomes.
KEY WORDS: Retromolar trigone, TORS, Transoral robotic surgery, Oral cavity
RIASSUNTO
Le difficoltà riscontrate nella corretta esposizione del campo operatorio rendono impegnativo l'approccio transorale al trigono retromolare. Con il presente lavoro é nostra intenzione descrivere un approccio innovativo alla resezione dei tumori interessanti il trigono retromolare, mediante chirurgia robotica transorale. Presenteremo tre casi nei quali pazienti con diagnosi di tumore del trigono retromolare ad istologia squamocellulare, sono stati sottoposti con successo ad una resezione della lesione con metodica robotica transorale. In tutti i pazienti sono stati effettuati simultaneamente, e senza registrare alcuna complicanza, sia la resezione del trigono retromolare mediante chirurgia robotica, che lo svuotamento latero cervicale sovraomoioideo. In conclusione la chirurgia robotica transorale, applicata alla resezione dei tumori maligni del trigono retromolare, é una tecnica sicura, che offre un outcome favorevole con complicanze minime.
Introduction
The retromolar trigone (RMT) is the portion of the oral cavity mucosa overlying the ascending ramus of the mandible at the junction of two dental arcades behind the last molar. This region can be a challenging transoral surgical site due to the difficulty of visualization. Cancers originating in the RMT, although rare, are usually squamous cell carcinoma (SCC). On occasion minor salivary gland tumours can also originate from RMT 1-3. The presence of bone invasion leads to poor prognosis. Sequential therapy starting with surgery is the recommended treatment 4 5. Transoral robotic surgery (TORS) has been reported to be safe and feasible in transoral resection of laryngopharyngeal tumours 6-8. However, there has been no report related to transoral robotic RMT resection (TORRR). This report presents a new technique of TORS for RMT cancer resection.
Case series
Description of clinical cases
Case 1: a 63-year-old Caucasian male presented to a dental clinic with a persistent RMT lesion after dental extraction three months ago. He denied any symptoms other than mild left posterior oral pain. Otolaryngologic exam showed a 2.5 cm ulcerative, erythematous and granular lesion at the left retromolar trigone. Biopsy revealed SCC. He was a heavy smoker and alcohol consumer. The patient was evaluated with CT of the neck to exclude possible mandibular invasion.
Final pathologic staging after TORRR demonstrated a T1N1 RMT carcinoma with perineural and lymphovascular invasion with negative surgical resection margins. He has completed adjuvant radiotherapy and is disease free at 15 months clinical follow-up.
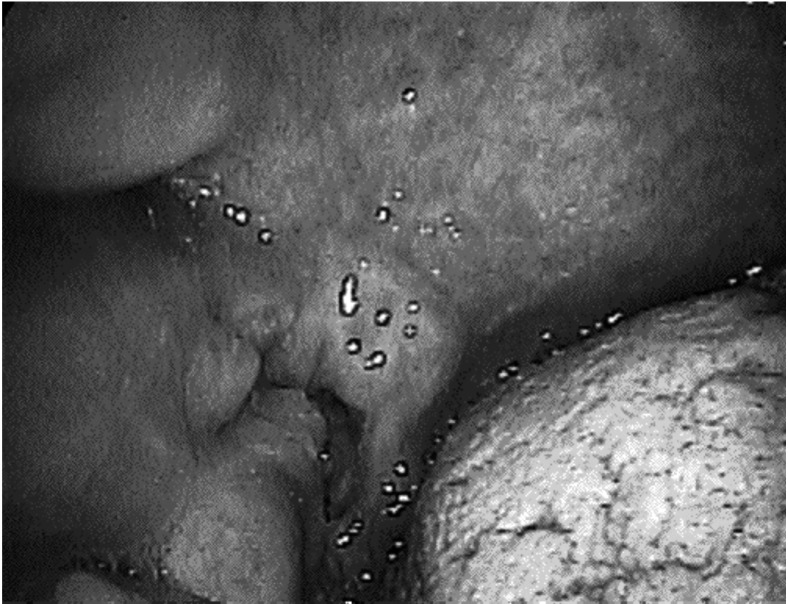
Case 2: a 57-year-old Caucasian male presented to his dentist with a right-sided oral cavity mass. Food occasionally got stuck in this region, but he denied pain, bleeding, or a neck mass. Subsequent biopsy of the 2 cm granular lesion of the right RMT involving the anterior tonsillar pillar showed SCC (Fig. 1). He was also a heavy smoker and drinker. There was no radiological evidence of mandibular invasion in CT of the neck.
Fig. 1.
Clinical picture showing a right RMT carcinoma.
Final pathologic staging confirmed a T1N0 carcinoma with negative surgical margins. He did not need any adjuvant treatment and is disease free at 16 months follow-up.
Case 3: an 80-year-old male with history of larynx cancer and previous radiation treatment presented with right sided globus sensation and intermittent pain for 6 weeks. He denied dysphagia, odynophagia or a neck mass. He was a heavy smoker and previous drinker. Physical examination showed a 3 cm ulcerative mobile lesion at the right RMT. Biopsy of the lesion showed SCC. Radiological evaluation with neck CT excluded any mandibular invasion.
The patient underwent transoral robotic surgery and concurrent bilateral neck dissection. Final pathological staging confirmed T2N2b carcinoma with lymphovascular and perineural invasion. Surgical margins were negative. The patient was disease free at 1 month follow-up. All three RMT carcinoma cases were HPV negative.
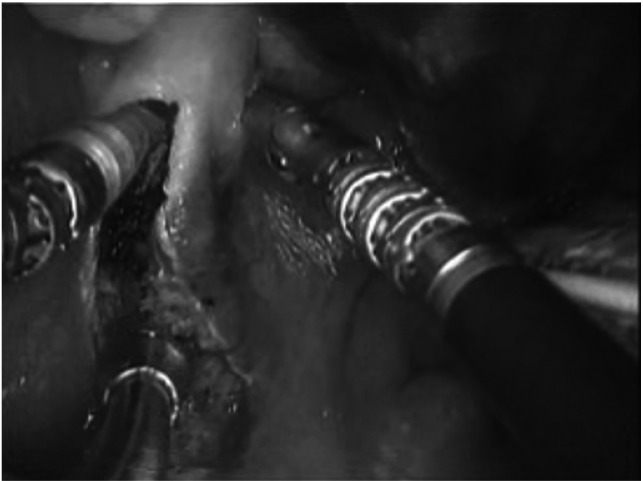
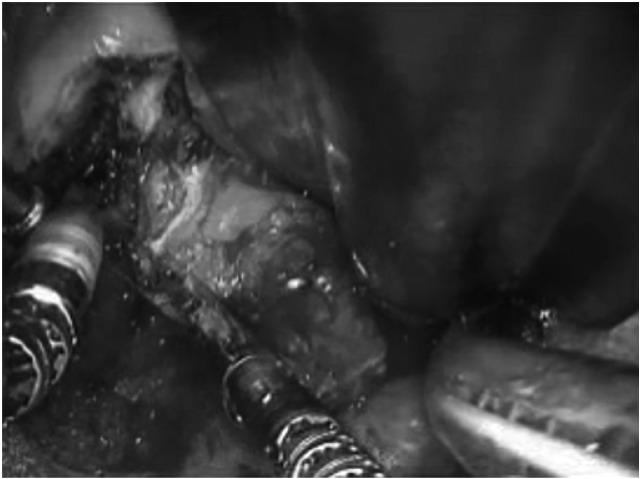
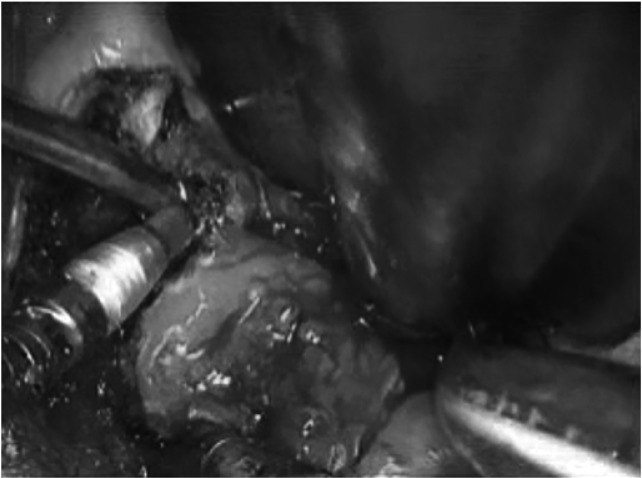
Surgical technique and results
Similar surgical steps were followed for all TORRR procedures. Robotic retromolar trigone resection and concurrent selective neck dissections (Levels I-IV) were performed. Standard TORS room setting was used in the surgery. After the transoral intubation a Crowe-Davis mouth gag was placed to expose RMT region (Fig. 2). A straight (0°) robotic camera provided optimal exposure without necessitating the 30° camera. 5 mm monopolar cautery and Maryland dissectors were used for resection (Figs. 3, 4). Mucosa and submucosa were incised deep to mandibular periosteum. The resection plane was reached and resection extended up to anterior tonsillar pillar medial to the mandibular bone. Superficial layer of tongue base muscles and the lingual nerve formed the deep margin of excision. A non-robotic marginal mandibulectomy was needed to get a safe margin for the second case only. Exposed mandibular bone after tumour removal was reconstructed and covered with local mucosal advancement flaps.
Fig. 2.
Transoral robotic resection of the left RMT carcinoma; just after the start of the incision.
Fig. 3.
Transoral robotic resection of the left RMT carcinoma; in progress.
Fig. 4.
Transoral robotic resection of the left RMT carcinoma; excision is complete, and the specimen is free.
The average robotic setup time was 20 min, TORRR time was 7 min, with estimated blood loss of 20 ml for these robotic RMT resections.
Discussion
Exposure and resection of RMT carcinoma is a challenge especially when it involves the posterior floor of the mouth, base of tongue, or pharynx. Traditional surgical approaches to the RMT region are transoral surgery with or without laser for early stage and open transfacial/transcervical approaches for advanced stage disease. Minimally- invasive procedures with minimal collateral tissue damage are preferred to decrease surgical morbidity, postoperative complications and improve quality of life together with a shorter hospital stay 1-3.
Robotic assisted surgeries have been popularized more in other surgical fields like gynaecology, urology and cardiac surgery before it was used in the head and neck area in the last four to five years 4. Compared to conventional surgical techniques, a robotic transoral approach offers potential advantages. The primary advantage of this approach is decreased surgical morbidity for patients 5. Robotic optics gives magnified three-dimensional visualization with the option of angled camera. Tissue dissection with TORS avoids external incision while respecting the uninvolved tissues that would otherwise be involved in open surgical approaches.
TORS is shown to be feasible and safe procedure with minimal complications and blood loss 6-8. Advantages of TORS over transoral laser surgery include wide, angled and more comprehensive visualization of the surgical field and significantly shorter operative time. Robotic RMT resections take only 7 min to complete. The only disadvantage of the current robotic tools is the need of a bone resecting robotic arm in the event of bone invasion.
Conclusions
TORRR is a feasible, safe and effective procedure with minimal complications and favourable outcomes for the resection of benign and malignant tumours of the RMT. This procedure may be useful in patients where optimal visualization of the RMT lesion is not possible with the naked eye or a straight microscopic view.
References
- 1.Ayad T, Gélinas M, Guertin L, et al. Retromolar trigone carcinoma treated by primary radiation therapy: an alternative to the primary surgical approach. Arch Otolaryngol Head Neck Surg. 2005;131:576–582. doi: 10.1001/archotol.131.7.576. [DOI] [PubMed] [Google Scholar]
- 2.Hao SP, Tsang NM, Chang KP, et al. Treatment of squamous cell carcinoma of the retromolar trigone. Laryngoscope. 2006;116:916–920. doi: 10.1097/01.mlg.0000214900.07495.39. [DOI] [PubMed] [Google Scholar]
- 3.Huang CJ, Chao KS, Tsai J, et al. Cancer of retromolar trigone: long-term radiation therapy outcome. Head Neck. 2001;23:758–763. doi: 10.1002/hed.1108. [DOI] [PubMed] [Google Scholar]
- 4.Dallan I, Castelnuovo P, Vicini C, et al. The natural evolution of endoscopic approaches in skull base surgery: robotic assisted surgery? Acta Otorhinolaryngol Ital. 2011;31:390–394. [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein GS, O'Malley BW, Jr, Snyder W, et al. Transoral robotic surgery: radical tonsillectomy. Arch Otolaryngol Head Neck Surg. 2007;133:1220–1226. doi: 10.1001/archotol.133.12.1220. [DOI] [PubMed] [Google Scholar]
- 6.Hurtuk A, Teknos T, Ozer E. Robotic-assisted lingual tonsillectomy. Laryngoscope. 2011;121:1480–1482. doi: 10.1002/lary.21767. [DOI] [PubMed] [Google Scholar]
- 7.Mercante G, Ruscito P, Pellini R, et al. Transoral Robotic Surgery (TORS) for tongue base tumors. Acta Otorhinolaryngol Ital. 2013;33:230–235. [PMC free article] [PubMed] [Google Scholar]
- 8.Pellini R, Mercante G, Ruscito P, et al. Ectopic lingual goiter treated by transoral robotic surgery. Acta Otorhinolaryngol Ital. 2013;33:343–346. [PMC free article] [PubMed] [Google Scholar]