SUMMARY
Benign tumours account for approximately 60-80% of parotid neoplasms and among these, Warthin's tumour is the second most common benign neoplasm accounting for approximately 15% of all parotid epithelial tumours. The medical records of 100 consecutive patients with Warthin's tumour of the parotid gland admitted for treatment at the Department of Head and Neck Surgery and Otorhinolaryngology, Hospital A.C. Camargo, São Paulo, Brazil, between 1983 and 2011 were retrospectively analyzed. The surgical procedures included 104 (96%) subtotal parotidectomies and 4 (3.7%) total parotidectomies. One hundred and eight parotidectomies were performed in 100 patients with Warthin's tumour. Postoperative complications occurred in 67 (62.3%) of surgical procedures, and facial nerve dysfunction was the most frequent complication, occurring in 51 of 108 surgeries (47.2%). The marginal mandibular branch of the facial nerve was affected in 46 of the 48 cases (95.8%) of facial nerve dysfunction. Frey's syndrome was diagnosed in the late postoperative period in 19 patients (17.6%). We conclude that either superficial or total parotidectomy with preservation of facial nerve are the treatment of choice for Warthin's tumour with no case of recurrence seen after long-term follow-up. Facial nerve dysfunction and Frey's syndrome were the main complications associated with this surgery. Thus, if on one hand total parotidectomy is an appropriate radical resection of parotid parenchyma reducing, in theory, the risk of recurrence, on the other hand superficial parotidectomy is also a radical and efficient method with lower morbidity in terms of facial nerve dysfunction and Frey's syndrome.
KEY WORDS: Warthin's tumour, Treatment, Complications, Recurrence, Parotid, Parotid tumours
RIASSUNTO
Le neoplasie benigne rappresentano circa il 60-80% dei tumori della ghiandola parotide e fra questi, il tumore di Warthin è il secondo istotipo più frequente con una prevalenza del15% circa dei tumori epiteliali della parotide. Abbiamo analizzato retrospettivamente le cartelle cliniche di 100 pazienti affetti da tumore di Warthin trattati fra il 1983 e il 2011 presso il dipartimento di chirurgia della testa e del collo dell'ospedale di San Paolo "A.C. Camargo" (Brasile). Nei 100 pazienti analizzati furono effettuate 108 parotidectomie di cui 104 parotidectomia subtotale (96%), e 4 parotidectomia totali (3,7%). Complicanze post operatorie si sono verificate nel 62,3% delle procedure chirurgiche e in particolare la disfunzione del nervo facciale fu la più frequentemente osservata (51/108 procedure effettuate – 47,2%). Una disfunzione del ramo marginalis mandibulae del nervo facciale eè stata riscontrata in 46 dei 48 casi (95,8%) con disfunzione del facciale. La sindrome di Frey's fu riscontrata invece tardivamente in 19 pazienti (17,6% dei casi). Nella nostra casistica anche ad un follow-up a lungo termine non sono state apprezzate recidive di tumori di Warthin dopo parotidectomia esofacciale o totale con preservazione del nervo facciale. La disfunzione del nervo facciale e la sindrome di Frey erano le principali complicanze osservate dopo la chirurgia. Benché la parotidectomia totale rappresenti l'approccio chirurgico più radicale i nostri dati dimostrano che la parotidectomia superficiale non solo consente di ottenere una buona radicalità chirurgica ma allo stesso tempo si associa ad una bassa moribidità in termini di disfunzione del nervo facciale e sindorme di Frey.
Introduction
Benign tumours account for approximately 60-80% of parotid neoplasms and comprise a heterogeneous group with distinct clinical and histological features and biological behaviour 1. Among these, Warthin's tumour, also known as adenolymphoma or papillary lymphomatous cystadenoma, is the second most common benign neoplasm and accounts for approximately 15% of parotid epithelial tumours 2-4.
Warthin's tumour is most common in male patients (4:1 male:female ratio) during the sixth and seventh decades of life 5. Unlike other benign neoplasms of the salivary glands, this tumour has a tendency towards bilateral involvement, and approximately 90% of lesions occur in the superficial lobe of the parotid gland 6. Histologically, the tumour has an oncocytic epithelial component forming uniform rows of cells surrounded by cystic spaces associated with a lymphoid stroma often showing the presence of germinal centres (Figs. 1, 2) 7. Treatment consists of partial, subtotal or total parotidectomy with preservation of the facial nerve 8. Malignant transformation is described in only 0.1% of cases, and usually arises in the epithelial component of the lymphoid tissue tumour 9. The incidence of recurrence after surgical treatment is extremely rare 5.
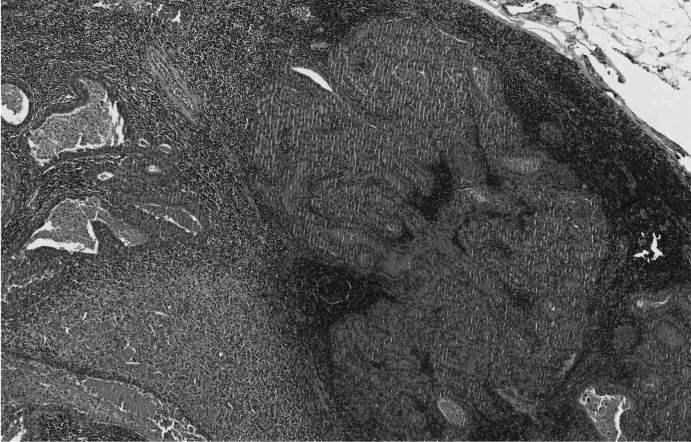
Fig. 1.
Histological section stained with HE with 40x magnification, showing the interface between the salivary gland and the tumor.
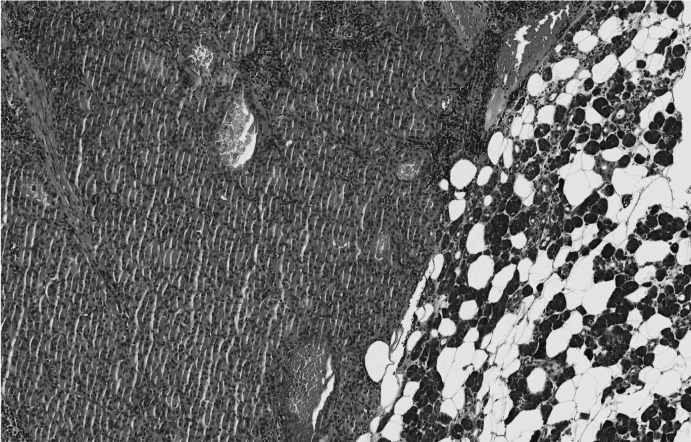
Fig. 2.
Histological section stained with HE with 40x magnification, demonstrating the neoplasm characterized by cystic and solid areas, cells with abundant granular and eosinophilic cytoplasm with central nuclei. The stroma is rich in lymphocytes.
The aim of this study is to describe the outcomes of patients with Warthin's tumour of the parotid gland considering clinical and demographic characteristics, type of surgery, complications and the incidence of recurrence.
Patients and methods
The medical records of 100 consecutive patients with Warthin's tumour of the parotid gland admitted for treatment at the Department of Head and Neck Surgery and Otorhinolaryngology, Hospital "A.C. Camargo", São Paulo, Brazil, between 1983 and 2011 were retrospectively analyzed. One hundred and thirteen tumours were diagnosed in 100 patients with a median age of 58 years (range 32-84 years). There were 72 males and 28 females. Of these, 75 patients (75%) were Caucasian. Tobacco use was reported at diagnosis by 72 patients and 11 reported a previous history of smoking. Four patients had bilateral synchronous tumours and 9 had bilateral metachronous tumours. The treatment employed was surgery in all cases. The surgeries were performed by several surgeons from the same department, mostly residents directly supervised by specialists in head and neck surgery. The surgical procedures included 104 (96%) subtotal/superficial parotidectomies, defined by the resection of tumours located in the superficial portion of the gland (above the nerve) and 4 (3.7%) total parotidectomies, indicated for those tumours located in the deep lobe of gland. The facial nerve was identified and preserved in all cases. In three of the four patients with bilateral synchronous tumours, surgery was performed only on the side where the tumour was larger. Otherwise, in 9 patients with metachronous bilateral tumours, contralateral parotidectomy was performed in 7 cases. All eight contralateral parotidectiomies in patients with bilateral tumours were performed at different times. In five patients with bilateral tumours, the second side was not operated because of patient refusal or for clinical reasons (small tumours and few symptoms).
Routinely, the facial nerve trunk is identified before making the identification and dissection of its branches. No devices were used to identify the nerve in primary surgeries. In two patients, the mandibular branch of facial nerve was sacrificed because of reported tumour involvement, and these cases were not included in the analysis of postoperative nerve dysfunction. Rotation of sternocleidomastoid muscle flap (SMF) was performed in the last 10 years to fill the parotid bed after resection and to reduce the incidence of Frey's syndrome. The type of drain used varied during the study period. The Penrose drains that were originally used were replaced in 1994 by vacuum drainage Hemovac (Portovac), and in the last decade we have used silicone drains (Jackson-Pratt and Blake) to facilitate postoperative care and allow early hospital discharge.
SPSS 17.0 was used for statistical analysis. The association between variables with the occurrence of complications was evaluated by chi-square or Fisher's exact test, as appropriate. The Mann-Whitney test was used to evaluate the difference between the mean length of hospitalization. A p value < 0.05 was considered statistically significant.
Results
One hundred and eight parotidectomies were performed in 100 patients with Warthin's tumour. The time of hospitalization varied from 1 to 19 days (median, 2 days). Postoperative complications occurred in 67 (62.3%) surgical procedures, and facial nerve dysfunction was the most frequent complication, followed by other less frequent complications such as seroma and infection (Table I). There was no total facial nerve dysfunction or postoperative mortality. The mean and median days of hospitalization between the patients who did or did not have postoperative complications were similar and not statistically different. Similarly, the incidence of postoperative complications did not show statistically significant correlation with gender, age, smoking and alcohol, type of parotidectomy, nodule size and use of the sternocleidomastoid muscle flap.
Table I.
Complications in 108 parotidectomies for Warthin's tumour.
| Complication | n | % |
|---|---|---|
| Number* | 44 | 40.7 |
| Facial nerve dysfunction | 51 | 47.2 |
| Infection | 10 | 9.2 |
| Seroma | 2 | 0.9 |
| Haematoma | 2 | 0.9 |
| Fistula | 2 | 0.9 |
Some patients had more than one complication.
Postoperative facial nerve dysfunction occurred in 51 of 108 surgeries (47.2%) (Table I). In 43 cases (84.3%), dysfunction was transitory with recovery of function occurring in a period ranging from 1 to 19 months (median, 4 months). Unfortunately, in eight cases there was no detailed report in the clinical chart regarding recovery from facial mobility. The marginal mandibular branch of the facial nerve was affected in 46 of the 49 cases (93.8%). Six cases (12.2%) had dysfunction of other associated branches. Only one patient had postoperative dysfunction of all branches of the facial nerve.
Seroma and haematoma were found in 2 of 108 (1.9%) procedures. All were treated conservatively with aspiration. Wound infection was observed in 10 of 108 (9.2%) procedures. There was no statistically significant correlation with the incidence of wound infection and the type of drain used. Two cases of fistula occurred.
Frey's syndrome was diagnosed in the late postoperative period in 19 patients (17.6%) (Table II). There were no reports of bilateral Frey's syndrome in patients with surgery on both sides. Frey's syndrome occurred less frequently in patients who underwent rotation of the sternocleidomastoid muscle flap (SMF) to fill the parotidectomy field (10 of 67; 14.9%) compared with cases that did not undergo flap reconstruction (9 of 41; 22%), but this difference was not statistically significant.
Table II.
Incidence of Frey's Syndrome.
| Frey's Syndrome | |||
|---|---|---|---|
| No | Yes | ||
| Parotidectomy | Partial | 78 | 19 |
| Total | 4 | 0 | |
| SMF | No | 21 | 9 |
| Yes | 59 | 10 | |
| Follow-up | Min | 6 m | |
| Max | 20 y | ||
| Mean | 4.13 y | ||
| Median | 2 y | ||
SMF: sternocleidomastoid muscle flap; m: month; y: years.
Discussion
Warthin's tumour is a benign neoplasm, first described by Aldred Warthin in 1929, which occurs predominantly in the parotid gland and represents approximately 15% of parotid tumours 5 9. Fewer than 10% of cases occur outside this gland 5. Furthermore, bilateralism is described in 5-15% of cases and multifocality in 6-20% 9-12. In our series, we studied only tumours of the parotid gland, and bilateral Warthin's tumours were observed in 13 (13%) patients, (4 synchronous cases and 9 metachronous cases). Although the occurrence of bilateral Warthin's tumour is relatively common in this group of patients, the presence of a bilateral synchronic tumour is rare 11-14.
The origin of Warthin's tumour is unknown and its classification as cancer is controversal 15 16. Surgery is the main mode of therapy used and is associated with a low recurrence rate 15. Several authors have correlated recurrence rate with the extent of surgery, which ranges from 0-13% 5 11 17. In our study, superficial parotidectomy with facial nerve preservation was used in 97% of cases, and there were no cases of recurrence after a median followup of 31 months. Although superficial parotidectomy is the treatment of choice for patients with benign tumours of the parotid gland, it is associated with both early and late complications 18 19.
The main complications associated with surgery of the parotid gland are facial nerve dysfunction and Frey's syndrome. Postoperative dysfunction of the facial nerve may be total or partial (some branches), and transient or permanent 20 21. On the other hand, Frey's syndrome is detected later, may be symptomatic or asymptomatic and its diagnosis is performed with the Minor test that is based on application of a solution containing 1.5 g of iodine, 10 g of castor oil and 88.5 g of absolute alcohol that must be applied to the skin of the parotid region. After drying, starch powder should be applied, which together with local sweating, will produce a blue iodine-starch reaction 22 23.
In the literature, the incidence of transient dysfunction of the facial nerve has been reported in 10-68% of cases, while permanent dysfunction occurs in 0-19% 20 24. In our series, the incidence of postoperative dysfunction of facial nerve was 47.2%. The marginal mandibular branch was the most affected with 90% of cases of nerve dysfunction, although total dysfunction (all branches) was detected in only 1 patient. Classification regarding the degree of facial nerve dysfunction could not be done since this was a retrospective study, and this data was not evaluated in most cases.
Dysfunction of the marginal mandibular branch is a major problem and has been reported in 48-59% of cases in the literature 21 25. Several factors have been described to be associated with an increased incidence of postoperative dysfunction of the facial nerve after parotidectomy 26. Yuan, in 2009, studied 626 patients undergoing surgery for benign disease of the parotid and found that the factors associated with increased postoperative dysfunction of the facial nerve were the extent of parotidectomy and diabetes mellitus 21. Similarly, Koch in 2010 observed facial nerve dysfunction in 32.7% of cases, and the main factor was the extent of surgery 19. In another study of 162 patients who underwent parotidectomy for benign disease, the presence of facial nerve dysfunction was observed in 40% of cases. In this study, the presence of inflammation and parotidectomy for Warthin's tumour were the factors that were most relevant to dysfunction 27. In our study, there were no factors that significantly correlated with postoperative dysfunction of the facial nerve.
Frey's syndrome has been described as a main complication related to surgery of the parotid gland. The incidence of this syndrome varies widely according to the diagnostic investigation. It is reported spontaneously for about 10% of patients, but when questioned actively about the existence of gustatory sweating, approximately 30-40% of patients report the presence of such symptoms. Moreover, when under diagnostic investigation, Frey's syndrome is seen in up to 95% of patients undergoing parotidectomy 23. In our study, the diagnosis of Frey's syndrome was made based on spontaneously clinical complaints of the patient or after being questioned by the attending physician about symptoms during follow-up, and was seen in 17.6% of patients. This occurred more often in patients in whom a SMF was not used to fill the parotid space (22% vs. 14.9%). However, this difference was not statistically significant. When symptomatic, Frey's syndrome was treated with botulinum toxin injection in the most severe cases, and by applying deodorants or antiperspirants in milder cases. Queiroz Filho, in 2004, studied the occurrence of Frey's syndrome in 2 groups of patients according to the presence or absence of SMF and found that 47.4% (9/19) of patients in the group who did not receive the flap had complaints of gustatory sweating, and in 36.8% (7/12) of patients the Minor test was positive. Otherwise, in the group that received the flap, complaints or a positive test for Minor were not found 28. In a systematic literature review, Sanabria concluded that there is not sufficient clinical evidence to determine that the use of SMF in preventing Frey's syndrome is an effective procedure in preventing Frey's syndrome 29.
We conclude that either superficial or total parotidectomy with preservation of the facial nerve are the preferred treatments for Warthin's tumour with no case of tumour recurrence seen during long-term follow-up. Facial nerve dysfunction and Frey's syndrome were the main complications associated with this surgery. Thus, if in one hand, total parotidectomy is an appropriate radical resection of parotid parenchyma reducing, in theory, the risk of recurrence, on the other superficial parotidectomy is also a radical and efficient method with low morbidity in terms of facial nerve dysfunction and Frey's syndrome. Currently, resections such as those of the lower extremity of the superficial pole of parotid should not be ruled out, as they can be performed safely in lower tumours, allowing lower manipulation of cranial branches of the facial nerve with less morbidity. However, further prospective and randomized studies are needed to reach a more definitive conclusion.
References
- 1.Freedman LS, Oberman B, Sadetzki S. Using time-dependent covariate analysis to elucidate the relation of smoking history to Warthin's tumor risk. Am J Epidemiol. 2009;170:1178–1185. doi: 10.1093/aje/kwp244. [DOI] [PubMed] [Google Scholar]
- 2.Bussu F, Parrilla C, Rizzo D, et al. Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngol Ital. 2011;31:135–143. [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes L, Eveson JW, Reichart P, et al. World Health Organization classification of tumors. Lyon: IARC Press; 2005. Pathology and genetics, head and neck tumours; pp. 209–281. [Google Scholar]
- 4.Neville BW, Damm DD, Allen CM, et al. Oral and Maxillofacial Pathology. 3rd ed. Vol. 11. St. Louis, MO: Saunders Elsevier; 2009. Salivary Gland Pathology; pp. 461–462. [Google Scholar]
- 5.Yoo GH, Eisele DW, Askin FB, et al. Warthin's tumor: a 40-year experience at The Johns Hopkins Hospital. Laryngoscope. 1994;104:799–803. doi: 10.1288/00005537-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Thangarajah T, Reddy VM, Castellanos-Arango F, et al. Current controversies in the management of Warthin tumour. Postgrad Med J. 2009;85:3–8. doi: 10.1136/pgmj.2008.071282. [DOI] [PubMed] [Google Scholar]
- 7.Piccioni LO, Fabiano B, Gemma M, et al. Fine-needle aspiration cytology in the diagnosis of parotid lesions. Acta Otorhinolaryngol Ital. 2011;31:1–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Bussu F, Parrilla C, Rizzo D, et al. Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngol Ital. 2011;31:135–143. [PMC free article] [PubMed] [Google Scholar]
- 9.Faur A, Lazfér E, Cornianu M, et al. Warthin tumor: a curious entity – case reports and review of literature. Rom J Morphol Embryol. 2009;50:269–273. [PubMed] [Google Scholar]
- 10.Maiorano E, Lo Muzio L, Favia G, et al. Warthin's tumour: a study of 78 cases with emphasis on bilaterality, multifocality and association with other malignancies. Oral Oncol. 2002;38:35–40. doi: 10.1016/s1368-8375(01)00019-7. [DOI] [PubMed] [Google Scholar]
- 11.Guntinas-Lichius O, Gabriel B, Klussmann JP. Risk of facial palsy and severe Frey's syndrome after conservative parotidectomy for benign disease: analysis of 610 operations. Acta Otolaryngol. 2006;126:1104–1109. doi: 10.1080/00016480600672618. [DOI] [PubMed] [Google Scholar]
- 12.Teymoortash A, Krasnewicz Y, Werner JA. Clinical features of cystadenolymphoma (Warthin's tumor) of the parotid gland: a retrospective comparative study of 96 cases. Oral Oncol. 2006;42:569–573. doi: 10.1016/j.oraloncology.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 13.Favia GF, Pratelli D, Bux M, et al. Bilateral adenolymphoma (Warthin's tumor) of the parotid. The anatomicoclinical, diagnostic and therapeutic aspects of 2 cases. Italian. Minerva Stomatol. 1994;43:535–542. Review. [PubMed] [Google Scholar]
- 14.Ascani G, Pieramici T, Rubini C, et al. Synchronous bilateral Warthin's tumours of the parotid glands: a case report. Acta Otorhinolaryngol Ital. 2010;30:310–312. [PMC free article] [PubMed] [Google Scholar]
- 15.Baj A, Beltramini GA, Demarchi M, et al. Bilateral SMAS rhytidectomy in parotid recurrent pleomorphic adenoma. Acta Otorhinolaryngol Ital. 2011;31:256–258. [PMC free article] [PubMed] [Google Scholar]
- 16.Arida M, Barnes EL, Hunt JL. Molecular assessment of allelic loss in Warthin tumors. Mod Pathol. 2005;18:964–968. doi: 10.1038/modpathol.3800379. [DOI] [PubMed] [Google Scholar]
- 17.García Purrinõs FJ. Thirteen years' experience with superficial partial parotidectomy as treatment for benign parotid tumours. Acta Otorrinolaringol Esp. 2011;62:10–13. doi: 10.1016/j.otorri.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Rigante M, Visocchi M, Petrone G, et al. Synovial sarcoma of the parotid gland: a case report and review of the literature. Acta Otorhinolaryngol Ital. 2011;31:43–46. [PMC free article] [PubMed] [Google Scholar]
- 19.Koch M, Zenk J, Iro H. Long-term results of morbidity after parotid gland surgery in benign disease. Laryngoscope. 2010;120:724–730. doi: 10.1002/lary.20822. [DOI] [PubMed] [Google Scholar]
- 20.Upton DC, McNamar JP, Connor NP, et al. Parotidectomy: ten-year review of 237 cases at a single institution. Otolaryngol Head Neck Surg. 2007;136:788–792. doi: 10.1016/j.otohns.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 21.Yuan X, Gao Z, Jiang H, et al. Predictors of facial palsy after surgery for benign parotid disease: multivariate analysis of 626 operations. Head Neck. 2009;31:1588–1592. doi: 10.1002/hed.21134. [DOI] [PubMed] [Google Scholar]
- 22.Govindaraj S, Cohen M, Genden EM, et al. The use of acellular dermis in the prevention of Frey's syndrome. Laryngoscope. 2001;111(11 Pt 1):1993–1998. doi: 10.1097/00005537-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Bree R, Waal I, Leemans CR. Management of Frey syndrome. Head Neck. 2007;29:773–778. doi: 10.1002/hed.20568. Review. [DOI] [PubMed] [Google Scholar]
- 24.Bron LP, O'Brien CJ. Facial nerve function after parotidectomy. Arch Otolaryngol Head Neck Surg. 1997;123:1091–1096. doi: 10.1001/archotol.1997.01900100065009. [DOI] [PubMed] [Google Scholar]
- 25.Gaillard C, Peries S, Susini B, et al. Facial nerve dysfunction after parotidectomy: the role of local factors. Laryngoscope. 2005;115:287–291. doi: 10.1097/01.mlg.0000154735.61775.cd. [DOI] [PubMed] [Google Scholar]
- 26.Eisele DW, Wang SJ, Orloff LA. Electrophysiologic facial nerve monitoring during parotidectomy. Head Neck. 2010;32:399–405. doi: 10.1002/hed.21190. [DOI] [PubMed] [Google Scholar]
- 27.Nouraei SA, Ismail Y, Ferguson MS, et al. Analysis of complications following surgical treatment of benign parotid disease. ANZ J Surg. 2008;78:134–138. doi: 10.1111/j.1445-2197.2007.04388.x. [DOI] [PubMed] [Google Scholar]
- 28.Filho WQ, Dedivitis RA, Rapoport A, et al. Sternocleidomastoid muscle flap preventing Frey syndrome following parotidectomy. World J Surg. 2004;28:361–364. doi: 10.1007/s00268-003-7304-1. [DOI] [PubMed] [Google Scholar]
- 29.Sanabria A, Kowalski LP, Bradley PJ, et al. Sternocleidomastoid muscle flap in preventing Frey's syndrome after parotidectomy: A systematic review. Head Neck. 2012;34:589–598. doi: 10.1002/hed.21722. [DOI] [PubMed] [Google Scholar]