Abstract
Background
Physical therapy is commonly prescribed for patients with lumbar spinal stenosis (LSS); however, little is known about its effectiveness.
Purpose
The purpose of this study was to systematically review randomized controlled trials (RCTs), controlled trials, and cohort studies evaluating the effectiveness of physical therapy for LSS.
Data Sources
Studies were searched on electronic databases to January 2012.
Study Selection
Inclusion criteria were: clinical diagnosis of LSS with confirmatory imaging, evaluation of physical therapy treatment, presence of a comparison group, and outcomes of pain, disability, function, or quality of life.
Data Extraction
Outcomes were extracted and, when possible, pooled using RevMan 5, a freely available review program from the Cochrane Library.
Data Synthesis
Ten studies were included: 5 RCTs, 2 controlled trials, 2 mixed-design studies, and 1 longitudinal cohort study. Pooled effects of 2 studies revealed that the addition of a physical therapy modality to exercise had no statistically significant effect on outcome. Pooled effects results of RCTs evaluating surgery versus physical therapy demonstrated that surgery was better than physical therapy for pain and disability at long term (2 years) only. Other results suggested that exercise is significantly better than no exercise, that cycling and body-weight–supported treadmill walking have similar effects, and that corsets are better than no corsets.
Limitations
The limitations of this review include the low quality and small number of studies, as well as the heterogeneity in outcomes and treatments.
Conclusions
No conclusions could be drawn from the review regarding which physical therapy treatment is superior for LSS. There was low-quality evidence suggesting that modalities have no additional effect to exercise and that surgery leads to better long-term (2 years) outcomes for pain and disability, but not walking distance, than physical therapy in patients with LSS.
Lumbar spinal stenosis (LSS) is a condition in which narrowing of the central spinal canal, lateral recess, or foramen leads to compression of the neural and vascular structures, resulting in back and leg pain, disability (particularly decreased walking capacity), and substantially diminished health-related quality of life.1–7 Although the prevalence of LSS is unknown, there has been a steady, dramatic rise in spine surgery rates over recent decades,8–10 with spinal stenosis being the most common diagnosis associated with spinal surgery in adults over 60 years of age.9–11
Physical therapy is commonly recommended for patients with mild to moderate LSS, and patients with severe LSS typically undergo a trial of conservative treatment before surgery is proposed.12,13 Within a cohort of community-based patients with the clinical diagnosis of LSS in Canada, 59% of the patients interviewed reported having received physical therapy. Among these, 27% received massage, 23% received strengthening exercises, 18% received flexion exercises, 14% received aerobic conditioning, and 14% received bracing or walking devices.12 Although physical therapy is commonly used and recommended in clinical practice guidelines for patients with LSS, there is still little information about its effectiveness in this patient group.12,14 With the assortment of available treatments, the increasing population age, and the rising prevalence of LSS and its expensive associated health costs, it is important to identify the most effective physical therapy treatments available for patients with LSS.
To our knowledge, no systematic review specifically evaluating the effectiveness of physical therapy treatments has been published. Previously published systematic reviews have evaluated the effectiveness of nonsurgical interventions; these reviews included treatments such as steroidal injections that are outside the scope of physical therapist practice, or they did not fully explore the literature on physical therapy treatments.15–18 A recently published systematic review of nonoperative treatments for neurogenic claudication (including conditions other than degenerative LSS, such as spondylolisthesis) included literature published through 2010.16 The review found 4 randomized controlled trials (RCTs) evaluating physical therapy alone and 4 RCTs comparing a multimodal conservative package, including physical therapy, to surgical interventions. The authors of the review concluded that a wide variety of physical therapy treatments were used, limiting comparisons, but that there was low-quality evidence, suggesting that exercise is better than no intervention for pain and function and that surgery is better than a multimodal program for pain in the short term. Another recently published systematic review evaluating the effects of land-based exercises on functional outcomes of patients with LSS with literature searches up to June 201119 also found surgery to be significantly more effective than land-based exercises. However, the reviewers concluded that, given the known complications of surgery, exercise therapy should be considered before surgery.
The tendency to conglomerate the wide variety of physical therapy interventions into one category of intervention—“physical therapy”—is an issue, with many studies evaluating the efficacy of physical therapy interventions. Therefore, the purpose of this study was to systematically review studies evaluating the effectiveness of physical therapy interventions in the treatment of LSS, considering the specific type of physical therapy treatment and how it was applied. Because we expected a small number of RCTs to be available, we also searched for cohort studies and clinical controlled trials (CCTs) with a comparison group.
Method
Data Sources and Study Selection
Databases were searched electronically to identify appropriate articles. The databases examined included MEDLINE via Ovid (1950 to January 2012), EMBASE via Ovid (to January 2012), CINAHL (to January 2012), Scopus (to January 2012), Cochrane Library (to January 2012), and PEDro (to January 2012). Key words related to LSS and physical therapy treatment were selected for each database (Appendix). A manual search also was conducted on reference lists of a systematic review. Additionally, an ISI Web of Science search was conducted to identify potentially eligible studies that have cited the studies included here. The literature search was conducted in 2 stages. First, a search was conducted in November 2011, and 2 independent reviewers screened the database search results for potential articles based on titles and abstracts. Then, a third investigator performed another search in January 2012 with the objective of updating the search and expanding the inclusion criteria to non-English trials. The title and abstracts of the identified studies were screening by 2 independent reviewers. The full texts of the selected articles were further evaluated using an inclusion/exclusion criteria form to assess the suitability of articles for inclusion in the review. The review of each full text was conducted by 2 of the authors independently (L.G.M., A.H., L.K., J.M., L.T., and M.Y.), with 1 of the other authors resolving any disagreements.
The inclusion criteria of this study were:
Clinical trials with a comparison group (RCTs, CCTs, and prospective cohort studies).
Evaluation of interventions within the scope of physical therapist practice in North America.20 Multimodal studies where physical therapy was offered as part of a treatment package were included (eg, physical therapy + education + nonsteroidal anti-inflammatory drugs (NSAIDs). Studies where physical therapy was offered to patients, but it was unclear whether all patients in that treatment group had received it, were excluded.
Outcome measures of pain, disability, function, or health-related quality of life.
Clinical diagnosis of LSS, with confirmatory imaging. Because a universally accepted case definition for the diagnosis of degenerative LSS is not available, an age cutoff for inclusion of patients (commonly 40 years, 50 years or older) in LSS samples is frequently used.21,22 Therefore, as the systematic review was focused on degenerative LSS, we initially planned to include studies in which patients were at least 50 years of age. However, because we were able to identify only 3 studies that met the aforementioned criteria and included patients older than 50 years, we decided to modify our inclusion criteria to include studies of patients with a mean age greater than 50 years.
Quality Assessment
The PEDro scale was used to assess the quality of clinical trials (RCTs and CCTs).23 PEDro scores range from 0 to 10, with 10 being the highest quality. PEDro scores of RCTs were extracted from the PEDro database. As PEDro scores of CCTs were not available in the PEDro database, 2 reviewers (L.G.M., A.H., L.K., J.M., L.T., and M.Y.) independently rated the studies, and a third reviewer was used to resolve disagreements.
Because some of the important methodological features of RCTs, such as randomization, allocation concealment, blinding of participants, blinding of therapist, and an intention-to-treat analysis, are not relevant to the design or quality of cohort studies, a different scale was used to evaluate the quality of the cohort studies. A modified version of the Newcastle-Ottawa Quality Assessment scale24 that included modifications to better evaluate intervention-based cohort studies instead of cohort studies that examined prognostic factors was used. In the original Newcastle-Ottawa Quality Assessment scale, no credit was given if the study used a self-assessment tool as an outcome measure. However, most intervention-based cohort studies in this field have no other way to assess subjective factors such as pain or quality of life than with self-assessment scales. Thus, the modified scale gave credit to the study if it used a standardized self-assessment tool. In addition, the criteria “ascertainment of exposure,” “demonstration that the outcome of interest was not present at the start of the study,” and “the follow-up length in relation to the time needed for the outcome measure to be evaluated” were eliminated. All other items of the scale involving selection, comparability, and outcome remained the same in the modified scale. The modified Newcastle-Ottawa Quality Assessment scale was rated from 0 to 5. Scoring of each study was performed by 2 independent reviewers (L.G.M., A.H., L.K., J.M., L.T., and M.Y.), and a third reviewer was consulted if discrepancies arose.
Data Extraction
Two independent reviewers (L.G.M., A.H., L.K., J.M., L.T., and M.Y.) extracted data from the included studies by using standardized data extraction forms. Mean score, standard deviation, and sample size were extracted from the studies. When this information was not provided in the trials, the values were calculated or estimated by use of methods recommended in the Cochrane Handbook for Systematic Reviews of Interventions.25 Dichotomous data were extracted, noting the number of individuals experiencing an event and the sample size for that intervention group. Ordinal data were dichotomized and treated as dichotomous outcomes, as suggested in the Cochrane Handbook for Systematic Reviews of Interventions.25 When there was insufficient information about the studies to allow data analysis, the authors of the included studies were contacted.
The data also were organized according to follow-up periods: short term (less than 3 months), intermediate (3 months to 1 year), and long term (greater than 12 months). The descriptions of the treatment groups and outcome measures used were recorded in as much detail as possible. The following information was recorded if available in the studies: the number and length of treatment sessions, the duration of the program, the expertise of the caregiver, the presence or absence of home exercises, treatment adherence, harmful or adverse events, and how patients were assigned to treatment groups for cohort studies.
Data Synthesis and Analysis
Results were pooled if the studies were reasonably homogeneous with respect to the population, interventions, and outcome measures. Pain and disability outcomes were transformed to a 0 to 100 scale to allow pooling and facilitate interpretation of the results. For each study, weighted mean difference (WMD) or odds ratios and confidence intervals (CIs) were calculated for each outcome and time point. When trials were statistically homogeneous (I2<50%), estimates of pooled effects were calculated using a fixed-effects model. When trials were statistically heterogeneous (I2>50%), estimates of pooled effects were obtained using a random-effects model.25 Results of single studies are presented as mean difference (MD) and 95% CI. RevMan 5 from the Cochrane Library was used for statistical analysis.
The GRADE approach for grading the level of the evidence available was used to summarize the conclusion of this review.25 Depending on the number and quality of the studies included in the review, the evidence was classified into high, moderate, low, or very low quality.
Results
Study Selection
The final database search yielded 1,733 articles after duplicates were removed. Upon screening titles and abstracts, 31 records were deemed potentially eligible for full-text analysis.11,13,26–53 After examining these records against the pre-established inclusion criteria, 10 articles were deemed eligible for data extraction and analysis (Fig. 1).11,13,26–33 Not being able to delineate physical therapy treatments from non–physical therapy interventions was the primary reason for exclusions of potentially eligible studies. Often, multiple forms of conservative treatments were provided, and we were unable to identify whether all patients received a physical therapy intervention.
Figure 1.
Flowchart of systemic review inclusion and exclusion. Randomized controlled trials and cohort or clinical trials with comparison groups were considered.
Methodological Quality
The PEDro scale was used to rate a total of 9 studies (5 RCTs, 2 mixed-design studies with an RCT arm, and 2 nonrandomized crossover trials). The median PEDro score of the 5 RCTs11,13,27,29,32 was 7 (range=6–8), and the most commonly absent item was blinding of therapist or study participants. The 2 mixed-design studies had PEDro scores of 326 and 6,33 with the most commonly absent items being blinding of therapist, assessor, or study participants and poor follow-up rates. In addition, the 2 nonrandomized crossover trials had PEDro scores of 454 and 6,28 again with absence of all types of blinding and randomization.
The 2 mixed-design studies scored 2 on the modified Newcastle-Ottawa Quality Assessment scale, with patients not being selected from the same community or having similar characteristics. Most often, patients with greater severity were referred for surgery, and only patients with mild stenosis were referred for physical therapy. The simple cohort study30 had a score of 3 on the scale, with the primary weakness being an inadequate description of the study population and its characteristics.
Study Characteristics
Of the 10 studies included in this systematic review, 4 were RCTs comparing one physical therapy regimen against another.11,13,27,32 Whitman et al13 investigated the addition of manual therapy or flexion exercises to a progressive treadmill walking program. Goren et al11 investigated the addition of ultrasound or sham ultrasound to a standardized exercise program or against a control group. Koc et al27 evaluated the addition of a physical therapy modality regimen (ie, ultrasound, hot pack, and transcutaneous electrical nerve stimulation [TENS]) to a home exercise program. Lastly, Pua et al32 compared outcomes for body-weight–supported treadmill training against cycling when both were added to a standardized physical therapy program (ie, shortwave diathermy and mechanical lumbar traction).
Four studies (1 RCT, 2 mixed-design studies, and 1 cohort study) compared surgical intervention and physical therapy. The nonoperative arms consisted of: (1) lumbar isometric and stretching exercises, NSAIDs, and an undefined “physical therapy” treatment regimen plus education30; (2) education, static and dynamic postural modification, individualized muscle strengthening, endurance exercise, and modalities29; (3) a custom-fitted orthotic device to promote back extension, education (“back school”), ambulation, and stabilization exercises26; and (4) active physical therapy, back schools, home exercises, and other interventions (the latter could include non-physical therapy interventions such as steroid injections).33
Two controlled trials compared different varieties of corsets against each other. Levendoglu et al28 compared different corset types with varying degrees of body-weight support and no corset at all. Prateepavanich et al54 compared only one type of lumbosacral corset with no corset. Additional information about the interventions is available in Table 1.
Table 1.
Details of Included Studies and Interventions Provideda
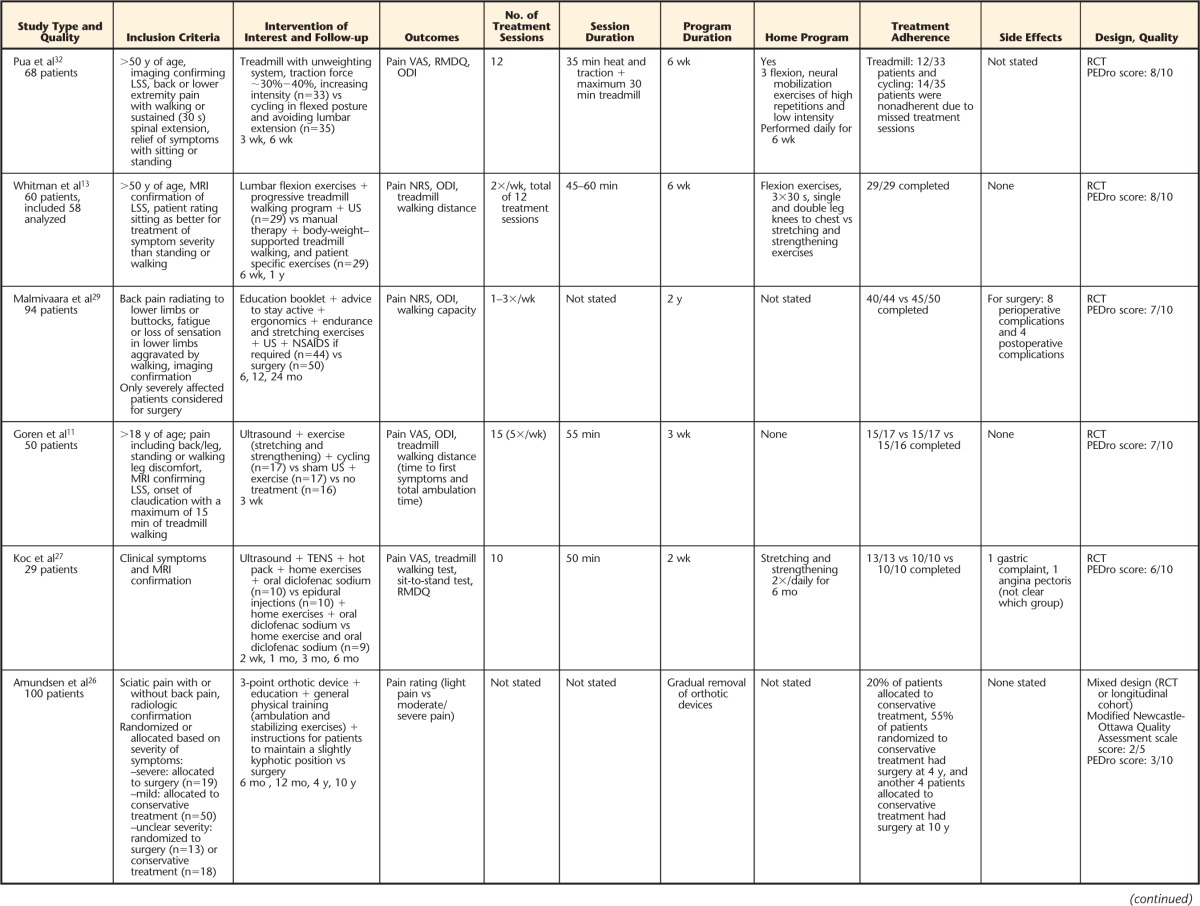

LSS=lumbar spinal stenosis, VAS=visual analog scale, RMDQ=Roland-Morris Disability Questionnaire, ODI=Oswestry Disability Index, RCT=randomized controlled trial, MRI=magnetic resonance imaging, US=ultrasound, NRS=numeric rating scale, NSAIDs=nonsteroidal anti-inflammatory drugs, TENS=transcutaneous electrical nerve stimulation, SF-36=36-Item Short-Form Health Survey.
Physical Therapy Treatment Compared With Other Physical Therapy Treatments or Controls
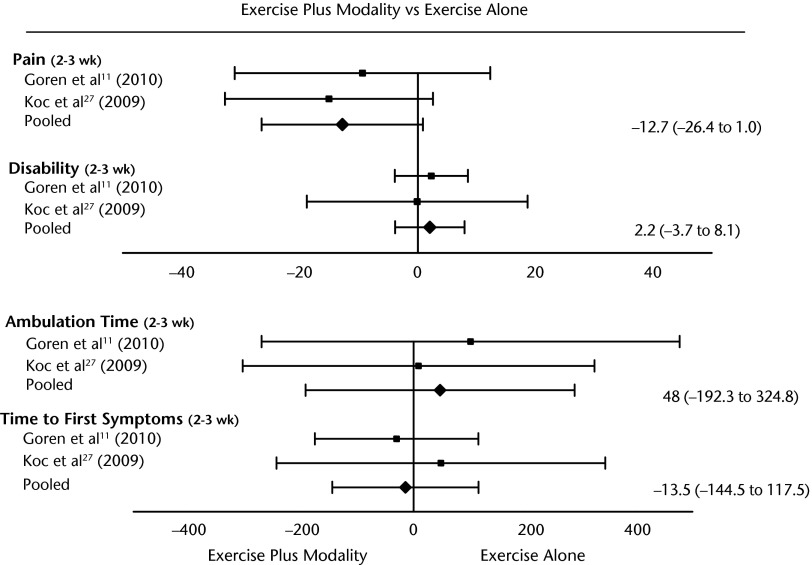
We were able to pool the results of 2 studies (49 patients) evaluating the addition of modalities (ultrasound, TENS, and heat pack) to an exercise program at short-term follow-up.11,27 The pooled results demonstrated that the addition of modalities had no significant effect on pain, disability, or walking capacity in the short term (2–3 weeks) (Fig. 2). The long-term (6 months) nonpooled results for the study of Koc et al27 also demonstrated no significant additional benefit of modalities for any of the outcomes studied (Tab. 2). Furthermore, nonpooled results of the study by Goren et al11 showed that an exercise program plus modalities was significantly better than no exercise in the short term (3 weeks) for back pain (MD=−23.3, 95% CI=−43.7 to −2.9), leg pain (effect size [ES]=−28.0, 95% CI=−49.6 to −6.4), and disability (Oswestry Disability Index) (ES=−7.1, 95% CI=−13.7 to −0.5).
Figure 2.
Forest plot of randomized controlled trials evaluating the addition of physical therapy modalities to an exercise program. Values represent weighted mean difference (95% confidence interval). The pooled effects were calculated using fixed-effect models (all I2=0%). Pain and disability outcomes are presented on a 0 to 100 scale, and walking ability measures are presented in seconds.
Table 2.
Results of Individual Studies That Were Not Pooled, With Outcomes Presented as Mean Difference and 95% Confidence Interval (95% CI) Comparing a Physical Therapy Treatment With Another Form of Physical Therapy Treatment or Controla

For all comparisons, effect estimates represent the group receiving the first therapy listed minus the group receiving the second therapy listed. Therefore, positive effect estimates indicate a lower mean score for first therapy listed, and negative values indicate a lower score for the second therapy listed. US=ultrasound, VAS=visual analog scale, NRS=numeric rating scale, RMDQ=Roland-Morris Disability Questionnaire, ODI=Oswestry Disability Index. *P<.05.
The results of the study by Pua et al32 showed that body-weight–supported treatment was not significantly better than cycling for any of the short-term pain and disability outcomes (3–6 weeks). Finally, the study by Whitman et al13 demonstrated that manual therapy in addition to flexion exercises and walking had effects similar to those of flexion exercises and walking alone for any of the outcomes evaluated in the short term (6 weeks) and long term (1 year) (Tab. 2).
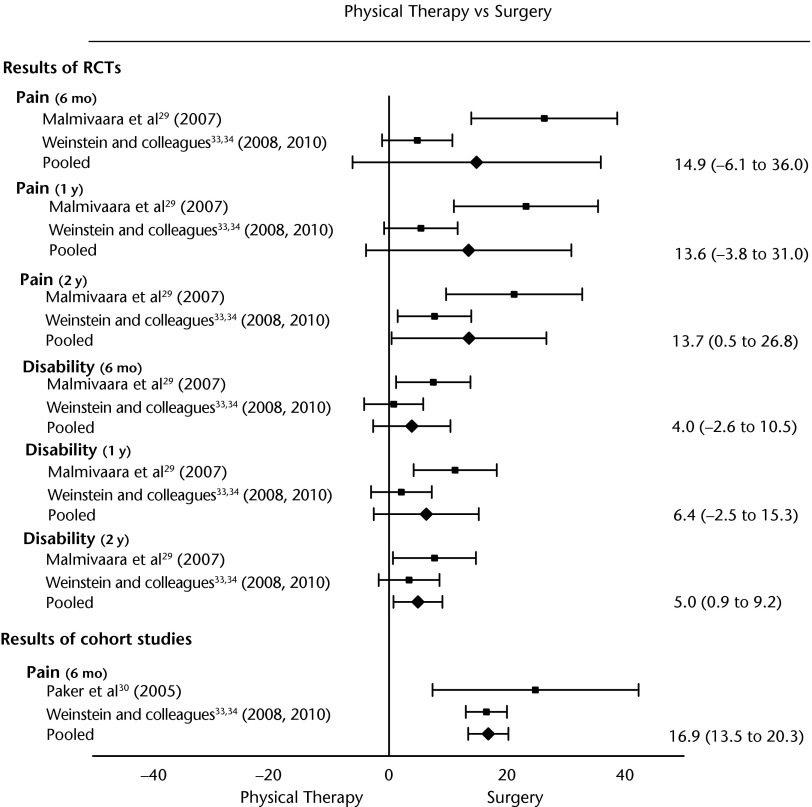
Physical Therapy Treatment Compared With Surgery
The studies included in this contrast consisted of RCTs, cohort studies, and mixed-design studies. When evaluating the possibility of pooling the studies, the research design used was taken into consideration. Therefore, RCTs were pooled with RCTs or the RCT arm of a mixed-design study (all using an intention-to-treat analysis), and cohort studies were pooled with other cohort studies or with the cohort arm plus the RCT arm of mixed-design studies considering the as-treated analysis (Fig. 3).
Figure 3.
Forest plot of randomized controlled trials (RCTs) comparing physical therapy and surgery. Values represent weighted mean difference (95% confidence interval). The pooled effects were calculated using fixed-effect models (all I2=0%) for pain at 6 months for the cohort studies and for disability at 2 years. All other pooled effects were calculated using random-effects models. Pain at 6 months RCTs I2=89%, pain at 1 year RCT I2=85%, pain at 2 years RCT I2=76%, disability at 6 months I2=63%, and disability at 1 year I2=76%. Pain and disability outcomes are presented on a 0 to 100 scale, and walking ability is presented in meters. Positive values favor surgery for the outcomes of pain and disability but favor physical therapy for ambulation time because high pain and disability are unfavorable outcomes, whereas high walking time is favorable.
We were able to pool the results for pain and disability for 2 RCTs that used continuous outcomes.29,33 We found that outcomes were not statistically significantly different between surgery and physical therapy for pain at intermediate term (340 patients at 6 months, WMD=14.9 points, 95% CI=−6.1 to 36.0), pain at long term (335 patients at 1 year, WMD=13.6 points, 95% CI=−3.8 to 31.0), disability at intermediate term (340 patients at 6 months, WMD=4.0 points, 95% CI=−2.6 to 10.5), and disability at long term (335 patients at 1 year, WMD=6.4 points, 95% CI=−2.5 to 15.3). However, the results favored surgery over physical therapy for pain at long-term follow-up at 2 years (308 patients at 2 years, WMD=13.7 points, 95% CI=0.5 to 26.8) and disability at long-term follow-up at 2 years (308 patients at 2 years, WMD=5.0 points, 95% CI=0.9 to 9.2). The results for pain and disability at intermediate and long-term follow-up (6 months and 1 year) did not favor one intervention over the other, and the results of the 2 applicable studies were contradictory. In the study by Malmivaara et al,29 the results favored surgery over physical therapy on all outcomes for all time points, and the results of the study by Weinstein et al33 demonstrated no significant different between groups.
Additionally, we were able to pool the result of 1 cohort study30 and one mixed-design study33 for pain at the intermediate term and found the results to favor surgery over physical therapy at 6 months (566 patients, WMD=16.9 points (95% CI=13.5 to 20.3).
The results of walking capacity were not pooled, as they were reported by 2 studies using different methods.29,30 The results of both studies indicated there was no significant difference in walking capacity between treatment groups.
The results favored surgery over physical therapy for leg pain (6 months, 1 and 2 years) for the study by Malmivaara et al29 and for pain and disability (3 months, 3 and 4 years) for the study by Weinstein et al33 when considering an as-treated analysis. The results were not different between groups when considering the outcomes of the RCT arm of the study by Weinstein et al when using the intention-to-treat analysis (Tab. 3).
Table 3.
Results of Individual Studies That Were Not Pooled, With Outcomes Presented as Mean Difference and 95% Confidence Interval (95% CI) Comparing Physical Therapy Treatment With Surgerya
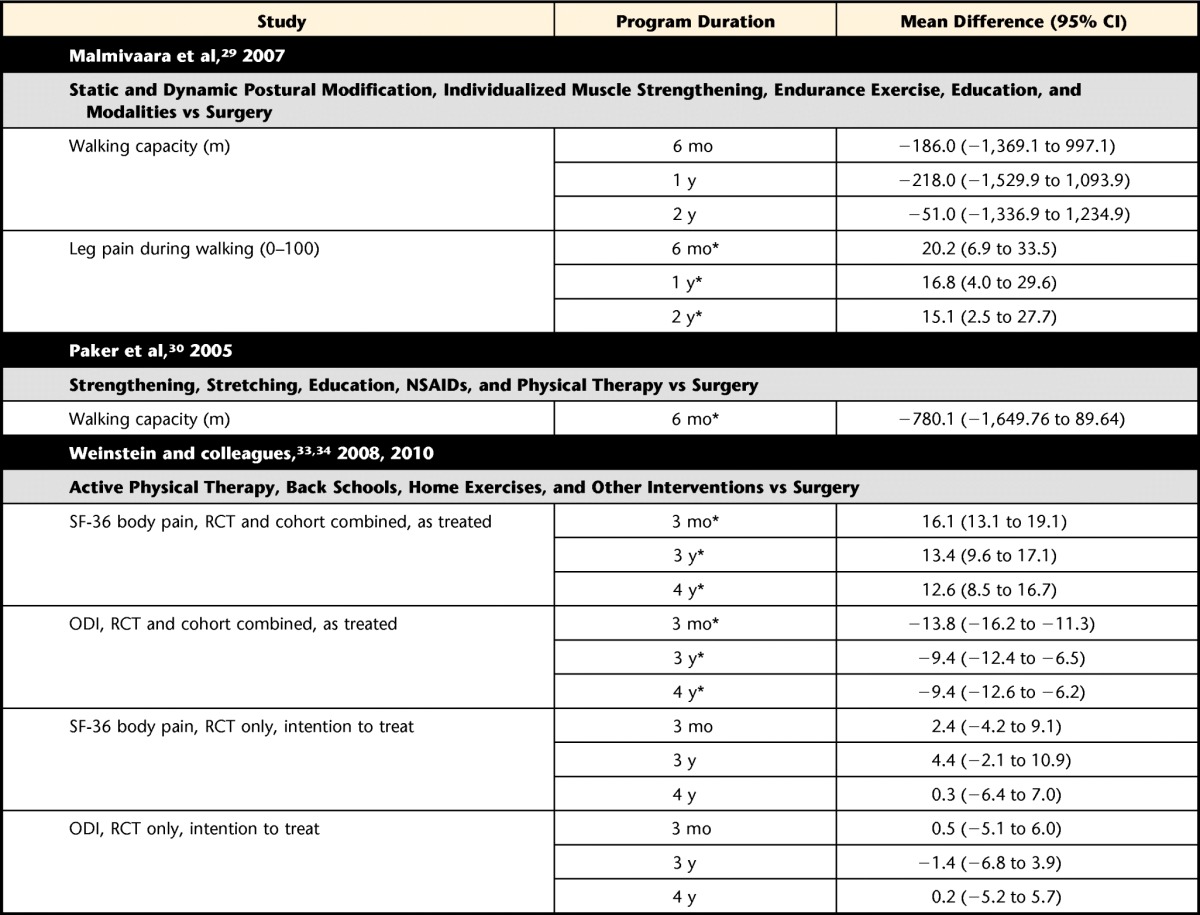
For all comparisons, effect estimates represent the group receiving the first therapy listed minus the group receiving the second therapy listed. Therefore, positive effect estimates indicate a lower mean score for the first therapy listed while negative values indicate a lower score for the second therapy listed. Weinstein and colleagues' results are adjusted for age, sex, baseline scores, income, treatment preference, duration of symptoms, compensation, smoking status, body mass index, baseline sciatica bothersomeness, and joint, stomach, and bowel problems and are presented as mean difference from the change from baseline. NSAIDs=nonsteroidal anti-inflammatory drugs, SF-36=36-Item Short-Form Survey, RCT=randomized controlled trial, ODI=Oswestry Disability Index. *P<.05.
The results for pain of the study Amundsen et al26 were transformed into dichotomous variables for the purpose of this analysis, with patients separated into those having moderate or severe pain versus those having no pain or light pain. Patients who crossed over between interventions were excluded from the analysis. The results demonstrated that the odds of a patient having moderate to severe pain were not statistically significantly different for those receiving physical therapy or surgery (Tab. 4).
Table 4.
Results of Dichotomous Outcomes Calculated as Odds Ratio (OR) and 95% Confidence Interval (95% CI) for Physical Therapy Treatment Versus Surgerya
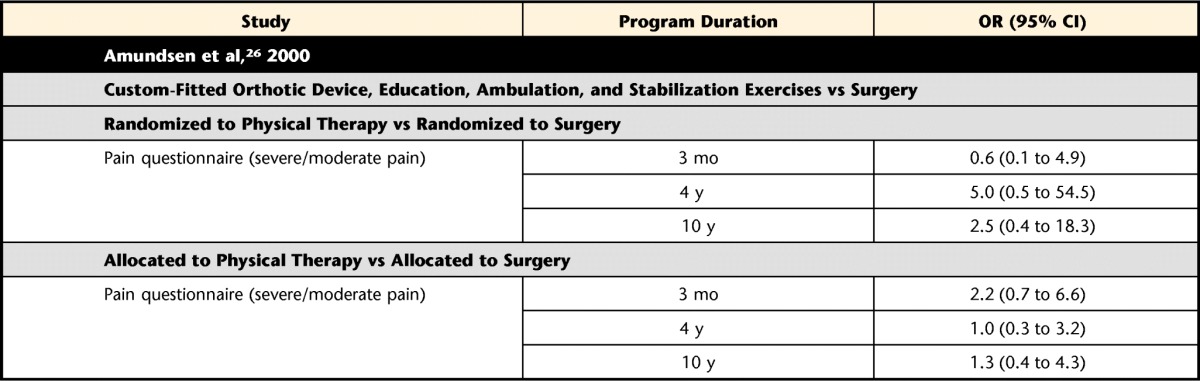
Odds ratio of less than 1 means that the odds of having moderate to severe pain was greater in the surgery group, whereas an OR value greater than 1 means that the odds of having moderate to severe pain was greater in the physical therapy group.
Comparison of Corsets With and Without Load Reduction and Controls
All outcomes regarding corsets were collected while walking on a treadmill with or without the use of a corset. The nonpooled results of single studies demonstrated that a lumbar corset was statistically significantly better than no corset for pain severity (MD=−12.0, 95% CI=−19.4 to −4.6) and walking ability, tested using time to first symptoms (MD=29.5, 95% CI=13.2 to 45.8) and total walking time (MD=51.3, 95% CI=23.1 to 79.5),28 but not for walking distance.54 The results also showed that 20% and 25% weight reduction with a corset were statistically significantly better than no corset for time to first symptoms and walking time (Tab. 5). Twenty-five percent weight reduction was significantly better than lumbar corset with no weight reduction for time to first symptoms only (MD=−29.3, 95% CI=−51.6 to −7.0), but 20% weight reduction was no better than a lumbar corset alone. Furthermore, 25% weight reduction was significantly better than 20% weight reduction for time to first symptoms (MD=−25.3, 95% CI=−50.2 to −0.4). The results also showed that an elastic woolen corset was not significantly better than no corset.
Table 5.
Results of Individual Studies That Were Not Pooled, With Outcomes Presented as Mean Difference and 95% Confidence Interval (95% CI) Comparing Different Types of Corsetsa
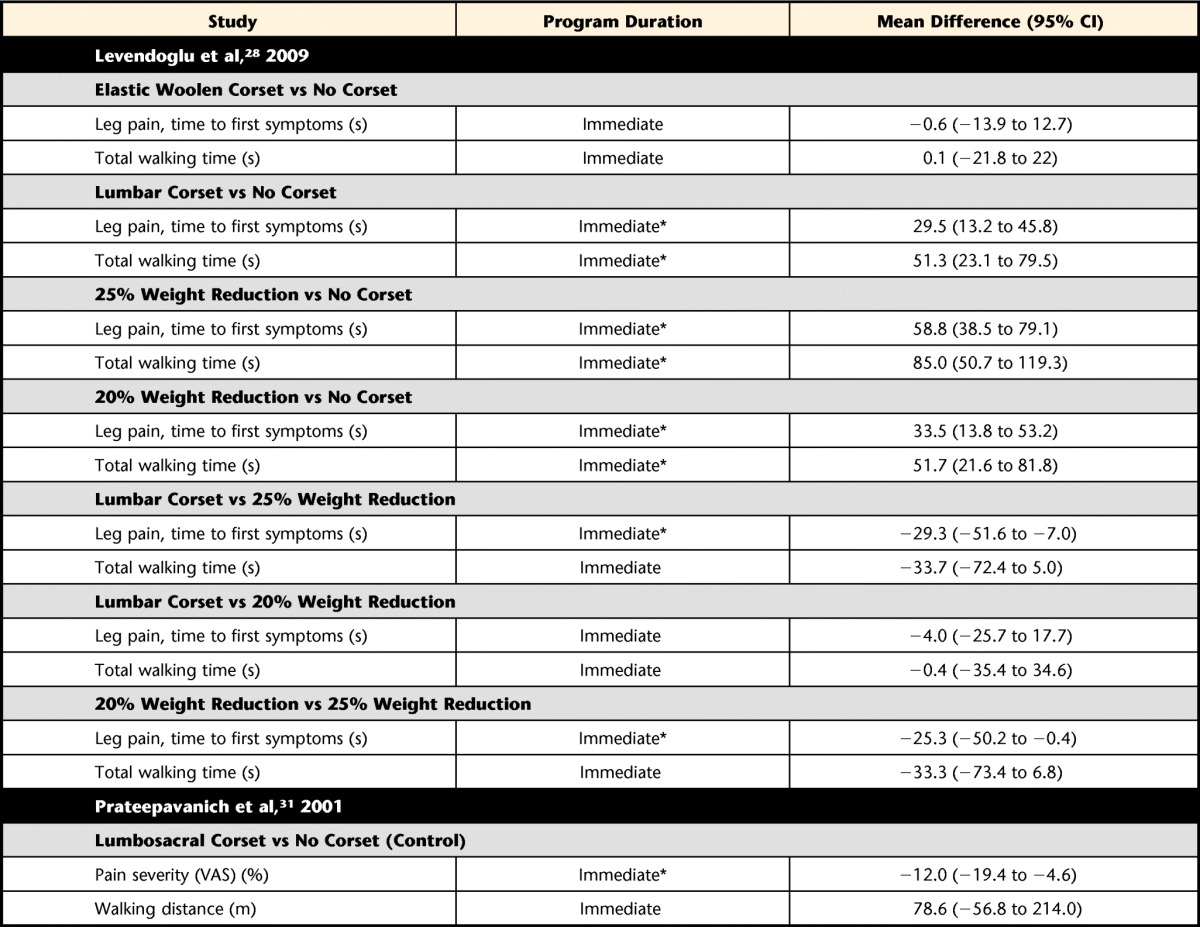
For all comparisons, effect estimates represent the group receiving the first therapy listed minus the group receiving the second therapy listed. Therefore, positive effect estimates indicate a lower mean score for the first therapy listed, whereas negative values indicate a lower score for the second therapy listed. VAS=visual analog scale. *P<.05.
Discussion
In this systematic review, we assessed the effectiveness of physical therapy treatments for patients with LSS through RCTs, CCTs, and cohort studies with a comparison group. A large range of physical therapy treatments were studied, which limited pooling and conclusions about a specific intervention. Furthermore, there were only 5 good-quality RCTs, whereas all other studies with different study designs were of moderate to poor quality. Thus, the results of the review should be viewed with caution.
There is low-quality evidence suggesting that exercise therapy leads to better short-term outcomes than no exercise with respect to disability and back and leg pain. However, the mean effect for disability was small (7.1 on a 100 scale) and clinically questionable. There is low-quality evidence that modalities (ultrasound, TENS, heat packs) and manual therapy have no additional benefit than an exercise program alone. Given the small sample sizes of the studies included in the contrast evaluating the addition of modalities to exercise and the results for the outcome of pain in Figure 2, it is possible that larger sample sizes would lead to statistically significant results. However, differences in the outcome of pain between groups would likely still be smaller than 20 on a 0 to 100 scale and, therefore, below the limits of clinical significance.55 Furthermore, there is low-quality evidence that exercise involving treadmill walking with body-weight support is no more effective than cycling for short-term outcomes. There is moderate-quality evidence suggesting that surgery leads to better long-term (2 years) outcomes for pain and disability, but not walking distance, than physical therapy. Again, the mean effects for disability were small (5 on a 100 scale) and of questionable clinical importance. The results also provided low-quality evidence suggesting that the 2 interventions are not different for pain and disability at long term (1 year) and contradictory evidence for the intermediate-term results. There is low-quality evidence from individual studies suggesting that walking ability is improved while wearing a lumbar corset in comparison with an elastic woolen corset or no corset. Additionally, a corset with 25% weight reduction was found to be better than one with 20% or no weight reduction for time to first symptoms while walking on a treadmill.
The results of this review have significant implications because they contradict reports of common clinical practice.12 For instance, 68% of physical therapists treating patients with LSS reported using some type of modalities for this patient group.12 Moreover, 66% of physical therapists reported providing some type of manual therapy to patients with LSS. If current evidence suggests that modalities and manual therapy have little or no effect above that of exercise, it may be prudent for physical therapists to refocus their treatment to a more active approach, unless further evidence indicates otherwise.
It has been identified that only 12% of therapists recommend the use of corsets in clinical practice.12 Despite the fact that the results of this study regarding corsets are limited due to the small number of studies and types of outcomes evaluated, the results suggest that the use of lumbar support corsets has significantly better effects in increasing walking ability (distance) than not using corsets.54 Therefore, although future studies are needed to corroborate this finding, therapists may want to consider recommending the use of this inexpensive device during daily activities that require walking.
Weight reduction treadmill training devices are expensive and required in clinic use and, therefore, have been used primarily in research with the expectation that decreasing the load on the spine will decrease pain.28 Concordantly, a 25% weight reduction corset was found to be better than a regular lumbar corset in decreasing time to first symptoms while walking. However, because weight reduction devices can only be used for training in clinical practice and the results of this review suggest that cycling has effects similar to those of a weight reduction corset with respect to short-term pain and disability outcomes, cycling would appear to be the treatment of choice because it is less expensive, easier to apply, and requires less training and time from the treating therapist and patient.
The results of this review suggest that surgery is better than physical therapy for pain and disability at the long term (2 years), and the results are still somewhat controversial for pain and disability at intermediate term and long term (6 months and 1 year). However, as mentioned in the “Results” section of this study, the results of the 2 studies included in the contrast evaluating pain and disability at intermediate term were contradictory.
The results of the study by Malmivaara et al29 favored surgery over physical therapy on all outcomes evaluated, and the results of the study by Weinstein et al33 were not significantly different between groups. It is worth noting that the results of the RCT arm of the study by Weinstein et al were not free of bias, as there was a large crossover of patients between treatment groups, and the use of an intention-to-treat analysis in this case does not help in maintaining the benefits of randomization. It is possible that the positive surgical results of those patients who were initially randomized to conservative treatment but received surgery inflated the results of the conservative arm when using the intention-to-treat analysis. Furthermore, generalizing the results of the cohort studies and RCTs using an as-treated analysis are limited due to the fact that patients were often allocated to receive surgery based on the baseline levels of pain. Thus, we can conclude that there is moderate-quality evidence suggesting that surgery is better than physical therapy for pain and disability at the long term (2 years), but there is very low-quality evidence suggesting that the 2 interventions are similar in relation to walking capacity or to pain and disability at the short term and long term. Furthermore, the results of for pain at intermediate term (6 months) for the RCTs and cohort studies are contradictory and need further investigation.
The review of Ammendolia et al16 summarizing the results of nonsurgical interventions for patients with LSS identified 7 of the 10 studies included in this systematic review. The review of Jarrett et al19 summarizing the results of land-based exercises identified 6 of the 10 studies included in this review. However, by depicting the facets of the physical therapy interventions, we were able to evaluate additional comparisons, such as the addition of modalities to exercise versus exercise alone, and we were able to perform a meta-analysis for a few of these comparisons. The overall messages of the 3 reviews, that exercise seems to be better than no exercise and that surgery appears to be superior to physical therapy for pain, are somewhat similar. However, the current summary of evidence on specific physical therapy interventions such as modalities (eg, ultrasound, heat pack), manual therapy, and corsets added another dimension beyond the results of the earlier reviews.
A weakness of this review was the heterogeneity in interventions and outcomes used among studies, as well as the variation in study designs. This weakness made it difficult to compare studies. Because treatments often were “bundled,” the effect of a particular physical therapy treatment could not be discerned. Physical therapy programs also typically were not described in detail (eg, parameters, dosage) and often were ambiguously listed as “typical physical therapy treatment.” Physical therapy programs need to be more clearly defined to allow better interpretation of the study results, replication in future studies, and application. Several studies had to be excluded because epidural steroids were the primary form of treatment in addition to physical therapy. This limitation made it difficult to identify what aspect of the conservative treatment affected a patient's pain, especially because epidural steroids are a potent form of pain medication. However, we allowed NSAIDs to be part of conservative treatment, as long as it was not a major part of the treatment, because we believe many patients will be taking some form of anti-inflammatory or pain medication when receiving physical therapy treatment for LSS. In one study comparing physical therapy, education, and NSAIDs with surgery, 52% of the patients receiving the nonsurgical treatment also received steroidal injections.33 As the use of injection was a cointervention received outside of the treatments given as part of the RCT, the study was not excluded from this review.
Caution needs to be taken in generalizing the results of this review, given the small number of studies evaluating each treatment and the quality of evidence available. The literature evaluating physical therapy interventions for patients with LSS is scarce, and high-quality long-term RCTs are warranted. Studies evaluating the best physical therapy intervention or package of interventions to be delivered to this patient population are crucial. Exercises appear to be a commonality among the interventions evaluated; however, the best type of exercise (specific or general), weight reduction protocols, corsets, and addition of manual therapy and other forms of treatment to exercise need to be further investigated. However, possible mechanisms of action of these and other interventions need to be carefully considered and presented to support future studies worthy of the time and resources required.
Appendix.
Search Strategies
MEDLINE via Ovid
1. spinal stenosis.mp or spinal stenosis/
2. exp lumbar vertebrae/ or lumbar spinal stenosis.mp
3. lumbago.mp or exp low back pain/
4. sciatica.mp or exp sciatica/
5. back pain.mp or exp back pain/
6. 2 or 3 or 4 or 5
7. exp cervical vertebrae
8. 1 and 6
9. 8 NOT 7
10. limit 10 to humans
11. limit 11 to case reports or clinical conference or clinical trial, all or clinical trial phase I–IV or comparative study or controlled clinical trial or randomized controlled trial
EMBASE via Ovid
1. exp vertebral canal stenosis/
2. exp cervical spine/
3. 1 NOT 2
4. limit 3 to (human and (clinical trial or randomized controlled trial or controlled clinical trial or multicenter study or phase 1 clinical trial or phase 2 clinical trial or phase 3 clinical trial or phase 4 clinical trial))
CINAHL
(MH & quot, lumbar vertebrae & quot;) OR (“ lumbar & quot;) AND (spinal stenosis or lumbar spinal stenosis NOT cervical vertebrae)
Limit to human
Scopus
LSS or spin* stenosis AND (physical therapy or physiotherapy or intervention or treatment)
PEDro
Search term: stenosis
Body part: lumbar spine, sacro-iliac joint, or pelvis
Cochrane Library
Spinal stenosis
Footnotes
Dr Macedo, Mr Mo, Mr Yeung, and Professor Battié provided concept/idea/research design. All authors provided writing. Dr Macedo, Mr Hum, Ms Kuleba, Mr Mo, Ms Truong, and Mr Yeung provided data collection and analysis. Dr Macedo, Mr Yeung, and Professor Battié provided project management. Mr Mo provided clerical support. Dr Macedo, Mr Mo, and Mr Yeung provided consultation (including review of manuscript before submission).
Dr Macedo received support from Alberta Innovates Health Solutions and the Canadian Institutes of Health Research, and Dr Battié was supported by the Canada Research Chairs Program.
References
- 1. Haig AJ, Tong HC, Yamakawa KSJ, et al. Spinal stenosis, back pain, or no symptoms at all? A masked study comparing radiologic and electrodiagnostic diagnosis to the clinical impression. Arch Phys Med Rehabil. 2006;87:897–903 [DOI] [PubMed] [Google Scholar]
- 2. Jansson KA, Nemeth G, Granath F, et al. Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Joint Surg Br. 2009;91:210–216 [DOI] [PubMed] [Google Scholar]
- 3. Atlas SJ, Keller RB, Wu YA, et al. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine Lumbar Spine Study. Spine (Phila Pa 1976). 2005;30:936–943 [DOI] [PubMed] [Google Scholar]
- 4. Fritz JM, Erhard RE, Delitto A, et al. Preliminary results of the use of a two-stage treadmill test as a clinical diagnostic tool in the differential diagnosis of lumbar spinal stenosis. J Spinal Disord. 1997;10:410–416 [PubMed] [Google Scholar]
- 5. Kapural L, Mekhail N, Bena J, et al. Value of the magnetic resonance imaging in patients with painful lumbar spinal stenosis (LSS) undergoing lumbar epidural steroid injections. Clin J Pain. 2007;23:571–575 [DOI] [PubMed] [Google Scholar]
- 6. Penning L, Wilmink JT. Posture-dependent bilateral compression of L4 or L5 nerve roots in facet hypertrophy: a dynamic CT-myelographic study. Spine (Phila Pa 1976). 1987;12:488–500 [DOI] [PubMed] [Google Scholar]
- 7. Battié MC, Jones A, Schopflocher DP, Hu RW. Health-related quality of life and comorbidities associated with lumbar spinal stenosis. Spine J. 2012;12:189–195 [DOI] [PubMed] [Google Scholar]
- 8. Ciol MA, Deyo RA, Howell E, Kreif S. Assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44:285–290 [DOI] [PubMed] [Google Scholar]
- 9. Taylor VM, Deyo RA, Cherkin DC, et al. Low back pain hospitalization: recent United States trends and regional variations. Spine (Phila Pa 1976). 1994;19:1207–1213 [DOI] [PubMed] [Google Scholar]
- 10. Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005;30:1441–1445 [DOI] [PubMed] [Google Scholar]
- 11. Goren A, Yildiz N, Topuz O, et al. Efficacy of exercise and ultrasound in patients with lumbar spinal stenosis: a prospective randomized controlled trial. Clin Rehabil. 2010;24:623–631 [DOI] [PubMed] [Google Scholar]
- 12. Tomkins CC, Dimoff KH, Forman HS, et al. Physical therapy treatment options for lumbar spinal stenosis. J Back Musculoskelet Rehabil. 2010;23:31–37 [DOI] [PubMed] [Google Scholar]
- 13. Whitman JM, Flynn TW, Childs JD, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: a randomized clinical trial. Spine (Phila Pa 1976). 2006;31:2541–2549 [DOI] [PubMed] [Google Scholar]
- 14. Diagnosis and treatment of degenerative lumbar spinal stenosis. 2011. Available at: http://www.spine.org Accessed August 16, 2013
- 15. Tran DQH, Duong S, Finlayson RJ. Lumbar spinal stenosis: a brief review of the nonsurgical management. Can J Anaesth. 2010;57:694–703 [DOI] [PubMed] [Google Scholar]
- 16. Ammendolia C, Stuber K, de Bruin LK, et al. Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: a systematic review. Spine (Phila Pa 1976). 2012;37:E609–E616 [DOI] [PubMed] [Google Scholar]
- 17. Reiman MP. Manual therapy interventions for patients wtih lumbar spinal stenosis: a systematic review. NZ J Physiother. 2009;37:17–28 [Google Scholar]
- 18. Kovacs FM, Urrutia G, Alarcon JD. Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials. Spine (Phila Pa 1976). 2011;36:1335–1351 [DOI] [PubMed] [Google Scholar]
- 19. Jarrett MS, Orlando JF, Grimmer-Somers K. The effectiveness of land based exercise compared to decompressive surgery in the management of lumbar spinal-canal stenosis: a systematic review. BMC Musculoskelet Disord. 2012;13:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. American Physical Therapy Association Today's Physical Therapist: A Comprehensive Review of a 21st Century Health Care Profession. 2011. Available at: http://www.apta.org/uploadedFiles/APTAorg/Practice_and_Patient_Care/PR_and_Marketing/Market_to_Professionals/TodaysPhysicalTherapist.pdf Accessed August 16, 2013
- 21. Tomkins CC, Battié MC, Hu R. Construct validity of the physical function scale of the swiss spinal stenosis questionnaire for the measurement of walking capacity. Spine (Phila Pa 1976). 2007;32:1896–1901 [DOI] [PubMed] [Google Scholar]
- 22. Iversen MD, Katz JN. Examination findings and self-reported walking capacity in patients with lumbar spinal stenosis. Phys Ther. 2001;81:1296–1306 [PubMed] [Google Scholar]
- 23. Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro: a database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5:223–226 [DOI] [PubMed] [Google Scholar]
- 24. Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute; 2011. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed August 16, 2013 [Google Scholar]
- 25. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011] The Cochrane Collaboration, 2011. Available at: http://handbook.cochrane.org Accessed August 16, 2013 [Google Scholar]
- 26. Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical management? A prospective 10-year study. Spine (Phila Pa 1976). 2000;25:1424–1436 [DOI] [PubMed] [Google Scholar]
- 27. Koc Z, Ozcakir S, Sivrioglu K, et al. Effectiveness of physical therapy and epidural steroid injections in lumbar spinal stenosis. Spine (Phila Pa 1976). 2009;34:985–989 [DOI] [PubMed] [Google Scholar]
- 28. Levendoglu F, Oguz H, Polat E, Bodur S. The effect of corset on walking time in lumbar spinal stenosis. Turkiye Klinikleri J Med Sci. 2009;29:1172–1177 [Google Scholar]
- 29. Malmivaara A, Slatis P, Heliovaara M, et al. Surgical or nonoperative treatment for lumbar spinal stenosis: a randomized controlled trial. Spine (Phila Pa 1976). 2007;32:1–8 [DOI] [PubMed] [Google Scholar]
- 30. Paker N, Turkmen C, Bugdayci D, et al. Comparison of conservative and surgical treatment results in lumbar spinal stenosis. Turk Neurosurg. 2005;15:182–184 [Google Scholar]
- 31. Prateepavanich PS, Thanapipatsiri S, Santisatisakul P, et al. The effectiveness of lumbosacral corset in symptomatic degenerative lumbar spinal stenosis. J Med Assoc Thai. 2001;84:572–576 [PubMed] [Google Scholar]
- 32. Pua YH, Cai CC, Lim KC. Treadmill walking with body weight support is no more effective than cycling when added to an exercise program for lumbar spinal stenosis: a randomised controlled trial. Aust J Physiother. 2007;53:83–89 [DOI] [PubMed] [Google Scholar]
- 33. Weinstein JN, Tosteson TD, Lurie JD, et al. ; SPORT Investigators Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976). 2010;35:1329–3138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Akyol Y, Durmus D, Alayli G, et al. Effectiveness of physical therapy agents in patients with lumbar spinal stenosis [in Turkish]. Turk J Phys Med Rehabil. 2009;55:141–146 [Google Scholar]
- 36. Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X STOP device in patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2006;4:463–471 [DOI] [PubMed] [Google Scholar]
- 37. Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, part III: 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 1996;21:1787–1795; discussion 1974–1975 [DOI] [PubMed] [Google Scholar]
- 38. Atlas SJ, Keller RB, Robson D, et al. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the Maine Lumbar Spine Study. Spine (Phila Pa 1976). 2000;25:556–562 [DOI] [PubMed] [Google Scholar]
- 39. Chang Y, Singer DE, Wu YA, et al. The effect of surgical and nonsurgical treatment on longitudinal outcomes of lumbar spinal stenosis over 10 years. J Am Geriatr Soc. 2005;53:785–792 [DOI] [PubMed] [Google Scholar]
- 40. Hsu KY, Zucherman JF, Hartjen CA, et al. Quality of life of lumbar stenosis-treated patients in whom the X STOP interspinous device was implanted. J Neurosurg Spine. 2006;5:500–507 [DOI] [PubMed] [Google Scholar]
- 41. Mariconda M, Fava R, Gatto A, et al. Unilateral laminectomy for bilateral decompression of lumbar spinal stenosis: a prospective comparative study with conservatively treated patients. J Spinal Disord Tech. 2002;15:39–46 [DOI] [PubMed] [Google Scholar]
- 42. Zucherman JF, Hsu KY, Hartjen CA, et al. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J. 2004;13:22–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zucherman JF, Hsu KY, Hartjen CA, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results [with consumer summary]. Spine (Phila Pa 1976). 2005;30:1351–1358 [DOI] [PubMed] [Google Scholar]
- 44. Athiviraham A, Yen D. Is spinal stenosis better treated surgically or nonsurgically? Clin Orthop Relat Res. 2007;458:90–93 [DOI] [PubMed] [Google Scholar]
- 45. Burnett MG, Stein SC, Bartels RH. Cost-effectiveness of current treatment strategies for lumbar spinal stenosis: nonsurgical care, laminectomy, and X-STOP. J Neurosurg Spine. 2010;13:39–46 [DOI] [PubMed] [Google Scholar]
- 46. Iversen MD, Choudhary VR, Patel SC; North American Spine Society Therapeutic exercise and manual therapy for persons with lumbar spinal stenosis [with consumer summary]. Int J Clin Rheumatol. 2010;5:425–437 [Google Scholar]
- 47. Iwamoto J, Sato Y, Takeda T, Matsumoto H. Effectiveness of exercise in the treatment of lumbar spinal stenosis, knee osteoarthritis, and osteoporosis. Aging Clin Exp Res. 2010;22:116–122 [DOI] [PubMed] [Google Scholar]
- 48. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sahin F, Yilmaz F, Kotevoglu N, Kuran B. The efficacy of physical therapy and physical therapy plus calcitonin in the treatment of lumbar spinal stenosis. Yonsei Med J. 2009;50:683–688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yaksi A, Ozgonenel L, Ozgonenel B. The efficiency of gabapentin therapy in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 2007;32:939–942 [DOI] [PubMed] [Google Scholar]
- 52. Onel D, Sari H, Donmez C. Lumbar spinal stenosis: clinical/radiologic therapeutic evaluation in 145 patients: conservative treatment or surgical intervention? Spine (Phila Pa 1976). 1993;18:291–298 [PubMed] [Google Scholar]
- 53. Simotas AC, Dorey FJ, Hansraj KK, Cammisa F. Nonoperative treatment for lumbar spinal stenosis: clinical and outcome results and a 3-year survivorship analysis. Spine (Phila Pa 1976). 2000;25:197–204 [DOI] [PubMed] [Google Scholar]
- 54. Prateepavanich P, Thanapipatsiri S, Santisatisakul P, et al. The effectiveness of lumbosacral corset in symptomatic degenerative lumbar spinal stenosis. J Med Assoc Thai. 2001;84:572–576 [PubMed] [Google Scholar]
- 55. Ostelo RW, Deyo RA, Stratford PW, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33:90–94 [DOI] [PubMed] [Google Scholar]