Abstract
Outcome prediction based on tumor stage reflected by the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) tumor node metastasis (TNM) system is currently regarded as the strongest prognostic parameter for patients with colorectal cancer. For affected patients, the indication for adjuvant therapy is mainly guided by the presence of regional lymph node metastasis. In addition to the extent of surgical lymph node removal and the thoroughness of the pathologist in dissecting the resection specimen, several parameters that are related to the pathological work-up of the dissected nodes may affect the clinical significance of lymph node staging. These include changing definitions of lymph nodes, involved lymph nodes, and tumor deposits in different editions of the AJCC/UICC TNM system as well as the minimum number of nodes to be dissected. Methods to increase the lymph node yield in the fatty tissue include methylene blue injection and acetone compression. Outcome prediction based on the lymph node ratio, defined as the number of positive lymph nodes divided by the total number of retrieved nodes, may be superior to the absolute numbers of involved nodes. Extracapsular invasion has been identified as additional prognostic factor. Adding step sectioning and immunohistochemistry to the pathological work-up may result in higher accuracy of histological diagnosis. The clinical value of more recent technical advances, such as sentinel lymph node biopsy and molecular analysis of lymph nodes tissue still remains to be defined.
Keywords: Colon cancer, Rectum cancer, Tumor staging, Lymph node metastasis, Prognosis, Sentinel lymph node, Lymph node ratio, Extracapsular invasion, Immunohistochemistry, Molecular analysis
Core tip: For patients with colorectal cancer, the indication for adjuvant therapy is mainly guided by the presence of regional lymph node metastasis. This review provides an in depth analysis of parameters affecting the clinical significance of lymph node staging, focusing on changing definitions of lymph nodes, involved lymph nodes, and tumor deposits in different editions of the American Joint Committee on Cancer/Union for International Cancer Control tumor node metastasis staging system, the minimum number of lymph nodes that should be evaluated, lymph node ratio, extracapsular invasion, sentinel node biopsy, and the potential benefit of ancillary techniques, such as immunohistochemistry and molecular analysis.
INTRODUCTION
Colorectal cancer is one of the most common cancers worldwide. In the United States, approximately 102480 new cases of colon cancer and 40340 new cases of rectal cancer have been estimated for 2013. For the same time period, 50830 deaths from colorectal cancer have been calculated, accounting for about 9% of all cancer deaths[1].
Surgical resection is the treatment of choice for patients with locally confined disease. Outcome prediction based on tumor stage reflected by the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) tumor node metastasis (TNM) system is currently regarded as the strongest prognostic parameter. Adjuvant chemotherapy, which is primarily based on 5-fluorouracil, has decreased tumor recurrence in AJCC/UICC stage III patients, while neoadjuvant chemotherapy and total mesorectal excision have improved local control in patients with rectal cancer. The indication for adjuvant therapy is mainly guided by the presence of regional lymph node metastasis[2-4].
A plethora of controversies exists how the evaluation of resected lymph nodes should be performed, many of these affecting the clinical significance of lymph node staging in daily routine practice (Table 1). This already starts with varying definitions of lymph nodes as such, lymph nodes involved by metastatic tumor tissue, and their differentiation from tumor deposits, as is reflected by changing criteria in different editions of the AJCC/UICC TNM staging system[5]. The number of examined lymph nodes has been identified as an additional important issue. Some investigators claim the lymph node ratio, defined as the number of positive lymph nodes divided by the total number of retrieved nodes, to be more important than the absolute number of positive nodes[6-9]. Likewise, the identification of extracapsular invasion by cancer cells may help to improve the prognostic significance of lymph node staging[10-13].
Table 1.
Parameters affecting the clinical significance of lymph node staging in colorectal cancer
| Extent of surgical lymph node removal |
| Thoroughness of the pathologist in dissecting the resection specimen |
| Technical methods to increase lymph node yield |
| Methylene blue injection |
| Fat clearing |
| Acetone compression |
| Changing definitions of lymph nodes, involved lymph nodes, and tumor deposits in different editions of the AJCC/UICC TNM staging system |
| History of neoadjuvant treatment |
| Absolute number of retrieved lymph nodes |
| Absolute number of positive lymph nodes |
| Lymph node ratio |
| Presence of extracapsular invasion |
| Sentinel node biopsy |
| Number of histological sections |
| Use of immunohistochemistry to identify micrometastasis and/or isolated tumor cells |
| Use of molecular techniques to identify minimal tumor disease in lymph node tissue |
AJCC: American Joint Committee on Cancer; UICC: Union for International Cancer Control; TNM: Tumor node metastasis.
Manual dissection with subsequent histological assessment based on routinely hematoxylin and eosin (HE) stained slides is the standard approach in the examination of regional lymph nodes in cancer specimens (Figure 1)[14]. However, some studies have raised the suspicion that analysis based solely on HE stained slides is insufficient for a proper evaluation. This notion has led to the introduction of new techniques, such as sentinel node biopsy, immunohistochemical and molecular analyses in the work-up of cancer specimens[15].
Figure 1.
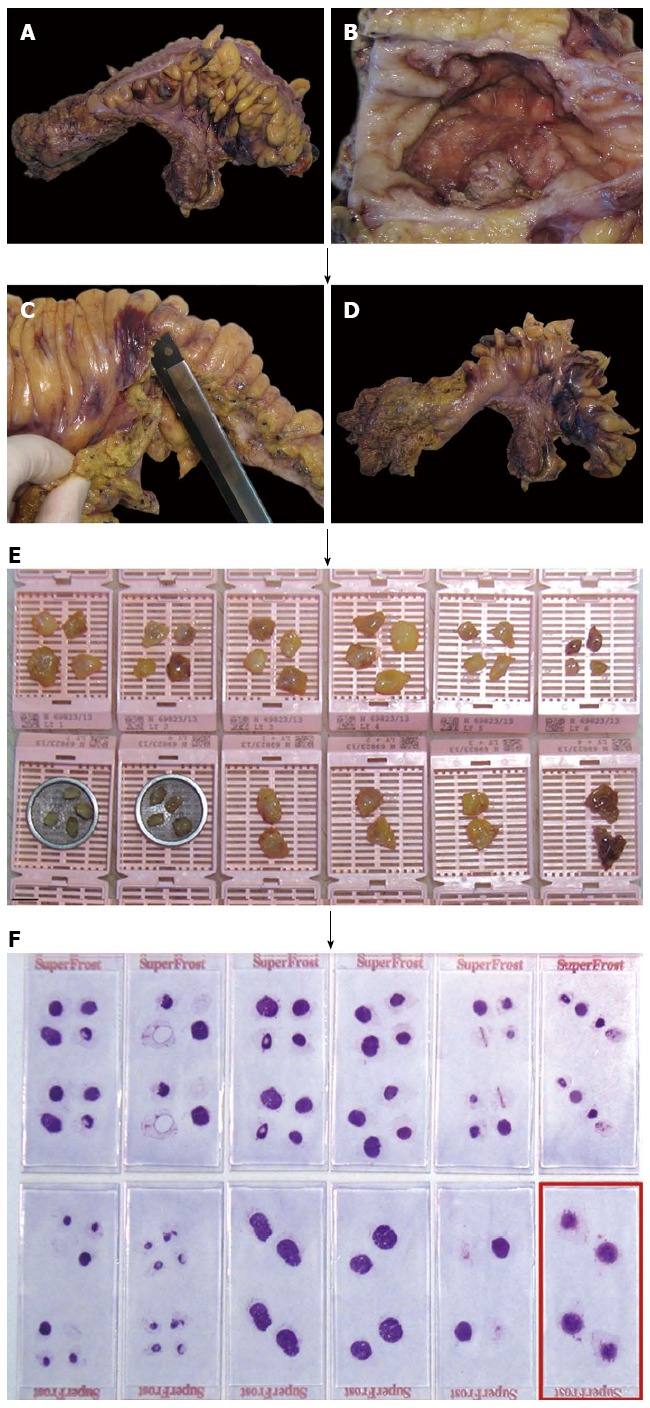
Manual dissection with subsequent histological assessment based on routinely hematoxylin and eosin stained slides is the standard approach in the examination of regional lymph nodes in cancer specimens. A: Rectum cancer specimen of a 56-year-old female; B: Ulcerated primary tumor, measuring 5 cm in largest diameter; C: After preparation of the primary tumor (including the fatty tissue underneath the lesion and the circumferential margin) the remaining perirectal/mesocolic fatty tissue is carefully removed; D: Specimen for subsequent manual lymph node dissection; E: 36 presumed lymph nodes are isolated, of which the largest four are cut into halves and embedded on their own, respectively (lower right); F: 31 lymph nodes are confirmed on hematoxylin and eosin stained slides, one of which with metastatic cancer tissue (encircled).
In this review, we will refer to the controversies mentioned above in detail, focusing on both clinical impact and technical issues. Data for this review were compiled using MEDLINE/PubMed and Thomson Reuters Web of Science®, assessing articles published before August 2013. The search terms included colorectal cancer, colon cancer, rectum cancer, TNM classification, lymph node metastasis, lymph node ratio, extracapsular invasion, sentinel lymph node, immunohistochemistry, and molecular analysis. Only articles published in English were considered.
LYMPH NODE STAGING ACCORDING TO THE AJCC/UICC TNM SYSTEM
Quantitative lymph node evaluation has repeatedly been validated as a powerful prognostic tool in patients with colorectal cancer. In particular, the absolute number of positive nodes has been identified as a highly effective predictor of adverse outcome, as shown by worsening of prognosis with increasing number of lymph nodes involved by cancer[16,17].
Hence, in the AJCC/UICC staging system the prognostic stratification of nodal disease is based on the absolute number of positive lymph nodes. Difficulties, however, arise with respect to changing definitions of lymph nodes as such, involved lymph nodes, and/or tumor deposits (satellites) in different editions[5]. Tumor deposits are macroscopic or microscopic nests or nodules of cancer found in the pericolic and/or perirectal adipose tissue’s lymph drainage area of a primary carcinoma (away from the leading edge of the infiltrating tumor) without histological evidence of residual lymph node in the nodule. They are histologically heterogeneous and may be seen associated with distinct anatomic structures, such as veins[18]. These deposits may represent discontinuous primary tumor spread, venous invasion with extravascular spread, or a totally replaced lymph node (Figure 2A-C).
Figure 2.
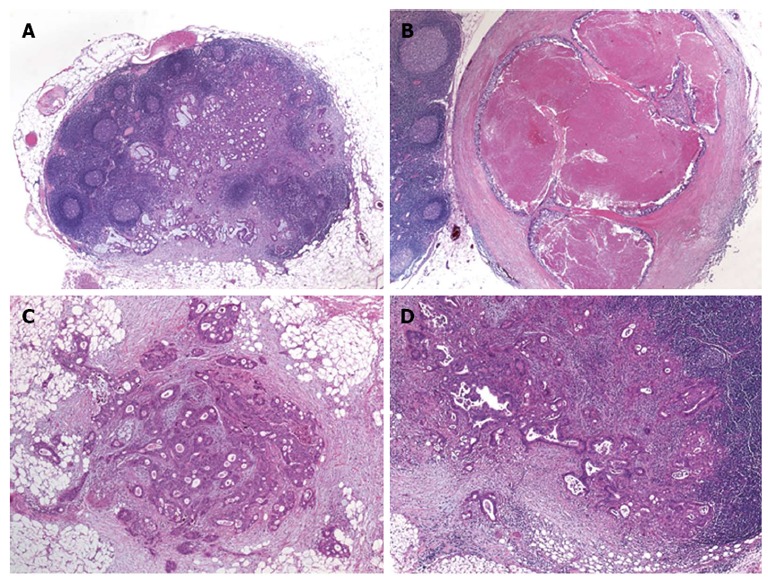
Lymph node metastases and tumor deposits in patients with colorectal cancer. A: Metastatic adenocarcinoma within a mesocolic lymph node [hematoxylin and eosin (HE) original magnification, × 100]; B: Mesocolic lymph node totally replaced by metastatic cancer tissue, note the smooth contour of the lesion (HE, original magnification, × 150); C: Tumor deposit (satellite) within the mesocolic fatty tissue, note the irregular contour of the lesion (HE, original magnification, × 250); D: Mesocolic lymph node metastasis with extracapsular extension of cancer tissue (original magnification, × 250).
The main differences between the different editions of the AJCC/UICC TNM system regarding lymph node staging are as follows: The 5th edition of the TNM system (TNM-5) introduced the 3 mm rule for their classification, providing a tool based exclusively on the size of the lesions[19]. The 6th edition (TNM-6) discarded the size criterion and referred to the contour of the lesions[20]. The 7th edition (TNM-7) focused on the differentiation of lymph node metastases from tumor deposits, including the latter in the pN category (pN1c)[21]. Details are presented in Table 2.
Table 2.
Changing definitions of lymph nodes, involved lymph nodes, and tumor deposits in different editions of the American Joint Committee on Cancer/Union for International Cancer Control tumor node metastasis staging system
| TNM-5 | A tumor nodule greater than 3 mm in diameter in perirectal or pericolic adipose tissue without histological evidence of a residual lymph node in the nodule is classified as regional lymph node metastasis. However, a tumor nodule up to 3 mm in diameter is classified in the T category as discontinuous extension, i.e., T3 |
| TNM-6 | A tumor nodule in the pericolic/perirectal adipose tissue without histological evidence of residual lymph node in the nodule is classified in the pN category as a regional lymph node metastasis if the nodule has the form and smooth contour of a lymph node. If the nodule has an irregular contour, it should be classified in the T category and also coded as V1 (microscopic venous invasion) or V2, if it was grossly evident, because there is a strong likelihood that it represents venous invasion. |
| TNM-7 | Tumor deposits (satellites), i.e., macroscopic or microscopic nests or nodules, in the pericolorectal adipose tissue’s lymph drainage area of a primary carcinoma without histological evidence of residual lymph node in the nodule, may represent discontinuous spread, venous invasion with extravascular spread (V1/2) or a totally replaced lymph node (N1/2). If such deposits are observed with lesions that would otherwise be classified as T1 or T2, then the T classification is not changed, but the nodule(s) is recorded N1c. If a nodule is considered by the pathologist to be a totally replaced lymph node (generally having a smooth contour), it should be recorded as a positive lymph node and not as a satellite, and each nodule should be counted separately as lymph node in the final pN determination. |
TNM: Tumor node metastasis.
Nagtegaal et al[5] have proven lymph node staging according to TNM-5 to be superior to TNM-6, as demonstrated in two independent populations. Therefore, several national guidelines in Europe still refer to TNM-5 for classification. It is simpler, more reproducible, allows for comparison with preoperative imaging, and is effective and accurate[5]. The potential value of TNM-7 remains to be evaluated in larger prospective studies. The fact that all patients with tumor deposits will now be classified in the node-positive group has raised major concerns. This holds true particular for the evaluation of tumor regression and residual tumor foci after neoadjuvant therapy. In the group of patients who did not receive preoperative treatment, however, staging according to TNM-7 appears to be highly prognostic and possibly superior to TNM-5 and TNM-6[5]. The reproducibility of the definitions given in the latest version may, however, be imperfect. In a recent interobserver variability study of lymph nodes and tumor deposits by Rock et al[22], seven gastrointestinal pathologists completely agreed on only 11 of 25 lesions (κ-value 0.48; 95%CI: 0.28-0.67). Top-ranked features for the differentiation of lymph node metastases from tumor deposits included round shape, peripheral lymphocyte rim, peripheral lymphoid follicles, subcapsular sinus, residual lymph node surrounding fibroadipose tissue, and thick capsule. As inconsistency remains even under expert pathologists, it is currently unclear whether the criteria that are available for the distinction of lymph node metastases from tumor deposits are feasible in everyday routine practice performed by general pathologists.
MINIMUM NUMBER OF LYMPH NODES
Adequate assessment of nodal status depends on the total number of retrieved lymph nodes that are available for histological evaluation. A recommendation put forward by Fielding et al[23] stated the ideal minimum to be 12 nodes since below this cut-off value there is a high risk of false-negative reporting of lymph node involvement due to inadequate sampling[16]. This recommendation was adopted by the AJCC/UICC TNM system and has been included in various clinical practice guidelines[2-4,24]. The minimum number of lymph nodes that should be assessed ensures adequate staging, prognostication, and accurate treatment, since affected lymph nodes are the primary determinant for the use of adjuvant chemotherapy.
The variability in the number of retrieved lymph nodes remains to be a major problem in patient management since often the recommended minimum number of 12 lymph nodes is not achieved. This may be due to differences in the extent of surgical lymph node removal, the thoroughness of the pathologist in dissecting the cancer specimen, and/or the actual number of regional lymph nodes that is related to tumor location[25,26]. In rectal cancer, the increasing use of neoadjuvant therapy represents another important factor affecting lymph node yield. Under combined chemo-and radiotherapy regional lymph nodes undergo a process of regression. Thus, the recommended number of 12 lymph nodes was reached in only about 20% of cases in large international trials that investigated the benefit of neoadjuvant therapy in rectal cancer. This observation prompted the question whether the insufficient number of lymph nodes is due to the disappearance of the nodes, or just reflects progressive atrophy and fibrosis with subsequent reduction in lymph node size, rendering them undetectable during routine pathological work-up[27].
Due to the fact that the recommended number of nodes is often not reached by traditional manual dissection new technical methods were introduced to facilitate lymph node harvest in the fatty tissue. These include fat clearing methods, methylene blue-assisted lymph node dissection, as well as acetone elution with subsequent compression of adipose tissue (“acetone compression”). The method of methylene blue-assisted lymph node dissection was introduced in 2007 as a cheap and simple tool[28]. The method is based on ex vivo intraarterial injection of 15-20 mL of methylene blue solution in the fresh or shortly formalin-fixed resection specimen. After fixing overnight lymph nodes are dissected manually. This technique results in dramatically increased lymph node counts compared to conventional dissection. The effect is particularly evident in rectal cancer patients after neoadjuvant therapy and helps to ensure a sufficient lymph node harvest in these patients. However, according to a recently published study[29], the application of this technique does not seem to be associated with an increased detection of lymph node metastases. In this study, comparing methylene blue assisted dissection with standard dissection, neither the rate of nodal positive cases, nor the rate of pN2 cases differed between the two groups. The most probable explanation for this finding is the fact that mostly involved lymph nodes are enlarged and therefore easy to find[30].
The acetone elution and compression method was introduced by Basten et al[31]. After manual dissection for large palpable lymph nodes (usually > 1 cm in diameter) the mesorectal fat is perforated with a needle roller and transferred to acetone. After elution in acetone, tissue samples are mechanically compressed using a manual squeezing machine, as described in detail by Gehoff et al[27]. By this method a reduction of about 90% of mesorectal fat volume is achieved. Specifically, acetone compression facilitates the detection of any tumor deposit in mesorectal and mesenteric fatty tissue and therefore provides a reliable survey of tumor cell deposits including perineural cancer infiltrates, particularly after neoadjuvant therapy[27]. As for methylene blue-assisted lymph node dissection, the total number of harvested lymph nodes markedly increased in that study, the number of positive lymph nodes, however, did not change. From a biological standpoint it is interesting to note that, basically, the number of lymph nodes is independent of pretreatment status[27].
LYMPH NODE RATIO OR ABSOLUTE NUMBER OF INVOLVED LYMPH NODES?
Several studies have demonstrated that simply the analysis of a larger number of lymph nodes results in a survival advantage for patients with stage II and III disease, while the situation for stage I disease is less clear[32-36]. A study by Lykke et al[36] demonstrated that in patients with more than 12 nodes, there was a significantly higher proportion of stage III disease, indicating that stage migration takes place when high numbers of lymph nodes are harvested. To overcome the dependence on the number of harvested lymph nodes, a ratio-based node staging system has been proposed.
The lymph node ratio, defined as the number of positive lymph nodes divided by the total number of retrieved nodes, has gained increasing attention. A large number of studies showed that the prognostic significance of lymph node ratio is superior to that of the absolute number of involved lymph nodes[6,8,36-44]. Lymph node ratio was identified as an independent predictor of disease-free survival, overall survival, and cancer-specific survival in stage III disease. Notably, lymph node ratio remains to be an independent prognosticator even after neoadjuvant therapy, despite reduction of the absolute number of retrieved nodes[45]. The lymph node ratio may thus improve TNM-based prognostic stratification and may help to identify patients at high risk of disease recurrence and/or progression.
Problems, however, remain, particularly as different cut-off values were applied in the studies that identified lymph node ratio as promising tool. Currently, we do not know which cut-off value is ideal and whether this value may be the best for both colon and rectum cancer. Future prospective studies, applying a data-driven approach are urgently needed to accurately define these cut-off values, as obviously “not one size fits all”[40].
Although the concept of lymph node ratio was developed to generate a prognostic marker that is independent from the number of examined nodes data are still conflicting in this regard. According to Chen et al[43], lymph node ratio independently estimates survival, irrespective of the number of nodes examined. In the study by Berger et al[38], lymph node ratio was a significant parameter when 10 or more lymph nodes were removed, but not for patients with less than 10 lymph nodes.
EXTRACAPSULAR LYMPH NODE INVASION
Extracapsular lymph node invasion refers to the extension of cancer cells through the nodal capsule into the perinodal fatty tissue (Figure 2D)[46]. This phenomenon has gained considerable attention as prognostic variable in several solid organ tumors, particularly in cancers originating from breast and head and neck region as well as in several gastrointestinal malignancies.
In colorectal cancer, extracapsular invasion has been observed in 18% to 68% of stage III tumors[10-13,46]. According to Komuta et al[10], extracapsular invasion occurs more likely in lymph nodes that are occupied for more than 50% by cancer cells, compared to lymph nodes with less than 50% occupation. Its occurrence has been related to high pT-classification, high number of involved nodes, and presence of positive distant lymph nodes, which allows the conclusion that extracapsular invasion is more likely to be found in advanced tumor stage[11-13].
The ability of metastatic nodes to recruit degradation factors that permit cancer cells to break through the lymph node capsule reflects the invasiveness and aggressiveness of the primary tumor, even in an immunologically hostile environment[46]. Thus, patients with extracapsular invasion at metastatic sites are at particularly high risk to develop disease progression and distant cancer spread[12,13]. In particular, survival and recurrence rates of patients with extracapsular invasion are significantly worse than those of patients without, and extracapsular invasion has been identified as independent predictor of disease-free and overall survival in patients with node positive cancers[11,12,47,48].
Overall, the detection and, possibly, quantification of extracapsular invasion may help to individualize post-operative treatment strategies by identification of a subgroup of patients with significantly poorer long-term survival and poorer local control who might benefit from intensified adjuvant therapy[46].
SENTINEL LYMPH NODE BIOPSY
The sentinel lymph node, defined as the first lymphatic station within a given lymph drainage area, is considered to be of eminent importance in oncologic practice. Sentinel node detection may be accomplished by injection of blue dye (e.g., methylene blue) or radiotracers near to the tumor. Afterwards the surgeon detects the node by visual inspection or by use of gamma probe or Geiger counter. In clinical practice, sentinel lymph node biopsy has been found to be highly effective in correctly predicting the nodal status in malignant melanoma and breast cancer[49]. Commonly, a frozen section procedure is employed so if neoplasia is detected further lymph node dissection may be performed. If, however, the sentinel node is free of cancer the extent of operation may be kept to a minimum.
Within the last two decades, several investigators aimed to enlarge the field of application and have evaluated sentinel lymph node biopsy in various malignancies[50]. In colorectal cancer, the potential benefit of sentinel lymph node biopsy is different from that of malignant melanoma and breast cancer. Here, the method does not intend to reduce the extent of surgery but aims to identify conditions that might lead to more extensive surgical lymph node dissection. Another purpose is to establish more accurate lymph node staging in order to identify patients at risk for disease recurrence and/or progression[51].
According to a recent meta-analysis[52], the pooled sentinel node identification rate is approximately 90% in patients with colorectal cancer, with a significantly higher rate in studies including more than 100 patients or studies using an ex vivo approach. The pooled sensitivity of the procedure is approximately 70%. Subgroups with significantly higher sensitivity could be identified. These include individuals with ≥ 4 sentinel nodes identified (vs individuals < 4 nodes), colonic location (vs rectal location), and early, i.e., pT1/2 carcinomas (vs advanced, i.e., pT3/4 carcinomas).
How sentinel lymph node biopsy may be successfully incorporated in routine practice has recently been illustrated in a study by Saha et al[53]. The authors investigated 192 patients undergoing surgery for colon cancer and identified aberrant drainage, i.e., drainage outside the standard resection margin requiring change of the extent of operation, in 22% of patients. Notably, nodal positivity was higher in patients undergoing change of operation (62%) compared to those undergoing only standard oncologic resection (43%).
Major drawbacks remain to be the still imperfect detection rate and the comparably low sensitivity for the identification of nodal disease. The detection rate is significantly influenced by several patient-and disease-specific factors, the most important of which being body mass index, center experience, and learning curve[49]. The considerably high false-negative rate to identify node-positive patients may be explained by aberrant drainage sites and the presence of skip lesions. It is known that skip lesions occur when lymphatics are obstructed by tumor. Retter et al[54] showed that in 63% of their false negative tumors, lymphatic and venous invasion by cancer cells was present.
The extent of the pathological work-up is another major factor with significant impact on the performance and clinical significance of the sentinel node biopsy concept. According to the meta-analysis cited above, adding step sectioning and immunohistochemistry, e.g., using antibodies directed against pankeratin (Figure 3), to the pathological work-up resulted in a mean upstaging in 18.9% (range 0%-50%). True upstaging defined as micrometastases [pN1(mi)] rather than isolated tumor cells [pN0(i+)] occurred in 7.7%[52]. The optimal technical method how sentinel lymph nodes should be evaluated still has to be defined. Several papers have addressed this topic, the three most relevant will be referred to in detail.
Figure 3.
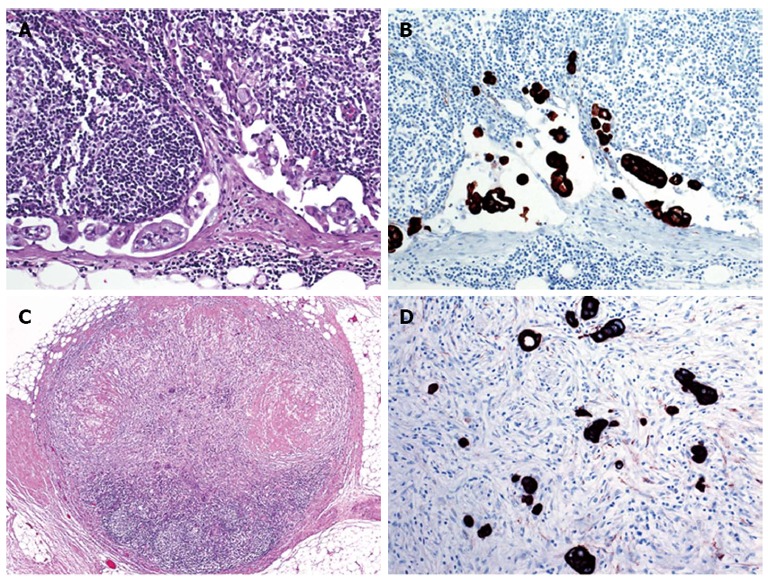
Value of immunohistochemistry in the evaluation of lymph nodes from patients with colorectal cancer. A: Micrometastasis in the subcapsular sinus of a mesocolic sentinel node evaluated by standard hematoxylin and eosin (HE) staining (original magnification, × 400); B: Micrometastasis in the subcapsular sinus of a mesocolic sentinel node evaluated by immunohistochemistry using an antibody preparation directed against pankeratin (serial section to A, original magnification, × 400); C: Atrophic perirectal lymph node with marked fibrosis after neoadjuvant treatment (original magnification, × 100); D: Identification of residual cancer cells by pankeratin immunostaining (original magnification, × 400).
In the study by Bembenek et al[49], a total of 141 of 186 patients classified as nodal negative by routine HE staining underwent step sectioning and immunohistochemical analysis for pankeratin (MNF116) of their sentinel lymph nodes. Thirty of these patients revealed micrometastases (n = 7) or isolated tumor cells (n = 23), resulting in an overall upstaging rate of 30 of 141 (21.3%). In the clinically important subgroup of stage II patients, upstaging occurred in 24.2% (21 of 91).
In the study by van der Zaag et al[51], three serial sections (cut at 500 μm intervals) of all 908 lymph nodes from 58 patients with pN0 carcinomas (according to standard evaluation on HE stained slides) were examined with three different antibodies [directed against pankeratin (Cam5.2), keratin 20, and Ber-EP4]. The examination revealed occult tumor cells in 33% (19 of 58) of histologically pN0 patients (12% micrometastases and 21% isolated tumor cells). Occult tumor cells were predominantly found in sentinel nodes with an overall sensitivity of sentinel mapping for occult tumor cells of 88%.
In the study by Märkl et al[55], applying methylene blue injection in an ex vivo approach lymph node metastases were found in 20 of 47 (43%) cases with skip metastases occurring in four of them. Performing three additional HE step sections and immunohistochemical staining for pankeratin (MNF116) in sentinel lymph nodes and all other lymph nodes, resulted in true upstaging (N0N1mi) in 1 of 23 cases (4%).
MOLECULAR ANALYSIS OF LYMPH NODES - A FEASIBLE APPROACH?
The identification of lymph node involvement is the most important factor to predict outcome and qualify affected patients for adjuvant chemotherapy[55]. Manual dissection of fatty tissue and histopathology based on HE stained sections remain to be the standard approach in pathological lymph node evaluation.
This may, however, lead to underestimation of disease and understaging of patients. About 30% of the patients with histopathology-negative lymph nodes (AJCC/UICC TNM stages I and II) develop recurrent and/or progressive disease, likely associated with undetected metastatic deposits[15,56-59]. As shown above, the use of additional step sections and immunohistochemistry may improve the identification of positive lymph nodes. Of note, many patients initially staged lymph node-negative, who experienced disease recurrence had isolated tumor cells and/or micrometastases after advanced evaluation[60]. A major limitation of the histological examination is the fact that only a small portion of the lymph node, usually the section(s) with the largest cut surface, is assessed leaving most parts of the nodes uninspected[61].
As current techniques for nodal examination may be inadequate for the detection of micrometastases and/or isolated tumor cells, molecular analysis of lymph node tissue has been introduced as additional tool in the work-up of cancer patients. The identification of minimal disease in lymph nodes by molecular techniques may help to identify patients at high risk for recurrence and/or progression, who could benefit from adjuvant therapy[62]. The following features are relevant: (1) no expression of the respective marker in immune cells; (2) no or weak downregulation in tumors compared to normal tissue; and (3) relatively high and constant expression in tumor tissue irrespective of tumor stage[63]. Several molecular markers have been applied (Table 3). In the following we will refer to some of them in detail.
Table 3.
Markers for molecular lymph node staging
| Keratin 20 |
| Keratin 19 (including one-step nucleic acid amplification technique) |
| Mucin apoprotein 2 |
| Guanylyl cylase C |
| Carcinoembryonic antigen |
| CEACAM6 |
| CEACAM1-S |
| CEACAM1-L |
| CEACAM7-1 |
| CEACAM7-2 |
| c-Met |
| K-ras mutation |
| Estrogen receptor promoter methylation |
Keratin 20 (K20) is constitutively expressed in intestinal epithelia and is the most important keratin subtype expressed in colorectal cancer. It can be found in more than 90% of primary tumors. Immunoreactivity in metastatic tissues is known to match well with that of corresponding primary tumors, with high concordance for lymph node and distant metastases, respectively[64]. The significance of quantitative real-time polymerase chain reaction (RT-PCR) for the detection of K20 mRNA in regional lymph nodes of cancer patients has been investigated by several groups, mainly in sentinel node biopsies[15,57,65-71]. In general, these studies demonstrated a higher sensitivity of molecular analysis compared to standard evaluation based on HE stained slides and also compared to advanced evaluation applying immunohistochemistry.
MUC2 apoprotein, which is secreted from non-neoplastic intestinal goblet cells and is expressed in the majority of colorectal cancers, has been introduced as another promising marker[15,63,72,73]. Some groups investigated carcinoembryonic antigen[63,68,69,72,74], while others referred to guanylyl cylase C (GCC)[58,68,75]. GCC is a receptor for bacterial enterotoxins and the paracrine ligands guanylin and uroguanylin and is expressed selectively by intestinal epithelium. Comparable to mucin apoprotein 2 (MUC2), the expression of GCC is preserved throughout the transition from adenoma to carcinoma in colorectal tissues[56,58]. Most recently, so-called one-step nucleic acid amplification (OSNA) has been introduced to detect keratin 19 (K19) mRNA as a surrogate for lymph node metastasis. K19 is expressed in many types of cancer, albeit in varying frequencies. OSNA is based on reverse transcription-loop-mediated isothermal amplification to amplify K19 mRNA[59,61,76].
All these techniques allow the examination of the entire lymph node, thereby overcoming the problem of sampling bias due to insufficient analysis of material in the standard histological approach. This may lead to improved staging and better selection of patients for adjuvant chemotherapy. More importantly the molecular detection of tumor cells in regional lymph nodes has been associated with disease recurrence and poor survival in node-negative colorectal cancer[14,77].
Problems, however, remain. The value of quantitative RT-PCR assays for the detection of occult tumor cells in regional lymph nodes relies on the balance between sensitivity and specificity in order to minimize the occurrence of false-positive or false-negative results[78]. None of the markers are really specific. K19 has been used as a molecular marker in a variety of studies dealing with several types of cancer, including colorectal cancer. Doubt has arisen about the tissue specificity of K19 gene expression. Already in 1996, Gunn et al[79] noted K19 gene expression in 34 of 40 lymph nodes from patients who underwent bowel resection for benign disease. The reasons for the observed false-positivity rate are not entirely clear. In addition to simple contamination or dissemination of tumor cells and/or tumor cell fragments via the lymphatics during the procedure, amplification of K19 pseudogenes may play a role[78]. Finally, Bustin et al[68] detected K20, carcinoembryonic antigen, and GCC mRNA in 47%, 89% and 13% of 149 lymph nodes, respectively from patients with benign disease indicating that K19 is not the only marker for which specificity problems remain to be solved.
Nevertheless, the molecular approach has opened new options concerning the diagnosis of isolated tumor cells and micrometastases in patients with histopathology-negative lymph nodes[57]. Benefits of the molecular approach have to be weighed against potential drawbacks. A major reason for controversy is the lack of standardization of molecular analyses hampering comparison of different studies as well as inclusion of molecular techniques into routine practice[57]. According to current practice guidelines, AJCC/UICC stage III patients receive adjuvant treatment. This strategy results in significantly improved outcome when nodal disease is proven histologically. However, it is currently not entirely clear whether the patients with nodal disease proven on a molecular level experience similar benefits if chemotherapy is given.
CONCLUSION
Lymph node staging is a major prognostic factor in colorectal cancer and remains to be the most important criterion to select patients for adjuvant treatment. Changing definition of lymph nodes, involved lymph nodes, and tumor deposits in different editions of the AJCC/UICC TNM system have influenced the significance of lymph node staging in the past. The standard approach for lymph node evaluation is based on manual dissection and histological evaluation of HE stained slides. Methylene blue injection and fat clearing methods increase lymph node harvest in cancer specimens. Adding step sectioning and immunohistochemistry to the pathological work-up may result in higher accuracy of histological diagnosis. The clinical value of more recent techniques, such as sentinel lymph node biopsy and molecular analysis of lymph nodes tissue still remains to be defined.
Footnotes
P- Reviewers: Milone M, Manfredi S, Takao S S- Editor: Gou SX L- Editor: A E- Editor: Zhang DN
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 2.Washington MK. Colorectal carcinoma: selected issues in pathologic examination and staging and determination of prognostic factors. Arch Pathol Lab Med. 2008;132:1600–1607. doi: 10.5858/2008-132-1600-CCSIIP. [DOI] [PubMed] [Google Scholar]
- 3.Benson AB, Arnoletti JP, Bekaii-Saab T, Chan E, Chen YJ, Choti MA, Cooper HS, Dilawari RA, Engstrom PF, Enzinger PC, et al. Colon cancer. J Natl Compr Canc Netw. 2011;9:1238–1290. doi: 10.6004/jnccn.2011.0104. [DOI] [PubMed] [Google Scholar]
- 4.Benson AB, Bekaii-Saab T, Chan E, Chen YJ, Choti MA, Cooper HS, Engstrom PF, Enzinger PC, Fakih MG, Fuchs CS, et al. Rectal cancer. J Natl Compr Canc Netw. 2012;10:1528–1564. doi: 10.6004/jnccn.2012.0158. [DOI] [PubMed] [Google Scholar]
- 5.Nagtegaal ID, Tot T, Jayne DG, McShane P, Nihlberg A, Marshall HC, Påhlman L, Brown JM, Guillou PJ, Quirke P. Lymph nodes, tumor deposits, and TNM: are we getting better? J Clin Oncol. 2011;29:2487–2492. doi: 10.1200/JCO.2011.34.6429. [DOI] [PubMed] [Google Scholar]
- 6.Sjo OH, Merok MA, Svindland A, Nesbakken A. Prognostic impact of lymph node harvest and lymph node ratio in patients with colon cancer. Dis Colon Rectum. 2012;55:307–315. doi: 10.1097/DCR.0b013e3182423f62. [DOI] [PubMed] [Google Scholar]
- 7.Akagi Y, Adachi Y, Kinugasa T, Oka Y, Mizobe T, Shirouzu K. Lymph node evaluation and survival in colorectal cancer: review of population-based, prospective studies. Anticancer Res. 2013;33:2839–2847. [PubMed] [Google Scholar]
- 8.Wang LP, Wang HY, Cao R, Zhu C, Wu XZ. Proposal of a new classification for stage III colorectal cancer based on the number and ratio of metastatic lymph nodes. World J Surg. 2013;37:1094–1102. doi: 10.1007/s00268-013-1940-x. [DOI] [PubMed] [Google Scholar]
- 9.Schiffmann L, Eiken AK, Gock M, Klar E. Is the lymph node ratio superior to the Union for International Cancer Control (UICC) TNM system in prognosis of colon cancer? World J Surg Oncol. 2013;11:79. doi: 10.1186/1477-7819-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Komuta K, Okudaira S, Haraguchi M, Furui J, Kanematsu T. Identification of extracapsular invasion of the metastatic lymph nodes as a useful prognostic sign in patients with resectable colorectal cancer. Dis Colon Rectum. 2001;44:1838–1844. doi: 10.1007/BF02234464. [DOI] [PubMed] [Google Scholar]
- 11.Heide J, Krüll A, Berger J. Extracapsular spread of nodal metastasis as a prognostic factor in rectal cancer. Int J Radiat Oncol Biol Phys. 2004;58:773–778. doi: 10.1016/S0360-3016(03)01616-X. [DOI] [PubMed] [Google Scholar]
- 12.Fujii T, Tabe Y, Yajima R, Yamaguchi S, Tsutsumi S, Asao T, Kuwano H. Extracapsular invasion as a risk factor for disease recurrence in colorectal cancer. World J Gastroenterol. 2011;17:2003–2006. doi: 10.3748/wjg.v17.i15.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fujii T, Tabe Y, Yajima R, Yamaguchi S, Tsutsumi S, Asao T, Kuwano H. Process of distant lymph node metastasis in colorectal carcinoma: implication of extracapsular invasion of lymph node metastasis. BMC Cancer. 2011;11:216. doi: 10.1186/1471-2407-11-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahbari NN, Bork U, Motschall E, Thorlund K, Büchler MW, Koch M, Weitz J. Molecular detection of tumor cells in regional lymph nodes is associated with disease recurrence and poor survival in node-negative colorectal cancer: a systematic review and meta-analysis. J Clin Oncol. 2012;30:60–70. doi: 10.1200/JCO.2011.36.9504. [DOI] [PubMed] [Google Scholar]
- 15.Nordgård O, Oltedal S, Kørner H, Aasprong OG, Tjensvoll K, Gilje B, Heikkilä R. Quantitative RT-PCR detection of tumor cells in sentinel lymph nodes isolated from colon cancer patients with an ex vivo approach. Ann Surg. 2009;249:602–607. doi: 10.1097/SLA.0b013e31819ec923. [DOI] [PubMed] [Google Scholar]
- 16.Vather R, Sammour T, Kahokehr A, Connolly A, Hill A. Quantitative lymph node evaluation as an independent marker of long-term prognosis in stage III rectal cancer. ANZ J Surg. 2011;81:883–888. doi: 10.1111/j.1445-2197.2010.05595.x. [DOI] [PubMed] [Google Scholar]
- 17.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, Editors . AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010. [Google Scholar]
- 18.Puppa G, Sonzogni A, Colombari R, Pelosi G. TNM staging system of colorectal carcinoma: a critical appraisal of challenging issues. Arch Pathol Lab Med. 2010;134:837–852. doi: 10.5858/134.6.837. [DOI] [PubMed] [Google Scholar]
- 19.Sobin LH, Wittekind C, editors . International Union Against Cancer. TNM Classification of Malignant Tumors. 5th ed. New York: Wiley-Liss; 1997. [Google Scholar]
- 20.Sobin LH, Wittekind C, editors . International Union Against Cancer. TNM Classification of Malignant Tumors. 6th ed. Hoboken: John Wiley & Sons; 2002. [Google Scholar]
- 21.Sobin LH, Gospodarowicz MK, Wittekind C, editors . International Union Against Cancer. TNM Classification of Malignant Tumors. 7th ed. Oxford: Wiley-Blackwell; 2009. [Google Scholar]
- 22.Rock JB, Washington MK, Adsay NV, Greenson JK, Montgomery EA, Robert ME, Yantiss RK, Lehman AM, Frankel WL. Debating Deposits: An Interobserver Variability Study of Lymph Nodes and Pericolonic Tumor Deposits in Colonic Adenocarcinoma. Arch Pathol Lab Med. 2013:Epub ahead of print. doi: 10.5858/arpa.2013-0166-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fielding LP, Arsenault PA, Chapuis PH, Dent O, Gathright B, Hardcastle JD, Hermanek P, Jass JR, Newland RC. Clinicopathological staging for colorectal cancer: an International Documentation System (IDS) and an International Comprehensive Anatomical Terminology (ICAT) J Gastroenterol Hepatol. 1991;6:325–344. doi: 10.1111/j.1440-1746.1991.tb00867.x. [DOI] [PubMed] [Google Scholar]
- 24.Jass JR, O’Brien J, Riddell RH, Snover DC. Recommendations for the reporting of surgically resected specimens of colorectal carcinoma: Association of Directors of Anatomic and Surgical Pathology. Am J Clin Pathol. 2008;129:13–23. doi: 10.1309/6UHNC7MAD8KWNAWC. [DOI] [PubMed] [Google Scholar]
- 25.Huh JW, Kim CH, Kim HR, Kim YJ. Factors predicting oncologic outcomes in patients with fewer than 12 lymph nodes retrieved after curative resection for colon cancer. J Surg Oncol. 2012;105:125–129. doi: 10.1002/jso.22072. [DOI] [PubMed] [Google Scholar]
- 26.Bilimoria KY, Palis B, Stewart AK, Bentrem DJ, Freel AC, Sigurdson ER, Talamonti MS, Ko CY. Impact of tumor location on nodal evaluation for colon cancer. Dis Colon Rectum. 2008;51:154–161. doi: 10.1007/s10350-007-9114-2. [DOI] [PubMed] [Google Scholar]
- 27.Gehoff A, Basten O, Sprenger T, Conradi LC, Bismarck C, Bandorski D, Merkelbach-Bruse S, Schneider-Stock R, Stoehr R, Wirtz RM, et al. Optimal lymph node harvest in rectal cancer (UICC stages II and III) after preoperative 5-FU-based radiochemotherapy. Acetone compression is a new and highly efficient method. Am J Surg Pathol. 2012;36:202–213. doi: 10.1097/PAS.0b013e31823fa35b. [DOI] [PubMed] [Google Scholar]
- 28.Märkl B, Kerwel TG, Wagner T, Anthuber M, Arnholdt HM. Methylene blue injection into the rectal artery as a simple method to improve lymph node harvest in rectal cancer. Mod Pathol. 2007;20:797–801. doi: 10.1038/modpathol.3800824. [DOI] [PubMed] [Google Scholar]
- 29.Märkl B, Schaller T, Krammer I, Cacchi C, Arnholdt HM, Schenkirsch G, Kretsinger H, Anthuber M, Spatz H. Methylene blue-assisted lymph node dissection technique is not associated with an increased detection of lymph node metastases in colorectal cancer. Mod Pathol. 2013;26:1246–1254. doi: 10.1038/modpathol.2013.61. [DOI] [PubMed] [Google Scholar]
- 30.Märkl B, Rößle J, Arnholdt HM, Schaller T, Krammer I, Cacchi C, Jähnig H, Schenkirsch G, Spatz H, Anthuber M. The clinical significance of lymph node size in colon cancer. Mod Pathol. 2012;25:1413–1422. doi: 10.1038/modpathol.2012.92. [DOI] [PubMed] [Google Scholar]
- 31.Basten O, Bandorski D, Bismarck C, Neumann K, Fisseler-Eckhoff A. [Acetone compression. A fast, standardized method to investigate gastrointestinal lymph nodes] Pathologe. 2010;31:218–224. doi: 10.1007/s00292-009-1256-7. [DOI] [PubMed] [Google Scholar]
- 32.Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99:433–441. doi: 10.1093/jnci/djk092. [DOI] [PubMed] [Google Scholar]
- 33.Chen HH, Chakravarty K D, Wang JY, Changchien CR, Tang R. Pathological examination of 12 regional lymph nodes and long-term survival in stages I-III colon cancer patients: an analysis of 2,056 consecutive patients in two branches of same institution. Int J Colorectal Dis. 2010;25:1333–1341. doi: 10.1007/s00384-010-1020-8. [DOI] [PubMed] [Google Scholar]
- 34.Johnson PM, Porter GA, Ricciardi R, Baxter NN. Increasing negative lymph node count is independently associated with improved long-term survival in stage IIIB and IIIC colon cancer. J Clin Oncol. 2006;24:3570–3575. doi: 10.1200/JCO.2006.06.8866. [DOI] [PubMed] [Google Scholar]
- 35.Norwood MG, Sutton AJ, West K, Sharpe DP, Hemingway D, Kelly MJ. Lymph node retrieval in colorectal cancer resection specimens: national standards are achievable, and low numbers are associated with reduced survival. Colorectal Dis. 2010;12:304–309. doi: 10.1111/j.1463-1318.2009.01788.x. [DOI] [PubMed] [Google Scholar]
- 36.Lykke J, Roikjaer O, Jess P. The relation between lymph node status and survival in Stage I-III colon cancer: results from a prospective nationwide cohort study. Colorectal Dis. 2013;15:559–565. doi: 10.1111/codi.12059. [DOI] [PubMed] [Google Scholar]
- 37.Vaccaro CA, Im V, Rossi GL, Quintana GO, Benati ML, Perez de Arenaza D, Bonadeo FA. Lymph node ratio as prognosis factor for colon cancer treated by colorectal surgeons. Dis Colon Rectum. 2009;52:1244–1250. doi: 10.1007/DCR.0b013e3181a65f0b. [DOI] [PubMed] [Google Scholar]
- 38.Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol. 2005;23:8706–8712. doi: 10.1200/JCO.2005.02.8852. [DOI] [PubMed] [Google Scholar]
- 39.Del Rio P, Dell’Abate P, Papadia C, Angeletta A, Montana C, Iapichino G, Sianesi M. Impact of lymph node ratio in the colorectal cancer staging system. Ann Ital Chir. 2012;83:399–403; discussion 403-404. [PubMed] [Google Scholar]
- 40.Medani M, Kelly N, Samaha G, Duff G, Healy V, Mulcahy E, Condon E, Waldron D, Saunders J, Coffey JC. An appraisal of lymph node ratio in colon and rectal cancer: not one size fits all. Int J Colorectal Dis. 2013;28:1377–1384. doi: 10.1007/s00384-013-1707-8. [DOI] [PubMed] [Google Scholar]
- 41.Tayyab M, Sharma A, Macdonald AW, Gunn J, Hartley JE, Monson JR. Prognostic significance of lymph node ratio in patients undergoing abdominoperineal resection of rectum. Langenbecks Arch Surg. 2012;397:1053–1057. doi: 10.1007/s00423-012-0986-9. [DOI] [PubMed] [Google Scholar]
- 42.Thomas M, Biswas S, Mohamed F, Chandrakumaran K, Jha M, Wilson R. Dukes C colorectal cancer: is the metastatic lymph node ratio important? Int J Colorectal Dis. 2012;27:309–317. doi: 10.1007/s00384-011-1340-3. [DOI] [PubMed] [Google Scholar]
- 43.Chen SL, Steele SR, Eberhardt J, Zhu K, Bilchik A, Stojadinovic A. Lymph node ratio as a quality and prognostic indicator in stage III colon cancer. Ann Surg. 2011;253:82–87. doi: 10.1097/SLA.0b013e3181ffa780. [DOI] [PubMed] [Google Scholar]
- 44.Lu YJ, Lin PC, Lin CC, Wang HS, Yang SH, Jiang JK, Lan YT, Lin TC, Liang WY, Chen WS, et al. The impact of the lymph node ratio is greater than traditional lymph node status in stage III colorectal cancer patients. World J Surg. 2013;37:1927–1933. doi: 10.1007/s00268-013-2051-4. [DOI] [PubMed] [Google Scholar]
- 45.Kang J, Hur H, Min BS, Lee KY, Kim NK. Prognostic impact of the lymph node ratio in rectal cancer patients who underwent preoperative chemoradiation. J Surg Oncol. 2011;104:53–58. doi: 10.1002/jso.21913. [DOI] [PubMed] [Google Scholar]
- 46.Wind J, Lagarde SM, Ten Kate FJ, Ubbink DT, Bemelman WA, van Lanschot JJ. A systematic review on the significance of extracapsular lymph node involvement in gastrointestinal malignancies. Eur J Surg Oncol. 2007;33:401–408. doi: 10.1016/j.ejso.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 47.Lupattelli M, Maranzano E, Bellavita R, Tarducci R, Latini R, Castagnoli P, Bufalari A, Corgna E, Pinaglia D, Rossetti R, et al. Adjuvant radiochemotherapy in high-risk rectal cancer results of a prospective non-randomized study. Tumori. 2001;87:239–247. doi: 10.1177/030089160108700406. [DOI] [PubMed] [Google Scholar]
- 48.Al Sahaf O, Myers E, Jawad M, Browne TJ, Winter DC, Redmond HP. The prognostic significance of extramural deposits and extracapsular lymph node invasion in colon cancer. Dis Colon Rectum. 2011;54:982–988. doi: 10.1097/DCR.0b013e31821c4944. [DOI] [PubMed] [Google Scholar]
- 49.Bembenek AE, Rosenberg R, Wagler E, Gretschel S, Sendler A, Siewert JR, Nährig J, Witzigmann H, Hauss J, Knorr C, et al. Sentinel lymph node biopsy in colon cancer: a prospective multicenter trial. Ann Surg. 2007;245:858–863. doi: 10.1097/01.sla.0000250428.46656.7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kitagawa Y, Ohgami M, Fujii H, Mukai M, Kubota T, Ando N, Watanabe M, Otani Y, Ozawa S, Hasegawa H, et al. Laparoscopic detection of sentinel lymph nodes in gastrointestinal cancer: a novel and minimally invasive approach. Ann Surg Oncol. 2001;8:86S–89S. [PubMed] [Google Scholar]
- 51.van der Zaag ES, Kooij N, van de Vijver MJ, Bemelman WA, Peters HM, Buskens CJ. Diagnosing occult tumour cells and their predictive value in sentinel nodes of histologically negative patients with colorectal cancer. Eur J Surg Oncol. 2010;36:350–357. doi: 10.1016/j.ejso.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 52.van der Zaag ES, Bouma WH, Tanis PJ, Ubbink DT, Bemelman WA, Buskens CJ. Systematic review of sentinel lymph node mapping procedure in colorectal cancer. Ann Surg Oncol. 2012;19:3449–3459. doi: 10.1245/s10434-012-2417-0. [DOI] [PubMed] [Google Scholar]
- 53.Saha S, Johnston G, Korant A, Shaik M, Kanaan M, Johnston R, Ganatra B, Kaushal S, Desai D, Mannam S. Aberrant drainage of sentinel lymph nodes in colon cancer and its impact on staging and extent of operation. Am J Surg. 2013;205:302–305; discussion 302-305. doi: 10.1016/j.amjsurg.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 54.Retter SM, Herrmann G, Schiedeck TH. Clinical value of sentinel node mapping in carcinoma of the colon. Colorectal Dis. 2011;13:855–859. doi: 10.1111/j.1463-1318.2010.02293.x. [DOI] [PubMed] [Google Scholar]
- 55.Märkl B, Arnholdt HM, Jähnig H, Spatz H, Anthuber M, Oruzio DV, Kerwel TG. A new concept for the role of ex vivo sentinel lymph nodes in node-negative colorectal cancer. Ann Surg Oncol. 2010;17:2647–2655. doi: 10.1245/s10434-010-1030-3. [DOI] [PubMed] [Google Scholar]
- 56.Hyslop T, Waldman SA. Molecular staging of node negative patients with colorectal cancer. J Cancer. 2013;4:193–199. doi: 10.7150/jca.5830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lotspeich E, Schoene M, Gerngross H, Schmidt R, Steinmann R, Ramadani M, Gansauge S. Detection of disseminated tumor cells in the lymph nodes of colorectal cancer patients using a real-time polymerase chain reaction assay. Langenbecks Arch Surg. 2007;392:559–566. doi: 10.1007/s00423-007-0184-3. [DOI] [PubMed] [Google Scholar]
- 58.Haince JF, Houde M, Beaudry G, L’espérance S, Garon G, Desaulniers M, Hafer LJ, Heald JI, Lyle S, Grossman SR, et al. Comparison of histopathology and RT-qPCR amplification of guanylyl cyclase C for detection of colon cancer metastases in lymph nodes. J Clin Pathol. 2010;63:530–537. doi: 10.1136/jcp.2009.072983. [DOI] [PubMed] [Google Scholar]
- 59.Croner RS, Schellerer V, Demund H, Schildberg C, Papadopulos T, Naschberger E, Stürzl M, Matzel KE, Hohenberger W, Schlabrakowski A. One step nucleic acid amplification (OSNA) - a new method for lymph node staging in colorectal carcinomas. J Transl Med. 2010;8:83. doi: 10.1186/1479-5876-8-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Iddings D, Ahmad A, Elashoff D, Bilchik A. The prognostic effect of micrometastases in previously staged lymph node negative (N0) colorectal carcinoma: a meta-analysis. Ann Surg Oncol. 2006;13:1386–1392. doi: 10.1245/s10434-006-9120-y. [DOI] [PubMed] [Google Scholar]
- 61.Yamamoto H, Sekimoto M, Oya M, Yamamoto N, Konishi F, Sasaki J, Yamada S, Taniyama K, Tominaga H, Tsujimoto M, et al. OSNA-based novel molecular testing for lymph node metastases in colorectal cancer patients: results from a multicenter clinical performance study in Japan. Ann Surg Oncol. 2011;18:1891–1898. doi: 10.1245/s10434-010-1539-5. [DOI] [PubMed] [Google Scholar]
- 62.Koyanagi K, Bilchik AJ, Saha S, Turner RR, Wiese D, McCarter M, Shen P, Deacon L, Elashoff D, Hoon DS. Prognostic relevance of occult nodal micrometastases and circulating tumor cells in colorectal cancer in a prospective multicenter trial. Clin Cancer Res. 2008;14:7391–7396. doi: 10.1158/1078-0432.CCR-08-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ohlsson L, Hammarström ML, Israelsson A, Näslund L, Oberg A, Lindmark G, Hammarström S. Biomarker selection for detection of occult tumour cells in lymph nodes of colorectal cancer patients using real-time quantitative RT-PCR. Br J Cancer. 2006;95:218–225. doi: 10.1038/sj.bjc.6603206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harbaum L, Pollheimer MJ, Kornprat P, Lindtner RA, Schlemmer A, Rehak P, Langner C. Keratin 20 - a diagnostic and prognostic marker in colorectal cancer? Histol Histopathol. 2012;27:347–356. doi: 10.14670/HH-27.347. [DOI] [PubMed] [Google Scholar]
- 65.Nordgård O, Oltedal S, Kørner H, Aasprong OG, Tjensvoll K, Gilje B, Heikkilä R. The potential of cytokeratin 20 and mucin 2 mRNA as metastasis markers in regional lymph nodes of colon cancer patients investigated by quantitative RT-PCR. Int J Colorectal Dis. 2009;24:261–268. doi: 10.1007/s00384-008-0613-y. [DOI] [PubMed] [Google Scholar]
- 66.Conzelmann M, Dieterle CP, Linnemann U, Berger MR. Cytokeratin 20 and guanylyl cyclase C mRNA is largely present in lymph node and liver specimens of colorectal cancer patients. Int J Cancer. 2003;107:617–628. doi: 10.1002/ijc.11425. [DOI] [PubMed] [Google Scholar]
- 67.Lassmann S, Bauer M, Rosenberg R, Nekarda H, Soong R, Rüger R, Höfler H, Werner M. Identification of occult tumor cells in node negative lymph nodes of colorectal cancer patients by cytokeratin 20 gene and protein expression. Int J Colorectal Dis. 2004;19:87–94. doi: 10.1007/s00384-003-0530-z. [DOI] [PubMed] [Google Scholar]
- 68.Bustin SA, Siddiqi S, Ahmed S, Hands R, Dorudi S. Quantification of cytokeratin 20, carcinoembryonic antigen and guanylyl cyclase C mRNA levels in lymph nodes may not predict treatment failure in colorectal cancer patients. Int J Cancer. 2004;108:412–417. doi: 10.1002/ijc.11596. [DOI] [PubMed] [Google Scholar]
- 69.D’Armento G, Daniele L, Mariani S, Ottaviani D, Mussa A, Cassoni P, Sapino A, Bussolati G. Added value of combined gene and protein expression of CK20 and CEA in non-macroscopically involved lymph nodes of colorectal cancer. Int J Surg Pathol. 2009;17:93–98. doi: 10.1177/1066896908328574. [DOI] [PubMed] [Google Scholar]
- 70.Bilchik AJ, Hoon DS, Saha S, Turner RR, Wiese D, DiNome M, Koyanagi K, McCarter M, Shen P, Iddings D, et al. Prognostic impact of micrometastases in colon cancer: interim results of a prospective multicenter trial. Ann Surg. 2007;246:568–75; discussion 575-7. doi: 10.1097/SLA.0b013e318155a9c7. [DOI] [PubMed] [Google Scholar]
- 71.Oberg AN, Lindmark GE, Israelsson AC, Hammarström SG, Hammarström ML. Detection of occult tumour cells in lymph nodes of colorectal cancer patients using real-time quantitative RT-PCR for CEA and CK20 mRNAS. Int J Cancer. 2004;111:101–110. doi: 10.1002/ijc.20231. [DOI] [PubMed] [Google Scholar]
- 72.Ohlsson L, Israelsson A, Öberg Å, Palmqvist R, Stenlund H, Hammarström ML, Hammarström S, Lindmark G. Lymph node CEA and MUC2 mRNA as useful predictors of outcome in colorectal cancer. Int J Cancer. 2012;130:1833–1843. doi: 10.1002/ijc.26182. [DOI] [PubMed] [Google Scholar]
- 73.Nordgård O, Oltedal S, Aasprong OG, Søreide JA, Søreide K, Tjensvoll K, Gilje B, Heikkilä R, Guriby M, Lothe RA, et al. Prognostic relevance of occult metastases detected by cytokeratin 20 and mucin 2 mRNA levels in sentinel lymph nodes from colon cancer patients. Ann Surg Oncol. 2012;19:3719–3726. doi: 10.1245/s10434-012-2454-8. [DOI] [PubMed] [Google Scholar]
- 74.Noura S, Ohue M, Seki Y, Yamamoto T, Idota A, Fujii J, Yamasaki T, Nakajima H, Murata K, Kameyama M, et al. Evaluation of the lateral sentinel node by indocyanine green for rectal cancer based on micrometastasis determined by reverse transcriptase-polymerase chain reaction. Oncol Rep. 2008;20:745–750. [PubMed] [Google Scholar]
- 75.Merrie AE, Phillips LV, Yun K, McCall JL. Skip metastases in colon cancer: assessment by lymph node mapping using molecular detection. Surgery. 2001;129:684–691. doi: 10.1067/msy.2001.113887. [DOI] [PubMed] [Google Scholar]
- 76.Güller U, Zettl A, Worni M, Langer I, Cabalzar-Wondberg D, Viehl CT, Demartines N, Zuber M. Molecular investigation of lymph nodes in colon cancer patients using one-step nucleic acid amplification (OSNA): a new road to better staging? Cancer. 2012;118:6039–6045. doi: 10.1002/cncr.27667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nicastri DG, Doucette JT, Godfrey TE, Hughes SJ. Is occult lymph node disease in colorectal cancer patients clinically significant? A review of the relevant literature. J Mol Diagn. 2007;9:563–571. doi: 10.2353/jmoldx.2007.070032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tsouma A, Aggeli C, Pissimissis N, Lembessis P, Zografos GN, Koutsilieris M. Circulating tumor cells in colorectal cancer: detection methods and clinical significance. Anticancer Res. 2008;28:3945–3960. [PubMed] [Google Scholar]
- 79.Gunn J, McCall JL, Yun K, Wright PA. Detection of micrometastases in colorectal cancer patients by K19 and K20 reverse-transcription polymerase chain reaction. Lab Invest. 1996;75:611–616. [PubMed] [Google Scholar]


