Abstract
McBurney’s procedure represented the gold-standard for acute appendicitis until 1981, but nowadays the number of laparoscopic appendectomies has progressively increased since it has been demonstrated to be a safe procedure, with excellent cosmetic results and it also allows a shorter hospitalization, a quicker and less painful postoperative recovery. The aim of this editorial was to perform a review of the literature in order to address controversial issues in the treatment of acute appendicitis.
Keywords: Acute appendicitis, Surgery, Laparoscopy
Core tip: There are still controversial issues in the treatment of acute appendicitis such as comparison between laparoscopic and open appendectomy and the correct approach in special categories of patients. The aim of this editorial was to perform a review of the literature in order to address controversial issues in the treatment of acute appendicitis.
INTRODUCTION
In 1894, McBurney[1] described a new technique for the management of acute appendicitis: this method is still used when an open approach is required.
McBurney’s procedure represented the gold-standard for acute appendicitis until 1981, when Semm[2] performed the first laparoscopic appendectomy in Germany, a “culture shock” in general surgery since a revolutionary method was discovered by a gynecologist[3]. But a real “laparoscopic revolution” took place only in 1985 with the first laparoscopic cholecystectomy performed by Erich Muhe, using Semm’s technique and instruments. Laparoscopy was not easily accepted since it was not considered a safe procedure; nowadays laparoscopic surgery is gaining a primary role in many surgical settings.
The number of laparoscopic appendectomies (LA) has progressively increased since it has been demonstrated to be a safe procedure, with excellent cosmetic results; furthermore, LA allows a shorter hospitalization, a quicker and less painful postoperative recovery.
But is laparoscopic surgery the best choice for appendectomy? Which are the correct surgical indications? What are the results from the comparison between LA vs classic open appendectomy (OA)? Are there selected groups of patients in which one of these approaches should be preferred? The aim of this editorial was to perform a review of the literature in order to address these controversial issues.
OPEN VS LAPAROSCOPIC APPENDECTOMY
Many comparative studies have already demonstrated the advantages of LA over OA in terms of length of hospital stay, use of postoperative analgesics and earlier return to work[4]. The most controversial issues of these studies have been taken into consideration.
Surgical-site infection
Surgical-site infection (SSI) rate was significantly lower in the LA than in the OA group (1.6% vs 3.2% respectively) and this gap between the two groups increased in severe forms of appendicitis, such as gangrenous and perforated. Some authors estimated that one wound infection could be prevented for every 23.7 patients treated with LA, instead of OA[5]: this can be explained with the use of the extraction bag (endo-bag) in LA, which prevents the direct contact between the infected appendix, the wound edges and the inflamed tissues around the appendix during its removal[5,6].
Other studies found a higher SSI rate in OA, but also a significantly higher intraabdominal abscess (IIA) rate in LA. The difference in the postoperative complications according to the surgical technique were remarkable when inflammation of the appendix was more severe: in fact, when a periappendiceal abscess was present, there were more cases of paralytic ileus (PI) in the LA group and more cases of SSI in the OA group. This result can be due to the leakage of infected substances, the appendiceal stump not being inverted and the resection side being exposed in the intraabdominal cavity during the removal of the appendix in LA[7]. Some authors suggest that the use of an Endo-GIA stapler could help minimize these adverse effects[8]. Finally, these differences are not statistically significant in case of gangrenous or/and perforated appendicitis[7].
Intraabdominal abscess
In an interesting study that considered 2464 patients, 52 experienced postoperative abscesses. The patients with a diagnosis of complicated appendicitis had a significant correlation with a higher incidence of intraabdominal abscess development (67% in complicated appendicitis vs 25% in uncomplicated appendicitis, P = 0.01). The majority of abscesses developed in the pelvis (41%), especially in those patients who had complicated rather than uncomplicated appendicitis (63% vs 18% respectively, P = 0.01). It is interesting to notice how the formation of an IIA in patients with a diagnosis of complicated appendicitis did not differ significantly between those who underwent LA and those who underwent OA (5.9% vs 4.1% respectively, P = 0.44). Moreover, in patients with complicated appendicitis there was no significant increase in presenting symptoms or in the severity of the case history, quite independently from the surgical approach. The only remarkable difference was that the patients who underwent OA presented earlier symptoms and received a more timely diagnosis of IIA than the patients who underwent LA (6 d in OA group vs 11 d in LA group)[9].
A multivariate analysis has shown that development of abscesses has a higher correlation with the initial diagnosis than with the type of surgical approach. The evaluation of selected patients demonstrated a 30% increase of the risk of IIA for every decade of life. This could be clinically relevant because it suggests the need for careful monitoring of elderly patients who initially presented complicated appendicitis, since they are at higher risk for postoperative IIA[9]. Finally an explanation for the formation of IIA could be found in the surgical technique itself: currently, surgeons performing LA tend to apply irrigation more freely; therefore, contaminating the entire peritoneal cavity[10]; although irrigation as a cause of IIA is yet controversial.
Incisional hernia
The incidence of incisional hernia is low in both techniques (0.7% in OA group vs 1% in LA): the development of post incisional hernias is higher with McBurney’s incision, whereas in LA there are incisional hernias only in those patients who undergo conversion[11].
Small bowel obstruction
Finally, as far as long-term complications are concerned, some studies assessed that small bowel obstruction can present many years after surgery, especially for open appendectomy. The prevalence of bowel obstruction after appendectomy increased from 0.63% after 1 year, to 0.97% after 10 years, to 1.30% after 30 years of follow up[11]. In a randomized study, a second look laparoscopy was performed on 40 patients who had histological confirmation of acute appendicitis, 3 mo after the first operation: there were adhesions in the 80% of patients that underwent OA, but only in 10% of LA group[5]. Therefore, LA seems to be associated with an easier second-look procedure and a minor infertility rate due to less adhesions[12].
Among long-term complications, small bowel obstruction has a very low incidence, between 0.33% and 1.51% in OA. It is known that the risk is higher with negative appendectomy or appendectomy through a midline laparotomic incision. Then, the choice of LA in suspected appendicitis is correct because it avoids unnecessary appendectomy if the appendix is normal and it prevents unnecessary wide incisions[13].
SUSPECTED APPENDICITIS
The differential diagnosis of most of the surgical abdominal emergencies is based on clinical grounds, laboratory data and diagnostic imaging. The problem, however, is to obtain a correct diagnosis of the exact localization of the lesion to determine surgical indications and to decide the best surgical approach. Laparoscopy is a valuable instrument in the case of suspected appendicitis allowing the surgeon to correctly evaluate the intraperitoneal condition of practically every single patient[14].
At first, considering its exploratory nature and its diagnostic accuracy, besides the advantage of a shorter time of hospitalization and reduction of pain on day 1[15], LA can be considered the first choice in suspected appendicitis, especially in particular categories, such as premenopausal women. In fact, in these patients, in the presence of right lower quadrant pain, differential diagnosis between acute appendicitis, ectopic pregnancy and pelvic inflammatory disease (PID), is necessary. A laparoscopic exploration of the abdominal cavity allows a rapid and safe diagnosis; for the former two affections laparoscopy also represents a therapeutic option, while in the latter one, samples for culture may also be taken, with the advantage of avoiding “negative” appendectomies, with a high diagnostic accuracy (96% in women and 100% in men)[16].
Morino et al[17] evaluated, in a prospective, randomized, single-institution trial, the role of early laparoscopy in the management of nonspecific abdominal pain (NSAP) in young women. NSAP was defined as an abdominal pain in right iliac or hypogastric area lasting more than 6 h and less than 8 d, without fever, leukocytosis, or obvious peritoneal signs and uncertain diagnosis after physical examination and baseline investigations including abdominal sonography. Patients were randomly assigned to early (< 12 from admission) laparoscopic group or to clinical observation group. Compared with active clinical observation, early laparoscopy did not show a clear benefit in women with NSAP. A higher number of diagnosis and a shorter hospital stay in the laparoscopic group did not lead to a significant reduction in symptoms recurrences at 1 year.
LA may be performed safely in pregnant patients with appendicitis according to the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines[18].
COMPLICATED APPENDICITIS
Excellent results are mentioned in several studies about the use of LA in complicated appendicitis, though a higher incidence of intraabdominal abscesses has been noticed. Some studies have demonstrated that LA is almost totally comparable to OA as far as operating time, hospital stay and postoperative complications are concerned. The rate of postoperative IIA was significantly higher in LA when compared with OA (respectively, 14% vs 0%), while wound infection and pulmonary complication rate were significantly lower (respectively 2.3% vs 8.2% in OA group and 0% vs 4.9% in LA group)[19].
The incidence rate of IIA increases considerably when a periappendiceal abscess or a postoperative ileus are present. Particularly, the incidence of IIA in complicated appendicitis increases remarkably (67% in complicated vs 25% in uncomplicated appendicitis): in these patients, there are no significant differences in the postoperative outcome or in the development of the abscess according to the surgical technique; therefore in the presence of an initial diagnosis of complicated appendicitis with a severe clinical background there is a higher probability of developing an abscess regardless of the adopted surgical approach[9].
In another 5-year non randomized study considering 1133 patients of which 244 had a complicated appendicitis (and among them, 175 underwent LA and 69 OA), LA patients had a shorter operative time (55 min vs 70 min), reduced length of stay (5 d vs 6 d) and a lower incidence of SSI (0.6% vs 10%)[10]. In the case of complicated appendicitis (gangrenous or perforated), the laparoscopic approach also reduced postoperative pain[20].
SPECIAL CATEGORIES OF PATIENTS
There are clinical settings in which laparoscopy may be the preferred approach: obese patients, immunocompromised patients and elderly patients.
In obese patients, in fact, laparoscopy is undeniably useful[21], considering at first the difficult exposure of the right lower quadrant during OA, which may require large, morbidity-prone incisions that are at risk of infections and of wound complications[5,22]. It is known that BMI is a risk factor for SSI[23]. Furthermore, obese patients have a higher risk of incisional hernias: laparoscopic approach reduces the risk of incisional hernia[24].
Immunocompromised patients include heart transplanted patients and those who received immunosuppressive therapy for autoimmune diseases, cancer and AIDS; the risk of infections is higher and the immunity response could be partial and ineffective due to immunodepression. Therefore, these patients may not exhibit the typical signs and symptoms of appendicitis and may only have a barely positive examination[25]. In these patients laparoscopic approach represents the best option: compared with OA, LA is characterized by a lower rate of postoperative complications (10.36% in LA group vs 22.56% in OA group), a shorter hospitalization (2.9 d vs 4.9 d) and a lower mortality (0.16% vs 0.61%). These results can be observed in both uncomplicated and complicated appendicitis, with a considerably lower incidence of complications (27.52% in LA group vs 57.50% in OA group) and a shorter hospital stay (5.92 d in LA group vs 9.67 d in OA group)[26].
Finally, elderly patients might significantly benefit from a laparoscopic approach[24]; in these patients it is quite difficult to collect anamnestic data, in addition to a mild abdominal examination and to laboratory and radiological tests which might not be so diriment. Laparoscopy can clarify the diagnosis and also represent a good therapeutical strategy[27].
INFLAMMED APPENDICEAL STUMP
Stump appendicitis is the acute inflammation of the residual portion of the appendix and is a rare complication of incomplete appendectomy[28].
Due to the relevant recurrence rate, a second appendectomy 3 mo after the outbreak of inflammation, could be necessary. In a histopathological study Gahukamble demonstrated that 13 of the 14 removed appendices had a pervious lumen with a higher risk of recurrent appendicitis. More recently authors focused the problem of a very long stump also on patients undergoing LA; in fact, the presence of an excessively long appendiceal stump could be at risk of recurrence also in these patients. Pain in the lower right abdominal quadrant in a patient that has undergone LA does not rule out a second episode of acute appendicitis[29]. The possibility of a recurring appendiceal stump abscess as a complication of LA is high. When performing LA, the appendiceal stump should be as short as possible and its ligation should not determine ischemia of the stump[30].
The tactical modification of appendiceal stump closure, replacing the invaginating suture that nowadays has become the procedure of choice consists in a single endoligature. Alternatively, there are methods which make use of an endostapler, endoligature (endo-loop), metal clips, bipolar endocoagulation and polymeric clips. All the different techniques have advantages and disadvantages depending on the different stages of acute appendicitis; so, the right knowledge about the possible methods and the appropriate choice between them according to every single case allows a safe and efficient management of patients as well as a reduction in hospital costs[31].
Drainage placement, ultrasound and perhaps an exploratory-therapeutical laparoscopy could be very useful in the management of this complication[30]. Finally the use of CT imaging allows a precise definition of the surrounding anatomy, in particular of the length of the appendiceal stump[32]. Several authors identify the removal of the whole appendiceal stump as the major suggested mean to avoid recurrence of appendicitis[33].
CONSERVATIVE MANAGEMENT OF ACUTE APPENDICITIS
Acute appendicitis is one of the most frequent conditions seen in a surgical department; urgent appendectomy is considered the treatment of choice because of the low incidence of major complications and the relative rapidity of operation and hospital stay. Nevertheless surgical treatment exposes the patient to risks due to general anaesthesia and other complications such as surgical site infection, adhesions and intestinal obstruction, incisional hernia, infertility in female and pneumonia[34]; in this setting, the role of conservative treatment with antibiotics has been investigated in literature.
A recent Cochrane review assessed five low to moderate quality randomized controlled trials[35]; with the limit of the analyzed studies, surgical approach remains the gold standard treatment for acute uncomplicated appendicitis. Another large meta-analysis compared the two strategies in the scenario of complicated appendicitis, abscess or phlegmon[36]; in this case, radiologic-assisted drainage of appendiceal abscess could be another helpful conservative strategy. The analysis of seventeen studies revealed that conservative management, with or without interval appendectomy, was associated with less overall complication rates, less reoperations and similar hospital stay compared with urgent appendectomy.
In the absence of high quality studies, laparoscopic or traditional appendectomy is still the treatment of choice for acute appendicitis; some in-progress prospective studies[34,37] could be helpful in understanding the role of conservative management.
NORMAL APPENDIX: LAPAROSCOPIC MANAGEMENT
Negative or white appendectomy refers to the removal of non-inflamed appendix and is performed in about 15%-25% of patients undergoing surgery for suspected acute appendicitis[38]. White appendectomy rate is declining over time as cited by large studies, due to the availability of computed tomography and laparoscopy[39]; in open surgery, the appendix is generally always removed[40].
Thanks to the widespread use of laparoscopy, laparoscopic management of normal appendix represents a dilemma for the surgeon and no guidelines are available in this field[41]. When laparoscopy is performed for suspected appendicitis, exploration is negative in 8%-15% but in up to 27% another condition is diagnosed[40]. The risks of leaving in situ an apparent normal appendix are: later appendicitis, misdiagnosed subclinical or ‘‘endo’’-appendicitis, missed appendiceal malignancy (carcinoid), risk of patient confusion and persisting symptoms[42]. At present, the laparoscopic strategy in front of a normal appendix remains controversial.
Conversions from laparoscopic to laparotomic appendectomy
In case of conversion, it is useful to perform an adequate laparotomic incision and an accurate and complete abdominal toilette. The conversion of perforated appendicitis is often burdened with a higher postoperative morbidity [60% in conversion appendectomy (CA), 22% in LA and 38% in OA][8].
A recent study in 2011, which included 745 patients that underwent LA or OA, asserts that conversion rate was about 8.6% and mentions that the first cause of conversion was the presence of a severe acute inflammatory process (38.7% of the factors which determine conversion to OA during operation). In this study, 77.42% of the patients that underwent CA had previous abdominal surgery and only 25.81% had a conversion due to adhesions.
Conversion was necessary especially in women over 65 years old (4.30% rather than 4.02% in the rest of patients)[43]. It is quite interesting that surgeons who performed at least 50 LA through their study period had a higher CA rate and this could reflect their will to attempt LA in the greatest part of patients, even in not strictly indicated cases. At the same time the number of conversions decreases progressively throughout the career of a surgeon and his equipe[43].
Another study indicates the presence of a generalized purulent peritonitis as the only significant risk factor for conversion. Moreover, although patients with previous abdominal surgery are at higher risk of conversion, this is not significantly correlated with sex and age. Converted patients are at higher risk of relaparotomy and incisional hernia, independently of the duration of the operation[11].
Finally, for patients that underwent LA with complications requiring reintervention following laparoscopy, there is the possibility of a relaparoscopy for a second look: this has the advantage of maintaining the reduced morbidity allowed by the first operation. Relaparoscopy is very useful for abscess drainage, because it provides the accurate identification of the causes, for example in case of appendicular stump insufficiency[44].
LAPAROSCOPY VS LAPAROTOMY: WHICH FACTORS DETERMINE SURGEON'S DECISION?
It is known that laparoscopic approach is more expensive, as many studies have reported: an American study evaluated hospital cost behaviour in the years 2000-2005, including all patients undergoing both LA and OA. Costs for LA are 22% higher in uncomplicated and 9% higher in complicated appendicitis. They estimate that in 2005 exclusive use of open appendectomy would have saved 93 million dollars: this finding is particularly important because appendectomy is a common routine operation in all hospitals. The authors suggest OA as the gold standard for acute appendicitis, reserving LA only for special categories of patients[45].
Cothren et al[46] compared the costs for LA and OA, which were significantly higher for LA: the authors noted that the total costs for LA were higher although operative time and stay in hospital were not so different between the two methods. Higher costs for LA might be due to the use of specific disposable surgical material for laparoscopy.
Another important factor for the hospital costs is the severity of illness of the patients at the initial diagnosis[47]. Even if more expensive, throught the years LA has become more common because there are undeniable benefits in hospitalization time and in recovery time: this way, higher costs are balanced out by a more precocious return to work of working patients. Recently, one study found that predicted costs for LA were 1856$ lower than for OA while the postoperative complication rate did not differ significantly[47].
Another crucial factor which influences the choice between LA and OA is the training and experience of surgical equipe. An interesting study compares the experience in academic-affiliated and community hospitals. The rate of LA and OA in the two kinds of hospitals is quite the same, but in academic-affiliated ones the operative time is longer both for LA and for OA (47 min vs 38 min for LA and 49 min vs 44 min for OA): this could be explained considering the intrinsic didactic nature of academic hospitals which inevitably causes a little delay in the operations. Finally in both types of hospitals, hospitalization for LA was shortened by 1 d[48].
A parameter to assess the value of a surgical approach is long-term quality of life. A German study determined how a group of patients - including both LA and OA - perceived their quality of life 7 years after appendectomy, through the administration of a specific questionnaire. The most satisfied patients were those who underwent LA, both for the quick recovery and for the cosmetic result[49]. Another work obtained information about overall satisfaction by a telephone interview: the LA group had fewer complications and returned earlier to work (median 13 d for OA vs 8 d for LA)[13].
Laparoscopic appendectomy: Techniques
Recently several methods have been proposed to perform appendectomy in a laparoscopic fashion. In the most popular approach, 3 abdominal wall incisions are performed to insert instruments in the abdominal cavity. According to the patients’ demand of scar-free surgery, new minimally invasive methods have been developed.
Traditional laparoscopic appendectomy [3 port(s) laparoscopic appendectomy]: In conventional laparoscopic appendectomy, 3 ports are used to place instruments in the abdomen (Figure 1). The laparoscope is inserted in the umbilicus and pneumoperitoneum is induced; the site of the other 2 trocars for operative instruments is variable, according to the surgeon’s preference and ability. The most used locations for trocars are: the lower left quadrant and suprapubic or lower left quadrant and lower right quadrant or suprapubic and lower right quadrant or both trocars placed on the “bikini line” (suprapubic)[50]. Nevertheless, the trocars are inserted respecting the triangulation rule, with the appendix at the apex of a triangle. The umbilical port is 5-12 mm in diameter while the others are generally 5 mm large[51].
Figure 1.
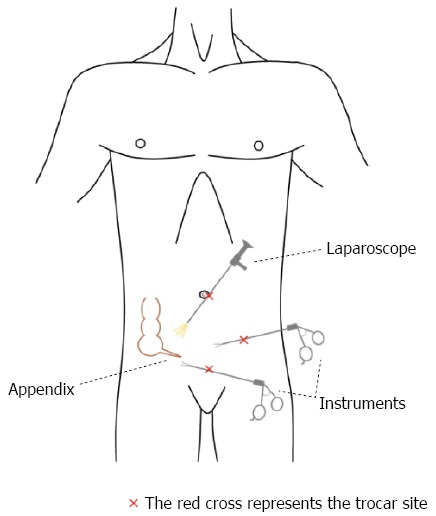
Traditional laparoscopic appendectomy: 3 ports are used to place instruments in the abdomen.
During surgical procedure, many methods are used to amputate and extract the appendix and to perform proper hemostasis; the routinely use of peritoneal irrigation and drainage placement is not recommended[52]. The number of trocars can be reduced to 2 using the “puppeteer technique”; in this variant, the appendix is suspended using transabdominal threads[53].
A laparoscopic surgeon must be skilled with the open approach; in fact, open appendectomy represent the first step in the training of an operator who desires to perform laparoscopic appendectomy. But when is the learning curve completed? It is generally accepted that it is completed after 20 operations[54].
To improve the cosmetic result, needlescopic appendectomy has been developed; this term refers to an evolution of conventional laparoscopy. The only difference between the two regards the instruments’ diameter, in fact in the needlescopic approach 3-mm or less trocars are used[55]. The first needlescopic appendectomy was performed in 1994. The use of smaller trocars potentially reduces postoperative pain and length of hospital stay due to minor abdominal wall incisions[56]; patients can quickly return to normal activity. On the other hand, this technique is more challenging for surgeons with a risk of longer duration of surgery and higher conversion rate[57]; these disadvantages will probably disappear after an appropriate learning curve and an increase of surgical skill. Needlescopic appendectomy is likely to be more expensive than the traditional approach due to equipment costs[58]. This fascinating laparoscopic evolution is not routinely recommended because of the lack of scientific evidence: large randomized controlled trials are necessary. It can, however, represents an option in selected patients, like young women.
Single-incision laparoscopic surgery: The continuous evolution of laparoscopic surgery and the ambition of better cosmetic results always tend to less invasive procedures. Single Incision Laparoscopic Surgery (SILS) for acute appendicitis in children began in 1992[59]. The development and diffusion of this technique was quite slow due to the lack of adequate instruments; healthcare engineering ideated multilumen ports, special laparoscopes and articulating instruments to facilitate the surgeon’s work[60]. SILS is now diffused in many surgical specialties and skilled surgeons can perform several operations in this way, i.e., adrenalectomy, Heller myotomy, large bowel surgery, splenectomy, bariatric surgery[61].
In SILS, a multi-luminal and single port device is placed transumbilically: through this device, laparoscope and instruments can reach the abdominal cavity. The proposed advantages of SILS are better cosmetic results, reduced wound infection, postoperative pain, bleeding, visceral injury and port site hernia due to the presence of a unique abdominal wall incision: for this reason it is known as “scarless” surgery. In a recent randomized controlled trial, SILS was associated with higher post-opertative pain and more intravenous analgesics requirement; better wound cosmesis and higher satisfaction scores were also observed[62]. On the other hand it also has some technical challenges, like loss of triangulation (the cornerstone of laparoscopy) and instrument crowding (sword fighting)[63]. Although it is a technical challenge, in skilled hands, it is considered a safe procedure; patients seem to appreciate when a SILS approach is performed because surgical incisions are hidden in the umbilicus. Recent studies compared SILS and conventional laparoscopic appendectomy: no significative differences in the operative time, length of hospital stay, post operative pain and complication were observed[64,65].
The learning curve of single incision laparoscopic appendectomy is between 5 to 10 cases[66]. To reduce the need of special materials and the costs, SILS can be performed using nonarticulating instruments and conventional trocars: early data suggests that it can represent an economic and safe option, even if operative time is longer[67]. In this approach, an adequate follow-up to detect the risk of post-incisional hernia is needed because many trocars are inserted in a very small area. There are also original ideas to reduce costs, i.e., the use of a surgical glove like a multi-lumen port where instruments pass via the cutting fingers[63]. However, it is very difficult to determine the costs of SILS[68].
Lacking of available evidence, no recommendations can be made on the effectiveness of SILS vs conventional multi-incision laparoscopic appendectomy[69].
Natural orifice transluminal endoscopic surgery: In 2004 Rao et al[70] described a new real “scarless” procedure performing a transgastric appendectomy. Natural Orifice Transluminal Endoscopic Surgery (NOTES) represents the forefront of laparoscopic surgery and the next worldwide focus on minimally invasive surgery[71]; using a multichannel endoscope, the access to the peritoneal cavity is obtained via natural orifices like vagina, rectum, stomach and bladder. This technique allows to perform many surgical operations without visible scars; avoiding abdominal-wall incisions, postoperative pain is minor and recovery is faster. SILS is considered a bridge between conventional multi-ports laparoscopy and NOTES.
Regarding acute appendicitis, in female patients a transvaginal approach can be used (TVA, TransVaginal Appendectomy); an incision performed in the posterior fornix of vagina permits the access to the peritoneal cavity (Figure 2).
Figure 2.
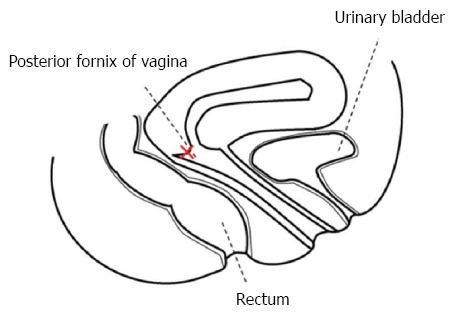
Notes procedure: Transvaginal approach is performed through the posterior fornix of the vagina.
A prospective study comparing TVA to traditional 3-port laparoscopic appendectomy showed significantly less post-operative analgesia demand (Patient Controlled Analgesia morphine utilization) and faster return to normal activity; compared with the conventional laparoscopic approach there were no differences in the length of stay and operative time[72]. There were no differences in pre- and post-operatively sexual function; no post-operative dispareunia was noted and TVA vs conventional laparoscopy sexual outcome was comparable. Even though the authors of this prospective study concluded that TVA is a safe and feasible procedure in women with acute non-perforated appendicitis, the authors of this review believe that large randomized controlled trials are necessary before proposing this procedure to a young woman.
CONCLUSION
Patient selection is important in both LA and OA. LA is the preferred approach in immunocompromised, obese and elderly patients. LA presents longer operative time, but also a shortening of hospital stay, a better and earlier recovery and return to everyday occupations and to work and, last but not least, a better cosmetic result.
ACKNOWLEDGMENTS
We are very grateful to Jean Jimenez, Researcher of English Language and Linguistics at the University of Calabria, for her help in reviewing the English language of this paper.
Footnotes
P- Reviewers: Amin AI, Okumura K, Vettoretto N S- Editor: Zhai HH L- Editor: A E- Editor: Zhang DN
References
- 1.McBurney C. IV. The Incision Made in the Abdominal Wall in Cases of Appendicitis, with a Description of a New Method of Operating. Ann Surg. 1894;20:38–43. doi: 10.1097/00000658-189407000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 3.Litynski GS. Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm’s impact on the “laparoscopic revolution”. JSLS. 1998;2:309–313. [PMC free article] [PubMed] [Google Scholar]
- 4.Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929–1939. doi: 10.1007/s11605-012-1972-9. [DOI] [PubMed] [Google Scholar]
- 5.Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545–553. doi: 10.1016/s1072-7515(98)00080-5. [DOI] [PubMed] [Google Scholar]
- 6.Suh YJ, Jeong SY, Park KJ, Park JG, Kang SB, Kim DW, Oh HK, Shin R, Kim JS. Comparison of surgical-site infection between open and laparoscopic appendectomy. J Korean Surg Soc. 2012;82:35–39. doi: 10.4174/jkss.2012.82.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim SG, Ahn EJ, Kim SY, Chung IY, Park JM, Park SH, Choi KW. A Clinical Comparison of Laparoscopic versus Open Appendectomy for Complicated Appendicitis. J Korean Soc Coloproctol. 2011;27:293–297. doi: 10.3393/jksc.2011.27.6.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piskun G, Kozik D, Rajpal S, Shaftan G, Fogler R. Comparison of laparoscopic, open, and converted appendectomy for perforated appendicitis. Surg Endosc. 2001;15:660–662. doi: 10.1007/s004640020072. [DOI] [PubMed] [Google Scholar]
- 9.Asarias JR, Schlussel AT, Cafasso DE, Carlson TL, Kasprenski MC, Washington EN, Lustik MB, Yamamura MS, Matayoshi EZ, Zagorski SM. Incidence of postoperative intraabdominal abscesses in open versus laparoscopic appendectomies. Surg Endosc. 2011;25:2678–2683. doi: 10.1007/s00464-011-1628-y. [DOI] [PubMed] [Google Scholar]
- 10.Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007;205:60–65. doi: 10.1016/j.jamcollsurg.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Swank HA, Eshuis EJ, van Berge Henegouwen MI, Bemelman WA. Short- and long-term results of open versus laparoscopic appendectomy. World J Surg. 2011;35:1221–126; discussion 1221-126;. doi: 10.1007/s00268-011-1088-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lehmann-Willenbrock E, Mecke H, Riedel HH. Sequelae of appendectomy, with special reference to intra-abdominal adhesions, chronic abdominal pain, and infertility. Gynecol Obstet Invest. 1990;29:241–245. doi: 10.1159/000293326. [DOI] [PubMed] [Google Scholar]
- 13.Kouhia ST, Heiskanen JT, Huttunen R, Ahtola HI, Kiviniemi VV, Hakala T. Long-term follow-up of a randomized clinical trial of open versus laparoscopic appendicectomy. Br J Surg. 2010;97:1395–1400. doi: 10.1002/bjs.7114. [DOI] [PubMed] [Google Scholar]
- 14.Casciola L, Ceccarelli G, Bartoli A, D’Ajello F, Bellochi R, Valeri R, Rambotti M, Spaziani A, Mazzoli W, Di Zitti L. [Laparoscopic approach versus laparotomy for suspected acute appendicitis] G Chir. 2002;23:440–444. [PubMed] [Google Scholar]
- 15.Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2002;(1):CD001546. doi: 10.1002/14651858.CD001546. [DOI] [PubMed] [Google Scholar]
- 16.Cariati A, Brignole E, Tonelli E, Filippi M, Guasone F, De Negri A, Novello L, Risso C, Noceti A, Giberto M, et al. [Laparoscopic or open appendectomy. Critical review of the literature and personal experience] G Chir. 2001;22:353–357. [PubMed] [Google Scholar]
- 17.Morino M, Pellegrino L, Castagna E, Farinella E, Mao P. Acute nonspecific abdominal pain: A randomized, controlled trial comparing early laparoscopy versus clinical observation. Ann Surg. 2006;244:881–86; discussion 881-86. doi: 10.1097/01.sla.0000246886.80424.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearl J, Price R, Richardson W, Fanelli R. Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc. 2011;25:3479–3492. doi: 10.1007/s00464-011-1927-3. [DOI] [PubMed] [Google Scholar]
- 19.Pokala N, Sadhasivam S, Kiran RP, Parithivel V. Complicated appendicitis--is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg. 2007;73:737–741; discussion 741-742. [PubMed] [Google Scholar]
- 20.Garg CP, Vaidya BB, Chengalath MM. Efficacy of laparoscopy in complicated appendicitis. Int J Surg. 2009;7:250–252. doi: 10.1016/j.ijsu.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Markar SR, Venkat-Raman V, Ho A, Karthikesalingam A, Kinross J, Evans J, Bloom I. Laparoscopic versus open appendicectomy in obese patients. Int J Surg. 2011;9:451–455. doi: 10.1016/j.ijsu.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Enochsson L, Hellberg A, Rudberg C, Fenyö G, Gudbjartson T, Kullman E, Ringqvist I, Sörensen S, Wenner J. Laparoscopic vs open appendectomy in overweight patients. Surg Endosc. 2001;15:387–392. doi: 10.1007/s004640000334. [DOI] [PubMed] [Google Scholar]
- 23.Cantürk Z, Cantürk NZ, Cetinarslan B, Utkan NZ, Tarkun I. Nosocomial infections and obesity in surgical patients. Obes Res. 2003;11:769–775. doi: 10.1038/oby.2003.107. [DOI] [PubMed] [Google Scholar]
- 24.Mason RJ, Moazzez A, Moroney JR, Katkhouda N. Laparoscopic vs open appendectomy in obese patients: outcomes using the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg. 2012;215:88–99; discussion 99-100. doi: 10.1016/j.jamcollsurg.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 25.Flum DR, Steinberg SD, Sarkis AY, Wallack MK. Appendicitis in patients with acquired immunodeficiency syndrome. J Am Coll Surg. 1997;184:481–486. [PubMed] [Google Scholar]
- 26.Masoomi H, Mills SD, Dolich MO, Dang P, Carmichael JC, Nguyen NT, Stamos MJ. Outcomes of laparoscopic and open appendectomy for acute appendicitis in patients with acquired immunodeficiency syndrome. Am Surg. 2011;77:1372–1376. [PubMed] [Google Scholar]
- 27.Watters JM, Blakslee JM, March RJ, Redmond ML. The influence of age on the severity of peritonitis. Can J Surg. 1996;39:142–146. [PMC free article] [PubMed] [Google Scholar]
- 28.Kanona H, Al Samaraee A, Nice C, Bhattacharya V. Stump appendicitis: a review. Int J Surg. 2012;10:425–428. doi: 10.1016/j.ijsu.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Daniels ED, Pettifor JM, Schnitzler CM, Russell SW, Patel DN. Ethnic differences in bone density in female South African nurses. J Bone Miner Res. 1995;10:359–367. doi: 10.1002/jbmr.5650100305. [DOI] [PubMed] [Google Scholar]
- 30.Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Appendiceal stump abscess as an early complication of laparoscopic appendectomy: report of a case. Surg Today. 2002;32:919–921. doi: 10.1007/s005950200182. [DOI] [PubMed] [Google Scholar]
- 31.Gomes CA, Nunes TA, Soares C, Gomes CC. The appendiceal stump closure during laparoscopy: historical, surgical, and future perspectives. Surg Laparosc Endosc Percutan Tech. 2012;22:1–4. doi: 10.1097/SLE.0b013e31823fbf15. [DOI] [PubMed] [Google Scholar]
- 32.Roberts KE, Starker LF, Duffy AJ, Bell RL, Bokhari J. Stump appendicitis: a surgeon’s dilemma. JSLS. 2011;15:373–378. doi: 10.4293/108680811X13125733356954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Watkins BP, Kothari SN, Landercasper J. Stump appendicitis: case report and review. Surg Laparosc Endosc Percutan Tech. 2004;14:167–171. doi: 10.1097/01.sle.0000129392.75673.97. [DOI] [PubMed] [Google Scholar]
- 34.Tugnoli G, Giorgini E, Biscardi A, Villani S, Clemente N, Senatore G, Filicori F, Antonacci N, Baldoni F, De Werra C, et al. The NOTA study: non-operative treatment for acute appendicitis: prospective study on the efficacy and safety of antibiotic treatment (amoxicillin and clavulanic acid) in patients with right sided lower abdominal pain. BMJ Open. 2011;1:e000006. doi: 10.1136/bmjopen-2010-000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev. 2011;(11):CD008359. doi: 10.1002/14651858.CD008359.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147:818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 37.Paajanen H, Grönroos JM, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Dean K, Jartti A, Mecklin JP, et al. A prospective randomized controlled multicenter trial comparing antibiotic therapy with appendectomy in the treatment of uncomplicated acute appendicitis (APPAC trial) BMC Surg. 2013;13:3. doi: 10.1186/1471-2482-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sakorafas GH, Mastoraki A, Lappas C, Sampanis D, Danias N, Smyrniotis V. Conservative treatment of acute appendicitis: heresy or an effective and acceptable alternative to surgery? Eur J Gastroenterol Hepatol. 2011;23:121–127. doi: 10.1097/MEG.0b013e32834233b6. [DOI] [PubMed] [Google Scholar]
- 39.Mariadason JG, Wang WN, Wallack MK, Belmonte A, Matari H. Negative appendicectomy rate as a quality metric in the management of appendicitis: impact of computed tomography, Alvarado score and the definition of negative appendicectomy. Ann R Coll Surg Engl. 2012;94:395–401. doi: 10.1308/003588412X13171221592131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Navez B, Therasse A. Should every patient undergoing laparoscopy for clinical diagnosis of appendicitis have an appendicectomy? Acta Chir Belg. 2003;103:87–89. doi: 10.1080/00015458.2003.11679371. [DOI] [PubMed] [Google Scholar]
- 41.Jaunoo SS, Hale AL, Masters JP, Jaunoo SR. An international survey of opinion regarding investigation of possible appendicitis and laparoscopic management of a macroscopically normal appendix. Ann R Coll Surg Engl. 2012;94:476–480. doi: 10.1308/003588412X13373405385377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Vlodrop V, Pattyn P, Ceelen W. Management of the ‘normal’ appendix during surgery for right fossa syndrome: proposed clinical algorithm. Acta Chir Belg. 2007;107:8–11. doi: 10.1080/00015458.2007.11680004. [DOI] [PubMed] [Google Scholar]
- 43.Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic appendectomy conversion rates two decades later: an analysis of surgeon and patient-specific factors resulting in open conversion. J Surg Res. 2012;176:42–49. doi: 10.1016/j.jss.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 44.Leister I, Becker H. [Relaparoscopy as an alternative to laparotomy for laparoscopic complications] Chirurg. 2006;77:986–997. doi: 10.1007/s00104-006-1252-x. [DOI] [PubMed] [Google Scholar]
- 45.Sporn E, Petroski GF, Mancini GJ, Astudillo JA, Miedema BW, Thaler K. Laparoscopic appendectomy--is it worth the cost? Trend analysis in the US from 2000 to 2005. J Am Coll Surg. 2009;208:179–85.e2. doi: 10.1016/j.jamcollsurg.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 46.Cothren CC, Moore EE, Johnson JL, Moore JB, Ciesla DJ, Burch JM. Can we afford to do laparoscopic appendectomy in an academic hospital? Am J Surg. 2005;190:950–954. doi: 10.1016/j.amjsurg.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 47.Haas L, Stargardt T, Schreyoegg J. Cost-effectiveness of open versus laparoscopic appendectomy: a multilevel approach with propensity score matching. Eur J Health Econ. 2012;13:549–560. doi: 10.1007/s10198-011-0355-6. [DOI] [PubMed] [Google Scholar]
- 48.Ingraham AM, Cohen ME, Bilimoria KY, Pritts TA, Ko CY, Esposito TJ. Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery. 2010;148:625–35; discussion 635-7. doi: 10.1016/j.surg.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 49.Kapischke M, Friedrich F, Hedderich J, Schulz T, Caliebe A. Laparoscopic versus open appendectomy--quality of life 7 years after surgery. Langenbecks Arch Surg. 2011;396:69–75. doi: 10.1007/s00423-010-0715-1. [DOI] [PubMed] [Google Scholar]
- 50.Vettoretto N, Agresta F. A brief review of laparoscopic appendectomy: the issues and the evidence. Tech Coloproctol. 2011;15:1–6. doi: 10.1007/s10151-010-0656-2. [DOI] [PubMed] [Google Scholar]
- 51.McKinlay R, Mastrangelo MJ. Current status of laparoscopic appendectomy. Curr Surg. 2003;60:506–512. doi: 10.1016/S0149-7944(03)00128-4. [DOI] [PubMed] [Google Scholar]
- 52.Vettoretto N, Gobbi S, Corradi A, Belli F, Piccolo D, Pernazza G, Mannino L. Consensus conference on laparoscopic appendectomy: development of guidelines. Colorectal Dis. 2011;13:748–754. doi: 10.1111/j.1463-1318.2011.02557.x. [DOI] [PubMed] [Google Scholar]
- 53.Roberts KE. True single-port appendectomy: first experience with the “puppeteer technique”. Surg Endosc. 2009;23:1825–1830. doi: 10.1007/s00464-008-0270-9. [DOI] [PubMed] [Google Scholar]
- 54.Lin YY, Shabbir A, So JB. Laparoscopic appendectomy by residents: evaluating outcomes and learning curve. Surg Endosc. 2010;24:125–130. doi: 10.1007/s00464-009-0691-0. [DOI] [PubMed] [Google Scholar]
- 55.Gagner M, Garcia-Ruiz A. Technical aspects of minimally invasive abdominal surgery performed with needlescopic instruments. Surg Laparosc Endosc. 1998;8:171–179. [PubMed] [Google Scholar]
- 56.Matthews BD, Mostafa G, Harold KL, Kercher KW, Reardon PR, Heniford BT. Minilaparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech. 2001;11:351–355. doi: 10.1097/00129689-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Sajid MS, Khan MA, Cheek E, Baig MK. Needlescopic versus laparoscopic appendectomy: a systematic review. Can J Surg. 2009;52:129–134. [PMC free article] [PubMed] [Google Scholar]
- 58.Chock A, Seslar S, Stoopen E, Tristan A, Hashish H, Gonzalez JJ, Franklin ME. Needlescopic appendectomy. Surg Endosc. 2003;17:1451–1453. doi: 10.1007/s00464-002-8732-y. [DOI] [PubMed] [Google Scholar]
- 59.Pelosi MA, Pelosi MA. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy) J Reprod Med. 1992;37:588–594. [PubMed] [Google Scholar]
- 60.Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009;23:1419–1427. doi: 10.1007/s00464-009-0463-x. [DOI] [PubMed] [Google Scholar]
- 61.Greaves N, Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011;93:437–440. doi: 10.1308/003588411X590358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Teoh AY, Chiu PW, Wong TC, Poon MC, Wong SK, Leong HT, Lai PB, Ng EK. A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg. 2012;256:909–914. doi: 10.1097/SLA.0b013e3182765fcf. [DOI] [PubMed] [Google Scholar]
- 63.Rehman H, Ahmed I. Technical approaches to single port/incision laparoscopic appendicectomy: a literature review. Ann R Coll Surg Engl. 2011;93:508–513. doi: 10.1308/147870811X13137608455091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gill RS, Shi X, Al-Adra DP, Birch DW, Karmali S. Single-incision appendectomy is comparable to conventional laparoscopic appendectomy: a systematic review and pooled analysis. Surg Laparosc Endosc Percutan Tech. 2012;22:319–327. doi: 10.1097/SLE.0b013e31824f2cf8. [DOI] [PubMed] [Google Scholar]
- 65.Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: a randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367–1371. doi: 10.1007/s00464-012-2617-5. [DOI] [PubMed] [Google Scholar]
- 66.Moazzez A, Mason RJ, Katkhouda N. Laparoscopic appendectomy: new concepts. World J Surg. 2011;35:1515–1518. doi: 10.1007/s00268-011-1032-8. [DOI] [PubMed] [Google Scholar]
- 67.Colon MJ, Telem D, Divino CM, Chin EH. Laparoendoscopic single site surgery can be performed completely with standard equipment. Surg Laparosc Endosc Percutan Tech. 2011;21:292–294. doi: 10.1097/SLE.0b013e31822474a4. [DOI] [PubMed] [Google Scholar]
- 68.Ahmed K, Wang TT, Patel VM, Nagpal K, Clark J, Ali M, Deeba S, Ashrafian H, Darzi A, Athanasiou T, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25:378–396. doi: 10.1007/s00464-010-1208-6. [DOI] [PubMed] [Google Scholar]
- 69.Rehman H, Rao AM, Ahmed I. Single incision versus conventional multi-incision appendicectomy for suspected appendicitis. Cochrane Database Syst Rev. 2011;(7):CD009022. doi: 10.1002/14651858.CD009022.pub2. [DOI] [PubMed] [Google Scholar]
- 70.Rao GV, Reddy DN, Banerjee R. NOTES: human experience. Gastrointest Endosc Clin N Am. 2008;18:361–370; x. doi: 10.1016/j.giec.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 71.Huang C, Huang RX, Qiu ZJ. Natural orifice transluminal endoscopic surgery: new minimally invasive surgery come of age. World J Gastroenterol. 2011;17:4382–4388. doi: 10.3748/wjg.v17.i39.4382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roberts KE, Solomon D, Mirensky T, Silasi DA, Duffy AJ, Rutherford T, Longo WE, Bell RL. Pure transvaginal appendectomy versus traditional laparoscopic appendectomy for acute appendicitis: a prospective cohort study. Ann Surg. 2012;255:266–269. doi: 10.1097/SLA.0b013e31823b2748. [DOI] [PubMed] [Google Scholar]


