Abstract
HIV and intimate partner violence (IPV) risks are linked in Hispanic women, so integrated interventions can efficiently produce meaningful change. Integrated interventions for Hispanic women are promising, but factors that put Hispanic women at risk for HIV and violence may also impede engagement with interventions. This study examined barriers and facilitators of engagement in a group educational intervention, SEPA (Salud, Educación, Prevención y Autocuidado [Health, Education, Prevention, and Self-Care]), for Hispanic women. A total of 274 Hispanic women from South Florida in the SEPA condition of a randomized controlled trial completed baseline measures of violence, depression, familism, Hispanic stress, acculturation, and demographics, and 57% of the women engaged (attended two of five sessions). Education, IPV, and acculturation predicted engagement. Understanding engagement advances intervention development/refinement. Hispanic women who experience relationship violence are open to group interventions. Further program development and outreach work are needed to connect women with low education, who are particularly vulnerable.
Keywords: Latino, population focus, violence, health behavior/symptom focus, HIV/AIDS, women, intervention engagement, acculturation
Creating tailored interventions for specific cultural groups may reduce or eliminate health disparities. The participation of members of these groups is fundamental for accruing the full benefits of these interventions. Understanding the factors linked to participation can also help to refine tailored interventions. This study examines predictors of participation in a tailored intervention for Hispanic women, a rapidly increasing group with unique health risks. The terms Hispanic and Latino are used to describe a very diverse group of individuals in the United States who have Spanish (Hispanic) or Latin American (Latino) descent. There are large variations in regard to preferences in the use of the term Hispanic or Latino among academics and lay people alike. We use the term Hispanic in this article because it is the term more commonly used in tracking demographics and is often preferred by individuals from this origin (Pew Hispanic Research Center, 2012; U.S. Census Bureau, 2012).
Hispanic women are at disproportionate risk for HIV and intimate partner violence (IPV). In 2008, Hispanic women were nearly five times as likely to have AIDS or to be diagnosed with HIV as were non-Hispanic White women, and in 2007, Hispanic women were more than four times more likely than non-Hispanic White women to die of HIV/AIDS (Centers for Disease Control and Prevention [CDC], 2010). The prevalence rate of physical abuse from an intimate partner within the past 5 years for Hispanic women is estimated at over two times that of non-Hispanic White women (Bonomi, Anderson, Cannon, Slesnick, & Rodriguez, 2009). Among a national sample of couples, IPV incidence and recurrence for more than 5 years was found to be higher among Hispanic couples compared with non-Hispanic White couples, at 58% versus 14% and 37% versus 6%, respectively (Caetano, Field, Ramisetty-Mikler, & McGrath, 2005). The rate of recurrence for severe IPV was four times higher for Hispanic couples than for non-Hispanic White couples.
HIV risk and IPV are correlated in women across cultural groups (Gielen et al., 2007; Sareen, Pagura, & Grant, 2009) and among Hispanic women in particular (González-Guarda, Peragallo, Urrutia, Vasquez, & Mitrani, 2008; González-Guarda, Vasquez, Urrutia, Villaruel, & Peragallo, 2011; Raj, Silverman, & Amaro, 2004). Women acquire HIV primarily through heterosexual contact, and a key sociocultural mechanism believed to underlie the overlapping risks for HIV and IPV are gender-role norms. These norms promote uneven power between couples, contributing to coercive relationships, double standards regarding sexual fidelity, and women’s difficulty negotiating for safer sex with partners who engage in sexual risk behaviors (Amaro, 1995; Gielen et al., 2007; Krishnan et al., 2008; Moreno, 2007). In addition, socioeconomic factors, including poverty and low educational attainment, which are more common in Hispanics than among non-Hispanic Whites (CDC, 2011a), are risk factors for a myriad of health conditions including HIV and IPV (Caetano et al., 2005; Cunradi, Caetano, Clark, & Schaefer, 2000; Newcomb & Carmona, 2004), and exacerbate women’s vulnerability to partner coercion.
Because of the underlying relational pathways that link HIV and IPV risk for women, interventions that address both conditions simultaneously by improving women’s skills for negotiating with partners can have high impact as risk-reduction approaches (Gielen et al., 2007; Krishnan et al., 2008). In addition, because women, especially Hispanic women, are not likely to report IPV and seek health services for IPV, it is important to embed primary and secondary prevention for IPV within existing clinical services and community-based health programs that they are more likely to access (Lipsky, Caetano, & Roy-Byrne, 2009). However, very few interventions have been designed to simultaneously address HIV risk and IPV in women (Gielen et al., 2007; Krishnan et al., 2008), and of these, only two have been designed specifically for Hispanic women. In a pilot study testing a two-session group intervention, Entre Amigas (“Between Friends” in English) aimed at reducing HIV and IPV among at-risk Hispanic women, Davila, Bonilla, Gonzalez-Ramirez, and Villaruel (2007) found that the intervention resulted in increased intention to perform HIV-IPV-risk-reduction behaviors. A group intervention for Hispanic women, SEPA (Salud, Educación, Prevención y Autocuidado [Health, Education, Prevention, and Self-Care]), has been tested in two randomized controlled trials. The first trial (SEPA I; Peragallo et al., 2005) showed that women assigned to SEPA had improved HIV knowledge, partner communication, and condom use compared with a no-intervention control. The second trial (SEPA II; Peragallo, González-Guarda, McCabe, & Cianelli, 2011) showed that women randomly assigned to SEPA had improved HIV knowledge, partner communication, and condom use, and reduced IPV as compared with controls. Data from this trial, the second randomized trial of SEPA (i.e., SEPA II), were used in this study.
Although the findings of these intervention studies are promising, the factors that put Hispanic women at risk for HIV and IPV may also impede their willingness and ability to follow through with services and participate in interventions, thereby amplifying these health disparities. Hispanics have been found to be less likely than non-Hispanic Whites to use preventive services for chronic health disorders (CDC, 2011b) and to access mental health interventions (Marques et al., 2011; Padgett, Patrick, Burns, & Schlesinger, 1994). Barriers to health service utilization are even more pronounced among monolingual Spanish speakers (Fiscella, Franks, Doescher, & Saver 2002; Lanouette, Folsom, Sciolla, & Jeste, 2009). Gender role norms may also contribute to suboptimal utilization of HIV/IPV services in particular. Davila and colleagues (2007) conducted focus groups with Hispanic community women and service agency workers serving Hispanic women and found that partners’ monitoring of women’s activities, disapproval of their discussing the partner’s risk behaviors, and intolerance for absences from the home dampened the women’s willingness to participate in HIV/IPV prevention programs.
Understanding the client characteristics that facilitate or impede participation in HIV/IPV interventions is useful for designing outreach and retention strategies to strengthen the impact of programs aimed at improving sexual and relational health for Hispanic women. However, our review of the literature revealed only one study investigating the factors that predict participation of Hispanic women in HIV- or IPV-risk-reduction interventions. In the randomized trial of SEPA (i.e., SEPA I; Peragallo et al., 2005), employment, depression, younger age, and low intention to reduce risk behaviors predicted intervention dropout in multivariate analysis (Kim, Peragallo, & DeForge, 2006).
Purpose
The aim of this study was to examine participant characteristics that served as barriers and facilitators of engagement in the second, recently completed, randomized trial of SEPA (SEPA II; Peragallo et al., 2011) that was conducted with Hispanic women in a different region of the United States. Based on the literature cited above, we hypothesized that the following variables would serve as barriers to participation and predict nonengagement (defined as attending less than two sessions): (a) competing role obligations related to family (number of minor children and living with a partner) and employment, (b) IPV in the woman’s current relationship, (c) depressive symptoms, (d) Hispanic cultural factors (familism, Hispanic stress, Hispanicism, and low Americanism), and (e) lower levels of education.
Method
Participants
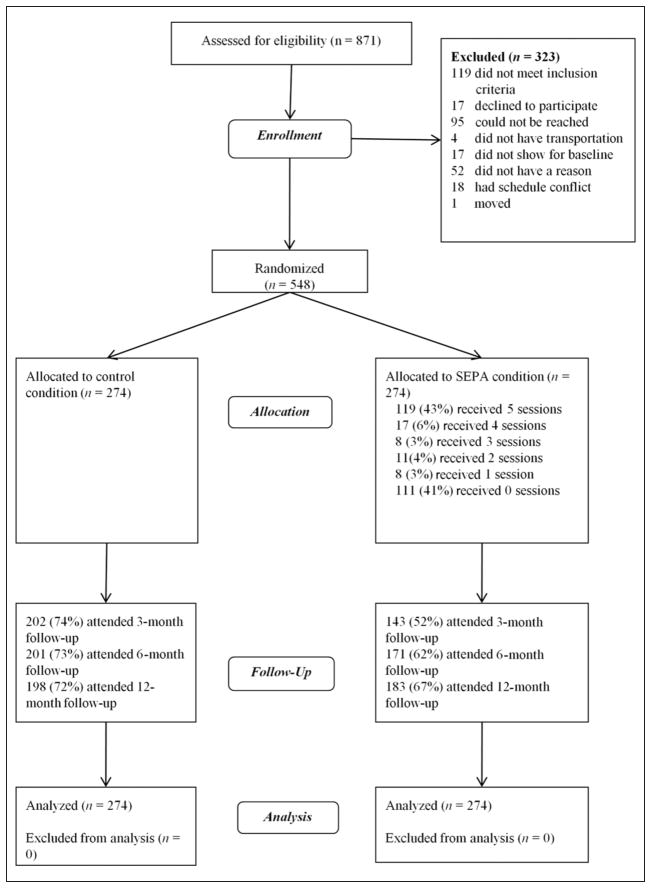
Participants in this study were 274 women assigned to receive the group intervention in the second randomized trial of SEPA (Peragallo et al., 2011). Figure 1 shows participant flow through the study. Eligibility criteria were as follows: self-identifying as Hispanic, aged between 18 and 50 years, and reporting sexual intercourse in the past 3 months. The sample size of the trial was determined to have sufficient power (.80) to detect a small difference in condom use between the SEPA and control condition (Peragallo et al., 2005). Table 1 shows characteristics of the women assigned to the SEPA group intervention. The control condition of the randomized trial was a delayed intervention with a brief version of SEPA. Those participants are not included in the current study.
Figure 1. CONSORT participant flow diagram.
Note: SEPA = Salud, Educación, Prevención y Autocuidado [Health, Education, Prevention, and Self-Care].
Table 1.
Baseline Characteristics of Women Assigned to the SEPA Intervention.
| Characteristic | SEPA (n = 274) |
|---|---|
| Age in years, M (SD) | 37.31 (8.34) |
| Education in years, M (SD) | 13.62 (3.38) |
| Employed, n (%) | 92 (34) |
| Monthly after-tax family incomea, n (%) | |
| ≤US$2000 | 194 (71) |
| US$2000-US$3000 | 41 (15) |
| ≥US$3000 | 37 (14) |
| Years in the United States, M (SD) | 11.84 (10.78) |
| Born outside of the United States, n (%) | 256 (93) |
| Americanism, M (SD) | 2.40 (0.79) |
| Hispanicism, M (SD) | 3.53 (0.44) |
| Living with partner, n (%) | 181 (66) |
| Number of sexual partners (past 3 months), M (SD) | 1.11 (0.65) |
| Intimate partner violence, M (SD) | 0.41 (0.52) |
| Physical violence, n (%) | 25 (9) |
| Forced sex, n (%) | 6 (2) |
| Emotional violence, n (%) | 182 (66) |
| Response to violence, n (%) | 11 (4) |
Note: SEPA = Salud, Educación, Prevención y Autocuidado [Health, Education, Prevention, and Self-Care].
Two women did not report their income.
Procedures
The University of Miami and Florida Department of Health and Human Services Institutional Review Boards approved the study prior to recruitment. Participants were recruited from (a) a community-based social service (e.g., English classes, child care, job development and placement, and health education) organization for Hispanics, (b) an urban Florida Department of Health site, and (c) flyers posted in the community. Study participants also referred family members and friends to the study. The study was conducted between January 2008 and April 2009. After recruitment and informed consent, women were interviewed by trained bilingual female research team members using a standardized protocol and a structured interview (questionnaire) in offices at or near a community service agency. The average length of the interview was 2 hrs. Assessors asked participants questions and recorded answers using a web-based research management software system (e-Velos). Participants were compensated US$50 for travel expenses and their time at assessments, and US$20 for attending the group sessions. To foster retention in the study, study staff obtained and used information for multiple participant contacts, and offered interviews at convenient, comfortable sites.
Intervention
SEPA is a sexual health group intervention developed for Hispanic women. The SEPA intervention is guided by a conceptual framework that integrates the social-cognitive model of behavioral change (Bandura, 1977) for the content and activities of the intervention, and Friere’s (1970) pedagogy for the delivery and contextual tailoring of the intervention. The intervention consisted of five 2-hr sessions delivered to small groups of women (M = 4.79, SD = 1.97). Session content included HIV and AIDS in the Hispanic community, sexually transmitted infections, prevention of HIV and AIDS (e.g., condom use), negotiation and communication with the partner, IPV, and substance abuse. Skill-building techniques included role-play, participatory sessions, videos, and discussions. Five Hispanic female facilitators with a range of education (bachelors to doctoral) delivered the intervention. Interventions took place in community sites that were easily accessible to the participants. If a woman missed a group meeting, study staff would meet with the women before the following session to ask them to attend an available concurrent session.
Measures
The predictor measures reported in this study are from the larger battery of measures collected at baseline in the parent trial.
Engagement Into Treatment
This was defined as the women attending at least two sessions. This definition is consistent with previous intervention participation research (Coatsworth, Santisteban, McBride, & Szapocznik, 2001; Mitrani, Feaster, Weiss-Laxer, & McCabe, 2011; Mitrani, Prado, Feaster, Robinson-Batista, & Szapocznik, 2003). For analyses, nonengaged women were coded as zero and engaged as one.
Demographics
These (e.g., country of origin, years living in the United States, income, education) were collected at the beginning of the assessments through administration of a standardized form designed for studies of Hispanic samples. This form was developed at the research center at which the parent study was conducted.
Competing Obligations
This was derived from the following variables in the demographics form: the number of minors living with the woman, living with a partner (1 = living with a sexual partner, 0 = not), and employment (1 = employed, 0 = not employed).
IPV
This was assessed with a modified version of the Partner-to-You scale from the Revised Conflict Tactics Scale short form (Straus & Douglas, 2004). Respondents report how often 12 behaviors (e.g., “insulted you,” “beat you up,” “forced you to have sex”) occur on a 4-point scale (0 = never, 1 = once, 2 = twice, 3 = three or more times) in the past 3 months. These items were summed into a total score. In this sample, Cronbach’s alpha was .85. These items were categorized into four subareas: emotional violence, physical violence, forced sex, and response to violence.
Depressive Symptoms
The Center for Epidemiologic Studies–Depression Scale (CES-D; Radloff, 1977) has 20 questions addressing the frequency (0 = rarely or none of the time, 3 = most of the time) of depressive symptoms experienced in the past week. The Spanish version described by Roberts, Vernon, and Rhoades (1989) was used. Responses to each item are added for a total ranging from 0 to 60. In the current sample, the scale had very high reliability (α = .94).
Hispanic Cultural Factors
Hispanic stress was assessed with the Hispanic Stress Inventory (Cervantes, Padilla, & Salgado de Snyder, 1991). The immigrant version of this scale was used as the vast majority of the sample was foreign-born (93%). The original version includes five subscales that measure Economic Stress, Parental Stress, Family/Cultural Stress, Marital Stress, and Immigration Stress via 73 items. The Parental Stress subscale was not used in this study because not all of the participants were parents. Responses to these items screen for common stressors Hispanics face in the United States by asking participants whether they have experienced these stressors.
If participants respond “yes,” they are asked to evaluate how much this stressor affected them. Two scores are calculated for each subscale. The Economic, Family/Cultural, Marital, and Immigration Stress subscales had high reliability (α = .76, .80, .74, .82, respectively). In this study, the total number of stressors was used to represent Hispanic stress because the subscales were significantly correlated, rs = .34 to .58.
Acculturation
This was measured with the Bidimensional Acculturation Scale (Marín & Gamba, 1996), which consists of 24 items that measure acculturation in a bidimensional manner. This scale has two subscales that measure how acculturated Hispanics are to American culture (Americanism) and to their culture of origin (Hispanicism). Americanism and Hispanicism are calculated by adding and averaging the responses to the 12 questions in each of these cultural domains. Scores for each domain can range from 1 to 4. In this sample, both acculturation scales had high reliability: Americanism (α = .95) and Hispanicism (α = .85).
Familism
This was assessed with the Familism scale (Sabogal, Marín, Otero-Sabogal, Marín, & Perez-Stable, 1987). This scale was created to assess the Hispanic cultural value that emphasizes the important role of family and loyalty, and responsibility to them. The scale contains 15 items organized into three areas: (a) family obligations (6 items) indexes perceived obligation to assist the family (e.g., “A person should share her home with uncles, aunts, or first cousins if they are in need”), (b) family support (3 items) assesses beliefs that the family should be a source of social support (e.g., “One can count on help from her relatives to solve most problems”), and (c) family as referent (5 items) assesses the belief that relatives should be used as behavioral and attitudinal referents (e.g., “One should be embarrassed by the bad things done by members of his family”). These subscales were summed into a total Familism scale. In this sample, reliability was acceptable (α = .74).
Results
More than half (n = 155, 57%) of the women randomized to SEPA engaged into the treatment. The nonengagers consisted of 119 women, 111 of whom did not attend any sessions and 8 women who only attended a single session. On average, women randomized to SEPA attended 2.62 (SD = 2.34) group sessions. Women who engaged (attended at least two group sessions) attended an average of 4.57 (SD = 0.88) sessions, and the majority (n = 119, 77%) attended all five group sessions. There were no differences in participant engagement rates between intervention facilitators, χ2(df = 4, N = 163) = 3.43, p = .488.
Hypothesis Tests
Separate univariate chi-square and logistic regression analyses were used to test the relationship of the 10 hypothesized predictors to engagement. As shown in Table 2, only three variables predicted engagement in univariate regression analyses. Higher levels of education, B = 0.12, SE = 0.04, p = .002; IPV, B = 0.62, SE = 0.26, p = .016; and Americanism, B = 0.44, SE = 0.16, p = .006, were all associated with higher odds of engagement.
Table 2.
Results of Univariate Analyses to Predict Engagement Into Treatment.
| Variable | χ2 | df | p |
|---|---|---|---|
| Live with partner | 0.08 | 1.00 | .776 |
| Employed | 0.62 | 1.00 | .432 |
|
| |||
| B | SE | p | |
|
| |||
| Education | 0.12 | 0.04 | .002 |
| No. of minors in home | −0.08 | 0.14 | .539 |
| Intimate partner violence | 0.62 | 0.26 | .016 |
| Depressive symptoms | −0.01 | 0.01 | .554 |
| Hispanic stress | 0.01 | 0.01 | .436 |
| Hispanicism | −0.25 | 0.28 | .369 |
| Americanism | 0.44 | 0.16 | .006 |
| Familism | −0.29 | 0.22 | .192 |
Note: Significant predictors are shown in bold.
All three of the variables (education, IPV, and Americanism) that were univariate predictors of engagement in the initial analyses remained significant predictors after controlling for the effects of the other two in a single multivariate follow-up logistic regression analysis. Results of the multivariate analysis showed that six additional years of education (approximately 2 SD in this sample) corresponded to about twice the odds of engagement, B = 0.12, SE = 0.04, p = .002, odds ratio (OR) = 1.13; every additional item of IPV endorsed by the woman was related to nearly twice the odds of engaging in the intervention, B = 0.67, SE = 0.28, p = .015, OR = 1.96; and women were nearly 1.5 times at greater odds of engaging in treatment for a one-unit increase in Americanism, B = 0.34, SE = 0.16, p = .040, OR = 1.40.
Follow-Up Analyses
Because IPV worked in the opposite direction than hypothesized, we sought to gain a better understanding of this phenomenon through follow-up analyses. These analyses tested the relationship between each of four subscales from the IPV measure (emotional violence, physical violence, forced sex, and response to violence) to engagement in separate chi-square analyses. We used dichotomous IPV variables because we were interested in knowing whether the presence of one or more types of IPV was associated with engagement and because these subscales had widely different scales and variability. Only physical violence, χ2(1, N = 274) = 4.23, p = .040, OR = 2.63, was associated with engagement into treatment. Experiencing forced sex, χ2(1, N = 274) = 1.79, p = .181, was not a statistically significant predictor, although the effect size (OR = 3.93) was larger than with physical violence. In a sample with a larger number of women reporting forced sex, this may have been statistically significant. Emotional violence, χ2(1, N = 274) = 1.09, p = .297, and the response to violence, χ2(1, N = 274) = 0.02, p = .890, were not related to engagement.
Although the definition of engagement used in this study (attending two or more sessions) was consistent with past research, only eight women did not return for a second session after having attended a first session. This indicated that attending a single session was an important milestone in participation. As a follow-up, we tested whether the predictor variables that were related to engagement, defined as attending two or more sessions, also predicted whether a woman attended one session versus no sessions, using a single multivariate logistic regression analysis. All three variables, education, B = 0.11, SE = 0.04, p = .003; IPV, B = 0.58, SE = 0.26, p = .021; but not Americanism, B = 0.37, SE = 0.16, p = .109, were significant predictors of attending at least one session.
Discussion
The results of this study indicated that three predictors, education, IPV, and Americanism, were associated with women engaging in the SEPA intervention. The other hypothesized variables, related to competing role obligations, depressive symptoms, and Hispanic cultural identity and experiences, were not associated with engagement. Thus, the current study did not reproduce the findings of the SEPA engagement study (Kim et al., 2006), even though the measures were the same across studies. Specifically, employment, depressive symptoms, age, and low intention to reduce risk behaviors predicted engagement in the first SEPA trial, but none of these variables predicted engagement in the current SEPA trial. Discrepancies between these two findings may have been due to the different study environments. Although SEPA I took place in Chicago, where Hispanics are a minority (29%), SEPA II took place in Miami and Hollywood (Florida), two cities where Hispanics represent a larger proportion of the population (70% and 33%, respectively; U.S. Census Bureau, 2012). It may be that more populated Hispanic cities provide more formal and informal support systems that buffer the effects that these variables may have on engagement. More research needs to be conducted to describe how the environment where Hispanics reside may interact with individual level factors to impact health behaviors. Unlike in SEPA I, women were born in many more countries (Table 3), which made it difficult to compare engagement rates to nativity. However, there was no difference in engagement between women born in the United States and those born outside the United States, χ2(1, N = 274) = 0.02, p = .904.
Table 3.
Countries of Origin for Women in SEPA Condition.
| Country of origin | N | % |
|---|---|---|
| Cuba | 34 | 12 |
| Dominican Republic | 10 | 4 |
| Puerto Rico | 15 | 5 |
| Guatemala | 1 | <1 |
| Mexico | 6 | 2 |
| El Salvador | 7 | 3 |
| Honduras | 12 | 4 |
| Nicaragua | 20 | 7 |
| Panama | 4 | 1 |
| Colombia | 96 | 35 |
| Venezuela | 11 | 4 |
| Ecuador | 2 | 1 |
| Peru | 28 | 10 |
| Argentina | 5 | 2 |
| Paraguay | 1 | <1 |
| Uruguay | 2 | 1 |
| United States | 18 | 7 |
| Other/unknown | 2 | 1 |
Note: SEPA = Salud, Educación, Prevención y Autocuidado [Health, Education, Prevention, and Self-Care].
IPV had the opposite effect from what we hypothesized. We presumed that women experiencing IPV would feel restricted in being able to attend the intervention, but we found that physical violence from a partner actually spurred, rather than inhibited, engagement. Women who were experiencing difficulties with partners may have been attracted to the study by the recruitment flyer, which mentioned discussion “about communication with partner, HIV and drug prevention, violence and risky behaviors in your communities.” It is possible that the barrier, if any, of having a violent partner would have manifested itself earlier in the process, so that women would not have enrolled in the study if they feared reprisals from partners. Women who experienced violence might have been interested in learning how to reduce domestic violence and how to improve communication with their partners. The presentation of both of these topics occurred after the first session. This study demonstrates that Hispanic women who are experiencing violence in relationships are amenable and able to follow through with receiving group educational/supportive interventions addressing HIV and IPV. In addition, this finding also supports the importance of embedding primary and secondary prevention strategies for IPV within existing community-based health programs that are not identified as targeting victims of IPV.
This study used a bidimensional approach to assessing acculturation. Americanism was associated with engagement, but Hispanicism and the other factors tapping identification with Hispanic cultural values/experiences were neither a barrier nor facilitator of engagement. It is noteworthy that Hispanicism scores in this sample were high across the board, so that the more Americanized women were likely to be bicultural rather than alienated from Hispanic culture. The SEPA intervention was culturally tailored for Hispanic women, and study procedures were designed to be accessible and welcoming for Hispanic women across a spectrum of acculturation—All staff were fully bilingual, SEPA groups were available in Spanish and English, and the study was conducted at community sites. The program’s ability to engage, specifically returning to a second session after attending a first session, Americanized women is encouraging given research suggesting that acculturation may be associated with elevated risk for HIV (Moreno & El-Bassel, 2007; Rojas-Guyler, Ellis, & Sanders, 2005) and IPV (Caetano, Ramisetty-Mikler, Caetano Vaeth, & Harris, 2007) among Hispanic women.
Some limitations of this study should be noted when interpreting results. The use of a convenience sample limits generalizability. Also, Hispanics are a heterogeneous group, so it is possible that predictors of engagement differ in Hispanic women from other geographic areas (as in fact they were in the first SEPA trial, which was conducted in a different region of the United States). The engagement process should be studied further as SEPA is disseminated with different populations. Self-report measures are subject to several biases, including imperfect recall and perceived social pressures. The IPV measure in this study was the woman’s report. However, it should be noted that other measures of IPV, for example, reports to authorities, also have well-known drawbacks. Acculturation is a complex, multidimensional process. Although the acculturation measure used in this study improved on single-item measures (e.g., language preference) by assessing two dimensions of acculturation, the use of multidimensional measures could further address the complexity of the acculturation process. Finally, research has suggested a u-shaped relationship between IPV and acculturation such that couples with moderate levels of acculturation are at higher risk for IPV than couples with lower levels of acculturation or couples with higher levels of acculturation (Caetano, Ramisetty-Mikler, & McGrath, 2004). This study did not specifically examine the relationship between IPV and acculturation, but did show they had independent links to engagement. Future longitudinal research should examine the specific pathways between acculturation, IPV, HIV risk behaviors, and engagement in prevention programs.
The intersection of HIV and IPV among Hispanic women calls for interventions addressing the gender-related pathways that serve as common mechanisms for both of these conditions. However, offering such interventions does not guarantee they will be utilized, and programs must be designed to engage the women who need them most. The results of this study demonstrate that women experiencing physical violence from an intimate partner, who were more Americanized and/or were more educated were more likely to engage in a culturally tailored HIV/IPV prevention intervention. Two out of three of these findings are encouraging, given the elevated risk of women who are already experiencing IPV and who are more acculturated. Women who experience IPV are willing to participate in group interventions, including interventions targeting other outcomes. We recommend that IPV prevention/reduction interventions be combined with other interventions whenever feasible to meet the needs of women who experience IPV. Further program development and outreach work is needed to engage women with low levels of education, as they are also particularly vulnerable. We recommend that future program development be informed by clarifying the reasons that women with less formal education were less likely to engage, for example, whether engagement was driven by aspects of the intervention itself or by external factors, such as location, timing, or availability of transportation.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the National Center on Minority Health and Health Disparities Grant 2P60 MD002266—Center of Excellence for Health Disparities Research: El Centro (Nilda Peragallo, Principal Investigator).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Reprints and permissions: sagepub.com/journalsPermissions.nav
References
- Amaro H. Love, sex, and power: Considering women’s realities in HIV prevention. American Psychologist. 1995;50:437–447. doi: 10.1037/0003-066X.50.6.437. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Bonomi AE, Anderson ML, Cannon EA, Slesnick N, Rodriguez MA. Intimate partner violence in Latina and non-Latina women. American Journal of Preventive Medicine. 2009;36:43–48. doi: 10.1016/j.amepre.2008.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Field CA, Ramisetty-Mikler S, McGrath C. The 5-year course of intimate partner violence among white, black, and Hispanic couples in the United States. Journal of Interpersonal Violence. 2005;20:1039–1057. doi: 10.1177/0886260505277783. [DOI] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Caetano Vaeth PA, Harris TR. Acculturation, stress, drinking, and intimate partner violence among Hispanic couples in the U.S. Journal of Interpersonal Violence. 2007;22:1431–1447. doi: 10.1177/0886260507305568. [DOI] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, McGrath C. Acculturation, drinking, and intimate partner violence among Hispanic couples in the United States: A longitudinal study. Hispanic Journal of Behavioral Sciences. 2004;26:60–78. doi: 10.1177/0739986303261812. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance report diagnoses of HIV infection and AIDS in the United States and dependent areas, 2008. 2010 Retrieved from http://www.cdc.gov/hiv/surveillance/resources/reports/2008report/pdf/2008SurveillanceReport.pdf.
- Centers for Disease Control and Prevention. HIV infection—United States, 2005 and 2008. CDC health disparities and inequalities report—United States, 2011. Morbidity and Mortality Weekly Report. 2011a May;60:87–89. [Google Scholar]
- Centers for Disease Control and Prevention. Surveillance of health status in minority communities—Racial and ethnic approaches to community health across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morbidity and Mortality Weekly Report. 2011b May;60:1–41. [PubMed] [Google Scholar]
- Cervantes RC, Padilla AM, Salgado de Snyder N. The Hispanic Stress Inventory: A culturally relevant approach to psychosocial assessment. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:438–447. doi: 10.1037/1040-3590.3.3.438. [DOI] [Google Scholar]
- Coatsworth JD, Santisteban DA, McBride CK, Szapocznik J. Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process. 2001;40:313–332. doi: 10.1111/j.1545-5300.2001.4030100313.x. [DOI] [PubMed] [Google Scholar]
- Cunradi CB, Caetano R, Clark C, Schaefer J. Neighborhood poverty as a predictor of intimate partner violence among white, black, and Hispanic couples in the United States: A multilevel analysis. Annals of Epidemiology. 2000;10:297–308. doi: 10.1016/s1047-2797(00)00052-1. [DOI] [PubMed] [Google Scholar]
- Davila YR, Bonilla E, Gonzalez-Ramirez D, Villaruel AM. HIV-IPV prevention: Perceptions of what Latinas want and need. Hispanic Health Care International. 2007;5:101–108. doi: 10.1891/1540-4153.5.3.101. [DOI] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care. 2002;40:52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Freire P. Pedagogy of the Oppressed. New York, NY: Continuum; 1970. [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma, Violence, & Abuse. 2007;8:178–198. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- González-Guarda RM, Peragallo N, Urrutia MT, Vasquez EP, Mitrani VB. HIV risks, substance abuse, and intimate partner violence among Hispanic women and their intimate partners. Journal of the Association of Nurses in AIDS Care. 2008;19:252–266. doi: 10.1016/j.jana.2008.04.001. [DOI] [PubMed] [Google Scholar]
- González-Guarda RM, Vasquez EP, Urrutia MT, Villaruel AM, Peragallo N. Hispanic women’s experiences with substance abuse, intimate partner violence, and risk for HIV. Journal of Transcultural Nursing. 2011;22:46–54. doi: 10.1177/1043659610387079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YJ, Peragallo N, DeForge B. Predictors of participation in an HIV risk reduction intervention for socially deprived Latino women: A cross sectional cohort study. International Journal of Nursing Studies. 2006;43:527–534. doi: 10.1016/j.ijnurstu.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Krishnan S, Dunbar MS, Minnis AM, Medlin CA, Gerdts CE, Padian NS. Poverty, gender inequities, and women’s risk of human immunodeficiency virus/AIDS. Annals of the New York Academy of Sciences. 2008;1136:101–110. doi: 10.1196/annals.1425.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanouette NM, Folsom DP, Sciolla A, Jeste DV. Psychotropic medication nonadherence among United States Latinos: A comprehensive literature review. Psychiatric Services. 2009;60:157–174. doi: 10.1176/appi.ps.60.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsky S, Caetano R, Roy-Byrne P. Racial and ethnic disparities in police-reported intimate partner violence and risk of hospitalization among women. Women’s Health Issues. 2009;19:109–118. doi: 10.1016/j.whi.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín G, Gamba RJ. A new measurement of acculturation for Hispanics: The bidimensional acculturation scale for Hispanics (BAS) Hispanic Journal of Behavioral Sciences. 1996;18:297–316. doi: 10.1177/07399863960183002. [DOI] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, Diniz JB. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders. 2011;44:412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, Feaster DJ, Weiss-Laxer NS, McCabe BE. Malaise, motivation, and motherhood: Predictors of engagement in behavioral interventions from a randomized controlled trial for HIV+ women in drug abuse recovery. AIDS and Behavior. 2011;15:396–406. doi: 10.1007/s10461-010-9714-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, Prado G, Feaster DJ, Robinson-Batista C, Szapocznik J. Relational factors and family treatment engagement among low-income, HIV-positive African American mothers. Family Process. 2003;42:31–45. doi: 10.1111/j.1545-300.2003.00031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno CL. The relationship between culture, gender, structural factors, abuse, trauma and HIV/AIDS for Latinas. Qualitative Health Research. 2007;17:340–352. doi: 10.1177/1049732306297387. [DOI] [PubMed] [Google Scholar]
- Moreno CL, El-Bassel N. Dominican and Puerto Rican women in partnerships and their sexual risk behaviors. Hispanic Journal of Behavioral Sciences. 2007;29:336–348. doi: 10.1177/0739986307303756. [DOI] [Google Scholar]
- Newcomb MD, Carmona JV. Adult trauma and HIV status among Latinas: Effects upon psychological adjustment and substance abuse. AIDS and Behavior. 2004;8:417–428. doi: 10.1007/s10464-004-7326-1. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, Schlesinger HJ. Women and outpatient mental health services: Use by black, Hispanic, and white women in a national insured population. Journal of Mental Health Administration. 1994;21:347–360. doi: 10.1007/BF02521354. [DOI] [PubMed] [Google Scholar]
- Peragallo N, Deforge B, O’Campo P, Lee SM, Kim YJ, Cianelli R, Ferrer L. A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nursing Research. 2005;54:108–118. doi: 10.1097/00006199-200503000-00005. [DOI] [PubMed] [Google Scholar]
- Peragallo NP, González-Guarda RM, McCabe BE, Cianelli R. The efficacy of an HIV risk reduction program for Hispanic women. AIDS and Behavior. 2011 doi: 10.1007/s10461-011-0052-6. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Hispanic Research Center. When labels don’t fit: Hispanic and their views of identity. 2012 Retrieved from http://www.pewhispanic.org/2012/04/04/whenlabels-dont-fit-hispanics-and-their-views-of-identity/
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Raj A, Silverman JG, Amaro H. Abused women report greater male partner risk and gender-based risk for HIV: Findings from a community-based study with Hispanic women. AIDS Care. 2004;16:519–529. doi: 10.1080/09540120410001683448. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Vernon SW, Rhoades HM. Effects of language and ethnic status on reliability and validity of the Center for Epidemiologic Studies–Depression Scale with psychiatric patients. Journal of Nervous and Mental Disease. 1989;177:581–592. doi: 10.1097/00005053-198910000-00001. [DOI] [PubMed] [Google Scholar]
- Rojas-Guyler L, Ellis N, Sanders S. Acculturation, health protective sexual communication, and HIV/AIDS risk behavior among Hispanic women in a large Midwestern city. Health Education & Behavior. 2005;32:767–779. doi: 10.1177/1090198105277330. [DOI] [PubMed] [Google Scholar]
- Sabogal F, Marín G, Otero-Sabogal R, Marín BV, Perez-Stable EJ. Hispanic familism and acculturation: What changes and what doesn’t? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. doi: 10.1177/07399863870094003. [DOI] [Google Scholar]
- Sareen J, Pagura J, Grant B. Is intimate partner violence associated with HIV infection among women in the United States? General Hospital Psychiatry. 2009;31:274–278. doi: 10.1016/j.genhosppsych.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Straus MA, Douglas EM. A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence and Victims. 2004;19:507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. State & county quickfacts. 2012 Retrieved from http://quickfacts.census.gov/qfd/states/12/1245000.html.