Abstract
Laypeople and healthcare professionals use demographic cues when making pain management decisions. These decisions can negatively affect patient outcomes. This study examined whether laypeople base their pain management decisions in part on pain-related postures and demographic cues. Virtual human (VH) technology was used to research whether sex and race, as well as body posture, influenced pain management decisions. Ninety-seven laypersons examined VH patients exhibiting low back pain related body postures whose demographic cues varied by VH sex and VH race. T tests validated that participants were able to distinguish between high pain related body postures and low pain related body postures. The participants assessed male VH patients to be experiencing more pain than female VH patients. This study suggests that participants use sex as a cue when assessing pain. Participants may perceive VH male patients as experiencing high pain intensity if the participants are willing to counter male stereotypes and acknowledge that the male VH patients display pain behaviors.
Introduction
Research on sex and race has been conducted in both medical and nonmedical settings. Such research considers whether decision making is influenced, at least in part, by sex and race.1–3 One area of medical research that has identified biases in patient assessment and treatment is pain research. The pain literature previously has found that undergraduates, healthcare trainees, and healthcare professionals use sex and race to influence their pain assessment and treatment decisions.4–7 Sex and race cue use may bias pain assessment, independent of pain level. At present, there are no medical or mechanistic reasons that patients should be treated or assessed differently because of their sex or race.
Unbiased assessment of patient pain behaviors (i.e., behaviors that serve to communicate that a person is experiencing pain) is important because clinicians generally must draw conclusions about their patients' pain experience based on their observation of those pain behaviors.8,9 Observing patients' pain behaviors is also a key way for healthcare providers to assess their patients' pain in situations where patients cannot describe their pain verbally, or when there may be significant factors influencing a patient's verbal pain report.9 Pain behavior assessment, whether standardized or anecdotal, is very likely to be a part of every clinical encounter. It is important to understand how nonpain cues such as race and sex influence healthcare professionals' pain assessment and treatment decisions.
Healthcare professionals frequently rely on facial expressions. Facial expressions are readily accessible, continuously available, and change rapidly depending on the level of pain.10 Examples of facial expressions that display pain are brow lowering, tightening of the orbital muscles, nose wrinkling/upper lip raising, and eye closure.10 Pain-related body postures are also a reliable method of pain assessment.8,9,11 Five pain behaviors that are commonly associated with back pain are guarded movement, bracing, rubbing, touching the painful area, grimacing, and sighing.8 Healthcare professionals can view the pain-related body postures while walking the patient to or from an exam room and while meeting with the patient. However, there has been limited research on whether the assessment of pain-related body postures is influenced by gender and race, similar to the influence of demographic cue use in the evaluation of facial pain expression. In order to answer this question, the study examined pain-related body postures of patients experiencing low back pain because low back pain is one of the most common reasons patients seek medical treatment.12
Virtual human (VH) technology represents an innovative method for examining sex and race cues in pain assessment and treatment decisions. In previous VH research, investigators found that undergraduates, healthcare trainees, and healthcare professionals use gender and race, at least in part, to make pain assessment and treatment decisions.13–16 In these previous studies, participants assessed pain via VH facial expressions that have high visual and expressive fidelity in expressing high and low pain. Participants also read a scenario in which the VH-patients had been experiencing chronic back pain for more than a year. One criticism of the previous work was the lack of consideration of pain-related body postures as cues for pain. However, there is limited research on whether a patient's sex and race impacts the perception of the patient's pain-related body posture.
The current study sought to extend the literature by examining whether participants used the VHs' sex, race, and pain-related body postures to guide the pain assessment and treatment decisions of patients experiencing low back pain.
Method
Participants
A total of 97 University of Florida students (65 women) completed the study. The majority of the participants were Caucasian (62%). The rest of the sample was composed of Asians (24%), African-Americans (7%), and “other” (7%). The participants in the study were primarily Non-Hispanic (76%). The average age of the participants was 21.43 years, with a range of 18–44 years. All participants provided informed consent, and were compensated $15 for their participation.
Procedure
This study was approved by the Institutional Review Board (IRB) at the University of Florida. Participants were recruited via flyers posted throughout the University of Florida campus. Participants who expressed interest in participating in the study were directed to a secure, password protected Web site. Participants provided electronic consent and completed a demographic questionnaire. All of the participants observed 16 VH patient profiles presented in random order. The VH patient profiles are a novel, valid, and reliable method of researching how demographic cues affect a participant's pain assessment and treatment decisions. When observing a patient profile, participants read the following clinical vignette of a low back pain patient:
Patient presents with lower back pain for the past year of greater than 1 year duration. Patient reports that the pain began after a work-related lifting incident. The pain is located in the lumbar region of the back. The pain limits patient's ability to move around freely. Patient reports no prior surgical treatments and has current prescriptions for anti-inflammatory and analgesic medications.
In addition to reading the clinical vignette, participants viewed a 20-second looped video of the bodies of low pain and high pain expressing VH patients displaying back pain. Each of the 20-second looped VH patient videos contained two cues: VH sex (male, female) and VH race (Caucasian, African-American). The VH sex and VH race cues were portrayed by changing the VH patients' appearance (e.g., skin tone, hair color, hair length). Each cue combination was presented twice in order to achieve the optimal test sensitivity. In order to control for order effect, participants viewed all 16 VH videos in a random order. Participants were required to complete all VH profiles and were not permitted to skip or revisit a completed VH profile. Figures 1 and 2 depict still frame images of VH patients expressing high and low pain.
FIG. 1.
Still-frame of VH cues representing male sex, Caucasian race, and high pain expression.
FIG. 2.
Still-frame of VH cues representing female sex, African-American race, and low pain expression.
In order to obtain a realistic VH body displaying back pain, two physical therapists modeled how patients experiencing back pain (e.g., guarded movement, bracing, rubbing, and touching the painful area) and no back pain walk.8 The physical therapists' behavior was captured using Autodesk® MotionBuilder® that recorded the physical therapists' stick figures devoid of sex and race features. The two motion capture animations were created in order to represent accurately patients expressing high and low back pain. Validating the representativeness of the VH stick figure, 100% of a validation sample (17/17 participants) correctly identified high versus low pain stick figures. Figures 3 and 4 are still-frame images of the validated high pain and low pain stick figure motion captures. After the motion capture data were validated, VH bodies (e.g., those of men, women, Caucasians, and African-Americans) from Evolver® software were mapped onto the stick figures created in Autodesk® MotionBuilder®.
FIG. 3.

Still-frame of low pain expressing stick figure.
FIG. 4.
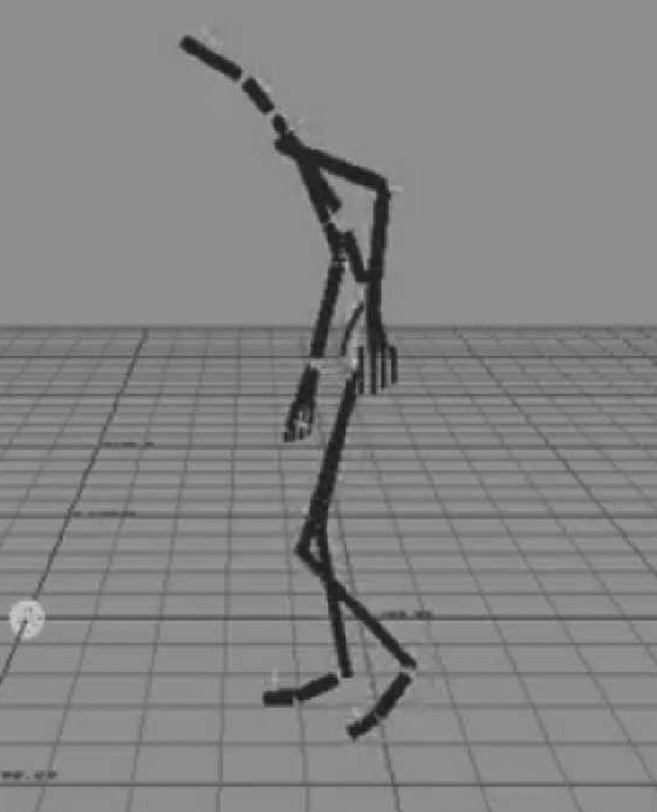
Still-frame of high pain expressing stick figure.
For each VH patient, participants rated the level of pain intensity and their willingness to administer opioids. Ratings were recorded on separate 100-point visual analogue scales (VAS). Endpoints ranged from “no pain sensation” to “most intense pain imaginable” (pain intensity), and “not at all likely” to “complete certainty” (willingness to administer opioid analgesics).
Statistical analysis
All data analyses were performed using SPSS for Windows (v20). Descriptive statistical analyses were conducted to summarize the demographic and background characteristics of the sample. Independent t test analyses were conducted to determine whether participants could distinguish between the VH patients' high and low pain expression. Repeated measures analysis of covariance was conducted to determine whether participants' sex influenced pain assessment and treatment ratings. Repeated measures analysis of variance (RANOVA) was performed to examine assessment and treatment decisions made by participants as a function of the VH patient's personal characteristics (sex and race). The virtual patient independent variables in this study are sex and race; the dependent variables include pain intensity and the willingness to administer opioid analgesics.
Results
Realism of VH bodies pain expression
Of the 97 participants who participated in the study, 86 (88.7%) indicated that the VH patients displayed realistic depictions of pain.
Validation of high and low pain expressing VH bodies
Participants rated pain intensity higher and were more willing to administer opioid analgesics to high pain expressing VH patients than to low pain expressing VH patients (p<0.05). The results of the t tests are consistent with previous research, and serve as validation of the VH pain expression stimuli. Since the participants were able to distinguish between high pain and low pain body behaviors, this study will only report on the high pain expressing bodies to examine laypeople's pain assessment and treatment decisions. Table 1 presents the results of the t test analyses.
Table 1.
Validating the Difference Between High and Low Pain Related Body Postures When Making Pain Assessment and Treatment Decisions
| Decision | Cue | Pain level | Mean | SD | t | Cohen's d |
|---|---|---|---|---|---|---|
|
Pain assessment | ||||||
| Pain intensity |
Female African-American |
Low pain expression |
17.17 |
14.45 |
−19.031*** |
−2.11 |
| |
|
High pain expression |
53.76 |
19.76 |
|
|
| |
Female Caucasian |
Low pain expression |
19.06 |
16.22 |
−15.56*** |
−0.68 |
| |
|
High pain expression |
53.59 |
20.47 |
|
|
| |
Male African-American |
Low pain expression |
20.49 |
16.45 |
−17.80*** |
−0.70 |
| |
|
High pain expression |
57.13 |
20.42 |
|
|
| |
Male Caucasian |
Low pain expression |
19.50 |
15.34 |
−19.82*** |
−0.73 |
| |
|
High Pain Expression |
57.05 |
19.72 |
|
|
|
Pain treatment | ||||||
| Administering opioid analgesics |
Female African-American |
Low pain expression |
17.97 |
20.58 |
−11.35*** |
−0.52 |
| |
|
High pain expression |
46.41 |
25.32 |
|
|
| |
Female Caucasian |
Low pain expression |
18.75 |
20.99 |
−10.40*** |
−0.49 |
| |
|
High pain expression |
44.95 |
25.17 |
|
|
| |
Male African-American |
Low pain expression |
18.00 |
18.49 |
−11.83*** |
−0.56 |
| |
|
High pain expression |
44.95 |
25.17 |
|
|
| |
Male Caucasian |
Low pain expression |
17.87 |
22.83 |
−12.49*** |
−0.50 |
| High pain expression | 47.63 | 28.99 | ||||
p<0.001.
Pain assessment and treatment RANOVAs
Pain assessment
Participants assessed VH patients who were male as having greater pain intensity than those who were female, F(1, 90)=11.74, p=0.001, partial η2=0.12. Table 2 presents the results for pain intensity.
Table 2.
Results of the RANOVA Analyses for Pain Assessment and Treatment Decisions
| Decision | Main effect/interaction | F | DF | Partial η2 |
|---|---|---|---|---|
|
Pain assessment | ||||
| Pain intensity |
VH sex |
11.740*** |
(1.90) |
0.115 |
| |
VH race |
0.017 |
(1.90) |
0.00 |
| |
VH race×VH sex |
5.86* |
(1.90) |
0.06 |
|
Pain treatment | ||||
| Willingness to administer opioid analgesics |
VH Sex |
2.302 |
(1.90) |
0.025 |
| |
VH Race |
0.376 |
(1.90) |
0.004 |
| VH Sex*VH Race | 0.600 | (1.90) | 0.007 | |
p<0.05; ***p<0.001.
Pain treatment
There were no significant findings for pain treatment ratings. Table 2 presents the nonsignificant results for willingness to administer opioid analgesics.
Participants' sex as a covariate
In order to determine whether participants' sex influences pain assessment and treatment ratings, participants' sex was included as a covariate in the RANCOVAs. The pain assessment and treatment RANCOVAs, however, were not statistically significant.
Discussion
Laypersons, healthcare trainees, and healthcare professionals are influenced by patient sex and race in their pain assessment and treatment decisions.13–16 There are a number of pain behavior assessment methodologies (direct observation of patients' pain behaviors via continuous observation, duration recording, frequency recording or interval recording, the Pain Behavior Observation System, actigraphy, etc.) that assess stereotypical nonverbal, and nonfacial expressions of pain.8,9,17 This is the first study to use VH technology to assess patients' pain-related body postures. The study found that, using this new VH technology, participants were able to distinguish reliably between patients' high and low pain related body postures. Similarly, 88.7% of the participants indicated that the VH patients in this study showed realistic depictions of pain.
There has been limited research examining whether sex and race influence pain assessment and treatment ratings based on pain-related body postures instead of pain-expressing faces. The current study addressed this gap in the literature by using VH technology to examine how VH sex and race influences pain-expressing body decision making. Unlike previous work that examined only facial expressions of pain, participants rated male VH patients as having greater pain than female VH patients when observing the same low back pain related behaviors. The study did not find VH race to impact participants' pain intensity ratings significantly. There were also no significant VH sex or race influences for willingness to administer opioids.
Typically, experimental research examining commonly held stereotypes of sex differences in pain are assessed via questionnaires, using the Gender Role Expectations of Pan Questionnaire (GREP),18,19 without the presence or aid of a visual pain cue. Gender role theories have suggested that men and women are socialized to respond differently to pain and have different expectations relative to pain perception. Previous gender role pain research has found that both men and women indicate that the typical woman is more willing to report pain, more sensitive to pain, and less likely to endure pain than the typical man.18 However, results of this study differ from previous work on gender role theories of pain and facial expressions of pain, where women were generally perceived as having more pain.13–16 It is possible that providing a behavioral display of pain via body posture and impaired movement may work in conjunction with these stereotypes to alter pain ratings, and may serve to counter stereotypical assessments. Previous clinical research suggests that healthcare providers perceive men as less likely to report experiencing pain, or displaying pain behaviors, unless they are experiencing high levels of pain.20 Clinical samples of chronic pain patients show small or nonsignificant sex differences for patients seeking care at a chronic pain clinic.21 In this study, both male VH patients and female VH patients displayed high pain intensity related body postures. The increased number of pain cues that can be gleaned from the full body posture may have led participants to rate the pain of male VH patients higher than female VH patients on the stereotypical belief that men who are willing to display pain postures must be in significantly greater pain than women. Unlike previous clinical studies where the male VH patients were more likely to be treated more aggressively than female VH patients, participants in this study were no less willing to administer opioid analgesics to female VH patients than they were to male VH patients.1
Results of this study also differ from previous work because this study did not find significant differences in pain intensity assessment or willingness to administer opioid analgesics to VHs of different races or ethnicities. There is fairly consistent evidence that racial/ethnic minorities suffer disproportionately from unrelieved pain and are less likely to receive pain medication than whites in clinical settings.22 It is possible that participants rely more heavily on race and ethnicity as a cue to make pain assessment and treatment decisions when observing facial pain expressions than when observing pain-related postures.
A limitation of this study, which could account for some of the differences from previous work, is that none of the participants were healthcare providers with prescription privileges or experience. It is possible that the participants in this study, unlike those which included healthcare professionals, did not feel as comfortable rating pain intensity or prescribing opioids at different rates to the VH patients. However, it was important to conduct the research first with laypeople to determine whether participants were able to distinguish pain-related body movements the VH patients performed before asking healthcare trainees or professionals to spend time evaluating the patients. Second, not only will a portion of this college educated sample go on to healthcare careers, but the expectations, attitudes, beliefs, and biases of laypersons about pain are important for a variety of health policy issues. These individuals represent consumers of healthcare and are voters.
There are multiple public health implications for the results of this study. While the results demonstrate that the participants were able to identify the VH-patients who were experiencing high and low pain correctly by observing their pain-related body postures, it is also apparent that participants used sex and race cues in addition to the VH patients' pain expressions to make their pain assessment and treatment decisions. The use of such sex and race cues, which are unrelated to the health of the patient, can result in pain not being appropriately treated—either under- or overtreated. Thus, another implication of the study is to suggest the benefits of implementing or improving existing pain management programs for healthcare professionals. In addition, the results of the study suggest that it would be beneficial to create pain education programs for laypeople likely to encounter others in pain, for example caregivers and coaches.
Future studies should also examine whether viewing both pain-related body postures and pain-expressing faces affects the use of demographic cues by participants when making pain management decisions. The contradictory findings from pain facial expression and postural expression make this an important next step, and will also increase the ecological validity of the findings. Additional work is needed to examine ways of influencing or altering the cue use based on best practices (which generally do not recommend race or sex as cues for pain assessment).
This study has several additional limitations. The participants in the study might represent a select sample, which would limit the generalizability of our findings. Also, the sample for this study was relatively homogenous, primarily women, Caucasians, and young adults. Participant responses might not be representative of actual healthcare professionals. It might be that the pain ratings of laypeople and their willingness to prescribe opioid analgesics is not the same as those of healthcare professionals or trainees. However, now that it is clear that the VH bodies can be used to evaluate pain assessment decision policies, this research can be extended to those populations.
In summary, this study found that participants rated male VH patients as having higher pain than female VH patients displaying the same pain behaviors. Future research may benefit from examining whether stereotypes about demographic groups influence patient pain assessment and treatment ratings. The results of this study, and previous VH studies, can inform future clinical practices, research, and education about the use of sex and race cues when making pain management decisions.
Acknowledgments
We thank the National Institute of Dental and Craniofacial Research (R01DE013208) for funding our research. This work was supported in part by grants to Dr. Michael Robinson from the National Institute of Dental and Craniofacial Research (R01DE013208).
Author Disclosure Statement
Although we do not think there is a conflict of interest for this paper, Lok does have ownership interest in Shadow Health, Inc. Shadow Health is an education company using virtual patients for nursing school education.
References
- 1.Borkhoff CM, Hawker FA, Wright JG. Patient gender affects the referral and recommendation for total joint arthroplasty. Clinical Orthopedics & Related Research 2011; 469:1829–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dijkstra AF, Verdonk P, Lagro-Janssen ALM. Gender bias in medical textbooks: examples from coronary heart disease, depression, alcohol abuse, and pharmacology. Medical Education 2008; 42:1021–8 [DOI] [PubMed] [Google Scholar]
- 3.Schneider DJ. (2005) Content of stereotypes: gender, race, and age. The psychology of stereotyping. New York: Guilford Press, pp. 434–73 [Google Scholar]
- 4.Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer 2000; 88:1929–38 [PubMed] [Google Scholar]
- 5.Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. New England Journal of Medicine 1994; 330:592–6 [DOI] [PubMed] [Google Scholar]
- 6.Edwards CL, Fillingim RB, Keefe F. Race, ethnicity, and pain. Pain 2001; 94:133–7 [DOI] [PubMed] [Google Scholar]
- 7.Robinson ME, Wise EA, Gagnon C, et al. Influences of gender role and anxiety on sex differences in temporal summation of pain. Journal of Pain 2004; 5:77–82 [DOI] [PubMed] [Google Scholar]
- 8.Keefe FJ, Wilkins RH, Cook WA. Direct observation of pain behaviors in low back pain patients during physical examination. Pain 1984; 20:59–68 [DOI] [PubMed] [Google Scholar]
- 9.Keefe FJ, Somers TJ, Williams DA, et al. , eds. (2011) Assessment of pain behaviors. New York: Guilford Press [Google Scholar]
- 10.Craig KD, Prkachin KM, Grunau RE, eds. (2011) The facial expression of pain. New York: Guilford Press [Google Scholar]
- 11.Keefe F, Block AR. Development of an observation method for assessing pain behavior in chronic low back pain patients. Behavior Therapy 1982; 13:363–75 [Google Scholar]
- 12.Watson PJ. (2011) Clinical assessment of low back pain. In Turk DC, Melzack R, eds. Handbook of pain assessment. 3rd ed. New York: Guilford Press, pp. 294–308 [Google Scholar]
- 13.Stutts LA, Hirsh AT, George SZ, et al. Investigating patient characteristics on pain assessment using virtual human technology. European Journal of Pain 2010; 14:1040–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hirsh AT, George SZ, Robinson ME. Pain assessment and treatment disparities: a virtual human technology investigation. Pain 2009; 143:106–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirsh AT, Alqudah AF, Stutts LA, et al. Virtual human technology: capturing sex, race, and age influences in individual pain decision policies. Pain 2009; 140:231–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wandner LD, Stutts LA, Alquadah AF, et al. Virtual human technology: patient demographics and healthcare training factors in pain observation and treatment recommendations. Journal of Pain Research 2010; 3:241–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prkachin KM. The consistency of facial expressions of pain: a comparison across modalities. Pain 1992; 51:297–306 [DOI] [PubMed] [Google Scholar]
- 18.Robinson ME, Riley JL, Myers CD, et al. Gender role expectations of pain: relationship to sex differences in pain. The Journal of Pain 2001; 2:251–7 [DOI] [PubMed] [Google Scholar]
- 19.Wise EA, Price DD, Myers CD, et al. Gender role expectations of pain: relationship to experimental pain perception. Pain 2002; 96:335–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myers CD, Riley JL, Robinson ME. Psychosocial contributions to sex-correlated differences in pain. The Clinical Journal of Pain 2003; 19:225–32 [DOI] [PubMed] [Google Scholar]
- 21.Robinson ME, Wise EA, Riley JL III, et al. Sex differences in clinical pain: a multisample study. Journal of Clinical Psychology in Medical Settings 1998; 5:413–24 [Google Scholar]
- 22.Shavers VL, Bakos A, Sheppard VB. Race, ethnicity, and pain among the U.S. adult population. Journal of Health Care for the Poor & Underserved 2010; 21:177–220 [DOI] [PubMed] [Google Scholar]




