Abstract
The SilverSneakers fitness program is a health plan benefit for Medicare beneficiaries that provides older adults with fitness center membership, customized group exercise classes, and a supportive social environment that promotes socialization among participants. This study evaluated the impact of the SilverSneakers program on physical and emotional health and activities of daily living (ADLs). A quasi-experimental retrospective analysis compared annual survey responses from SilverSneakers members (treatment N=5586) to a matched national random sample of Medicare Advantage organization beneficiaries (comparison N=22,344) in Cohort 10 of the Medicare Health Outcomes Survey. Matching was performed based on 6 demographic and 6 disease status variables. Survey responses from 2007 and 2009 were evaluated using categorical and logistic regression analysis. The treatment group showed significantly better physical and emotional health and lower impairment in both 2007 and 2009, less impairment for 4 of 6 ADLs in 2007, and all 6 in 2009, and a higher average number of days of good health within the prior month for both years. Three-year longitudinal analyses indicated a significantly more favorable survey response trend for the treatment group for nearly all measures of health and ADLs. Members who exercised less frequently had poorer health and functioning. Overall, participation in the SilverSneakers program was associated with more favorable overall physical and social/emotional health status and fewer activity impairments, suggesting that the provision of senior-oriented group fitness programs may be a valuable approach to improve quality of life and reduce the burden associated with declining health and functioning as older adults age. (Population Health Management 2013;16:364–372)
Introduction
The American population is undergoing a dramatic shift toward an older demographic, and the associated changes in the size and makeup of the US Medicare program are rapidly increasing federal health care spending accounted for by seniors in our society. In 2010, there were nearly 40 million adults age 65 and older covered by Medicare, a number projected to reach 79 million by 2030.1,2 Overall US health care spending is projected to rise from $2.7 trillion in 2011 to $4.6 trillion by 2020;3 spending on Medicare is projected to increase 6.9% per year from 2009 to 2019.4 The aging of the baby boomer generation and the current economic environment are creating tremendous pressure on the fiscal viability of Medicare as it currently stands. The most recent estimates (2011) are that the Medicare Hospital Insurance Trust Fund will be depleted in 2024, 5 years earlier than was reported in the year 2010 congressional report.1
Chronic disease and associated comorbidities also are taking on an ever-increasing role in driving Medicare spending. Nearly 91% of people age 65 and older have 1 or more chronic conditions; more than half of this population are treated for 5 or more conditions and this group accounts for a disproportionate amount of spending (79%).5,6 Approximately one fourth of people with chronic illness also have 1 or more limitations in activities of daily living (ADLs), such as walking, bathing, and dressing, and their health care spending often more than doubles in cost.5,7,8 Not surprisingly, most people with activity limitations are Medicare members.5
In addition to disease-related morbidity and functional decline, seniors often face loneliness, social isolation, and depression, which can have additional negative influences on their health and overall quality of life. These factors working in combination with chronic conditions and impairments can seriously compromise seniors' health and well-being. Social interactions have been shown to be associated with positive physiological benefits that can promote better health outcomes.9 A study conducted on the importance of self-rated health in myocardial infarction patients found that low social support, high anxiety, and depression were found to be predictive of poor self-related health, a valid predictor of health and mortality.10 Another study of seniors age 75 and older showed that less decline in future self-rated health was predicted by a more active physical and social life.11 Other research has indicated that strong social support is associated with improved quality of life in critically ill patients12 and is a significant predictor of 1-year mortality after acute myocardial infarction.13
Physical inactivity is a common risk factor among all Americans, but is particularly problematic in older adults and brings with it an increased risk of many chronic diseases and other poor health outcomes. A 2007 Centers for Disease Control and Prevention report showed that, based on Healthy People 2010 guidelines, only 39% of adults age 65 and older are getting the recommended amount of weekly physical activity (30 or minutes of moderate intensity activity 5 days per week, or 20 minutes of vigorous intensity activity 3 days per week).14 Alternatively, the benefits that seniors can gain from being physically active are well documented and extensive. As well as reducing the risk of chronic disease, being physically active can help seniors to strengthen bones and muscles, improve their ability to do daily activities, prevent falls, reduce the risk of depression, control weight, and increase life expectancy.15,16
To combat the negative effects of a sedentary lifestyle and the psychosocial issues that often accompany aging, fitness-based wellness programs developed for seniors are offered through certain health plans. Recent studies have reported the favorable health and financial impact of these programs. Nguyen and associates reported that participation in an exercise program benefit (SilverSneakers) was significantly associated with fewer hospital admissions and lower health care costs after 2 years.17 Additional studies of the same program found that participation also was associated with lower risk of depression,18 and those members who exercise more displayed a greater decrease in health care costs when compared to members who exercise less.19 Similarly, a study of a health maintenance organization-based senior physical activity program showed that participants had annual adjusted total costs that were $1186 lower than nonparticipants in the second year of the program.20 A separate study of Medicare-eligible adults demonstrated that members who participated in a community-based exercise program 1 or more times weekly had total health care costs that were 79.3% of those of the control study group.21
The American Recovery and Reinvestment Act of 2009 included $1.1 billion dollars to fund health-related comparative effectiveness research. In alignment with this federal initiative, further research is needed to better understand the impact of physical activity programs targeted at seniors. Further emphasizing this point, this research topic is also a key area of focus for the National Institutes of Health, which recently published a list of highest priority Challenge topics that specifies the need for comparative effectiveness research on disability prevention and risk-reduction strategies for older persons.22 The current study was undertaken to demonstrate the impact of participation in a physical activity program tailored to seniors (the SilverSneakers fitness program) offered by some Medicare Advantage, group retiree, and Medicare supplement plans. A comparative effectiveness framework using a retrospective matched comparison group was used to evaluate the hypothesis that SilverSneakers members would report better physical and emotional health, less impairment in ADLs, and a more favorable trend in these measures over time compared to similar seniors who did not participate in SilverSneakers.
Methods
A quasi-experimental retrospective analysis was conducted comparing annual health survey responses from SilverSneakers members to the general population of Medicare Advantage members. SilverSneakers provides older adults with fitness center membership and customized age appropriate fitness activities that focus on flexibility, strength, balance, and endurance. Program members have access to conditioning classes, exercise equipment, health education seminars, and other amenities and events that promote the benefits of a healthy lifestyle. Program members have assistance from an experienced Senior Advisor at the fitness center to help them get started in and get the most out of program activities. Members also have online access to member support programs that can help them lose weight, quit smoking, or reduce stress. Additionally, the program provides seniors with the opportunity to participate in social activities and fitness classes in an environment that promotes socialization with others in their age group as part of physical activities programs.
The treatment group (N=5586) is comprised of members who were continually enrolled in the SilverSneakers fitness program from 2007 to 2010 and who completed an annual survey each year. No stipulation was required as to when enrollment in the SilverSneakers program occurred prior to 2007; therefore, 2007 was considered a treatment year and, as such, there is no stipulated study baseline. The comparison group (N=22,344) was a matched sample of Medicare beneficiaries who participated in the 2007 and 2009 Medicare Health Outcomes Survey (HOS). This study was not submitted to an institutional review board because only existing de-identified survey data were used for this analysis in alignment with institutional review board exclusion criteria outlined in the Code of Federal Regulations.
The HOS is an annual Medicare managed care survey initiated in 1998 and conducted to monitor and evaluate the quality of care across all Medicare Advantage managed care organizations. A random sample of beneficiaries is drawn from each Medicare Advantage organization and surveyed during the spring of each year. The same sample is then surveyed again 2 years later using the same outcomes survey.23,24 The comparison group was drawn from HOS Cohort 10 (N=188,315), who took the survey in both 2007 and 2009. Comparison study group members were matched (exact) with random sampling at a 4-to-1 ratio to treatment group members based on age group, sex, race, education, marital status, body mass index group, number of reported health conditions, and reported status for the following diseases: congestive heart failure, coronary artery disease, diabetes, lung disease, and stroke.
The SilverSneakers program administers an annual survey that contains many of the same survey items used in the HOS. Survey responses from 2007 and 2009 for these shared items were used in study analyses. Eight separate survey items (questions) measuring physical and/or emotional health and physical functioning were used in analyses (Table 1). Responses for 6 of the 8 questions were recoded as categorical responses as shown in Table 1. Each item is referred to by its “measure name.” The emotional health item was not included in the SilverSneakers 2007 survey, ruling out a 2007-to-2009 longitudinal comparison for this question. However, treatment group data from 2008 and 2010 on this question were available and used as a substitute in conducting the longitudinal study group comparison. Members with out of range responses (>30) were excluded from analyses of the physical health and emotional health items.
Table 1.
Study Outcome Variables
| Measure name | Survey item | Item responses | Response classification |
|---|---|---|---|
| Health status |
In general, would you say your health is: |
Excellent |
Favorable |
| |
|
Very good |
|
| |
|
Good |
|
| |
|
Fair |
Unfavorable |
| |
|
Poor |
|
| Health status change |
Compared to 1 year ago, how would you rate your health in general now? |
Much better now than 1 year ago |
Favorable |
| |
|
Somewhat better now than 1 year ago |
|
| |
|
About the same as 1 year ago |
|
| |
|
Somewhat worse now than 1 year ago |
Unfavorable |
| |
|
Much worse now than 1 year ago |
|
| Functioning—Climbing stairs |
Does your health now limit you in [climbing several flights of stairs]? If so, how much? |
Yes, limited a lot |
Unfavorable |
| |
|
Yes, limited a little |
|
| |
|
No, not limited at all |
Favorable |
| Social limitations due to health |
During the past 4 weeks, how much of the time has your physical health or emotional problems interfered with your social activities (like visiting friends, relatives, etc.)? |
All of the time |
Unfavorable |
| |
|
Most of the time |
|
| |
|
Some of the time |
|
| |
|
A little of the time |
Favorable |
| |
|
None of the time |
|
| Work or activity limitations due to health |
During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of your physical health? -Were limited in the kind of work or other daily activities |
No, none of the time |
Favorable |
| |
|
Yes, a little of the time |
|
| |
|
Yes, some of the time |
Unfavorable |
| |
|
Yes, most of the time |
|
| |
|
Yes, all of the time |
|
| Physical health |
Thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good? |
Freeform (number of days) |
N/A |
| Emotional health |
Thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good? |
Freeform (number of days) |
N/A |
| Activities of daily living |
Because of a health or physical problem, do you have any difficulty doing the following activities? (separate responses for each following activity: bathing, dressing, eating, getting in or out of chairs, walking, using toilet) |
I am unable to do this activity |
Impaired |
| |
|
Yes, I have difficulty |
|
| No, I do not have difficulty | Not Impaired |
ADL responses were evaluated as the percent impaired for each ADL as well as using 2 different summary measures. For one summary measure, study members were compared based on the percentage of members with no reported ADL impairments. For the second summary measure, a disability index was calculated as previously published by Vita and colleagues.25 Responses for each ADL were recoded as: “I do not have difficulty”=0, “Yes, I have difficulty”=1, “I am unable to do this activity”=2. The index is calculated as the mean using these recoded values for the 5 ADL categories: dressing, eating, in-out of chair, walking, and hygiene. The most severe of the initial ADL responses for “bathing” and “using toilet” were used as the hygiene index input. Members with responses to 4 or more of the ADL index inputs are represented in the mean summary measures.
For statistical comparisons of the treatment and comparison group, within-year comparisons of dichotomized variables were conducted using the nonparametric Pearson chi-square test and longitudinal analyses of trend differences employed goodness-of-fit chi-square statistical testing. For continuous measures, within-year comparisons were conducted using the Wilcoxon 2-sample nonparametric test because of parametric assumptions not being met. Statistical comparisons of the change across years were carried out using the Satterthwaite t test.
Member physical activity was captured by self-report in the SilverSneakers survey. To evaluate the impact of frequency of exercise within the treatment group, focused analysis using 3 health survey items was conducted on treatment subgroups defined by the number of days each week that treatment group member reported 30 min or more of moderately intense physical activity (all at once or in at least 10-min blocks of time). An exercise frequency grouping variable was produced for 2007 and 2009, categorizing treatment members into exercise frequency subgroups defined as low (0–2 days), medium (3–4 days), and high (5–7 days) based on their survey responses. Analysis was limited to members with a populated exercise frequency level in both years and the same exercise frequency level in 2007 and 2009 (N=3046) to ensure the distinction between member exercise frequency subgroups. Multivariate logistic regression modeling was used to test if the exercise frequency was significantly associated with responses to 3 selected measures of health and functioning, while controlling for potential differences in treatment subgroups using all of the 12 matching variables in the analytical model. A variable (defined as 1 or 0) also was constructed for the analysis of change across years to differentiate members who maintained unfavorable status (as defined by the study question) or declined in status from 2007 to 2009 from those who maintained favorable status or improved over the same time frame. Multivariate logistic modeling was conducted using the constructed change variable to determine if exercise frequency is a significant predictor of change across years, while controlling for other demographic and morbidity indicators. Controlling for these factors was necessary in this analysis because no matched comparison group was available. Results are summarized as odds ratios (ORs) and associated 95% confidence intervals. Members with missing data were excluded from analyses requiring those data. Data manipulation and analysis was conducted using SAS version 9.2 software (SAS Institute Inc., Cary, NC).
Results
The matching procedure resulted in the production of study groups that were equivalent with respect to all matching variables. Population characteristics with respect to all matching variables are shown in Table 2.
Table 2.
Characteristics of Matched Study Groups
| Matching variable | Treatment N=5586 | Comparison N=22,344 |
|---|---|---|
| Age group* | ||
| Younger than 65 |
1.2% |
1.2% |
| 65 to 74 |
63.8% |
63.8% |
| 75 and older |
35.0% |
35.0% |
| Percent female* |
56.4% |
56.4% |
| Race* | ||
| White |
96.1% |
96.1% |
| Black |
1.9% |
1.9% |
| Other |
2.0% |
2.0% |
| Educational level* | ||
| <high school graduate or GED |
5.3% |
5.3% |
| High school graduate or GED |
35.5% |
35.5% |
| Greater than high school or GED |
59.2% |
59.2% |
| Percent married* |
70.2% |
70.2% |
| Percent obese (BMI 30 or above)* |
16.6% |
16.6% |
| Reported disease* | ||
| Congestive heart failure (COPD) |
1.1% |
1.1% |
| Angina pectoris or coronary artery disease |
7.1% |
7.1% |
| Diabetes, high blood sugar, or sugar in urine |
11.7% |
11.7% |
| Emphysema, asthma, or COPD |
6.6% |
6.6% |
| Stroke |
1.9% |
1.9% |
| Number of conditions* | ||
| 0 |
15.7% |
15.7% |
| 1 |
24.7% |
24.7% |
| 2 |
24.5% |
24.5% |
| 3 |
16.8% |
16.8% |
| 4 |
11.0% |
11.0% |
| 5 or more** | 7.4% | 7.4% |
Chi-square, P=1.0; **Matching was performed on specific number of conditions up to 9.
BMI, body mass index; GED, general equivalency degree; COPD, chronic obstructive pulmonary disease.
Table 3 presents comparisons of study groups with respect to 5 dichotomized physical and emotional health survey measures. The treatment group reported significantly better physical and emotional health relative to the comparison group for all 5 presented measures in both 2007 and 2009 (P<0.0001). Three-year longitudinal analyses indicated the treatment group had a significantly more favorable trend than the comparison group for 4 of the 5 measures evaluated.
Table 3.
Comparison of Physical and Emotional Health Measures
| |
|
2007 |
2009 |
|
|
||
|---|---|---|---|---|---|---|---|
| Survey measure | Study group | Total responses | % Unfavorable response | Total responses | % Unfavorable response | 2007 to 2009 change | Difference in change |
| Health status |
Treatment |
5548 |
3.7%* |
5393 |
4.3%* |
0.6% |
-2.4%*** |
| |
Comparison |
22,085 |
12.6% |
22040 |
15.6% |
3.0% |
|
| Health status change |
Treatment |
5542 |
3.1%* |
5370 |
4.7%* |
1.6% |
-2.2%*** |
| |
Comparison |
22,282 |
17.7% |
22146 |
21.5% |
3.8% |
|
| Functioning—Climbing stairs |
Treatment |
5466 |
35.6%* |
5020 |
39.3%* |
3.7% |
-2.2%** |
| |
Comparison |
21,584 |
48.4% |
21521 |
54.3% |
5.9% |
|
| Social limitations because of health |
Treatment |
5430 |
6.9%* |
5414 |
7.4%* |
0.5% |
-2.8%*** |
| |
Comparison |
22,242 |
15.6% |
22109 |
18.9% |
3.3% |
|
| Work or activity limitations because of health |
Treatment |
5447 |
17.1%* |
5082 |
23.5%* |
6.4% |
0.8% |
| Comparison | 21,740 | 28.7% | 21631 | 34.3% | 5.6% | ||
Within-year treatment vs. comparison Pearson chi-square P value<0.0001; **Treatment vs. comparison across-years trend goodness of fit statistic chi-square P<0.01; ***Treatment vs comparison across-years trend goodness of fit statistic chi-square P<0.0001.
Table 4 reveals that the treatment group reported significantly fewer days than the comparison group that physical health was “not good” within the prior month for both 2007 and 2009 (P<0.0001). Likewise, the treatment group also reported significantly fewer “not good” emotional health days within the prior month for 2009 (P<0.0001; treatment group 2007 data not available). Comparison of the 3-year trend between study groups using the available 2008 to 2010 treatment group data displayed a significantly more favorable trend for the treatment group with respect to this emotional health measure (P<0.05).
Table 4.
Comparison of Physical and Emotional Health in Prior 30 Days
| |
|
2007 |
2009 |
2010 |
|
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Survey measure | Study group | Total responses | Average days health was “not good” | Total responses | Average days health was “not good” | Total responses | Average days health was “not good” | Change from initial to final year | Difference in change |
| Physical health |
Treatment |
4573 |
1.76* |
4950 |
2.41* |
NA |
NA |
0.73 |
0.12 |
| |
Comparison |
21,881 |
3.40 |
21,658 |
4.02 |
NA |
NA |
0.61 |
|
| |
|
Initial Survey Yeara |
|
|
|
|
|
|
|
| Emotional health |
Treatmenta |
5015 |
1.37 |
4962 |
1.39* |
5046 |
1.51 |
0.18a |
−0.20** |
| Comparison | 21,935 | 1.95 | 21,740 | 2.33 | NA | NA | 0.38 | ||
The mental question was not included in the treatment group survey in 2007. However, 2008 and 2010 data were available; 2008 used as initial survey year for treatment group and change across years for treatment was measured between 2008 and 2010.
Treatment vs. comparison within-year comparison, Wilcoxon 2-sample test, P<0.0001; **Treatment vs. comparison, comparison of change across years, t test (Satterthwaite), P<0.05.
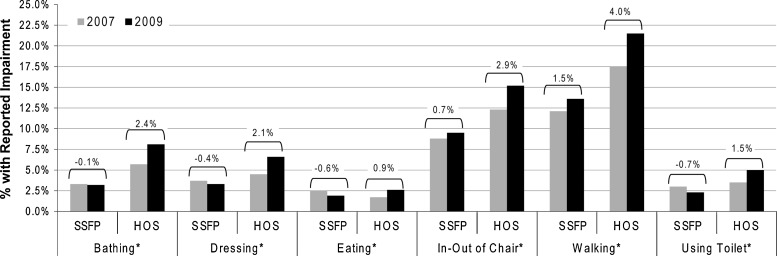
The treatment group reported significantly less impairment in 4 of 6 ADLs than the comparison group in 2007 (P<0.05), and for all 6 ADLs in 2009 (P<0.001). Figure 1 presents these data showing the 2007 to 2009 trend of both study groups for each ADL. All 6 ADLs present a more favorable trend (less decline or greater improvement) for the treatment group (P<0.0001). The treatment group also presents a significantly greater percentage of members with no impaired ADLs than the comparison group for both 2007 (83.7% vs. 78.7%, P<0.0001) and 2009 (82.4% vs. 74.8%, P<0.0001) and a significantly better associated trend across years with regard to the percentage having no impaired ADLs (−1.3% vs. −3.9%, P<0.0001). Table 5 presents the calculated disability index of each study group for both 2007 and 2009 and the change across years. The treatment group displays a significantly lower disability index for both 2007 and 2009 (P<0.0001) and a significantly more favorable trend across years (P<0.0001).
FIG. 1.
Comparison of activities of daily living impairment between the treatment and comparison groups; *P<0.0001 for 2007 to 2009 trend goodness of fit chi-square test. HOS, Health Outcomes Survey; SSFP, SilverSneakers fitness program.
Table 5.
Disability Index Comparison
| |
2007 |
2009 |
|
|
||
|---|---|---|---|---|---|---|
| Study group | N | Disability Index, Mean | N | Disability Index, Mean | 2007 to 2009 change | Difference in change |
| Treatment |
5368 |
0.081* |
5340 |
0.075* |
−0.004 |
−0.033** |
| Comparison | 22,267 | 0.092 | 22,066 | 0.121 | 0.029 | |
Treatment vs. comparison within-year comparison, Wilcoxon 2-sample test P<0.0001; **Treatment vs. comparison, comparison of change across years, t test (Satterthwaite) P<0.0001.
Table 6 displays the results of modeling of the impact of exercise frequency among treatment members on selected health and functioning measures. With the exception of only the health status survey question in 2007, members in the low- and medium-frequency (0–2 days and 3–4 days per week, respectively) exercise subgroups had significantly higher odds of reporting poorer health and functional limitations for evaluated survey questions than members in the high-frequency (5–7 days per week) subgroup for both 2007 and 2009. In modeling the impact of frequency of exercise participation on change across years for the same 3 analyzed survey questions, exercise subgroups presented similar results to those already reported. Specifically, members in the low and medium exercise frequency subgroups displayed significantly higher odds of a nonfavorable trend across the time period of 2007-to-2009 than members in the high-frequency subgroup.
Table 6.
Within-Subject Comparison of Odds of Unfavorable Responses for Health and Functioning Measures by Frequency of Exercise
| Survey measure | Exercise frequency group Comparisona | 2007 OR point estimate (95% C.I.)b | 2009 OR point estimate (95% C.I.)b | ‘Status Change’ Odds Ratio point estimate (95% C.I.)c,d |
|---|---|---|---|---|
| Health status |
Low vs. high frequency |
1.7 (0.8–3.7) |
4.2 (2.0–8.8) |
4.2 (2.0–8.7) |
| |
Medium vs. high frequency |
1.3 (0.9–2.1) |
2.8 (1.7–4.7) |
2.8 (1.7–4.6) |
| Functioning—Climbing stairs |
Low vs. high frequency |
2.4 (1.7–3.6) |
3.1 (2.1–4.5) |
3.2 (2.2–4.8) |
| |
Medium vs. high frequency |
1.8 (1.5–2.2) |
2.0 (1.7–2.4) |
2.0 (1.7–2.4) |
| Work or activity |
Low vs. high frequency |
3.0 (2.0–4.5) |
2.6 (1.8–3.9) |
2.5 (1.7–3.8) |
| limitations because of health | Medium vs. high frequency | 1.7 (1.4–2.2) | 1.9 (1.5–2.3) | 1.9 (1.5–2.3) |
All comparisons were conducted among treatment group members. bOdds ratios from logistic model were adjusted for age group, sex, race, education, marital status, body mass index group, number of reported conditions, and diagnoses of congestive heart failure, coronary artery disease, diabetes, lung disease, and stroke. c Status change modeling dependent variable: Maintained unfavorable status or declined in status across the 2007–2009 time period. dLogistic model controlled for group differences using the 12 demographic and comorbid variables used in study. Low frequency, 0–2 days per week; medium frequency, 3–4 days per week; high frequency, 5–7 days per week.
Discussion
In alignment with previous research demonstrating the variety of benefits of regular physical and social activity for seniors, the results presented here indicate that SilverSneakers participants report significantly better physical and emotional health and less impairment in daily activities relative to a matched comparison group. Additionally, 3-year longitudinal analyses revealed more favorable trends among SilverSneakers participants with respect to nearly all measures of health and impairment, suggesting that the program may help to slow or reverse natural trajectories toward declining health and functioning among seniors. Focused analyses to determine the impact of exercise frequency consistently showed that less frequent/regular exercise is significantly associated with poorer reported health and functioning, indicating that the program goal of initiating regular physical activity among seniors is contributing to the favorable program effect.
The risks of living a sedentary life can be severe, especially for seniors. Physical inactivity is associated with an increased risk of many chronic diseases, which are the leading cause of death in the United States. Additionally, recent survey research of the US population using the Gallup-Healthways Well-Being Index shows a decrease with age in the proportion of Americans who exercise 3 or more days a week, with a steady downward trend from age 70–74 through age 85–89.26 Controlling health risk behaviors, physical inactivity being one, is an important preventive practice that can substantially reduce morbidity and mortality from chronic disease.27–29 Physical activity has been shown to be of particular priority among healthy behaviors; Well-Being Index national data indicate that regular exercise is more important to seniors' reported health status than is a healthy diet.26 Consistent with many of the results of this study on SilverSneakers, the additional benefits seniors can gain from participating in regular moderate-intensity physical activity are wide ranging, including lowering the risk of depression, mitigating the development of disabilities, and improving the ability to do daily activities.30–32
Research by Coughlin indicates that certain aspects of well-being decline with age in seniors (life evaluation and physical health) while other domains of well-being actually increase in the senior years (healthy behaviors, emotional health, basic access, and work environment).33 The results are consistent with the SilverSneakers program as a means to not only augment the aspects of well-being that are already strong among seniors, but also to help improve the physical health trajectory of seniors, a major issue for senior well-being. With respect to emotional health, study results found that the treatment group reported fewer days of poor mental health (including stress, depression, and emotional problems) than the comparison group, and a more favorable trend over time. This study's findings with regard to emotional health are associative and add research support to a prior study of the positive impact of SilverSneakers participation associated with a lower risk of depression.18 Research by Ozminkowski et al indicates that, when combined with other chronic conditions, depressive symptoms result in an even greater negative impact on quality of life.34 The demonstrated benefits of SilverSneakers participation to both emotional and physical health measures denote the strong positive impact the program can have on the well-being of seniors.
The ADL functional status measures used in the present study also have been used as an indicator of frailty and functional impairment, and used in the development of the Centers for Medicare and Medicaid Services frailty adjustment model, a Medicare payment mechanism that pays Medicare managed care organizations based on the makeup of their community-residing plan enrollees.35 Frailty has been documented as a strong predictor of hospitalization, nursing home admission, and mortality.36 Increased limitations in ADLs and compromised health also have been associated with recurrent falls, common events among seniors that can lead to increased health care utilization and cost.37 Reported ADL impairment also has been shown to improve the ability to predict inpatient admissions.38 The present study results show that treatment group members have better reported health and fewer ADL limitations, and also decline with respect to these measures at a slower rate than the comparison group members. The implications of these findings are that participation in SilverSneakers also may help to prevent falls and reduce the associated cost burden, outcomes that should be explored in future research. Further, the positive impact noted in study findings on more proximal markers of health and well-being may represent leading indicators of associated reductions in utilization and health care cost. These results are thus complementary to Nguyen and Ackermann's research displaying slower growth in health care costs among seniors who participated in a health plan-sponsored fitness program.17–21
Social engagement is beneficial to the health and well-being of America's seniors. Recent research by Thomas shows that increasing social engagement was associated with a lower risk of mortality, after accounting for other known predictors of mortality.39 Han et al report that factors predicting 6-month mortality include general health perceptions, ADLs, social functioning, and energy/fatigue.40 These factors align well with the measures that were evaluated in this study and found to be positively impacted by the SilverSneakers program; therefore, future research should investigate reduced mortality as a program outcome.
Multiple studies support that a social environment and support from friends and family are strongly associated with participation in regular physical activity programs.41,42 Other studies point to associations of increased program participation and increased exercise adherence with the socializing and support that class participants receive from each other.43,44 Deforche and DeBourdeaudhuij found that seniors who participated in group physical activity programs reported higher overall activity and higher self-efficacy when compared to seniors who did not participate in organized physical activity.45 Based on this prior research, the social aspect of the SilverSneakers program may not only have independent benefits, as discussed, but also may promote regular program participation over time and thus magnify the physical program benefits.
Limitations
The treatment group in this study is comprised of health plan members who voluntarily joined SilverSneakers; thus, there is the possibility of self-selection bias. To mitigate this potential confounder, study groups were matched on a variety of demographic and reported medical conditions to help account for potential dissimilarities between groups. Furthermore, these matching factors were controlled for in modeling analyses. There is the small possibility that a member in the treatment group also might have been randomly selected into the comparison group; even though the occurrence would be unlikely, this confounder actually would serve to diminish the treatment effect and thus should not affect the study conclusions.
The study results are not necessarily generalizable to populations with different demographic and health characteristics. Additionally, the use of self-reported exercise frequency data prevents the ability to equate exercise frequency with participation in SilverSneakers exercise classes.
Although it is possible that selection bias toward program participants who were already healthier and physically active was the reason for a difference in outcomes in the first year, taken together, the longitudinal results indicate that selection bias alone cannot account for the differences between the groups. For example, the study group demonstrated improvement in the disability index. If participants had largely been exercising consistently throughout their lives, and thus would have continued regardless of the SilverSneakers offering, it is unlikely that the group would have exhibited further improvement as seniors.
Future research
Additional research is needed to substantiate reported study outcomes in different populations and over a longer time frame to further evaluate the generalizability and sustainment of positive impact. Additionally, future research can investigate the potential impact of SilverSneakers on other important outcomes such as the growth in chronic disease prevalence and comorbidities along with mortality rates.
Conclusion
Given the growth of the Medicare population and the associated trends of increasing morbidity and functional decline, there is a critical need for senior-oriented programs that improve health and preserve and extend functional capabilities, effectively improving senior's overall quality of life. Furthermore, there is significant evidence of the relationship between improvements in these outcomes and reduced health care expenditures, an important tie given the economic problems that both the Medicare program and the overall federal budget are facing. Taken collectively, the results of this study concur with a large body of prior research regarding socialization and physical activity for seniors and demonstrate the power of combining these elements into a program that is effective in improving the physical and emotional health of this group. The findings also demonstrate that ADLs are less impaired in SilverSneakers participants—an outcome that can be linked directly to decreases in morbidity, accidental injury, health care costs, and potentially even mortality. Senior fitness programs should continue to be explored and invested in as a means to improve the health and well-being of seniors, thereby creating the potential for reducing overall health care costs and the burden on an increasingly strained health care delivery system.
Disclosure Statement
Drs. Hamar, Coberley, Pope, and Rula are employees of Healthways, Inc. and own stock in the company.
References
- 1.2011 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds May13, 2011. Available at: https://www.cms.gov/ReportsTrustFunds/downloads/tr2011.pdf Accessed January19, 2012
- 2.Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare Available at www.medpac.gov/documents/jun07_entirereport.pdf Accessed March3, 2012
- 3.Keehan SP, Sisko AM, Truffer CJ, et al. . National health spending projections through 2020: Economic recovery and reform drive faster spending growth. Health Aff (Millwood) 2011;30:1594–1605 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services. National Health Expenditure Data Available at http://www.cms.gov/NationalHealthExpendData/25_NHE_Fact_Sheet.asp Accessed January20, 2012
- 5.Anderson G. Chronic care: Making the case for ongoing care. Available at: http://www.rwjf.org/content/dam/web-assets/2010/01/chronic-care Accessed January23, 2012
- 6.Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood) 2010;29:718–724 [DOI] [PubMed] [Google Scholar]
- 7.Anderson G. Chronic Conditions: Making the Case for Ongoing Care. Baltimore, MD: Partnership for Solutions, John Hopkins University; 2004 [Google Scholar]
- 8.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep 2004;119:263–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karelina K, DeVries AC. Modeling social influences on human health. Psychosom Med 2011;73:67–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerber Y, Benyamini Y, Goldbourt U, Drory Y. Prognostic importance and long-term determinants of self-rated health after initial acute myocardial infarction. Med Care 2009;47:342–349 [DOI] [PubMed] [Google Scholar]
- 11.Benyamini Y, Blumstein T, Murad H, Lerner-Geva L. Changes over time from baseline poor self-rated health: For whom does poor self-rated health not predict mortality? Psychol Health 2011;26:1446–1462 [DOI] [PubMed] [Google Scholar]
- 12.Duffy JP, Kao K, Ko CY, et al. . Long-term patient outcome and quality of life after liver transplantation: Analysis of 20-year survivors. Ann Surg 2010;252:652–661 [DOI] [PubMed] [Google Scholar]
- 13.Mookadam F, Arthur HM. Social support and its relationship to morbidity and mortality after acute myocardial infarction: Systematic overview. Arch Intern Med 2004;164:1514–1518 [DOI] [PubMed] [Google Scholar]
- 14.Prevalence of self-reported physically active adults–United States, 2007. MMWR Morb Mortal Wkly Rep 2008;57:1297–1300 [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Physical activity and health Available at http://www.cdc.gov/physicalactivity/everyone/health/index.html Accessed January20, 2012
- 16.US Department of Health and Human Services Physical activity and health: A report of the Surgeon General. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996 [Google Scholar]
- 17.Nguyen HQ, Ackermann RT, Maciejewski M, et al. . Managed-Medicare health club benefit and reduced health care costs among older adults. Prev Chronic Dis 2008;5:A14. [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen HQ, Koepsell T, Unutzer J, Larson E, LoGerfo JP. Depression and use of a health plan-sponsored physical activity program by older adults. Am J Prev Med 2008;35:111–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen HQ, Maciejewski ML, Gao S, Lin E, Williams B, Logerfo JP. Health care use and costs associated with use of a health club membership benefit in older adults with diabetes. Diabetes Care 2008;31:1562–1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ackermann RT, Williams B, Nguyen HQ, Berke EM, Maciejewski ML, LoGerfo JP. Healthcare cost differences with participation in a community-based group physical activity benefit for Medicare managed care health plan members. J Am Geriatr Soc 2008;56:1459–1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ackermann RT, Cheadle A, Sandhu N, Madsen L, Wagner EH, LoGerfo JP. Community exercise program use and changes in healthcare costs for older adults. Am J Prev Med 2003;25:232–237 [DOI] [PubMed] [Google Scholar]
- 22.National Institutes of Health. NIH Challenge Grants in Health and Science Research (RC1), 05-AG-102* Prevention and Risk Factor Reduction Strategies for Disabilities Available at: http://grants.nih.gov/grants/funding/challenge_award/High_Priority_Topics.pdf#topic_05 Accessed October2, 2012
- 23.Medicare Health Outcomes Survey Limited Data Sets File Specifications for Cohorts 9–11. Available at http://www.hosonline.org/surveys/hos/download/HOS_Cohort_9–11_LDS_File_Specifications.pdf Accessed March3, 2012
- 24.Cooper JK, Kohlmann T, Michael JA, Haffer SC, Stevic M. Health outcomes. New quality measure for Medicare. Int J Qual Health Care 2001;13:9–16 [DOI] [PubMed] [Google Scholar]
- 25.Vita AJ, Terry RB, Hubert HB, Fries JF. Aging, health risks, and cumulative disability. N Engl J Med 1998;338:1035–1041 [DOI] [PubMed] [Google Scholar]
- 26.Gallup website In old age, exercise more closely tied to health than diet. Available at http://www.gallup.com/poll/155075/old-age-exercise-closely-tied-health-diet.aspx Accessed October11, 2012
- 27.Li C, Balluz LS, Okoro CA, et al. . Surveillance of certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2009. MMWR Surveill Summ 2011;60:1–250 [PubMed] [Google Scholar]
- 28.Jordan CO, Slater M, Kottke TE. Preventing chronic disease risk factors: Rationale and feasibility. Medicina (Kaunas) 2008;44:745–750 [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. CDC's Healthy Communities Program Preventing chronic diseases and reducing health risk factors. Available at http://www.cdc.gov/healthycommunitiesprogram/overview/diseasesandrisks.htm Accessed February2, 2012
- 30.Salguero A, Martinez-Garcia R, Molinero O, Marquez S. Physical activity, quality of life and symptoms of depression in community-dwelling and institutionalized older adults. Arch Gerontol Geriatr 2011;53:152–157 [DOI] [PubMed] [Google Scholar]
- 31.Bruce B, Fries JF, Hubert H. Regular vigorous physical activity and disability development in healthy overweight and normal-weight seniors: A 13-year study. Am J Public Health 2008;98:1294–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Visser M, Simonsick EM, Colbert LH, et al. . Type and intensity of activity and risk of mobility limitation: The mediating role of muscle parameters. J Am Geriatr Soc 2005;53:762–770 [DOI] [PubMed] [Google Scholar]
- 33.Coughlin J. Facets of well-being across the age spectrum in the American population. Available at http://www.healthways.com/success/library.aspx?id=618&terms=coughlin Accessed March3, 2012
- 34.Ozminkowski RJ, Musich S, Bottone FG Jr, et al. . The burden of depressive symptoms and various chronic conditions and health concerns on the quality of life among those with Medicare supplement insurance. Int J Geriatr Psychiatry 2012;27:948–958 [DOI] [PubMed] [Google Scholar]
- 35.Kautter J, Ingber M, Pope GC. Medicare risk adjustment for the frail elderly. Health Care Financ Rev 2008;30:83–93 [PMC free article] [PubMed] [Google Scholar]
- 36.Hastings SN, Purser JL, Johnson KS, Sloane RJ, Whitson HE. Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc 2008;56:1651–1657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: Incidence, associated factors, and impact on health care. Phys Ther 2009;89:324–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perrin NA, Stiefel M, Mosen DM, Bauck A, Shuster E, Dirks EM. Self-reported health and functional status information improves prediction of inpatient admissions and costs. Am J Manag Care 2011;17:e472–e478 [PubMed] [Google Scholar]
- 39.Thomas PA. Trajectories of social engagement and mortality in late life. J Aging Health 2012;24:547–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han PK, Lee M, Reeve BB, et al. . Development of a prognostic model for six-month mortality in older adults with declining health. J Pain Symptom Manage 2012;43:527–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Booth ML, Owen N, Bauman A, Clavisi O, Leslie E. Social-cognitive and perceived environment influences associated with physical activity in older Australians. Prev Med 2000;31:15–22 [DOI] [PubMed] [Google Scholar]
- 42.Stahl T, Rutten A, Nutbeam D, et al. . The importance of the social environment for physically active lifestyle—Results from an international study. Soc Sci Med 2001;52:1–10 [DOI] [PubMed] [Google Scholar]
- 43.Belza B, Walwick J, Shiu-Thornton S, Schwartz S, Taylor M, LoGerfo J. Older adult perspectives on physical activity and exercise: Voices from multiple cultures. Prev Chronic Dis 2004;1:A09. [PMC free article] [PubMed] [Google Scholar]
- 44.Chiang KC, Seman L, Belza B, Tsai JH. “It is our exercise family”: Experiences of ethnic older adults in a group-based exercise program. Prev Chronic Dis 2008;5:A05. [PMC free article] [PubMed] [Google Scholar]
- 45.Deforche B, De Bourdeaudhuij I. Differences in psychosocial determinants of physical activity in older adults participating in organised versus non-organised activities. J Sports Med Phys Fitness 2000;40:362–372 [PubMed] [Google Scholar]