Abstract
Drugs that enhance GABAergic inhibition alleviate inflammatory and neuropathic pain after spinal application. This antihyperalgesia occurs mainly through GABAA receptors (GABAARs) containing α2 subunits (α2-GABAARs). Previous work indicates that potentiation of these receptors in the spinal cord evokes profound antihyperalgesia also after systemic administration, but possible synergistic or antagonistic actions of supraspinal α2-GABAARs on spinal antihyperalgesia have not yet been addressed. Here we generated two lines of GABAAR-mutated mice, which either lack α2-GABAARs specifically from the spinal cord, or, which express only benzodiazepine-insensitive α2-GABAARs at this site. We analyzed the consequences of these mutations for antihyperalgesia evoked by systemic treatment with the novel non-sedative benzodiazepine site agonist HZ166 in neuropathic and inflammatory pain. Wild-type mice and both types of mutated mice had similar baseline nociceptive sensitivities and developed similar hyperalgesia. However, antihyperalgesia by systemic HZ166 was reduced in both mutated mouse lines by about 60% and was virtually indistinguishable from that of global point-mutated mice, in which all α2-GABAARs were benzodiazepine insensitive. The major (α2-dependent) component of GABAAR-mediated antihyperalgesia was therefore exclusively of spinal origin, whereas supraspinal α2-GABAARs had neither synergistic nor antagonistic effects on antihyperalgesia. Our results thus indicate that drugs that specifically target α2-GABAARs exert their antihyperalgesic effect through enhanced spinal nociceptive control. Such drugs may therefore be well-suited for the systemic treatment of different chronic pain conditions.
Keywords: neuropathic pain, analgesia, GABA, benzodiazepine, spinal cord, mouse model
INTRODUCTION
Chronic neuropathic pain syndromes are frequently unresponsive to classical analgesic drugs including cyclooxygenase inhibitors and opioids. Drugs most effective in these pain conditions include anticonvulsant drugs that modulate or block voltage-gated Na+ or Ca2+ channels (Sang and Hayes, 2006). Other anticonvulsive drugs with a different mode of action include the benzodiazepine site agonists, which enhance neuronal inhibition through facilitation of GABAA receptor-mediated neurotransmission. Diminished GABAergic or glycinergic inhibition in the spinal dorsal horn (ie, in the sensory part of the spinal cord) has been shown to be a major contributor to chronic pain syndromes (Ahmadi et al, 2002; Coull et al, 2003; Harvey et al, 2004), suggesting that drugs that facilitate spinal inhibition might correct a major component of the maladaptive neuroplasticity underlying chronic pain states. In line with this concept, previous work has shown that spinal injection of benzodiazepine site agonists provides pain relief in a number of rodent models of inflammatory and neuropathic pain (Knabl et al, 2008; Luger et al, 1995; Witschi et al, 2011).
Mammalian GABAARs form a heterogeneous family of heteropentameric ion channels assembled from a repertoire of 19 subunits. The most prevalent subtypes of GABAARs contain two α-, two β- and one γ2- subunits. Pharmacological properties of the different GABAAR subtypes are best characterized by the type of α-subunit present in the individual receptors (Olsen and Sieghart, 2008). Experiments in genetically modified mice demonstrated a particular relevance of GABAARs with an α2-type benzodiazepine pharmacology (α2-GABAARs) for antihyperalgesia mediated by spinally applied benzodiazepines (Knabl et al, 2008). These and subsequent experiments (Knabl et al, 2009) established that the antihyperalgesic actions of benzodiazepine site agonists occur independently from the sedative action, which is mediated by α1-GABAARs (Rudolph et al, 1999). More recent experiments using novel benzodiazepine site ligands with improved subunit specificity (ie, reduced or absent activity at α1-GABAARs) have shown that such novel compounds reduce nerve injury-induced and inflammation-induced hyperalgesia also after systemic administration (Di Lio et al, 2011; Knabl et al, 2008; Knabl et al, 2009; Munro et al, 2009; Munro et al, 2008; Reichl et al, 2012). While the contribution of spinal GABAARs to this antihyperalgesia is likely, although still not formally proven, the relevance of GABAAR subtypes in supraspinal circuits is unclear. Such supraspinal GABAARs might contribute to antihyperalgesia through a genuine antihyperalgesic effect, eg, through GABAARs in the rostral agranular insular cortex (Jasmin et al, 2003), or indirectly through the reversal of anxiety-induced or stress-induced hyperalgesia (Andre et al, 2005). The latter possibility is particularly relevant as α2-GABAARs also contribute to benzodiazepine-mediated anxiolysis (Löw et al, 2000; Morris et al, 2006). In contrast, supraspinal GABAARs might also counteract spinal antihyperalgesia through the silencing antinociceptive tracts descending from the periaqueductal gray or the rostroventromedial medulla (Harris and Westbrook, 1995; Luger et al, 1995; Tatsuo et al, 1999). It is thus possible that activation of supraspinal GABAARs either facilitates or constrains spinal antihyperalgesia.
To address these questions, we have generated two lines of GABAAR-mutated mice. The first line (hoxb8-α2−/−) carries a tissue-specific deletion of the GABAAR α2 subunit from all spinal neurons, astrocytes, and primary sensory neurons up to the mid cervical level (approximately C4). This tissue-specific ablation was achieved by crossing mice that carried a GABAAR α2 (Gabra2) allele flanked by two loxP sites (α2fl; Witschi et al, 2011) with mice expressing the cre recombinase under the transcriptional control of the hoxb8 homeobox gene (Witschi et al, 2010). The second line can be viewed as a tissue-specific point-mutated α2-GABAAR mouse line (hoxb8-α2R/−), which carries in addition to one α2fl allele, a benzodiazepine-insensitive H101R point-mutated Gabra2 allele (α2R; Löw et al, 2000), and the hoxb8-cre transgene. At supraspinal sites, this line expresses the point-mutated allele together with a fully functional (‘wild-type') α2fl allele, whereas in primary sensory neurons and in the spinal nervous system only the point-mutated allele is expressed. For pharmacological analyses, we used the novel non-sedative 8-acetyleno-2′-pyridoimidazobenzodiazepine HZ166 (ethyl 8-ethynyl-6-(pyridin-2-yl)-4H-benzo[f]imidazo[1,5-a][1,4]diazepine-3-carboxylate, compound 2 in Rivas et al, 2009), which has previously been shown to exhibit antihyperalgesic properties in the absence of sedation in mice (Di Lio et al, 2011). Analysis of the antihyperalgesic effects of HZ166 in the two mutated mouse lines and comparison of these effects with those obtained in wild-type mice and in mice in which all α2-GABAARs had been rendered benzodiazepine-insensitive revealed that activation of supraspinal α2-GABAARs neither exerts a positive nor a negative impact on the antihyperalgesic actions of systemically applied HZ166.
MATERIALS AND METHODS
Generation of GABAAR-Mutated Mice
Three strains of GABAAR α2 (gabra2)-mutated mice were used to generate the genotypes needed for the present study: (i) mice carrying GABAAR α2 alleles flanked by loxP sites (α2fl; Witschi et al, 2011), (ii) mice carrying a H101R point-mutated ‘knock-in' allele (α2R; Löw et al, 2000), and (iii) hoxb8-cre transgenic mice (Witschi et al, 2010). Hoxb8-α2−/− mice and hoxb8-cre-negative (α2fl/fl) littermates were obtained from crossings of hoxb8-cre-positive α2fl/fl mice with α2fl/fl mice. Hoxb8-α2R/− mice and hoxb8-cre-negative (α2R/fl) littermates were generated by crossing hoxb8-cre-positive α2fl/fl mice with α2R/R. All mouse lines had been backcrossed to a C57BL/6 J background for at least 10 generations and were maintained on this background throughout the study. During the breeding of hoxb8-α2−/− mice, a small number of mice were born carrying a non-conditional knockout allele of the gabra2 gene, which had occurred through undesired recombination events in the germline. To ensure that these mice were excluded from all experiments and breeding, we verified the absence of the knockout allele through PCR analyses performed on DNA extracted from ear biopsies. This tissue was chosen because analysis of hoxb8-cre ROSA26-lacZ double transgenic reporter mice had demonstrated that hoxb8-cre was not expressed in outer ear tissue at any developmental stage.
Morphology
Distribution of GABAAR α2 protein was studied in brain and spinal cord sections obtained from adult hoxb8-α2−/− and hoxb8-α2R/– mice and from hoxb8-cre− littermates (α2fl/fl and α2R/fl mice). For immunoperoxidase stainings, a polyclonal antibody directed against the N-terminal nine amino acids (NIQEDEAKN) of the GABAAR α2 subunit (Fritschy and Möhler, 1995) was used as the primary antibody. Stainings (triplicates) were made as described previously (Paul et al, 2012). Sections from GABAA receptor-mutated mice and from control littermates were treated in a strictly parallel fashion.
Quantitative reverse Transcriptase PCR
Four to six lumbar spinal cords, lumbar DRGs, and hippocampi were rapidly removed from euthanized adult hoxb8-α2−/− mice and α2fl/fl littermates. mRNA was transcribed into cDNA using the QuantiTect Reverse Transcription Kit (Qiagen no.205311). Expression of GABAAR subunits was assessed using β-actin as reference gene (for details of the assays see Witschi et al (2011)).
[3H]Ro 15-4513 Binding Assay
HEK293 cells maintained in DMEM/10% FBS in poly-lysine-coated culture dishes (10 cm) were transfected with plasmids containing the subunit combination α2β3γ2 or α2(H101R)β3γ2 (7 mg total DNA, ratio 1 : 1 : 2) using jetPEI transfection reagent (Polyplus-transfection). Twenty-four hours after transfection, HEK293 cells were collected in PBS. HEK293 cells were homogenized in 10 vol 10 mM Tris pH 7.5, 0.32 M sucrose, protease inhibitor cocktail (complete Mini, Roche Applied Science) and centrifuged at 1000 g for 10 min. The supernatant was carefully removed and centrifuged at 4 °C again for 20 min at 25 000 g at 4 °C. The crude membrane pellet was resuspended in 10 mM Tris-HCl pH 7.4, protease inhibitor cocktail and washed once by centrifugation and re-suspension. Aliquots of the crude membranes prepared from HEK293 cells expressing the α2β3γ2 or α2(H101R)β3γ2 subunit combination (150–200 μg protein) were incubated with increasing concentrations of HZ166 (10−8–10−4 M) and 6.3 nM [3H]Ro 15-4513 (22.7 Ci/mmol, PerkinElmer) in a total volume of 200 μl for 90 min on ice. Subsequently, the samples were filtered onto glass fiber filters using a 12-channnel semiautomated cell harvester (Scatron) and washed with ice-cold buffer (10 mM Tris-HCl pH 7.4). Non-specific [3H]Ro 15-4513 binding was measured using 10 μM flumazenil. The radioactivity of the filters was determined by liquid scintillation counting using a Tricarb 2500 liquid scintillation analyzer. Binding data were analyzed using the GraphPad Prism software (version 5.02, GraphPad Software, USA).
Electrophysiological Analyses
The effects of HZ166 on GABAARs were studied in HEK293 cells transiently expressing GABAARs and in spinal cord slices of hoxb8-α2−/− mice and wild-type (hoxb8-cre-negative α2fl/fl) littermates. HEK293 cells were transfected with rat α2/α2(H101R), β3 and γ2 GABAAR expression vectors (Benson et al, 1998) using lipofectamine LTX (Invitrogen). The transfection mixture contained (in μg) 1 α2/β3, 3 γ2 and 0.5 EGFP (used as a marker of successful transfection). Recordings were made 18–36 hours after transfection. Whole-cell patch-clamp recordings of GABA-evoked currents were made at room temperature (20–24 °C) and at a holding potential of −60 mV. The external solution contained (in mM) 150 NaCl, 10 KCl, 2.0 CaCl2, 1.0 MgCl2, 10 HEPES (pH 7.4), and 10 glucose. Recording electrodes were filled with internal solution containing (in mM) 120 CsCl, 10 EGTA, 10 HEPES (pH 7.40), 4 MgCl2, 0.5 GTP, and 2 ATP. CsCl was used instead of KCl to block GABAB receptor-evoked K+ currents. GABA was applied to the recorded cell using a manually controlled pulse (4–6 s) of a low subsaturating GABA concentration (EC5). GABA EC5 values were determined for wild-type α2β3γ2 and mutant α2(H101R)β3γ2 receptors separately. EC50 values and Hill coefficients (nh) were obtained from fits of normalized concentration–response curves to the equation IGABA=Imax [GABA]nh/([GABA]nh+[EC50]nh). Imax was determined as the current elicited by a saturating concentration of GABA (500 μM). HZ166 was co-applied together with GABA without preincubation.
Transverse spinal cord slices were prepared from 2- to 3-week-old mice of either sex as described previously (Ahmadi et al, 2002). Slices were kept in oxygenated (95% O2/5% CO2) external solution containing (in mM) 120 NaCl, 5 HEPES, 26 NaHCO3, 1.25 NaH2PO4, 2.5 KCl, 2 CaCl2, 1 MgCl2, and 10 glucose (pH 7.35) at 35 °C. Superficial dorsal horn neurons were visually identified using an infrared gradient contrast equipment. Whole-cell patch-clamp recordings were performed at room temperature at a holding potential of −60 mV. Patch pipettes were filled with internal solution containing (in mM) 120 CsCl, 10 EGTA, 4 MgCl2, 0.5 GTP, 2 ATP, and 10 HEPES (pH 7.30 adjusted with CsOH). QX-314 (5 mM) was added to block voltage-activated Na+ currents in the recorded cell. Slices were continuously superfused with oxygenated external solution at a flow rate of 1.3–1.6 ml/min. After 4–5 min of baseline recording, GABA (50 μM) was bath-applied. Steady-state GABA-evoked currents were achieved usually 3–5 min after application. Subsequently, HZ166 (10 μM) was co-applied with the same GABA concentration for 6 to 7 min. Afterward, GABA and HZ166 were washed-out, or bicuculline (20 μM) was applied. Recordings in which recovery to baseline currents before GABA application was less than 85–90% were excluded from the analysis.
Behavioral Testing
Experiments were performed in 7- to 10-week-old male and female mice. Care was taken to ensure equal numbers of age-matched male and female mice in all experiments. Mechanical and thermal nociceptive sensitivities of hoxb8-α2−/− and of hoxb8-cre-negative α2fl/fl littermates were determined using electronic von Frey filaments and the plantar test, respectively (for details see Witschi et al, 2011).
Antihyperalgesic properties of HZ166 were studied in two models: (i) activity against neuropathic hyperalgesia was assessed in the chronic constriction injury (CCI) model (Bennett and Xie, 1988); unilateral constriction of the left sciatic nerve was performed as described previously (Hösl et al, 2006) and (ii) inflammation was evoked through subcutaneous injection of zymosan A (0.06 mg in 20 μl saline (0.9% NaCl)) into one hindpaw. HZ166 was tested 7 days after CCI surgery or 48 h after zymosan A injection, when sensitization had reached a maximum (Witschi et al, 2011). Sensitivities of the injured/inflamed paw and of the contralateral control paw were measured alternately and at least five measurements were taken per mouse and time point. Antihyperalgesia was quantified for the time interval of 60–90 min post drug injection, when the drug effect was maximal, and expressed as percent maximum possible analgesia=(Rpost-drug−Rpre-drug)/(Rbaseline−Rpre-drug) × 100%, where R is the average response latency or threshold under baseline condition (Rbaseline), after induction of neuropathy or inflammation but before drug injection (Rpre-drug), and 60–90 min after drug injection (Rpost-drug).
Locomotor activity was assessed as described before (Di Lio et al, 2011). HZ166 was administered immediately before placing the mice into the open field arena, and the number of beam crosses per 24 min was determined for a total of 96 min after drug administration.
Motor coordination of hoxb8-α2−/− and of hoxb8-cre-negative α2fl/fl littermates was investigated in the rotarod test either at two fixed rotational speeds (5 and 10 r.p.m.) for analysis of baseline motor coordination, or with increasing rotational velocity (from 4 r.p.m. to 40 r.p.m. within 5 min) for the analysis of effects of HZ166 on motor coordination. Each mouse was tested three times. HZ166 was given 60 min before testing on the rotarod. Permission for the animal experiments was obtained from the Veterinäramt des Kantons Zürich (ref. no. 135/2009).
RESULTS
To assess a possible influence of supraspinal α2-GABAARs to GABAergic analgesia, three prerequisites were needed: (i) mice that express benzodiazepine-sensitive α2-GABAARs only in the brain, (ii) a benzodiazepine site agonist that causes significant antihyperalgesia after systemic administration at doses that do not produce confounding sedation or motor impairment, and (iii) we needed to demonstrate that the facilitating action of this agonist on α2-GABAARs was lost in H101R point-mutated receptors.
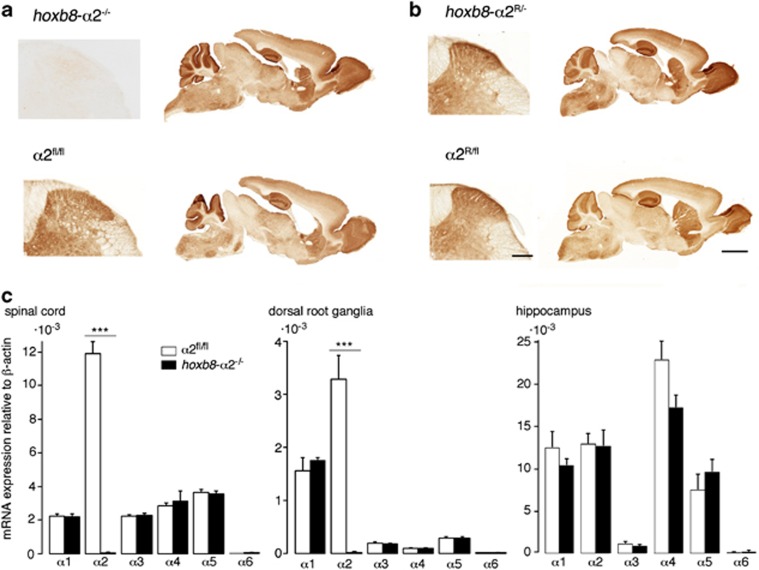
In order to reach the first prerequisite, we generated two lines of α2-GABAAR-mutated mice using the cre/loxP system. The first line lacked the GABAAR α2 subunit from the spinal cord and from all primary sensory neurons (hoxb8-α2−/−), but showed unchanged GABAAR α2 subunit expression in the brain. These mice carried a hoxb8-cre transgene and two floxed GABAAR α2 (α2fl) alleles. The second line was a conditional point-mutated (hoxb8-α2R/–) mouse line, whose spinal α2-GABAARs were rendered benzodiazepine insensitive. These mice carried the hoxb8-cre transgene together with a α2fl allele and a point-mutated (H101R) GABAAR α2 (α2R) allele. Morphological analyses demonstrated that the supraspinal GABAAR α2 subunit distribution of hoxb8-α2−/− mice was indistinguishable from that of α2fl/fl (wild-type) littermates (Figure 1a). However, transverse sections of the lower lumbar spinal cord of hoxb8-α2−/− mice did not show any GABAAR α2 subunit immunoreactivity, indicating highly effective hoxb8-cre-mediated gene recombination. Sagittal sections of the cervical spinal cord revealed the expected progressive rostral to caudal loss of GABAAR α2 subunit expression within the upper cervical segments (not shown). The apparent lack of α2-GABAARs from the lumbar spinal cord of hoxb8-α2−/− mice indicates that only few, if any, spinal α2-GABAARs reside on processes of neurons descending from supraspinal areas. In conditional point-mutated (hoxb8-α2R/-) mice and hoxb8-cre-negative (α2R/fl) littermates, no differences in α2-subunit immunoreactivity were observed in either the brain or the spinal cord (Figure 1b), suggesting that the loss of one allele had no apparent effect on the amount of GABAAR α2 subunit expressed.
Figure 1.
GABAAR α2-subunit distribution in brains and spinal cords of hoxb8-α2−/− and hoxb8-α2R/fl mice and changes in GABAAR α-subunit expression. (a, b), immunoperoxidase staining of GABAAR α2 subunits in horizontal sections of the lumbar spinal dorsal horn and in sagittal brain sections of spinal cord-specific GABAAR α2-knockout (hoxb8-α2−/−) and α2(H101R)-knock-in mice (hoxb8-α2R/-). Bottom row, sections obtained from the respective control littermates (hoxb8-cre-negative wild-type and α2R/fl). Similar results were obtained from at least two additional mice of each genotype. Scale bars are 200 μm (dorsal horn) and 1 mm (brain), and apply to all sections. (c) Quantitative reverse transcriptase PCR measurements of all six GABAAR α-subunits in lumbar DRGs, lumbar spinal cords, and hippocampi of hoxb8-α2−/− and α2fl/fl littermates. mRNA expression relative to β-actin (mean±SEM, n=6–7 mice per genotype and tissue). mRNA encoding for α6 GABAAR subunit was not detectable in any of the three tissues. ***P<0.001, P>0.13 for all other comparisons, ANOVA followed by Bonferroni post hoc correction for 18 independent pair-wise comparisons.
To further corroborate the loss of GABAAR α2 gene expression and to assess possible compensatory changes in the expression of other GABAAR α-subunits, we performed qRT-PCR analyses from lumbar DRGs, lumbar spinal cords, and hippocampi of hoxb8-α2−/− mice and hoxb8-cre-negative α2fl/fl (wild-type) littermates (Figure 1c). In all three tissues, we detected mRNA encoding for GABAAR α1–α5 subunits, but no α6 subunit mRNA. As expected, the α2 subunit was the most extensively expressed GABAAR α-subunit in the lumbar spinal cords and DRGs. Its expression was completely lost in lumbar DRGs and spinal cords of hoxb8-α2−/− mice, but remained unchanged in the hippocampus. No significant changes were seen in the expression of the other GABAAR α subunits in any of the three tissues. For spinal cord and DRG tissue, we also analyzed the expression of ρ1, ρ2, and ρ3 subunit genes, which are able to form functional, benzodiazepine-insensitive GABAA (or sometimes also called GABAC) receptors. Expression of ρ-subunits was unchanged in hoxb8-α2−/− mice (data not shown).
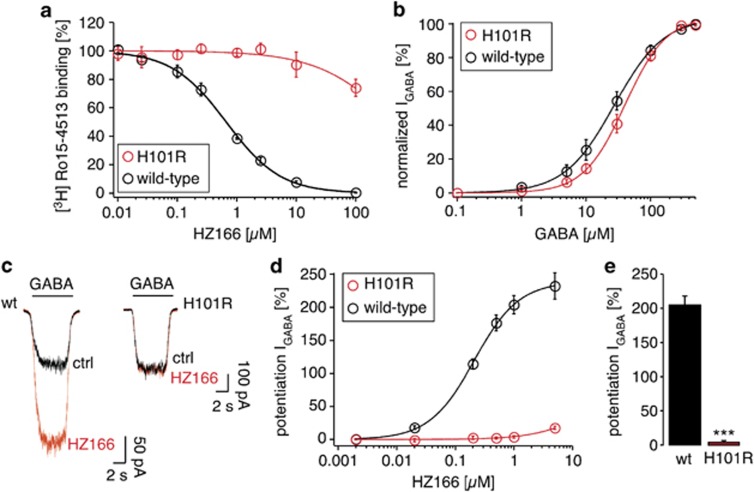
In order to assess the contribution of supraspinal α2-GABAARs to benzodiazepine-mediated antihyperalgesia, we used the new non-sedative partial benzodiazepine site agonist HZ166 (Rivas et al, 2009), which exerts pronounced antihyperalgesic actions in mice in the absence of sedation (Di Lio et al, 2011). Among the different available compounds with improved subtype specificity, we chose HZ166 because it possesses higher intrinsic activity at α2-GABAARs than for example TPA023 (Atack et al, 2006) or NS 11394 (Mirza et al, 2008), and has better pharmacokinetic properties in mice than L-838,417 (Scott-Stevens et al, 2005). Before we analyzed its antihyperalgesic actions in GABAAR-mutated mice, we had to verify that the H101R point mutation abolished modulation by HZ166. Although it has previously been shown that this mutation dramatically reduces the binding of and facilitation by diazepam (Wieland et al, 1992), it can have different effects on the action of other benzodiazepine site ligands. The potentiating effect of bretazenil for example is enhanced in the point-mutated receptors, and the action of Ro 45-1513 is converted from negative to positive modulation (Benson et al, 1998). We therefore compared the binding affinity of HZ166 with wild-type α2/β3/γ2 and point-mutated α2(H101R)/β3/γ2-GABAARs (Figure 2a). In wild-type α2/β3/γ2-GABAARs, HZ166 displaced [3H] Ro 45-1513 binding with a Ki of 221±22 nM (mean±SEM, n=4). In α2(H101R)/β3/γ2 point-mutated receptors competition was abolished at HZ166 concentration ⩽10 μM. Only at 100 μM, a small displacement was detected (26±3%, mean±SEM, n=4). Subsequent electrophysiological experiments in HEK293 cells transfected with either wild-type or point-mutated α2(H101R)/β3/γ2 GABAARs verified that both receptors responded similarly to GABA (Figure 2b). We then investigated the impact of the point mutation on potentiation of α2/β3/γ2 GABAARs by HZ166 and showed that HZ166 completely lost its ability for positive allosteric modulation in the point-mutated receptors (Figure 2c–e). Although HZ166 potentiated GABA-evoked currents through wild-type receptors by 232±20% (HZ166, 5 μM, n=8), potentiation was virtually absent in the point-mutated receptors at HZ166 concentrations ⩽1 μM and reached only 17.6±2.4% at 5 μM (n=7; P<0.001 unpaired student t-test, wild-type vs point-mutated receptors).
Figure 2.
HZ166 binding properties to recombinant wild-type and α2(H101R)β3γ2-GABAARs and potentiation by HZ166. (a) Binding affinity of HZ166 to wild-type and α2(H101R)β3γ2 point-mutated GABAARs determined by [3H] Ro15-4513 displacement. Ki in wild-type GABAARs was 221±22 nM (mean±SEM, n=4). (b–e) Electrophysiological analyses (e). (b) Activation of wild-type and α2(H101R)β3γ2 GABAARs exhibited similar dependence on GABA concentration. EC50 was 27±1 μM (mean±SEM, n=8) and 40±2 μM (n=7) for wild-type and α2(H101R)β3γ2 point-mutated GABAARs, respectively. Hill coefficients were 1.2±0.03 and 1.4±0.07, and maximum currents were 3.6±0.4 nA and 3.5±0.7 nA. (c–e) Potentiation by HZ166. (c) Example of current traces evoked by GABA (EC5=5 μM) in the presence or absence of HZ166 (1 μM). (d) Concentration–response curves of wild-type and α2(H101R)β3γ2 point-mutated GABAARs for HZ166. EC50 of HZ166 for wild-type GABAARs: 217±20 nM. (e) Statistical comparison of potentiation by HZ166 (1 μM). ***P<0.001 (wild-type vs point-mutated receptors), unpaired Student's t-test.
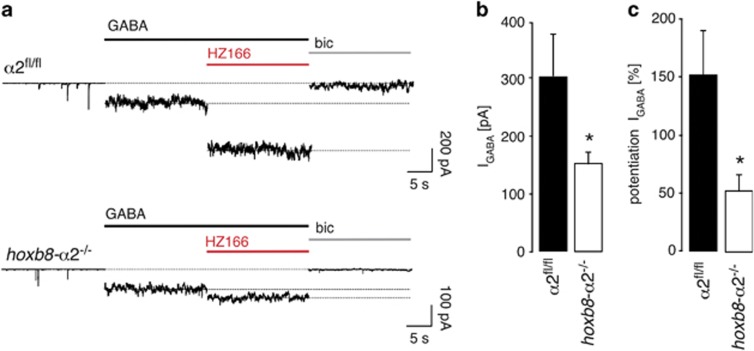
Before proceeding to behavioral experiments, we also investigated the impact of hoxb8-cre-mediated ablation of GABAAR α2 subunits on the amplitude of native GABAARs in the spinal dorsal horn and on their sensitivity to HZ166 (Figure 3). To this end, we used lumbar spinal cord slices and recorded GABAergic membrane currents from neurons located in the superficial dorsal horn of hoxb8-α2−/− mice and of wild-type (α2fl/fl) littermates. Superfusion of the slices with 50 μM GABA elicited average currents of 306±73 pA (mean±SEM, n=6) in wild-type mice and smaller currents in neurons of hoxb8-α2−/− mice (153±20 pA, n=8, P=0.04, unpaired student t-test) (Figure 3a, b). HZ166 (10 μM) potentiated GABAAR currents in both genotypes. However, potentiation was significantly smaller in hoxb8-α2−/− mice (52±14%, n=8) than in wild-type (α2fl/fl) littermates (151±39%, n=6, P=0.02, unpaired student t-test) (Figure 3c). Amplitudes of GABAAR currents were thus reduced by about half, whereas potentiation by HZ166 was reduced by two-thirds suggesting the presence of both benzodiazepine (HZ166)-sensitive and benzodiazepine (HZ166)-insensitive GABAAR current components in spinal dorsal horn neurons. The retention of benzodiazepine-sensitive GABAAR currents in hoxb8-α2−/− mice is in line with the results of our qRT-PCR experiments, which had demonstrated the expression of three benzodiazepine-sensitive GABAAR α-subunits (α1, α3, and α5) in addition to α2 (Figure 1c). Conversely, unchanged expression of ρ-subunits likely explains the reduced benzodiazepine (HZ166) sensitivity of GABAAR currents in hoxb8-α2−/− mice.
Figure 3.
Effects of HZ166 on GABA-evoked membrane currents in hoxb8-α2−/− mice and in wild-type (α2fl/fl) littermates. (a) Whole-cell voltage-clamp recordings of GABA (50 μM)-evoked membrane currents in superficial dorsal horn neurons of wild-type (α2fl/fl) (top) and hoxb8-α2−/− mice (bottom). HZ166 (10 μM) was coapplied together with GABA. Bicuculline (bic; 20 μM) was added at the end of the experiment to verify that all currents measured were GABAAR currents. (b, c) Statistical analysis of GABAAR current amplitudes (b) and of their potentiation by 10 μM HZ166 (c). n=6 and 8 cells for wild-type (α2fl/fl) and hoxb8-α2−/− mice, respectively. *P<0.05, unpaired Student's t-test.
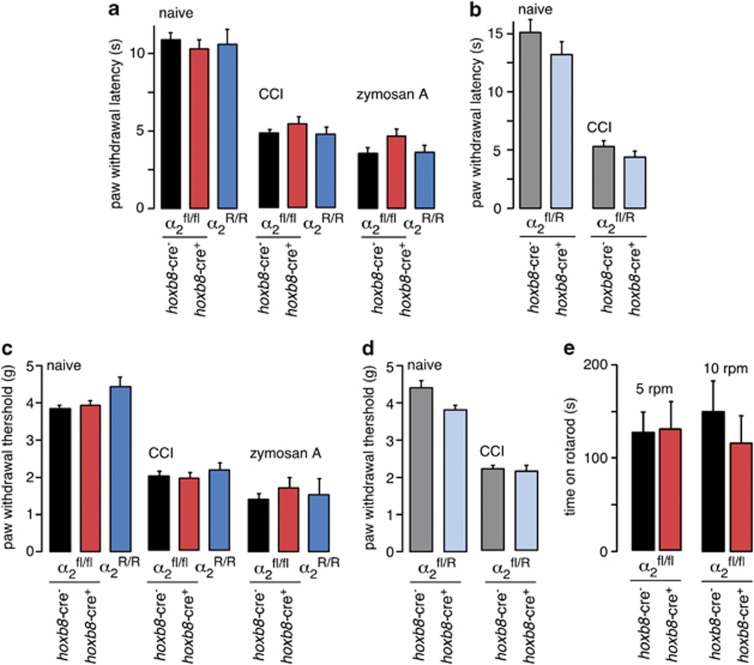
We then went on to investigate hoxb8-α2−/− and hoxb8-α2R/− mice in behavioral pain models and addressed their susceptibility to antihyperalgesia by systemically applied HZ166. The analysis of hoxb8-α2R/− mice was particularly interesting here because the unchanged expression of α2-GABAARs in the spinal cord (compare Figure 1b) rendered compensatory and adaptive changes highly unlikely. In addition to hoxb8-α2−/− mice and hoxb8-α2R/− mice (and their hoxb8-cre-negative littermates), we also included homozygous point-mutated mice (α2R/R). The comparison of HZ166-induced antihyperalgesia in α2R/R mice and in wild-type mice allowed us to determine the total contribution of α2-GABAARs to antihyperalgesia by HZ166, independent of their location. Conditional hoxb8-α2−/− knock-out mice and conditional hoxb8-α2R/− knock-in mice as well as the hoxb8-cre-negative (α2fl/fl and α2R/fl) littermates and global α2R/R point-mutated mice responded similarly to mechanical stimulation of their hindpaws with electronic von Frey filaments and to thermal stimulation with defined radiant heat (Figure 4a–d). Neuropathic pain sensitization induced through chronic constriction injury (CCI) of the sciatic nerve, and inflammatory hyperalgesia evoked by local subcutaneous zymosan A injection also developed similarly in all genotypes (Figure 4a–d). As a further control experiment, we assessed motor coordination in hoxb8-α2−/− and wild-type (α2fl/fl) littermates in the rotarod test at two different fixed rotational speeds (5 and 10 r.p.m.). Both lines managed to remain on the rotarod for similar time periods (Figure 4e).
Figure 4.
Characterization of baseline nociceptive sensitivity and of neuropathic and inflammatory hyperalgesia and of baseline motor coordination. (a) Baseline heat sensitivity, and neuropathic (CCI) and inflammatory (zymosan A) heat hyperalgesia in hoxb8-α2−/− mice (n=13, 6, and 7, for naïve, CCI, zymosan A-injected mice), in wild-type (α2fl/fl) littermates (n=27, 12, and 15), and in separately bred global α2R/R point-mutated mice of the same genetic background (n=13, 6, and 7). P>0.25, ANOVA followed by Bonferroni post hoc test. (b) Same as a, but spinal cord-specific α2(H101R) point-mutated (hoxb8-α2R/-) mice (n=6, for both naïve and CCI mice) and hoxb8-cre-negative hoxb8-α2R/fl littermates (n=7, for both naïve and CCI mice). P>0.26, unpaired student t-test. (c, d) Same as a, b, but mechanical sensitivity and hyperalgesia. P>0.51, ANOVA followed by Bonferroni post hoc test (c), and P>0.9 unpaired Student's t-test (d). n=6–7 mice, for all genotypes, pain models and tests. (e) Motor coordination assessed in the rotarod test. Time (mean±SEM) for which the mouse managed to remain on the rod rotating at two different rotational velocities. Unpaired student's t-test, P=0.45, for hoxb8-α2−/− (n=8) and wild-type (α2fl/fl) littermates (n=11), respectively.
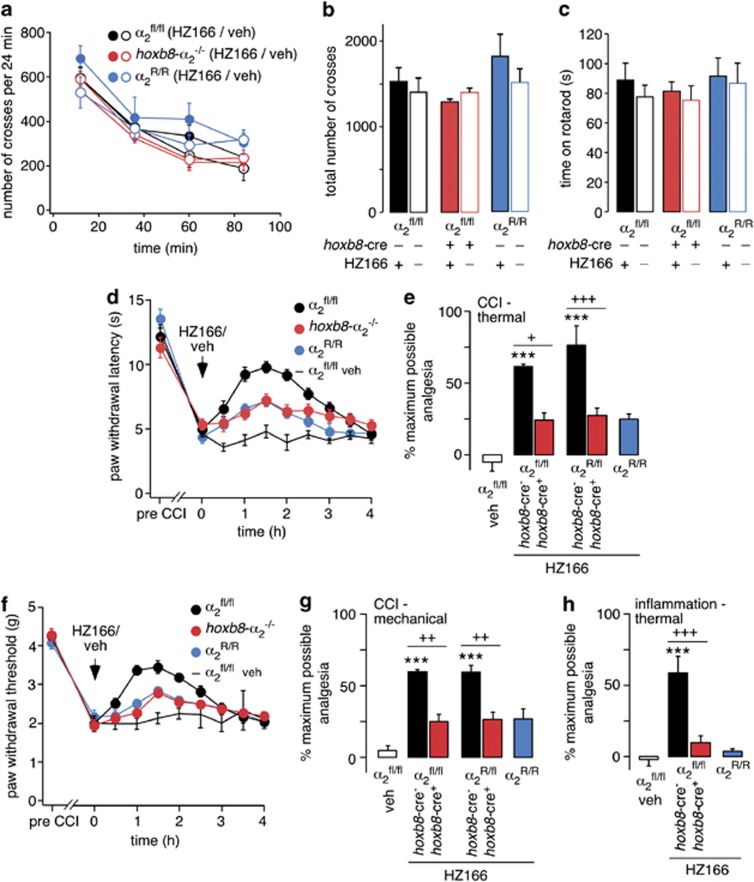
Finally, we addressed the antihyperalgesic action of HZ166 against neuropathic pain in the three types of mutant mice (hoxb8-α2−/−, hoxb8-α2R/− and α2R/R mice) and in the hoxb8-cre-negative wild-type (α2fl/fl) and α2R/fl littermates. For these experiments, we chose a dose of 16 mg/kg body weight applied intraperitoneally (i.p.), which has previously been shown to produce a saturating antihyperalgesic response in the absence of confounding sedation or motor impairment (Di Lio et al, 2011). We first verified that this dose of HZ166 had no effect on motor coordination or locomotor activity in neuropathic mice (Figure 5a–c). We then tested the effects of HZ166 against mechanical and thermal hyperalgesia in neuropathic mice (Figure 5d–g). The antihyperalgesic drug response reached a maximum between 60 and 90 min after drug injection (Figure 5d and f). This time interval was subsequently used to quantify HZ166-induced antihyperalgesia, expressed as percent maximum possible effect (MPE). In wild-type (hoxb8-cre-negative α2fl/fl) mice, HZ166 reduced thermal and mechanical hyperalgesia by 59.9±1.4% and 61.5±1.5% of pre-drug values (% MPE, mean±SEM, n=6, each) (Figure 5e and g). Both the time course and the degree of antihyperalgesia were very close to those reported previously by our group for wild-type C57BL/6 J mice (Di Lio et al, 2011). Antihyperalgesia by HZ166 was reduced in α2R/R mice to 24.7±3.6% and 26.6±7.0% of the maximum possible effect (thermal and mechanical hyperalgesia, respectively, n=6, each), indicating that about 60% of the antihyperalgesic actions of HZ166 were mediated by α2-GABAARs. The degrees of antihyperalgesia observed in both hoxb8-α2−/− mice (24.0±5.1% and 25.0±5.1%, n=6 each, for thermal and mechanical hyperalgesia, respectively) and hoxb8-α2R/− mice (27.4±5.1% and 26.4±5.2%, n=6 each) were virtually indistinguishable from that in global α2R/R point-mutated mice, indicating that supraspinal α2-GABAARs were not required for antihyperalgesia by systemic HZ166. We also investigated antihyperalgesic properties of HZ166 against thermal inflammatory hyperalgesia (Figure 5h). In wild-type (hoxb8-cre-negative α2fl/fl) mice, HZ166 reduced thermal hyperalgesia by 58.7±11.5% (n=7). This antihyperalgesia was almost lost in hoxb8-α2−/− mice (9.7±4.7%, n=7) and in global α2-point-mutated (α2R/R) mice (3.8±0.2%, n=7). Antihyperalgesia against mechanical stimuli was relatively small in wild-type mice (26.1±9.4%, n=7) and almost completely lost in hoxb8-α2−/− mice (4.7±12.5%, n=8). However, the difference between wild-type and hoxb8-α2−/− mice did not reach statistical significance (P=0.19) and effects of conditional deletion or mutation of the α2 subunit were therefore not further investigated.
Figure 5.
Locomotor activity, motor coordination and antihyperalgesia by HZ166 in α2-GABAA receptor-mutant mice. (a, b) Effects of HZ166 (16 mg/kg body weight i.p.) on locomotor activity in hoxb8-α2−/−, α2fl/fl, α2R/R mice with neuropathic hyperalgesia (7 days after CCI surgery). (a) Time course. Total number of beam crosses (mean±SEM) per 24 min over time (0–96 min). (b) Statistical analysis. Two-way ANOVA followed by Bonferroni post hoc test. Genotype treatment F(5,42)=1.15, P=0.35. (c) Same genotypes and treatments as in a,b, but effects on motor coordination. Time spent on an accelerating rotarod (rotational velocity increasing from 4 r.p.m. to 40 r.p.m. within 5 min) (s, mean±SEM). Genotype treatment F(5,42)=0.36, P=0.87. (d–g) Antihyperalgesic actions of the same dose of HZ166 in conditional knock-out (hoxb8-α2−/−) and conditional knock-in (hoxb8-α2R/-) mice with neuropathic hyperalgesia (7 days after CCI surgery). (d) Changes in heat hyperalgesia (paw withdrawal latency, s, mean±SEM) over time after HZ166 (16 mg/kg) or vehicle administration. (e) Statistical analysis. ANOVA followed by Bonferroni post hoc test. F(5,31)=15.9. ***P<0.001 significant against vehicle. +P<0.05, and +++P<0.001 significantly different from hoxb8-cre-negative littermates. (f, g) Same as d, e, but mechanical hyperalgesia (paw withdrawal thresholds, g). F(5,39)=13.57. ++P<0.01 significant against hoxb8-cre-negative littermates. (h) Same as e, but antihyperalgesic effects of HZ166 against inflammatory heat hyperalgesia 48 hrs after zymosan A injection. F(3,25)=17.4. P<0.001, significant against hoxb8-cre-negative littermates; ***P<0.001 significant against vehicle.
The results of our experiments not only exclude that analgesia or antihyperalgesia by HZ166 requires supraspinal α2-GABAARs, but also render significant indirect effects (such as reversal of anxiety or stress induced hyperalgesia) through supraspinal α2-GABAARs unlikely. They thus provide firm evidence for a genuine antihyperalgesic action of systemically applied benzodiazepine site agonists through a specific interaction with nociceptive circuits at the spinal level.
DISCUSSION
Studies performed in mice carrying point-mutated benzodiazepine-insensitive GABAARs have allowed us to attribute the different in vivo actions of benzodiazepines to distinct GABAAR subtypes (Möhler et al, 2002). In the course of these studies, it was shown that the sedative actions of benzodiazepines depend on α1-GABAARs, (McKernan et al, 2000; Rudolph et al, 1999), whereas the anxiolytic actions were caused by a facilitation of α2-GABAARs (Löw et al, 2000). Other studies employing the same mouse lines helped to establish additional, less obvious potential indications for subtype-selective benzodiazepine site agonists (Rudolph and Knoflach, 2011). One example of such a previously unforeseen action is antihyperalgesia, ie, the reversal of pathologically exaggerated sensitivity to pain. Although several studies in rodents had suggested pain-modulating actions of benzodiazepine site agonists, it has been notoriously difficult to distinguish apparent analgesia or antihyperalgesia from confounding sedation. Work with GABAAR point-mutated mice provided for the first time compelling evidence for a pain-relieving action of spinal benzodiazepines and demonstrated a critical role of α2-GABAARs in this process (Knabl et al, 2008). In these experiments, pain relief manifested primarily in a reversal of pathologically increased pain sensitivity rather than in reduced responses to acute noxious stimuli, indicating that spinal benzodiazepines exerted a hyperalgesic rather than a genuine analgesic effect.
The availability of non-sedative benzodiazepine site agonists suitable for systemic administration prompted the question about a possible role in antihyperalgesia of α2-GABAARs residing in supraspinal circuits. This appears as an important issue because α2-GABAARs are not only found in the spinal cord but also in supraspinal CNS areas where they mediate for example the anxiolytic effects of classical benzodiazepines (Löw et al, 2000). α2-GABAARs in the brain might have contributed to benzodiazepine-induced antihyperalgesia through a genuine effect on the supraspinal nociceptive circuits, eg, in the rostral insular cortex (Jasmin et al, 2003). Alternatively, their antihyperalgesic effects could also have been secondary, reflecting eg, a reversal of anxiety-induced hyperalgesia (Andre et al, 2005; Vidal and Jacob, 1982). Furthermore, supraspinal GABAARs in the brainstem, in particular in the rostroventromedial medulla, are known to inhibit antinociceptive fiber tracts descending to the spinal cord and might thereby produce a pronociceptive effect (Harris and Westbrook, 1995; Luger et al, 1995; Tatsuo et al, 1999). In the present study, we have measured nociceptive withdrawal responses to address these questions. Although these nociceptive responses are primarily mediated by spinal circuits (ie, they remain in spinalized animals, see for example Schouenborg et al (1992)), they are highly susceptible to modulation by supraspinal pain control centers, such as the rostral insular cortex (Jasmin et al, 2003), the amygdala (Carrasquillo and Gereau, 2007), the rostroventromedial medulla (Tatsuo et al, 1999), and the periaqueductal gray (Harris and Westbrook, 1995). As such, they are well-suited for investigating the effects of supraspinal GABAA receptors on hyperalgesia. In the present study, the actions of HZ166 on nociceptive withdrawal responses were nearly identical in α2R/R, hoxb8-α2−/− and hoxb8-α2R/− mice, indicating that supraspinal α2-GABAARs did not have a detectable influence on HZ166-mediated antihyperalgesia. The present data therefore unambiguously demonstrate that the major (ie, the α2-GABAAR-mediated) component of antihyperalgesia by benzodiazepines occurs through a genuine effect on the spinal cord and that this antihyperalgesia is not secondary to effects of benzodiazepines on neuronal circuits in the brain. Our results hence also disprove the possibility that a reversal of anxiety-induced or stress-induced hyperalgesia contributed significantly to the antihyperalgesia measured in our experiments.
Previous studies had used intrathecal injections of diazepam or related benzodiazepines at the lumbar spinal level to demonstrate pain-relieving actions of benzodiazepines or of GABAAR agonists (reviewed in Zeilhofer et al, 2009). A critical role of α2-GABAARs in neuronal circuits of the spinal cord was therefore likely, yet still not proven, as the compounds injected might have reached supraspinal sites through rostral diffusion. The present work establishes that the spinal cord is the most relevant site for the antihyperalgesic actions of benzodiazepine site agonists.
In a previous study, we have examined the contribution of a subset of spinal α2-GABAARs, which reside on the central terminals of primary nociceptive afferent fibers (Witschi et al, 2011). This subset of α2-GABAARs was specifically ablated through sns-cre-mediated gabra2 gene deletion. The respective sns-α2−/− mice were analyzed in the same inflammatory and neuropathic pain models that have been used in the present study. These previous experiments had revealed that primary afferent α2-GABAARs make a partial (about 50% of the total α2 component) contribution to inflammatory antihyperalgesia. The present study shows that the α2-GABAAR-mediated component of inflammatory antihyperalgesia was completely lost in hoxb8-α2−/− mice and hence entirely of spinal origin. Analysis of the sns-α2−/− mice in neuropathic pain models had revealed that α2-GABAARs on primary nociceptors did not make any contribution to neuropathic antihyperalgesia. Again this antihyperalgesic action was completely lost in hoxb8-α2−/− mice and therefore also exclusively of spinal origin. Early in situ hybridization studies had found no α2-GABAARs on intrinsic dorsal horn neurons (Persohn et al, 1991; Wisden et al, 1991), but more recent work provided clear evidence for the expression of these receptors by excitatory and inhibitory neurons in the spinal dorsal horn (Paul et al, 2012), which is in line with the data presented here.
Subsequent to the discovery that α2-GABAARs are the major target for the anxiolytic actions of benzodiazepines, a significant number of benzodiazepine site agonists have been developed which show reduced sedative properties through improved α2 over α1 subtype selectivity (Rudolph and Knoflach, 2011). These compounds allowed an assessment of the potential analgesic and antihyperalgesic actions of such compounds after systemic administration in wild-type mice without confounding sedation. Studies testing these newly developed compounds revealed significant analgesic or antihyperalgesic properties in rodent pain models (Di Lio et al, 2011; Knabl et al, 2008; Nickolls et al, 2011, for a review see Zeilhofer et al, 2012). Comparison of the antihyperalgesic efficacies of different compounds with their pharmacological profiles at different GABAAR subtypes suggests that a rather high intrinsic activity at α2-GABAARs and a high α2 over α1 selectivity profile are necessary for significant antihyperalgesia in the absence of sedation (Zeilhofer et al, 2012). Although these results were consistent with the findings obtained in the GABAAR point-mutated mice discussed above, final proof that these antihyperalgesic effects indeed originated from α2-GABAARs was missing. Here we focused on one such compound, the novel partial benzodiazepine site agonist HZ166. The present study demonstrates that the antihyperalgesic actions of HZ166 were to a large extent mediated by α2-GABAARs (about 90% and 60% for inflammatory and neuropathic hyperalgesia, respectively).
Antihyperalgesia was not completely lost in the different GABAAR α2-mutant mice investigated here. Depending on the model used (ie, inflammatory or neuropathic hyperalgesia), between 10 and 40% of the total antihyperalgesia were retained in hoxb8-α2−/−, hoxb8-α2R/−, and α2R/R mice. This is consistent with our previous study employing intrathecal diazepam injections, where between 30 and 50% of the antihyperalgesia remained in α2R/R mice. At the spinal level, this remaining component was mediated by α3-GABAARs and/or α5-GABAARs (Knabl et al, 2008). It is likely that these spinal receptors also account for the antihyperalgesia retained in HZ166-treated hoxb8-α2−/− and hoxb8-α2R/− mice. For a given benzodiazepine site agonist, the actual contribution of α2-GABAAR vs α3-GABAARs and α5-GABAARs will depend on its potentiating effects at these GABAAR subtypes. Until similar studies as the present one have also been performed for α3- and α5-GABAARs, it cannot be excluded that GABAARs different from α2 (ie, α3-GABAARs and α5-GABAARs) also contribute through a supraspinal site.
The present study provides strong evidence for a genuine antihyperalgesic action of systemically applied non-sedative benzodiazepine site agonists and demonstrates the pivotal contribution of spinal cord circuits to this antihyperalgesia. A critical role of inhibitory neurons and neurotransmitter receptors in the spinal dorsal horn has been first proposed in the gate control theory of pain (Melzack and Wall, 1965), but attempts to translate this concept to pain therapy have largely been unsuccessful. The present results show that an enhancement of fast GABAergic inhibition in the spinal dorsal horn is a possible strategy to reverse pathological hyperalgesia. Provided that the results obtained with genetic mouse mutants translate to the action of α2-GABAAR selective drugs in humans, these agents should be devoid of sedation and memory impairment (Rudolph and Knoflach, 2011). Conversely, it is likely that such drugs will exert in addition to their antihyperalgesic actions also anxiolytic and possibly muscle relaxant properties (Rudolph and Knoflach, 2011), both of which should be beneficial to many chronic pain patients. The present finding therefore provide additional impetus for the development of subtype-selective benzodiazepine site agonists as novel antihyperalgesic agents.
FUNDING AND DISCLOSURE
This work was in part supported by a project grant from the Swiss National Science Foundation [131093 to HUZ], by the Special Programme on University Medicine (SPUM) ‘Novel approaches to chronic pain' of the Swiss National Science Foundation [124117 to HUZ], by an advanced investigator grant from the European Research Council [DHISP 250128 to HUZ], and by a grant from the National Institutes of Health [NS076517 to JC]. The authors declare that over the past three years, JC has received compensation for professional services from Promentis Pharmaceuticals Inc. and Addiction Therapeutix, UR has received compensation for professional services from Sunovion and from Concert Pharmaceuticals. JC holds a patent on HZ166 and analogs. HUZ has received compensation for professional services from AMT AG Advanced Materials Technology, AstraZeneca Canada, Concert Pharmaceuticals, Geistlich Pharma AG, Grünenthal, Novartis Pharma Schweiz AG, Roche Pharma AG Germany, and Sigma tau Pharma AG. After completion of this study, ADL became an employee of Clinipace Worldwide, JP became an employee of Vifor Pharma, and RW became an employee of Pfizer AG, Switzerland. The remaining authors declare no conflict of interest.
Acknowledgments
We thank Mike Poe for the synthesis of HZ166, Isabelle Camenisch for excellent technical assistance, and Dennis Kwame Boadum for animal care.
References
- Ahmadi S, Lippross S, Neuhuber WL, Zeilhofer HU. PGE2 selectively blocks inhibitory glycinergic neurotransmission onto rat superficial dorsal horn neurons. Nat Neurosci. 2002;5:34–40. doi: 10.1038/nn778. [DOI] [PubMed] [Google Scholar]
- Andre J, Zeau B, Pohl M, Cesselin F, Benoliel JJ, Becker C. Involvement of cholecystokininergic systems in anxiety-induced hyperalgesia in male rats: behavioral and biochemical studies. J Neurosci. 2005;25:7896–7904. doi: 10.1523/JNEUROSCI.0743-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atack JR, Wafford KA, Tye SJ, Cook SM, Sohal B, Pike A, et al. TPA023 [7-(1,1-Dimethylethyl)-6-(2-ethyl-2H-1,2,4-triazol-3-ylmethoxy)-3-(2-fluor ophenyl)-1,2,4-triazolo[4,3-b]pyridazine], an agonist selective for α2- and α3-containing GABAA receptors, is a nonsedating anxiolytic in rodents and primates. J Pharmacol Exp Ther. 2006;316:410–422. doi: 10.1124/jpet.105.089920. [DOI] [PubMed] [Google Scholar]
- Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87–107. doi: 10.1016/0304-3959(88)90209-6. [DOI] [PubMed] [Google Scholar]
- Benson JA, Löw K, Keist R, Möhler H, Rudolph U. Pharmacology of recombinant γ-aminobutyric acidA receptors rendered diazepam-insensitive by point-mutated α-subunits. FEBS Lett. 1998;431:400–404. doi: 10.1016/s0014-5793(98)00803-5. [DOI] [PubMed] [Google Scholar]
- Carrasquillo Y, Gereau RW. Activation of the extracellular signal-regulated kinase in the amygdala modulates pain perception. J Neurosci. 2007;27:1543–1551. doi: 10.1523/JNEUROSCI.3536-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coull JA, Boudreau D, Bachand K, Prescott SA, Nault F, Sik A, et al. Trans-synaptic shift in anion gradient in spinal lamina I neurons as a mechanism of neuropathic pain. Nature. 2003;424:938–942. doi: 10.1038/nature01868. [DOI] [PubMed] [Google Scholar]
- Di Lio A, Benke D, Besson M, Desmeules J, Daali Y, Wang ZJ, et al. HZ166, a novel GABAA receptor subtype-selective benzodiazepine site ligand, is antihyperalgesic in mouse models of inflammatory and neuropathic pain. Neuropharmacology. 2011;60:626–632. doi: 10.1016/j.neuropharm.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritschy JM, Möhler H. GABAA-receptor heterogeneity in the adult rat brain: differential regional and cellular distribution of seven major subunits. J Comp Neurol. 1995;359:154–194. doi: 10.1002/cne.903590111. [DOI] [PubMed] [Google Scholar]
- Harris JA, Westbrook RF. Effects of benzodiazepine microinjection into the amygdala or periaqueductal gray on the expression of conditioned fear and hypoalgesia in rats. Behav Neurosci. 1995;109:295–304. doi: 10.1037//0735-7044.109.2.295. [DOI] [PubMed] [Google Scholar]
- Harvey RJ, Depner UB, Wässle H, Ahmadi S, Heindl C, Reinold H, et al. GlyRα3: an essential target for spinal PGE2-mediated inflammatory pain sensitization. Science. 2004;304:884–887. doi: 10.1126/science.1094925. [DOI] [PubMed] [Google Scholar]
- Hösl K, Reinold H, Harvey RJ, Müller U, Narumiya S, Zeilhofer HU. Spinal prostaglandin E receptors of the EP2 subtype and the glycine receptor α3 subunit, which mediate central inflammatory hyperalgesia, do not contribute to pain after peripheral nerve injury or formalin injection. Pain. 2006;126:46–53. doi: 10.1016/j.pain.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Jasmin L, Rabkin SD, Granato A, Boudah A, Ohara PT. Analgesia and hyperalgesia from GABA-mediated modulation of the cerebral cortex. Nature. 2003;424:316–320. doi: 10.1038/nature01808. [DOI] [PubMed] [Google Scholar]
- Knabl J, Witschi R, Hösl K, Reinold H, Zeilhofer UB, Ahmadi S, et al. Reversal of pathological pain through specific spinal GABAA receptor subtypes. Nature. 2008;451:330–334. doi: 10.1038/nature06493. [DOI] [PubMed] [Google Scholar]
- Knabl J, Zeilhofer UB, Crestani F, Rudolph U, Zeilhofer HU. Genuine antihyperalgesia by systemic diazepam revealed by experiments in GABAA receptor point-mutated mice. Pain. 2009;1413:233–238. doi: 10.1016/j.pain.2008.10.015. [DOI] [PubMed] [Google Scholar]
- Löw K, Crestani F, Keist R, Benke D, Brünig I, Benson JA, et al. Molecular and neuronal substrate for the selective attenuation of anxiety. Science. 2000;290:131–134. doi: 10.1126/science.290.5489.131. [DOI] [PubMed] [Google Scholar]
- Luger TJ, Hayashi T, Weiss CG, Hill HF. The spinal potentiating effect and the supraspinal inhibitory effect of midazolam on opioid-induced analgesia in rats. Eur J Pharmacol. 1995;275:153–162. doi: 10.1016/0014-2999(94)00759-z. [DOI] [PubMed] [Google Scholar]
- McKernan RM, Rosahl TW, Reynolds DS, Sur C, Wafford KA, Atack JR, et al. Sedative but not anxiolytic properties of benzodiazepines are mediated by the GABAA receptor α1 subtype. Nat Neurosci. 2000;3:587–592. doi: 10.1038/75761. [DOI] [PubMed] [Google Scholar]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Mirza NR, Larsen JS, Mathiasen C, Jacobsen TA, Munro G, Erichsen HK, et al. NS11394 [3'-[5-(1-hydroxy-1-methyl-ethyl)-benzoimidazol-1-yl]-biphenyl-2-carbonitr ile], a unique subtype-selective GABAA receptor positive allosteric modulator: in vitro actions, pharmacokinetic properties and in vivo anxiolytic efficacy. J Pharmacol Exp Ther. 2008;327:954–968. doi: 10.1124/jpet.108.138859. [DOI] [PubMed] [Google Scholar]
- Morris HV, Dawson GR, Reynolds DS, Atack JR, Stephens DN. Both α2 and α3 GABAA receptor subtypes mediate the anxiolytic properties of benzodiazepine site ligands in the conditioned emotional response paradigm. Eur J Neurosci. 2006;23:2495–2504. doi: 10.1111/j.1460-9568.2006.04775.x. [DOI] [PubMed] [Google Scholar]
- Munro G, Ahring PK, Mirza NR. Developing analgesics by enhancing spinal inhibition after injury: GABAA receptor subtypes as novel targets. Trends Pharmacol Sci. 2009;30:453–459. doi: 10.1016/j.tips.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Munro G, Lopez-Garcia JA, Rivera-Arconada I, Erichsen HK, Nielsen EO, Larsen JS, et al. Comparison of the novel subtype-selective GABAA receptor-positive allosteric modulator NS11394 [3'-[5-(1-hydroxy-1-methyl-ethyl)-benzoimidazol-1-yl]-biphenyl-2-carbonitr ile] with diazepam, zolpidem, bretazenil, and gaboxadol in rat models of inflammatory and neuropathic pain. J Pharmacol Exp Ther. 2008;327:969–981. doi: 10.1124/jpet.108.144568. [DOI] [PubMed] [Google Scholar]
- Möhler H, Fritschy JM, Rudolph U. A new benzodiazepine pharmacology. J Pharmacol Exp Ther. 2002;300:2–8. doi: 10.1124/jpet.300.1.2. [DOI] [PubMed] [Google Scholar]
- Nickolls S, Mace H, Fish R, Edye M, Gurrell R, Ivarsson M, et al. A Comparison of the α2/3/5 Selective Positive Allosteric Modulators L-838,417 and TPA023 in Preclinical Models of Inflammatory and Neuropathic Pain. Adv Pharmacol Sci. 2011;2011:608912. doi: 10.1155/2011/608912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen RW, Sieghart W. International Union of Pharmacology. LXX. Subtypes of γ-aminobutyric acidA receptors: classification on the basis of subunit composition, pharmacology, and function. Update. Pharmacol Rev. 2008;60:243–260. doi: 10.1124/pr.108.00505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul J, Zeilhofer HU, Fritschy JM. Selective distribution of GABAA receptor subtypes in mouse spinal dorsal horn neurons and primary afferents. J Comp Neurol. 2012;520:3895–3911. doi: 10.1002/cne.23129. [DOI] [PubMed] [Google Scholar]
- Persohn E, Malherbe P, Richards JG. In situ hybridization histochemistry reveals a diversity of GABAA receptor subunit mRNAs in neurons of the rat spinal cord and dorsal root ganglia. Neuroscience. 1991;42:497–507. doi: 10.1016/0306-4522(91)90392-2. [DOI] [PubMed] [Google Scholar]
- Reichl S, Augustin M, Zahn PK, Pogatzki-Zahn EM. Peripheral and spinal GABAergic regulation of incisional pain in rats. Pain. 2012;153:129–141. doi: 10.1016/j.pain.2011.09.028. [DOI] [PubMed] [Google Scholar]
- Rivas FM, Stables JP, Murphree L, Edwankar RV, Edwankar CR, Huang S, et al. Antiseizure activity of novel γ-aminobutyric acidA receptor subtype-selective benzodiazepine analogues in mice and rat models. J Med Chem. 2009;52:1795–1798. doi: 10.1021/jm801652d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph U, Crestani F, Benke D, Brünig I, Benson JA, Fritschy JM, et al. Benzodiazepine actions mediated by specific γ-aminobutyric acidA receptor subtypes. Nature. 1999;401:796–800. doi: 10.1038/44579. [DOI] [PubMed] [Google Scholar]
- Rudolph U, Knoflach F. Beyond classical benzodiazepines: novel therapeutic potential of GABAA receptor subtypes. Nat Rev Drug Discov. 2011;10:685–697. doi: 10.1038/nrd3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sang CS, Hayes KS.2006Anticonvulsant medications in neuropathic painIn: McMahon SB, Koltzenburg M (eds)Wall and Melzack's Textbook of Pain6th edn.Elsevier [Google Scholar]
- Schouenborg J, Holmberg H, Weng HR. Functional organization of the nociceptive withdrawal reflexes. II. Changes of excitability and receptive fields after spinalization in the rat. Exp Brain Res. 1992;90:469–478. doi: 10.1007/BF00230929. [DOI] [PubMed] [Google Scholar]
- Scott-Stevens P, Atack JR, Sohal B, Worboys P. Rodent pharmacokinetics and receptor occupancy of the GABAA receptor subtype selective benzodiazepine site ligand L-838417. Biopharm Drug Dispos. 2005;26:13–20. doi: 10.1002/bdd.423. [DOI] [PubMed] [Google Scholar]
- Tatsuo MA, Salgado JV, Yokoro CM, Duarte ID, Francischi JN. Midazolam-induced hyperalgesia in rats: modulation via GABAA receptors at supraspinal level. Eur J Pharmacol. 1999;370:9–15. doi: 10.1016/s0014-2999(99)00096-5. [DOI] [PubMed] [Google Scholar]
- Vidal C, Jacob J. Hyperalgesia induced by non-noxious stress in the rat. Neurosci Lett. 1982;32:75–80. doi: 10.1016/0304-3940(82)90232-4. [DOI] [PubMed] [Google Scholar]
- Wieland HA, Lüddens H, Seeburg PH. A single histidine in GABAA receptors is essential for benzodiazepine agonist binding. J Biol Chem. 1992;267:1426–1429. [PubMed] [Google Scholar]
- Wisden W, Gundlach AL, Barnard EA, Seeburg PH, Hunt SP. Distribution of GABAA receptor subunit mRNAs in rat lumbar spinal cord. Brain Res Mol Brain Res. 1991;10:179–183. doi: 10.1016/0169-328x(91)90109-b. [DOI] [PubMed] [Google Scholar]
- Witschi R, Johansson T, Morscher G, Scheurer L, Deschamps J, Zeilhofer HU. Hoxb8-Cre mice: A tool for brain-sparing conditional gene deletion. Genesis. 2010;48:596–602. doi: 10.1002/dvg.20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witschi R, Punnakkal P, Paul J, Walczak J-S, Cervero F, Fritschy J-M, et al. Presynaptic α2-GABAA receptors in primary afferent depolarization in spinal pain control. J Neurosci. 2011;31:8134–8142. doi: 10.1523/JNEUROSCI.6328-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeilhofer HU, Benke D, Yévenes GE. Chronic pain states: pharmacological strategies to restore diminished inhibitory spinal pain control. Annu Rev Pharmacol Toxicol. 2012;52:111–133. doi: 10.1146/annurev-pharmtox-010611-134636. [DOI] [PubMed] [Google Scholar]
- Zeilhofer HU, Witschi R, Hösl K. Subtype-selective GABAA receptor mimetics—novel antihyperalgesic agents. J Mol Med. 2009;87:465–469. doi: 10.1007/s00109-009-0454-3. [DOI] [PubMed] [Google Scholar]