Abstract
AIM: To clarify the safety and efficacy of repeat endoscopic submucosal dissection (re-ESD) for locally recurrent gastric cancers after ESD.
METHODS: A retrospective evaluation was performed of the therapeutic efficacy, complications and follow-up results from ESD treatment for early gastric cancers in 521 consecutive patients with 616 lesions at St. Luke`s International Hospital between April 2004 and November 2012. In addition, tumor size, the size of resected specimens and the operation time were compared between re-ESD and initial ESD procedures. A flex knife was used as the primary surgical device and a hook knife was used in cases with severe fibrosis in the submucosal layer. Continuous variables were analyzed using the non-parametric Mann-Whitney U test and are expressed as medians (range). Categorical variables were analyzed using a Fisher’s exact test and are reported as proportions. Statistical significance was defined as a P-value less than 0.05.
RESULTS: The number of cases in the re-ESD group and the initial ESD group were 5 and 611, respectively. The median time interval from the initial ESD to re-ESD was 14 (range, 4-44 mo). En bloc resection with free lateral and vertical margins was successfully performed in all re-ESD cases without any complications. No local or distant recurrence was observed during the median follow-up period of 48 (range, 11-56 mo). Tumor size was not significantly different between the re-ESD group and the initial ESD group (median 22 mm vs 11 mm, P = 0.09), although the size of resected specimens was significantly larger in the re-ESD group (median 47 mm vs 34 mm, P < 0.05). There was a non-significant increase observed in re-ESD operation time compared to initial ESD (median 202 min vs 67 min, respectively, P = 0.06).
CONCLUSION: Despite the low patient number and short follow-up, the results suggest that re-ESD is a safe and effective endoscopic treatment for recurrent gastric cancer after ESD.
Keywords: Endoscopic submucosal dissection, Recurrent gastric cancer, Gastric cancer, Endoscopic mucosal resection, Therapeutic endoscopy
Core tip: Although endoscopic submucosal dissection (ESD) is widely accepted as one of the standard treatments for early gastric cancers, there are few reports on re-ESD in the literature. This study clarifies that re-ESD is a safe and effective endoscopic treatment for locally recurrent gastric cancers after ESD.
INTRODUCTION
Early gastrointestinal neoplasms have a low frequency of lymph node and distant metastases, which enables less invasive treatments using therapeutic endoscopy[1-4]. Endoscopic mucosal resection (EMR) is an accepted minimally invasive treatment for early gastrointestinal neoplasms[5-9]. Endoscopic submucosal dissection (ESD) is a safe and effective endoscopic treatment technique that directly dissects the submucosal layer allowing en bloc resection of early gastric cancers (EGCs). It improves the quality of life compared with surgical treatment and has an important role in the treatment of EGCs[10-13]. Although ESD yields histologically complete resections, cases of locally recurrent gastric tumors after initial ESD still occur[14-16].
There is currently no established standard treatment for these recurrent lesions, and there are few reports on repeated ESD (re-ESD) procedures. Therefore, the aim of the present study was to clarify the safety and efficacy of re-ESD for locally recurrent gastric cancers.
MATERIALS AND METHODS
Study populations
The clinical database of all patients who underwent ESD for EGCs at St. Luke’s International Hospital, Tokyo was retrospectively reviewed. Gastric ESD was performed in a total of 521 consecutive patients with 616 lesions and re-ESD was performed in five locally recurrent gastric cancers between April 2004 and November 2012. Gastric cancer treatment guidelines were applied to all re-ESD cases including those issued in 2004 and 2010 by the Japanese Gastric Cancer Association as well as the proposed extended criteria of Gotoda et al[17,18].
Re-ESD methods
Re-ESD was performed with a conventional single-accessory-channel endoscope (GIF-Q260J; Olympus Medical Systems, Tokyo, Japan). Marking dots for the incision were made 3-5 mm outside of lesion margins with a flex knife[19-21] (Flex KnifeTM, KD-630L; Olympus Medical Systems, Tokyo, Japan) (Figure 1A and B). A solution of 0.4%-0.5% sodium hyaluronate was injected into the submucosal layer beneath the lesion, and circumferential incisions were made around the marking dots with a flex knife. In cases where severe fibrosis prevented injection of the sodium hyaluronate solution, a hook knife (Hook Knife, KD-620LR; Olympus Medical Systems) was used for the dissection of the fibrotic layer[22-24] (Figure 1C). Hemostatic forceps (SDB2422; Pentax Co, Tokyo, Japan) were used during the procedure to control bleeding while the re-ESD was completed (Figures 2 and 3).
Figure 1.
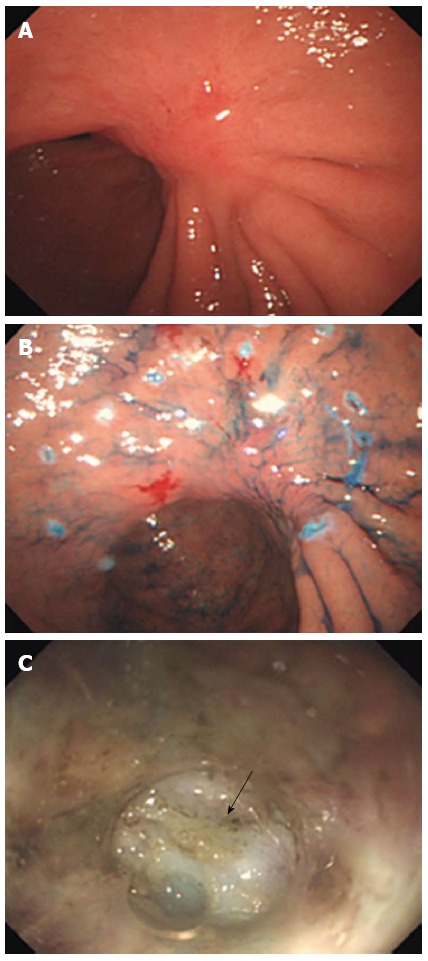
Conventional endoscopic view. A: Showing locally recurrent gastric cancer located in the lesser curvature of the gastric angulus; B: Marking dots for the incision delineating the outside margin of the lesion; C: Severe submucosal fibrosis was observed through a small-caliber transparent hood (arrow).
Figure 2.
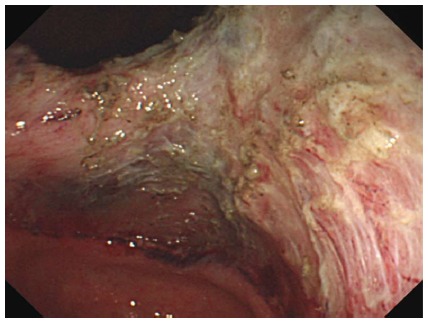
View of the post-endoscopic submucosal dissection ulcer.
Figure 3.
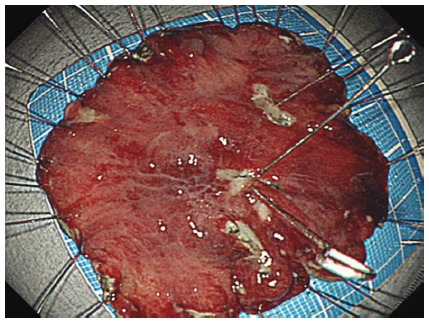
En bloc resection of the tumor without any complications.
Pathological assessment
Perpendicular sections at 2 mm intervals of re-ESD specimens were evaluated. Treatment was considered curative if specimens did not indicate invasion deeper than the submucosal or lymphovascular layer or show lateral and vertical margin involvement. En bloc resection was defined as resection of the entire lesion in one piece. All resections were categorized according to the National Comprehensive Cancer Network (NCCN) as follows: negative resection margin (R0), microscopic tumor infiltration (R1), and macroscopic residual tumor (R2). Endoscopic examinations and computed tomography (CT) were performed at 6 mo after re-ESD to check for local recurrence as well as lymph node and distant metastases.
Statistical analysis
Continuous variables were analyzed using the non-parametric Mann-Whitney U test and are expressed as median (range). Categorical variables were analyzed using a Fisher’s exact test and are reported as proportion. Statistical significance was defined as a P-value less than 0.05.
RESULTS
The characteristics of the initial ESD for 5 cases are summarized in Table 1. One patient was considered R1 with positive horizontal margins, but others were considered R0 with complete resection. Of the initial ESD procedures evaluated, 97.6% (601/616) were en bloc resections, 1.3% (8/616) required additional surgical intervention due to an incomplete resection (such as deep invasion of the tumor or lymph vascular invasion), 1.3% (8/616) resulted in postoperative bleeding, and 1.8% (11/616) had perforation. Pathological evaluation resulted in categorization of 95.3% (587/616) of resections as R0, with the remaining 4.7% (29/616) as R1 resections.
Table 1.
Characteristics of 5 initial endoscopic submucosal dissection cases
| Patient No. | Sex | Age, yr | Tumor location | Macroscopic type | Tumor size, mm | Specimen size, mm | Operation time, min | Histologicaltype | Resection margin category |
| 1 | Male | 78 | LB LC | I + IIa | 23 | 40 | 69 | Tub2 | R0 |
| 2 | Male | 67 | LB PW | IIc | 8 | 37 | 70 | Tub1 | R0 |
| 3 | Male | 64 | Ant PW | IIa + IIc | 14 | 36 | 47 | Tub1 | R0 |
| 4 | Male | 76 | Ang PW | IIc | 65 | 70 | 442 | Tub2 | R1 |
| 5 | Male | 51 | Ang LC | IIc | 40 | 45 | 44 | Tub2 | R0 |
| Median | 67 | 23 | 40 | 69 |
Ang: Angulus; Ant: Antrum; LB: Lower body; LC: Lesser curvature; PW: Posterior wall; R0: Negative resection margin; R1: Microscopic tumor infiltration; Tub1: Well differentiated adenocarcinoma; Tub2: Moderately differentiated adenocarcinoma; I: Elevated lesion; IIa: Slightly elevated lesion; IIc: Slightly depressed lesion.
Five of the 616 cases developed locally recurrent tumors and were treated by re-ESD (Table 2). The median time interval from the initial ESD to re-ESD was 14 (range, 4-44 mo). En bloc resections with free lateral and vertical margins were successfully performed without any complications in all re-ESD cases. Furthermore, there were no local or distant recurrences observed during the follow-up period, at a median of 48 (range, 11-56 mo). There was no significant difference in tumor size between re-ESD cases and all initial cases (22 mm vs 11 mm). However, there was a tendency for increased operation time for ESD procedures (202 min vs 67 min, P = 0.06), and re-ESD specimens were significantly larger than the initial resected specimens (47 mm vs 34 mm, P = 0.02) (Table 3).
Table 2.
Characteristics of re-endoscopic submucosal dissection in 5 cases
| Patient No. | Time after initial ESD, mo | Macroscopic type | Tumor size, mm | Specimen size, mm | Operation time, min | Histological type | Resection margin category | Complication |
| 1 | 44 | IIa | 22 | 47 | 210 | Tub2 | R0 | None |
| 2 | 9 | IIc | 8 | 45 | 82 | Tub1 | R0 | None |
| 3 | 14 | IIc | 11 | 32 | 43 | Tub1 | R0 | None |
| 4 | 12 | IIc | 27 | 59 | 353 | Tub1 | R0 | None |
| 5 | 4 | IIc | 42 | 77 | 202 | Por | R0 | None |
| Median | 14 | 22 | 47 | 202 |
R0: Negative resection margin; Tub1: Well differentiated adenocarcinoma; Tub2: Moderately differentiated adenocarcinoma; Por: Poorly differentiated adenocarcinoma; IIa: Slightly elevated lesion; IIc: Slightly depressed lesion; ESD: Endoscopic submucosal dissection.
Table 3.
Comparisons between re-endoscopic submucosal dissection and initial endoscopic submucosal dissection cases
| Re-ESD (n = 5) | Initial ESD (n = 606) | P value | |
| Tumor size | 22 mm | 11 mm | 0.09 |
| Median (range) | (8-42 mm) | (1.5-65 mm) | |
| Specimen size | 47 mm | 34 mm | 0.02 |
| Median (range) | (32-77 mm) | (13-92 mm) | |
| Operation time | 202 min | 67 min | 0.06 |
| Median (range) | (43-353 min) | (10-510 min) |
ESD: Endoscopic submucosal dissection.
DISCUSSION
ESD is accepted as one of the standard treatments for EGCs, enabling large en bloc resections. While this procedure typically results in histologically complete resections, cases of locally recurrent gastric tumors have occurred, with reported incidence rates between 0% and 3%[14-16,25]. Laparoscopic wedge resection, intragastric surgery, and laparoscopic-associated distal gastrectomy are some of the invasive treatment options for locally recurrent gastric cancers[26-28]. A recent report by Higashimaya et al[25] documented re-ESD as a minimally invasive, safe and effective procedure in a series of recurrent EGCs. In this study, re-ESD was successfully performed by en bloc resection with free lateral and vertical margins without any complications. Treatment of locally recurrent gastric cancers using the re-ESD technique results in less pain, less mortality, and shorter hospital stays, which obviates invasive surgical interventions.
Re-ESD operations tended to take longer than the initial ESD procedures, possibly because the tumor specimens were larger in size. The re-ESD procedure is considered technically difficult as a result of severe fibrosis in the submucosal layer that occurs at the site of the initial ESD. There is currently no efficient ESD method for lesions with submucosal fibrosis, therefore the surrounding tissue should first be dissected to evaluate the anatomical structure, followed by dissection towards the fibrotic lesion. Of additional importance in performing ESD and re-ESD procedures is the selection of an appropriate electrosurgical knife, such as a flash knife, flex knife, dual knife, or as in this study, the hook knife, which was used to dissect the submucosal layer with severe fibrosis.
Several limitations of this study should be noted. First, the study was of a retrospective design involving a limited number of cases from a single center, as the recurrence rate after ESD is very low. Second, even though experienced endoscopists performed the re-ESDs, the success rate depends on the technical proficiency of the endoscopists and the condition of the lesion. Although structural differences may result in variations in technical difficulty, this study did not establish whether the location of the lesion or macroscopic type affects the difficulty of the procedure.
In conclusion, this study demonstrates that re-ESD is a safe and effective endoscopic treatment for locally recurrent gastric cancer after ESD. As a result of the limited case number, further studies evaluating larger sample sizes and longer follow-ups are needed to assess the use of this procedure as a standard treatment for recurrent gastric tumors.
COMMENTS
Background
Endoscopic resection has been accepted as a minimally invasive treatment for early gastrointestinal neoplasms. Endoscopic submucosal dissection (ESD) allows for the dissection of the submucosa with resection of lesions en bloc. Although complete resection is expected in this procedure, incidences of local recurrence after the initial ESD are not fully eliminated. There is currently no standard treatment for these locally recurrent gastric cancers.
Research frontiers
There are few reports on repeat endoscopic submucosal dissection (re-ESD) for locally recurrent gastric cancers, and the safety and efficacy of this procedure have not been unequivocally addressed. In this study, the authors encountered 5 cases of recurrent gastric cancers, which were successfully treated with re-ESD procedures.
Innovations and breakthroughs
Repeat ESD for locally recurrent gastric tumors is not yet considered a standard treatment. This study demonstrates the safety and efficacy of the re-ESD technique. Furthermore, comparisons were made of tumor size, resected specimen size, and operation time between initial ESD and re-ESD procedures.
Applications
By demonstrating that re-ESD is a safe and effective therapy, this study presents a strategy for the treatment of patients with recurrent gastric tumors.
Terminology
ESD is a minimally invasive endoscopic technique for the treatment of early gastrointestinal neoplasms allowing direct dissection of the submucosal layer of the lesion with en bloc resection. Re-ESD is an endoscopic treatment technique for gastric tumors that locally recur after an initial ESD.
Peer review
The authors describe the treatment of recurrent early gastric cancers with re-ESD in a retrospective study. Five cases of recurrent tumors that were encountered following ESD treatment of early gastric cancer are described and analyzed. The employment of re-ESD procedures resulted in successful treatments with no observed complications, which may facilitate the establishment of this method as a standard treatment for recurrent gastric lesions.
Footnotes
P- Reviewers: Li XL, Tham TCK, Vivas S S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
References
- 1.Folli S, Morgagni P, Roviello F, De Manzoni G, Marrelli D, Saragoni L, Di Leo A, Gaudio M, Nanni O, Carli A, et al. Risk factors for lymph node metastases and their prognostic significance in early gastric cancer (EGC) for the Italian Research Group for Gastric Cancer (IRGGC) Jpn J Clin Oncol. 2001;31:495–499. doi: 10.1093/jjco/hye107. [DOI] [PubMed] [Google Scholar]
- 2.Hyung WJ, Cheong JH, Kim J, Chen J, Choi SH, Noh SH. Application of minimally invasive treatment for early gastric cancer. J Surg Oncol. 2004;85:181–15; discussion 186. doi: 10.1002/jso.20018. [DOI] [PubMed] [Google Scholar]
- 3.Pech O, May A, Gossner L, Rabenstein T, Manner H, Huijsmans J, Vieth M, Stolte M, Berres M, Ell C. Curative endoscopic therapy in patients with early esophageal squamous-cell carcinoma or high-grade intraepithelial neoplasia. Endoscopy. 2007;39:30–35. doi: 10.1055/s-2006-945040. [DOI] [PubMed] [Google Scholar]
- 4.Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, Fujisaki J, Sano T, Yamaguchi T. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–152. doi: 10.1007/s10120-009-0515-x. [DOI] [PubMed] [Google Scholar]
- 5.Tada M, Murakami A, Karita M, Yanai H, Okita K. Endoscopic resection of early gastric cancer. Endoscopy. 1993;25:445–450. doi: 10.1055/s-2007-1010365. [DOI] [PubMed] [Google Scholar]
- 6.Inoue H, Tani M, Nagai K, Kawano T, Takeshita K, Endo M, Iwai T. Treatment of esophageal and gastric tumors. Endoscopy. 1999;31:47–55. doi: 10.1055/s-1999-13647. [DOI] [PubMed] [Google Scholar]
- 7.Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229. doi: 10.1136/gut.48.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katada C, Muto M, Manabe T, Ohtsu A, Yoshida S. Local recurrence of squamous-cell carcinoma of the esophagus after EMR. Gastrointest Endosc. 2005;61:219–225. doi: 10.1016/s0016-5107(04)02756-7. [DOI] [PubMed] [Google Scholar]
- 9.Higuchi K, Tanabe S, Koizumi W, Sasaki T, Nakatani K, Saigenji K, Kobayashi N, Mitomi H. Expansion of the indications for endoscopic mucosal resection in patients with superficial esophageal carcinoma. Endoscopy. 2007;39:36–40. doi: 10.1055/s-2006-945148. [DOI] [PubMed] [Google Scholar]
- 10.Neuhaus H, Costamagna G, Devière J, Fockens P, Ponchon T, Rösch T. Endoscopic submucosal dissection (ESD) of early neoplastic gastric lesions using a new double-channel endoscope (the “R-scope”) Endoscopy. 2006;38:1016–1023. doi: 10.1055/s-2006-944830. [DOI] [PubMed] [Google Scholar]
- 11.Oda I, Saito D, Tada M, Iishi H, Tanabe S, Oyama T, Doi T, Otani Y, Fujisaki J, Ajioka Y, et al. A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer. 2006;9:262–270. doi: 10.1007/s10120-006-0389-0. [DOI] [PubMed] [Google Scholar]
- 12.Oka S, Tanaka S, Kaneko I, Mouri R, Hirata M, Kawamura T, Yoshihara M, Chayama K. Advantage of endoscopic submucosal dissection compared with EMR for early gastric cancer. Gastrointest Endosc. 2006;64:877–883. doi: 10.1016/j.gie.2006.03.932. [DOI] [PubMed] [Google Scholar]
- 13.Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, Ohnita K, Mizuta Y, Shiozawa J, Kohno S. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58:331–336. doi: 10.1136/gut.2008.165381. [DOI] [PubMed] [Google Scholar]
- 14.Yamamoto H, Kawata H, Sunada K, Satoh K, Kaneko Y, Ido K, Sugano K. Success rate of curative endoscopic mucosal resection with circumferential mucosal incision assisted by submucosal injection of sodium hyaluronate. Gastrointest Endosc. 2002;56:507–512. doi: 10.1067/mge.2002.128108. [DOI] [PubMed] [Google Scholar]
- 15.Oda I, Oyama T, Abe S, Ohnita K, Kosaka T, Hirasawa K, Ishido K, Nakagawa M, Takahashi S. Preliminary results of multicenter questionnaire study on long-term outcomes of curative endoscopic submucosal dissection for early gastric cancer. Dig Endosc. 2013:Epub ahead of print. doi: 10.1111/den.12141. [DOI] [PubMed] [Google Scholar]
- 16.Onozato Y, Ishihara H, Iizuka H, Sohara N, Kakizaki S, Okamura S, Mori M. Endoscopic submucosal dissection for early gastric cancers and large flat adenomas. Endoscopy. 2006;38:980–986. doi: 10.1055/s-2006-944809. [DOI] [PubMed] [Google Scholar]
- 17.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 18.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 19.Yahagi N, Fujishiro M, Imagawa A, Kakushima N, Iguchi M, Omata M. Endoscopic submucosal dissection for the reliable en bloc resection of colorectal mucosal tumors. Dig Endosc. 2004;16:S89–S92. [Google Scholar]
- 20.Ishii N, Itoh T, Horiki N, Matsuda M, Setoyama T, Suzuki S, Uemura M, Iizuka Y, Fukuda K, Suzuki K, et al. Endoscopic submucosal dissection with a combination of small-caliber-tip transparent hood and flex knife for large superficial colorectal neoplasias including ileocecal lesions. Surg Endosc. 2010;24:1941–1947. doi: 10.1007/s00464-010-0883-7. [DOI] [PubMed] [Google Scholar]
- 21.Ishii N, Horiki N, Itoh T, Uemura M, Maruyama M, Suzuki S, Uchida S, Izuka Y, Fukuda K, Fujita Y. Endoscopic submucosal dissection with a combination of small-caliber-tip transparent hood and flex knife is a safe and effective treatment for superficial esophageal neoplasias. Surg Endosc. 2010;24:335–342. doi: 10.1007/s00464-009-0560-x. [DOI] [PubMed] [Google Scholar]
- 22.Chiu PW, Chan KF, Lee YT, Sung JJ, Lau JY, Ng EK. Endoscopic submucosal dissection used for treating early neoplasia of the foregut using a combination of knives. Surg Endosc. 2008;22:777–783. doi: 10.1007/s00464-007-9479-2. [DOI] [PubMed] [Google Scholar]
- 23.Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M, Miyata Y. Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol. 2005;3:S67–S70. doi: 10.1016/s1542-3565(05)00291-0. [DOI] [PubMed] [Google Scholar]
- 24.Oyama T. Counter traction makes endoscopic submucosal dissection easier. Clin Endosc. 2012;45:375–378. doi: 10.5946/ce.2012.45.4.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higashimaya M, Oka S, Tanaka S, Numata N, Sanomura Y, Yoshida S, Arihiro K, Chayama K. Endoscopic submucosal dissection for residual early gastric cancer after endoscopic submucosal dissection. Gastrointest Endosc. 2013;77:298–302. doi: 10.1016/j.gie.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 26.Asano M. Endoscopic submucosal dissection and surgical treatment for gastrointestinal cancer. World J Gastrointest Endosc. 2012;4:438–447. doi: 10.4253/wjge.v4.i10.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yano H, Kimura Y, Iwazawa T, Monden T. Laparoscopic management for local recurrence of early gastric cancer after endoscopic mucosal resection. Surg Endosc. 2005;19:981–985. doi: 10.1007/s00464-004-8172-y. [DOI] [PubMed] [Google Scholar]
- 28.Tonouchi H, Mohri Y, Kobayashi M, Tanaka K, Ohi M, Kusunoki M. Laparoscopy-assisted distal gastrectomy with laparoscopic sentinel lymph node biopsy after endoscopic mucosal resection for early gastric cancer. Surg Endosc. 2007;21:1289–1293. doi: 10.1007/s00464-007-9221-0. [DOI] [PubMed] [Google Scholar]


