Abstract
Background
Hepatitis E virus (HEV) has been described as an emerging pathogen in Brazil and seems to be widely disseminated among swine herds. An autochthonous human case of acute hepatitis E was recently reported. To obtain a better understanding of the phenotypic profiles of both human and swine HEV strains, a experimental study was conducted using the animal model, Macaca fascicularis.
Methods
Six cynomolgus monkeys (Macaca fascicularis) were inoculated intravenously with swine HEV genotype 3 that was isolated from naturally and experimentally infected pigs in Brazil and the Netherlands. Two other monkeys were inoculated with HEV genotype 3 that was recovered from Brazilian and Argentinean patients with locally acquired acute and fulminant hepatitis E. The haematological, biochemical, and virological parameters of all animals were monitored for 67 days.
Results
Subclinical hepatitis was observed in all monkeys after inoculation with HEV genotype 3 that was recovered from the infected swine and human patients. HEV RNA was detected in the serum and/or faeces of 6 out of the 8 cynomolgus monkeys between 5 and 53 days after inoculation. The mild inflammation of liver tissues and elevations of discrete liver enzymes were observed. Seroconversions to anti-HEV IgM and/or IgG were detected in 7 animals. Reactivities to anti-HEV IgA were also detected in the salivary samples of 3 animals. Interestingly, all of the infected monkeys showed severe lymphopenia and a trend toward monocytosis, which coincided with elevations in alanine aminotransferase and antibody titres.
Conclusions
The ability of HEV to cross the species barrier was confirmed for both the swine (Brazilian and Dutch) and human (Argentinean) strains, thus reinforcing the zoonotic risk of hepatitis E in South America. Cynomolgus monkeys that were infected with HEV genotype 3 developed subclinical hepatitis that was associated with haematological changes. Haematological approaches should be considered in future studies of HEV infection.
Keywords: Swine HEV, Human HEV, Lymphopenia, Fulminant hepatic failure, Genotype 3, Macaca fascicularis
Background
Infection with hepatitis E virus (HEV) has been well documented in endemic areas, such as southeastern and central Asia, the Middle East, the northern and western parts of Africa, and North America [1]. In areas of poor sanitation, epidemics occur periodically, and infection is mainly transmitted via the faecal contamination of water. However, the global burden of HEV infection is more influenced by sporadically transmitted hepatitis cases than by epidemics [2]. In South America and other non-endemic areas, epidemics of hepatitis E have not yet been reported. Nevertheless, sporadic cases of both acute, self-limited hepatitis and fulminant hepatic failure have been reported in Venezuela, Brazil, and Argentina [3]. In most of these cases, the human isolates were related to swine genotype 3 HEV strains from the same region.
In Brazil, HEV genotype 3 seems to be widely disseminated. The virus has been detected in swine and effluent samples from farms and slaughterhouses. Among swine handlers, the anti-HEV IgG seroprevalence is estimated to be 6 to 8% [4,5] and is approximately 2% in urban areas [6,7]. Although national data show high numbers of alleged cases, the true incidence of hepatitis E in the Brazilian population is uncertain because a testing protocol for HEV has not yet been established. A retrospective study of sera from patients with non-A-C acute hepatitis from 2005–2009 led to the identification of the first autochthonous human case of acute HEV infection. The genetic relatedness of this strain and the genotype 3 HEV in pigs is indicative of the zoonotic circulation of HEV in Brazil [8-10].
Infection studies using Macaca fascicularis, Aotus trivirgatus, Macaca mulatta, and Pan troglodytes that have evaluated the course of HEV infection have been previously described [11-16]. These studies have created an experimental foundation for the understanding of the immunological behaviour of HEV, including the cross-reactivities among different isolated strains [17,18] and the conferral of cross-immunity among genotypes 3 and 4 in swine hosts [19]. HEV genotype 3 shows dose-dependent infectivity [20] and is able to cross species barriers [21-23], causing infection in species such as the cynomolgus monkey [24], which is considered to be a well-established model for human HEV infection.
Currently, most experimental studies of HEV investigate only virological and hepatic parameters. However, there is limited information available describing the extra-hepatic manifestations of HEV infection, including a few reports highlighting other clinical findings, such as pancreatitis, thrombocytopenia, aplastic anaemia, acute thyroiditis, glomerulonephritis, and neurologic disorders, as reviewed by Dalton et al. [25]. To obtain a better understanding of the phenotypic profiles of both human and swine Brazilian HEV strains, a descriptive study was conducted in the experimental model Macaca fascicularis. Human and swine HEV samples from Argentina and the Netherlands were also used as inocula. This article describes, for the first time, haematological disorders that could be interpreted as extra-hepatic manifestations of HEV infection.
Methods
Animals
Ten clinically healthy young adult cynomolgus monkeys, each weighing 1.5–6.0 kg, were provided for use in this study by the Non-Human Primates Breeding Service Centre (CECAL) of the Oswaldo Cruz Foundation (Fiocruz), Rio de Janeiro, Brazil. The study protocol was approved (L-0033/07) by the Ethics Committee for Animal Use (CEUA), Fiocruz, and was conducted in strict accordance with the recommendations from the Guide for the Care and Use of Laboratory Animals of the Brazilian Society of Science in Laboratory Animals (SBCAL) and the National Council for Control of Animal Experimentation (CONCEA, Brazil). The animals that were selected for the study were free of simian immunodeficiency virus (SIV) and simian type D retrovirus (SRV/D). They were also negative for anti-HEV IgG in their sera and had no inflammatory changes in their pre-study liver biopsies. During the study and quarantine periods, the monkeys were maintained at Animal Biosafety Level 2 in CECAL, Fiocruz, and were kept individually in stainless steel squeeze-back cages in a climate-controlled room (temperature of 22 ± 1°C and humidity 55 ± 5%) with a 12 h light/dark cycle.
Inocula
The Brazilian swine HEV (Br-swine) genotype 3b (GenBank EF591853.1) strain was isolated from a faecal suspension that was obtained from a naturally infected pig from a commercial farm in Rio de Janeiro state [12]. The Dutch swine HEV (D-swine) genotype 3 (GenBank DQ996399) strain, which was kindly supplied by the Central Veterinary Institute of Wageningen University and Research Centre, the Netherlands, was obtained from an experimentally infected pig [23].
The Brazilian human HEV (Br-human) genotype 3b (GenBank GQ421465) strain was isolated from a 1-ml serum sample that was obtained from a 30-year-old male with acute hepatitis E [26]. The Argentinean human HEV (Ar-human) sample was kindly provided by the Dr. Carlos Malbran Institute, Buenos Aires, and was prepared from a pool of 1 ml of serum and the faeces of a 3-month-old female with fulminant acute hepatic failure (Table 1). This study was approved by the institutional review boards (CEP-Fiocruz No. 22/03), and a signed informed consent form was obtained from each participant.
Table 1.
Sources of hepatitis E virus inocula used to infect the cynomolgus monkeys
| Source | Inocula | Anti-HEV serology | HEV RT-PCR/real-time PCR | Genotype | Age of monkey (years) | Animal ID |
|---|---|---|---|---|---|---|
| Swine |
Pooled faeces (3.0 ml) |
_ |
HEV RNA+/105 copies/ml |
3 |
15 |
I3 |
| 18 |
Q11 |
|||||
| 2 |
X15 |
|||||
| Swine |
Pooled faeces (3.0 ml) |
_ |
HEV RNA+/106 copies/ml |
3 |
11 |
O1 |
| 17 |
G3 |
|||||
| 19 |
F3 |
|||||
| Child, female, 3 months old (FALF*) |
Serum and faeces (1.0 ml) |
Undetectable |
Undetectable/103 copies/ml |
3 |
7 |
R7 |
| Adult, male, 30 years old (AH**) |
Serum (1.0 ml) |
IgG+/IgM+ |
HEV RNA+/106 copies/ml |
3 |
14 |
J3 |
| - | 10% Phosphate-buffered saline (1.0 ml) | _ | Undetectable | _ | 16 |
I2 |
| 18 | Q12 |
FALF* – fatal acute liver failure; AH** – acute hepatitis.
Experimental design
Eight cynomolgus monkeys were intravenously inoculated with either Br-swine (monkeys X15, Q11, and I3), Dutch swine (O1, G3, and F3), Br-human (J3), or Ar-human (R7) viruses. As a control, 2 monkeys (Q12 and I2) were inoculated with a 10% phosphate-buffered saline (PBS) solution (pH 7.3). All of the animals had been previously screened for the anti-hepatitis A virus (HAV) and anti-HEV antibodies by the enzyme-linked immunosorbent assay (ELISA) using the Bioelisa HAV kit (Spain Biokit, Barcelona, Spain) and the IgG anti-HEV kit (MP Biomedicals, California, USA), respectively. During the study and quarantine periods, the monkeys were housed in an Animal Biosafety Level 2 facility. The animals were clinically monitored for 67 days post infection (dpi); they were monitored daily by the veterinary staff and checked weekly for rectal temperature and weight changes. Whole-blood samples (3 ml) were collected by venipuncture at 0, 7, 14, 25, 32, 39, 46, 53, and 67 dpi for HEV RNA and antibody detection. Faecal samples were collected at 0, 5, 7, 12, 14, 18, 21, 25, 27, 32, 35, 39, 42, 49, 53, 56, 63, and 67 dpi for HEV RNA detection and were stored in polystyrene tubes at -20°C until use. Salivary samples were collected from Q11, J3, O1, G3, F3, I3, and Q12 using OraSure® collection devices (OraSure Technologies Incorporated, Pennsylvania, USA) at 0, 7, 14, 21, 28, 35, 42, and 53 dpi for IgA detection. For the collection of saliva and blood and liver biopsies (weekly), the animals were anaesthetised with ketamine hydrochloride at 20 mg/kg (Vetanarcol, König, Argentina) and xylazine hydrochloride at 0.1 mg/kg (Syntec Brazil, São Paulo, Brazil). At 67 dpi, all of the animals were euthanised under deep barbiturate anaesthesia with sodium thiopental 2.5% at 25 mg/kg (Thiopentax, Cristalia, São Paulo, Brazil), which was delivered intravenously. Subsequently, cardiac punctures were performed, and the animals were euthanised by exsanguination.
ELISA tests
The presence of anti-HEV IgG was detected using a commercial ELISA Kit (MP Biomedicals, Ohio, USA) according to the manufacturer’s instructions. Pre- and post-inoculation samples were also tested for macaque anti-HEV IgG, IgM (sera), and IgA (saliva) using a modified protocol (Dr. Julio Moran Laboratories, Zurich, Switzerland) for the commercially available DiaCheck anti-human HEV antibody assay with an adapted goat anti-macaque immunoglobulin conjugate (Fitzgerald Industries International, Inc., Massachusetts, USA).
Real-time PCR (qPCR)
Total RNA was extracted from 140 μl of a serum and faecal suspension (10% w/v in PBS) using the QIAamp Viral RNA Kit (Qiagen, California, USA). Reverse transcription was performed using 25 μl of RNA, 200 IU/ml Superscript III reverse transcriptase (Life technologies Corp., USA), and 20 pmol/μl random primer (Life technologies Corp., USA). A quantitative TaqMan real-time PCR assay was performed using a standard curve that was generated with a plasmid clone from a Brazilian swine strain that had been previously characterised as having genotype 3 [26]. Plasmid serial dilutions ranging from 108 to 101 were used to provide quantification parameters.
The qPCR reactions were performed in duplicate in a final volume of 25 μl consisting of 12.5 μl Universal PCR Master Mix (Life technologies Corp., USA), 5 μl cDNA, endonuclease-free water, and the previously described primers and probes [27]. The following conditions were used for the qPCR: 50°C for 2 min to activate the uracil N-glycosylase (UNG), an initial denaturation step at 95°C for 15 min, 45 cycles of denaturation at 95°C for 10 sec, and annealing/extension at 55°C for 1 min. The amplification data were collected and analysed with Applied Biosystems 7500 Software® v2.0. Samples were considered to be positive when the signal crossed the threshold line, presenting a characteristic sigmoid curve. The number of viral genome copies (GC) was determined by adjusting the values according to the volumes that were used for each step of the procedure (i.e., extraction, cDNA synthesis, and the qPCR reaction).
Liver function
Alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), and total bilirubin (Tb) serum levels were determined using a commercial enzymatic colorimetric method (Abbott, IL, USA). The baseline levels were obtained from blood samples of the pre-inoculation and control groups.
Peripheral blood cell counts
Haematological, biochemical, and serological parameters were established for each animal using individual pre-inoculation samples. Blood samples were collected using ethylenediaminetetraacetic acid (EDTA) capillary tubes. Peripheral blood cells were counted using a commercial veterinary haematology analyser (Roche Diagnostica, Brazil).
Histopathological analyses
Liver biopsies were collected at 0, 7, 14, 25, 32, 39, 46, 53, and 67 dpi by ultrasound-guided liver puncture, as described previously [28]. A portion of each sample was stored in 10% buffered formalin (pH 7.0) before being processed and embedded in paraffin according to standard methods. Paraffin blocks were sectioned at 4 μm and stained with haematoxylin-eosin, Giemsa stain, and Masson’s trichrome stain (Sigma-Aldrich, USA). The slides were examined under light microscopy, and inflammatory lesions were quantified using a scale from 0 to 4 that was based on the number of focal mononuclear cell infiltrates per 10 hepatic lobules: 0 = no inflammation, 1 = 1 to 2 focal infiltrates (poor), 2 = 3 to 5 focal infiltrates (mild), 3 = 6 to 10 focal infiltrates (moderate), and 4 = over 10 focal infiltrates (severe) as described previously [29]. A portion of each liver sample was stored in liquid nitrogen until the HEV analysis was performed. Pre-inoculation liver biopsies were performed to confirm the absence of other liver diseases.
HEV antigen detection
Frozen liver sections (4 μm) that had been obtained at 67 dpi were examined by indirect immunofluorescence using a rabbit anti-HEV polyclonal antibody at a 1:150 dilution (Research Diagnostics Inc., USA) as the primary antibody (1 mg/ml), followed by a FITC-labelled goat anti-rabbit IgG antibody (2 mg/ml) at a 1:750 dilution (Sigma-Aldrich) as the secondary antibody. The slides were counterstained with Evans Blue, mounted with ProLong© Gold Slow Fade in glycerol with DAPI stain (Life technologies Corp., USA), and covered with a coverslip. Images of the positive fields were obtained by confocal microscopy (LSM Zeiss 510 Meta Carl Zeiss, Oberkochen, Germany).
Statistical analyses
Data are expressed as the means ± standard deviations (SD). Statistical analyses for the continuous variables were performed using 2-way ANOVA non-parametric statistics. A value of P < 0.05 was considered to be statistically significant. All of the calculations were performed using The R Project for Statistical Computing [30], and the graphics were produced using GraphPad InStat version 5.01 for Windows (GraphPad Software, San Diego, CA, USA).
Results
Cynomolgus monkeys inoculated with faecal suspensions from Brazilian and Dutch swine
Detection of HEV RNA in serum and faecal samples
After inoculation with the Brazilian swine HEV (Br-swine), all of the animals were successfully infected. HEV RNA was detected by qPCR in the sera and faeces of all infected cynomolgus monkeys with the exception of monkey X15, which did not have viraemia but exhibited viral shedding in the faeces between 14 and 21 dpi. One animal showed a protracted pattern of viral shedding in the faeces from 21 dpi onwards. Out of the 3 animals that were inoculated with the Dutch swine HEV (D-swine), HEV RNA was detected at earlier time points in 2 (O1 and G3), with the virus being detected in the faeces at 5 or 7 dpi and in the sera at 7 to 14 dpi (Table 2).
Table 2.
Summary of biochemical, histopathological, and virological patterns during HEV (genotype 3) infection in cynomolgus monkeys
| Inocula | Animal ID |
ALT |
AST |
GGT |
Tb |
**Liver injury |
HEV RNA detection |
***anti-HEV |
Clinical interpretation**** | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (IU/dL) ( # maximum value obtained) | (Score) |
(dpi*) |
(EIA reactivity) |
||||||||||
|
Serum |
Saliva |
||||||||||||
| Serum | Faeces | IgM | IgG | IgA | IgA | ||||||||
| Br-swine |
X15 |
73 |
295 |
315 |
0.8 |
2 |
--- |
14 - 21 |
+ |
+ |
+ |
nt |
Subclinical hepatitis E |
| Q11 |
24 |
31 |
64 |
0.7 |
1 |
14 |
7 - 21 |
+ |
+ |
+ |
- |
Subclinical hepatitis E without biochemical disorders |
|
| I3 |
40 |
54 |
224 |
0.8 |
2 |
39 - 53 |
21 - 53 |
- |
- |
- |
+ |
Subclinical hepatitis E |
|
| D-swine |
01 |
40 |
119 |
237 |
0.8 |
1 |
14 |
5 - 18 |
+ |
+ |
+ |
- |
Subclinical hepatitis E |
| G3 |
32 |
42 |
138 |
0.8 |
1 |
7 - 14 |
7 - 18 |
+ |
+ |
+ |
+/- |
Subclinical hepatitis E without biochemical disorders |
|
| F3 |
99 |
302 |
238 |
0.7 |
1 |
--- |
--- |
+ |
+ |
+ |
+ |
Biochemical and histological hepatitis E |
|
| Br-human |
J3 |
57/46 |
50 |
293 |
0.8 |
1 |
--- |
--- |
- |
+ |
- |
- |
Biochemical and histological hepatitis E |
| Ar-human |
R7 |
21 |
213 |
188 |
0.8 |
0 |
--- |
14 - 27 |
+ |
+ |
+ |
nt |
Subclinical hepatitis E |
| Control | I2 |
21 |
43 |
92 |
0.8 |
0 |
--- |
--- |
- |
- |
- |
nt |
Uninfected |
| Q12 | 21 | 116 | 103 | 0.7 | 0 | --- | --- | - | - | - | - | Uninfected | |
*dpi: days post inoculation.
**Liver sections were prepared from large liver samples collected during necropsy; liver injury score (adapted from [29]): 0 – without inflammation, 1 – 1 to 2 lymphohistiocytic inflammatory infiltrates/10 liver lobules, 2–3 to 5 inflammatory infiltrates/10 lobules, 3–6 to 10 inflammatory infiltrates/10 lobules, 4- >10 inflammatory infiltrates/10 lobules (adapted from [29]).
***DiaCheck anti-human HEV antibody assay that was modified with a goat anti-macaque secondary antibody.
#The maximum value obtained during the entire follow-up period is provided.
****Subclinical hepatitis was considered when the animals presented only laboratorial finds of infection, Biochemical hepatitis was considered using species-specific normal values and pre-inoculation values. Liver enzymes values were elevated at least twice above baseline in the context of an HEV infection. Histological hepatitis was considered when the animals presented lymphohistiocytic inflammatory infiltrates in liver biopsy.
Br: Brazilian, Ar: Argentinian, D: Dutch, EIA: Enzyme immunoassay, nt: not tested, (they did not produced enough saliva).
Biochemical and histopathological findings
Individual values for ALT, AST, GGT, and Tb did not vary significantly during the follow-up period. Exceptions included monkeys X15 (inoculated with the Br-swine virus) and F3 (inoculated with D-swine), of which serum levels for ALT, AST, and GGT were higher compared with their respective pre-inoculation values and the cynomolgus standard normal values (Table 2).
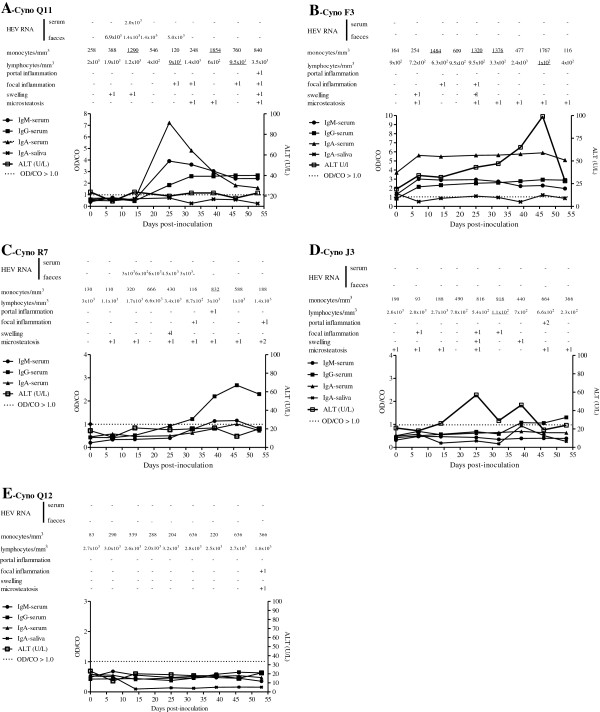
The histological analyses of the pre-inoculation liver sections were normal in all animals. After inoculation, the most prominent inflammatory reaction was observed for monkey X15 (Brazilian inoculum), which exhibited a mild portal inflammation with lymphocytes and histiocytes. Monkeys I3 and Q11 showed mild to moderate hyperplasia of the Ito cells from day 0 throughout the follow-up period. Cynomolgus monkeys that were inoculated with the Dutch swine HEV showed changes that were compatible with biochemical and histological HEV-related hepatitis, including mild inflammatory reactions with multifocal lobular lymphohistiocytic infiltrates (Figure 1B and Table 2). Slight to mild fatty changes and mild diffuse swelling of the hepatic cells were detected in all of the animals, even in the absence of an inflammatory response. Monkeys I3 and Q11 showed mild to moderate Ito cell hyperplasia from day 0 until the end of the experiment (Figure 1A and Table 2).
Figure 1.
Virological, inflammatory, biochemical, and antibody titre assessments from selected cynomolgus inoculated with HEV genotype 3. The data for monkeys Q11, F3, R7, J3, and Q12 are represented in panels A, B, C, D, and E, respectively. The values of antibody levels are reported as optical density/cutoff ratios, with a OD/CO > 1.0 considered positive in the DiaCheck anti-human HEV antibody assay that was modified for use with goat anti-macaque secondary antibodies. Underlined values are considered changed compared with baseline levels.
Detection of HEV antibodies in serum and saliva
Animals that were inoculated with the Br-swine inoculum (Figure 2C) exhibited specific antibody responses, with their IgG and IgM serum titres beginning to rise at 25 dpi. The exception was monkey I3, for which the only detectable antibody was salivary IgA.
Figure 2.
Liver sections from cynomolgus (A and B) and Brazilian HEV infected pig (C). A. Focal area of hepatocyte necrosis with polymorphic inflammation (histiocytes, lymphocytes, and neutrophils). Stained with hematoxylin and eosin; B. Detection of HEV antigen (marked in green) in the cytoplasm of hepatocytes and Kupffer cells at 67 dpi (cynomolgus G3); and C. Detection of HEV antigen (marked in red) in the cytoplasm of hepatocytes from a naturally infected pig obtained from a commercial pig farm in Brazil (inoculum).
All animals that were inoculated with the D-swine HEV showed IgM, IgG, and IgA anti-HEV titres in the serum samples that were collected during the follow-up period. Both IgA and IgM were transient and decreased after 46 and 55 dpi, respectively (Figure 1B). The IgG titre remained high until the end of the study. The highest salivary IgA titre was detected at 39 dpi. In monkey F3, the highest IgA (serum and saliva), IgM, and IgG titres were detected immediately following HEV inoculation. Focal necrosis (Figure 2A) and HEV Ag were detectable until 67 dpi (Figure 2B). Monkeys O1 and G3 seroconverted and had biochemical and histological hepatitis in association with transient viraemia and faecal shedding. In monkey F3, sudden rises in serum IgM, IgG, and IgA titres occurred at 7 dpi, suggesting a pre-exposure to HEV without detectable HEV antibodies in the pre-inoculation screening (Figure 1B).
Cynomolgus monkeys inoculated with biological samples from patients from Brazil and Argentina
Cynomolgus monkey inoculated with Brazilian human HEV
The animal that was inoculated with the Brazilian human virus (cynomolgus J3) exhibited rising levels of anti-HEV IgG antibodies in association with the development of inflammatory liver lesions, which was consistent with immunomediated liver injury (Table 2). Slight to mild fatty changes and mild diffuse swelling of the hepatic cells were found in the pre-inoculation liver sample in addition to those that were sampled throughout the experiment. At 46 and 53 dpi, this monkey showed mild portal infiltration, and at necropsy, the liver histopathology was scored as 1 using the severity assessment scoring system for inflammatory lesions (Table 2). Two slight variations in ALT levels were observed at 25 and 39 dpi. A change in GGT was detected at 25 dpi, and variations in TB were detected at 7, 14, and 32 dpi (Figure 1D).
Cynomolgus monkey inoculated with Argentinean human HEV
Cynomolgus monkey R7 was inoculated with the Argentinean human HEV sample (Ar-human) and developed biochemical and histological hepatitis with viral shedding. Mild to moderate hyperplasia of the Ito cells and mild portal infiltration were observed at 25 dpi and 7 dpi, respectively. Liver samples that were obtained at necropsy showed histological recovery (Table 2 and Figure 1C).
Negative controls
Both of the negative controls (monkeys Q12 and I2) developed non-significant biochemical alterations directly following the liver puncture procedures. Liver biopsies were scored as 0 using the severity assessment scoring system for inflammatory lesions (Figure 1E).
Peripheral blood cell counts
In general, the average number of platelets and red blood cells did not change over the course of the experiment. However, severe episodes of lymphopenia (< 200 cells/mm3) were observed throughout the follow-up period. The average lymphocyte count was reduced (P < 0.01) in comparison with the baseline value of lymphocytes in the peripheral blood (2,800 ± 1,000 cells/ml) (Figures 3A and 3B). Discrete monocytosis (> 900 cells/mm3) was also observed in the inoculated animals (Figures 3C and 3D).
Figure 3.

Haematological changes in cynomolgus monkeys experimentally infected with HEV. Lymphopenia was observed in the HEV-inoculated groups. An average lymphocyte was calculated at each of nine time points for all monkeys in each group (A) and in individuals (B). A trend toward monocytosis was observed in the inoculated groups. An average monocyte count for all HEV-inoculated monkeys in each group (C), and significant differences were observed in some individuals (D) (ANOVA, **P < 0.01, *P < 0.05).
Discussion
This article describes a successful, original approach for the experimental infection of cynomolgus macaques with HEV genotype 3 from different sources (human and swine) and different clinical manifestations. In their original hosts, these viruses were associated with varying clinical manifestations, ranging from none in the swine to fatal acute liver failure or acute hepatitis in the humans. HEV samples from different geographical regions, including Argentina, The Netherland and Brazil where hepatitis E is rare and/or under-diagnosed, were used in the present study. The intravenous route was employed for inoculation to ensure the best bioavailability of the inocula. Furthermore, our previous experience with the experimental transmission of enterically transmitted viral hepatitis in different non-human primates indicated that the only difference between oral and intravenous inoculation is the period of viral incubation, which is generally shorter for the intravenous route. Similar to the other experimental studies employing the cynomolgus monkey as a model for HEV infection, we found slight biochemical and histological alterations [31].
We observed that the first HEV-related event was viral shedding (at 5 to 21 dpi), as has been previously reported [32]. We assume that all of the animals presented with subclinical viral hepatitis independent of the source of the inoculum (swine or human) and the clinical presentation of the original host organism [22,31]. Even the animal that was inoculated with the Brazilian human HEV strain showed rising titres of anti-HEV IgG after 39 dpi. Indeed, there were no indications that the passive transfer of antibodies had occurred (Figure 1D). A late seroconversion to HEV (at 6–7 weeks pi) has previously been detected in cynomolgus monkeys that were inoculated intravenously with HEV from rabbits [33]. The absence of detectable HEV RNA in the faeces or sera may be explained by the presence of an IgG antibody response in the inoculum (human serum), which may have reduced the infectivity of the HEV particles, and/or by the lengthy time period that the samples had been stored. However, in both of these scenarios, the HEV peptides would have sensitised the macaque immune systems.
Cynomolgus monkey F3 presented with biochemical and histological hepatitis E (Table 2) without detectable viraemia or faecal shedding. However, early increases in antibody titres (IgM, IgA, and IgG) were observed concomitantly with slow and progressive ALT elevation. Apparently, the HEV infection was controlled in this monkey, accounting for the small number of focal inflammatory areas. A previous natural infection [34,35] or another HEV-like pathogen may explain this resistance to infection [36,37]. This result was intriguing because the main criterion for the inclusion of cynomolgus monkeys in our experimental protocol was the absence of anti-HEV IgG in the pre-inoculation serum. All of the animals that were provided by the animal breeding centre had been screened twice for HEV antibodies using two different assays. Sixteen out of the 76 captive cynomolgus monkeys were reactive to anti-HEV IgG in this screening and were therefore excluded from this study. All of the non-reactive animals were considered to be naive to HEV infection. Other authors have assumed that HEV or an HEV-related agent circulates naturally among Indian macaques [34,35,38,39]. A previous natural exposure may prevent a new (experimental) HEV infection [40,41]. In contrast, cynomolgus monkey I3 (Table 2) showed lymphopenia, prolonged viraemia (starting at 39 dpi), and faecal shedding (starting at 19 dpi) without seroconversion until the end of the experiment and possibly beyond that period. Such a pattern of prolonged viraemia and viral elimination without seroconversion or liver enzyme elevation has been described for HEV-infected, immunocompromised individuals [42-44], haemodialysis patients [45], and an immature neonate [44]. The protective roles of specific antibodies in controlling HEV infection have been confirmed in non-human primate studies [40,46-48] for both naturally acquired and experimentally induced infections [38,48,49] and in convalescent human patients [50]. The presence of activated lymphocytes during the resolution of hepatitis E infection has been demonstrated in acute hepatitis [51], acute liver failure [52], and acute hepatitis during pregnancy [53].
Interestingly, all of the infected monkeys showed severe lymphopenia and discrete monocytosis, coinciding with elevations in ALT and antibody titres. This study describes, for the first time, the haematological disorders that are associated with HEV infection, thus providing an additional parameter for future experimental protocols. In addition, we observed a progressive reduction in the average neutrophil counts of the inoculated animals compared with their baseline levels (data not shown). Other uncommon extra-hepatic manifestations, such as thrombocytopenia, anaemia [54], and neurological symptoms, have been previously described in HEV-infected patients [55]. Monocytosis has also been observed, typically in animals that have been inoculated with swine HEV. However, the restricted number of animals and inocula and the large individual variability among haematological values do not allow for precise conclusions to be drawn. The lymphohistiocytic hepatitis that was detected in our study has also been described in a rodent model of infection with HEV genotype 4 [56]. The elevated presence of infiltrated lymphocytes in the portal area and the focal inflammation that was detected in our study may be consequences of the intra-hepatic flow of lymphocytes, which was observed during this study for CD8+ cells in the cynomolgus monkeys with subclinical hepatitis E (data not shown). The same findings have also been reported in transplant patients with chronic hepatitis E [57] and in the liver parenchyma after HEV-induced acute liver failure [56]. Other authors have also observed lymphopenia in patients with hepatitis-virus-associated aplastic anaemia (HAA), suggesting that HAA may be influenced by the immune-mediated destruction of bone marrow [58]. Several viruses are considered to be triggers for autoimmunity and overt autoimmune disease. The virus-specific evasion mechanism, which is termed molecular mimicry, may serve as an accelerating factor for hepatic and extra-hepatic pathogenesis [59]. Further immunological approaches using peripheral blood cells and their precursors in bone marrow samples will contribute to understand the haematological manifestations of hepatitis E infection.
With the goal of improving HEV diagnoses, the serum titres for the IgA and IgM immunoglobulins were measured and showed similar profiles, with temporary increases being observed in most of the animals that were considered to be HEV-infected. Although the collection of salivary samples is less invasive than that of blood, the irregularities and fluctuations in the specific IgA levels in the saliva during the follow-up period indicate that this marker cannot replace classical testing that uses serum antibodies as markers for acute infection in routine diagnostics.
Our study indicate that HEV is capable of inter-species infection, which has been corroborated by other studies that have been conducted with HEV genotype 3 [21,60]. Because autochthonous hepatitis E cases have been associated with genotype 3 isolates, the zoonotic aspect of HEV infection should be considered in non-endemic, developing countries, such as Brazil and Argentina. Additional serological, molecular, and epidemiological studies will provide a better understanding of the dynamics and profile of this disease in Latin America.
Conclusions
Finally, this work confirmed the ability of HEV to cross the species barrier for both the swine (Brazilian and Dutch) and human (Argentinean) strains, thus reinforcing the zoonotic risk of hepatitis E in South America. Cynomolgus monkeys that were infected with HEV genotype 3, obtained from different clinical presentations, developed subclinical hepatitis that was associated with haematological changes.
Abbreviations
HEV: Hepatitis E virus; CEUA: Ethics committee for animal use; HAV: Hepatitis A virus; CONCEA: The national council for control of animal experimentation; SIV: Simian immunodeficiency virus; SRV/D: Simian type D retrovirus; HAA: Hepatitis-virus-associated aplastic anaemia; CECAL: Animal breeding centre; EDTA: Ethylenediaminetetraacetic acid; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; GGT: Gamma-glutamyl transferase; Tb: Total bilirubin.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MAP conceived the idea, managed the study, participated in the analysis of data and the preparation of the manuscript; LGC and DRLS participated in the study design and performed the experiments; WHMVP, JEG, and MSM provided the inocula; VSP and LGC performed the molecular biology tests; RSM and MP-M performed the histopathological and confocal analysis, respectively; LMP participated in the immunofluorescence analysis; JM: performed the serological tests; OGC realized the statistical analysis; MAP and JMO wrote the paper. All authors read and approved the final manuscript.
Authors’ information
Please use the form below to submit correspondence to the authors or contact them at the following address.
Marcelo Alves Pinto, Laboratório de Desenvolvimento Tecnológico em Virologia, Instituto Oswaldo Cruz, Fundação Oswaldo Cruz, Ministério do Saúde, Governo Federal, Brasil. Pavilhão Helio e Peggy Pereira sala B221, Avenida Brasil 4365, Manguinhos, Rio de Janeiro, CEP 21045–900.
LM L, is fellowship of CNPq.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Lilian G de Carvalho, Email: liliangc2@yahoo.com.br.
Renato S Marchevsky, Email: march@bio.fiocruz.br.
Debora RL dos Santos, Email: deborabio@gmail.com.
Jaqueline M de Oliveira, Email: jackie@ioc.fiocruz.br.
Vanessa S de Paula, Email: vdepaula@ioc.fiocruz.br.
Leilane M Lopes, Email: leilaneb@ioc.fiocruz.br.
Wilhelmus HM Van der Poel, Email: Wim.vanderPoel@wur.nl.
Jorge E González, Email: jegonzalez@anlis.gov.ar.
Maria S Munné, Email: smunne@anlis.gov.ar.
Julio Moran, Email: julio@moran.ch.
Ana Carolina R A Cajaraville, Email: anacarolina.reis@bio.fiocruz.br.
Marcelo Pelajo-Machado, Email: mpelajo@ioc.fiocruz.br.
Oswaldo G Cruz, Email: ogcruz@gmail.com.
Marcelo A Pinto, Email: marcelop@ioc.fiocruz.br.
Acknowledgements
We would like to thank the staff of the Centro de Experimentação Animal at the Instituto Oswaldo Cruz/Fiocruz, especially Felipe de Carvalho Resende (DVM) for his animal care, as well as the staff of the Confocal Microscopy Technological Platform/Fiocruz, the Clinical Laboratory of Laboratory Animals of the Technological Platforms/Fiocruz, especially Simone Ramos for haematological analysis, and the Animal Breeding Centre, CECAL/Fiocruz. This study was sponsored by Conselho Nacional de Desenvolvimento Cientifico e Tecnológico-CNPq (grant numbers 30 8951/2010-7 and 57832/2008-3 to MAP), Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro - FAPERJ (grant number 111.145/2011 to MAP) and Laboratório de Desenvolvimento Tecnológico em Virologia, Instituto Oswaldo Cruz/Fiocruz grants to MAP (POM-IOC/Fiocruz).
References
- Mushahwar IK. Hepatitis E virus: molecular virology, clinical features, diagnosis, transmission, epidemiology, and prevention. J Med Virol. 2008;80:646–658. doi: 10.1002/jmv.21116. [DOI] [PubMed] [Google Scholar]
- Kumar S, Subhadra S, Singh B, Panda BK. Hepatitis E virus: the current scenario. Int J Infect Dis. 2013;17:e228–e233. doi: 10.1016/j.ijid.2012.11.026. [DOI] [PubMed] [Google Scholar]
- Echevarria JM, Gonzalez JE, Lewis-Ximenez LL, Dos Santos DR, Munne MS, Pinto MA, Pujol FH, Rodriguez-Lay LA. Hepatitis E virus infection in Latin America: a review. J Med Virol. 2013;85:1037–1045. doi: 10.1002/jmv.23526. [DOI] [PubMed] [Google Scholar]
- Silva SM, Oliveira JM, Vitral CL, Vieira Kde A, Pinto MA, Souto FJ. Prevalence of hepatitis E virus antibodies in individuals exposed to swine in Mato Grosso, Brazil. Mem Inst Oswaldo Cruz. 2012;107:338–341. doi: 10.1590/S0074-02762012000300007. [DOI] [PubMed] [Google Scholar]
- Vitral CL, Pinto MA, Lewis-Ximenez LL, Khudyakov YE, dos Santos DR, Gaspar AM. Serological evidence of hepatitis E virus infection in different animal species from the Southeast of Brazil. Mem Inst Oswaldo Cruz. 2005;100:117–122. doi: 10.1590/S0074-02762005000200003. [DOI] [PubMed] [Google Scholar]
- Bortoliero AL, Bonametti AM, Morimoto HK, Matsuo T, Reiche EM. Seroprevalence for hepatitis E virus (HEV) infection among volunteer blood donors of the regional blood bank of Londrina, State of Parana, Brazil. Rev Inst Med Trop Sao Paulo. 2006;48:87–92. doi: 10.1590/S0036-46652006000200006. [DOI] [PubMed] [Google Scholar]
- Santos DC, Souto FJ, Santos DR, Vitral CL, Gaspar AM. Seroepidemiological markers of enterically transmitted viral hepatitis A and E in individuals living in a community located in the North Area of Rio de Janeiro, RJ, Brazil. Mem Inst Oswaldo Cruz. 2002;97:637–640. doi: 10.1590/S0074-02762002000500007. [DOI] [PubMed] [Google Scholar]
- dos Santos DR, de Paula VS, de Oliveira JM, Marchevsky RS, Pinto MA. Hepatitis E virus in swine and effluent samples from slaughterhouses in Brazil. Vet Microbiol. 2011;149:236–241. doi: 10.1016/j.vetmic.2010.10.024. [DOI] [PubMed] [Google Scholar]
- de Souza AJ, Gomes-Gouvea MS, Soares Mdo C, Pinho JR, Malheiros AP, Carneiro LA, Dos-Santos DR, Pereira WL. HEV infection in swine from Eastern Brazilian Amazon: evidence of co-infection by different subtypes. Comp Immunol Microbiol Infect Dis. 2012;35:477–485. doi: 10.1016/j.cimid.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Gardinali NR, Barry AF, da Silva PF, de Souza C, Alfieri AF, Alfieri AA. Molecular detection and characterization of hepatitis E virus in naturally infected pigs from Brazilian herds. Res Vet Sci. 2012;93:1515–1519. doi: 10.1016/j.rvsc.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Bradley DW, Krawczynski K, Cook EH Jr, McCaustland KA, Humphrey CD, Spelbring JE, Myint H, Maynard JE. Enterically transmitted non-A, non-B hepatitis: serial passage of disease in cynomolgus macaques and tamarins and recovery of disease-associated 27- to 34-nm viruslike particles. Proc Natl Acad Sci U S A. 1987;84:6277–6281. doi: 10.1073/pnas.84.17.6277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta H, Joshi YK, Varma A, Shenoy S, Sriramchari S, Iyenger B, Tandon BN. Transmission of enteric non-A, non-B hepatitis virus in Macaca mulatta monkeys by intraportal route: subsequent passages of HEV virus. J Gastroenterol Hepatol. 1990;5:608–615. doi: 10.1111/j.1440-1746.1990.tb01114.x. [DOI] [PubMed] [Google Scholar]
- Longer CF, Denny SL, Caudill JD, Miele TA, Asher LV, Myint KS, Huang CC, Engler WF, LeDuc JW, Binn LN, Ticehurst JR. Experimental hepatitis E: pathogenesis in cynomolgus macaques (Macaca fascicularis) J Infect Dis. 1993;168:602–609. doi: 10.1093/infdis/168.3.602. [DOI] [PubMed] [Google Scholar]
- Tsarev SA, Emerson SU, Tsareva TS, Yarbough PO, Lewis M, Govindarajan S, Reyes GR, Shapiro M, Purcell RH. Variation in course of hepatitis E in experimentally infected cynomolgus monkeys. J Infect Dis. 1993;167:1302–1306. doi: 10.1093/infdis/167.6.1302. [DOI] [PubMed] [Google Scholar]
- McCaustland KA, Krawczynski K, Ebert JW, Balayan MS, Andjaparidze AG, Spelbring JE, Cook EH, Humphrey C, Yarbough PO, Favorov MO, Carson D, Bradley DW, Robertson BH. Hepatitis E virus infection in chimpanzees: a retrospective analysis. Arch Virol. 2000;145:1909–1918. doi: 10.1007/s007050070065. [DOI] [PubMed] [Google Scholar]
- Ji Y, Zhu Y, Liang J, Wei X, Yang X, Wang L, Li L, Chang Y, Tang R, Zhuang H. Swine hepatitis E virus in rural southern China: genetic characterization and experimental infection in rhesus monkeys (Macaca mulatta) J Gastroenterol. 2008;43:565–570. doi: 10.1007/s00535-008-2196-3. [DOI] [PubMed] [Google Scholar]
- Pillot J, Turkoglu S, Dubreuil P, Cosson A, Lemaigre G, Meng J, Lazizi Y. Cross-reactive immunity against different strains of the hepatitis E virus transferable by simian and human sera. C R Acad Sci III. 1995;318:1059–1064. [PubMed] [Google Scholar]
- Meng J, Pillot J, Dai X, Fields HA, Khudyakov YE. Neutralization of different geographic strains of the hepatitis E virus with anti-hepatitis E virus-positive serum samples obtained from different sources. Virology. 1998;249:316–324. doi: 10.1006/viro.1998.9346. [DOI] [PubMed] [Google Scholar]
- Sanford BJ, Dryman BA, Huang YW, Feagins AR, Leroith T, Meng XJ. Prior infection of pigs with a genotype 3 swine hepatitis E virus (HEV) protects against subsequent challenges with homologous and heterologous genotypes 3 and 4 human HEV. Virus Res. 2011;159:17–22. doi: 10.1016/j.virusres.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouwknegt M, Lodder-Verschoor F, van der Poel WH, Rutjes SA, de Roda Husman AM. Hepatitis E virus RNA in commercial porcine livers in The Netherlands. J Food Prot. 2007;70:2889–2895. doi: 10.4315/0362-028x-70.12.2889. [DOI] [PubMed] [Google Scholar]
- Meng XJ, Halbur PG, Shapiro MS, Govindarajan S, Bruna JD, Mushahwar IK, Purcell RH, Emerson SU. Genetic and experimental evidence for cross-species infection by swine hepatitis E virus. J Virol. 1998;72:9714–9721. doi: 10.1128/jvi.72.12.9714-9721.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aggarwal R, Kamili S, Spelbring J, Krawczynski K. Experimental studies on subclinical hepatitis E virus infection in cynomolgus macaques. J Infect Dis. 2001;184:1380–1385. doi: 10.1086/324376. [DOI] [PubMed] [Google Scholar]
- Bouwknegt M, Frankena K, Rutjes SA, Wellenberg GJ, de Roda Husman AM, van der Poel WH, de Jong MC. Estimation of hepatitis E virus transmission among pigs due to contact-exposure. Vet Res. 2008;39:40. doi: 10.1051/vetres:2008017. [DOI] [PubMed] [Google Scholar]
- Agrawal S, Gupta D, Panda SK. The 3′ end of hepatitis E virus (HEV) genome binds specifically to the viral RNA-dependent RNA polymerase (RdRp) Virology. 2001;282:87–101. doi: 10.1006/viro.2000.0819. [DOI] [PubMed] [Google Scholar]
- Dalton HR, Hunter JG, Bendall RP. Hepatitis e. Curr Opin Infect Dis. 2013;26:471–478. doi: 10.1097/01.qco.0000433308.83029.97. [DOI] [PubMed] [Google Scholar]
- Lopes Dos Santos DR, Lewis-Ximenez LL, da Silva MF, de Sousa PS, Gaspar AM, Pinto MA. First report of a human autochthonous hepatitis E virus infection in Brazil. J Clin Virol. 2010;47:276–279. doi: 10.1016/j.jcv.2009.12.021. [DOI] [PubMed] [Google Scholar]
- Jothikumar N, Cromeans TL, Robertson BH, Meng XJ, Hill VR. A broadly reactive one-step real-time RT-PCR assay for rapid and sensitive detection of hepatitis E virus. J Virol Methods. 2006;131:65–71. doi: 10.1016/j.jviromet.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Pinto MA, Marchevsky RS. Serial opened biopsies applied in nonhuman primate model to study the pathogenesis of hepatitis A virus. Virus Reviews and Research. 2001;6:26–33. [Google Scholar]
- Halbur PG, Kasorndorkbua C, Gilbert C, Guenette D, Potters MB, Purcell RH, Emerson SU, Toth TE, Meng XJ. Comparative pathogenesis of infection of pigs with hepatitis E viruses recovered from a pig and a human. J Clin Microbiol. 2001;39:918–923. doi: 10.1128/JCM.39.3.918-923.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The R Project for Statistical Computing. [ http://www.r-project.org]
- Erker JC, Desai SM, Schlauder GG, Dawson GJ, Mushahwar IK. A hepatitis E virus variant from the United States: molecular characterization and transmission in cynomolgus macaques. J Gen Virol. 1999;80(Pt 3):681–690. doi: 10.1099/0022-1317-80-3-681. [DOI] [PubMed] [Google Scholar]
- van Cuyck-Gandre H, Cockman-Thomas R, Caudill JD, Asher LS, Armstrong KL, Hauroeder B, Clements NJ, Binn LN, Longer CF. Experimental African HEV infection in cynomolgus macaques (Macaca fascicularis) J Med Virol. 1998;55:197–202. doi: 10.1002/(SICI)1096-9071(199807)55:3<197::AID-JMV3>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Liu P, Bu QN, Wang L, Han J, Du RJ, Lei YX, Ouyang YQ, Li J, Zhu YH, Lu FM, Zhuang H. Transmission of hepatitis E virus from rabbits to cynomolgus macaques. Emerg Infect Dis. 2013;19:559–565. doi: 10.3201/eid1904.120827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirano M, Ding X, Tran HT, Li TC, Takeda N, Sata T, Nakamura S, Abe K. Prevalence of antibody against hepatitis E virus in various species of non-human primates: evidence of widespread infection in Japanese monkeys (Macaca fuscata) Jpn J Infect Dis. 2003;56:8–11. [PubMed] [Google Scholar]
- Huang F, Yu W, Hua X, Jing S, Zeng W, He Z. Seroepidemiology and molecular characterization of hepatitis E virus in Macaca Mulatta from a Village in Yunnan, China, where Infection with this virus is endemic. Hepat Mon. 2011;11:745–749. doi: 10.5812/kowsar.1735143X.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto H, Takahashi M, Nishizawa T, Usui R, Kobayashi E. Presence of antibodies to hepatitis E virus in Japanese pet cats. Infection. 2004;32:57–58. doi: 10.1007/s15010-004-3078-0. [DOI] [PubMed] [Google Scholar]
- Liu J, Zhang W, Shen Q, Yang S, Huang F, Li P, Guo X, Yang Z, Cui L, Zhu J, Hua X. Prevalence of antibody to hepatitis E virus among pet dogs in the Jiang-Zhe area of China. Scand J Infect Dis. 2009;41:291–295. doi: 10.1080/00365540902767031. [DOI] [PubMed] [Google Scholar]
- Arankalle VA, Chadha MS, Banerjee K, Srinivasan MA, Chobe LP. Hepatitis E virus infection in pregnant rhesus monkeys. Indian J Med Res. 1993;97:4–8. [PubMed] [Google Scholar]
- Nakamura S, Tsuchiya H, Okahara N, Nakagawa T, Ohara N, Yamamoto H, Li TC, Takeda N, Ogasawara K, Torii R. Epidemiology of hepatitis E virus in indoor-captive cynomolgus monkey colony. J Vet Med Sci. 2011;74:279–283. doi: 10.1292/jvms.11-0394. [DOI] [PubMed] [Google Scholar]
- Arankalle VA, Chadha MS, Chobe LP, Nair R, Banerjee K. Cross-challenge studies in rhesus monkeys employing different Indian isolates of hepatitis E virus. J Med Virol. 1995;46:358–363. doi: 10.1002/jmv.1890460411. [DOI] [PubMed] [Google Scholar]
- Tsarev SA, Tsareva TS, Emerson SU, Rippy MK, Zack P, Shapiro M, Purcell RH. Experimental hepatitis E in pregnant rhesus monkeys: failure to transmit hepatitis E virus (HEV) to offspring and evidence of naturally acquired antibodies to HEV. J Infect Dis. 1995;172:31–37. doi: 10.1093/infdis/172.1.31. [DOI] [PubMed] [Google Scholar]
- Pischke S, Suneetha PV, Baechlein C, Barg-Hock H, Heim A, Kamar N, Schlue J, Strassburg CP, Lehner F, Raupach R, Bremer B, Magerstedt P, Cornberg M, Seehusen F, Baumgaertner W, Klempnauer J, Izopet J, Manns MP, Grummer B, Wedemeyer H. Hepatitis E virus infection as a cause of graft hepatitis in liver transplant recipients. Liver Transpl. 2009;16:74–82. doi: 10.1002/lt.21958. [DOI] [PubMed] [Google Scholar]
- le Coutre P, Meisel H, Hofmann J, Rocken C, Vuong GL, Neuburger S, Hemmati PG, Dorken B, Arnold R. Reactivation of hepatitis E infection in a patient with acute lymphoblastic leukaemia after allogeneic stem cell transplantation. Gut. 2009;58:699–702. doi: 10.1136/gut.2008.165571. [DOI] [PubMed] [Google Scholar]
- Khuroo MS, Kamili S. Clinical course and duration of viremia in vertically transmitted hepatitis E virus (HEV) infection in babies born to HEV-infected mothers. J Viral Hepat. 2009;16:519–523. doi: 10.1111/j.1365-2893.2009.01101.x. [DOI] [PubMed] [Google Scholar]
- Zekavat OR, Makarem A, Karami MY, Amanat A, Mohandes M, Habibagahi M. Serological investigation for hepatitis E virus infection in the patients with chronic maintenance hemodialysis from southwest of Iran. Asian J Transfus Sci. 2013;7:21–25. doi: 10.4103/0973-6247.106724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsarev SA, Tsareva TS, Emerson SU, Govindarajan S, Shapiro M, Gerin JL, Purcell RH. Successful passive and active immunization of cynomolgus monkeys against hepatitis E. Proc Natl Acad Sci U S A. 1994;91:10198–10202. doi: 10.1073/pnas.91.21.10198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arankalle VA, Chadha MS, Chobe LP. Long-term serological follow up and cross-challenge studies in rhesus monkeys experimentally infected with hepatitis E virus. J Hepatol. 1999;30:199–204. doi: 10.1016/S0168-8278(99)80062-2. [DOI] [PubMed] [Google Scholar]
- Arankalle VA, Goverdhan MK, Banerjee K. Antibodies against hepatitis E virus in old world monkeys. J Viral Hepat. 1994;1:125–129. doi: 10.1111/j.1365-2893.1994.tb00111.x. [DOI] [PubMed] [Google Scholar]
- Kamili S, Spelbring J, Carson D, Krawczynski K. Protective efficacy of hepatitis E virus DNA vaccine administered by gene gun in the cynomolgus macaque model of infection. J Infect Dis. 2004;189:258–264. doi: 10.1086/380801. [DOI] [PubMed] [Google Scholar]
- Bryan JP, Tsarev SA, Iqbal M, Ticehurst J, Emerson S, Ahmed A, Duncan J, Rafiqui AR, Malik IA, Purcell RH, Legters LJ. Epidemic hepatitis E in Pakistan: patterns of serologic response and evidence that antibody to hepatitis E virus protects against disease. J Infect Dis. 1994;170:517–521. doi: 10.1093/infdis/170.3.517. [DOI] [PubMed] [Google Scholar]
- TrehanPati N, Sukriti S, Geffers R, Hissar S, Riese P, Toepfer T, Guzman CA, Sarin SK. Gene expression profiles of T cells from hepatitis E virus infected patients in acute and resolving phase. J Clin Immunol. 2011;31:498–508. doi: 10.1007/s10875-010-9506-2. [DOI] [PubMed] [Google Scholar]
- Pfefferle S, Frickmann H, Gabriel M, Schmitz N, Gunther S, Schmidt-Chanasit J. Fatal course of an autochthonous hepatitis E virus infection in a patient with leukemia in Germany. Infection. 2012;40:451–454. doi: 10.1007/s15010-011-0220-7. [DOI] [PubMed] [Google Scholar]
- Prabhu SB, Gupta P, Durgapal H, Rath S, Gupta SD, Acharya SK, Panda SK. Study of cellular immune response against hepatitis E virus (HEV) J Viral Hepat. 2011;18:587–594. doi: 10.1111/j.1365-2893.2010.01338.x. [DOI] [PubMed] [Google Scholar]
- Amarapurkar DN, Amarapurkar AD. Extrahepatic manifestations of viral hepatitis. Ann Hepatol. 2002;1:192–195. [PubMed] [Google Scholar]
- Cheung MC, Maguire J, Carey I, Wendon J, Agarwal K. Review of the neurological manifestations of hepatitis E infection. Ann Hepatol. 2012;11:618–622. [PubMed] [Google Scholar]
- Li L, Zhu Y, Fu H, Wei X, Wang L, Liang J, Ji Y, Tang R, Zhuang H. Full-genome nucleotide sequence and analysis of a Chinese swine hepatitis E virus isolate of genotype 4 identified in the Guangxi Zhuang autonomous region: evidence of zoonotic risk from swine to human in South China. Liver Int. 2009;29:1230–1240. doi: 10.1111/j.1478-3231.2009.02012.x. [DOI] [PubMed] [Google Scholar]
- Kamar N, Selves J, Mansuy JM, Ouezzani L, Peron JM, Guitard J, Cointault O, Esposito L, Abravanel F, Danjoux M, Durand D, Vinel JP, Izopet J, Rostaing L. Hepatitis E virus and chronic hepatitis in organ-transplant recipients. N Engl J Med. 2008;358:811–817. doi: 10.1056/NEJMoa0706992. [DOI] [PubMed] [Google Scholar]
- Ikeda T, Morimoto A, Nakamura S, Yokoyama K, Hayase T, Oh Y, Kashii Y, Yotsumoto S, Okamoto H, YM M. A marked decrease in CD4-positive lymphocytes at the onset of hepatitis in a patient with hepatitis-associated aplastic anemia. J Pediatr Hematol Oncol. 2012;34:375–377. doi: 10.1097/MPH.0b013e31822bf699. [DOI] [PubMed] [Google Scholar]
- Mizukawa Y, Shiohara T. Virus-induced immune dysregulation as a triggering factor for the development of drug rashes and autoimmune diseases: with emphasis on EB virus, human herpesvirus 6 and hepatitis C virus. J Dermatol Sci. 2000;22:169–180. doi: 10.1016/S0923-1811(99)00083-3. [DOI] [PubMed] [Google Scholar]
- Meng XJ. Swine hepatitis E virus: cross-species infection and risk in xenotransplantation. Curr Top Microbiol Immunol. 2003;278:185–216. doi: 10.1007/978-3-642-55541-1_7. [DOI] [PubMed] [Google Scholar]