Owing to impaired interleukin 17 immunity, interleukin 12βR1 (IL-12βR1)–deficient patients have mucocutaneous candidiasis, which is usually recurrent or persistent in spite of antifungal treatment. Candidiasis may be the first clinical manifestation in IL-12βR1–deficient patients.
Keywords: Interleukin-12 receptor β1 chain, primary immunodeficiency, Candida, Mycobacterium, Salmonella
Abstract
Background. Interleukin 12Rβ1 (IL-12Rβ1)–deficient patients are prone to clinical disease caused by mycobacteria, Salmonella, and other intramacrophagic pathogens, probably because of impaired interleukin 12–dependent interferon γ production. About 25% of patients also display mucocutaneous candidiasis, probably owing to impaired interleukin 23–dependent interleukin 17 immunity. The clinical features and outcome of candidiasis in these patients have not been described before, to our knowledge. We report here the clinical signs of candidiasis in 35 patients with IL-12Rβ1 deficiency.
Results. Most (n = 71) of the 76 episodes of candidiasis were mucocutaneous. Isolated oropharyngeal candidiasis (OPC) was the most common presentation (59 episodes, 34 patients) and was recurrent or persistent in 26 patients. Esophageal candidiasis (n = 7) was associated with proven OPC in 2 episodes, and cutaneous candidiasis (n = 2) with OPC in 1 patient, whereas isolated vulvovaginal candidiasis (VVC; n = 3) was not. Five episodes of proven invasive candidiasis were documented in 4 patients; 1 of these episodes was community acquired in the absence of any other comorbid condition. The first episode of candidiasis occurred earlier in life (median age±standard deviation, 1.5 ± 7.87 years) than infections with environmental mycobacteria (4.29 ± 11.9 years), Mycobacterium tuberculosis (4 ± 3.12 years), or Salmonella species (4.58 ± 4.17 years) or other rare infections (3 ± 11.67 years). Candidiasis was the first documented infection in 19 of the 35 patients, despite the vaccination of 10 of these 19 patients with live bacille Calmette-Guérin.
Conclusions. Patients who are deficient in IL-12Rβ1 may have candidiasis, usually mucocutaneous, which is frequently recurrent or persistent. Candidiasis may be the first clinical manifestation in these patients.
Mendelian susceptibility to mycobacterial diseases (MSMD) is characterized by a selective predisposition to clinical disease caused by mycobacteria and Salmonella [1]. Nine disease-causing genes have been described, including 3 genes controlling the response to interferon (IFN) γ (IFNGR1, IFNGR2, STAT1), 4 involved in IFN-γ production (IL12B, IL12RB1, NEMO, ISG15) [1, 2], 1 involved in the IFN-γ–dependent induction of interleukin 12 (IL-12; IRF8) [3], and another gene controlling the macrophage respiratory burst, which can be triggered by IFN-γ (CYBB) [4].
Interleukin 12Rβ1 (IL-12Rβ1) deficiency is the most common genetic cause of MSMD [5, 6], with 156 patients reported to date (Supplementary Table 1). IL12RB1 encodes the first chain of the IL-12 (IL-12Rβ1) and interleukin 23 (IL-23) receptors. Interleukin 12 is an important cytokine for the development of IFN-γ–producing T cells and for IFN-γ production [7]. Conversely, IL-23 is important for the expansion and maintenance of the interleukin 17 (IL-17)–producing T-cell population [8, 9]. Interleukin 12Rβ1 deficiency is the genetic cause of MSMD for which the most infections other than mycobacteriosis has been reported [1]. Salmonellosis is very common, as in IL-12p40 deficiency, but much more so than in other genetic etiologies of MSMD [1, 10, 11]. However, other infections due to intramacrophagic pathogens have also been reported (Supplementary Table 1) [1, 6]. The impairment of IL-23 immunity, alone or together with IL-12 immunity, may contribute to this relatively broad infectious phenotype [1, 9].
We recently noted that about 25% of IL-12Rβ1–deficient patients also have mild forms of chronic mucocutaneous candidiasis (CMC) [6]. This is consistent with the role of IL-23 in the maintenance of IL-17–producing T cells and the low proportions of IL-17 T cells in the patients with IL-12Rβ1 deficiency studied [9]. Indeed, patients with disorders associated with impaired IL-17–mediated immunity have CMC, including patients with autoimmune polyendocrinopathy syndrome type I (APS-I), autosomal dominant (AD) hyper–immunoglobulin E syndrome (AD-HIES) due to dominant-negative mutations of STAT3, or more rarely those with caspase recruitment domain–containing protein 9 (CARD9) deficiency [12–17]. Isolated CMC, also known as CMC disease (CMCD), has been shown to result from AD IL-17F deficiency, autosomal recessive deficiency of IL-17RA (the receptor for both IL-17A and IL-17F), from NF-κB activator 1 (ACT1) deficiency, or from an AD gain of STAT1 activity [18–22]. Surprisingly, the clinical features of candidiasis have never been studied in series of patients with these inborn errors of immunity. We report here the clinical features of candidiasis in 35 patients with IL-12Rβ1 deficiency.
PATIENTS AND METHODS
Patients
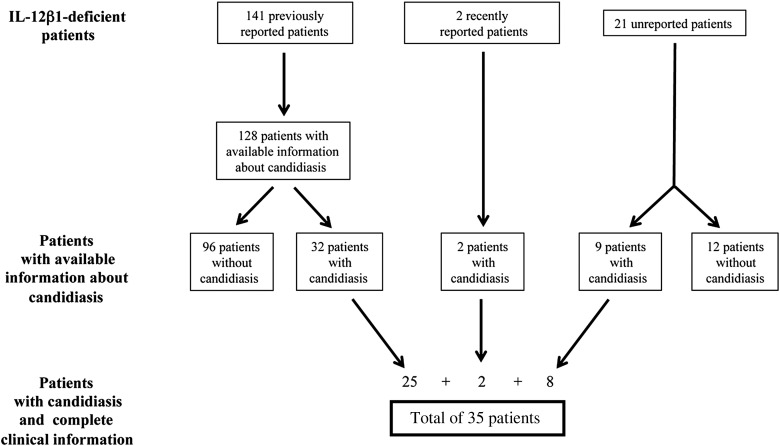
Candidiasis was reported in 32 (25%) of the 128 IL-12Rβ1–deficient patients previously reported (of a total of 141) for whom information about Candida infections was available [6]. Candidiasis was also documented in 2 recently reported IL-12Rβ1–deficient patients [23, 24] and in 9 of 21 with recent diagnoses who were not previously reported. A questionnaire was sent to physicians caring for the 34 previously reported IL-12Rβ1–deficient patients with candidiasis [6, 23, 24] and the 9 with recent diagnoses who were previously unreported. Detailed information about candidiasis was obtained for 35 patients (Figure 1).
Figure 1.
Selection process for interleukin (IL)-12Rβ1–deficient patients with or without candidiasis and questionnaires with complete clinical information received. The occurrence of candidiasis was included in a complete questionnaire sent to the physicians caring for the 141 patients previously reported [6]; no data about the occurrence of candidiasis were available in 13 of these patients. Candidiasis was also documented in 2 patients reported in 2011 and 2012 [23, 24]; specific questionnaires about candidiasis were sent to the physicians caring for these 2 patients. For 21 previously unreported patients, before questionnaires were sent, physicians caring for the patients were consulted about the presence of candidiasis. Questionnaires were sent only for the 9 patients with documented candidiasis, for whom 8 questionnaires with complete clinical information were received.
The questionnaire included items relating to demographic data, IL12RB1 mutations, and infectious diseases. For candidiasis, we recorded the date and patient age at the time of the episode, the Candida species identified, sites involved, whether the episode was community-acquired or hospital-acquired candidiasis, clinical signs and duration before treatment, use of antibiotics during or before candidiasis, use of immunosuppresants, polymorphonuclear granulocyte counts, the presence of comorbid conditions and age at onset of these conditions, clinical features for each episode, antifungal treatment and duration, and time to clinical remission. Informed consent was obtained from each patient or the patient's family. The protocol was approved by the local ethics committees of the various institutions involved.
The diagnosis of esophageal candidiasis was based on the demonstration of candidiasis by biopsy culture and/or esophagoscopy. The diagnosis of invasive candidiasis was based on the cultivation of Candida from normally sterile clinical fluids or biopsy specimens. We considered that an episode of candidiasis was a relapse of a previous infection when the infection reappeared at the same site <1 month after treatment withdrawal. Patients were considered to have recurrent candidiasis if they had had ≥3 Candida infections and the second episode or subsequent episodes occurred ≥1 month after withdrawal of treatment for a previous episode. Recurrent VVC was defined as ≥4 episodes of VVC in 1 year. Persistent candidiasis was defined as the presence of repeated episodes of candidiasis despite treatment resulting in rarely observed candidiasis-free periods. For statistical purposes, patients with persistent or recurrent candidiasis were analyzed together.
Statistical Analysis
Quantitative variables are presented as arithmetic means ± standard deviations, except for the age at onset of infectious diseases, given as medians ± standard deviations. Frequency distributions were compared using χ2 tests or Fisher exact tests, as necessary, and odds ratios with 95% confidence intervals were calculated. Statistical analyses were performed using the LIFETEST and PHREG procedures of SAS software version 9.2 (SAS, Cary, NC, USA).
RESULTS
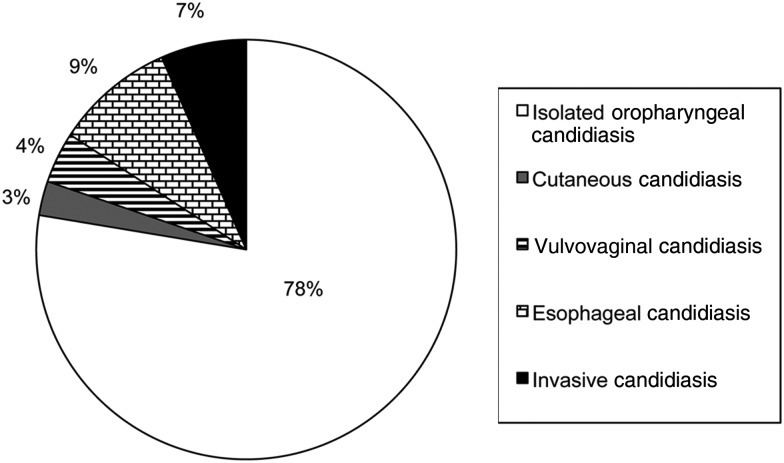
We studied 35 IL-12Rβ1–deficient patients who had candidiasis. The clinical and genetic features of the patients are summarized in Table 1. There were 76 documented episodes of candidiasis, and the epidemiological characteristics of the episodes are shown in Table 2. Most episodes (n = 53) corresponded to documented infections in patients with recurrent or persistent candidiasis, and 23 episodes corresponded to documented infections that did not recur. Candida infections were documented at various anatomic sites (Figure 2). Most episodes (n = 59; 78%) involved only the oropharyngeal cavity, but esophageal (n = 7), cutaneous (n = 2), and vulvovaginal (n = 3) sites were also affected. However, 5 episodes of proven disseminated candidiasis were also recorded.
Table 1.
Genetic and Clinical Features of Interleukin 12Rβ1–Deficient Patients With Candidiasis
| Patient No. | Code in Reference [6] | Country of Origin | Mutation | Age, ya/Sex | Follow-up Outcome | Candidiasis Onset (Age, y) | BCG Onset (Age, y) | EM Onset (Age, y) | Mycobacterium tuberculosis Onset (Age, y) | Salmonella Onset (Age, y) | Other Infections (Age, y) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 30 II.5 | Spain | NG | 6.9/M | Deceased | Candida spp. (birth) | NV | … | … | Salmonella enteritidis (5.9) | Varicella (chickenpox) (5) |
| 2 | 30 II.6 | Spain | 1791 +2 T > G | 30.2/M | Deceased | Candida albicans (2.1) | NV | … | … | S. enteritidis, Salmonella portland (6) | Measles (4), varicella (5), mumps (6), Campylobacter jejuni (28) |
| 3 | 97 II.1 | Tunisia | NG | 29/M | Alive | C. albicans (7) | R | … | M. tuberculosis (4) | … | Streptococcus spp. (27), Aerococcus viridans (27), herpes (17) |
| 4 | 83 II.1 | Turkey | 783 + 1G > A | 4/M | Alive | Candida spp. (2) | D (0.5) | … | … | … | … |
| 5 | 75 II.2 | Turkey | 783 + 1G > A | 4/M | Deceased | C. albicans (0.83) | D (2) | … | … | … | … |
| 6 | 75 II.1 | Turkey | 783 + 1G > A | 7/F | Deceased | C. albicans (3) | D (0.33) | … | … | … | … |
| 7 | 73 II.1 | Turkey | 783 + 1G > A | 4/M | Deceased | C. albicans (birth) | D (0.33) | … | … | … | … |
| 8 | 73 II.2 | Turkey | 783 + 1G > A | 11/F | Alive | C. albicans (1) | NVb | Mycobacterium spp. (0.75)b | … | Salmonella group B, Salmonella group D? (6) | … |
| 9 | 64 II.2 | Netherlands | Q376X | 28.4/F | Deceased | Candida spp. (4.1) | NV | Mycobacterium avium (4) | … | Salmonella typhimurium (4) | Rotavirus (3) |
| 10 | 10 II.2 | Israel (Bedouin Arab) | 700 + 362_1619–944del | 10.5/M | Alive | C. albicans (4) | NV | … | … | Salmonella group D (NA) | Kingella kingae (1.6, Trichophyton rubrum (4), Streptococcus pneumoniae (4.1), herpes (9.4) |
| 11 | 4 II.1 | Cyprus | 1623_1624delinsTT | 40/M | Alive | Candida spp. (2.3) | R | Mycobacterium triplex, Mycobacterium genevense (17) | … | S. enteritidis (11) | … |
| 12 | 7 II.5 | Turkey | R173P | 17/M | Deceased | C. albicans (17) | R | Mycobacterium fortuitum-chelonae complex (10), M. avium (17) | M. tuberculosis (7) | … | Acinetobacter baumani (17) |
| 13 | 49 II.1 | Turkey | 783 + 1G > A | 1.9/M | Deceased | Candida spp. (1) | D (1.3) | … | … | … | Staphylococcus aureus (NA) |
| 14 | 39 II.2 | Turkey | 628–644dup | 6/M | Deceased | Candida spp. (1.6) | D (1.5) | M. avium (3.7) | … | Salmonella spp. (4.2) | … |
| 15 | 39 II.5 | Turkey | 628–644dup | 2.5/M | Alive | Candida spp. (birth) | D (0.91) | … | … | … | … |
| 16 | 41 II.2 | Turkey | 783 +1 G > C | 3.1/M | Deceased | Candida spp. (birth) | R | … | … | S. enteritidis (1) | … |
| 17 | 38 II.2 | Turkey | 711 ins C | 2/F | Deceased | Candida spp. (birth) | D (0.5) | … | … | … | … |
| 18 | 44 II.1 | Mexico | 1791 +2 T > G | 3.5/F | Deceased | C. albicans (2.7) | D (0.5) | … | … | … | … |
| 19 | 57 II.1 | Mexico | 1791 +2 T > G | 16/M | Deceased | Candida spp. (15.6) | D (0.75) | … | … | … | Herpes (0.33) |
| 20 | 78 II.2 | Mexico | R486X | 4.6/M | Deceased | C. albicans (4.4) | D (0.5) | Mycobacterium spp. (4.6) | … | Salmonella spp. (2) | Klebsiella pneumoniae (4.6) |
| 21 | 25 II.1 | Spain | 1791 +2 T > G | 7.5/F | Deceased | Candida glabrata–C. albicans (4) | NV | M. avium (3.3) | … | S. enteritidis (0.91) | … |
| 22 | 18 II.1 | France | Q376X | 30.8/M | Alive | C. albicans (birth) | R | … | … | Salmonella dublin (2) | Enterobacter spp., Serratia spp. (3) |
| 23 | 81 II.1 | Turkey | 64 + 2T > G | 4.5/M | Alive | Candida spp. (1.2) | D (0.5) | … | … | … | … |
| 24 | 89 II.1 | Turkey | 1791 + 2T > G | 5.5/F | Alive | Candida spp. (2) | D (2) | … | … | … | … |
| 25 | 82 II.5 | Turkey | 1425delC | 3/M | Alive | Candida spp. (5) | D (0.5) | … | … | S. enteritidis (16) | … |
| 26 | Turkey | 64 + 1G- > T | 2.1/M | Alive | Candida spp. (5) | D (0.58) | … | … | … | … | |
| 27 | United States | W466X/Q541X | 2.5/M | Alive | Candida spp. (2.3) | NV | M. avium (1.8) | … | … | … | |
| 28 | Israel | 700 + 362_1619–944del | 16/M | Deceased | C. albicans (7.6) | NV | Mycobacterium spp. (15) | … | Salmonella spp. (10.4) | … | |
| 29 | Brazil | C474S | 7/M | Alive | Candida spp. (0.75) | D (0.25) | Mycobacterium spp. (2) | M. tuberculosis (0.75) | Salmonella spp. (2) | … | |
| 30 | Colombia | C291Y | 2.6/M | Alive | Candida spp. (1.8) | D (0.33) | … | … | … | Staphylococcus epidermis (0.75) | |
| 31 | Iran | Q410X | 6.4/F | Deceased | C. albicans (1.3) | NV | Mycobacterium spp. (4.9) | … | Salmonella typhi (1.6), Salmonella group D (4.2) | K. pneumoniae (2) | |
| 32 | Turkey | R211X | 7.6/F | Alive | C. albicans (1.5) | D (1.5) | … | … | Salmonella spp. (5) | Escherichia coli (1.5) | |
| 33 | Chile | 169delA | 3.5/M | Alive | Candida spp. (0.16) | D (0.25) | … | … | … | … | |
| 34 | The Netherlands | 1561G.C | 49/M | Alive | C. albicans (43.2) | NV | M. genevense (43.5) | … | … | E. coli (43.5) K. pneumoniae (44.4), S. pneumoniae (44.4) | |
| 35 | Russia | Q209X/1387del6 | 8.5/F | Alive | C. albicans (2) | D (0.33) | … | … | S. enteritidis (6) | Yersinia spp. (2), varicella (3) |
Abbreviations: BCG, bacille Calmette-Guérin; Candida spp., patient had Candida infection but the species was not identified; D, BCG disease after vaccination; EM, environmental mycobacteria (nontuberculous mycobacteria); NG, not genotyped, diagnosis of IL12RB1 deficiency was based on clinical phenotype, family history, and identification of IL12RB1 mutations in relatives; F, female; M, male; Mycobacterium spp., patient had mycobacterial infection but the species was not identified; NA, not available; NV, not vaccinated; R, resistant to vaccination; Salmonella spp., patient had nontyphoidal salmonellosis, but the species was not identified.
a Age at last follow-up or death.
b In this patient, BCG disease was suspected, probably acquired from the affected older brother's lesion. The mycobacterial species was not identified.
Table 2.
Epidemiological Characteristics of 76 Episodes of Candida Infection in 35 Patients With Interleukin 12Rβ1 Deficiencya
| Characteristics | Episodes, No. (%) |
|---|---|
| Type of candidiasis | |
| Recurrent or persistent | 53 (70)b |
| Acute | 23 (30) |
| Community acquired | 69 (91) |
| Hospital acquiredc | 7 (9) |
| Risk factors | |
| Antibiotic treatment | 42 (55) |
| Immunosuppression | 2 (3) |
| Antibiotics plus immunosuppression | 5 (7) |
| Neutropenia | 0 |
| Comorbid conditionsd | 0 |
| Central venous catheter plus antibiotics | 2 (3) |
| Abdominal surgery plus antibiotics | 1 (1) |
| Esophageal carcinoma plus antibiotics | 1 (1) |
| Bone marrow transplantation plus antibiotics | 1 (1) |
| No risk factors recorded | 27 (36) |
| Candida species | |
| Candida albicans | 40 (53) |
| Species not identified | 34 (45) |
| C. albicans plus other Candida species | 2 (3)e |
| Other fungal infections | |
| Trichophyton rubrum | 1 (1) |
a The median patient age at onset of first Candida infection ( ± standard deviation) was 1.5 ± 7.87 years.
b When the corresponding physician stated that a patient had multiple episodes of candidiasis, but only 1 episode was noted in the questionnaire, the patient was considered to have recurrent or persistent candidiasis, and only the reported episode was considered in the statistical analysis.
c Candida infections that occurred when the patients were hospitalized were considered probable cases of nosocomial infection.
d Comorbid conditions conferring a predisposition to candidiasis, such as diabetes, renal insufficiency, or pancreatitis.
e Coinfection with C. albicans and Candida glabrata was recorded in 2 episodes.
Figure 2.
Candida infections (episodes) in patients with interleukin 12Rβ1 deficiency. Two episodes of esophageal candidiasis and 1 of cutaneous candidiasis were associated with oropharyngeal candidiasis.
Oropharyngeal Candidiasis
Oropharyngeal candidiasis (OPC) was the predominant manifestation (34 of 35 patients), and no risk factors were identified for 23 of the 62 episodes (59 episodes of isolated OPC and 3 episodes of OPC associated with esophageal [n = 2], or cutaneous [n = 1] candidiasis). The risk factors for the remaining 39 episodes included antibiotic treatment in all cases and the use of immunosuppressive drugs in 6 cases. Twenty-six patients had recurrent or persistent OPC despite oral or intravenous antifungal treatment (Supplementary Figure 1). Six patients have had OPC since birth and continuing after the age of 6 months. A combination of stomatitis, aphtous ulcers, and oral thrush was noted in 2 patients. Secondary prophylaxis with fluconazole or itraconazole (in 2 patients each) controlled OPC, although candidiasis recurred in both patients when prophylaxis was withdrawn. However, 2 patients continued to have candidiasis in spite of prophylaxis with fluconazole (both patients) or itraconazole (1 patient); 1 of these patients (patient 25), continued to have OPC after intravenous amphotericin B followed by intravenous caspofungin, even though Candida isolates were sensitive to fluconazole, itraconazole, and amphotericin B.
Cutaneous Candidiasis
Cutaneous candidiasis was observed in 2 patients. Despite repeated treatments with oral fluconazole, griseofulvin, and itraconazole, patient 10 had recurrent skin and scalp infections with Trichophyton rubrum and Candida albicans in the absence of known risk factors. Patient 25 had a dermal lesion caused by Candida spp. on the left shoulder and neck during antibiotic treatment. The infection resolved after 2 weeks of treatment with intravenous amphotericin B.
Vulvovaginal Candidiasis
Vulvovaginal candidiasis due to C. albicans was recorded in 3 episodes in 3 patients (patient 9, age 26 years; patient 21, age 4 years; and patient 32, age 5 years). Two of these patients (patients 9 and 21) were receiving antibiotic treatment, and 1 patient was receiving immunosuppressive treatment. Coinfection with Candida glabrata was observed in 1 episode (in patient 21). All 3 episodes resolved following local antifungal treatment. No recurrent VVC was recorded.
Esophageal Candidiasis
Five patients (7 episodes) had esophageal candidiasis (Supplementary Figure 2), which manifested as decreased appetite, weight loss, and/or odynophagia. One case of community-acquired C. albicans superinfection of a well-differentiated squamous cell carcinoma of the esophagus (SCEC) was observed, in patient 2. This patient was receiving irregular prophylaxis with ciprofloxacin [25]. Patients 27, 28, 31, and 34 had community-acquired esophageal candidiasis at the ages of 2 years and 3 months, 9 years, 30 months, and 43 years, respectively. Patient 27 was receiving antimycobacterial treatment, and patient 31 was receiving cotrimoxazole treatment, but patients 28 and 34 were not taking antibiotics and had no other risk factors. Patients 2, 27, and 28 had previously had OPC. Patient 34 had a second episode of community-acquired esophageal candidiasis at age 44.5 years when he was receiving antimycobacterial treatment. Patient 28 also had hospital-acquired esophageal candidiasis when he was 15 years old, while receiving ceftriaxone plus prednisone treatment. Patient 2 responded to treatment with oral fluconazole, but no response to oral fluconazole was observed twice in patient 34. Secondary prophylaxis with oral fluconazole (patient 27) or oral itraconazole (patient 31) controlled esophageal candidiasis in 2 patients, although prophylaxis with oral fluconazole was ineffective in patient 28.
Systemic and Deep-Seated Candida Infections
Five episodes of documented invasive or disseminated candidiasis were recorded in 4 patients (Table 3 and Supplementary Material 2). Two patients (patients 9 and 12) had catheter-related candidemia with sepsis, caused by C. albicans. One of them (patient 9) developed an invasive infection of the ileus by C. albicans following laparotomy 1 month after an episode of candidemia. Despite antifungal treatment, 2 ileum biopsy specimen cultures were positive for C. albicans 9 months later. One patient had community-acquired disseminated candidiasis; patient 3 had acute pulmonary edema and endocarditis caused by Candida spp. Patient 20 had a systemic response, neurological symptoms, aplasia, and paralysis due to a C. albicans infection that was confirmed by cultures of urine and cerebrospinal fluid. However, the clinical course of the invasive candidiasis in patient 20 did not allow us to exclude the possibility that this episode was hospital acquired. Three of these patients (patients 3, 9, and 20) had had oral candidiasis since childhood. No other comorbid condition was identified in patient 3, and possible risk factors documented in patient 20 included intravenous antimycobacterial and antifungal treatment and surgical debridement of a dorsolumbar abscess.
Table 3.
Invasive Episodes of Candida Infection in Patients With Interleukin 12Rβ1 Deficiency
| Documented Candida Infections |
HAC or CAC | Previous Candidiasis | Candida Species | IFN-γa | ||
|---|---|---|---|---|---|---|
| Patient No. | Candida Site | Risk Factor | ||||
| 9 | Candidemia with sepsis | Catheter antimycobacterial treatment | HAC | Oral candidiasis, VVC | C. albicans | Yes |
| 9 | Gastrointestinal | Laparotomy, antimycobacterial treatment | HAC | Oral candidiasis, VVC | C. albicans | Yes |
| 12 | Candidemia with sepsis | Catheter, antimycobacterial treatment | HAC | … | C. albicans | No |
| 3 | Endocarditis | No | CAC | Oral candidiasis | Candida spp. | No |
| 20 | Urine and cerebrospinal fluid | Antimycobacterial treatment, Surgical debridement (dorsolumbar abscess) | HAC | Oral candidiasis | C. albicans | Yes |
Abbreviations: CAC, community-acquired candidiasis; HAC, hospital-acquired candidiasis; IFN, interferon; VVC, vulvovaginal candidiasis.
a IFN-γ treatment at the time of the episodes.
Onset of Candidiasis
In the 35 patients with candidiasis, the first episode of candidiasis occurred earlier in life (1.5 ± 7.87 years; range, birth to 43 years) than reported for classic MSMD-defining infections, such as those caused by environmental mycobacteria (4.29 ± 11.9 years; range, 9 months to 43 years), Mycobacterium tuberculosis (4 ± 3.12 years; range, 9 months to 7 years), or Salmonella species (4.58 ± 4.17 years; range, 11 months to 16 years) or other infections (3 ± 11.67 years; range, 4 months to 43.5 years). By contrast, BCG vaccination induced disease at even younger ages (0.5 ± 0.57 years; range, 3 months to 2 years) than Candida or other infections. Nevertheless, Candida was the first documented infection in 19 of the 35 patients, despite the vaccination of 10 of these 19 patients with BCG vaccine, suggesting that >10% of patients with IL-12Rβ1 deficiency may first present with Candida infections.
Mortality
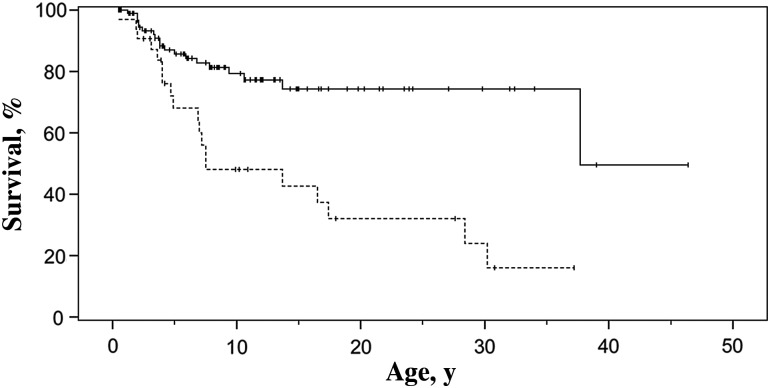
The mortality rate in our 35 patients with candidiasis (49%) was higher than that previously reported for 132 symptomatic IL-12Rβ1–deficient patients (31.8%) [6]. We did not have up-to-date data for many of the previously reported patients, particularly those without candidiasis. However, we analyzed mortality for the previously reported 128 symptomatic IL-12Rβ1–deficient patients (of the 141 patients described elsewhere) for whom information about Candida infection was available (Table 4) [6]. Mortality rates were significantly higher (P = .00004) for patients with candidiasis (19 of 32 [59%]) than for those without Candida infection (20 of 96 [21%]; odds ratio, 5.84; 95% confidence interval, 2.46–13.9). Likewise, Kaplan–Meier survival analysis (Figure 3) showed survival to be significantly lower for patients with candidiasis (P = .0001 by log-rank test) than for those without Candida infection.
Table 4.
Infections and Outcome for the Interleukin 12Rβ1–Deficient Patients With or Without Candidiasisa
| Infections and Outcomes | Interleukin 12Rβ1–Deficient Patients, No. (%)b |
|
|---|---|---|
| Without Candidiasis (n = 96) | With Candidiasis (n = 32) | |
| Age at last follow-up or death, mean ± SD, y | 10.9 ± 9.48c | 10.49 ± 10.06 |
| Male sex | 50 (52) | 21 (66) |
| Mycobacterial disease | 74/96 (77) | 25/32 (78) |
| BCG disease | 59/96 (61) | 18/32 (56) |
| BCG resistantd | 18/77 (23) | 6/24 (25) |
| EM disease | 8/96 (8) | 6/32 (19) |
| In BCG-vaccinated patients | 4/77 (5) | 3/24 (12) |
| In patients with BCG disease | 2/59 (3) | 1/18 (6) |
| Mycobacterium tuberculosis disease | 7/96 (7) | 2/26 (8) |
| Salmonellosis | 35/96 (36) | 15/32 (47) |
| Mortalitye | 20/96 (21) | 19/32 (59) |
| Mean age at death, mean ± SD, y | 6.69 ± 8.22 yc | 9.0 ± 8.54 y |
Abbreviations: BCG, bacille Calmette-Guérin; EM, environmental mycobacteria (nontuberculous mycobacteria); SD, standard deviation.
a Data are from reference [6]; only those patients for whom information about Candida infection was available were included.
b Values represent No. (%) of patients unless otherwise specified.
c No data were available for 1 patient.
d BCG-vaccinated patients resistant to BCG disease.
e Mortality was 23% for the 13 of the 141 patients described elsewhere [6], for whom no information about Candida infection was available.
Figure 3.
Kaplan–Meier estimation of survival for patients with interleukin 12Rβ1 deficiency with (dashed line) or without (solid line) Candida infections (log-rank χ2 14.56; P = .0001).
DISCUSSION
We recently noted that about 25% of IL-12Rβ1–deficient patients have chronic CMC [6]. Oropharyngeal candidiasis, skin infections, and/or onychomycosis due to C. albicans were the most common forms of mucocutaneous candidiasis in patients with AD-HIES (43%–56% of patients) [26, 27], APS-I (all patients by age 40 years and 30% in the first 2 years of life) [28, 29], or CMCD due to mutations of IL17F, IL17RA or ACT1 or gain-of-function mutations of STAT1 [18–22]. Oropharyngeal C. albicans infection was by far the most common presentation of Candida infection in our series of patients and was present in 6 patients at birth. Other forms of mucocutaneous candidiasis were rare in our patients. Only 3 episodes of VVC were recorded in the 9 female patients in our series. Vulvovaginal candidiasis, even if recurrent, is also common in healthy women with no known risk factors [30, 31]. In the absence of large epidemiological studies, it is probably not possible to associate the occurrence of VVC with impairments of immunity mediated by the IL-23/IL-17/interleukin 22 axis. Likewise, only 2 episodes of dermal infection were documented, and no onychomycosis was observed.
Other patients with MSMD due to mutations impairing IFN-γ–mediated responses (IFNGR1, IFNGR2, or STAT1 deficiencies due to loss-of-function alleles) do not seem to be prone to Candida infections, even when treated with prolonged courses of antibiotics or long-term prophylaxis [32, 33]. Overall, our data indicate a potentially causal role of IL-23/IL-17 circuit impairment, but not of IL-12/IFN-γ circuit impairment, in susceptibility to mucocutaneous candidiasis in patients with IL-12Rβ1 deficiency. The absence of onychomycosis in our patients and their lower incidence of oral and skin infections than in patients with other primary immunodeficiencies (PIDs) resulting in impaired IL-17 immunity may reflect a milder impairment of IL-17–mediated responses in patients with IL-12Rβ1 deficiency than in those with AD-HIES, APS-I, or CMCD [9, 18–22].
Esophageal candidiasis was observed in 5 patients (7 episodes) in our series. Patient 2 had esophageal candidiasis at age 25 years, coinciding with the diagnosis of SCEC, in the absence of overt predisposing factors [25]. Esophageal candidiasis is relatively common in patients with APS-I (14 of 91 Finnish patients with APS-I), but it is unusual in patients with AD-HIES [26–29, 34]. It has been suggested that there is an association between CMC and predisposition to oral and esophageal carcinomas [35]. We cannot formally exclude the possibility that candidiasis was an SCEC-predisposing factor in our patient, but the 2 conditions, candidiasis and SCEC, were diagnosed simultaneously. The IL-12/IFN-γ axis has a dramatic antitumor effect, and IL-17–producing T cells have been reported to have both anti- and protumorigenic effects [36]. Other patients with MSMD have also had cancer at young ages [25].
Most IL-12Rβ1–deficient patients continued to have recurrent or persistent OPC despite treatment with oral nystatin or fluconazole. Remarkably, fluconazole prophylaxis did not control candidiasis in 2 of 4 patients with OPC and in 1 of 2 patients with esophageal candidiasis; itraconazole prophylaxis did not eradicate candidiasis in 1 of 4 patients, but it controlled the infection in 1 patient with esophageal candidiasis. Poor responses to treatment with azoles were found to be unrelated to resistances to these antifungals in 2 patients with OPC treated with oral fluconazole or intravenous fluconazole. Likewise, itraconazole and fluconazole prophylaxis did not control esophageal candidiasis by a C. albicans strain sensitive to both drugs. No antifungal prophylaxis was documented in patients without candidiasis. (For a proposal of antifungal treatment in IL-12Rβ1–deficient patients with candidiasis see Supplementary Material 3 [37].)
Remarkably, disseminated candidiasis was observed in 4 of our 35 patients, with a total of 5 episodes. Three of these 5 episodes were nosocomial, and the clinical course of the invasive candidiasis in patient 20 does not exclude the possibility that it was hospital acquired. However, 1 patient had disseminated community-acquired candidiasis in the absence of predisposing factors other than the PID. Disseminated candidiasis is extremely rare in patients with APS-I, AD-HIES, or CMCD and is thought to be nosocomial [26–29, 34, 38]. Likewise, patients with isolated inborn errors of IL-17 or IFN-γ immunity do not seem to display invasive candidiasis, even though the latter also have severe mycobacterial and salmonella infections and often require similar in-hospital procedures [32, 33]. By contrast, invasive and fatal Candida infections, such as meningeal candidiasis, are observed in patients with CARD9 deficiency, the only known PID conferring a predisposition to invasive candidiasis . However, CARD9 deficiency may impair several immune responses to Candida and other fungi through mechanisms other than the impaired IL-17–mediated immunity [16, 17].
We acknowledge several limitations to our study. First, no data were available on the occurrence of candidiasis in 13 previously reported patients [6]. In addition, we cannot exclude the possibility that some episodes, particularly of OPC, were treated by primary care physicians and that they were not reported to the physicians providing care at tertiary hospitals. Second, 16 of the 35 patients studied were from a single country (Turkey), which could bias our data. However, the remaining 19 patients were from 13 countries in Europe, Africa, North and South America, and the Middle East. Third, it is difficult to know whether some episodes of candidiasis were only consequence of the PID or could have been secondary to other factors, such as hospital exposure, particularly in patients with invasive candidiasis who underwent surgery or in those with central lines. Fourth, our data suggest that IL-12Rβ1–deficient patient with candidiasis may have a poorer prognosis than those without candidiasis. However, there is not enough information to ascertain whether the groups of patients with or without candidiasis were comparable in terms of severity, exposure to healthcare, or other comorbid conditions; therefore, a causal relationship cannot be established.
Immune responses to Candida are anatomically compartmentalized, and the roles of the IL-12/IFN-γ and IL-23/IL-17 circuits in predisposition to invasive candidiasis remain unclear [21, 30, 31, 39, 40]. In a mouse model of oral infection, the IL-12/IFN-γ circuit was found to be more relevant than the IL-23/IL-17 axis for limiting the invasiveness of the fungus beyond the oral cavity [30, 31]. Thus, the pathogenesis of invasive candidiasis may involve the combined impairment of IL-17 and IFN-γ immunity, as in IL-12Rβ1–deficient patients. However, candidemia is the fourth most common cause of nosocomial bloodstream infections in much of the developed world [37]. Further data are needed to draw firm conclusions about susceptibility to invasive candidiasis in IL-12Rβ1–deficient patients. Finally, our data expand the known infectious phenotype of IL-12Rβ1 deficiency and indicate that candidiasis may be the first clinical manifestation in IL-12Rβ1–deficient patients.
Supplementary Material
Notes
Acknowledgments. We thank the patients and their families for their trust.
Author contributions. M. O., I. S., E. H. R., J. B., C. P., A. P., S. B. D., L. A., J. L. C., and C. R. G. performed the research and analyzed and interpreted data. O. S., A. I., I. T., F. D., S. P. S., M. K., G. T., C. N., E. C., D. K., J. L., N. Kutukculer, C. A., M. Bhatti, N. Karaca, R. B., A. B., E. G., J. L. F., N. P., I. R., A. Strickler, A. Shcherbina, A. Somer, A. Segal, A. A. M., J. L. L. F., M. Bejaoui, M. B. D. V., S. K., T. S., and I. B. M. were responsible for the clinical evaluation of the patients and also collected data. J. L. C. and C. R. G. designed the research, analyzed and interpreted data, and wrote the manuscript, and M. O. collaborated in the writing of the manuscript.
Disclaimer. The sponsors of the study had no role in its design, the collection, analysis, and interpretation of the data, or the writing of the manuscript.
Financial support. This work was supported by Fondo de Investigaciones Sanitarias, Ministerio de Economía y Competitividad (grants PI06/1031 and PI10/01718), the European Regional Development Fund–European Social Fund (FEDER-FSE), Fundación Canaria de Investigación y Salud (Canarian government; INREDCAN 05/06), Foundation Caja Rural de Canarias-Chil y Naranjo (research prize 2004), Universidad de Las Palmas de Gran Canaria (fellowship to E. H. R), INSERM, University Paris Descartes, Rockefeller University, National Center for Research Resources and the National Center for Advancing Sciences of the National Institutes of Health (grant 8UL1TR000043), Laboratoire d'Excellence “Integrative Biology of Emerging Infectious Diseases” (grant ANR-10-LABX-62-IBEID), the European Research Council, Agence Nationale de la Recherche (grant GENCMCD 11-BSV3-005-01), the St Giles Foundation, the Candidoser Association, and Consejo Nacional de Ciencia y Tecnología de Mexico (grants 69992 and 182817).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Filipe-Santos O, Bustamante J, Chapgier A, et al. Inborn errors of IL-12/23- and IFN-gamma-mediated immunity: molecular, cellular, and clinical features. Semin Immunol. 2006;18:347–61. doi: 10.1016/j.smim.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Bogunovic D, Byun M, Durfee LA, et al. Mycobacterial disease and impaired IFN-γ immunity in humans with inherited ISG15 deficiency. Science. 2012;337:1684–8. doi: 10.1126/science.1224026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hambleton S, Salem S, Bustamante J, et al. IRF8 mutations and human dendritic-cell immunodeficiency. N Engl J Med. 2011;365:127–38. doi: 10.1056/NEJMoa1100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bustamante J, Arias AA, Vogt G, et al. Germline CYBB mutations that selectively affect macrophages in kindreds with X-linked predisposition to tuberculous mycobacterial disease. Nat Immunol. 2011;12:213–21. doi: 10.1038/ni.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fieschi C, Dupuis S, Catherinot E, et al. Low penetrance, broad resistance, and favorable outcome of interleukin 12 receptor beta1 deficiency: medical and immunological implications. J Exp Med. 2003;197:527–35. doi: 10.1084/jem.20021769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Beaucoudrey L, Samarina A, Bustamante J, et al. Revisiting human IL-12Rbeta1 deficiency: a survey of 141 patients from 30 countries. Medicine (Baltimore) 2010;89:381–402. doi: 10.1097/MD.0b013e3181fdd832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trinchieri G, Pflanz S, Kastelein RA. The IL-12 family of heterodimeric cytokines: new players in the regulation of T cell responses. Immunity. 2003;19:641–4. doi: 10.1016/s1074-7613(03)00296-6. [DOI] [PubMed] [Google Scholar]
- 8.Korn T, Bettelli E, Oukka M, Kuchroo VK. IL-17 and Th17 Cells. Annu Rev Immunol. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710. [DOI] [PubMed] [Google Scholar]
- 9.de Beaucoudrey L, Puel A, Filipe-Santos O, et al. Mutations in STAT3 and IL12RB1 impair the development of human IL-17-producing T cells. J Exp Med. 2008;205:1543–50. doi: 10.1084/jem.20080321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacLennan C, Fieschi C, Lammas DA, et al. Interleukin (IL)-12 and IL-23 are key cytokines for immunity against Salmonella in humans. J Infect Dis. 2004;190:1755–7. doi: 10.1086/425021. [DOI] [PubMed] [Google Scholar]
- 11.Prando C, Samarina A, Bustamante J, et al. Inherited IL-12p40 deficiency: genetic, immunologic, and clinical features of 49 patients from 30 kindreds. Medicine (Baltimore) 2013;92:109–22. doi: 10.1097/MD.0b013e31828a01f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puel A, Doffinger R, Natividad A, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med. 2010;207:291–7. doi: 10.1084/jem.20091983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kisand K, Bøe Wolff AS, Podkrajsek KT, et al. Chronic mucocutaneous candidiasis in APECED or thymoma patients correlates with autoimmunity to Th17-associated cytokines. J Exp Med. 2010;207:299–308. doi: 10.1084/jem.20091669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minegishi Y, Saito M, Tsuchiya S, et al. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 2007;448:1058–62. doi: 10.1038/nature06096. [DOI] [PubMed] [Google Scholar]
- 15.Chandesris MO, Melki I, Natividad A, et al. Autosomal dominant STAT3 deficiency and hyper-IgE syndrome: molecular, cellular, and clinical features from a French national survey. Medicine (Baltimore) 2012;91:e1–19. doi: 10.1097/MD.0b013e31825f95b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puel A, Cypowyj S, Maródi L, Abel L, Picard C, Casanova JL. Inborn errors of human IL-17 immunity underlie chronic mucocutaneous candidiasis. Curr Opin Allergy Clin Immunol. 2012;12:616–22. doi: 10.1097/ACI.0b013e328358cc0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lanternier F, Pathan S, Vincent QB, et al. Deep dermatophytosis and inherited CARD9 deficiency. N Engl J Med. 2013;369:1704–14. doi: 10.1056/NEJMoa1208487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–8. doi: 10.1126/science.1200439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van de Veerdonk FL, Plantinga TS, Hoischen A, et al. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N Engl J Med. 2011;365:54–61. doi: 10.1056/NEJMoa1100102. [DOI] [PubMed] [Google Scholar]
- 20.Liu L, Okada S, Kong XF, et al. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J Exp Med. 2011;208:1635–48. doi: 10.1084/jem.20110958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cypowyj S, Picard C, Maródi L, Casanova JL, Puel A. Immunity to infection in IL-17-deficient mice and humans. Eur J Immunol. 2012;42:2246–54. doi: 10.1002/eji.201242605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boisson B, Wang C, Pedergnana V, et al. An ACT1 mutation selectively abolishes interleukin-17 responses in humans with chronic mucocutaneous candidiasis. Immunity. 2013;39:676–86. doi: 10.1016/j.immuni.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aytekin C, Dogu F, Tuygun N, et al. Bacille Calmette-Guerin lymphadenitis and recurrent oral candidiasis in an infant with a new mutation leading to interleukin-12 receptor beta-1 deficiency. J Investig Allergol Clin Immunol. 2011;21:401–4. [PMC free article] [PubMed] [Google Scholar]
- 24.Potjewijd J, de Paus RA, van Wengen A, Damoiseaux J, Verbon A, van de Vosse E. Disseminated Mycobacterium genavense infection in a patient with a novel partial interleukin-12/23 receptor β1 deficiency. Clin Immunol. 2012;144:83–6. doi: 10.1016/j.clim.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Cardenes M, Angel-Moreno A, Fieschi C, et al. Oesophageal squamous cell carcinoma in a young adult with IL-12R beta 1 deficiency. J Med Genet. 2010;47:635–7. doi: 10.1136/jmg.2009.071910. [DOI] [PubMed] [Google Scholar]
- 26.Schimke LF, Sawalle-Belohradsky J, Roesler J, et al. Diagnostic approach to the hyper-IgE syndromes: immunologic and clinical key findings to differentiate hyper-IgE syndromes from atopic dermatitis. J Allergy Clin Immunol. 2010;126:611–7. doi: 10.1016/j.jaci.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 27.Woellner C, Gertz EM, Schäffer AA, et al. Mutations in STAT3 and diagnostic guidelines for hyper-IgE syndrome. J Allergy Clin Immunol. 2010;125:424–32. doi: 10.1016/j.jaci.2009.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perheentupa J. Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. J Clin Endocrinol Metab. 2006;91:2843–50. doi: 10.1210/jc.2005-2611. [DOI] [PubMed] [Google Scholar]
- 29.Betterle C, Greggio NA, Volpato M. Clinical review 93: autoimmune polyglandular syndrome type 1. J Clin Endocrinol Metab. 1998;83:1049–55. doi: 10.1210/jcem.83.4.4682. [DOI] [PubMed] [Google Scholar]
- 30.Pirofski LA, Casadevall A. Rethinking T cell immunity in oropharyngeal candidiasis. J Exp Med. 2009;206:269–73. doi: 10.1084/jem.20090093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conti HR, Gaffen SL. Host responses to Candida albicans: Th17 cells and mucosal candidiasis. Microbes Infect. 2010;12:518–27. doi: 10.1016/j.micinf.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dorman SE, Picard C, Lammas D, et al. Clinical features of dominant and recessive interferon gamma receptor 1 deficiencies. Lancet. 2004;364:2113–21. doi: 10.1016/S0140-6736(04)17552-1. [DOI] [PubMed] [Google Scholar]
- 33.Sologuren I, Boisson-Dupuis S, Pestano J, et al. Partial recessive IFN-gammaR1 deficiency: genetic, immunological and clinical features of 14 patients from 11 kindreds. Hum Mol Genet. 2011;20:1509–23. doi: 10.1093/hmg/ddr029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirkpatrick CH. Chronic mucocutaneous candidiasis. Pediatr Infect Dis J. 2001;20:197–206. doi: 10.1097/00006454-200102000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Rosa DD, Pasqualotto AC, Denning DW. Chronic mucocutaneous candidiasis and oesophageal cancer. Med Mycol. 2008;46:85–91. doi: 10.1080/13693780701616023. [DOI] [PubMed] [Google Scholar]
- 36.Zou W, Restifo NP. T(H)17 cells in tumour immunity and immunotherapy. Nat Rev Immunol. 2010;10:248–56. doi: 10.1038/nri2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pappas PG, Kauffman CA, Andes D, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35. doi: 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freeman AF, Holland SM. The hyper-IgE syndromes. Immunol Allergy Clin North Am. 2008;28:277–91. doi: 10.1016/j.iac.2008.01.005. viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang W, Na L, Fidel PL, Schwarzenberger P. Requirement of interleukin-17A for systemic anti-Candida albicans host defense in mice. J Infect Dis. 2004;190:624–31. doi: 10.1086/422329. [DOI] [PubMed] [Google Scholar]
- 40.Lin L, Ibrahim AS, Xu X, et al. Th1-Th17 cells mediate protective adaptive immunity against Staphylococcus aureus and Candida albicans infection in mice. PLoS Pathog. 2009;5:e1000703. doi: 10.1371/journal.ppat.1000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.