The results of a survey of 1,396 occupational therapy practitioners on their preparation for early identification of children with autism provides baseline information concerning identified skills, practices, and barriers as well as opportunities for professional development.
MeSH TERMS: autistic disorder; child development disorders, pervasive; early diagnosis; occupational therapy; professional competence
Abstract
The purpose of this study was to examine the perceived preparedness of practitioners in the early identification of children ages birth to 6 yr with autism spectrum disorder (ASD). Both occupational therapists and occupational therapy assistants were included in this survey study. The online survey instrument consisted of 29 questions within six sections capturing participant demographics, delivery of occupational therapy services, action when autism is suspected, service delivery experience, resource sharing, and barriers to conducting autism screening. The results of the study provide baseline information concerning identified skills, practices, and barriers among 1,396 practitioners. Additionally, opportunities are revealed for professional development necessary to support practitioners in the early identification of children at risk for ASD through surveillance and screening among children ages birth to 6 yr.
Autism spectrum disorders (ASD) are a group of developmental disabilities with characteristics that include qualitative impairment in social interaction; communication disorders; and stereotyped, repetitive patterns of behaviors or a restricted range of interests, according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM–IV–TR; American Psychiatric Association [APA], 2000). Autistic disorder, Asperger syndrome, and pervasive developmental disorder–not otherwise specified (PDD–NOS) were diagnostic ASD categories dependent on the level and distribution of symptoms at the time of the study. The 5th edition of the DSM has since been published; it includes these ASD categories under the single ASD diagnosis (APA, 2013). In the United States, the prevalence of ASD is 11.3 per 1,000 children, or 1 in 88, and 1 in 54 among boys (Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators, 2012). ASD have become an important public health concern and are the second most common serious developmental disability after mental retardation/intellectual impairment (Centers for Disease Control and Prevention [CDC], 2011).
The current DSM–IV–TR diagnostic criteria for ASD were validated in children 3 yr and older (APA, 2000); however, 80% of parents of children with ASD notice abnormalities in their child by age 24 mo (Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators, 2009; Landa, 2008). Social responsiveness; social initiation; social–emotional interaction; communication and play; and sensory, motor, or attention behaviors have been identified as key behavioral characteristics reported before 24 mo of age in retrospective and prospective studies for children later diagnosed with autism (Landa, 2008). In the United States, ASD is typically diagnosed between age 3 and 6 yr (Landa, 2008; Mandell, Novak, & Zubritsky, 2005; Matson, Wilkins, & Gonzalez, 2008). However, there are systematic testing procedures for a reliable diagnosis of ASD as early as age 2 yr (CDC, 2012; Matson et al., 2008). The earlier the behavior characteristics associated with ASD are detected, the earlier the child can be evaluated by a specialist to determine a diagnosis.
Surveillance and screening are two methods used to identify earlier potential risk for autism among young children. The use of surveillance and screening for ASD has become more widespread among pediatricians and other health care providers working with young children and families. Surveillance involves the use of a systematic but informal means to discern developmental risk and protective factors (American Academy of Pediatrics [AAP], 2006). Screening involves the use of standardized instruments to determine the extent of risk and whether referral is warranted (AAP, 2006). Surveillance is less formal than screening and includes listening to familial concerns, maintaining an accurate history and record of concerns, and using observations (AAP, 2006). In 2006 the AAP recommended developmental surveillance at every well-child preventive care visit with developmental screening at 9, 18, 24, or 30 mo. In addition, the AAP recommended that all children be screened specifically for autism during regular well-child doctor visits at 18 and 24 mo. Early detection and intervention services for ASD are critical to improved outcomes. Early identification combined with intense and specific intervention leads to improved language skill development (Virués-Ortega, 2010), intelligence, and adaptive behavior (Dawson et al., 2010).
Occupational therapy is second to speech–language therapy as the most frequently provided service to people with ASD throughout the United States (American Occupational Therapy Association [AOTA], 2010a; Interactive Autism Network, 2009). Occupational therapy services are a primary service under Part C of the Individuals With Disabilities Education Improvement Act of 2004 (IDEA 2004; Pub. L. 108–446) and are a related service under Part B of IDEA to help students with disabilities, including ASD, benefit from special education (IDEA 2004, §602[26][A]). These children have a range of occupational and performance issues that inhibit their full participation in school, home, and community activities. AOTA (2010) defined the role of occupational therapy practitioners when serving children with autism as “enhancing participation in and performance of activities of daily living (ADLs), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation within their natural and daily contexts” (p. S126) and as “[working] collaboratively with individuals on the autism spectrum, their families, other professionals, organizations, and community members in multiple contexts to advocate for and provide a range of needed resources and services that support the individuals’ ability to participate fully in life” (p. S125).
Occupational therapy practitioners exhibit a key role in service delivery among children with autism in the literature. However, the literature is unclear on the role of practitioners in the early identification of autism.
The “Learn the Signs. Act Early.” public awareness campaign aims to educate parents about childhood development, including early warning signs of autism and other developmental disorders, and encourages developmental screening and intervention (CDC, 2012). AOTA educates the public and advances the profession by providing resources, setting standards, and serving as an advocate to improve health care. The ongoing partnership between these two organizations enhances education in ASD while advancing the profession of occupational therapy through resource sharing, standard setting, and advocacy related to ASD. The purpose of this study was to examine occupational therapy practitioner perceptions regarding their preparedness for the early identification of ASD in children ages birth to 6 yr through an online survey targeting all 50 U.S. states and two U.S. territories.
Method
Research Design
Occupational therapy practitioners are defined as occupational therapists and occupational therapy assistants; both types of professionals were included in this online survey. The survey was developed through a partnership between the CDC and AOTA. The study received institutional review board approval from the University of South Carolina. All participants provided electronic informed consent that contained information about the purpose of the study, procedures, benefits of participating, voluntary participation, and contact information of the researchers.
Participants
Participants were solicited to voluntarily participate in an online survey through e-mail invitations to the AOTA Pediatric Listserv; Infant–Toddler Coordinators Association; AOTA Autism Specialty Conference attendees; the National Early Childhood Technical Assistance Center Listserv; state occupational therapy association presidents; the South Carolina IDEA, Part C Team for Early Childhood Solutions Listserv; and other volunteer occupational therapy pediatric work groups. The survey link was posted on the AOTA Web site under Children and Youth, on the AOTA home page, and on the AOTA Twitter and Facebook accounts. It was also printed in the Infant and Toddler Coordinator Association Newsletter and in OT Practice. Reminders were posted to the online sites within the open survey time frame.
Instrument
The survey consisted of 29 items within six sections capturing participant demographics; delivery of occupational therapy services; action when autism is suspected; service delivery experience; resource sharing; and barriers to conducting autism screening. Survey items were adapted from a prior survey conducted through a CDC–Association of University Centers on Disabilities Collaboration Research Award (Nalty, 2010) and a prior survey of Illinois service coordinators developed through the Illinois Leadership Education in Neurodevelopmental and Related Disabilities (Pizur-Barnekow, Muusz, Karpinski, O’Connor, & Cutler, 2012). The survey questions were adapted to address the unique roles and perceived preparedness of occupational therapy practitioners in serving young children with special needs and their families. Survey item formats included Likert scale with forced-choice (n = 5), multiple-choice (n = 12), and select-all-that-apply (n = 12) questions. The survey items captured participants’ autism-specific screening practices, experiences communicating with families, referral practices, experiences with sharing resources, and barriers to screening.
The survey was peer reviewed by key stakeholders including staff members of the AOTA Professional Affairs Division and AOTA Special Interest Section and work group members. CDC partners and collaborators representing speech–language pathology and the American Physical Therapy Association provided reviews during phases of the survey study development. Modifications were made to the study survey based on stakeholder feedback.
Procedures
A Survey Monkey (Surveymonkey.com, Portland, OR) link was used for national dissemination of the survey. The online survey was open for a 4-mo time frame. During this time, reminder e-mails were sent to individuals, and information was repeatedly posted on the online venues listed earlier.
Data Collection and Analysis
The final raw data were downloaded from Survey Monkey into a Microsoft Excel file for analysis using SAS software (Version 9.2; SAS Institute, Cary, NC). Descriptive statistics were used to provide baseline information concerning survey participants.
Results
A total of 1,396 respondents participated in the survey; 305 participants (22%) did not complete responses to all items. However, every collected completed item response was included in the final analysis. The total sample size of potential participants is unknown because the number of people registered with the Listserv groups or who responded through Web site links was not tracked. The study provided baseline information about identified skills, practices, and barriers determined through the completed responses of practitioners who support the early identification of autism among children ages birth to 6 yr. Online survey participation was received from all 50 states and two U.S. territories (Puerto Rico and Northern Marianas Islands). However, the data collected cannot be determined to be representative of these regions or the profession as a whole.
Section 1: Demographic Information
The first section of the survey collected demographic information. The sample consisted of practitioners (occupational therapists or occupational therapy assistants) with experience working with children with ASD ages birth–6 yr. A total of 95% of the respondents (n = 1,227) were occupational therapists, and 5% (n = 60) were occupational therapy assistants. A majority of respondents (91%, n = 1,171) identified themselves as White. Ethnicity was collected as Hispanic (4%, n = 51) and non-Hispanic (96%, n = 1,236) and gender as male (2%, n = 28) and female (98%, n = 1,269).
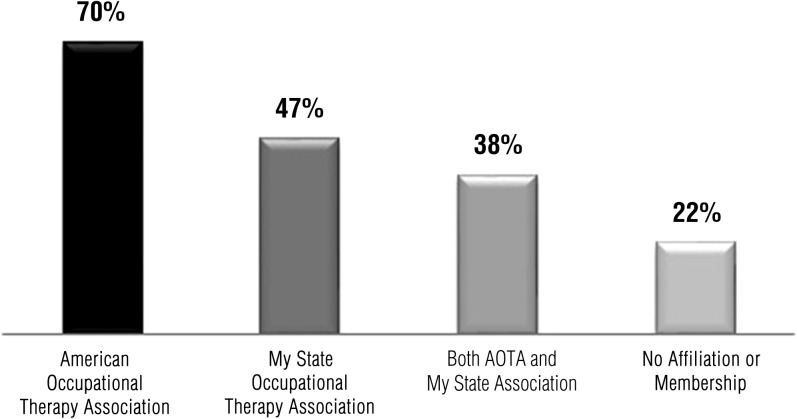
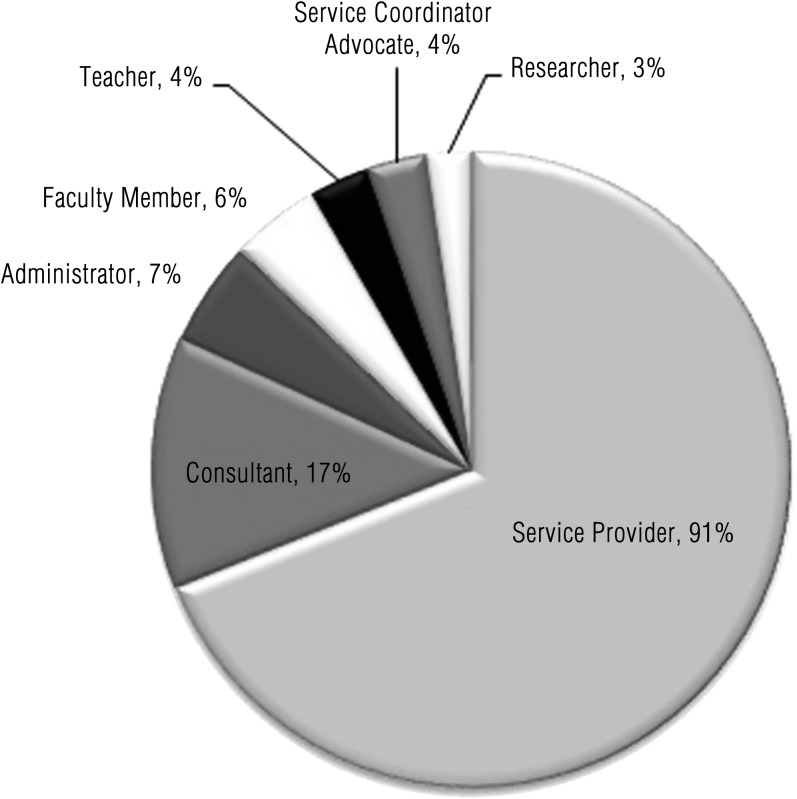
Of the respondents who identified association membership affiliation, 70% (n = 894) were members of AOTA (Figure 1). Among respondents who indicated their primary job role, 91% (n = 1,146) were service providers (Figure 2). Of the respondents who identified the number of years working in the profession, 64% (n = 816) had more than 10 yr of work experience. The states with greatest representation were Maryland (8% of respondents, n = 95); California and Virginia (6%, n = 76 and 74, respectively); and Washington, New York, and South Carolina (5%, n = 62, 61, and 57, respectively).
Figure 1.
Membership affiliation.
Figure 2.
Primary job role.
Section 2: Screening Practices
Section 2 of the survey included items related to the practices used by occupational therapy practitioners when delivering services to children with autism and their families. The major findings within this section were that 68% of respondents (n = 765) reported informally screening for autism when testing; 70% (n = 808) reported not using psychometrically sound screening instruments designed to detect children who may be at risk for autism; and 86% (n = 1,019) reported that occupational therapy profiles (participation history) are useful in helping to identify some of the early signs of autism.
Section 3: Action When Autism Is Suspected
The items in Section 3 related to practices of occupational therapy practitioners when working with a child when autism is suspected. Many respondents (63%, n = 609) used no psychometrically sound screening instruments to determine level of risk when autism was suspected. Respondents who used psychometrically sound screening instruments indicated that the most commonly used developmental screeners were the Ages and Stages Questionnaire (Bricker & Squires, 2009) and Ages and Stages Questionnaire Social–Emotional (Bricker & Squires, 2002). The most commonly used autism-specific screeners were the Modified Checklist for Autism in Toddlers (Robins, Fein, & Barton, 1999) and the Autism Behavior Checklist (Krug, Arick, & Almond, 1980). Fewer than 10% indicated using the CHecklist for Autism in Toddlers (Baron-Cohen et al., 2000); Parents’ Evaluation of Developmental Status (Glascoe, 1997); Pervasive Developmental Disorders Screening Test—2nd Edition (Seigel, 2004); Social Communication Questionnaire (Rutter, Bailey, & Lord, 2003); Communication and Symbolic Behavior Scales Developmental Profile (Wetherby & Prizant, 2002); Infant Toddler Checklist (Wetherby & Prizant, 2002); Systematic Observation of Red Flags (Wetherby & Woods, 2002); or the Screening Tool for Autism in Two-Year-Olds (Stone & Ousley, 1997).
This section also included questions about practitioners’ familiarity with the CDC’s “Learn the Signs. Act Early.” campaign. The results revealed that only 30% (n = 351) indicated being familiar with the campaign. Of the respondents who were familiar with the CDC’s campaign, 56% (n = 193) indicated knowing how to access campaign materials, and 28% (n = 88) indicated having shared materials with families. A total of 33% (n = 111) indicated not knowing how to access, share, copy, or display campaign materials.
Section 4: Service Delivery Experience
Section 4 of the survey contained items related to occupational therapy practitioner experiences when working with children with autism and their families. Results revealed that 58% (n = 628) felt most prepared to discuss current research evidence about autism with families; 90% (n = 980) felt most prepared to explain indicators of autism that have relevance to occupational therapy; 96% (n = 1,048) felt most prepared to discuss typical developmental milestones with families; 80% (n = 871) felt most prepared to explain the role of occupational therapy in early identification of autism; and 52% (n = 561) felt most prepared to explain information about autism to families of differing cultures. Concerning least preparedness, respondent results revealed that 75% (n = 809) felt least prepared to select screening instruments for autism, and 68% (n = 736) felt least prepared to use screening instruments to determine whether a child may be at risk for autism.
Section 5: Preferred Methods of Acquiring Information
Section 5 included items related to types of information practitioners prefer and how practitioners prefer to acquire information to support their role in the early identification of children with autism. Results revealed that 85% (n = 903) of respondents wanted information on current research evidence in the field of autism; 81% (n = 857) wanted information about screening and screening instruments for autism; 76% (n = 803) wanted information for families about autism that is easy to read and understand; 73% (n = 775) wanted information about occupational therapy evaluation procedures when autism is a concern; 69% (n = 727) wanted methods for explaining information about autism to families of differing cultures; 64% (n = 679) wanted information about occupational therapy indicators of autism; and 63% (n = 670) wanted information with recommendations for the role of occupational therapy practitioners in early identification of autism.
The major findings within this section relate to how practitioners preferred to acquire information based on a variety of options presented in survey. Substantial majorities of respondents preferred acquiring information from the Internet (99%, n = 1,045); from attending professional meetings and conferences (97%, n = 1,029); from colleagues and specialists (97%, n = 1,028); and from journal articles (95%, n = 1,004). Respondents also expressed a preference for acquiring information from hard-copy products, such as brochures and fact sheets (89%, n = 939); from textbooks (84%, n = 893); and from e-mail updates, such as newsletters and e-mail lists (82%, n = 869). Lesser proportions preferred acquiring information from online networks and forums, such as podcasts, webinars, blogs, wikis, and Facebook and other social media (64%, n = 678); from preservice or university graduate-level training (48%, n = 503); or from CDC’s “Learn the Signs. Act Early.” campaign (26%, n = 279).
Section 6: Barriers to Conducting Autism Screening
The last section included items related to the occupational therapy practitioners’ perceived barriers to conducting autism-specific screenings. The major findings within this section were that 81% (n = 857) of respondents perceived lack of knowledge about autism-specific screening instruments as a barrier; 64% (n = 674) perceived a lack of skills for conducting autism-specific screening as a barrier; and 58% (n = 590) perceived state occupational therapy licensure laws–scope of practice as a barrier.
Discussion
Occupational therapy practitioners in this study reported limited use of published autism-specific screening instruments in their practice as a means of identifying early risk factors for autism. Given that surveillance alone is not the most effective method for detecting developmental delays and is associated with poor sensitivity (Rydz, Shevell, Majnemer, & Oskoui, 2005), practitioners indicated benefit from professional development focused on the identification and selection of psychometrically sound screening instruments and best practices for administering, scoring, and interpreting these instruments for children at risk for autism.
First, note that many respondents found creation of the occupational profile useful as an informal screening or surveillance method; however, they may benefit from professional development focused on defining informal screening or surveillance and training that outlines best practices for identifying risk and protective factors in children suspected of having autism. Although practitioners have unique knowledge about occupation-based evaluation instruments and appropriate use of these assessments once a child is referred to occupational therapy after an autism diagnosis, the respondents in this study revealed the need for training on the use of interdisciplinary, psychometrically sound screening instruments in conjunction with the occupational profile to assist families in referral for further evaluation.
Second, more than half of the respondents indicated that they were unfamiliar with the CDC’s “Learn the Signs: Act Early.” campaign. The purpose of this campaign is to “educate parents about childhood development, including early warning signs of autism and other developmental disorders, and [to encourage] developmental screening and intervention” (CDC, 2012). In addition, the campaign aims to support health care providers in early identification activities through provision of online resources and training. The findings from our study indicate that occupational therapy practitioners could benefit from professional development efforts that focus on improving awareness of the CDC campaign. The respondents in this study may benefit from strategies to share and disseminate information and resources with families and other professionals.
Third, regarding respondents’ perceptions about service delivery to families of children with autism, the findings suggest that practitioners could benefit from more information or resources that focus on (1) current research evidence in the field of autism; (2) screening, screening instruments, and referral processes for autism; (3) easy-to-read materials about autism for families; (4) occupational therapy evaluation procedures when autism is a concern; and (5) methods for explaining autism to culturally and linguistically diverse families. Although a notable percentage of respondents felt prepared to explain indicators of autism that have relevance to occupational therapy and felt prepared to discuss developmental milestones, they identified feeling less prepared to discuss evidence related to autism and to explain occupational therapy’s role in early identification. Early identification services fall under the realm of disease prevention and health promotion, and our findings suggest that the study respondents were less familiar with their role in health promotion or disease prevention in pediatric practice. Practitioners should be prepared to explain the role of occupational therapy in early identification and should share this information with families, other professionals, and referral sources to support early diagnosis of children with autism.
Fourth, many respondents indicated that additional information and education about the early identification of autism would be helpful. Practitioners in this study preferred methods of acquiring information such as conferences; opportunities for exposure to specialists; and expanded information about early identification within existing resources, including the AOTA Web site and autism microsite. Discussion about preservice and posteducation preparation in the early detection of autism and other disorders should take place at the national level. Early identification activities are most routinely conducted in primary care settings (i.e., pediatrician offices or family medical practices). The occupational therapy practitioner can administer assessments and interpret and communicate the results to the pediatrician while supporting the family as they make decisions about evaluations and procedures.
Metzler, Hartmann, and Lowenthal (2012) presented a compelling case for occupational therapy’s role in primary health care practice. Occupational therapy practitioners often are frontline providers of services for children with a developmental concern or delay. As a result, practitioners are in an ideal position within primary health care to assist with early identification by conducting whole-population screenings within homes, clinics, and other settings. Engagement in primary health care practice requires training and preparation for interdisciplinary and collaborative practice to occur. Although continuing education may meet some of the demand for development of these core competencies, the profession may need to consider how students are being prepared at the preservice level.
Finally, the results indicate that many practitioners in this study could benefit from professional development and continuing education opportunities that focus on specific screening instruments, including administering, scoring, interpreting, and communicating with families to ensure timely referral. Moreover, many practitioners saw a need to develop awareness about state policies that would support their role in early screening efforts. Perceived lack of knowledge about autism-specific screening instruments and perceived lack of skills were identified as considerable barriers to engagement in early identification practices. Although most respondents identified a lack of knowledge and skills as barriers, they also identified unfamiliarity with state laws and policies regarding screening as a notable barrier to early identification practices. Helping practitioners learn how they can access and interpret their respective state policies may reduce this barrier. Practitioners can address the gap in knowledge about autism-specific screening by exploring the CDC’s “Learn the Signs. Act Early.” campaign Web site, visiting the AOTA autism microsite, and attending professional development opportunities that address early identification.
Limitations
The findings of this study are limited because the respondents were self-identified and not randomly selected to participate. Although the results of this survey cannot be generalized to the larger population, the data provide some indication of current practices and needs of practitioners. In addition, the survey was administered electronically, and respondents needed to have access to a computer and a working knowledge of survey technology application to answer the questions. Finally, the blast e-mailing recruitment procedure did not allow for a calculated response rate. The study’s limitations need to be considered in the interpretation of the findings, but the results indicate that further professional development and training are needed by this group of respondents.
Recommendations for Future Research
Future research should investigate the most effective ways of disseminating information to practitioners that result in practice changes. Then this survey could be replicated to determine whether the dissemination practices were effective in changing practitioners’ knowledge, skills, and behavior.
Implications for Occupational Therapy Practice
Occupational therapy practitioners may benefit from professional development that
Provides more exposure to and discussion about evidence in the field of autism to be better prepared to share and discuss evidence with families;
Emphasizes the identification and selection of psychometrically sound screening tools to determine areas of focus when autism is suspected;
Provides training in administering, scoring, and interpreting results of assessment tools for use in family education and treatment planning;
Focuses on cultural competency and strategies to incorporate family perspectives, particularly those of culturally and linguistically diverse families, into assessment and evaluation; and
Provides strategies for accessing and sharing the CDC’s “Learn the Signs. Act Early.” campaign materials and other autism-related materials.
In addition, occupational therapy profiles are important tools and a unique contribution offered by our profession that also serve as a form of surveillance. Finally, practitioners may benefit from information and professional development to support their role in the early identification of children with autism disseminated through professional meetings and conferences, the Internet and websites, colleagues and specialists, hard-copy products (e.g., brochures, fact sheets), and journal articles.
Acknowledgments
This report was prepared under a research agreement with the American Occupational Therapy Association (AOTA) and the University of South Carolina (AOTA collaborating contact: Sandra Schefkind). It was also conducted through an AOTA partnership with the CDC; the American Physical Therapy Association; and the CDC/Association of University Centers on Disability Collaborative Research Award Recipient (Lily Nalty, University of South Carolina).
Contributor Information
Lesly W. James, Lesly W. James, PhD, OTR/L, FAOTA, is Research Assistant Professor, Department of Pediatrics, University of South Carolina, School of Medicine, Center for Disability Resources, Columbia, SC 29208; lesly.james@uscmed.sc.edu
Kris A. Pizur-Barnekow, Kris A. Pizur-Barnekow, PhD, OTR/L, is Associate Professor, Department of Occupational Science and Technology, University of Wisconsin–Milwaukee College of Health Sciences
Sandra Schefkind, Sandra Schefkind, MS, OTR, is Pediatric Coordinator, American Occupational Therapy Association, Bethesda, MD.
References
- American Academy of Pediatrics Council on Children With Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–420. doi: 10.1542/peds.2006-1231. http://dx.doi.org/10.1542/peds.2006-1231 . [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. The scope of occupational therapy services for individuals with an autism spectrum disorder across the life course. American Journal of Occupational Therapy. 2010;64(Suppl):S125–S136. doi: 10.5014/ajot.2015.696S18. http://dx.doi.org/10.5014/ajot.2010.64S125 . [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000. [Google Scholar]
- American Psychiatric Association. DSM–5 Autism spectrum disorder [Fact sheet] 2013, May. Retrieved from www.psychiatry.org/mental-health/key-topics/autism. [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR Surveillance Summaries. 2009;58:1–20. [PubMed] [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveillance Summaries. 2012;61:1–19. [PubMed] [Google Scholar]
- Baron-Cohen S., Wheelwright S., Cox A., Baird G., Charman T., Swettenham J., …, Doehring P. Early identification of autism by the CHecklist for Autism in Toddlers (CHAT) Journal of the Royal Society of Medicine. 2000;93:521–525. doi: 10.1177/014107680009301007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker D., Squires J. Ages and Stages Questionnaires: Social–Emotional (ASQ–SE): A parent-completed, child-monitoring system for social–emotional behaviors. Baltimore: Brookes; 2002. [Google Scholar]
- Bricker D., Squires J. Ages and Stages Questionnaires: A parent-completed, child-monitoring system. Baltimore: Brookes; 2009. [Google Scholar]
- Centers for Disease Control and Prevention. Metropolitan Atlanta Developmental Disabilities Surveillance Program. 2011. Retrieved from www.cdc.gov/ncbddd/dd/MADDSP.htm.
- Centers for Disease Control and Prevention. About the campaign. 2012. Retrieved from www.cdc.gov/ncbddd/actearly/about.html.
- Dawson G., Rogers S., Munson J., Smith M., Winter J., Greenson J., Varley J. Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver model. Pediatrics. 2010;125:e17–e23. doi: 10.1542/peds.2009-0958. http://dx.doi.org/10.1542/peds.2009-0958 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glascoe F. P. PEDS: Parent’s Evaluation of Developmental Status. Nashville, TN: Ellsworth & Vandermeer; 1997. [Google Scholar]
- Individuals With Disabilities Education Improvement Act of 2004, Pub. L. 108–446, 20 U.S.C. §602.
- Interactive Autism Network. IAN research findings: Treatment series. 2009. Retrieved from www.iancommunity.org/cs/ian_treatment_reports/overview.
- Krug D. A., Arick J. R., Almond P. J. Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1980;21:221–229. doi: 10.1111/j.1469-7610.1980.tb01797.x. http://dx.doi.org/10.1111/j.1469-7610.1980.tb01797.x . [DOI] [PubMed] [Google Scholar]
- Landa R. J. Diagnosis of autism spectrum disorders in the first 3 years of life. Nature Clinical Practice Neurology. 2008;4:138–147. doi: 10.1038/ncpneuro0731. http://dx.doi.org/10.1038/ncpneuro0731 . [DOI] [PubMed] [Google Scholar]
- Mandell D. S., Novak M. M., Zubritsky C. D. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116:1480–1486. doi: 10.1542/peds.2005-0185. http://dx.doi.org/10.1542/peds.2005-0185 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson J. L., Wilkins J., Gonzalez M. Early identification and diagnosis in autism spectrum disorders in young children and infants: How early is too early? Research in Autism Spectrum Disorders. 2008;2:75–84. http://dx.doi.org/10.1016/j.rasd.2007.03.002 . [Google Scholar]
- Metzler C. A., Hartmann K. D., Lowenthal L. A. Defining primary care: Envisioning the roles of occupational therapy. American Journal of Occupational Therapy. 2012;66:266–270. doi: 10.5014/ajot.2010.663001. http://dx.doi.org/10.5014/ajot.2010.663001 . [DOI] [PubMed] [Google Scholar]
- Nalty L. Involving allied health care professionals in helping parents navigate systems for ASD diagnosis. 2010. Retrieved from www.aucd.org/docs/ncbddd/rtoi/January%202011/Lily%20Nalty.pdf. [Google Scholar]
- Pizur-Barnekow K., Muusz M., McKenna C., O’Connor E., Cutler A. Service coordinators’ perceptions of autism-specific screening and referral practices in early intervention. Topics in Early Childhood Special Education. 2012;33:153–161. http://dx.doi.org/10.1177/0271121412463086 . [Google Scholar]
- Robins D., Fein D., Barton M. M-CHAT™ (Modified Checklist for Autism in Toddlers) Salt Lake City: Lineagen; 1999. [Google Scholar]
- Rutter M., Bailey A., Lord C. Social Communication Questionnaire (SCQ) Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- Rydz D., Shevell M. I., Majnemer A., Oskoui M. Topical review: Developmental screening. Journal of Child Neurology. 2005;20:4–21. doi: 10.1177/08830738050200010201. http://dx.doi.org/10.1177/08830738050200010201 . [DOI] [PubMed] [Google Scholar]
- Seigel B. Pervasive Developmental Disorders Screening Test—2nd edition (PDDST–II) San Antonio, TX: Psychological Corporation; 2004. [Google Scholar]
- Stone W. L., Ousley O. Y. STAT Manual: Screening Tool for Autism in Two-Year-Olds. 1997. Unpublished manuscript, Vanderbilt University, Nashville, TN. [Google Scholar]
- Virués-Ortega J. Applied behavior analytic intervention for autism in early childhood: Meta-analysis, meta-regression and dose–response meta-analysis of multiple outcomes. Clinical Psychology Review. 2010;30:387–399. doi: 10.1016/j.cpr.2010.01.008. http://dx.doi.org/10.1016/j.cpr.2010.01.008 . [DOI] [PubMed] [Google Scholar]
- Wetherby A. M., Prizant B. M. Communication and Symbolic Behavior Scales Developmental Profile™ (CSBS DP™) Baltimore: Brookes; 2002. [Google Scholar]
- Wetherby A., Woods J. Systematic observation of red flags for autism spectrum disorders in young children. Unpublished manual. Tallahassee: Florida State University; 2002. [Google Scholar]