Abstract
Purpose
To develop a simple risk-scoring system to forecast scrub typhus severity.
Patients and methods
Seven years’ retrospective data of patients diagnosed with scrub typhus from two university-affiliated hospitals in the north of Thailand were analyzed. Patients were categorized into three severity groups: nonsevere, severe, and dead. Predictors for severity were analyzed under multivariable ordinal continuation ratio logistic regression. Significant coefficients were transformed into item score and summed to total scores.
Results
Predictors of scrub typhus severity were age >15 years, (odds ratio [OR] =4.09), pulse rate >100/minute (OR 3.19), crepitation (OR 2.97), serum aspartate aminotransferase >160 IU/L (OR 2.89), serum albumin ≤3.0 g/dL (OR 4.69), and serum creatinine >1.4 mg/dL (OR 8.19). The scores which ranged from 0 to 16, classified patients into three risk levels: non-severe (score ≤5, n=278, 52.8%), severe (score 6–9, n=143, 27.2%), and fatal (score ≥10, n=105, 20.0%). Exact severity classification was obtained in 68.3% of cases. Underestimations of 5.9% and overestimations of 25.8% were clinically acceptable.
Conclusion
The derived scrub typhus severity score classified patients into their severity levels with high levels of prediction, with clinically acceptable under- and overestimations. This classification may assist clinicians in patient prognostication, investigation, and management. The scoring algorithm should be validated by independent data before adoption into routine clinical practice.
Keywords: severe scrub typhus, risk-scoring system, clinical prediction rule, prognostic predictors
Introduction
Scrub typhus is one of the common acute febrile illnesses encountered in tropical countries, including Thailand.1,2 The infection often causes vasculitis and multiple-organ failure.3,4 Patients with such complications usually have poor prognoses that may end with death, especially those with delayed diagnosis and treatment. Systemic complications commonly reported as causes of death include respiratory involvement (15%–36%),5–7 cardiovascular involvement (2%–34%),5,6,8,9 renal involvement (9%–20%),6,9–11 hepatic involvement (4%–31%),8,9 central nervous system involvement (4%–23%),8,12 or multiple-organ involvement (11.9%).13 Mortality is reported in up to 30% of cases.4,14
Clinical characteristics for prognostication of scrub typhus severity and death have been the subject of many studies. These characteristics may include any combinations of the following systems: respiratory system – dyspnea, crepitation, and abnormal chest film; cardiovascular system – septic shock; hepatobiliary system – serum albumin ≤3 g/dL, bilirubin >1.5 mg/dL, and more than twofold increase in aspartate aminotransferase (AST); and kidney system – serum creatinine > 1.4 mg/dL and positive urine albumin.12,15–17 Early detection of these characteristics might be used to assist clinical guidelines for patient management.
Clinical prediction rules to forecast disease severity were developed for a few infectious diseases, such as community-acquired pneumonia.18 However, there have been no studies attempting to develop a clinical risk-scoring system to forecast the severity of scrub typhus.
The present study was conducted to develop a simple clinical risk-scoring algorithm to predict the severity of scrub typhus in patients suspected of infection. The scoring system may assist routine clinical guidelines to improve patient management.
Patients and methods
This study was approved by the research ethics committees of the two hospitals in Chiang Mai and Chiang Rai, and the Faculty of Medicine at Chiang Mai University.
Patients
Retrospective data analysis was conducted at two university-affiliated general hospitals in the north of Thailand during 2004 and 2010. Patients were professionally diagnosed with scrub typhus, based on the exposure history of disease, presenting with acute fever and at least one of the following signs and symptoms: myalgia, headache, conjunctival injection, cough, profuse sweating, maculopapular rash, and lymphadenopathy,14 accompanied by the presence of eschar and/or positive immunochromatographic test for scrub typhus. Patients were classified into three groups: 1) nonsevere – patients without any complications; 2) severe – patients with severe complications; and 3) dead – those who died in hospital from scrub typhus. Patients undergoing any intervention trials during the same period were excluded from data analysis.
Definitions of severe scrub typhus
Severe scrub typhus was operationally defined as patients who presented with involvement of at least one of the following organ systems.
- Cardiovascular system – presence of any of the following:
- ○ Systolic blood pressure less than 90 mmHg
- ○ Abnormal cardiac arrhythmia with no previous history of
- § atrial fibrillation (AF),
- § supra ventricular tachycardia (SVT), or
- § frequent premature ventricular tachycardia (PVC)
- ○ Myocarditis: elevated creatine kinase MB above baseline
Respiratory system: presence of acute respiratory distress syndrome, defined as PaO2/FiO2 <200 mmHg, with bilateral interstitial infiltration on chest film with normal cardio/thoracic ratio, or no volume overload of central venous pressure from central venous catheter
- Central nervous system – presence of any of the following:
- ○ Glasgow Coma Scale ≤12 without other causes,
- ○ Seizure without other causes, or
- ○ Meningoencephalitis
Hematology: platelet count ≤20,000/mm3
Urinary tract: presence of acute renal failure, defined as creatinine ≥2 mg/dL or creatinine change >0.5 mg/dL/day
Gastrointestinal and hepatobiliary tract: presence of hepatitis, defined as elevated AST or alanine aminotransferase (ALT) more than fivefold.
Predictor parameters
Demographic and disease-exposure histories were obtained from medical files recorded at the time of admission: sex, age, underlying diseases (liver cirrhosis, chronic obstructive pulmonary disease, hypertension, diabetes, and human immunodeficiency virus infection), durations of fever.
Signs and symptoms were obtained from chief complaint, history-taking records, and physical examination notes: myalgia, headache, conjunctival injection, cough, maculopapular rash, eschar, lymphadenopathy, abdominal pain, nausea/vomiting, diarrhea, jaundice, hepatomegaly, splenomegaly, seizure, stiff neck, wheezing, crepitation, dyspnea, respiration rate, and presence of fever.
Hemodynamic profiles were obtained from vital-sign record forms: systolic and diastolic blood pressure and pulse rate. Laboratory profiles were obtained from laboratory investigations requested within 24 hours after admission: hematological, biochemistry, urine analyses.
Data analysis
Patient clinical characteristics were compared across the three severity groups by nonparametric trend tests across ordered groups. Strong potential predictors were explored by multivariable ordinal continuation ratio logistic regression (α<0.001). The coefficients of significant predictors were transformed into item scores and summed as scrub typhus severity scores. The scores were classified into risk levels based on inclining of actual risks. Score-categorized risk levels were compared to criterion risk levels to indicate the score performances.
Results
A total of 526 patients with document-confirmed professional diagnosis of scrub typhus were retrieved; 215 cases presented with only eschar, 227 cases had positive immunochromatographic test for scrub typhus, and 84 cases had shown both. These patients were classified as nonsevere scrub typhus (n=357), severe scrub typhus (n=100), and dead of scrub typhus (n=69). The majority of patients were males with similar underlying diseases and durations of fever, but were different according to age (Table 1).
Table 1.
Patient profiles (n=526)
| Characteristics | Nonsevere (n=357) n (%) | Severe (n=100) n (%) | Dead (n=69) n (%) | P-value |
|---|---|---|---|---|
| Demographics and history | ||||
| Male | 201 (56.3) | 55 (55.0) | 35 (50.7) | 0.413 |
| Age (years), median (IQR) | 17.0 (7.0–42.0) | 31.5 (12.5–50.0) | 46.0 (34.0–64.0) | <0.001 |
| Underlying diseases | 30 (8.4) | 14 (14.0) | 8 (11.6) | 0.186 |
| Durations of fever (days), median (IQR) | 6 (4–7) | 7 (4–7) | 7 (4–7) | 0.961 |
| Signs and symptoms | ||||
| Myalgia | 69 (19.3) | 23 (23.0) | 13 (18.8) | 0.820 |
| Headache | 117 (32.8) | 29 (29.0) | 14 (20.3) | 0.041 |
| Conjunctival injection | 330 (92.4) | 90 (90.0) | 64 (92.8) | 0.823 |
| Cough | 120 (33.6) | 32 (32.0) | 17 (24.6) | 0.172 |
| Maculopapular rash | 324 (90.8) | 95 (95.0) | 66 (95.7) | 0.086 |
| Eschar | 192 (53.8) | 60 (60.0) | 38 (55.1) | 0.557 |
| Lymphadenopathy | 237 (66.4) | 73 (73.0) | 63 (91.0) | <0.001 |
| Abdominal pain | 118 (33.1) | 35 (35.0) | 25 (36.2) | 0.565 |
| Nausea/vomiting | 83 (23.3) | 27 (27.0) | 12 (19.4) | 0.544 |
| Diarrhea | 60 (16.8) | 25 (25.0) | 17 (24.6) | 0.047 |
| Jaundice | 11 (3.1) | 21 (21.0) | 17 (24.6) | <0.001 |
| Hepatomegaly | 113 (31.7) | 36 (36.0) | 14 (20.3) | 0.198 |
| Splenomegaly | 40 (11.2) | 9 (9.0) | 4 (5.8) | 0.157 |
| Seizure | 4 (1.1) | 10 (10.0) | 12 (17.4) | <0.001 |
| Stiff neck | 6 (1.7) | 4 (4.0) | 4 (5.8) | 0.032 |
| Wheezing | 2 (0.6) | 6 (6.0) | 7 (10.1) | <0.001 |
| Crepitation | 13 (3.6) | 18 (18.0) | 25 (36.2) | <0.001 |
| Dyspnea | 7 (1.9) | 7 (7.0) | 25 (36.2) | <0.001 |
| Respiration (/min), median (IQR) | 20 (20–26) | 22 (20–32) | 22 (20–26) | 0.058 |
| Body temperature (°C), median (IQR) | 38.5 (37.5–39.4) | 37.8 (37.0–38.8) | 37.2 (37.0–38.0) | <0.001 |
| Hemodynamic profiles | ||||
| SBP (mmHg), median (IQR) | 100 (100–110) | 95 (80–110) | 100 (80–110) | <0.001 |
| DBP (mmHg), median (IQR) | 60 (60–70) | 60 (50–70) | 60 (50–70) | <0.001 |
| Pulse (/min), median (IQR) | 100 (86–120) | 100 (89–115) | 102 (90–124) | 0.049 |
Note:P-values from nonparametric trend test across ordered groups.
Abbreviations: IQR, interquartile range; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Clinical signs and symptoms were similar for myalgia, conjunctival injection, cough, abdominal pain, nausea/vomiting, maculopapular rash, eschar, hepatomegaly, splenomegaly, and respiration rate. Those that were different were headache, diarrhea, jaundice, lymphadenopathy, seizure, stiff neck, wheezing, crepitation, dyspnea, body temperature, systolic blood pressure, diastolic blood pressure, and pulse rate (Table 1).
Similar laboratory results included hematocrit, hemoglobin, serum globulin, potassium, and chloride. Differences were detected on white blood cell (WBC) count, platelets, neutrophils, lymphocytes, monocytes, total bilirubin, direct bilirubin, albumin, AST, ALT, alkaline phosphatase, blood urea nitrogen creatinine, blood sodium, carbon dioxide, urine albumin levels, and urine sugar (Table 2). There were some missing data, as indicated in the corresponding tables.
Table 2.
Laboratory profiles (n=526)
| Characteristics | Nonsevere (n=357) Median (IQR) |
Severe (n=100) Median (IQR) |
Dead (n=69) Median (IQR) |
P-value |
|---|---|---|---|---|
| Hematological | ||||
| Hemoglobin, g/dL | 12.0 (10.7–13.3) | 11.6 (10.4–12.9) | 12.1 (10.2–14.1) | 0.999 |
| Hematocrit, % | 35.8 (31.8–39.6) | 34.0 (30.4–38.8) | 36.4 (30.6–42.1) | 0.805 |
| Platelet count, ×1,000/mm3 | 117.0 (72.0–196.0) | 72.0 (42.5–143.5) | 50.0 (2.8–85.8) | <0.001 |
| WBC count, ×1,000/mm3 | 7.7 (5.5–11.2) | 10.45 (7.5–6.0) | 12.0 (8.8–6.1) | <0.001 |
| Neutrophils (%) | 68.0 (56.0–79.8) | 82.8 (68.3–88.1) | 84.0 (75.7–89.0) | <0.001 |
| Lymphocytes (%) | 22.0 (13.0–33.8) | 11.1 (6.8–20.0) | 8.1 (4.9–14.9) | <0.001 |
| Monocytes (%) | 6.0 (3.0–8.6) | 3.8 (2.0–6.0) | 3.4 (2.0–6.0) | <0.001 |
| Biochemistry | ||||
| Total bilirubin (mg/dL) | 0.7 (0.5–1.3) | 2.4 (0.8–5.7) | 4.4 (2.4–6.6) | <0.001 |
| Direct bilirubin (mg/dL) | 0.2 (0.1–0.5) | 1.1 (0.2–3.1) | 2.7 (1.5–4.4) | <0.001 |
| Albumin (g/dL) | 3.2 (2.7–3.6) | 2.7 (2.3–3.0) | 2.4 (2.1–3.0) | <0.001 |
| Globulin (g/dL) | 3.3 (2.8–3.7) | 3.0 (2.7–3.4) | 3.2 (2.7–3.9) | 0.199 |
| ALT (IU/L) | 67.0 (38.0–112.5) | 86.5 (47.0–158.0) | 99.5 (51.0–146.5) | <0.001 |
| AST (IU/L) | 103.0 (61.5–179.0) | 174.5 (77.0–300.0) | 274.0 (128.5–403.0) | <0.001 |
| ALP (IU/L) | 165.5 (120.5–267.5) | 27.6 (141.0–416.0) | 243.0 (128.0–342.0) | <0.001 |
| BUN (mg/dL) | 12.0 (9.0–17.0) | 31.0 (14.0–54.0) | 55.5 (27.0–72.0) | <0.001 |
| Creatinine (mg/dL) | 0.9 (0.7–1.2) | 1.4 (0.9–2.5) | 2.5 (1.5–5.0) | <0.001 |
| Na (mmol/L) | 134 (131–137) | 133 (129–136) | 132 (129–137) | 0.034 |
| K (mmol/L) | 3.5 (3.2–3.9) | 3.6 (3.2–3.8) | 3.7 (3.2–4.3) | 0.060 |
| Cl2 (mmol/L) | 101 (98–104) | 102 (97–104) | 100 (97–105) | 0.365 |
| CO2 (mmol/L) | 23 (20–25) | 20 (17–23) | 16 (12–20) | <0.001 |
| Urine analysis | ||||
| Urine albumin, n (%) | ||||
| <1+ | 190 (64.0) | 40 (47.1) | 12 (19.7) | <0.001 |
| ≥1+ | 107 (36.0) | 45 (52.9) | 49 (80.3) | |
| Urine sugar, n (%) | ||||
| <1+ | 292 (98.3) | 84 (98.8) | 59 (96.7) | 0.535 |
| ≥1+ | 5 (1.7) | 1 (1.2) | 2 (3.3) | |
Abbreviations: IQR, interquartile range; WBC, white blood cell; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; BUN, blood urea nitrogen.
Significant predictors
Multivariable significant (P<0.001) predictors for severity were age >15 years (odds ratio [OR] 4.09, 95% confidence interval [CI] 2.26–7.40), pulse rate >100/minute (OR 3.19, 95% CI 1.87–5.43), crepitation (OR 2.97, 95% CI 1.63–5.39), AST >160 IU/L (OR 2.89, 95% CI 1.89–4.43), serum albumin ≤3.0 g/dL (OR 4.69, 95% CI 2.95–7.45), and serum creatinine >1.4 mg/dL (OR 8.19, 95% CI 5.06–13.35) (Table 3). Multicollinearity among variables was tested and was insignificant.
Table 3.
Significant predictors and assigned item score
| Predictors | Category | OR | 95% CI | P-value | Coefficient | Score |
|---|---|---|---|---|---|---|
| Age (years) | >15 | 4.09 | 2.26–7.40 | <0.001 | 1.41 | 3 |
| ≤15 | Ref | |||||
| Pulse rate (/min) | >100 | 3.19 | 1.87–5.43 | <0.001 | 1.16 | 2 |
| ≤100 | Ref | |||||
| Crepitation | Yes | 2.97 | 1.63–5.39 | <0.001 | 1.09 | 2 |
| No | Ref | |||||
| AST (IU/L) | >160 | 2.89 | 1.89–4.43 | <0.001 | 1.06 | 2 |
| ≤160 | Ref | |||||
| Serum albumin (g/dL) | ≤3.0 | 4.69 | 2.95–7.45 | <0.001 | 1.55 | 3 |
| >3.0 | Ref | |||||
| Serum creatinine (mg/dL) | >1.4 | 8.19 | 5.06–13.25 | <0.001 | 2.10 | 4 |
| ≤1.4 | Ref | |||||
Notes: Coefficients from multivariable ordinal continuation ratio logistic regression.
Abbreviations: OR, odds ratio; CI, confidence interval; AST, aspartate aminotransferase.
The scoring system
Item scores were derived by dividing the coefficient of significant predictors with the smallest coefficient (1.06) and rounding up to the nearest discrete number. The item scores varied from the minimum of 0 to the maximum of 4. Each item scores were summed up to total scrub typhus severity score, which may vary from 0 to 16 (Table 3).
Discrimination
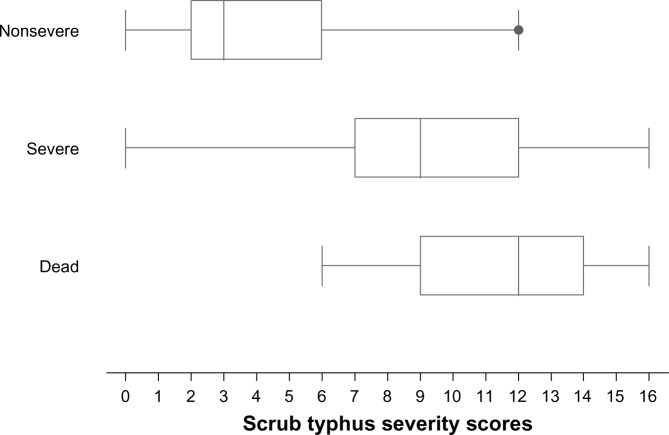
The mean severity scores in the nonsevere, severe, and dead groups were 4.2±2.5, 8.9±3.1, and 11.4±2.8 (Table 4 and Figure 1).
Table 4.
Score-classified severity levels, criterion-classified severity levels, and risk-estimation validity
| Score-classified severity levels | Score range | Criterion-classified severity levels
|
Risk-estimation validity*
|
||||
|---|---|---|---|---|---|---|---|
| Nonsevere n=357 | Severe n=100 | Dead n=69 | Over (%) | Correct (%) | Under (%) | ||
| Mean ± SD | 4.2±2.5 | 8.9±3.1 | 11.4±2.8 | ||||
| IQR | 2–6 | 7–12 | 9–14 | ||||
| Nonsevere (n=278) | ≤5 | 266 | 12 | 0 | – | 50.6 | 2.3 |
| Severe (n=143) | 6–9 | 81 | 43 | 19 | 15.4 | 8.2 | 3.6 |
| Fatal (n=105) | ≥10 | 10 | 45 | 50 | 10.4 | 9.5 | – |
| Total | 25.8 | 68.3 | 5.9 | ||||
Note:
Percentage of total patients.
Abbreviations: SD, standard deviation; IQR, interquartile range.
Figure 1.
Distribution of scrub typhus severity scores.
Clinical predictions
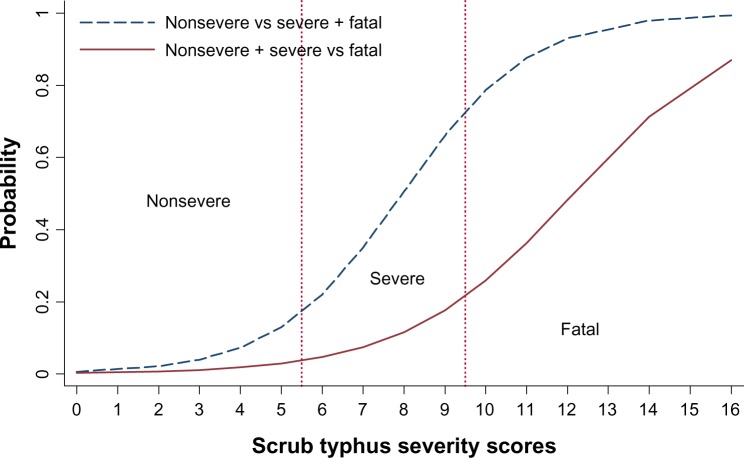
The scores discriminated patients with severe or fatal scrub typhus from those with nonsevere scrub typhus with highlevel validity (area under receiver operating characteristic curve (AuROC) 0.9148, 95% CI 0.8886–0.9410). The corresponding values for discriminating the fatal from the severe and nonsevere groups were lower (AuROC 0.9122, 95% CI 0.8823–0.9420) (Figure 2).
Figure 2.
Discrimination of severity based on scrub typhus severity scores.
By classifying the severity scores into three risk levels – nonsevere (scores ≤ 5), severe (scores 6–9), and most severe or fatal (scores ≥10) – the scores classified 266 out of 357 patients correctly in the nonsevere group, with underestimation by one level in twelve cases and no instances of underestimation by two levels. In the severe group, the score classified correctly 43 out of 100 patients, with 19 cases underestimated and 81 cases overestimated. In the dead group, classification was correct in 50 out of 69 cases, with overestimation by one level in 45 cases and overestimation by two levels in ten cases (Table 4).
Discussion
Although patients with early and nonsevere scrub typhus usually respond very well to prompt treatment, patients with complications have a poorer prognosis, and the disease may well be fatal for them. Researchers have attempted to develop scoring systems to predict infectious diseases or their severity to help clinical management. Examples were a dengue fever scoring system to differentiate dengue fever from rickettsial and Q fever, which was developed in Taiwan,19 decision-tree algorithms to differentiate and prognosticate dengue hemorrhagic fever,20 and a prediction rule to evaluate the risk for community-acquired pneumonia to help admission decisions.18 These prediction rules used parameters of epidemiologic, demographic, clinical signs and symptoms, or laboratory characteristics. They all shared similar limitations of relatively large numbers of parameters, complicated laboratory tests beyond routine investigations, or tests that may be unavailable in many settings. These restrictions limited clinical application in routine practice.
For scrub typhus, there have been no studies attempting to develop a clinical algorithm to forecast disease severity to assist clinical diagnosis, evaluation, or management. The present study proposed a simple scoring system based on routinely clinical parameters available in most health care settings.
Predictors proposed in this study were more or less similar to what have been proposed in previous studies, such as serum albumin ≤3 g/dL21 and serum creatinine >1.4 mg/dL.17 Some parameters were similar but different in categorization, such as the patient age21,22 and AST level.17 Some parameters were reported but were not significant in the present study, such as WBC count,17 platelets,17 and bilirubin.17
The present scrub typhus severity score, which ranged from 0 to 16 could be classified into three levels to simulate three levels of disease severities. We proposed the following interpretations and guidelines.
Patients scoring 0–5 were categorized as “nonsevere scrub typhus”. These patients may be managed as outpatients. Antirickettsial agents like doxycycline, chloramphenicol, or azithromycin should be prescribed23,24 and scheduled for follow-up.
Patients scoring 6–9 were categorized as “severe scrub typhus”. These patients are at higher risk of complications, and should be admitted to hospital for close observation. Further investigation and additional intervention may be needed. Patients encountered in lower-level hospitals might be referred to better-equipped hospitals.
Patients scoring 10 or above were classified as “fatal scrub typhus”. These patients experienced the highest risk of death and should be fully investigated for system abnormalities or other life-threatening clinical risks, and should be admitted to an intensive care unit for close monitoring.
An overestimation (25.8%) in the nonsevere group may have resulted in overzealous case management, but this may be considered beneficial for patients. Underestimation was observed in 3.6% of patients with severe scrub typhus. However, the same antirickettsial agents were routinely prescribed in these patients, and the clinical risk should therefore be considered acceptable.
The diagnosis of scrub typhus in the present study was defined as suspected cases based on World Health Organization criteria. This is the most practical definition used in poor, developing countries, where definite diagnosis like indirect immunofluorescence antibodies was hardly available in routine practice. We (the authors) believe that this definition, although not definite, is more relevant in the real world.
The present scoring system, like any other clinical prediction rules, should be validated by independent data before application to routine clinical practice.
Conclusion
The derived scrub typhus severity score classified patients into their severity levels with high levels of prediction, with clinically acceptable under- and overestimations. This classification may assist clinicians in patient prognostication, investigation, and management. Like other clinical prediction rules, the present scoring algorithm needs to be validated by independent data before being adopted into routine clinical practice.
Acknowledgments
The authors wish to thank the authorities of the two hospitals for their support. The study was partially funded by a grant from The Graduate School of Chiang Mai University, Chiang Mai, Thailand.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Leelarasamee A, Chupaprawan C, Chenchittikul M, Udompanthurat S. Etiologies of acute undifferentiated febrile illness in Thailand. J Med Assoc Thai. 2004;87(5):464–472. [PubMed] [Google Scholar]
- 2.Suttinont C, Losuwanaluk K, Niwatayakul K, et al. Causes of acute, undifferentiated, febrile illness in rural Thailand: results of a prospective observational study. Ann Trop Med Parasitol. 2006;100(4):363–370. doi: 10.1179/136485906X112158. [DOI] [PubMed] [Google Scholar]
- 3.Moron CG, Popov VL, Feng HM, Wear D, Walker DH. Identification of the target cells of Orientiatsutsugamushi in human cases of scrub typhus. Mod Pathol. 2001;14(8):752–759. doi: 10.1038/modpathol.3880385. [DOI] [PubMed] [Google Scholar]
- 4.Watt G, Kantipong P. Orientia tsutsugamushi and scrub typhus. In: Ruoult D, Parola P, editors. Rickettsial Diseases. New York: Information Healthcare; 2007. pp. 236–256. [Google Scholar]
- 5.Jeong YJ, Kim S, Wook YD, Lee JW, Kim KI, Lee SH. Scrub typhus: clinical, pathologic, and imaging findings. Radiographics. 2007;27(1):161–172. doi: 10.1148/rg.271065074. [DOI] [PubMed] [Google Scholar]
- 6.Tsay RW, Chang FY. Serious complications in scrub typhus. J Microbiol Immunol Infect. 1998;31(4):240–244. [PubMed] [Google Scholar]
- 7.Wang CC, Liu SF, Liu JW, Chung YH, Su MC, Lin MC. Acute respiratory distress syndrome in scrub typhus. Am J Trop Med Hyg. 2007;76(6):1148–1152. [PubMed] [Google Scholar]
- 8.Chanta C, Triratanapa K, Ratanasirichup P, Mahaprom W. Hepatic dysfunction in pediatric scrub typhus: role of liver function test in diagnosis and marker of disease severity. J Med Assoc Thai. 2007;90(11):2366–2369. [PubMed] [Google Scholar]
- 9.Kumar M, Krishnamurthy S, Delhikumar CG, Narayanan P, Biswal N, Srinivasan S. Scrub typhus in children at a tertiary hospital in southern India: clinical profile and complications. J Infect Public Health. 2012;5(1):82–88. doi: 10.1016/j.jiph.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Rathi N, Rathi A. Rickettsial infections: Indian perspective. Indian Pediatr. 2010;47(2):157–164. doi: 10.1007/s13312-010-0024-3. [DOI] [PubMed] [Google Scholar]
- 11.Yen TH, Chang CT, Lin JL, Jiang JR, Lee KF. Scrub typhus: a frequently overlooked cause of acute renal failure. Ren Fail. 2003;25(3):397–410. doi: 10.1081/jdi-120021152. [DOI] [PubMed] [Google Scholar]
- 12.Jim WT, Chiu NC, Chan WT, et al. Clinical manifestations, laboratory findings and complications of pediatric scrub typhus in eastern Taiwan. Pediatr Neonatol. 2009;50(3):96–101. doi: 10.1016/S1875-9572(09)60043-7. [DOI] [PubMed] [Google Scholar]
- 13.Suputtamongkol Y, Suttinont C, Niwatayakul K, et al. Epidemiology and clinical aspects of rickettsioses in Thailand. Ann NY Acad Sci. 2009;1166:172–179. doi: 10.1111/j.1749-6632.2009.04514.x. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization WHO recommended surveillance standards. [Accessed October 5, 2011]. Available from: http://www.who.int/csr/resources/publications/surveillance/whocdscsrisr992.pdf.
- 15.Lee CS, Hwang JH, Lee HB, Kwon KS. Risk factors leading to fatal outcome in scrub typhus patients. Am J Trop Med Hyg. 2009;81(3):484–488. [PubMed] [Google Scholar]
- 16.Thap LC, Supanaranond W, Treeprasertsuk S, Kitvatanachai S, Chinprasatsak S, Phonrat B. Septic shock secondary to scrub typhus: characteristics and complications. Southeast Asian J Trop Med Public Health. 2002;33(4):780–786. [PubMed] [Google Scholar]
- 17.Varghese GM, Abraham OC, Mathai D, et al. Scrub typhus among hospitalised patients with febrile illness in South India: magnitude and clinical predictors. J Infect. 2006;52(1):56–60. doi: 10.1016/j.jinf.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 19.Chang K, Lu PL, Ko WC, et al. Dengue fever scoring system: new strategy for the early detection of acute dengue virus infection in Taiwan. J Formos Med Assoc. 2009;108(11):879–885. doi: 10.1016/S0929-6646(09)60420-4. [DOI] [PubMed] [Google Scholar]
- 20.Tanner L, Schreiber M, Low JGH, et al. Decision tree algorithms predict the diagnosis and outcome of dengue fever in the early phase of illness. PLoS Negl Trop Dis. 2008;2(3):e196. doi: 10.1371/journal.pntd.0000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim DM, Kim SW, Choi SH, Yun NR. Clinical and laboratory findings associated with severe scrub typhus. BMC Infect Dis. 2010;10:108. doi: 10.1186/1471-2334-10-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu KM, Wu ZW, Peng GQ, Wu JL, Lee SY. Radiologic pulmonary findings, clinical manifestations and serious complications in scrub typhus: experiences from a teaching hospital in eastern Taiwan. Int J Gerontol. 2009;3(4):223–232. [Google Scholar]
- 23.Chrispal A, Boorugu H, Gopinath KG, et al. Scrub typhus: an unrecognized threat in South India – clinical profile and predictors of mortality. Trop Doct. 2010;40(3):129–133. doi: 10.1258/td.2010.090452. [DOI] [PubMed] [Google Scholar]
- 24.Suputtamongkol Y. Scrub typhus; Poster presented at: 13th International Congress on Infectious Diseases; June 19–22, 2008; Kuala Lumpur, Malaysia. [Google Scholar]