Abstract
Background
High average daily consumption of alcohol has been associated with elevated mortality risk, but more moderate consumption, relative to abstinence, has been associated with reduced mortality risk. However, average daily consumption can be complicated to assess, limiting its usefulness both in research and clinical practice. There are also concerns that average consumption fails to capture the risk associated with certain drinking patterns, such as heavy episodic drinking. The current study assessed mortality associated with drinking pattern, operationalized as the frequency of both heavy and non-heavy drinking occasions.
Methods
Data from the 1997 – 2001 administrations of the National Health Interview Survey (NHIS; n = 128 203) were paired with the current release of the NHIS Linked Mortality Files, which provided mortality follow-up data through the end of 2006. We estimated the impact of drinking pattern on all-cause mortality, operationalized as the frequency of heavy (5+ drinks) and non-heavy (less than 5 drinks) drinking occasions. Other covariates in the model included survey wave, sex, age, race/ethnicity, ratio of family income to poverty threshold, educational attainment, BMI and smoking status.
Results
Over a third of past-year drinkers reported heavy drinking. Mortality risk increased steadily as heavy drinking frequency increased; daily heavy drinkers exhibited an almost two-fold risk of death compared to abstainers (p < 0.001). Regular non-heavy drinking was associated with decreased mortality, similar to the “J-shaped curve” highlighted in past research on alcohol mortality; this potential protective effect peaked around 2 non-heavy occasions per week.
Conclusions
Any heavy drinking likely elevates mortality risk, and substantial health benefits could be realized by reducing heavy drinking occasions or limiting overall drinking. Heavy and non-heavy drinking frequency are valid targets for clinical screening and could be helpful in assessing risk and promoting less harmful drinking behavior.
Keywords: Alcohol-related mortality, drinking pattern, binge drinking, moderate drinking
Introduction
High average daily consumption of alcohol has been associated with elevated mortality risk, but more moderate consumption, relative to abstinence, is associated with reduced risk, both for all-cause (Bagnardi, Zambon, Quatto, & Corrao, 2004) and cardiovascular mortality (Costanzo, Di Castelnuovo, Donati, Iacoviello, & de Gaetano, 2010). A meta-analysis demonstrated that this apparent protective effect peaks at around 1 to 2 drinks per day, but that slightly higher average levels of daily consumption, around 4 drinks for men and 2 for women, are associated with increased mortality risk (Di Castelnuovo et al., 2006). The relationship between average dosing and mortality risk is commonly visualized as a J-shaped curve, whereby risk is plotted against average drinks per day—risk is reduced with light consumption compared to abstention, followed by a steep increase as the average daily dose increases.
Average daily consumption has several limitations, both for screening in research and clinical practice. Establishing average consumption could require a timeline follow-back covering recent time periods, necessitating that respondents recall specific drinking quantities and the days on which they occurred (Sobell, Maisto, Sobell, & Cooper, 1979). More importantly, average consumption does not fully capture individual differences in drinking patterns, both potentially underestimating risk for people who infrequently drink heavily, and mischaracterizing the protective effect associated with more moderate consumption (Roerecke & Rehm, 2010). For example, an individual who consumes 7 drinks twice each weekend would likely be at much higher risk for alcohol-related morbidity and mortality than another who consistently consumes 2 drinks every day, despite consuming similar amounts on average.
A variety of drinking patterns have been studied in relation to mortality, including overall drinking frequency (Mukamal et al., 2003), drinking primarily with meals (Stranges et al., 2004), drinking more than once per day (Britton & Marmot, 2004), drinking on weekends (Mørch, Johansen, Løkkegaard, Hundrup, & Grønbæk, 2007), and average consumption at different levels of drinking frequency (Baglietto, English, Hopper, Powles, & Giles, 2006). Although these drinking patterns capture a range of behaviors, those that show a consistent association with decreased risk primarily involve drinking frequency at low to moderate levels (McElduff & Dobson, 1997; Mukamal et al., 2003; Kerr, Greenfield, Bond, Ye, & Rehm, 2011), while increased risk is typically tied to binge or other heavy drinking (Murray et al., 2002). Additionally, many studies have observed differences in alcohol-related mortality risk based on demographic group for designs using both average consumption and drinking pattern; for example, based on sex (Bagnardi et al., 2004; Di Castelnuovo et al., 2006) and race/ethnicity (Kerr et al., 2011).
In contrast to research on average daily intake, studies investigating the impact of drinking pattern have had difficulty consistently demonstrating simultaneously both an increased risk associated with heavy drinking and a protective association with more moderate consumption (Roerecke & Rehm, 2010). Studies that have demonstrated a protective effect typically feature complex categorizations of drinking pattern based on several variables, such as drinking frequency, average drinks per day and heavy drinking status (e.g., Kerr et al., 2011; Mukamal, Chen, Rao, & Breslow, 2010; Breslow & Graubard, 2008). Though precise, this complexity makes categorizing individuals based on drinking pattern more difficult and likely limits clinical applicability. In the current study, we investigate a simplified concept of drinking pattern operationalized as the frequency of both heavy and non-heavy drinking occasions. We define heavy drinking as any occasion in which an individual consumes 5 or more drinks, a construct which is intended to capture a short-term drinking pattern that raises one’s blood alcohol to 0.08 or above (National Institute of Alcohol Abuse and Alcoholism, 2004). Conversely, we use non-heavy drinking to refer to drinking occasions in which heavy drinking did not occur, and calculated this value by subtracting heavy drinking frequency from overall drinking frequency. Non-heavy drinking does not necessarily correspond to “moderate” drinking at the level associated with the largest reductions in mortality risk seen in previous work, but still offers a simple way to assess drinking behavior at quantities well below those of typical heavy drinking episodes (Kanny, Liu, Brewer, Garvin, & Balluz, 2012).
Non-heavy and heavy drinking frequency are straightforward to assess and there are also large amounts of epidemiological reference data available. In the U.S., a number of surveys regularly include items assessing both drinking frequency and heavy drinking frequency, including the Behavioral Risk Factor Surveillance System, the National Survey on Drug Use and Health, and the National Health Interview Survey (Centers for Disease Control and Prevention, 2009; National Center for Health Statistics, 2011; RTI International, 2009). The availability and usefulness of these constructs will likely also increase; there have been recommendations to simplify screening for problematic drinking using the abbreviated AUDIT-C, which assesses drinking frequency, typical amount per day and frequency of drinking 6+ drinks (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), or single-question screening, such as, “How many times in the past year have you had five [for men] or four [for women and all adults older than age 65 years] or more drinks in a day?” (U.S. Preventive Services Task Force, 2012).
We utilized data from the National Health Interview Survey (NHIS) for the years 1997 through 2001, providing a large sample (n = 111,511) representative of the non-institutionalized, adult population of the United States. Alcohol use data from the NHIS for eligible respondents were paired with the NHIS Linked Mortality Files to determine all-cause mortality through 2006. The size of this sample also allows us to investigate differences in mortality based on demographic group, specifically race/ethnicity, sex and age cohort.
Methods
Subjects
Data from the 1997 – 2001 administrations of the National Health Interview Survey (NHIS) were merged to examine the relationship of drinking pattern variables to mortality. The NHIS is an ongoing survey, representative of the civilian, non-institutionalized, household population of the U.S. The waves analyzed here were administered by field interviewers trained by the U.S. Census Bureau using computer-assisted personal interview technology. The 1995 – 2005 administrations used the same sampling design, drawn from 358 county-level primary sampling units across all 50 states and included oversampling of Blacks and Hispanics (Moriarity, 2006). Household response rates for these years averaged 89.1% while individual response rates averaged 74.0%. The last major content revision was in 1997 (National Center for Health Statistics, 2002, 2011); we began with that year to ensure consistent operationalization of our independent variables and 2001 served as the final data year so that at least five years had passed for all subjects prior to the final mortality linkage that occurred in 2006.
NHIS Linked Mortality Files use probabilistic matching of death certificate data found in the National Death Index (NDI), a central database of death record information contributed by each state. NHIS records are submitted for matching to the NDI on the basis of fourteen identifying variables. There are seven potential combinations of identifiers that serve as pre-specified inclusion criteria for match attempts (e.g., social security number, full date of birth, and sex). Records not meeting these criteria are coded as “indeterminate” with regard to mortality status. Suitable NHIS records are then scored probabilistically and ranked to determine the true match (National Center for Health Statistics, 2009). Linked mortality data can also originate from the Social Security Administration and Centers for Medicare and Medicaid Services (National Center for Health Statistics, 2010), but only a small portion of the mortality records in our sample did not originate from the NDI (n = 31; 0.02%).
Alcohol-related variables and covariates
The NHIS adult interview assessed whether respondents had consumed at least 12 drinks in their lifetime; those who reported not meeting this threshold were classified as lifetime abstainers. Those who reported lifetime drinking, but not having drank in the past-year were classified as past-year abstainers, which was included as a covariate to address the potential “sick quitter” effect, whereby ex-drinkers in poor health are thought by some researchers to have biased previous work on the protective effect of more moderate drinking (Connor, 2006). Those who drank at least 12 drinks in their lifetime and any in the past year were considered past-year drinkers and were further characterized by their responses to two items assessing alcohol consumption. These included number of days in the past week in which any alcohol was consumed (drinking days) and the number of days in which 5 or more drinks were consumed (heavy drinking days; this item assessed drinking at the 5+ threshold for both men and women). The original NHIS items allowed respondents to choose the time period for which they were answering (i.e., week, month or year); these were converted to week for each item if they were not already in that format (i.e., by dividing by 4.34 for month and 52.18 for year). For our primary analyses, we assessed the degree to which mortality status at follow-up was associated with the frequency of both heavy and non-heavy drinking, the latter calculated as the difference between total drinking days and heavy drinking days. The alcohol variables included in our primary analyses are as follows:
Past-year abstainer status (had consumed 12+ drinks in lifetime, but none in past year)
Heavy drinking days (number of days in which 5+ drinks were consumed)
Non-heavy drinking days (total number of drinking days minus heavy drinking days)
For comparison, we also calculated average daily consumption for each respondent using overall drinking frequency and average drinks per drinking day, but this value was not used in our main analyses.
Covariates included survey wave, sex, age cohort, race/ethnicity, categorical ranking of ratio of family income to poverty threshold, educational attainment, BMI, smoking status, census region and self-reported health status. Age cohort was categorized as 18-30, 31-40, 41-50, 51-60 and over 60. Race/ethnicity was coded as non-Hispanic White, non-Hispanic Black, Hispanic, and other race/ethnicity. Educational attainment was coded as having: (a) less than a high school education, (b) some high school, (c) high school diploma or GED, (d) some college, but no degree, and (e) any college degree. Separate dummy variables were used to classify respondents as current smokers and former smokers. BMI was calculated based on self-reported height and weight. There were 4 census regions: Northeast, North Central/Midwest, South and West. The health status item in the NHIS allowed respondents to endorse one of 5 levels: excellent, very good, good, fair and poor. Preliminary analyses showed that poor health status had the largest impact on mortality and in subsequent models a dummy variable denoting poor health status was used.
Model development
Our core analyses assessed the relationship between all-cause mortality and alcohol consumption frequency and other covariates using a stratified Cox-proportional hazards model implemented in version 2.15 of the statistical language R (R Development Core Team, 2012). Preliminary analyses did not demonstrate a statistical difference between survey design or model-based specifications; our subsequent analyses utilized a model-based approach due to the potential loss of precision accompanied by the use of survey design variables in an appropriately specified model (Lumley, 2010).
We controlled for age at entry by stratifying and allowing baseline hazard function to vary by age cohort, which serves as a viable alternative to using age as time scale to control for potential age effects (Pencina, Larson, & D’Agostino, 2007). This method also gave us the ability to easily estimate age cohort interactions by heavy and non-heavy drinking frequency. We also stratified by former drinking status to further control for the potential sick quitter effect. Allowing baseline hazard to differ by stratum yields different survival curves for each group, but coefficients, and resulting hazard ratios, will remain the same. Stratified groups can also exhibit completely different hazard ratios; interaction terms are used to test for statistical differences between groups based on strata (Hosmer, Lemeshow, & May, 2008; Kleinbaum & Klein, 2012).
Residual plots from our preliminary modeling and screening suggested that it was reasonable to assume linearity for heavy drinking frequency; this was not the case for non-heavy drinking frequency and BMI, which we allowed to exhibit non-linear effects through the use of restricted cubic splines (Harrell, 2001; Bagnardi et al., 2004). Following the recommendation of Harrell (2001), number of knots was chosen based on the relative importance of the variable, with an eye toward controlling degrees of freedom while maintaining a compromise between flexibility and loss of precision; knot position can then be assigned at fixed quantiles based on number. Non-heavy drinking frequency was estimated with 4 knots at the .05, .35, .65 and .95 quantiles; BMI was estimated with 3 knots at the .10, .50 and .90 quantiles.
Poor health and current smoking status violated the proportional hazards assumption, requiring that we specify stratified Cox models in which baseline hazard function was allowed to vary based on these variables. We then tested interaction terms for these variables by heavy and non-heavy drinking frequency to determine if stratification adequately modeled their impact; at this time we also tested interactions for our a priori comparisons (race/ethnicity, sex and age cohort). All interactions were added and tested via the partial likelihood ratio test, with a Wald statistic of p < .05 serving as the threshold for inclusion into the final model (Hosmer, Lemeshow & May, 2008). This process yielded one significant interaction term for non-heavy drinking frequency by poor health status (p = .018); all other interactions were non-significant at p > .10. See Supplementary Table 1 for a list of all the variables in the final model.
Results
Sample Characteristics
The demographics of our final sample are described in Table 1, with respondents classified according to mortality status at follow-up. There were 3,364 decedents (3.01%); they were significantly older, less educated and less affluent than survivors. While there was a higher proportion of Blacks among decedents than survivors, there was a lower proportion of Hispanics, most likely due to the Hispanic population being, on average, younger than other demographic groups. There was a higher proportion of former drinkers among decedents, but lower proportions of lifetime abstainers and past-year drinkers.
Table 1.
Demographics of the 1997-2001 NHIS, Ages 18 through 64, by Mortality Status
| Overall | Decedents | Survivors | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total | 111511 | 100.00 | 3364 | 3.01 | 108147 | 96.98 |
| Sex | ||||||
| Women | 61340 | 55.01 | 1444 | 42.93 | 59896 | 55.38 |
| Men | 50171 | 44.99 | 1920 | 57.07 | 48251 | 44.62 |
| Age | ||||||
| 18-30 | 27402 | 24.57 | 175 | 5.20 | 27227 | 25.18 |
| 31-40 | 29694 | 26.63 | 355 | 10.55 | 29339 | 27.13 |
| 41-50 | 27114 | 24.32 | 758 | 22.53 | 26356 | 24.37 |
| 51-60 | 19787 | 17.74 | 1180 | 35.08 | 18607 | 17.21 |
| 61-64 | 7514 | 6.74 | 896 | 26.63 | 6618 | 6.12 |
| Ratio of Family Income to Federal Poverty Threshold | ||||||
| Under 1 | 13695 | 12.28 | 660 | 19.62 | 13035 | 12.05 |
| 1 to 1.99 | 16359 | 14.67 | 639 | 19.00 | 15720 | 14.54 |
| 2 to 2.99 | 15866 | 14.23 | 450 | 13.38 | 15416 | 14.25 |
| 3 to 4.99 | 24079 | 21.59 | 571 | 16.97 | 23508 | 21.74 |
| 5 and Over | 23938 | 21.47 | 489 | 14.54 | 23449 | 21.68 |
| Indeterminate | 17574 | 15.76 | 555 | 16.50 | 17019 | 15.74 |
| Drinking Status | ||||||
| Lifetime Abstainer | 22818 | 20.46 | 623 | 18.52 | 22195 | 20.52 |
| Former Drinker | 14907 | 13.37 | 906 | 26.93 | 14001 | 12.95 |
| Past-Year Drinker | 73786 | 66.17 | 1835 | 54.55 | 71951 | 66.53 |
| Self-Reported Health Status | ||||||
| Excellent | 38458 | 34.49 | 437 | 12.99 | 38021 | 35.16 |
| Very Good | 37159 | 33.32 | 725 | 21.55 | 36434 | 33.69 |
| Good | 25361 | 22.74 | 922 | 27.41 | 24439 | 22.60 |
| Fair | 8053 | 7.22 | 771 | 22.92 | 7282 | 6.73 |
| Poor | 2480 | 2.22 | 509 | 15.13 | 1971 | 1.82 |
| Race/Ethnicity | ||||||
| White | 72300 | 64.84 | 2181 | 64.83 | 70119 | 64.84 |
| Black | 15624 | 14.01 | 710 | 21.11 | 14914 | 13.79 |
| Hispanic | 19667 | 17.64 | 411 | 12.22 | 19256 | 17.81 |
| Other | 3920 | 3.52 | 62 | 1.84 | 3858 | 3.57 |
| Educational Attainment | ||||||
| Less than High School | 6472 | 5.80 | 368 | 10.94 | 6104 | 5.64 |
| Some high school | 12703 | 11.39 | 615 | 18.28 | 12088 | 11.18 |
| High school diploma or GED | 31681 | 28.41 | 1038 | 30.86 | 30643 | 28.33 |
| Some College, no degree | 23000 | 20.63 | 624 | 18.55 | 22376 | 20.69 |
| Any college degree | 37655 | 33.77 | 719 | 21.37 | 36936 | 34.15 |
Distribution of drinking patterns
Past-year drinkers constituted 66.17% (n = 73,786) of the sample. Those who reported any heavy drinking (n = 26,663) made up 36.14% of past-year drinkers and 23.91% of the full sample, while 7,176 respondents—9.73% of past-year drinkers and 6.44% of the full sample—reported heavy drinking as their only drinking behavior (see Table 2). Of past year drinkers, 46.15% (n = 34,051) averaged at least one drinking occasion a week (see Supplementary Table 2). Of weekly drinkers, 80.41% (n = 27,380) drank primarily non-heavily, that is, they reported non-heavy drinking at least once a week, but averaged less than one heavy drinking occasion. Weekly drinkers who engaged primarily in heavy drinking constituted 6.18% (n = 4,560) of past-year drinkers; they averaged at least one heavy drinking occasion, but less than one non-heavy occasion, per week. Finally, 2.62% (n = 1,934) of past-year drinkers exhibited mixed-pattern drinking, by combining, on average, at least one of both heavy and non-heavy occasions per week. Taking heavy and mixed-pattern drinkers together, 9.73% (n = 7,176) of past-year drinkers, or 6.43% of the full sample, reported drinking heavily at least once a week. We also assessed average daily consumption for past-year drinkers; overall, average consumption increased with more frequent drinking, both for heavy (r = .69, p < .001) and non-heavy (r = .29, p < .001) drinking frequency. Deaths by combination of non-heavy and heavy drinking frequency can also be seen in Table 2.
Table 2.
Past-Year Frequency of Non-Heavy and Heavy Drinking
| Non-Heavy Days Per Week | Heavy Drinking Days Per Week
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 0 - 0.99 | 1 - 1.99 | 2 - 2.99 | 3 - 3.99 | 4 - 4.99 | 5 - 5.99 | 6 - 6.99 | 7 | Total | |||||||||||
|
| ||||||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| 0 | -- -- | -- -- | 2616 | 3.55 | 1773 | 2.40 | 1235 | 1.67 | 529 | 0.72 | 181 | 0.25 | 156 | 0.21 | 87 | 0.12 | 599 | 0.81 | 7176 | 9.73 |
| 0 - 0.99 | 31497 | 42.69 | 9711 | 13.16 | 181 | 0.25 | 58 | 0.08 | 32 | 0.04 | 5 | 0.01 | 4 | 0.01 | 41 | 0.06 | -- -- | -- -- | 41529 | 56.28 |
| 1 - 1.99 | 7421 | 10.06 | 3289 | 4.46 | 364 | 0.49 | 139 | 0.19 | 37 | 0.05 | 13 | 0.02 | 46 | 0.06 | 17 | 0.02 | -- -- | -- -- | 11326 | 15.35 |
| 2 - 2.99 | 3709 | 5.03 | 1644 | 2.23 | 214 | 0.29 | 85 | 0.12 | 35 | 0.05 | 21 | 0.03 | 32 | 0.04 | -- -- | -- -- | -- -- | -- -- | 5740 | 7.78 |
| 3 - 3.99 | 1635 | 2.22 | 694 | 0.94 | 117 | 0.16 | 48 | 0.07 | 48 | 0.07 | 25 | 0.03 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 2567 | 3.48 |
| 4 - 4.99 | 618 | 0.84 | 503 | 0.68 | 78 | 0.11 | 51 | 0.07 | 59 | 0.08 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 1309 | 1.77 |
| 5 - 5.99 | 502 | 0.68 | 119 | 0.16 | 119 | 0.16 | 158 | 0.21 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 898 | 1.22 |
| 6 - 6.99 | 136 | 0.18 | 1272 | 1.72 | 228 | 0.31 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 1636 | 2.22 |
| 7 | 1605 | 2.18 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 1605 | 2.18 |
|
| ||||||||||||||||||||
| Total | 47123 | 63.86 | 19848 | 26.9 | 3074 | 4.17 | 1774 | 2.40 | 740 | 1.00 | 245 | 0.33 | 238 | 0.32 | 145 | 0.20 | 599 | 0.81 | 73786 | 100 |
| Deaths by Frequency of Non-Heavy and Heavy Drinking | ||||||||||||||||||||
| 0 | -- -- | -- -- | 61 | 2.33 | 30 | 1.69 | 32 | 2.59 | 17 | 3.21 | 6 | 3.31 | 9 | 5.77 | 3 | 3.45 | 69 | 11.52 | 227 | 3.16 |
| 0 - 0.99 | 726 | 2.3 | 169 | 1.74 | 6 | 3.31 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 25.00 | 2 | 4.88 | -- -- | -- -- | 904 | 2.18 |
| 1 - 1.99 | 162 | 2.18 | 64 | 1.95 | 6 | 1.65 | 4 | 2.88 | 4 | 10.81 | 1 | 7.69 | 5 | 10.87 | 2 | 11.76 | -- -- | -- -- | 248 | 2.19 |
| 2 - 2.99 | 78 | 2.10 | 27 | 1.64 | 13 | 6.07 | 5 | 5.88 | 2 | 5.71 | 2 | 9.52 | 3 | 9.38 | -- -- | -- -- | -- -- | -- -- | 130 | 2.26 |
| 3 - 3.99 | 37 | 2.26 | 17 | 2.45 | 5 | 4.27 | 2 | 4.17 | 5 | 10.42 | 2 | 8.00 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 68 | 2.65 |
| 4 - 4.99 | 17 | 2.75 | 20 | 3.98 | 2 | 2.56 | 4 | 7.84 | 5 | 8.47 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 48 | 3.67 |
| 5 - 5.99 | 21 | 4.18 | 4 | 3.36 | 8 | 6.72 | 11 | 6.96 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 44 | 4.9 |
| 6 - 6.99 | 4 | 2.94 | 56 | 4.40 | 12 | 5.26 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 72 | 4.4 |
| 7 | 94 | 5.86 | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | -- -- | 94 | 5.86 |
|
| ||||||||||||||||||||
| Total | 1139 | 2.42 | 418 | 2.11 | 82 | 2.67 | 58 | 3.27 | 33 | 4.46 | 11 | 4.49 | 18 | 7.56 | 7 | 4.83 | 69 | 11.52 | 1835 | 2.49 |
Note. Percentages in bottom portion reflect percentage of deaths of the corresponding cell in the upper portion.
Mortality analysis
Results from the stratified Cox model can be seen in Table 3. As noted, the model allowed for different baseline functions across groups based on poor health status, former drinking status and current smoking status. Additionally, there was a significant interaction between non-heavy drinking frequency and poor health status; mortality related to non-heavy drinking was different for those who indicated they were of poor health, both with regard to baseline hazard function and hazard ratio, as compared to the rest of the sample.
Table 3.
Regression Coefficients for Mortality Related to Heavy and Non-Heavy Drinking Frequency
| B | SE | p | |
|---|---|---|---|
| Non-heavy drinking frequency | -0.278 | 0.063 | < 0.001 |
| Non-heavy frequency, non-linear term | 2.241 | 0.455 | < 0.001 |
| Heavy drinking frequency | 0.084 | 0.015 | < 0.001 |
| Sex | 0.522 | 0.038 | < 0.001 |
| Former smoking status | 0.234 | 0.050 | < 0.001 |
| BMI | -0.049 | 0.010 | < 0.001 |
| BMI, non-linear term | 0.064 | 0.012 | < 0.001 |
| Race/ethnicity | |||
| White | ref | -- | -- |
| Black | 0.281 | 0.046 | < 0.001 |
| Hispanic | -0.241 | 0.060 | < 0.001 |
| Other | -0.425 | 0.130 | < 0.001 |
| Survey Wave | |||
| 1997 | ref | -- | -- |
| 1998 | 0.110 | 0.050 | 0.023 |
| 1999 | 0.082 | 0.054 | 0.133 |
| 2000 | 0.082 | 0.057 | 0.149 |
| 2001 | 0.072 | 0.061 | 0.240 |
| Census Region | |||
| Northeast | ref | -- | -- |
| North Central/Midwest | -0.049 | 0.055 | 0.370 |
| South | -0.004 | 0.049 | 0.944 |
| West | -0.112 | 0.059 | 0.057 |
| Educational attainment | |||
| Less than high school | ref | -- | -- |
| Some high school | 0.090 | 0.068 | 0.187 |
| High school diploma or GED | -0.039 | 0.066 | 0.552 |
| Some college | 0.054 | 0.072 | 0.449 |
| Any college degree | -0.193 | 0.073 | 0.008 |
| Ratio of Family Income to Federal Poverty Threshold | |||
| 1 to 1.99 | ref | -- | -- |
| 2 to 2.99 | -0.262 | 0.062 | < 0.001 |
| 3 to 4.99 | -0.420 | 0.060 | < 0.001 |
| 5 and Over | -0.601 | 0.066 | < 0.001 |
| Indeterminate | -0.320 | 0.059 | < 0.001 |
| Under 1 | 0.105 | 0.057 | 0.064 |
| Non-heavy frequency by poor health status interaction | |||
| Linear non-heavy term | 0.511 | 0.193 | 0.008 |
| Non-linear non-heavy term | -4.056 | 1.492 | 0.007 |
Note. n = 73,786
Figure 1 depicts mortality risk among past-year drinkers of better than poor health as a function of heavy and non-heavy drinking frequency. The linear dose-response relationship for heavy drinking and the non-linear relationship for non-heavy drinking are plotted separately (i.e., holding the other variable constant) to highlight the J-shaped relationship associated with non-heavy consumption. Supplementary Figure 1 also plots the relationship between non-heavy and heavy drinking frequency and mortality, but does so for the full range of drinking behaviors, depicting risk for mixed-drinking patterns. As can be seen in both, heavy drinking at any frequency was associated with increased risk, while non-heavy drinking frequency exhibited a protective effect that peaked around 2 occasions per week. As noted, non-heavy drinking frequency did not have a significant impact on mortality for respondents who reported poor health status, neither for the linear (B = 0.23, SE = 0.18, p = .20) nor for the non-linear terms (B = -1.82, SE = 1.42, p = .20); Supplementary Figure 2 depicts estimated hazard ratios by drinking pattern for those who reported poor health.
Figure 1.
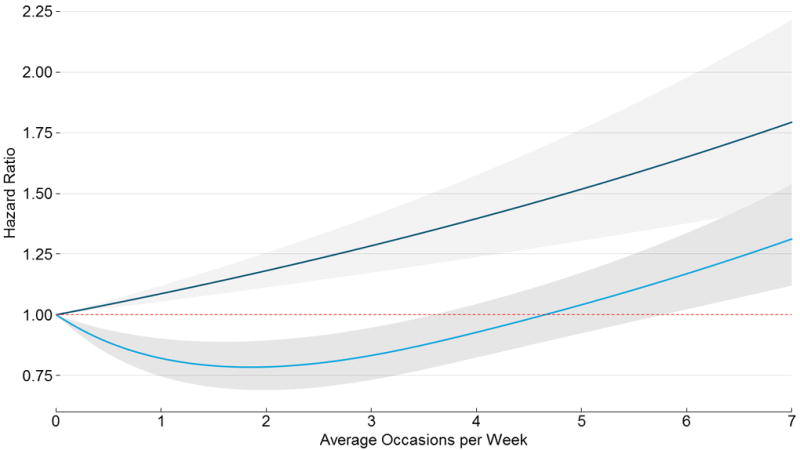
Mortality risk by frequency of heavy (5+ drinks; dark blue line) and non-heavy (<5 drinks; light blue line) drinking occasions per week. Hazard ratio, with 95% CI, is plotted separately for the frequency of each behavior. Data are based on the 1997 - 2001 waves of the National Health Interview Survey. Reflects an interaction model; results are for those respondents who did not indicate they were in poor health.
Conclusions
Summary of findings
Of those NHIS respondents who reported drinking, most drank non-heavily, but 36.14% (n = 26,663) reported any heavy drinking and 9.73% (n = 7,176) reported an average of at least one heavy drinking occasion per week. Lifetime abstainers served as the reference group in our mortality analyses and former drinkers constituted a categorically separate group, which, when coupled with stratification by health status, addresses potential confounding associated with the tendency for those in poor health to stop drinking, known as the sick quitter effect (Connor, 2006). Mortality estimated from frequency of heavy and non-heavy drinking suggested that there is no safe level of heavy drinking, the frequency of which was associated with increased risk relative to lifetime abstinence in a linear, dose-dependent manner across our whole sample (Figure 1). While the mortality analysis was also consistent with a protective effect based on drinking patterns characterized by non-heavy drinking for healthy individuals, heavy drinking could mitigate this potential effect. As depicted in Supplementary Figure 1, heavy drinking frequency impacted the apparent protective effect in mixed-pattern drinking behaviors if one assumes additive effects for non-heavy and heavy frequency. Additionally, we did not estimate a protective effect for those who reported poor health status, contrary to some past research (e.g., Mukamel et al., 2010), but this result is intuitive and suggests that any potential benefit from alcohol consumption is likely contingent upon current health. Finally, we did not observe differences based on sex, race/ethnicity or age cohort, despite substantial past research suggesting differences based on sex (e.g., Di Castelnuovo et al., 2006; Bagnardi et al., 2004), and to a lesser degree, race/ethnicity (e.g., Kerr et al., 2011).
These results also indicate that mortality estimates based on average daily consumption could mischaracterize risk for many drinkers, especially those who engage in infrequent heavy drinking episodes. Using risk thresholds for average daily consumption from past research (Di Castelnuovo et al., 2006) and focusing on those who drank heavily on at least a weekly basis, 5.01% (n = 3,736) of past-year drinkers in this sample would have their risk mischaracterized using the average daily consumption approach as compared to the frequency approach taken here. Specifically, heavy drinkers who averaged 1 to 4.99 drinks per day, but consumed those drinks primarily during heavy drinking occasions, would exhibit increased risk in our model while their average dosing suggests a protective effect. Although the average daily consumption approach estimates only slightly elevated risk at the 4 to 4.99 drinks per day level, our approach suggests those who consume such an amount over the course of 5 or more drinking occasions per week have a mortality risk almost 50% higher than that for abstainers (Figure 2).
Assessment of risk based on both heavy and non-heavy drinking frequency offers several advantages. Our model, based on a nationally representative U.S. sample, produced consistent, simultaneous associations for multiple drinking patterns and relates health risks to measures that are easy to assess in clinical practice and in epidemiological surveys. The potential reduction in risk for individuals who shift from heavy to non-heavy drinking also suggests that the assessment of heavy drinking frequency could be incorporated into harm reduction strategies, especially for individuals who drink heavily but are not dependent on alcohol, as often seen in college-age drinkers (Larimer & Cronce, 2002).
Limitations and conclusion
Several limitations should be kept in mind while interpreting these results. We focused on all-cause mortality and the data also represent a relatively short window for measuring mortality risk, both of which potentially contribute to uncertainty in estimates of long-term effects. This is less a concern when assessing heavy-drinking risk since a range of potential outcomes that affect mortality were captured, but a longer follow-up period, coupled with cause-specific mortality analyses, might be required to most accurately capture a protective effect associated with non-heavy consumption.
Both drinking pattern constructs cover a wide range of behaviors, but there is substantial evidence supporting the negative impact of heavy drinking (Rehm et al., 2003) and past research also suggests that heavy drinkers, both men and women, typically drink in excess of the 5+ binge threshold (Kanny et al., 2012). Heavy drinking frequency as defined exhibits sufficient face validity and is likely appropriately capturing risky drinking behavior.
The non-heavy drinking frequency construct is less precise and likely captures a broad range of behaviors, some of which might qualitatively differ in relation to mortality risk. As defined, non-heavy drinking frequency as a construct potentially contains: (a) truly protective levels of consumption, likely at around the 1 – 2 drinks per occasion threshold, where previous research has shown the greatest potential for a protective effect; (b) consumption that is on average risk-neutral; and (c) risky drinking behavior, especially for those who frequently consume 3+ drinks per occasion, or those who drink just below the heavy drinking threshold and drive after doing so. Non-heavy drinking might also be tapping into confounded factors not directly attributable to alcohol consumption (e.g., drinkers who consume wine with meals, whose reduced risk might stem from healthy lifestyle and diet). Lastly, respondents reported drinking more per occasion as their drinking frequency increased; it is possible that non-heavy drinking captured different drinking behaviors as respondents drank more often.
Even in light of these potential limitations, modeling alcohol-related mortality risk using heavy and non-heavy drinking frequency addresses shortcomings of other approaches and highlights future research needs. More precise assessment of lower-consumption frequency is warranted for future research on the protective effect of non-heavy drinking, perhaps by developing and validating a 1 – 2 drink threshold item for use in screening and research. Further research exploring differences in mortality based on demographic characteristics, such as sex and race/ethnicity, is also indicated. Additionally, even if the protective effect of non-heavy consumption has been overstated, as some investigators have suggested (Connor, 2006), risk associated with consumption at low thresholds would be significantly lower than that of heavy drinking and would at some point also likely be effectively risk-neutral. Promoting less-harmful drinking patterns by reducing heavy drinking frequency is an appropriate harm reduction strategy and assessing drinking pattern by determining the frequency of heavy and non-heavy drinking is a simple and fast way to determine risk and promote less risky drinking behavior.
Supplementary Material
Acknowledgments
Sources of funding included research grants T32DA07313 (ADP), K01DA025733 (PCR), K02DA021237 (LJB), R21DA0266 and R01DA031288 (RAG) from the National Institute on Drug Abuse and research grants P60AA011998 (HSM) and R01AA01744 (RAG) from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
ADP, HSM, PCR and RAG declare no conflicts of interest. LJB is listed as an inventor on Issued U.S. Patent 8,080,371, “Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction.
References
- Baglietto L, English DR, Hopper JL, Powles J, Giles GG. Average Volume of Alcohol Consumed, Type of Beverage, Drinking Pattern and the Risk of Death from All Causes. Alcohol and Alcoholism. 2006;41(6):664–671. doi: 10.1093/alcalc/agl087. [DOI] [PubMed] [Google Scholar]
- Bagnardi V, Zambon A, Quatto P, Corrao G. Flexible Meta-Regression Functions for Modeling Aggregate Dose-Response Data, with an Application to Alcohol and Mortality. American Journal of Epidemiology. 2004;159(11):1077–1086. doi: 10.1093/aje/kwh142. [DOI] [PubMed] [Google Scholar]
- Breslow RA, Graubard BI. Prospective Study of Alcohol Consumption in the United States: Quantity, Frequency, and Cause-Specific Mortality. Alcoholism: Clinical and Experimental Research. 2008;32(3):513–521. doi: 10.1111/j.1530-0277.2007.00595.x. [DOI] [PubMed] [Google Scholar]
- Britton A, Marmot M. Different measures of alcohol consumption and risk of coronary heart disease and all-cause mortality: 11-year follow-up of the Whitehall II Cohort Study. Addiction. 2004;99(1):109–116. doi: 10.1111/j.1360-0443.2004.00530.x. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Archives of internal medicine. 1998;158(16):1789. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2011 Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Google Scholar]
- Connor J. The Life and Times of the J-Shaped Curve. Alcohol and Alcoholism. 2006;41(6):583–584. doi: 10.1093/alcalc/agl079. [DOI] [PubMed] [Google Scholar]
- Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Alcohol consumption and mortality in patients with cardiovascular disease: a meta-analysis. Journal of the American College of Cardiology. 2010;55(13):1339–1347. doi: 10.1016/j.jacc.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol Dosing and Total Mortality in Men and Women: An Updated Meta-analysis of 34 Prospective Studies. Arch Intern Med. 2006;166(22):2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- Harrell FE. Regression Modeling Strategies. Springer; 2001. [Google Scholar]
- Hosmer DW, Lemeshow S, May S. Applied survival analysis: Regression modeling of time-to-event data. 2. Hoboken, New Jersey: Wiley; 2008. [Google Scholar]
- Kanny D, Liu Y, Brewer RD, Garvin WS, Balluz L. Vital Signs: Binge Drinking Prevalence, Frequency, and Intensity Among Adults. Morbidity and Mortality Weekly Report. 2012;61(1):14–19. [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Racial and Ethnic Differences in All-Cause Mortality Risk According to Alcohol Consumption Patterns in the National Alcohol Surveys. American Journal of Epidemiology. 2011;174(7):769–778. doi: 10.1093/aje/kwr147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinbaum DG, Klein M. Survival Analysis: A Self-Learning Text. 3. Springer; 2011. [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol and Drugs. 2002;(14):148. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- Lumley TS. Complex Surveys: A Guide to Analysis Using R. Hoboken, New Jersey: Wiley; 2010. [Google Scholar]
- McElduff P, Dobson AJ. How much alcohol and how often? Population based case-control study of alcohol consumption and risk of a major coronary event. BMJ. 1997;314(7088):1159–1159. doi: 10.1136/bmj.314.7088.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mørch LS, Johansen D, Løkkegaard E, Hundrup YA, Grønbæk M. Drinking pattern and mortality in Danish nurses. European Journal of Clinical Nutrition. 2007;62(6):817–822. doi: 10.1038/sj.ejcn.1602799. [DOI] [PubMed] [Google Scholar]
- Moriarity C. Sampling and Oversampling in the National Health Interview Survey. Hyattsville, MD: National Center for Health Statistics; 2006. [Google Scholar]
- Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol Consumption and Cardiovascular Mortality Among U.S. 1987 to 2002. Journal of the American College of Cardiology. 2010;55(13):1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA, Jr, Stampfer MJ, Willett WC, Rimm EB. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. New England Journal of Medicine. 2003;348(2):109–118. doi: 10.1056/NEJMoa022095. [DOI] [PubMed] [Google Scholar]
- Murray RP, Connett JE, Tyas SL, Bond R, Ekuma O, Silversides CK, Barnes GE. Alcohol Volume, Drinking Pattern, and Cardiovascular Disease Morbidity and Mortality: Is There a U-Shaped Function? American Journal of Epidemiology. 2002;155(3):242–248. doi: 10.1093/aje/155.3.242. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Data File Documentation, National Health Interview Survey, 2001 (machine readable data file and documentation) Hyattsville, Maryland: National Center for Health Statistics; 2002. Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2001/srvydesc.pdf. [Google Scholar]
- National Center for Health Statistics. The National Health Interview Survey (1986-2004) Linked Mortality Files, mortality follow-up through 2006: Matching Methodology. Hyattsville, Maryland: National Center for Health Statistics; 2009. Retrieved from http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhis_final.pdf. [Google Scholar]
- National Center for Health Statistics. NHIS Linked Mortality Public-Use Files: Frequencies for Selected Variables. Hyattsville, Maryland: National Center for Health Statistics; 2010. Retrieved from http://www.cdc.gov/nchs/data/datalinkage/nhis_frequency_of_selected_variables_public_2010.pdf. [Google Scholar]
- National Center for Health Statistics. Data File Documentation, National Health Interview Survey, 2010 (machine readable data file and documentation) Hyattsville, Maryland: National Center for Health Statistics; 2011. Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf. [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. NIAAA Council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3. [Google Scholar]
- Pencina MJ, Larson MG, D’Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Statistics in Medicine. 2007;26(6):1343–1359. doi: 10.1002/sim.2699. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Roerecke M, Rehm J. Irregular Heavy Drinking Occasions and Risk of Ischemic Heart Disease: A Systematic Review and Meta-Analysis. American Journal of Epidemiology. 2010;171(6):633–644. doi: 10.1093/aje/kwp451. [DOI] [PubMed] [Google Scholar]
- RTI International. 2010 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- Sobell L, Maisto S, Sobell M, Cooper A. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17(2):157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Stranges S, Wu T, Dorn JM, Freudenheim JL, Muti P, Farinaro E, Russell M, et al. Relationship of Alcohol Drinking Pattern to Risk of Hypertension A Population-Based Study. Hypertension. 2004;44(6):813–819. doi: 10.1161/01.HYP.0000146537.03103.f2. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse: Draft Recommendation Statement. 2012 doi: 10.7326/0003-4819-159-3-201308060-00652. (No. AHRQ Publication No. 12-05171-EF-2). Retrieved from http://www.uspreventiveservicestaskforce.org/draftrec.htm. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


