Abstract
BACKGROUND
Evidence is mixed regarding sugar-sweetened beverage (SSB) intake and adiposity among adults, perhaps due to reporting bias.
OBJECTIVE
To determine the impact of reporting bias on any associations between increased SSB intake and overweight/obesity.
DESIGN
Beverage intake and overweight/obese status (BMI ≥25 kg/m2) was examined among adults from a dietary assessment and doubly labeled water study (n=250). Four web-based, 24-hour recalls assessed dietary intake. SSB intake was categorized as no intake, 1–99 kcals per day, and >99 kcals per day. Logistic regression models adjusted for total caloric intake, age, race, education and diet quality compared SSB intake to overweight/obese status. To investigate dietary self-reporting bias, analyses were replicated in a subset of “true reporters”: those with self-reported total caloric intake within 25% of total energy expenditure per doubly labeled water assessments (n=108).
RESULTS
One-half of participants were overweight/obese; more overweight/obese participants consumed SSB than normal weight participants (69% vs. 47%; p<0.001). Intake of other beverages did not differ by adiposity. Less White participants (48%) consumed SSB compared to African-American participants (68%; p=0.002). Compared to no intake, SSB intake up to the median intake doubled the risk of being overweight/obese (OR: 2.1, 95% CI: 1.0–4.3; p=0.046), and SSB intake over the median more than doubled the risk (OR: 2.6, 95% CI: 1.2–6.0; p=0.018). When limited to true reporters, SSB intake significantly increased the risk of being overweight/obese by nearly 4 fold.
CONCLUSION
Underreporting of SSB intake may be attenuating true associations of SSB intake and the risk of being overweight/obese.
Keywords: Sugar-sweetened beverages, obesity, African-American, high-fructose corn syrup
INTRODUCTION
Limiting sugar intake is an important aspect of maintaining a healthy weight (1). Adults in the United Stated consume roughly 16% of their total calories from added sugars, 46% of which are in liquid form as sodas, energy or sports drinks and sugar-sweetened fruit drinks (1). Those drinks are commonly referred to as sugar sweetened beverages (SSB) as manufacturers add the sugars during processing (1). Consumption rates of SSB are increasing worldwide, with per capita intakes averaging 11.4 gallons per year (2). Consumption rates of SSB are highest in Mexico (31.5 gallons per person per year) and the United States (31.2 gallons per person per year (2). Evidence from over 39 observational studies (cross-sectional and prospective) supports a positive relationship between intake of SSB and the likelihood of being overweight or obese among children and adolescents (3–5). Fewer studies have examined this relationship among adults and results are mixed (3–7). Three prospective studies among adults support a positive association between increased SSB intake and weight gain (7), and a meta-analysis of 11 prospective studies (nine of which conducted in the United States) support a positive association between increased SSB consumption and the risk of developing metabolic syndrome and type II diabetes (herein referred to as diabetes) (8). Globally, Basu et al. (2013) report a positive association between per capita SSB intake estimated with sales data and the prevalence of overweight, obesity and diabetes over 75 countries (2). Those results were adjusted for dietary patterns and remained robust when limited to low- and middle-income countries (2).
The negative health consequences related to overweight and obesity are increasingly a worldwide burden (9). The World Health Organization encourages adults and children to reduce their intake of added sugars as part of a comprehensive strategy to reduce rates of overweight and obesity (9). However, the effect size between increased SSB intake and overweight and obesity varies across studies (10). Therefore, data are needed to better understand the impact SSB intake may have on overweight and obesity while accounting for potential sources of bias.
Many studies examining SSB intake among adults have estimated usual intake using food frequency questionnaires (FFQs) (3–6). Compared to FFQs, 24-hour dietary recalls are more precise in estimating intake of specific dietary components at the individual level (11). Nationally representative data of dietary intake based on one, 24-hour dietary recall suggest no association between SSB intake and the risk of being obese among US adults (12). Results from studies using multiple 24-hour dietary recalls (13, 14) or 7-day diet diaries (15) have also been mixed regarding SSB intake and adiposity. Unfortunately, differences in the classification of SSB across studies limit the interpretation of results (13–15). Dietary intake studies are also limited by systemic bias in reporting (11): overweight individuals are more likely to underreport their intake of unhealthy foods and overall total energy intake (11). This underreporting is observed in both the US and Europe (16, 17), and likely attenuates associations between SSB intake and obesity.
The objective of this study is to examine SSB intake and the odds of being overweight or obese among healthy adults based on multiple, web-based, 24-hour dietary recalls over a 30-day period. This study also assessed total energy expenditure with doubly labeled water, which among weight-stable adults, is an objective estimate of total energy intake. Analyses were repeated among participants with self-reported energy intake within 25% of total energy expenditure measured using doubly labeled water to assess the impact of reporting bias.
METHODS
Data are from the Energetics Dietary Assessment study (18), a cross-sectional study that enrolled N=261 healthy, non-smoking adults aged 21–69 years from greater Los Angeles. The study was designed to recruit an equal proportion of African-American and White participants; participants of Latino or other ethnicities were not specifically recruited. Participants were required to be weight stable and willing to undergo energy expenditure measurements using doubly labeled water. Participants completed three clinic visits (baseline, day 3, and day 13) and up to six web-based, 24-hour dietary recalls within 30 days of the baseline visit (DietDay, Centrax Corporation, Chicago, IL). Participants were invited to complete two additional web-based, 24-hour dietary recalls within 60 days of the baseline visit. Participants received $150 after completing the third clinic visit, and an additional $50 if they completed all eight web-based, 24-hour dietary recalls. The Institutional Review Board at the University of California-Los Angeles approved the study protocl, and participants provided written consent before participating in any study procedures.
Clinic Assessments
Participant characteristics and height (cm) were collected at the baseline visit; weight (kgs) was measured in triplicate at each clinic visit. This current analysis used height and the mean weight from the baseline visit to compute BMI, and participants were classified into two categories: normal (BMI <25 kg/m2) or overweight/obese (BMI ≥25 kg/m2). Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ) (19). The IPAQ assesses physical activity over work and leisure activities from the past seven days. Responses were converted to MET minutes per week of physical activity.
Doubly Labeled Water
Total energy expenditure was estimated using the doubly labeled water method (20) and samples were analyzed at the University of Wisconsin (Madison, Wisconsin).
This method measures carbon dioxide (CO2) production over a 2-week period and is a form of indirect calorimetry (21, 22). Briefly, participants ingested a solution of 10% H218O (1.9g/kg estimated body weight in water) and 99.9% 2H2O (0.12 g/kg estimated body weight in water) at the baseline, in-clinic visit. Estimated body weight in water was computed using the methods of Coward (23). Urine samples were collected at 2, 3 and 4 hours, and 14 days after ingestion; samples were analyzed using isotope ratio mass spectrometry. Results reflect total energy expenditure as kilocalories (kcals) per day assuming homeostasis. The methods used in this study are considered accurate and reliable (24–26). The doubly labeled water assessment was repeated at six months post-baseline among n=53 subjects; the intra-class correlation coefficient on the repeat measures was 0.88 (27). Participants whose self-reported caloric intake was within 25% of their total energy expenditure as estimated with doubly labeled water were defined as “true reporters” of dietary intake.
Dietary Assessments
Dietary intake was collected using DietDay, a validated, web-based, 24-hour dietary recall assessment (18, 28). DietDay uses a multipass process that incorporates skip patterns and internal logic checks to ensure accuracy of data entry. The DietDay database includes nearly 10,000 food and beverage items, with color images to assist participants with food types and portion sizes. Participants were also prompted to include all beverage intake including water. Nutrient content was based on the USDA nutrient database and included an expanded selection for mixed dishes and additional food product labels. This current analysis included the first four dietary assessments for each participant: the first dietary assessment from the baseline clinic visit and the next three sequential assessments completed within 30 days. A total of four assessments were chosen as a way to generate stable estimates of dietary intake while minimizing missing data. For each participant, total kcals, kcals for each beverage category and grams of total fat, saturated fat, and fiber were averaged over their four assessments to estimate daily intake. Analyses excluded outliers defined as those with total caloric intake greater than five standard deviations from the overall mean.
Beverage Classifications
All dietary entries coded as beverages were used for this study. Entry data included name of beverage, serving size, grams per serving and kcals per serving. Beverages were categorized by name and two study researchers reviewed coding; the study team was consulted to adjudicate differences. Meal replacement drinks and protein supplement shakes were not included as beverages but were coded as food intake.
Beverages were grouped into seven categories as follows: 1) SSB: soda, energy or sports drinks and fruit drinks (including non-carbonated flavored drinks such as lemonade or fruit punch, and low-calorie drink mixes such as diet lemonade), 2) fruit juice (considered to be 100% or mostly natural fruit juice), 3) diet soda, 4) dairy (plain and flavored milk such as chocolate milk or cocoa made with milk), 5) coffee/tea (sweetened or unsweetened), 6) alcohol, and 7) other beverages (vegetable juice, soy drinks, rice milk, coconut milk, tonic water that was not part of an alcoholic drink and smoothies from fast-food restaurants). Water was not included as a beverage category for this analysis. Beverage categories were mutually exclusive and mirror those used in the reporting of NHANES III survey data, except that sweetened tea was not included as SSB in this analysis because coffee or tea with added sugar were recorded separately by the DietDay software (29).
SSB intake was categorized into three groups based on the median daily intake among those who consumed any SSB (99 kcals/day). Categories were therefore zero intake, 1–99 kcals/day and >99 kcals/day.
Statistical Analyses
Participant characteristics were summarized overall and by body mass. The proportion of participants who consumed each beverage type was compared by adiposity and by race. The energy contribution of each beverage type (kcals/day) was summarized overall and by body mass and by race. Statistical comparisons were made using Chi-Square tests, T-Tests or Wilcoxon rank sum tests as appropriate.
Logistic regression was used to model the likelihood of being overweight/obese on SSB intake. Fully adjusted models included factors related to the overweight/obese status (i.e., age, race) and factors related to SSB intake (i.e., race, education) at the p<0.10 level. Since SSB intake may be related to overall diet quality (4, 13), three sensitivity models were run to determine if the intake of total fat, saturated fat or fiber could be confounding the association between SSB intake and overweight or obesity. In comparison to a logistic regression model including SSB intake adjusted for total caloric intake only, including fiber intake in the model reduced the coefficients for SSB by more than 10% (data not show). Therefore, all models in this study included fiber intake as a covariate. All analyses were repeated on the subset of participants defined as true reporters of caloric intake (detailed above) as assessed with doubly labeled water. Finally, as a comparison to SSB, all logistic regression models were repeated using fruit juice intake instead of SSB intake. Analyses were completed with the R language for statistical computing, version 2.11.0 (30).
RESULTS
Of the 261 participants who enrolled in the Energetics trial, 252 participants had at least four DietDay assessments within 30 days of the first clinic visit. The majority of participants (80%) completed all four assessments within 14 days; 92% completed all four within 21 days. Median time to the final, fourth assessment was 9 days (IQR: 7–13). Final analyses excluded two participants with extreme values of self-reported caloric intake (> 5 SDs from overall mean). The final sample size for this study was therefore n=250 participants, 123 (49.2%) were African-American.
N=108 participants were true reporters of total caloric intake (i.e., participants whose self-reported caloric intake was within 25% of their total energy expenditure as estimated with doubly labeled water). Estimated total energy expenditure among the subset of true reporters ranged from 1379–3726 kcals/day, and mean agreement between estimated energy expenditure and self-reported dietary intake among true reporters was 96%. The majority of non-true reporters (64.8%) under-reported their total energy intake, and mean agreement between self-reported dietary intake and energy expenditure was 61%. There were no significant differences in demographic characteristics for true reporters versus non-true reporters (data not shown); however, participants who under-reported their total energy intake were more likely to be overweight/obese (61.8%) compared to those who over-reported their total energy intake (37.8%; p=0.032). Regarding physical activity and dietary intake measures, non-true reporters self-reported a higher level of physical activity (p=0.003) and lower intakes of total fat (p=0.034) and saturated fat (p=0.027) compared to true reporters. There were no significant differences in total kcals or fiber intake by reporter status (data not shown).
One-half (51.2%) of all participants were overweight/obese (BMI ≥25 kg/m2), with African-Americans participants more likely to be overweight/obese than White participants (68.3% vs. 34.6%; p<0.001). Mean age of the sample was 38 years with overweight/obese participants older (42 years) than normal weight participants (33 years; p<0.001); however, baseline age did not differ by race (p=0.094). One-third (34.4%) of the sample was male with no difference by body mass (p=0.511), and 44.4% of the sample were college graduates with no difference by body mass (p=0.145). The distributions of participant characteristics for the subset of true reporters were consistent with those of all participants (data not shown). Supplemental table 1 displays baseline characteristics by body mass for the overall sample.
Overall, SSB included n=412 beverage entries: 54.9% were soda, 35.9% were fruit drinks and 9.2% were energy or sports drinks. There were n=291 fruit juice entries; the most common entries were orange juice (39.2%), cranberry juice (20.3%) and apple juice (11.0%). Of the n=129 other beverage entries, the most frequent were smoothies from fast-food restaurants (40.3%), soy based drinks (34.1%) and vegetable juice (14.7%).
Table 1 presents the proportion of participants who reported any consumption for each beverage type overall and for true reporters. Beverages accounted for 12.6% of total energy intake among all participants, and for 12.0% of total energy intake among the subset of true reporters. There was only one difference in the consumption of any beverage type by body mass: overweight/obese participants were more likely to consume SSB than normal weight participants among all participants (68.8% vs. 46.7%; p<0.001) and among true reporters (74.6% vs. 41.5%; p<0.001). SSB accounted for a greater portion of total caloric intake among all overweight/obese participants than normal weight participants overall (4.2% vs. 2.5%; p<0.001) and among true reporters only (4.2% vs. 2.0%; p=0.001). Any consumption of SSB was also higher among African-American participants than White participants among all participants (68.3% vs. 48.0%; p=0.002) and true reporters (67.9% vs. 48.1%; p=0.059), although not statistically significant among true reporters. African-American participants were less likely to report any consumption of alcohol (30.1% vs. 43.3%; p=0.042) and diet soda (7.3% vs. 29.9%; p<0.001) among all participants; results were consistent for true reporters (data not shown).
TABLE 1.
Rates of any consumption for each of seven beverage types among healthy adults enrolled in a dietary assessment and doubly labeled water study.1,2
| Overall (N=250) |
True Reporters (N=108) |
|
|---|---|---|
| SSB, n (%) | 145 (58.0%) | 63 (58.3%) |
| Fruit Juice, n (%) | 129 (51.6%) | 60 (55.6%) |
| Diet Soda, n (%) | 47 (18.8%) | 17 (15.7%) |
| Dairy, n (%) | 100 (40.0%) | 51 (47.2%) |
| Coffee/Tea, n (%) | 179 (71.6%) | 71 (65.7%) |
| Alcohol, n (%) | 92 (36.8%) | 36 (33.3%) |
| Other3, n (%) | 56 (22.4%) | 26 (24.1%) |
SSB: Sugar-sweetened beverages.
Any intake defined as any reported intake over each of the dietary recalls.
There were no significant differences in any consumption of each of the seven beverage types between true reports and non-true reports (all Chi-Square p>0.075).
Other beverages include vegetable juice, soy drinks, rice milk, coconut milk and tonic water.
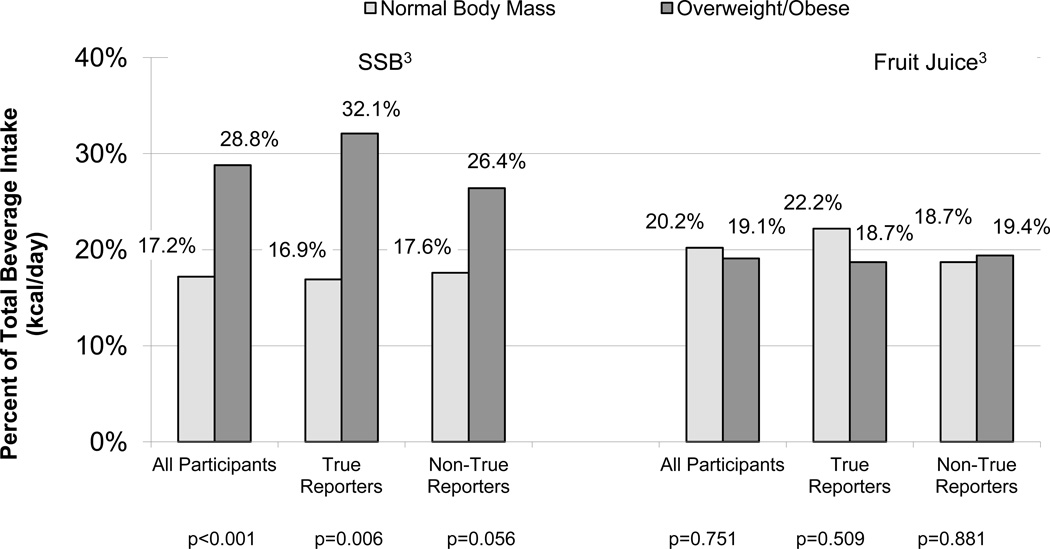
Among all participants, SSB was the greatest contributor of beverage kcals for overweight/obese participants at 29%; fruit juice was the second greatest contributor (19%). That is in comparison to normal weight participants, where SSB was the fourth greatest contributor of beverage kcals at 17% behind alcohol (23%), 100% fruit juice (20%) and coffee/tea (18%). Those trends were consistent among the subset of true reporters (data not shown). Figure 1 displays the contribution of SSB and 100% fruit juice to total beverage intake (kcals/day) by body mass for all participants and for the subsets of true reporters and non-true reporters of total energy intake. Overweight/obese participants appeared to under-report their intake of SSB. In comparison, there appeared to be less bias in the reporting of 100% fruit juice intake.
FIGURE 1.
Contribution of SSB and 100% fruit juice towards total daily beverage intake (kcals) among healthy adults participating in a dietary assessment study by adiposity: overall (N=250) and for the subsets of true reporters (N=108) and non-true reporters (N=142) of total energy intake.
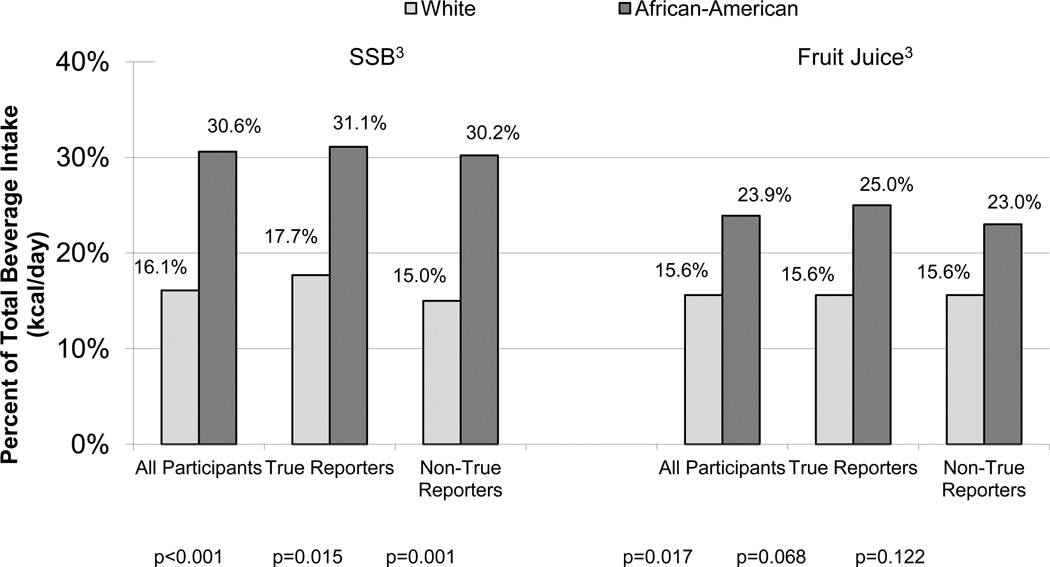
Among all participants, SSB was the greatest contributor of beverage kcals for African-American participants at 31%; fruit juice was the second greatest contributor (24%). That is in comparison to White participants, where SSB was tied with 100% fruit juice and dairy as the third greatest contributor of beverage kcals behind alcohol and coffee/teas, respectively (16% each). Those trends were consistent among the subset of true reporters (data not shown). Figure 2 displays the contribution of SSB and 100% fruit juice to total beverage intake (kcals/day) by race for all participants and for the subsets of true reporters and non-true reporters. Both SSB and 100% fruit juice made up a greater portion of total beverage kcals for African-American participants compared to White participants. There did not appear to be any patterns in reporting bias by race.
FIGURE 2.
Contribution of SSB and 100% fruit juice towards total daily beverage intake (kcals) among healthy adults participating in a dietary assessment study by race: overall (N=250) and for the subsets of true reporters (N=108) and non-true reporters (N=142) of total energy intake.
Table 2 presents physical activity level, total caloric intake and beverage intake for all participants and for the subset of true reporters by body mass. Among all participants, self-reported total caloric intake did not vary by adiposity status (p=0.436). When limited to the subset of true reporters, median caloric intake was approximately 190 kcals/day higher among overweight/obese participants compared to normal weight participants (p=0.003). There was also a reporting bias for beverage intake. Among all participants, median beverage intake was 58 kcals greater among overweight/obese participants than normal participants (p=0.070), and this between group difference increased to 147 kcals when limited to the subset of true reporters only (p=0.002). While the overall rates of SSB or 100% fruit juice consumption did not differ for all participants and the subset of true reporters, the median intake of 100% fruit juice was 30 kcals/day lower among the subset of true reporters compared to all participants, and also compared to non-true reporters (86 kcals/day), although that difference was not statistically significant (p=0.118).
TABLE 2.
Physical activity level, dietary intake and beverage intake among adults enrolled in a dietary assessment and doubly labeled water study: characteristics overall and by body mass for all participants (n=250) and true- reporters (n=108) separately.
| Overall (N=250) |
Normal Body Mass: BMI <25 kg/m2 (N=122) |
Overweight/Obese :BMI ≥25 kg/m2 (N=128) |
p-value1 | |
|---|---|---|---|---|
| Median (IQR) | ||||
| MET minutes per week | ||||
| All participants (n=250) | 2890 (1335 – 6239) | 2874 (1338 – 5712) | 2906 (1361 – 6633) | 0.449 |
| True reporters (n=108) | 2241 (1159 – 4671) | 2525 (1146 – 5718) | 1816 (1191 – 3908)* | 0.350 |
| Total caloric intake, kcals/day | ||||
| All participants (n=250) | 2177 (1752 – 2737) | 2185 (1668 – 2683) | 2170 (1846 – 2754) | 0.436 |
| True reporters (n=108) | 2201 (1907 – 2540) | 2102 (1675 – 2379) | 2291 (1992 – 2742) | 0.003 |
| Total fat intake, grams/day | ||||
| All participants (n=250) | 79 (61 – 115) | 77 (56 – 115) | 80 (65 – 116) | 0.352 |
| True reporters (n=108) | 84 (70 – 104) | 78 (61 – 99) | 89 (75 – 111) | 0.015 |
| Saturated fat intake, grams/day | ||||
| All participants (n=250) | 24 (18 – 35) | 24 (17 – 33) | 24 (19 – 35) | 0.546 |
| True reporters (n=108) | 26 (22 – 33) | 23 (18 – 30) | 28 (23 – 34) | 0.027 |
| Fiber intake, grams/day | ||||
| All participants (n=250) | 21 (14 – 29) | 20 (14 – 31) | 22 (14 – 28) | 0.800 |
| True reporters (n=108) | 19 (14 – 28) | 19 (15 – 28) | 18 (13 – 27) | 0.999 |
| Beverage caloric intake, kcals/day | ||||
| All participants (n=250) | 252 (123 – 414) | 214 (105 – 393) | 272 (149 – 428) | 0.070 |
| True reporters (n=108) | 252 (129 – 411) | 178 (113 – 294) | 325 (194 – 450) | 0.002 |
| Any SSB intake, n (%) | ||||
| All participants (n=250) | 145 (58.0%) | 57 (46.7%) | 88 (68.8%) | <0.001 |
| True reporters (n=108) | 63 (58.3%) | 22 (41.5%) | 41 (74.6%) | 0.001 |
| SSB caloric intake2, kcals/day | ||||
| All participants (n=250) | 99 (37 – 187) | 72 (36 – 151) | 107 (38 – 201) | 0.106 |
| True reporters (n=108) | 84 (IQR: 38 – 174) | 74 (IQR: 38 – 132) | 96 (IQR: 44 – 192) | 0.220 |
| Any 100% fruit juice intake, n (%) | ||||
| All participants (n=250) | 129 (51.6%) | 64 (52.5%) | 65 (50.8%) | 0.890 |
| True reporters (n=108) | 60 (55.6%) | 28 (52.8%) | 32 (58.2%) | 0.715 |
| 100% Fruit juice caloric intake2 kcals/day |
||||
| All participants (n=250) | 81 (35 – 121) | 81 (35 – 104) | 81 (35 – 169) | 0.340 |
| True reporters (n=108) | 52 (34 – 117) | 53 (39 – 94) | 46 (31 – 170) | 0.965 |
SSB: Sugar-sweetened beverages
p-value from Wilcoxon rank-sum test for medians.
SSB and 100% fruit juice intake limited to those who reported any SSB or 100% fruit juice intake only; i.e., among consumers only.
Results for the adjusted logistic regression model fitting body mass on SSB intake are presented in Table 3. Compared to no intake of SSB, an intake 1–99 kcals/day was associated with a 2.1 increased risk of being overweight/obese, and an intake of >99 kcals/day was associated with a 2.6 increased risk. The final logistic regression model was repeated on the subset of true reporters only (n=108). In that subset, SSB intake was associated with an approximate 4-fold increase in the risk of being overweight/obese.
TABLE 3.
Odds of being overweight/obese by sugar-sweetened beverage intake among 250 adults enrolled in a dietary assessment and doubly labeled water study: results overall and for the subset of true reporters.1,2,3
| All Participants (N=250) | True Reporters (N=108) | ||||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| SSB Intake | Median Intake | ||||
| None | 0 kcals/day | 1.0 | Referent | 1.0 | Referent |
| 1 – 99 kcals/day | 38 kcals/day | 2.1 (1.0 – 4.3) | 0.046 | 3.7 (1.2 – 12.1) | 0.025 |
| >99 kcals/day | 187 kcals/day | 2.6 (1.2 – 6.0) | 0.018 | 4.5 (1.2 – 18.0) | 0.029 |
| African-American vs. White race | 3.9 (2.1 – 7.5) | <0.001 | 3.4 (1.2 – 10.1) | 0.020 | |
SSB: Sugar-sweetened beverages.
Model also adjusted for age, education, total caloric intake (kcal/day) and fiber intake (grams/day).
True reporters defined as subset with self-reported total dietary intake within 25% of total energy expenditure as per doubly labeled water.
SSB intake categorized as no intake (n=107), and at the median intake level among consumers: 1–99 kcal/day (n=71) versus >99 kcal/day (n=72).
A sensitivity analyses repeated the final models unadjusted for race. Among both all participants and among the subset of true reporters, point estimates for SSB intake up to 99 kcals/day were consistent with the final model (data not shown). Specifically, the odds ratio for SSB intake up to 99 kcals/day increased 5.7% to 2.2 among all participants, and remained the same at 3.7 among the subset of true reporters. The point estimates for SSB intake > 99 kcals/day were slightly larger in the models unadjusted for race. Specifically, the odds ratio for SSB intake > 99 kcals/day increased 26.9% to 3.3 among all participants, and increased 17.8% to 5.3 among the subset of true reporters. Indeed, while 46.2% (n=12/26) of normal weight participants who consumed up to 99 kcals/day of SSB were African-American, 80.4% (n=37/46) of overweight/obese participants who consumed up to 99 kcals/day of SSB were African-American. However, there was no evidence of race moderating the association between SSB intake and body mass: the Likelihood Ratio Test comparing two nested models with and without an interaction term of SSB intake and race was non-significant (p=0.596).
Finally, to compare intake of SSB with intake of 100% fruit juice, all logistic regression models were repeated using intake of 100% fruit juice as the main independent variable. Intake was defined as zero intake, average daily intake of fruit juice up to the median intake among consumers (1–79 kcals/day), and average daily intake of fruit juice over the median intake among consumers (>79 kcals/day). There were no significant associations between intake of fruit juice and the likelihood of being overweight/obese among the entire sample or among the subset of true reporters only (data not shown).
DISCUSSION
These data indicate that SSB intake significantly increased the likelihood of being overweight or obese among otherwise healthy adults. When the sample was limited to participants who more accurately reported their total energy intake as determined with doubly labeled water, SSB intake increased the odds of being overweight/obese nearly 4-fold. These results support that SSB intake is associated with an increased odds of being overweight/obese, and that underreporting of SSB intake among overweight/obese adults may be attenuating the true association between SSB intake and body mass.
In comparison to the results from this study, Sun et al. (12) found no association between any SSB intake and obesity using nationally representative survey data. In that study, the methods used to classify SSB were similar to those used here; however, estimates of SSB intake and energy intake were based on one, 24-hour dietary recall. It is possible that reporting bias influenced the results of the Sun et al. analysis. For example, no difference in total energy intake by obesity status was reported (12). In comparison, there were no differences in total energy intake by body mass in this current study unless the sample was limited to the subset of true reporters of energy intake.
In this study, 58% of participants reported any SSB intake, which is similar to the 60% of adults in California who report occasional or daily intake of SSB (6) and to the 63% of adults nationwide with any reported SSB intake as collected with one, 24-hour dietary recall (29). However, quantities of SSB intake in this sample are lower compared to national estimates for adults aged 20 years or older. For example, mean intake for adults nationwide is 294 kcals/day based on data from the third and fourth National Health and Nutrition Examination Surveys (NHANES) (29) compared to 137 kcals/day in this study sample. The Energetics Study was based at an academic center in Los Angeles and recruited well-educated, healthy adults from the surrounding area who identified as weight stable. Thus, these adults likely consumed lower amounts of SSB as compared to the national average. Nonetheless, a strong relationship between SSB intake and body mass was found even at intake levels lower than national averages, suggesting that these findings may be conservative.
Consistent with nationally representative survey data from the United States (29), this study showed greater SSB intake among African-American adults as compared to Whites. In this study, African-American participants were 60% more likely to consume any SSB, and also consumed greater amounts of SSB per day than White participants. The final analysis based on logistic regression models showed that race may be mediating the association between SSB intake over 99 kcals/day and overweight/obese status. However, there was no interaction between SSB intake and race on body mass. Therefore, it is possible that the increased SSB intake among African-American compared to White participants may partially explain the differential rates of overweight/obese by race (31).
These data did not support an association between fruit juice intake and adiposity, even though the proportion of participants consuming fruit juice (52%) was similar to the proportion consuming SSB (58%). There was the suggestion that 100% fruit juice consumption was over-reported. Median intake of 100% fruit juice was 50 kcals per day among true reporters, an amount roughly equivalent to 4 fluid ounces of orange juice, compared to 80 kcals per day among all participants. Thus, results for 100% fruit juice are with respect to intake levels lower than those for SSB. However, this current study supports that SSB may have a unique impact on the risk of increased adiposity as compared to naturally sweet beverages such as juice (1, 3, 32–34). For example, while SSB and 100% fruit juice both contain fructose, SSB may be less satiating than fruit juice due to the lack of fiber (1, 3) and higher glycemic index than natural fruit juice (1, 32, 34).
Beverage intakes in this study were collected using multiple 24-hour dietary recalls and do not reflect infrequent intake of SSB such as a few times a month or less. Also, since this study was cross-sectional, inference regarding a cause and effect relationship between SSB intake and weight gain is limited. For example, intake of SSB may correlate with other unhealthy lifestyle behaviors that may impact adiposity (4, 13). However, several reviews support a cause and effect relationship between SSB intake and weight gain among children and adolescents (3, 5), and longitudinal data from the Nurses Health Study II show that adult women who increased their SSB intake over 4 years gained more weight than those who decreased their intake over this time (35). Similarly, it is possible that increased fruit juice intake is a proxy for overall healthier dietary and lifestyle behaviors among adults (36). However, no associations were found between orange and grapefruit juice consumption (maximum response of >=2 drinks per day) and incident diabetes among more than 40,000 women followed for 10 years as part of the Black Women’s Health Study, while that same study did find a positive association between SSB and fruit drink intake and incident diabetes (37). Additionally, some 100% fruit juices may provide health benefits to overweight adults when consumed in moderate amounts: a cross-over trial among overweight men aged 50–65 found improvements in cardiovascular disease biomarkers after 4-weeks of daily consumption of 8-ounce of orange juice, an effect likely mediated by hesperidin (38). To note, orange juice contributed the most to 100% fruit juice intake in this current sample at 39.2%. It is noted that many professional health associations including the American Academy of Pediatrics suggest limiting fruit juice intake among children to 4–6-ounces per day to help prevent overweight and obesity (39). Therefore, public health messages encouraging adults to reduce their SSB intake need to be cautious about promoting appropriate low- or no-calorie beverages to serve as SSB substitutes.
Estimating energy expenditure using doubly-labeled water is considered a valid, objective method. However, the doubly-labeled water methods are not without error. Several factors may influence the results including total body water volume, changes in body water volume over the assessment period, high alcohol intake, and atypical diets that vary in their primary source of fuel (i.e., carbohydrates, fats or proteins) (40). As such, some outliers are expected. However, by limiting this sample to a subset of true reporters as defined in reference to self-reported dietary intake, the likelihood that methodological errors are confounding results is low. For example, estimated total energy intake ranged from 1379–3726 kcals/day in the subset of true reporters; realistic values for this sample.
In summary, these data support a positive association between SSB intake and the likelihood of being overweight or obese among otherwise healthy adults, and underreporting of SSB intake may be attenuating true associations. Considering African-American adults are more likely to consume SSB than Whites, dietary interventions specifically targeting decreased SSB intake among African-Americans are warranted. These data add to the body of literature needed to inform evidence-based dietary guidelines regarding SSB intake among adults.
Supplementary Material
ACKNOWLEDGEMENTS
This funding for this project was provided by the National Institutes of Health grant R01CA105048, as well a T32 training grant, 3T3236GM084896-0251, under the National Institute of General Medical Sciences of the National Institutes of Health.
Footnotes
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interests for any of the authors involved in this study.
Supplementary information is available at the journal’s website.
REFERENCES
- 1.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 2.Basu S, McKee M, Galea G, Stuckler D. Relationship of Soft Drink Consumption to Global Overweight, Obesity, and Diabetes: A Cross-National Analysis of 75 Countries. Am J Public Health. 2013 Mar 14; doi: 10.2105/AJPH.2012.300974. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woodward-Lopez G, Kao J, Ritchie L. To what extent have sweetened beverages contributed to the obesity epidemic? Public Health Nutr. 2011;14(3):499–509. doi: 10.1017/S1368980010002375. [DOI] [PubMed] [Google Scholar]
- 4.Gibson S. Sugar-sweetened soft drinks and obesity: a systematic review of the evidence from observational studies and interventions. Nutr Res Rev. 2008;21(2):134–147. doi: 10.1017/S0954422408110976. [DOI] [PubMed] [Google Scholar]
- 5.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84(2):274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Babey SH, Jones M, Yu H, Goldstein H. Bubbling Over: Soda Consumption and Its Link to Obesity in California. [accessed 22 September 2011];UCLA Center for Health Policy Research. September 2009. Internet: http://www.healthpolicy.ucla.edu/pubs/Publication.aspx?pubID=375. [PubMed]
- 7.Olsen NJ, Heitmann BL. Intake of calorically sweetened beverages and obesity. Obes Rev. 2009;10(1):68–75. doi: 10.1111/j.1467-789X.2008.00523.x. [DOI] [PubMed] [Google Scholar]
- 8.Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. [Accessed May 7, 2013];Fact sheet: Obesity and overweight. No. 311. Updated March 2013. Available at http://www.who.int/mediacentre/factsheets/fs311/en/
- 10.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97(4):667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson FE, Subar AF. Dietary Assessment Methodology. In: Coulston AM, Rock CL, Monsen ER, editors. Nutrition in the Prevention and Treatment of Disease. San Diego, CA: Academic Press; 2001. pp. 3–39. [Google Scholar]
- 12.Sun SZ, Empie MW. Lack of findings for the association between obesity risk and usual sugar-sweetened beverage consumption in adults - A primary analysis of databases of CSFII-1989–1991, CSFII-1994–1998, NHANES III, and combined NHANES 1999–2002. Food Chem Toxicol. 2007;45(8):1523–1536. doi: 10.1016/j.fct.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Liebman M, Pelican S, Moore SA, Holmes B, Wardlaw MK, Melcher LM, et al. Dietary intake, eating behavior, and physical activity-related determinants of high body mass index in rural communities in Wyoming, Montana, and Idaho. Int J Obesity. 2003;27:684–692. doi: 10.1038/sj.ijo.0802277. [DOI] [PubMed] [Google Scholar]
- 14.O'Neil CE, Nicklas TA, Liu Y, Franklin FA. Impact of Dairy and Sweetened Beverage Consumption on Diet and Weight of a Multiethnic Population of Head Start Mothers. J Am Diet Assoc. 2009;109(5):874–882. doi: 10.1016/j.jada.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCarthy SN, Robson PJ, Livingstone MB, Kiely M, Flynn A, Cran GW, et al. Associations between daily food intake and excess adiposity in Irish adults: towards the development of food-based dietary guidelines for reducing the prevalence of overweight and obesity. Int J Obesity. 2006;30(6):993–1002. doi: 10.1038/sj.ijo.0803235. [DOI] [PubMed] [Google Scholar]
- 16.Kipnis V, Midthune D, Freedman L, Bingham S, Day NE, Riboli E, et al. Bias in dietary-report instruments and its implications for nutritional epidemiology. Public Health Nutr. 2002;5(6A):915–923. doi: 10.1079/PHN2002383. [DOI] [PubMed] [Google Scholar]
- 17.Heitmann BL, Lissner L. Dietary underreporting by obese individuals--is it specific or non-specific? BMJ. 1995;311(7011):986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arab L, Wesseling-Perry K, Jardack P, Henry J, Winter A. Eight Self-Administered 24-Hour Dietary Recalls Using the Internet Are Feasible in African Americans and Whites: The Energetics Study. J Am Diet Assoc. 2010;110(6):857–864. doi: 10.1016/j.jada.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sport Exer. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 20.Schoeller DA, Ravussin E, Schutz Y, Acheson KJ, Baertschi P, Jequier E. Energy-Expenditure by Doubly Labeled Water - Validation in Humans and Proposed Calculation. Am J Physiol. 1986;250(5):R823–R830. doi: 10.1152/ajpregu.1986.250.5.R823. [DOI] [PubMed] [Google Scholar]
- 21.Schoeller DA, Hnilicka JM. Reliability of the doubly labeled water method for the measurement of total daily energy expenditure in free-living subjects. J Nutr. 1996;126(1):S348–S354. [PubMed] [Google Scholar]
- 22.Schoeller DA. Recent advances from application of doubly labeled water to measurement of human energy expenditure. J Nutr. 1999;129(10):1765–1768. doi: 10.1093/jn/129.10.1765. [DOI] [PubMed] [Google Scholar]
- 23.Coward WA, Ritz P, Cole TJ. Revision of Calculations in the Doubly Labeled Water Method for Measurement of Energy-Expenditure in Humans. Am J Physiol-Endoc M. 1994;267(6):E805–E807. doi: 10.1152/ajpendo.1994.267.6.E805. [DOI] [PubMed] [Google Scholar]
- 24.Neuhouser ML, Tinker L, Shaw PA, Schoeller D, Bingham SA, Horn LV, et al. Use of recovery biomarkers to calibrate nutrient consumption self-reports in the Women's Health Initiative. Am J Epidemiol. 2008;167(10):1247–1259. doi: 10.1093/aje/kwn026. [DOI] [PubMed] [Google Scholar]
- 25.Trabulsi J, Troiano RP, Subar AF, Sharbaugh C, Kipnis V, Schatzkin A, et al. Precision of the doubly labeled water method in a large-scale application: Evaluation of a streamlined-dosing protocol in the Observing Protein and Energy Nutrition (OPEN) study. Eur J Clin Nutr. 2003;57(11):1370–1377. doi: 10.1038/sj.ejcn.1601698. [DOI] [PubMed] [Google Scholar]
- 26.Schoeller DA. Measurement of energy expenditure in free-living humans by using doubly labeled water. J Nutr. 1988;118(11):1278–1289. doi: 10.1093/jn/118.11.1278. [DOI] [PubMed] [Google Scholar]
- 27.Arab L, Tseng CH, Ang A, Jardack P. Validity of a multipass, web-based, 24-hour self-administered recall for assessment of total energy intake in blacks and whites. Am J Epidemiol. 2011;174(11):1256–1265. doi: 10.1093/aje/kwr224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arab L, Tseng C, Ang A, Jardack P. Validity of a multi-pass, web-based 24-hour self administered recall for assessment of total energy intake as strong among African Americans as Caucasians. Am J Epidemiol. In press doi: 10.1093/aje/kwr224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2009;89(1):372–381. doi: 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 30.R. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2008 [Google Scholar]
- 31.Freedman D. Centers for Disease Control and Prevention: Obesity - United States, 1998–2008. MMWR Morb Mortal Wkly Rep. 2010;60(Supple):73–77. [Google Scholar]
- 32.Apovian CM. Sugar-sweetened soft drinks, obesity, and type 2 diabetes. J Am Diet Assoc. 2004;292(8):978–979. doi: 10.1001/jama.292.8.978. [DOI] [PubMed] [Google Scholar]
- 33.Bray GA. How bad is fructose? Am J Clin Nutr. 2007;86(4):895–896. doi: 10.1093/ajcn/86.4.895. [DOI] [PubMed] [Google Scholar]
- 34.Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr. 2004;79(4):537–543. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 35.Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292(8):927–934. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 36.Pereira MA, Fulgoni VL3rd. Consumption of 100% fruit juice and risk of obesity and metabolic syndrome: findings from the national health and nutrition examination survey 1999–2004. J Am Coll Nutr. 2010;29(6):625–629. doi: 10.1080/07315724.2010.10719901. [DOI] [PubMed] [Google Scholar]
- 37.Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med. 2008 Jul 28;168(14):1487–1492. doi: 10.1001/archinte.168.14.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morand C, Dubray C, Milenkovic D, Lioger D, Martin JF, Scalbert A, Mazur A. Hesperidin contributes to the vascular protective effects of orange juice: a randomized crossover study in healthy volunteers. Am J Clin Nutr. 2011;93(1):73–80. doi: 10.3945/ajcn.110.004945. [DOI] [PubMed] [Google Scholar]
- 39.Wojcicki JM, Heyman MB. Reducing childhood obesity by eliminating 100% fruit juice. Am J Public Health. 2012;102(9):1630–1633. doi: 10.2105/AJPH.2012.300719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schoeller DA. Energy expenditure from doubly labeled water: some fundamental considerations in humans. Am J Clin Nutr. 1983;38(6):999–1005. doi: 10.1093/ajcn/38.6.999. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.