Abstract
There are numerous researches dealing with the correlation between the seasons and climatic factors and the pathogenesis of deep vein thrombosis (DVT). The presented researches show an undoubted correlation between the climatic factors and the pathogenesis of DVT. In the majority of researches, retrospection is noted as a disadvantage. Further prospective researches could aim on testing the correlation between both climatic and thrombotics factors and the pathogenesis of DVT. This may additionally clarify the pathophysiological mechanism of the DVT incidence and contribute to the prevention and treatment of risk groups of patients in certain periods of the year.
Keywords: Deep vein thrombosis, climatic factors, pathogenesis, prevention
Introduction
There are numerous researches dealing with correlation between the seasons and climatic factors and pathogenesis of deep vein thrombosis (DVT). The published results of the researches differ, which leads to further studies. It is assumed that the obtained results are controversial due to different methodology applied to conduct the researches, as well as to the fact that the influence of climatic factors is geographically dependent.
Correlation between seasons and pathogenesis of DVT
Only a few conducted researches show the absence of correlation between the seasons and pathogenesis of DVT. In Geneva, Bounameaux et al1conducted a retrospective study which included 7303 patients registered during the period from 1989 to 1994, with a suspected DVT. The presence of DVT was recorded in each seventh patient out of 300 patients with suspected DVT. The results of their research showed that there was no seasonal or monthly pattern concerning the occurrence of DVT for patients both with suspected and confirmed DVT. A retrospective research conducted by Galle et al, in Belgium2 during the period from 1982 to 1995, included 512 patients with a diagnosed lower limb DVT, also showed no correlation between the climatic factors and lower limb DVT. In their retrospective research in USA, which included data for a twenty-one-year period, Stein et al3 showed the absence of the seasonal character of DVT incidence. The absence of a correlation between the seasons and DVT incidence was also shown by Lee et al4 in a research which included 2774 patients with a diagnosed DVT in 2002 in Taiwan.
On the other hand, studies showing a correlation between the seasons and pathogenesis of DVT are far more numerous. A retrospective research by Boulay et al5 in France, which included 65081 patients with a diagnosed DVT, showed that the number of patients is far larger in winter than in the summer. The incidence of DVT for patients with protein C or protein S insufficiency was more frequent in the winter6. In Austria, Fink et al7 conducted a research which included 905 patients with a diagnosed lower limb DVT. The research showed a seasonal pattern in the incidence of lower limb DVT, which was significantly more frequent during the cold period of the calendar year (October – March). This study, which observed a correlation between the seasons and the location of lower limb DVT, showed that DVT below the knees was more frequent during the cold period of the year, while DVT above the knees was more frequent during the warm period (April – September).
Manfredini et al8 conducted a retrospective research which included 2119 patients with a diagnosed DVT, according to the data provided by 25 Italian hospitals, for the period from 2002 to 2004. The results showed that the incidence of DVT followed a rhythmical pattern, with its peak in September and October, and was the most frequent for men aged over 40, patients who had previously suffered a DVT and in immobilized patients. Brown et al9 conducted a retrospective research which included 37336 patients with DVT, based on data obtained from Scottish hospitals for a twenty year period. The results proved a seasonal pattern of DVT incidence, with its peak in the winter. Dentali et al10,11 conducted researches as well as a meta-analysis which confirmed the seasonal character of DVT with its peak during the winter in January. In this meta-analysis, which included about 35,000 patients, 12 studies implied a research on the seasonal variations of DVT, while 10 studies observed monthly variations of DVT.
The study conducted by Jang et al12 in Korea, included 1495 patients with DVT during the period from 2001 to 2010 and confirmed the seasonal character of DVT with its peak during the winter and in January. A retrospective research on the territory of South Serbia showed a seasonal pattern in the incidence of the idiopathic lower limb DVT with the highest frequency in the cold period of the year (October – March) and the peak in January13.
There are different explanations for the seasonal character of DVT. An acute, mainly respiratory infection, which is more frequent in the winter, increases the risk for DVT incidence14. Infection increases the concentration of fibrinogen, anticardiolipid antibodies and the C protein level, which leads to hypercoagulability that can be the reason for the DVT incidence15-17. In this respect, Masoti et al18 conducted a research which showed a statistically significantly higher level of C reactive protein, D–dimer and the platelets during the winter than in the summer, whereas Keatinge et al19 showed that the level of fibrinogen and the VII c coagulation factor were higher in the winter than during the summer period. During the cold periods, peripheral vasoconstriction and decreased physical activity may also be one of the reasons for higher frequency of DVT during the winter7.
Correlation between atmospheric temperature and the pathogenesis of DVT
Cold conditions make changes in the erythrocytes quality and in the number of leucocytes, increase the number of granulocytes and decrease the number of lymphocytes, which indicates the possibility of a potential cause for the development of inflammation and hypercoagulability20-21.
Exposure to low temperature in the winter period can be a risk factor for DVT incidence22. Chung et al23 conducted a study in 24 centers from 17 countries from Africa, Asia, Europe and South America (including the Caribbean). The study showed that a change of temperature for 5°C was not related to DVT incidence. A research conducted by Brown et al9 showed that the seasonal pattern in the incidence of DVT was related to the minimum and maximum temperature during a calendar year.
Explanations concerning the effect of temperature on DVT can be found in the results obtained from experimental researches. Marcer et al24 showed that a short-term exposure to cold performed by healthy volunteers, leads to haemoconcentration caused by the increase in the number of erythrocytes and granulocytes. Kawahara et al25 reported that exposure to cold conditions performed by healthy volunteers resulted in the increased activity of platelets, being thus a potential factor affecting the pathogenesis of DVT.
Correlation between atmospheric pressure and the pathogenesis of DVT
An experimental study conducted by LaCroix et al26 showed that the change of atmospheric pressure did not lead to hemostasis disorder. Esquenet et al27 proved a correlation between atmospheric pressure and DVT. Brown et al9 reported that each decrease of atmospheric pressure for 10 millibars, nine days before DVT was diagnosed, was related to the increase of the DVT incidence by 2.1%. A retrospective study which included patients from Niš, showed a correlation between the incidence of lower limb DVT and the increase of atmospheric pressure. Each change of atmospheric pressure for 1 millibar on the day of the DVT diagnosis and 7 days before that, was related to the increase of the incidence of lower limb DVT of 5.1%, as well as the increase of the incidence of the above-knee DVT of 5.9%28.
Correlation between air pollution and the pathogenesis of DVT
Researches dealing with the correlation between air pollution and the incidence of DVT reported the existence of such correlation. Baccarelli et al29 were the first to study the relation between DVT and air pollution. Compared to the control group, patients with DVT had higher exposure to particles with the aerodynamic diameter of 10 micrometers. The second study conducted by Baccarelli et al30 showed a correlation between air pollution and DVT in subjects residing near large traffic crossroads. A research conducted in Santiago, Chile31, showed that the increased concentrations of ozone, sulphordioxide, nitrodioxide and the increased number of particles smaller than or the same size as the size of the aerodynamic diameter of 2.5 micrometers, were related to the increased incidence of DVT.
There are many hypotheses explaining this correlation. A direct effect would be explained by hypercoagulability of vein circulation. An indirect effect of air pollution could be hypothetically explained by the increased number of lung and heart diseases32,33 which increase the possibility for DVT incidence.
Correlation among rain fall and wind speed with pathogenesis of DVT
Brown et al9 showed that increased rain fall by 1 mm and increased wind speed by 1 nod, 10 days before diagnosing DVT, caused an increase of the DVT incidence by 0.8% and 0.6% respectively. The authors stated that the mechanisms of correlation between the climatic factors and DVT are so far unknown and deserve further clarification.
The main characteristics of the studies which connect the influence of the climatic factors and the pathogenesis of DVT, are shown in Table 1.
Table 1. The studies which connect the influence of climatic factors and pathogenesis of DTV.
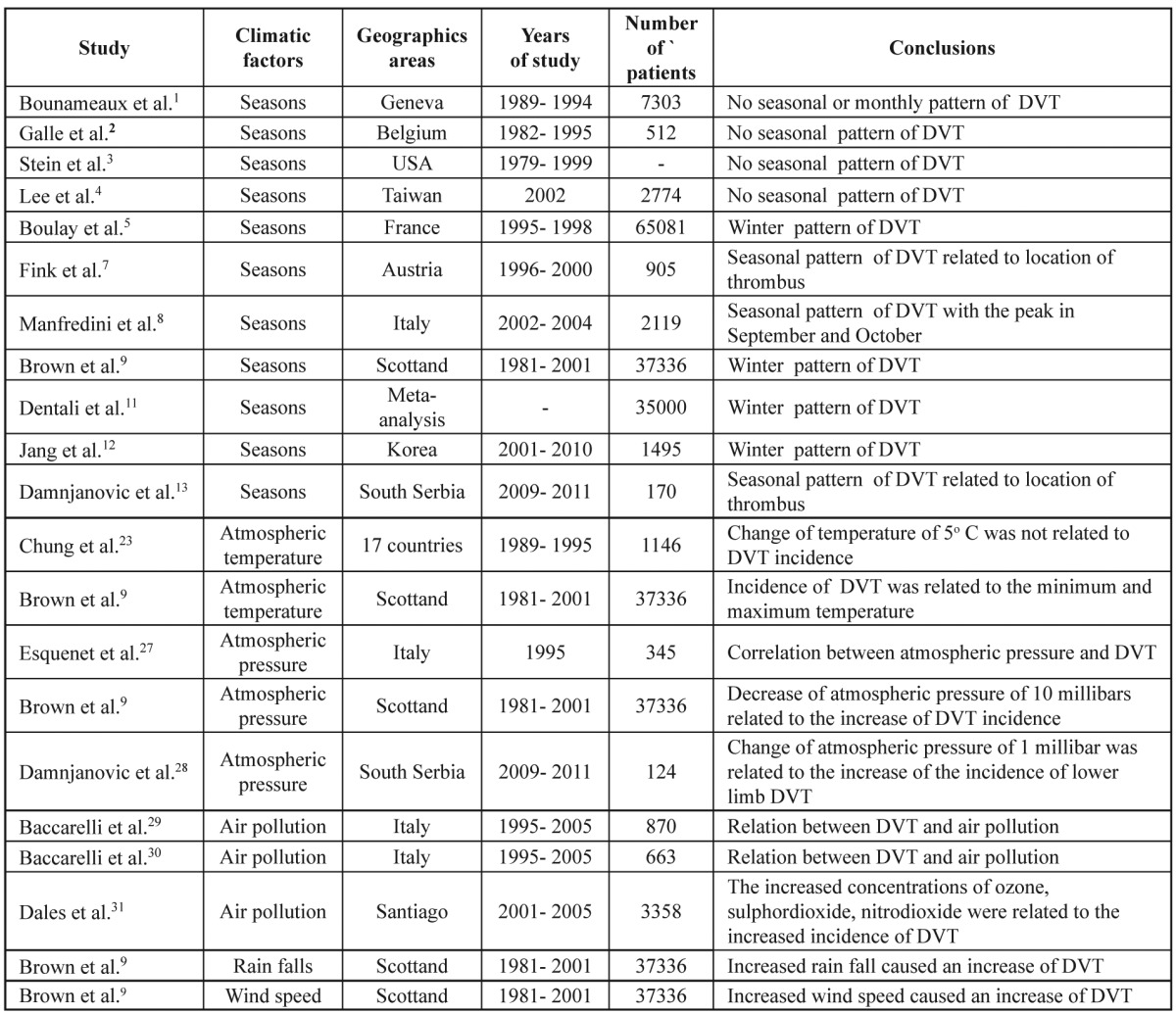
DVT: deep vein thrombosis
Conclusion
The presented researches show a positive correlation between climatic factors and the pathogenesis of DVT. In the majority of the researches, retrospection is a disadvantage. Therefore, further prospective studies should aim on testing the correlation between both the climatic and the thrombotic factors and the pathogenesis of DVT. This would additionally clarify the pathophysiological mechanism of the DVT incidence and contribute to the prevention and treatment of risk groups of patients in various periods of the year.
Conflict of Interest
The authors have no competing interests to declare
References
- 1.Bounameaux H, Hicklin L, Desmarais S. Seasonal variation in deep vein thrombosis. BMJ. 1996;312:284–285. doi: 10.1136/bmj.312.7026.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galle C, Wautrecht JC, Motte S, Le Minh T, Dehon P, Ferreira J, et al. [The role of season in the incidence of deep vein thrombosis] J Mal Vasc. 1998;23:99–101. [PubMed] [Google Scholar]
- 3.Stein PD, Kayali F, Olson RE. Analysis of occurrence of venous thromboembolic disease in the four seasons. Am J Cardiol. 2004;93:511–513. doi: 10.1016/j.amjcard.2003.10.061. [DOI] [PubMed] [Google Scholar]
- 4.Lee CH, Cheng CL, Lin LJ, Tsai LM, Yang YH. Epidemiology and predictors of short-term mortality in symptomatic venous thromboembolism. Circ J. 2011;75:1998–2004. doi: 10.1253/circj.cj-10-0992. [DOI] [PubMed] [Google Scholar]
- 5.Boulay F, Berthier F, Schoukroun G, Raybaut C, Gendreike Y, Blaive B. Seasonal variations in hospital admission for deep vein thrombosis and pulmonary embolism: analysis of discharge data. BMJ. 2001;323:601–602. doi: 10.1136/bmj.323.7313.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bilora F, Boccioletti V, Manfredini E, Petrobelli F, Tormene D, Simioni P, et al. Seasonal variation in the incidence of deep vein thrombosis in patients with deficiency of protein C or protein S. Clin Appl Thromb Hemost. 2002;8:231–237. doi: 10.1177/107602960200800306. [DOI] [PubMed] [Google Scholar]
- 7.Fink AM, Mayer W, Steiner A. Seasonal variations of deep vein thrombosis and its influence on the location of the thrombus. Thromb Res. 2002;106:97–100. doi: 10.1016/s0049-3848(02)00094-4. [DOI] [PubMed] [Google Scholar]
- 8.Manfredini R, Imberti D, Gallerani M, Verso M, Pistelli R, Aqueno W, et al. Seasonal variation in the occurrence of venous thromboembolism: data from the MASTER Registry. Clin Appl Thromb Hemost. 2009;15:309–315. doi: 10.1177/1076029608319947. [DOI] [PubMed] [Google Scholar]
- 9.Brown HK, Simpson AJ, Murchison JT. The influence of meteorological variables on the development of deep venous thrombosis. Thromb Haemost. 2009;102:676–682. doi: 10.1160/TH09-04-0214. [DOI] [PubMed] [Google Scholar]
- 10.Dentali F, Manfredini R, Ageno W. Seasonal variability of venous thromboembolism. Curr Opin Pulm Med. 2009;15:403–407. doi: 10.1097/MCP.0b013e32832d867a. [DOI] [PubMed] [Google Scholar]
- 11.Dentali F, Ageno W, Rancan E, Donati AV, Galli L, Squizzato A, et al. Seasonal and monthly variability in the incidence of venous thromboembolism. A systematic review and a meta-analysis of the literature. Thromb Haemost. 2011;106:439–447. doi: 10.1160/TH11-02-0116. [DOI] [PubMed] [Google Scholar]
- 12.Jang MJ, Kim HJ, Bang SM, Lee JO, Yhim HY, Kim YK, et al. Seasonal variation in the occurrence of venous thromboembolism: a report from the Korean Venous Thromboembolism Working Party. Thromb Res. 2012;13:e199–e202. doi: 10.1016/j.thromres.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Damnjanovic Z, Jovanovic M, Ilic N, Bogdanovic D, Kudumovic A, Kamenov A, et al. Seasonal variations in the incidence of idiopathic lower extremity deep vein thrombosis on the territory of South Serbia. HealthMED. 2012;6:2477–2481. [Google Scholar]
- 14.Malone PC, Agutter PS. To what extent might deep venous thrombosis and chronic venous insufficiency share a common etiology? Int Angiol. 2009;28:254–268. [PubMed] [Google Scholar]
- 15.Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet. 2006;367:1075–1079. doi: 10.1016/S0140-6736(06)68474-2. [DOI] [PubMed] [Google Scholar]
- 16.Stout RW, Crawford V, et al. Seasonal variations in fibrinogen concentrations among elderly people. Lancet. 1991;338:9–13. doi: 10.1016/0140-6736(91)90004-9. [DOI] [PubMed] [Google Scholar]
- 17.Macko RF, Ameriso SF, Gruber A, Griffin JH, Fernandez JA, Barndt R, et al. Impairments of the protein C system and fibrinolysis in infection-associated stroke. Stroke. 1996;27:2005–2011. doi: 10.1161/01.str.27.11.2005. [DOI] [PubMed] [Google Scholar]
- 18.Masotti L, Ceccarelli E, Forconi S, Cappelli R. Seasonal variations of pulmonary embolism in hospitalized patients. Respir Med. 2005;99:1469–1473. doi: 10.1016/j.rmed.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelets and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J (Clin Res Ed) 1984;289:1405–1408. doi: 10.1136/bmj.289.6456.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neild J, Syndercombe-Court D, Keatinge WR, Donaldson GC, Mattock M, Caunce M. Cold-induced increases in erythrocyte count, plasma cholesterol and plasma fibrinogen of elderly people without a comparable rise in protein C or factor X. Clin Sci (Lond) 1994;86:43–48. doi: 10.1042/cs0860043. [DOI] [PubMed] [Google Scholar]
- 21.Hawes AS, Fischer E, Marano MA, Van Zee KJ, Rock CS, Lowry SF, et al. Comparison of peripheral blood leukocyte kinetics after live Escherichia coli, endotoxin or interleukin-1 alpha administration. Studies using a novel interleukin-1 receptor antagonist. Ann Surg. 1993;218:79–90. doi: 10.1097/00000658-199307000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schuh A. [Not good for weak veins. Winter temperature promote thrombus formation] MMW Fortschr Med. 2003;145:31–32. [PubMed] [Google Scholar]
- 23.Chang CL, Shipley M, Marmot M, Poulter N. Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol. 2004;57:749–757. doi: 10.1016/j.jclinepi.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Mercer JB, Osterud B, Tveita T. The effect of short-term cold exposure on risk factors for cardiovascular disease. Thromb Res. 1999;95:93–104. doi: 10.1016/s0049-3848(99)00028-6. [DOI] [PubMed] [Google Scholar]
- 25.Kawahara J, Sano H, Fukuzaki H, Saito K, Hirouchi H. Acute effects of exposure to cold on blood pressure, platelet function and sympathetic nervous activity in humans. Am J Hypertens. 1989;2:724–726. doi: 10.1093/ajh/2.9.724. [DOI] [PubMed] [Google Scholar]
- 26.LaCroix KA, Davis GL, Schneider DA, Lavoie P, Kintzing E, Waterfield DA. The effects of acute exercise and increased atmospheric pressure on the hemostatic mechanism and plasma catecholamine levels. Thromb Res. 1990;57:717–728. doi: 10.1016/0049-3848(90)90029-c. [DOI] [PubMed] [Google Scholar]
- 27.Esquenet APD, Boudet J, Sevestre-Pietri MA, Ganry O, Pietri J. [Effect of meteorological variations on the emergence of deep venous thrombosis of the leg] J Mal Vasc. 1997;22:244–248. [PubMed] [Google Scholar]
- 28.Damnjanović Z, Jovanović M, Bogdanović D, Smiljković I, Ilić N, Damnjanović I. Relationship between the incidence of idiopathic lower extremity deep vein thrombosis and the location of the thrombus depending on the changes of atmospheric pressure. Chirurgia (Bucur) 2012;107:483–487. [PubMed] [Google Scholar]
- 29.Baccarelli A, Martinelli I, Zanobetti A, Grillo P, Hou LF, Bertazzi PA, et al. Exposure to particulate air pollution and risk of deep vein thrombosis. Arch Intern Med. 2008;168:920–927. doi: 10.1001/archinte.168.9.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baccarelli A, Martinelli I, Pegoraro V, Melly S, Grillo P, Zanobetti A, et al. Living near major traffic roads and risk of deep vein thrombosis. Circulation. 2009;119:3118–3124. doi: 10.1161/CIRCULATIONAHA.108.836163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dales RE, Cakmak S, Vidal CB. Air pollution and hospitalization for venous thromboembolic disease in Chile. J Thromb Haemost. 2010;8:669–674. doi: 10.1111/j.1538-7836.2010.03760.x. [DOI] [PubMed] [Google Scholar]
- 32.Martinelli N, Girelli D, Ciqolini D, Sandri M, Ricci G, Rocca G, et al. Access rate emergency department for venous thromboembolism in relationship with coarse and fine particulate matter air pollution. PloS One. 2012;7:e34831. doi: 10.1371/journal.pone.0034831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baccarelli A, Zanobetti A, Martinelli I, Grillo P, Hou L, Giacomini S, et al. Effects of exposure to air pollution on blood coagulation. J Thromb Haemost. 2007;5:252–260. doi: 10.1111/j.1538-7836.2007.02300.x. [DOI] [PubMed] [Google Scholar]


