Abstract
Introduction: Acute kidney injury (AKI) may result in complete recovery in some of the patients and partial recovery in others. AKI episodes may accelerate the progression to chronic kidney disease and end-stage renal failure, while risk for morbidity and mortality is high following AKI. Discharge of patients from the hospital, independently from dialysis is a crucial outcome. Many patients without a need for dialysis, require follow-up for various durations and different treatments. The objective of this study was to compare mean recovery time of the patients followed-up due to prerenal, renal and postrenal AKIs.
Method: In this prospective observational study, a total of 159 patients hospitalized in Bulent Ecevit Hospital, clinic of nephrology or monitored in the other wards and intensive care unit due to AKI, between June 2011 and January 2012, were enrolled. The cases were divided into three groups as prerenal, renal and postrenal, and monitored with the daily visits and renal function testing.
Results: Prerenal AKI was seen by 54%, while renal AKI was observed by 34% and post-renal AKI by 12%. Incidence of chronic kidney disease was 17.6%. Totally 43 patients required hemodialysis (27%). Of these patients, 23 were in the prerenal AKI (53.4%), 15 in the renal AKI (34.8%) and 5 (11.6%) in the postrenal AKI group. Blood urea nitrogen (BUN) and creatinine levels were dropped to the basal values only in the prerenal AKI group, on the seventh day of treatment. These levels remained higher in the postrenal and renal groups on the 7th day of treatment compared to the basal values. BUN levels decreased to the normal values on average 7th day in the postrenal, while remained higher in the renal group.
Conclusion: Prerenal AKI patients recovered in seven days with a proper treatment, although AKI patients due to other reasons should be followed-up for a longer time.
Keywords: Acute kidney injury, prerenal, renal, postrenal acute kidney injury, recovery time
Introduction
In acute kidney injury (AKI), an abrupt decrease in the renal function occurs within hours and days, resulting in fluid and electrolyte imbalance. Acute kidney injury is relatively common with an incidence about 80/million population/year. Numerous factors including aging, sepsis, cardiovascular and pulmonary regurgitation are associated with increased risk of AKI development. AKI may be seen in a wide range from mild renal function loss to end-stage renal failure requiring dialysis. AKI involves 5-7% of hospitalized patients and affects 1% to 25% of the patients in intensive care units (ICUs) with morbidity and mortality rates between 15% and 60%1,2. AKI is also associated with increased rate of morbidity and mortality caused by chronic renal failure and end-stage kidney disease in the long term3,4. RIFLE (Risk, Injury, Failure, Loss, and End-stage kidney disease) criteria are important for diagnosis, treatment and definition of prognosis in AKI. According to the RIFLE criteria, acute renal failure has been defined with risk, injury, failure, loss of the renal functions and end-stage kidney disease5. “Risk” is defined as serum creatinine (SCr) increase to 1.5 fold or glomerular filtration rate (GFR) decrease >25% from basaline and <0,5ml/kg/h for 6 hours urine output. “Injury” is inrease in SCr of 2.0 fold or GFR decrease >50% from basaline and <0,5ml/kg/h for 12 hours urine output. “Failure” is inrease in SCr of 3.0 fold or GFR decrease >75% from basaline or SCr >4mg/dl or <0,3ml/kg/h for 24 hours urine output or anuria for 12 hours. “Loss” is known as duration for >4 week of persistent acute renal failure. The last stages are defined by >3 month of complete loss of kidney function (“End-stage kidney disease”)6. Subsequently, AKI has been defined according to the AKIN criteria as an increase of the serum level of creatinine ≥0,3 mg/dl or ≥50% compared to the basal value or presence of oliguria for longer than 6 hours (<0,5 ml/kg/hour)6. In several studies, mild forms of AKI were also shown to be associated with increased risk for mortality7-10. The issue of how long the patients who developed AKI should be followed is not clear11-13. In this study, we assessed how long AKI patients who were consulted should be followed-up.
Materials and Methods
In this prospective observational study, patients hospitalized in Bulent Ecevit University Hospital, Clinic of Nephrology or monitored in the other wards and intensive care units due to AKI, between June 2011 and January 2012, were enrolled. Patients aged 18 or older with a level of creatinine increased by ≥0.3 mg/dL or ≥%50 were considered as to have AKI and included in the study4,5. AKI was defined according to the serum level of creatinine, urine output and need for renal replacement therapy. Patients were divided into three groups according to the causes of AKI, as prerenal, renal and postrenal. At the daily visits, blood urea nitrogen (BUN), creatinin, sodium, potassium, chloride, calcium, magnesium, phosphorus, uric acid, hemoglobin, hematocrit, white blood cells, platelets and fluid input-output amounts were monitored. The difference in mean values between intra- and inter- groups were evaluated with the student’s t-test and values of p<0.05 were considered as significant.
Results
A total of 159 patients with 78 females, having a mean age of 67 ± 16.4 years were included in the study. Majority of the patients followed-up were in the clinic of nephrology (31%) and cardiovascular clinic (15%) (Figure 1). AKI was due to prerenal in 54%, renal in 34% and postrenal reasons in 12% of the patients. Acute exacerbation on chronic kidney disease (CKD) basis was observed in 17.6% of the patients. Hemodialysis was needed in a total of 43 (27%) patients. Of these patients, 23 (53.4%) were in the prerenal, 15 (34.8) in the renal, and 5 (11.6%) in the postrenal AKI group. No significant difference was found between the groups in terms of the demographic data and laboratory tests, on the first day of treatment. BUN and creatinine levels were dropped to the basal values only in the prerenal AKI group on the seventh day of treatment (Figure 2 and Figure 3). Creatinin levels in prerenal group: 3.0 mg/dL, in renal group: 3.0 mg7dl, in postrenal group: 5.8 mg/dL. These levels remained higher in the postrenal and renal groups on the 7th day of treatment compared to the basal values (Figure 3). BUN levels decreased to the normal values on average on the 7th day, in the postrenal group, while remained higher in the renal group. Levels of hematocrit and white blood cells were significantly decreased in the postrenal AKI group than in the prerenal and renal AKI group. Serum levels of potassium were significantly decreased in all the groups. Serum levels of magnesium were significantly decreased in the prerenal and renal AKI groups, while phosphorus level was decreased only in the prerenal group (Table 1).
Figure 1. Clinics that follow up of patient with acute kidney injury %.
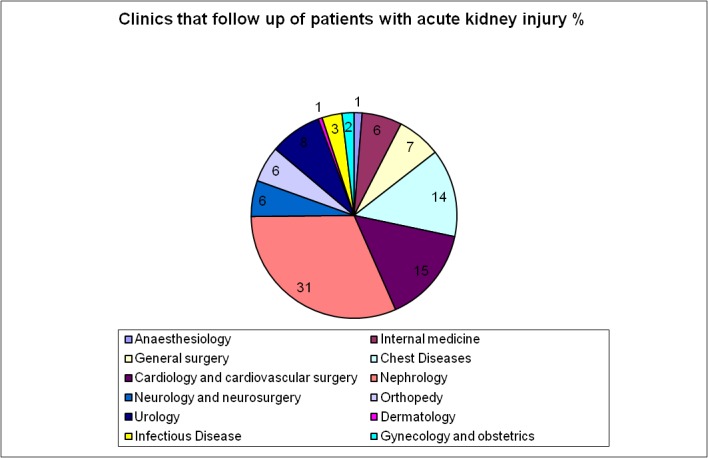
Figure 2. Follow up of patients with acute kidney injury. AKI: Acute kidney injury.
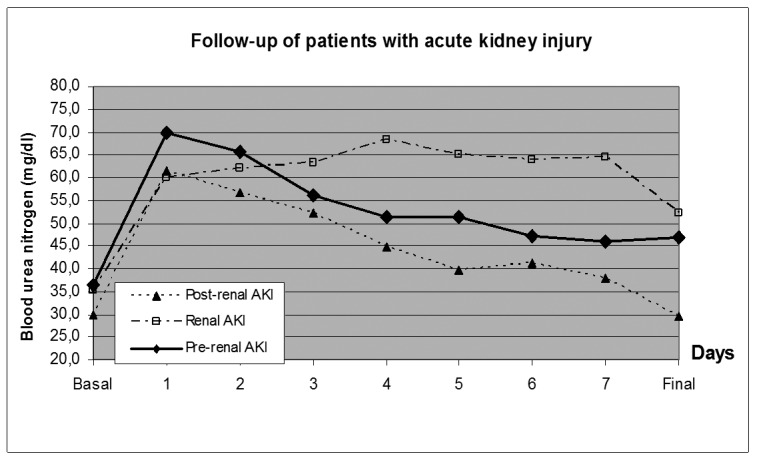
Figure 3. Follow up of patients with acute kidney injury. AKI: Acute kidney injury.
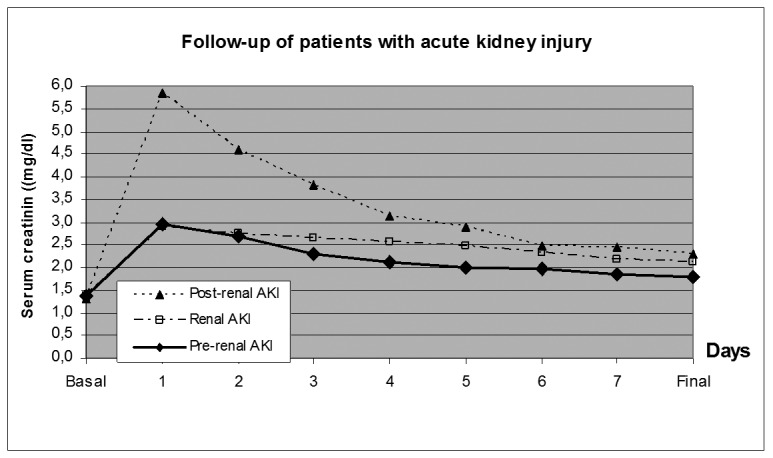
Table 1. Laboratory results of the prerenal, renal and post renal, acute kidney injury groups.
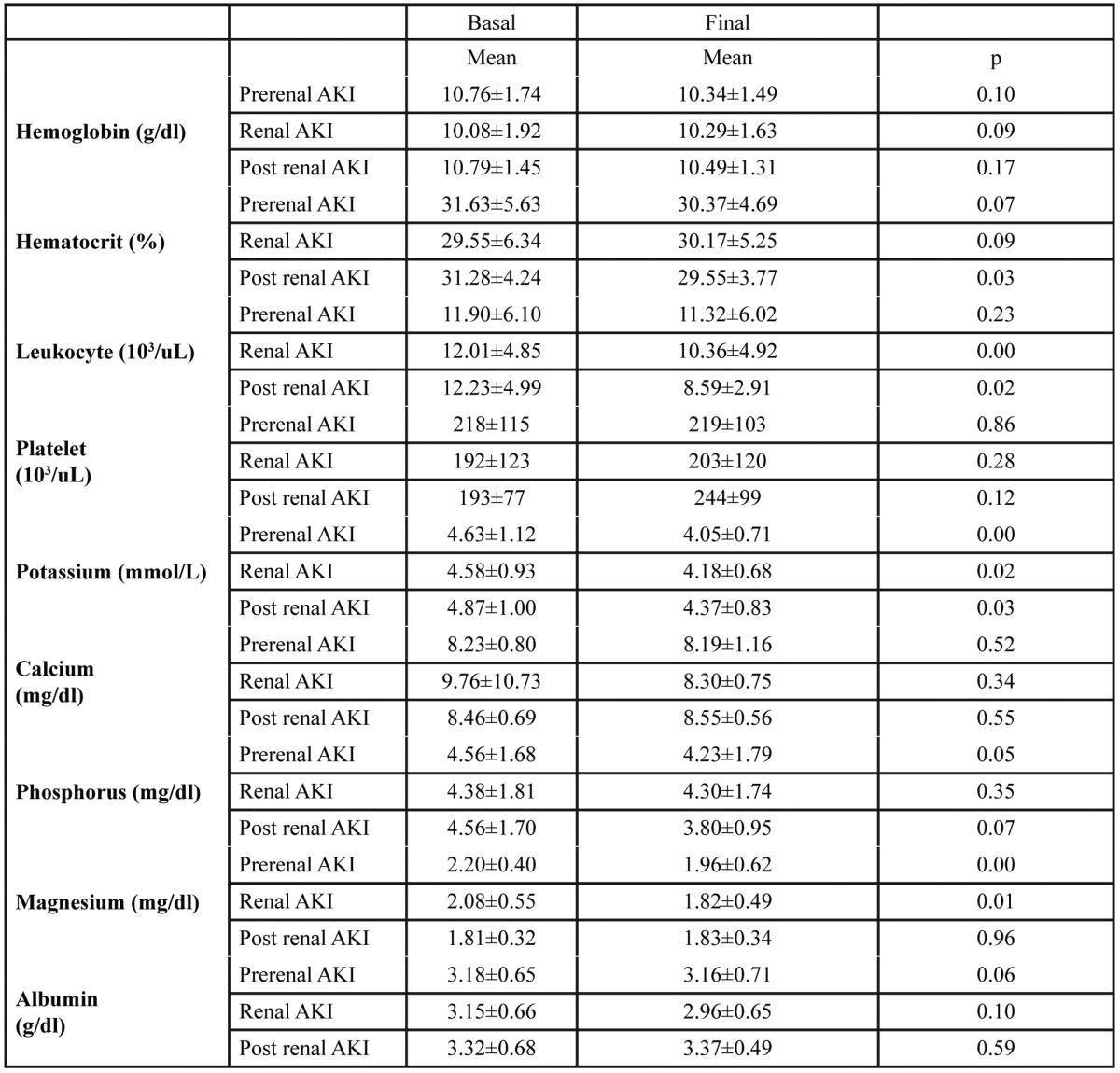
AKI: Acute kidney injury
Discussion
The kidneys are directly influenced by disorders of all the organ and systems in the body. Nephrologists are frequently been consulted, especially by acute kidney injury (AKI) patients from the external services. There is an acute condition in AKI, that may vary from a few hours to months and progresses from complete or partial recovery to death. In many observational studies in the literature, patient monitoring has been carried out, most commonly in the special groups of patients, who were admitted to intensive care units and had undergone cardiac catheterization and coronary bypass surgery14-16. In this study, most of the follow-ups of AKI patients were performed in the clinic of nephrology. This different distribution was resulted from AKI patients whom follow-ups were carried out on our behalf in intensive care units. In the patients diagnosed with acute renal failure, the factors used to define the need for renal replacement therapy included one or more of the symptoms of severe metabolic acidosis, hyperkalemia, hypervolemia, oliguria and anuria. HD and UF were carried out in all three groups, in the patients who hemodialysis (HD) and ultrafiltration (UF). In a study by Medcalfe et al, besides the patients with a normal renal function before acute kidney injury, 16% of the patients had CKD and only 3% of these patients were reported to need HD17. In this study, 43 (27%) from a total of 159 patients required hemodialysis. There was exacerbated acute kidney injury on CKD basis in 17.6% of these patients. Dialysis was needed in 53.4% of the prerenal, 34.4% of the renal and 11.6% postrenal AKI patients. In the follow-up of 425 patients with acute tubular necrosis, Schiffle reported that 57% of the patients returned to normal at discharge (Cr < 1.3 mg/dl), 33% of the patients had a level of creatinine between 1.3 and 3 mg/dl, and 10% of the patients had creatinine levels between 3 and 6 mg/dl and required dialysis18. Bagshaw et al stated that renal recovery occurred after 90 days in the patients with severe acute kidney injury19. In our study, BUN and creatinine levels were dropped to the basal values in the prerenal AKI group on the seventh day of treatment, although renal functions at the discharge did not reach the basal values in the patients with renal and postrenal acute kidney injury. Serum levels of potassium were significantly improved in all groups. This improvement might be attributed to the improvement of metabolic acidosis and recovery of the renal functions with the effective treatment carried out. Levels of magnesium were significantly decreased in the prerenal and renal AKI groups. A large percent of the total plasma magnesium is filtered at the glomerulus. Continued intake leads to hypermagnesemia, with loss of the renal function20. Elevated levels of magnesium can cause muscle contraction, seizures and coronary spasm, directly or by increasing the effects of uremic toxins. In addition, magnesium may increase sensitivity to cardiac arrhythmia similar to potassium20. In this study, levels of magnesium that were close to the upper limit, significantly decreased in the prerenal and renal AKI groups. Serum levels of phosphorus were increased whom oliguric patients ratio was high in prerenal AKI group than the renal and postrenal AKI group. Similarly, serum levels of phosphorus were decreased only in the prerenal AKI group. This might be attributable to the renal functions being normal (GFR above 90% or creatinine under 1.3 ml/dl) before development of acute kidney injury in the prerenal AKI group. In our study, postrenal AKI group was composed of 19 patients. In this group, surgical intervention caused intraoperative hemorrhage in three patients. This may lead the hematocrit decrease in the postrenal group. Such as urinary stones and urinary tract infections may be the reason to cause leukocytosis in postrenal AKI group. White blood cells were significantly decreased in the postrenal AKI group that albumin levels increased from 3.32 to 3.37 g/dl, indicating the recovery of inflammation and infection. Presence of the factors such as elevated serum creatinine, age and comorbidity during discharge are associated with a poor prognosis. As a result of the follow-ups and treatments administered, prerenal AKIs were observed to recover in average 7 days. Postrenal AKIs due to other reasons recovered later, while renal functions did not completely recover in the renal AKIs. Patients in these groups should be followed-up for a longer time.
Conflict of Interest
Authors report no conflict of interest.
References
- 1.Dennen P, Douglas IS, Anderson R. Acute kidney injury in the intensive care unit: an update and primer for the intensivist. Crit Care Med. 2010;38:261–275. doi: 10.1097/CCM.0b013e3181bfb0b5. [DOI] [PubMed] [Google Scholar]
- 2.Waikar SS, Liu KD, Chertow GM. Diagnosis, epidemiology, and outcomes of acute kidney injury. Clin J Am Soc Nephrol. 2008;3:844–861. doi: 10.2215/CJN.05191107. availiable from: http://globocan.iarc.fr/factsheet.asp, accessed 19/12/2012. [DOI] [PubMed] [Google Scholar]
- 3.Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365–3370. doi: 10.1681/ASN.2004090740. [DOI] [PubMed] [Google Scholar]
- 4.Coca SG, Peixoto AJ, Garg AX, Krumholz H, Parikh CR. The prognostic importance of a small acute decrement in kidney function in hospitalized patients: a systematic review and meta-analysis. Am J Kidney Dis. 2007;50:712–720. doi: 10.1053/j.ajkd.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 5.Kellum JA, Mehta RL, Angus DC, Palevsky P, Ronco C. ADQI Workgroup. The first international consensus conference on continuous renal replacement therapy. Kidney Int. 2002;62:1855–1863. doi: 10.1046/j.1523-1755.2002.00613.x. [DOI] [PubMed] [Google Scholar]
- 6.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;31:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 8.Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ricci Z, Cruz D, Ronco C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 2008;73:538–546. doi: 10.1038/sj.ki.5002743. [DOI] [PubMed] [Google Scholar]
- 10.Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med. 2006;34:1913–1917. doi: 10.1097/01.CCM.0000224227.70642.4F. [DOI] [PubMed] [Google Scholar]
- 11.Chertow GM, Christiansen CL, Cleary PD, Munro C, Lazarus JM. Prognostic stratification in critically ill patients with acute renal failure requiring dialysis. Arch Intern Med. 1995;155:1505–1511. [PubMed] [Google Scholar]
- 12.Spiegel DM, Ullian ME, Zerbe GO, Berl T. Determinants of survival and recovery in acute renal failure patients dialyzed in intensive-care units. Am J Nephrol. 1991;11:44–47. doi: 10.1159/000168271. [DOI] [PubMed] [Google Scholar]
- 13.Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30:2051–2058. doi: 10.1097/00003246-200209000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, et al. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol. 2006;17:2871–2877. doi: 10.1681/ASN.2006030301. [DOI] [PubMed] [Google Scholar]
- 15.Gruberg L, Mintz GS, Mehran R, Gangas G, Lansky AJ, Kent KM, et al. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol. 2000;36:1542–1548. doi: 10.1016/s0735-1097(00)00917-7. [DOI] [PubMed] [Google Scholar]
- 16.Lassnigg A, Schmid ER, Hiesmayr M, Falk C, Druml W, Bauer P, et al. Impact of minimal increases in serum creatinine on outcome in patients after cardiothoracic surgery: do we have to revise current definitions of acute renal failure? Crit Care Med. 2008;36:1129–1137. doi: 10.1097/CCM.0b013e318169181a. [DOI] [PubMed] [Google Scholar]
- 17.Metcalfe W, Simpson M, Khan IH, Prescott GJ, Simpson K, Smith WC, et al. Acute renal failure requiring renal replacement therapy: incidence and outcome. QJM. 2002;95:579–583. doi: 10.1093/qjmed/95.9.579. [DOI] [PubMed] [Google Scholar]
- 18.Schiffl H. Renal recovery from acute tubular necrosis requiring renal replacement therapy: a prospective study in critically ill patients. Nephrol Dial Transplant. 2006;21:1248–1252. doi: 10.1093/ndt/gfk069. [DOI] [PubMed] [Google Scholar]
- 19.Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care. 2005;9:700–709. doi: 10.1186/cc3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kielstein JT, David S. Magnesium: the ‘earth cure’ of AKI? Nephrol Dial Transplant. 2013;28:785–787. doi: 10.1093/ndt/gfs347. [DOI] [PubMed] [Google Scholar]


