Abstract
Pain reports have become increasingly common and problematic in thalassemia. As patients are living longer, there is a growing need to study pain and explore its impact on patient lives. The Brief Pain Inventory (BPI) was used quarterly to assess pain and pain interference in North American thalassemia patients. The SF-36 and HADS were used to assess quality of life, anxiety, and depression. Of the 252 participants, 56% reported pain at least once over the course of this study, with 32% reporting severe pain (≥7/10); 16% reported pain at all 4 visits. Increased pain severity significantly interfered with daily life (p<0.001; regression analysis), and participants with more sites of pain showed an increase in the amount of daily activities affected by pain (p=0.001). Participants reporting more visits with pain reported a significantly higher impact on affective and physical function (p <0.001). Physical quality of life decreased with increasing numbers of visits with pain (p <0.001). Those who reported one or more sites of pain showed increased symptoms of both depression (p <0.001) and anxiety (p= 0.003). Participants reporting at least two visits with pain had higher symptoms of anxiety (p= 0.002), and those with at least three visits, higher symptoms of depression (p= 0.003). Pain in thalassemia is a common, often chronic condition that interferes with life. The study highlights the significance of pain in thalassemia and its impact should be considered in future research and treatments.
Keywords: Thalassemia, Pain, Quality of Life
INTRODUCTION
Thalassemia is a group of inherited blood disorders that decrease hemoglobin production which can lead to mild or severe anemia [2]. Due to the wide variability in clinical severity, patients may require no intervention, while others need chronic blood transfusions and iron chelation therapy to remove excess iron in the body [2]. The accumulation of tissue iron is the leading cause of morbidity and mortality in thalassemia [4].
New developments in transfusion strategies, diagnostic testing and iron chelation therapies have resulted in extended life spans for patients with thalassemia [1–4]. Once known as a fatal disease, thalassemia has evolved into a chronic illness [3]. Effective disease management has increased survival into adulthood and has given patients the opportunity to achieve personal goals [2,3,5,6]. However, prolonged life expectancy has also revealed problems that are not well-understood [1,2,6]. Pain has become increasingly common and an emergent complication of thalassemia [5,7].
There are a limited number of studies that have observed pain as a significant problem in thalassemia. Scalone identified 62% of thalassemia patients on chelation reporting pain, although only 1% reported extreme pain [21]. 34% of participants reported bone pain in the Low Bone Mass Cross-sectional Observational Study (LBMCOS) [8]. Data from the Thalassemia Longitudinal Cohort (TLC) study showed 56% of children experience pain, with 11% reporting frequent pain in a 4 week period [7]. Pain increased significantly with age, with 69% of the adults/adolescents reporting bodily pain in the past 4 weeks, and 28% of those reporting at least moderate pain [7]. While these reports support that pain is problematic in thalassemia, the data describes pain at one point in time. Unlike these analyses, this pilot study examined pain longitudinally, at four time points, which solely focused on pain and its effects on quality of life.
Quality of life is known as an important indicator of overall well-being and has become a valuable tool in measuring the impact chronic illness has on everyday life [11,12]. Assessing quality of life makes it possible to measure disease burden and can be used to help determine risk factors that may lead to poor quality of life [11,12]. Published reports have shown that quality of life is significantly impaired in patients with hemoglobinopathies [2,11–14]. According to the PISCES study, patients with Sickle Cell Disease experience poorer quality of life than the general U.S. population [13]. Studies conducted in patients with thalassemia have also described poor quality of life often associated with depression and anxiety. Sobota reports that thalassemia patients had significantly lower quality of life in comparison to the US population; older patients and those with more disease complications reported the lowest quality of life [11]. Mednick found that 32% of thalassemia patients indicated experiencing symptoms of anxiety and 11% experiencing symptoms of depression, with more symptoms noted in the older patients [15]. These reports have helped provide an increased awareness into the burden of chronic health conditions and its impact on everyday life. However, this study was designed to observe the comorbidity of pain, and demonstrate its effects on quality of life, as well as lifetime achievements of education, employment and marital status.
As thalassemia patients age, pain reports are becoming more frequent which has prompted this study of pain and its influence on quality of life. Most of the studies that assess quality of life use only one time point and fail to examine emergent health issues such as pain. The Assessment of Pain Survey was designed to: (1) assess the prevalence and severity of pain in thalassemia, (2) identify common pain sites, (3) describe current pain management practices in thalassemia, (4) assess the impact of pain on functioning and well-being and, (5) assess the association of pain with potential risk factors. This analysis takes it one step further by examining longitudinal data, over several time points, and reports upon the current and relevant health issue of pain.
METHODS
The Thalassemia Clinical Research Network (TCRN) is sponsored by the National Institutes of Health/ National Heart, Lung and Blood Institute. The Assessment of Pain Survey and the Thalassemia Longitudinal Cohort (TLC) study were approved by the TCRN Data and Safety Monitoring Board and the institutional review boards at all TCRN centers. Informed consent, and assent in the case of a minor, was obtained.
Eligibility and Enrollment
Eligibility for the Pain study included patients with all thalassemia syndromes greater than 12 years of age who were being seen at one of 12 participating thalassemia treatment centers in North America. Clinically significant thalassemia syndromes were eligible and were categorized by β-thalassemia major, β-thalassemia intermedia, hemoglobin H disease, E-β thalassemia and homozygous α-thalassemia. Exclusions included thalassemia trait, non-thalassemia mutations and individuals who have undergone a bone marrow transplant. Eligible patients were stratified into three levels, chronically transfused patients (≥ 8 transfusions /year), intermittently transfused patients (< 8 transfusions/year) and those receiving no transfusions in the last year. 252 participants enrolled in the Assessment of Pain Survey. Study enrollment was achieved using a convenience sample of patients recruited by transfusion status during a scheduled clinic visit. As thalassemia patients are routinely seen in clinic on a frequent basis and these were not visits that were scheduled due to complaints of pain, there is no expected bias.
Assessment of Pain
The Assessment of Pain Survey used the Brief Pain Inventory (BPI) [16,17] to assess pain at four points in time; baseline and then quarterly over a nine month period. The BPI was used for all participants and coordinators reported no difficulties in comprehension for the pediatric patients. The primary pain dimensions assessed by the BPI include: severity, location, duration, and interference with daily life. Participants rate their worst, least and average pain over the last seven days, as well as their current pain. Participants also rate the level that pain interferes with activities of daily living in seven areas: general activity, mood, walking ability, work, relationships with people, sleep and enjoyment of life. Each scale can be classfied into two groups: physical (activity) and emotional (affective) function. The physical (activity) function is represented by walking, general activity and working; relations with others, enjoyment of life and mood compose the emotional (affective) function. Sleep is included in both groups due to its multiple effects. Pain is rated on a 0 to 10 scale, with 0=no pain/interference and 10=pain as bad as you can imagine/complete interference. Severe pain for this study was defined as ≥ 7 out of 10. Participants were grouped into two categories, no pain interference and any pain interference (1–10).
Assessment of Quality of Life
139 of the 252 participants (55%) enrolled in the Pain Survey concomitantly participated in the TLC. The Medical Outcomes Study 36-Item Short Form Health Survey version 2 (SF-36v2) [18] and the Hospital Anxiety and Depression Scale (HADS) [19] were questionnaires used annually in the TLC study to measure health-related quality of life, anxiety and depression. The SF-36 and HADS data closest in time to the pain assessment were analyzed for subjects participating in both studies. The SF-36 is a generic measure of health related functional status and well-being, which generates 8 subscale scores; physical functioning, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems and mental health. These domains are combined into two summary scores; a physical component summary (PCS) and mental component summary (MCS). Possible scores for each domain range from 0 (worst) to 100 (best), and can be normalized to a mean of 50 and standard deviation of 10. A difference of at least 2 points on the normalized SF-36 scores was considered clinically significant [11].
Assessment of Anxiety and Depression
The HADS is a 14-item self-report measure in which participants are asked to respond to items using a four-point Likert scale ranging from 0 to 3, with higher scores reflecting higher occurrence of symptoms of depression and anxiety. Scores range from 0–21 with the following interpretation; Normal: 0–7, Mild: 8–10, Moderate: 11–14, Severe: 15–21. On a population level, a change in average score even within the same interpretation category would indicate higher occurrence of symptoms of depression and anxiety in the population, with potentially fewer individuals scoring in the normal range.
Statistical Analysis
Descriptive statistics of patient characteristics, survey questions, and quality of life measures are presented. Tables I and II (number of study visits with pain) and Figures 1 and 2 report longitudinal data (i.e., data from all four study visits). The remaining tables and figures use baseline (first visit) data only. Logistic regression was used to model the effect of age on pain incidence. Age-adjusted models are reported from linear regression analyses of predictors of pain (gender, thalassemia diagnosis, transfusion frequency, number of study visits with pain), as well as pain as a predictor of interference, quality of life, and anxiety/depression measures between groups. Comparisons of education, employment, and marital status between participants with/without pain, as well as to the general US population, were made using chi-square tests. In all analyses, significance was accepted for alpha ≤0.05.
Table I.
Demographics and Pain Status for the Thalassemia Clinical Research Network (TCRN) Assessment of Pain Study (N=252)
| Age (at first visit) | |
| Mean ± SD | 28.8 ± 11.8 |
| Median, range | 27, 12 – 71 |
| Gender | |
| Male | 115 (46%) |
| Female | 137 (54%) |
| Race/Ethnicity | |
| White | 105 (42%) |
| Asian | 132 (52%) |
| Black | 6 (2%) |
| Hispanic | 2 (1%) |
| Native Hawaiian/Pacific Islander | 2 (1%) |
| Unknown | 5 (2%) |
| Educationa | |
| < High school diploma | 5 (3%) |
| High school diploma | 42 (29%) |
| BA/BS | 76 (52%) |
| Graduate/professional degree | 23 (16%) |
| Employment statusa | |
| Employed full-time | 77 (53%) |
| Employed part-time | 15 (10%) |
| Unemployed | 16 (11%) |
| Not in labor forceb | 38 (26%) |
| Marital status | |
| Single, divorced, or separated | 119 (64%) |
| Married | 67 (36%) |
| Diagnosis | |
| β-Thalassemia | 204 (81%) |
| E-β-Thalassemia | 28 (11%) |
| Other | 20 (8%) |
| Transfusion status | |
| Regularly transfused | 201 (80%) |
| Intermittently transfused | 14 (6%) |
| Not transfused in past year | 37 (15%) |
| Pain in the past 7 days | |
| Baseline visit (n=252) | 93 (37%) |
| Follow-up visit #1 (n=244) | 80 (33%) |
| Follow-up visit #2 (n=234) | 87 (37%) |
| Follow-up visit #3 (n=237) | 88 (37%) |
| At any visit (n=252) | 142 (56%) |
| # study visits with painc | |
| Zero | 100 (43%) |
| One | 38 (17%) |
| Two | 26 (11%) |
| Three | 29 (13%) |
| Four | 37 (16%) |
| # study visits with severe worst pain (≥ 7/10)c | |
| Zero | 156 (68%) |
| One | 33 (14%) |
| Two | 19 (8%) |
| Three | 12 (5%) |
| Four | 10 (4%) |
| Pain at any visit in thed | |
| Lower back | 121 (85%) |
| Either leg | 77 (54%) |
| Midback | 76 (54%) |
| Head | 74 (52%) |
| Upper back | 60 (42%) |
| Either hip | 58 (41%) |
| Abdomen | 55 (39%) |
| Chest | 46 (32%) |
| Either arm | 44 (31%) |
among those ages 25+ for education and employment and 20+ for marital status
e.g. student, homemaker, retired
among subjects with all visits (N=230)
among subjects with pain at any visit (N=142)
Table II.
Effects of pain on interference with lifea, quality of lifeb, anxietyc and depressionc. Results are presented as a mean ± SD.
| Affectivea | Activitya | QOL – physicalb | QOL – mentalb | Anxietyc | Depressionc | |
|---|---|---|---|---|---|---|
| General U.S. population | NA | NA | 50 ± 10 | 50 ± 10 | NAd | NAd |
| Total thalassemia study population | 3.6 ± 2.6 | 3.7 ±2.5 | 46.9 ± 9.4 | 49.4 ± 9.8 | 5.6 ± 4.0 | 3.2 ± 2.8 |
| Pain in the past 7 days | ||||||
| Yes | 3.6 ± 2.6 | 3.7 ± 2.5 | 41.8 ± 8.9 | 47.8 ± 9.7 | 6.9 ± 3.7 | 3.8 ± 3.3 |
| No | - | - | 50.9 ± 7.7 | 50.7 ± 9.6 | 4.6 ± 3.9 | 2.7 ± 2.4 |
| p-value | - | - | <0.001 | 0.19 | 0.007 | 0.17 |
| Average pain in the past 7 dayse | ||||||
| Mild severity (1–3) (N=33) | 2.5 ± 2.1 | 2.4 ± 1.8 | 43.0 ± 9.5 | 48.2 ± 10.6 | 7.2 ± 3.9 | 3.8 ± 2.9 |
| Moderate severity (4–6) (N= 46) | 3.9 ± 2.3 | 4.2 ± 2.3 | 42.5 ± 7.9 | 48.3 ± 10.3 | 6.6 ± 3.8 | 3.4 ± 3.2 |
| Severe (7–10) (N=10) | 7.0 ± 1.5 | 7.0 ± 2.0 | 35.0 ± 9.8 | 44.7 ± 6.3 | 7.0 ± 3.7 | 5.5 ± 4.5 |
| p-value | <.001 | <.001 | 0.17 | 0.68 | 0.87 | 0.35 |
| # sites with painf | ||||||
| 0 (N=162) | - | - | 50.7 ± 7.7 | 50.8 ± 9.5 | 4.6 ± 3.8 | 2.7 ± 2.4 |
| 1 (N=10) | 2.2 ± 2.3 | 2.2 ± 2.1 | 41.3 ± 6.4 | 51.9 ± 9.4 | 7.4 ± 3.7 | 3.1 ± 2.2 |
| ≥2 (N=79) | 3.9 ± 2.5 | 4.0 ± 2.4 | 41.6 ± 9.6 | 46.7 ± 9.8 | 6.9 ± 3.8 | 4.1 ± 3.5 |
| p-value | 0.001 | <.001 | <.001 | 0.012 | 0.003 | <.001 |
| Duration of paine | ||||||
| < 1 year (N=17) | 2.5 ± 2.5 | 3.0 ± 2.4 | 43.5 ± 9.7 | 52.2 ± 9.5 | 8.4 ± 5.2 | 3.6 ± 4.9 |
| 1–5 years (N=38) | 4.0 ± 2.5 | 4.1 ± 2.3 | 42.7 ± 9.5 | 45.7 ± 9.4 | 7.0 ± 3.6 | 3.5 ± 2.8 |
| ≥ 5 years (N=29) | 4.2 ± 2.6 | 4.2 ± 2.8 | 38.1 ± 8.2 | 50.3 ± 7.6 | 6.0 ± 2.9 | 3.9 ± 2.4 |
| p-value | 0.09 | 0.23 | 0.27 | 0.96 | 0.95 | 0.73 |
| # study visits with paing | ||||||
| Zero | - | - | 52.3 ± 7.0 | 51.3 ± 9.0 | 4.4 ± 3.5 | 2.4 ± 2.3 |
| One | 1.8 ± 2.2 | 1.9 ± 1.9 | 48.4 ± 6.6 | 52.0 ± 9.5 | 4.0 ± 2.9 | 2.3 ± 1.7 |
| Two | 3.0 ± 1.9 | 3.2 ± 1.9 | 47.6 ± 9.0 | 46.1 ± 8.4 | 6.7 ± 4.2 | 2.8 ± 1.9 |
| Three | 3.0 ± 1.8 | 3.1 ± 1.8 | 45.1 ± 9.3 | 45.4 ± 10.7 | 7.4 ± 4.7 | 4.5 ± 3.4 |
| Four | 4.5 ± 2.2 | 4.9 ± 2.2 | 37.0 ± 8.8 | 48.8 ± 8.5 | 7.0 ± 3.2 | 4.5 ± 3.9 |
| p-value | <.001 | <.001 | <.001 | 0.11 | 0.002 | 0.003 |
among those reporting pain (N=93 at baseline). Seven interference scales were measured, divided into two categories: affective (emotion) and activity (physical). The affective scale includes interpersonal relations, enjoyment of life, mood. The activity scale includes walking, general activity, working. Sleep is included in both scales. Higher scores indicate more interference.
Physical component summary (PCS) and mental component summary (MCS) scales of the SF-36 health survey. Higher scores indicate higher QOL. N=139 participants in both the Pain Study and the Thalassemia Longitudinal Cohort.
Anxiety and depression scales from the Hospital Anxiety and Depression Scale (HADS). Higher scores indicate higher levels of anxiety and depression. N=139 participants in both the Pain Study and the Thalassemia Longitudinal Cohort.
There are no population means available, but HADS scores range from 0–21 with the following interpretation: normal=0–7, mild=8–10, moderate=11–14, severe=15–21.
among those reporting pain
any back pain (upper, middle, lower) was counted as a single site.
among participants with all visits
Figure 1.
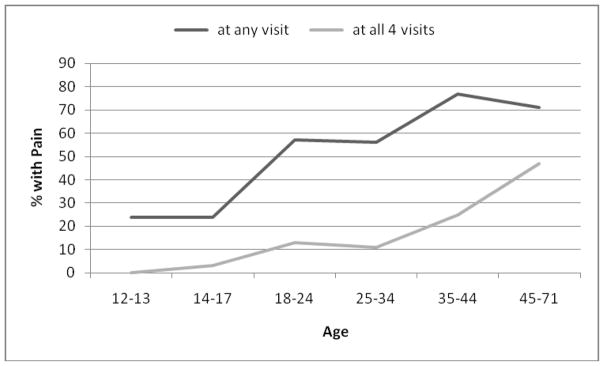
Percent of participants with pain in the past 7 days at any study visit and at all four study visits, by age. Both increase with age (p<0.001).
Figure 2.
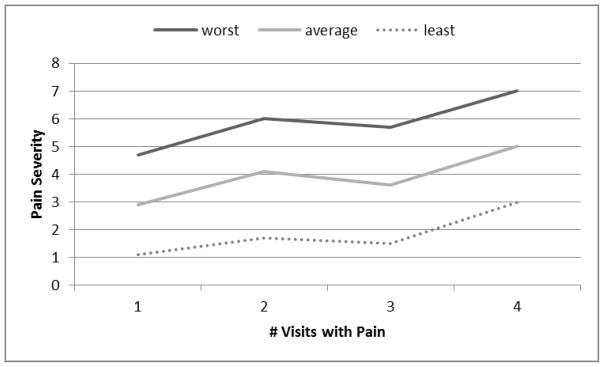
Worst, average, and least pain severity (0–10 scale) in the past 7 days, by number of study visits experiencing pain. All increase with the number of visits (p<0.001).
RESULTS
Demographics
There were 252 participants enrolled in the Assessment of Pain Survey, with 230 subjects (91%) who completed all four study visits. Participants were mainly had β-thalassemia major and ranged in age from 12–71 years, mean of 28.8 ± 11.8 (Table 1). The percent of participants reporting pain increased with age (p <0.001; Figure 1). Compared to participants under 18 years of age, pain reports doubled in the 18–34 cohort and tripled in participants 35 years and older. Therefore, all further analysis of pain controlled for the effect of age. Pain incidence, severity, and interference did not differ significantly by gender, thalassemia diagnosis, or transfusion frequency.
97% of participant had at least a high school diploma, and 67% had earned a college degree. 63% are employed. Physical quality of life scores were an average of 3 points lower than the general U.S. population (Table II), which is a clinically significant difference. Mental quality of life scores did not differ from the general population. Average anxiety and depression scores were within the normal range.
Pain
The longitudinal study showed that patients had pain repeatedly throughout the study (33–37% at each visit; Table 1). Over half of all participants, 142 (56%), reported pain at least once during the entire study, and 37 (16%) reported pain at all four study visits (Table I). Of the patients reporting pain, 79% reported a duration of at least one year, and 34% at least 5 years. Participants reported an average of 4.01 ± 2.0 sites of pain; among participants with pain at any study visit, 85% reported lower back as the most common site of pain (Table I). Severity of average pain was 4.1 ± 2.1; severity of worst pain was 5.8 ± 2.3. Pain severity increased in patients who reported pain at more visits (p <0.001; Figure 2).
Impact of Pain on Functioning
Pain Interference
Pain interference and its effects on affective (emotion) and activity (physical) scales were studied (Table II). Average pain interference was similar for the affective and activity scales: 3.6 vs. 3.7. As average pain severity increased, average interference scores for both affective and activity scales increased (p <0.001). Participants reporting mild pain (1–3) rated their interference as ~2.5, compared to an interference rating of 7.0 for those with severe pain (7–10). Similarly, as the number of sites of pain increased, interference scores increased for both scales. Participants reporting 2 or more sites of pain showed greater interference (~4.0) compared to those with only 1 site of pain (2.2; p≤0.001). Acute (< 1 year) vs. chronic pain (>1 year) did not interfere with affective or activity scales, although there was a trend towards higher pain interference for those with a longer duration of pain. Furthermore, participants reporting more study visits with pain reported a significantly higher impact on both scales (p <0.001).
Quality of Life (SF-36)
Quality of Life scores are presented as means and are compared to the general U.S. population (Table II). Lower scores indicate poorer quality of life. At baseline, physical quality of life scores for participants reporting pain in the last 7 days were ~9 points lower than those reporting no pain and the U.S. population, indicating a significantly poorer physical quality of life (p <0.001). A similar 9-point decrease was found for participants with pain at one vs. more than one site, with a 4-point decrease in mental quality of life among those with more than one site of pain (p=0.012). Physical quality of life decreased with increasing numbers of study visits with pain (p <0.001). Participants with pain at all four study visits reported a 15-point decrease in the physical quality of life score. Physical and mental quality of life scores were not significant for pain severity and duration of pain.
Anxiety and Depression
Higher HADS scores indicate higher symptoms of anxiety and depression, with scores ≤7 being considered normal and those ≥15 severe. Participants with pain showed more symptoms of anxiety (p = 0.007), with a trend towards more symptoms of depression (p= 0.17) (Table II). Those who reported one or more sites of pain showed increased symptoms of both depression (p <0.001) and anxiety (p= 0.003). Comparatively, participants reporting at least two study visits with pain had higher symptoms of anxiety (p= 0.002 for the overall group comparison), and those with at least three visits with pain, higher symptoms of depression (p= 0.003). Anxiety and depression scores did not vary significantly with pain severity or duration of pain.
Education, Employment and Marital Status
The effects of pain on education, employment and marital status were compared among participants with pain vs. no pain. There was no significant difference for attaining an education (p= 0.24) or employment status (p= 0.62) among participants with pain compared to those without pain. Those with pain were non-significantly more likely to be married (43% vs. 30%, p= 0.07).
DISCUSSION
As survival has dramatically changed in thalassemia, quality of life has become an important aspect of overall health. Pain is seen as a growing problem and there is a need to study its role in this population. The purpose of this report is to describe pain and examine its effects on daily life. A key characteristic of this study was to observe pain longitudinally, which showed a subset of the population with consistent pain over time in conjunction with increased severity. Increased severity and patients who reported pain at more study visits greatly impacted physical quality of life, anxiety and depression.
Data from the Brief Pain Inventory (BPI) has revealed that pain affects patients’ lives by interfering with multiple domains of daily life (average of 5/7 scales measured). The results have shown that as participants report more study visits with pain, more sites of pain, and/or as pain severity increases, pain decreases physical functioning (walking, working, general activities), social functioning (interpersonal relationships) and overall subjective well-being (enjoyment of life, mood). There is no significant relationship between transfusion frequency or diagnosis with interference with daily life. The effects of transfusion frequency and diagnosis on pain is poorly studied. However, to further assess the relationship between transfusion and pain, data from a substudy conducted as part of this study, is currently under analysis. In patients who reported taking pain medications, and hence were likely experiencing greater pain, pain interfered more with physical function than overall well-being.
The study also identified an association between pain, lower overall quality of life anxiety and depression. The findings reveal that patients who report pain at more study visits and multiple pain sites suffered from the poorest physical quality of life, and were more anxious and depressed. Overall, mental quality of life scores did not significantly vary with pain, which may be attributed to underreporting of mental health in minorities [20]. However, multiple pain sites had a significant effect on mental quality of life. Pain severity and duration of pain did not significantly affect physical and mental quality of life scores.
Major life events such as pursuing a higher education, maintaining a career and getting married are often assessed when studying quality of life. Pain had no observed effect on these experiences. The lack of significance with education and employment is probably a function of age. People obtain degrees and start jobs when they are younger. There is also less pain in younger patients. Interestingly, thalassemia patients were more educated, maintained full-time employment and were less likely to be married compared to the general U.S. population. The average age of the thalassemia population studied was 28 years old. These results are consistent with the Pakbaz study which showed that thalassemia patients were more likely to achieve a higher education compared to the general US population [6]. Based on what is known, pain appears to be a complication of thalassemia which warrants further investigation into its effects on these socioeconomic factors.
The success of the study may be attributed to the large sample size, age range and the detail of the data collected. However, there were several limitations to this study. While pain has been studied and reported in the general population, the study lacked a comparable control group. Although thalassemia patients have specific risk factors that are likely to be the cause of their pain, this study was not designed to determine the etiology of pain. The Brief Pain Inventory (BPI) proved to be an acceptable method of measuring pain in thalassemia, however, a limitation of the BPI was that it assessed pain medication use by patient report, which is subjective. Other study limitations include analysis of baseline BPI data from the pain study with a single time point in TLC quality of life data; not all pain study participants were enrolled in the TLC study; and longer follow up time would have made it more interesting to follow the progress of pain with age. Although this was a longitudinal study, establishing a causal sequence was a challenge. Analyzing mental health in diverse, ethnic populations has limitations in terms of comparability and could affect our mental health outcomes. When comparing education, employment and marital status, the age distributions were not ideally matched which is a weakness of the study. With an average age of 37 years old, the general US population was 9 years older than the thalassemia population studied, which may be a possible reason why thalassemia patients were less likely to be married.
This pilot study has provided valuable insight into the impact of pain on daily life and its influence on overall health in thalassemia. Pain in thalassemia is a common, often chronic condition that increases with age and interferes with life. As patients age, it is likely that chronic pain and quality of life will be important in making therapeutic decisions. Quality of life is increasingly being used as an outcome measure for interventions and better data is needed for thalassemia. The study highlights the significance of pain in thalassemia and its impact should be considered in future research and treatments.
Acknowledgments
This work was supported by the following NIH-NHLBI cooperative agreements: U01-HL65232 and NIH/NCRR UL1-RR-024134 to the Children’s Hospital of Philadelphia, U01-HL72291 and by Harvard Catalyst CTSC U-01RR025758 to Children’s Hospital, Boston, U01-HL65233 to University Health Network Toronto General Hospital, U01-HL65239 to Children’s Hospital & Research Center Oakland, U01-HL65244 and CTSC UL1-RR024996 to Weill Medical College of Cornell University, and U01-HL65238 to New England Research Institutes. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI.
The authors also wish to acknowledge the contributions of all the individuals with thalassemia who participated in this study.
Appendix 1
The following institutions and researchers contributed to the Thalassemia Clinical Research Network Assessment of Pain Study data reported in this paper:
Children’s Hospital, Boston: Ellis Neufeld, MD, PhD, Jennifer Eile, PNP, Research Nurse, Latoya Lashley, Study Coordinator; Satellites: Children’s Healthcare of Atlanta, Leann Schilling, MPH, Study Coordinator, Principal Investigator; Baylor College of Medicine, Bogden Dino, Study Coordinator. Weill Medical College of Cornell University: Dorothy Kleinert, RN, Research Nurse, Patricia Giardina, MD; The Children’s Hospital of Philadelphia: Alan Cohen, MD, Janet Kwiatkowski, MD, Marie Martin, RN, Research Nurse, Principal Investigator, Sage Green, Study Coordinator; Satellite: Children’s Memorial Hospital, Chicago, IL: Alexis Thompson, MD, Janice Beatty, RN, Research Nurse, Diane Calamaras, RN, CPNP, Research Nurse, Pauline Hess, Study Coordinator. Children’s Hospital at Oakland: Dru Haines, CPNP, Research Nurse, Principal Investigator, Olivia Oliveros, Study Coordinator, Elliott Vichinsky, MD; Satellites: Children’s Hospital of Los Angeles, Thomas Coates, MD, Principal Investigator, Susan Carson, RN, Research Nurse, Principal Investigator, Ani Dongelyan, Study Coordinator, Tatiana Hernandez, Study Coordinator; Children’s and Women’s Health Center of British Columbia, Jennifer Kies, Study Coordinator. Toronto General Hospital, Toronto, Ontario, Canada: Nancy Oliveri, MD, Cecilia Kim, BS, Study Coordinator; Satellite: Hospital for Sick Children: Manuela Merelles-Pulcini, RN, Study Coordinator. NHLBI oversight, Kathryn Hassell, MD. Data Coordinating Center: New England Research Institutes, Sonja McKinlay, PhD, Principal Investigator, Lisa Virzi, RN, MS, MBA, Project Director, Felicia Trachtenberg, PhD, Senior Statistician, Eric Gerstenberger, MS, Statistician.
References
- 1.Borgna-Pignatti C, Cappellini MD, De Stefano P, et al. Survival and complications in thalassemia. Ann N Y Acad Sci. 2005;1054:40–7. doi: 10.1196/annals.1345.006. [DOI] [PubMed] [Google Scholar]
- 2.Cohen AR, Galanello R, Pennell DJ, Cunningham MJ, Vichinsky E. Thalassemia. Hematol Educ Program Am Soc Hematol Am Soc Hematol Educ Program. 2004:14–34. doi: 10.1182/asheducation-2004.1.14. [DOI] [PubMed] [Google Scholar]
- 3.Kolnagou A, Kontoghiorghes GJ. Advances in the prevention and treatment are changing thalassemia from a fatal to a chronic disease. experience from a Cyprus model and its use as a paradigm for future applications. Hemoglobin. 2009;33(5):287–95. doi: 10.3109/03630260903212043. [DOI] [PubMed] [Google Scholar]
- 4.Olivieri NF, Brittenham GM. Iron-chelating therapy and the treatment of thalassemia. Blood. 1997;89(3):739–61. [PubMed] [Google Scholar]
- 5.Haines D, Martin M, Carson S, et al. Pain in thalassaemia: the effects of age on pain frequency and severity. Br J Haematol. 2013;160(5):680–7. doi: 10.1111/bjh.12177. [DOI] [PubMed] [Google Scholar]
- 6.Pakbaz Z, Treadwell M, Kim H-Y, et al. Education and employment status of children and adults with thalassemia in North America. Pediatr Blood Cancer. 2010;55(4):678–83. doi: 10.1002/pbc.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trachtenberg F, Foote D, Martin M, et al. Pain as an emergent issue in thalassemia. Am J Hematol. 2010;85(5):367–70. doi: 10.1002/ajh.21670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vogiatzi MG, Macklin EA, Fung EB, et al. Bone disease in thalassemia: a frequent and still unresolved problem. J Bone Miner Res Off J Am Soc Bone Miner Res. 2009;24(3):543–57. doi: 10.1359/jbmr.080505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haidar R, Musallam KM, Taher AT. Bone disease and skeletal complications in patients with β thalassemia major. Bone. 2011;48(3):425–32. doi: 10.1016/j.bone.2010.10.173. [DOI] [PubMed] [Google Scholar]
- 10.Vichinsky EP. The morbidity of bone disease in thalassemia. Ann N Y Acad Sci. 1998;850:344–8. doi: 10.1111/j.1749-6632.1998.tb10491.x. [DOI] [PubMed] [Google Scholar]
- 11.Sobota A, Yamashita R, Xu Y, et al. Quality of life in thalassemia: a comparison of SF-36 results from the thalassemia longitudinal cohort to reported literature and the US norms. Am J Hematol. 2011;86(1):92–5. doi: 10.1002/ajh.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panepinto JA. Health-related quality of life in patients with hemoglobinopathies. Hematol Educ Program Am Soc Hematol Am Soc Hematol Educ Program. 2012;2012:284–9. doi: 10.1182/asheducation-2012.1.284. [DOI] [PubMed] [Google Scholar]
- 13.McClish DK, Penberthy LT, Bovbjerg VE, et al. Health related quality of life in sickle cell patients: the PiSCES project. Health Qual Life Outcomes. 2005;3:50. doi: 10.1186/1477-7525-3-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pakbaz Z, Treadwell M, Yamashita R, et al. Quality of life in patients with thalassemia intermedia compared to thalassemia major. Ann N Y Acad Sci. 2005;1054:457–61. doi: 10.1196/annals.1345.059. [DOI] [PubMed] [Google Scholar]
- 15.Mednick L, Yu S, Trachtenberg F, et al. Symptoms of depression and anxiety in patients with thalassemia: prevalence and correlates in the thalassemia longitudinal cohort. Am J Hematol. 2010;85(10):802–5. doi: 10.1002/ajh.21826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cleeland CS. The Brief Pain Inventory User Guide [Internet] The University of Texas M. D. Anderson Cancer Center; 2009. Available from: http://dl.owneriq.net/b/bda4b416-56f9-4179-a75a-e102e933c0b1.pdf. [Google Scholar]
- 17.Patt RB. Cancer pain. Philadelphia: Lippincott; 1993. [Google Scholar]
- 18.Ware JE, Kosinski M, Bjorner B. User’s Manual for the SF-36v2 Health Survey. QualityMetric Incorporated; 2007. Available from: http://www.qualitymetric.com/WhatWeDo/GenericHealthSurveys/SF36v2HealthSurvey/tabid/185/Default.aspx. [Google Scholar]
- 19.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 20.Mossey JM. Defining racial and ethnic disparities in pain management. Clin Orthop. 2011;469(7):1859–70. doi: 10.1007/s11999-011-1770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scalone L, Mantovani LG, Krol M, et al. Costs, quality of life, treatment satisfaction and compliance in patients with beta-thalassemia major undergoing iron chelation therapy: the ITHACA study. Curr Med Res Opin. 2008:1905–17. doi: 10.1185/03007990802160834. [DOI] [PubMed] [Google Scholar]


