Abstract
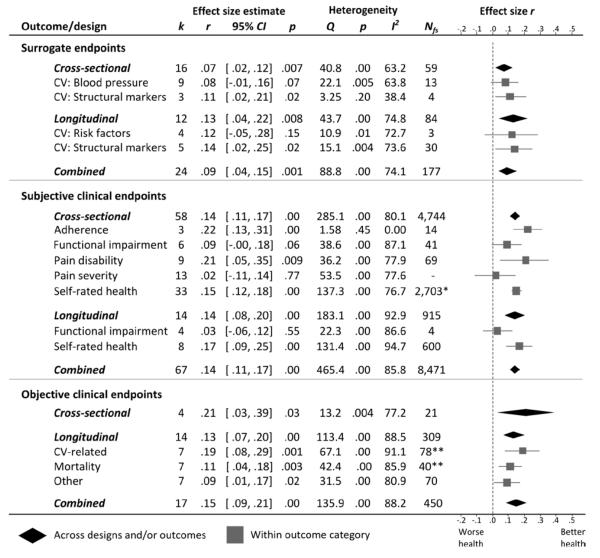
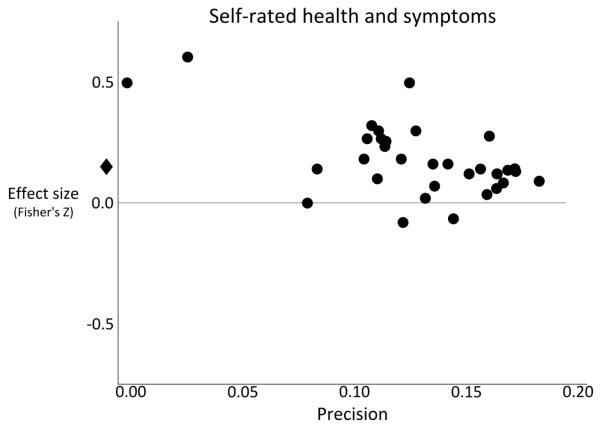
This meta-analysis reviewed 126 published empirical articles over the past 50 years describing associations between marital relationship quality and physical health in over 72,000 individuals. Health outcomes included clinical endpoints (objective assessments of function, disease severity, and mortality; subjective health assessments) and surrogate endpoints (biological markers that substitute for clinical endpoints, such as blood pressure). Biological mediators included cardiovascular reactivity and hypothalamic-pituitary-adrenal axis activity. Greater marital quality was related to better health, with mean effect sizes from r = .07 to .21, including lower risk of mortality, r = .11, and lower cardiovascular reactivity during marital conflict, r = −.13, but not daily cortisol slopes or cortisol reactivity during conflict. The small effect sizes were similar in magnitude to previously found associations between health behaviors (e.g., diet) and health outcomes. Effect sizes for a small subset of clinical outcomes were susceptible to publication bias. In some studies, effect sizes remained significant after accounting for confounds such as age and socioeconomic status. Studies with a higher proportion of women in the sample demonstrated larger effect sizes, but we found little evidence for gender differences in studies that explicitly tested gender moderation, with the exception of surrogate endpoint studies. Our conclusions are limited by small numbers of studies for specific health outcomes, unexplained heterogeneity, and designs that limit causal inferences. These findings highlight the need to explicitly test affective, health behavior, and biological mechanisms in future research, and focus on moderating factors that may alter the relationship between marital quality and health.
Keywords: marriage, marital quality, health, morbidity, mortality, meta-analysis
The link between “better” or “worse” marriages and “sickness and health” has been a subject of much empirical interest over the last half-century. During this period, marriage went through considerable sociodemographic transformations, including a declining marriage rate, increasing age of first marriage, increasing divorce rates during the 1960s and 1970s, and increasing cohabitation and same-sex marriage (Cherlin, 2010; Lee & Payne, 2010). The cultural meaning of marriage also went through “deinstitutionalization,” where marriage based on companionship through mutual social obligations and roles transitioned to a greater emphasis on personal choice and self-fulfillment (Cherlin, 2004).
In spite of the changes in the demographics and meanings of marriage, the impact of having a better or worse marriage – marital quality – on physical well-being has remained a topic of consistent interest among scholars, practitioners, and the public. Marital quality is defined as a global evaluation of the marriage along several dimensions (Fincham & Bradbury, 1987), including positive and negative aspects of marriage (e.g., support and strain; Burman & Margolin, 1992; Fincham, Beach, & Kemp-Fincham, 1997; Slatcher, 2010), attitudes, and reports of behaviors and interaction patterns (Bradbury, Fincham, & Beach, 2000). Thus, high marital quality is typically operationally defined by high self-reported satisfaction with the relationship, predominantly positive attitudes towards one’s partner, and low levels of hostile and negative behavior. Low marital quality is characterized by low satisfaction, predominantly negative attitudes towards one’s partner, and high levels of hostile and negative behavior. A narrative synthesis of research up to the early 1990s concluded that “marital variables affect health problems” (Burman & Margolin, 1992, p. 56). An updated review echoed the same conclusion and described research during the 1990s on biological mechanisms that could explain the “ample evidence that intimate relationships can impact illness processes or outcomes…” (Kiecolt-Glaser & Newton, 2001, p. 487).
Since the publication of those reviews, technological advances in measuring objective biological markers led to empirical advances in understanding marital functioning and health outcomes during the 2000s, including studies of ambulatory blood pressure, cardiovascular disease progression, and wound healing. Such methods were simply unavailable in previous decades. Beyond providing an updated picture of the past decade of research of marital quality and health research given these technological improvements, our overall goal is to conduct the first meta-analysis of the association between marital quality and health outcomes spanning the entire published literature of the past 50 years. In doing so, we aim to quantify the magnitude of the association between marital quality and health, which allows for comparing marital functioning to other established health-related risk factors, particularly health behaviors, and address substantive theoretical concerns and methodological issues in the existing literature. We begin by describing the state of theory on marital quality and health.
Explanatory theories
The connection between marital quality and health is part of a larger body of research that has consistently demonstrated robust links between social relationships and physical health (for reviews, see Berkman, Glass, Brissette, & Seeman, 2000; House, Landis, & Umberson, 1988; Uchino, 2009). A recent meta-analysis across 148 studies indicated a 50% greater likelihood of survival for participants with stronger social relationships (Holt-Lunstad, Smith, & Layton, 2010). Indeed, social support has been called “one of the most well-documented psychological factors influencing physical health outcomes” (Uchino, 2009, p. 236).
Two main types of models have been proposed to explain how social support influences physical health. In main-effect models, high levels of social integration are health promoting, regardless of whether or not one is under stress (Berkman, Glass, Brissette, & Seeman, 2000; S. Cohen, 2004; S. Cohen & Wills, 1985). Greater integration into one’s social network gives an individual identity, purpose, and control, a perceived sense of security and embeddedness, and a source of reinforcement for health-promoting behaviors or punishment for health-compromising behaviors, all of which can promote health (Thoits, 2011). In the stress-buffering model (Cohen & Wills, 1985), the negative effects of stress occurring outside of one’s social relationships (e.g., at work) are diminished by the presence of strong social support, which can mitigate stressful events directly (e.g., intervening on a friend’s behalf) or through reducing stress appraisals (Uchino, 2004). In both models, close personal relationships such as marriage should be a key roles source of social support.
Surprisingly, although many studies have investigated the links between measures of social support and health, and other studies have examined marital processes and health, virtually no studies have compared whether marriage confers special benefits above and beyond other long-term, committed, non-cohabitating social relationships in one’s social network. That said, marital relationship quality may have greater bearing on health relative to support and strain from other social network members for several reasons. Relative to non-cohabiting social network members (friends, co-workers) individuals in long-term romantic relationships such as marriage share the same space and time on a daily basis, co-participating in a wide variety of activities that include meals, leisure activities, domestic chores, child care, and sleep. Married spouses also share financial and other tangible resources (Carr & Springer, 2010) to a degree that is often larger relative to other cohabiting family members or friends. Likewise, married individuals are on average more committed and make more joint investments (specialization of labor, shared finances, children, home ownership) relative to cohabiting romantic partners or dating partners (Brines & Joyner, 1999). Thus, sharing of space, time, resources, and investments creates unique arenas for both support and conflict.
Changes in marriage: Implications for theory
The increased prevalence of nonmarital cohabitation in industrialized countries (Heuveline & Timberlake, 2004) may complicate existing theories explaining the benefits of marriage for health. However, research on cohabitation and its implications for health and well-being is in its infancy. The prevailing view is that cohabitation is associated with greater advantages for well-being relative to being nonpartnered, but fewer economic, psychological, and health benefits relative to being married (Carr & Springer, 2010; Liu & Reczek, 2012). At the same time, “cohabiting” is a heterogeneous category in terms of reasons for living together (e.g., as a prelude to eventual marriage or not), and because sociodemographic factors and selection effects that are associated with cohabitation (described later when we discuss marital status) also modify the association between cohabitation and health. Indeed, the effects of cohabitation relative to being married on mortality vary by ethnicity, socioeconomic status (SES), age, gender, and their interactions (Liu & Reczek, 2012). Moreover, data on the link between relationship quality and health outcomes, which is the pertinent question for this review, and whether it differs between married and cohabitating individuals is lacking. That said, we expect that in committed relationships (married or not), the quality of the relationship should be related to physical well-being.
Despite sociodemographic shifts away from marriage in industrialized countries (Fincham & Beach, 2010; Pew Research Center, 2010; United States Census Bureau, 2010), marriage continues to play an integral role in our social networks, even in comparison to other social relationships. In most countries, the proportion of individuals reporting that they were “ever married” is over 90% during the adult years (United Nations Department of Economic and Social Affairs, Population Division, 2009). Thus, marriage has understandably received much attention from researchers interested in close relationships and health.
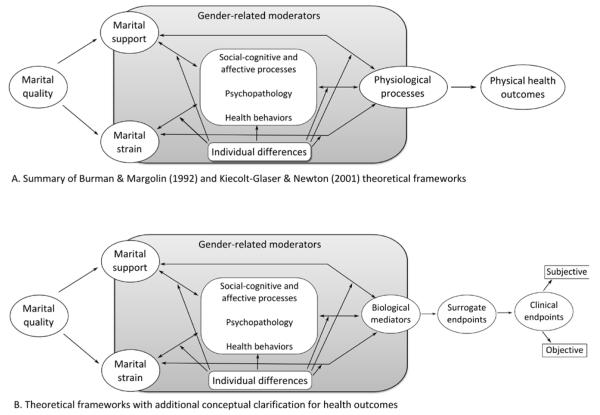
The existing theories explaining the relationship between marital quality and health are summarized in Figure 1A (Burman & Margolin, 1992; Kiecolt-Glaser & Newton, 2001; Slatcher, 2010). Below, we briefly review our conceptual understanding of health, explanatory mediators, and moderators in existing theories.
Figure 1.
Summary of conceptual models explaining links between marital quality and health
Defining “health”
A key issue for theory is how to effectively differentiate physiological pathways from indicators of physical health outcomes (termed “health status” by Burman & Margolin, 1992; and “functional status and pathophysiology” by Kiecolt-Glaser & Newton, 2001). The issue is especially important due to increased use of objective indicators of normal or pathological biological processes, referred to as biomarkers (Biomarker Definitions Working Group, 2001), in biobehavioral research over the past decade. For example, structural markers of cardiovascular function that actually quantify atherosclerosis (hardening of the arteries that causes later cardiovascular disease) came into regular use in biobehavioral research beginning in the late 1990s and early 2000s (Barnett, Spence, Manuck, & Jennings, 1997; Trieber et al., 2003). To what degree do those biomarkers actually reflect what health care providers and policymakers consider indicators of “health”? The answer to this question provides a guiding framework for this review.
The National Institutes of Health established an expert working group to propose terms and definitions to help guide research, clinical applications, and regulatory policy (Biomarker Definitions Working Group, 2001). Besides defining the term “biomarker” (described in the previous paragraph), the working group created a key definition that we consider the starting point for measuring “health”: Clinical endpoints. Defined as a “…characteristic or variable that reflects how a patient feels, functions, or survives” (Biomarker Definitions Working Group, 2001, p. 91), clinical endpoints are considered “the most credible characteristics used in the assessment of the benefits and risks of a therapeutic intervention in randomized clinical trials” (Biomarker Definitions Working Group, 2001, p. 91). For example, clinical endpoints may include occurrence of a heart attack, hospitalization due to a medical condition, or changes in quality-of-life or activities of daily living. Such observable endpoints would typically be recognized as important outcomes by patients and health care providers.
Clinical endpoints were distinguished from surrogate endpoints, defined as “A biomarker that is intended to substitute for a clinical endpoint…[that] is expected to predict clinical benefit (or harm…) based on epidemiologic, therapeutic, pathophysiologic, or other scientific evidence” (Biomarker Definitions Working Group, 2001, p. 91). Examples include low-density cholesterol levels or blood pressure (Psaty et al., 1999), which predict later cardiovascular disease endpoints (e.g., coronary artery disease, stroke), but may not have value for assessing how a patient currently feels, functions, or survives because they reflect early events in the causal chain (Temple, 1999). Surrogate endpoints covered in this review are described in Table 1. The distinction between clinical and surrogate endpoints is both conceptually and practically useful. For example, the United States Food and Drug Administration regulations of therapeutic agents allow for approval based on evidence of efficacy using surrogate endpoints.
Table 1.
Definitions of Surrogate Endpoints used in Cited Studies
| Endpoint category/endpoint | Definition |
|---|---|
| Functional cardiovascular markers | Abnormalities in the performance of the cardiovascular system (Cohn, Quyyumi, Hollenberg, & Jamerson, 2004). |
| Resting blood pressure | Product of the volume of blood expelled by the heart (cardiac output) during contraction (systole) or rest (diastole), and the amount of resistance against blood flow in the arteries that must be overcome to circulate blood (Gerin, Goyal, Mostofsky, & Shimbo, 2008). High blood pressure is strongly related to future cardiovascular risk. Typically measured in the office or laboratory setting using auscultatory (listening for sounds within the artery, in combination with a mercury sphygmomanometer) or oscillometric methods. |
| Ambulatory blood pressure | Automated blood pressure monitoring coupled with a portable device that allows monitoring in naturalistic environments (Janicki-Deverts & Kamarck, 2008). |
| Structural cardiovascular markers | Abnormalities in the framework of cells and tissues (evidence summarized in G. B. J. Mancini, Dahlof, & Diez, 2004). Several markers are strong predictors of future cardiovascular disease- related events (e.g., heart attack, stroke, death) |
| Carotid artery intima media thickness |
The thickness of the innermost layers of the prominent arteries in the neck (carotid), measured using ultrasound. Greater thickness indicates greater degree of atherosclerosis. |
| Coronary artery calcification | Degree of calcium deposition within the lining of the coronary artery (which supplies the heart) as part of a plaque accumulation of cells, debris, cholesterol, and lipids – the core pathology in cardiovascular disease). Imaged using electron-beam computed tomography. |
| Carotid plaque | Discrete enlarged areas within the carotid artery (as opposed to overall thickness of the artery wall) identified using ultrasound. Greater plaque score indicates greater degree of atherosclerosis. |
| Coronary artery luminal diameter | Diameter of the space inside the coronary artery, obtained through angiography. Smaller diameter indicates greater degree of atherosclerosis. |
| Left ventricular mass index | Thickening of heart muscle surrounding the left ventricle of the heart. Commonly observed in hypertension and a sign of early cardiovascular disease. Measured by electrocardiogram or echocardiogram (cardiac ultrasound). A related measure is relative wall thickness. |
| Other endpoints | |
| Body mass index | Proxy for body fat calculated by dividing an individual’s weight (kg) by height (m2) (Melmed, Polonsky, Larsen, & Kronenberg, 2011). |
| Glycosylated hemoglobin A1c (HbA1c) |
Measured in blood. High values indicate a poor ability to control glucose levels over a three-month period (Melmed, Polonsky, Larsen, & Kronenberg, 2011). |
| Antibody titers to influenza virus vaccine |
Protein produced by B-cells that binds to and neutralizes components of the influenza virus vaccine (Prather & Marsland, 2008). “Titer” refers to how antibodies are quantified. Higher titers related to better protection conferred by the vaccine. |
| Metabolic syndrome indices | Cluster of factors that increase risk for cardiovascular disease, stroke, and type 2 diabetes, including three or more of the following: High blood pressure, high fasting blood glucose, elevated waist circumference, low high density lipoprotein cholesterol, high triglyceride levels (http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004546/) |
| Observed signs of orofacial hypokinesia in Parkinson’s patients |
Indicators of motor slowing in the face and mouth, including reduced rates of speech, eye blinks, and longer duration of eye blinks. Slowed speech included in common rating scale assessments of Parkinson’s disease symptoms (Ramaker, Marinus, Stiggelbout, & van Hilten, 2002). |
Biomarkers that are not considered surrogate endpoints can be described as measures of biological mediators (Miller, Chen, & Cole, 2009), which include allostatic biological processes that change in response to short-term environmental demands like marital conflict discussions (McEwen, 1998; Robles & Carroll, 2011; Robles & Kiecolt-Glaser, 2003) and restorative biological processes that respond after short-term environmental demands have ceased (such as tissue growth and energy storage; Robles & Carroll, 2011). Most studies of marital quality and biological mediators have focused on allostatic processes: Acute changes in stress-related hormones and immune measures. While related in theory to clinical endpoints, such biological mediators do not have a sufficient evidence base to be elevated to surrogate endpoint status (Kiecolt-Glaser, Cacioppo, Malarkey, & Glaser, 1992), which requires rigorous evaluation and validation studies (described in Manolio, 2003). Figure 1B represents the incorporation of those key distinctions into the overall model, where biological mediators, surrogate endpoints, and clinical endpoints replace the concepts of physiological processes and health outcomes.
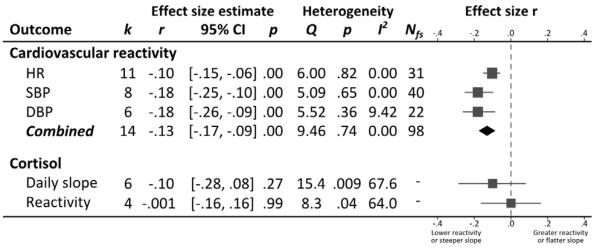
In this review, we examine the relationship between marital quality and the two endpoint categories (clinical and surrogate endpoints). We further subdivide clinical endpoints into subjective clinical endpoints that are reported by participants and patients, including self-rated health (physical health-related quality-of-life), physical symptoms, pain severity, and functional impairment; and objective clinical endpoints that are objectively measured and reflect patient functioning, including mortality. In a separate meta-analysis, we examine the relationship between marital quality and several frequently studied biological mediators1: Cardiovascular reactivity during laboratory-based conflict discussions, daily cortisol slopes in naturalistic studies, and cortisol responses to laboratory-based conflict discussions.
What explains the relationship between marital quality and health?
One of the major challenges to understanding the relationship between marital functioning and health is the direction of causality. Unhappy relationships may contribute to poorer health; on the other hand, chronic medical conditions, or factors that predispose an individual to poorer health, may act as enduring vulnerabilities that contribute to declines in marital satisfaction (Karney & Bradbury, 1995). A key way to address direction of causality is through prospective, longitudinal research designs (Kraemer et al., 1997; Robles & Kiecolt-Glaser, 2003). Moreover, as described by Burman and Margolin (1992) and summarized by Kiecolt-Glaser and Newton (2001): “…the most convincing way to document a causal relationship between marital functioning and health status would be first to confirm that marital interaction had direct effects on physiological processes and then to show that individuals who exhibited physiological changes were more likely to develop health problems…” (p. 491). Prevailing theories proposed several explanatory mediators, shown in Figure 1 and described below. While our descriptions primarily focus on how marital conflict is related to poor health, the same basic mechanisms likely explain how marital support is related to better health.
Social-cognitive and affective processes
How people in happy compared to unhappy marriages think about relationships may play an important mediating role in the links between marital quality and physical health. For example, people in unhappy marriages often attribute responsibility for negative behaviors to their partner (e.g., “Don came home late because he doesn’t care about his family”), while not attributing responsibility for positive behaviors to the partner (e.g., “Don came home early because his boss told him to do so”) (Bradbury, Beach, Fincham, & Nelson, 1996; Durtschi, Fincham, Cui, Lorenz, & Conger, 2011). Similarly, a “criticality bias” to misattribute a partner’s verbal and nonverbal communication as criticism (Smith & Peterson, 2008) is also associated with expressing criticism towards partners, using a negative tone in conversations, and greater “demanding” behaviors (Peterson, Smith, & Windle, 2009). While the specific role of social-cognitive processes in physical health remains understudied, attributing responsibility to the partner for negative behaviors predicted slower cortisol recovery following a conflict discussion in dating couples (Laurent & Powers, 2006).
Emotion regulation in couple interactions is also viewed as a key factor in links between marital quality and health (Burman & Margolin, 1992; Snyder, Simpson, & Hughes, 2006). Distressed couples show greater negative affect, particularly hostility, and escalation of negative affect during conversations with partners (Heyman, 2001). Greater displays of negative affect are related to biological mediators discussed below, including cardiovascular and neuroendocrine reactivity (Robles & Kiecolt-Glaser, 2003). On the other hand, emotional disclosure, which often occurs in the context of marital relationships (Laurenceau, Barrett, & Rovine, 2005), confers an array of physical health benefits, such as decreased work absenteeism and physician visits, which are attributed to changes in psychological well-being and biological mediators, particularly immune function (Frattaroli, 2006; Smyth, 1998). Coupled with findings suggesting that couples with a higher marital distress are less skillful in emotional disclosure (Cordova, Gee, & Warren, 2005; Mirgain & Cordova, 2007), limited emotional expression might mediate links between marital satisfaction and physical health.
Bidirectional associations with psychopathology
Marital distress has both concurrent and longitudinal associations with psychological distress (Proulx, Helms, & Buehler, 2007). In addition, marital problems predict the onset of psychopathology, including mood, anxiety, and substance use disorders (see Whisman & Baucom, 2012, for a review). Of those conditions, depression has received the most empirical attention; three decades of research clearly show a reliable, bidirectional association between depression and marital discord (Beach, Fincham, & Katz, 1998; Fincham & Beach, 1999) with moderate effect sizes (Whisman, 2001). In one direction, marital distress in combination with established diatheses (Hammen, 2005) increases risk for depression. In the other direction, depression is associated with affective dysregulation and cognitive biases (Gotlib & Joormann, 2010), all of which may filter into marital interactions. For example, conversations where one or both partners suffer from depression are characterized by high amounts of negative behaviors and affect alongside a low frequency of positive behaviors and affect (Rehman, Gollan, & Mortimer, 2008). Moreover, depressive behaviors such as excessive reassurance-seeking may be viewed as burdensome to the partner (Benazon & Coyne, 2000), who can react with criticism and rejection (Coyne, 1976).
Regardless of directionality between marital quality and depression, the link between depression and physical health is well-established (Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002). Symptoms like lack of motivation and fatigue may promote maladaptive health behaviors (i.e., sedentary behavior, poor diet and sleep, increased substance use). Depression is also associated with immune dysregulation (described below). Taken together, poor marital quality predicts subsequent depressive symptoms or diagnoses, which themselves are associated with emotion dysregulation and cognitive biases that may enhance marital dissatisfaction and promote further depression and concomitant poor physical health. Thus, our focus on depression as a psychopathology-related mediator of the relationship between marital quality and physical health is based in part on the significant amount of prior empirical work. In addition, depression was examined most frequently in the studies included in our meta-analysis.
Importantly, while there is a clear bidirectional relationship between stressful life events and episodes of major depression (Hammen, 2005) emerging research has indicated that stress generation (the propensity for depression to “create” subsequent interpersonal stressors) can occur in other psychological disorders beyond depression (Daley, Hammen, Davila, & Burge, 1998; Hammen & Shih, 2008). Indeed, other psychological conditions (i.e. anxiety, personality, substance use disorders) may be additional or comorbid explanatory mediators (Whisman & Baucom, 2012). Finally, interpersonal dysfunction in intimate relationships clearly occurs even among individuals without current depressive symptoms (Hammen & Brennan, 2002), and with sufficient duration can be a chronic stressor with the potential for long-term effects on physical health through the pathways described below (Robles & Kiecolt-Glaser, 2003), even in the absence of psychopathology.
Health behaviors
Marriage is a key context for efforts to change health-compromising behaviors (e.g., substance use, nonadherence) and initiate and maintain health-enhancing behaviors (e.g., physical activity, diet, adherence). Being married contributes to concordance in health behaviors over time between spouses (Homish & Leonard, 2008; Meyler, Stimpson, & Peek, 2007). One explanation is modeling, and another is the ways in which spouses exert social influence or control over health behaviors (Lewis & Butterfield, 2007; Lewis & Rook, 1999), which may be a key mechanism explaining how marital quality influences health behaviors more generally. For instance, positive control behaviors such as modeling a behavior were related to greater intentions to change health behaviors (in a health-promoting direction), whereas negative control behaviors, such as inducing fear, had no effect on intentions (Lewis & Butterfield, 2007). Importantly, social control attempts may be more successful against a backdrop of a satisfying compared to a distressed relationship (Tucker, 2002). Moreover, marital support may also buffer against the impact of non-marital stressors on health behaviors and increase personal resources (i.e., self-efficacy, self-regulatory capacity) needed for initiating and maintaining health behavior change (DiMatteo, 2004). Marital strain may add or interact with non-marital stressors leading to increased use of health-compromising behaviors to cope with such stressors, and decreasing personal resources that could be used during change attempts. For example, couples reporting higher marital conflict and/or lower marital satisfaction are at greater risk for future alcohol problems (Whisman, Uebelacker, & Bruce, 2006). In addition, couples seeking treatment for substance dependence have better outcomes when they are in high quality relationships (Heinz, Wu, Witkiewitz, Epstein, & Preston, 2009).
Biological mediators
Among the many plausible biological mediators of the link between marital quality and health, allostatic processes that respond during physical or psychological challenges (Robles & Carroll, 2011) have received the most attention in the marital literature (Robles & Kiecolt-Glaser, 2003). Key allostatic processes involve the cardiovascular, neuroendocrine, and immune systems, and dysregulation in those systems is implicated in the deleterious health effects of chronic stress (McEwen, 1998).
Cardiovascular reactivity
Individuals with greater cardiovascular reactivity to stress are at greater risk for future cardiovascular disease and faster disease progression (Linden, Gerin, & Davidson, 2003; Trieber et al., 2003). Some of the earliest studies demonstrating that interpersonal conflict and attempts to influence another person could evoke cardiovascular responses involved married couples (Smith & Brown, 1991; Ewart et al., 1991). Couples who show greater hostile behavior during marital discussions have elevated blood pressure and heart rate compared to less hostile couples (reviewed in Robles & Kiecolt-Glaser, 2003). Thus, cardiovascular reactivity to marital interactions is a likely mediator of the relationship between marital quality and cardiovascular health.
Neuroendocrine pathways
The primary neuroendocrine pathways of interest include the sympathetic-adrenal-medullary axis (SAM) and the hypothalamic-pituitary-adrenal axis (HPA; Robles & Kiecolt-Glaser, 2003). The hormones produced by both axes have wide-ranging effects across the body, and are considered key mediators of the association between psychological factors and physical health (McEwen, 1998). The SAM axis can be indexed indirectly by measuring cardiovascular reactivity and directly through circulating catecholamines (norepinephrine, epinephrine). Greater negative behavior during marital interactions has been related to elevated catecholamine levels during and after conflict discussions in both newlywed (Malarkey et al., 1994) and older adult couples (Kiecolt-Glaser et al., 1997)2.
In contrast to the SAM axis, the HPA axis has received significant empirical attention in the past decade, and sufficient numbers of studies were available to review. Our meta-analysis focused on the diurnal slope of cortisol and cortisol responses to marital conflict discussions. Diurnal cortisol slopes are of particular interest because of research linking daily cortisol measurements to surrogate markers (Matthews, Schwartz, Cohen, & Seeman, 2006), and clinical endpoints related to cardiovascular disease (Kumari, Shipley, Staffod, & Kivimaki, 2011).
Immune pathways
Due to its role in responding to infection and injury, the immune system received attention in early studies of marital functioning and biological processes (Kiecolt-Glaser, Fisher, Ogrocki et al., 1987; Kiecolt-Glaser, Kennedy, Malkoff et al., 1988). Comprehensive narrative reviews are available elsewhere (Robles & Kane, 2012; Robles & Kiecolt-Glaser, 2003), so we briefly summarize the findings here. Couples who showed greater hostile behavior during marital conflict, and higher levels of hostility in men, showed greater acute increases in the activity of natural killer cells (Kiecolt-Glaser et al., 1993; G. E. Miller, Dopp, Myers, Stevens, & Fahey, 1999), which play key roles in immediate responses to viral infection by killing virally-infected cells in the body. In addition, social rejection (potentially from one’s partner) contributes to inflammation (Slavich, O’Donovan, Epel, & Kemeny, 2010) which is the body’s immediate response to injury and infection. Chronic and persistent inflammation contributes to accumulating damage in tissues that surround sites of chronic infection, and has been implicated as a central mechanism explaining how psychosocial factors can contribute to chronic disease, including atherosclerosis and cancer (Miller, Chen, & Cole, 2009; Robles, Glaser, & Kiecolt-Glaser, 2005). In the context of marriage, higher levels of hostile behaviors during conflict were related to larger increases in circulating markers of inflammation (Kiecolt-Glaser et al., 2005). Moreover, recent work in a large national sample similarly found that low marital satisfaction was related to elevated inflammation (Whisman & Sbarra, 2012). Moving beyond immediate responses to infection, marital functioning is related to slower-acting yet highly specific immune responses (known as adaptive immunity). For example, low marital satisfaction and greater hostility during marital conflict were related to poorer ability to control Epstein-Barr Virus, a latent herpesvirus that infects most adults (Kiecolt-Glaser et al., 1997; Kiecolt-Glaser et al., 1988; Kiecolt-Glaser et al., 1993). In sum, poorer marital functioning, assessed through self-reports and behavioral data, shows associations with immunity that are similar to the effects of chronic stressful life events, consistent with previous conceptualizations of marital strain as a chronic stressor (Robles & Kiecolt-Glaser, 2003).
The state of mediating mechanisms
Despite suggestive evidence for each set of mediating pathways, no studies have firmly established that the association between marital quality and health outcomes is attenuated when including mediating variables that precede the health outcome in time. That said, many studies examine associations between marital quality and health outcomes before and after adjusting for other intervening variables. A quantitative estimate of associations between marital quality and health before and after adjusting for such covariates may provide an initial window into determining whether the candidate mediators of interest in Figure 1 truly serve as mediating variables.
For whom might marital quality and health matter?
The model in Figure 1 also suggests that links between marital quality and health may vary by different groups of individuals or couples, and existing theory highlights two primary moderators of interest: Gender, and personality characteristics related to negative affect including neuroticism and hostility (Suls & Bunde, 2005). Unfortunately, few studies included negative affectivity as predictors alongside marital quality, and none examined such personality characteristics as moderators. Thus, this review focuses on gender and gender-related moderators.
The effects of marital functioning on physiology may be stronger for women compared to men (Kiecolt-Glaser & Newton, 2001; Wanic & Kulik, 2011a). One explanation is that several gender-related factors contribute to women being more aware of and responsive to the affective quality of relational interactions, and spending more time thinking about relationships (Kiecolt-Glaser & Newton, 2001). Gender-related factors include: Self-representations that guide cognitions and behavior; traits that focus on the degree to which individuals focus and attend to others (communion) with the potential exclusion of the self (e.g., unmitigated communion, sociotropy); and roles in domestic labor and childcare. As a consequence, women’s goals and the ways they control their thoughts, feelings, and behavior may be influenced by their close relationships more so than men (Cross & Madson, 1997). Given that the personal relevance of stressful events plays an important role in modulating affective and biological responses to stressors (Lazarus, 1993), this interpersonal-orientation hypothesis (Wanic & Kulik, 2011a) predicts that since close relationships are more personally relevant to women compared to men, women should show greater physiological responses to stressors within the intimate relationship.
Wanic and Kulik (2011a) recently suggested a subordinate-reactivity hypothesis: That the gender difference in associations between marital functioning and physiology may be due to women’s relative subordinate position in marriage. Specifically, the relative social status of women as a whole in society, the interpersonal-orientation characteristics described in the previous paragraph, and economic and domestic labor-related power differentials within the marriage itself all contribute to wives having less power (on average) in the relationship. Coupled with data suggesting that lower status humans and primates have greater stress reactivity, the authors proposed that the subordinate-reactivity hypothesis may be a more comprehensive account of existing data (Wanic & Kulik, 2011b).
Both hypotheses emphasize the importance of factors that are strongly, but not exclusively related to biological sex, due to the combination of biological characteristics (i.e., women’s exclusive childbearing and nursing abilities) and social, economic, and ecological contexts (Wood & Eagly, 2002). Unfortunately, virtually all empirical research on marital functioning and health thus far has focused on sex differences, rather than the gender-related characteristics in both the interpersonal-orientation and subordinate-reactivity hypotheses. Thus, our meta-analysis is limited in the degree to which we can address either hypothesis; however, as discussed in the Method section, we make several attempts to consider the impact of gender and gender inequality as moderators.
What is not the focus of the meta-analysis?
This paper does not examine the association between marital status and health. The mechanisms by which marital status may influence health are distinct from those by which marital quality may influence health. The primary explanations for marital status effects include selection (individuals with better health and protective factors associated with better health may be more likely to get married/stay married), resources afforded by marriage (marriage affords access to joint economic, psychosocial, and societal benefits that are not available to unmarried individuals), and stress associated with marital disruption (divorce, separation, or widowhood are stressful events, and as a result may lead to poorer health outcomes; Sbarra, Law, & Portley, 2011; Stroebe, Schut, & Stroebe, 2007; see Liu & Umberson, 2008 for further elaboration on these explanations). While some explanations overlap, such as resources and stress associated with marital disruption, they are still distinct (e.g., lower social support resources due to a low quality marriage may have a different impact than lower social support due to the absence of a partner). Moreover, the explanations for why being married has benefits for health may have less to do with the effects of being married, and more to do with the effects of not being married (such as selection effects, loss of resources, and increased stress related to divorce, separation, or widowhood). Overall, the association between marital status and health is beyond the scope of the current review, but a quantitative review is certainly warranted.
Primary research aims
Our overall goals are to quantify, through meta-analysis, 1) the relationship between marital quality and health outcomes (surrogate endpoints, subjective clinical endpoints, and objective clinical endpoints), and 2) the relationship between marital quality and two commonly studied biological mediators: Cardiovascular reactivity and HPA axis function. We also examined several theory-based and methodology-related moderators of the expected heterogeneity in effect sizes between studies. To provide a preliminary assessment of the degree to which mediating pathways accounted for links between marital quality and health, we examined the changes in effect sizes for unadjusted and adjusted analyses.
Method
Search strategy
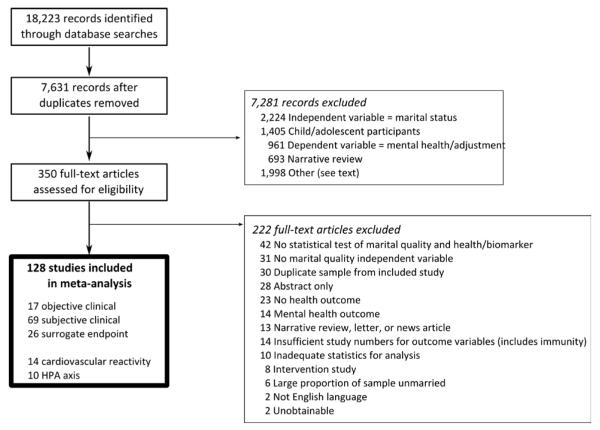
Electronic searches were performed in PsycINFO (1806 – 2011), PubMed (1946 – 2011), and Web of Science (Science Citation Index Expanded, 1899 – 2011; Social Sciences Citation Index, 1900 – 2011; Arts & Humanities Citation Index, 1975 – 2011) with final searches completed by December 26, 2011. The main search strategy used combinations of keywords for marital quality (marriage OR marital quality OR marital satisfaction OR marital adjustment OR marital conflict OR marital support) and health (disease OR risk OR diagnosis OR health OR surrogate marker OR clinical endpoint OR quality-of-life OR self-rated health OR morbidity OR cancer OR cardiovascular disease OR symptoms OR illness OR cardiovascular reactivity OR neuroendocrine OR HPA OR cortisol OR blood pressure OR heart rate OR pain OR mortality). In addition, we cross-referenced our search with articles cited in several seminal reviews of marriage and health research (Burman & Margolin, 1992; Kiecolt-Glaser & Newton, 2001; Leonard, Cano, & Johansen, 2006)3 and manually searched the reference lists of publications that we reviewed. Searches were conducted by manuscript authors and undergraduate research assistants in our laboratory, and search results were collated, checked for duplicates, and sorted by the first author. Full-text articles were reviewed by the authors, who selected articles for inclusion based on the criteria described below. Figure 2 shows the flow diagram.
Figure 2.
Flowchart describing identification and screening of studies.
Study selection
Independent variable: Marital quality
We defined marital quality broadly as global self- or other-reported evaluation of the marriage and/or behaviors within the marriage, in terms of positive dimensions (happiness, support, satisfaction) and negative dimensions (conflict, tension, strain; Bradbury et al., 2000; Fincham & Bradbury, 1987). Most theoretical frameworks of marital quality assume that patterns of behavior exchange between spouses are important antecedents, correlates, and consequences of marital quality (Karney & Bradbury, 1995). Thus, we included behavioral coding of spousal interactions because such measures often reflect aspects of marital quality that are difficult to measure through self-report, are correlated with self-report measures of marital quality, and have yielded significant insights into understanding marital communication (Heyman, 2001).
Self-report measures varied from well-established and widely-used measures such as the Marital Adjustment Test (MAT; Locke & Wallace, 1959) and Dyadic Adjustment Scale (DAS; Spanier, 1976), to validated but less widely-used measures such as the Stockholm Marital Stress Scale (Orth-Gomér et al., 2000), and single-use measures that had acceptable construct validity but were often idiosyncratic to particular studies. Behavioral measures included well-established behavioral coding systems such as the Marital Interaction Coding System (MICS; Heyman, Weiss, & Eddy, 1995), Specific Affect coding system (SPAFF; Gottman & Krokoff, 1989), and the Kategoriensystem für Partnerschaftliche Interaktion Interactional Coding System (KPI; Hahlweg, 1984).
Dependent variables: Health outcomes
Using the Biomarkers Definitions Working Group (2001) definitions, objective clinical endpoints included: Mortality, physician ratings of function or disease severity, diagnosis or incidence of a disease condition or disease-related event, hospitalizations or length of hospitalization, and objectively-assessed physical functioning. When incidence was self-reported by participants and verified clinically, it was considered an objective endpoint. When incidence was not was verified clinically, those outcomes were classified as subjective clinical endpoints, which included self-rated health (single-item measures of perceived health, Short-Form-36 Health Survey [SF-36; Ware, Kosinski, & Dewey, 2000], other physical health-related quality-of-life measures), symptoms (general or disease/condition-specific), pain severity, pain-related disability, adherence to medical recommendations, and functional impairment (e.g., activities of daily living [ADL], such as personal hygiene and self-feeding; or instrumental ADL ratings, such as shopping and housework). Two adherence measures were actually objective, including attendance at dialysis appointments (Kimmel et al., 2000) and electronic reports of continuous positive airway pressure (CPAP) downloaded from the CPAP device in sleep apnea patients (Baron, Smith, Czajkowski, Gunn, & Jones, 2009), which we categorized with subjective adherence measures in subanalyses of adherence outcomes to provide a sufficient number of studies. Surrogate endpoints were defined in Table 1, and the cardiovascular and metabolic markers in particular are considered surrogate endpoints by their respective fields (see references in Table 1, also Sacks et al., 2011).
Dependent variables: Biological mediators
Cardiovascular reactivity and HPA axis function studies had sufficient numbers of studies to include in a meta-analysis. Within HPA axis function, some studies obtained multiple samples during the day across multiple days to measure daily cortisol in naturalistic settings, while others obtained multiple samples before, during, and after a marital conflict discussion task in the laboratory.
Additional inclusion criteria
In addition to the criteria described above, inclusion criteria were as follows: 1) Publication in a peer-reviewed, English language journal; and 2) adequate statistics for computing an effect size r for the relationship between marital quality and health outcome(s). We excluded studies that: 1) only reported relationships between marital status and health, for reasons described in the Introduction; 2) only reported relationships between marital quality and sexual functioning (which have strong bidirectional associations with each other, Schwartz & Young, 2009) or mental health (including mental health-related quality-of-life and various indices of mental well-being and adjustment), which was covered in a previous meta-analytic reviews (Proulx, Helms, & Buehler, 2007); 3) examined marital quality as a dependent variable (e.g., the impact of disease diagnosis on marital quality) or reported results from a non-couples related intervention (e.g., medical treatment) on marital functioning, each of which would reflect the influence of changes in health on marital functioning rather than the reverse; 4) only reported relationships between marital quality and child or adolescent health, rather than adults; and 5) primarily focused on intimate partner violence as an independent variable, where violence and abuse directly contribute to health problems (Campbell, 2002). Participant populations ranged from healthy adults free of chronic illness to patients with chronic illness. We included both cross-sectional and longitudinal designs in the meta-analysis.
Data extraction
A rating sheet was prepared and revised several times during coding. Variables coded included: Study year, first author, country, participant composition, mean age, age range, percentage of women in the sample, marital quality measure, length of follow-up, covariates, and test statistics. All authors served as raters, and each study was coded by at least two raters.
For each study, we computed an effect size r for the relationship between marital quality and health outcome. We derived rs from: Unadjusted correlations between the two variables when reported; β-statistics (standardized regression coefficients) from multiple regression analyses if unadjusted correlations were not available, which were then transformed to rs using an imputation formula (r = β + .05λ, where λ equals 1 when β is nonnegative and 0 when β is negative, Peterson & Brown, 2005); t-statistics from independent-samples t-tests and multilevel modeling if df were available; χ2 statistics; and odds ratios using standard transformations (Borenstein, Hedges, Higgins, & Rothstein, 2009). Several studies reported hazard or risk ratios (HR or RR), which cannot be transformed to rs, and other studies reported p-values or p ranges only (e.g., < .05). For these studies, we converted the p to its one-tailed normal Z-value which corresponded to p = .0005, p = .005, p = .025, and p = .50 for p < .001, .01, .05, and ns, respectively, and computed . In cases where a paper did not provide sufficient statistics we contacted the author to obtain the necessary information.
Dependent samples in endpoint studies
In some cases, our literature search yielded several effect sizes from the same sample reported within the same study (e.g., an effect size for self-rated health and blood pressure). If the multiple dependent variables in a single study could be reasonably separated into the different endpoint categories they were analyzed separately in their respective categories. Multiple dependent variables within the same endpoint category were aggregated, but also analyzed separately in subanalyses (e.g., self-rated health and functional impairment, both subjective clinical endpoints). Our literature search yielded multiple papers from the same sample (rather than several effect sizes from a sample reported in the same paper). To avoid violating the assumption of sample independence (Borenstein et al., 2009), when multiple papers from the same sample had the potential to be in the same set of analyses (e.g., both studies from the Americans’ Changing Lives survey [Prigerson, Maciejewski, & Rosenheck, 1999; Umberson, Williams, Powers, Liu, & Needham, 2006] could be included in analyses of all longitudinal studies), we selected the study with the largest sample size for the analysis.
Multiple metrics in biological mediator studies
Studies examining cardiovascular reactivity to marital discussions (k = 14) typically reported results for heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), or some combination of the three. We extracted separate effect sizes for each metric, and reported aggregated effect sizes across outcomes (e.g., averaging the effect size for SBP and DBP within a study) and within each cardiovascular reactivity metric (HR k = 11, SBP k = 8, DBP k = 6). Most studies examined either absolute levels during marital discussions or changes from baseline to the discussion task.
Studies involving repeated sampling of cortisol during the day across multiple days reported various metrics, including area under the curve with respect to ground (which reflects the total concentration of cortisol during the day; Ditzen, Hoppmann, & Klumb, 2008; Vedhara, Tuinstra, Miles, Sanderman, & Ranchor, 2006), cortisol slope (change in cortisol from morning to evening; Barnett, Steptoe, & Gareis, 2005; Floyd & Riforgiate, 2008; Saxbe, Repetti, & Nishina, 2008; Vedhara et al., 2006), the change from waking to 30-45 min post-waking known as the cortisol awakening response (Barnett, Steptoe, & Gareis, 2005), and individual cortisol data points (e.g., waking cortisol levels; Floyd & Riforgiate, 2008; Saxbe et al., 2008). We had a sufficient number of studies (k > 2) to conduct a meta-analysis for cortisol slopes, but not other metrics. Studies involving cortisol response to marital discussions (k = 4) typically measured cortisol at baseline, and then during and in some cases after the discussions.
Effect size extraction
In analyses of an entire endpoint category, effect sizes were averaged to yield one effect size per study. Effect sizes for multiple related endpoints, most notably SBP and DBP, were averaged to yield a single effect size per study. Several studies reported effect sizes from multiple independent variables and a single endpoint (e.g., three different measures of marital quality related to self-rated health), and these effect sizes were similarly averaged to yield a single effect size per study. We considered using a correction technique to account for the dependency between effect sizes in these studies (Cheung & Chan, 2004, 2008) which is quite advantageous4, but ultimately chose a more conservative approach (increasing possible Type II error by overestimating sampling error) by using the actual sample sizes rather than any correction. Finally, several studies reported different effect sizes from the same sample at different points in time in different papers. If both papers could be included in the same analysis, we used the earlier report to increase the study sample size (i.e., later followup intervals had more attrition). For example, in a study of marital quality in congestive heart failure patients reported mortality, we used the 4-year (Coyne et al., 2001) rather than the 8-year follow-up (Rohrbaugh, Shoham, & Coyne, 2006).
Data analysis
All analyses, with the exception of multilevel models examining the effects of covariates on effect sizes, were conducted using the Comprehensive Meta-Analysis program (Version 2). We performed random effects modeling, which is appropriate since we aggregated data from independent studies that are not functionally identical, with the goal of generalizing to a larger range of studies (Borenstein et al., 2009). Effect sizes were weighted by the inverse of their variances, which allows larger studies to provide larger contributions to the aggregate effect size estimate compared to smaller studies. Throughout the paper, we report 95% confidence intervals (CI). We report two estimates of heterogeneity: Q, a statistical test of whether between-study variance is greater than within-study variance, and I2, the ratio of true heterogeneity to total variation in the observed effects. Larger I2 values (range 0 – 100) indicate that the observed heterogeneity is not spurious and may be systematically explained by moderating variables.
We conducted our primary analyses including cross-sectional and longitudinal designs together, followed by separate analyses for each endpoint and design5. If a paper reported both longitudinal and cross-sectional effect sizes, we included the longitudinal effect size.
Moderators
To examine the contribution of moderating variables, we combined results across cross-sectional or longitudinal studies to increase available study sample size. The contribution of moderating variables to observed heterogeneity was analyzed using random effects meta-regression (method of moments, Borenstein et al., 2009).
Theory-based moderators: Gender and gender inequality
We examined gender composition of the sample (% women) as a moderator, and also tested whether there were gender differences in the relationship between marital quality and health. For gender composition, we determined the proportion of women in each study, shown in Tables 2 - 4. If the relationship between marital quality and health is stronger for women compared to men, one could potentially expect that studies with a greater proportion of women may have larger effect sizes.
Table 2.
Surrogate Endpoint Studies
| Study | Sample characteristics | Marital quality | Dependent measure and effect sizes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| N; Description | M age | % women |
Measure | Validity rating |
Outcome | rmin | SE r | Covariates | rmax | Gender d |
|
| Cross-sectional studies | |||||||||||
| Cardiovascular risk factors – blood pressure | |||||||||||
| Baker et al. (1999) | 161; P/C Hypertension dx Canada |
34.6 | 46.3 | DAS Cohesion | 2.75 | BPa | .08 | .08 | 5 | - | - |
| Barnett et al. (2005) | 105; C, H Subsample of Whitehall United Kingdom |
55 | 36 | SS: Marital role quality – concerns |
3 | BPb | .08 | .08 | 6 | - | - |
| Carels et al., (2000) | 50; C, H Half with DAS > 100 |
33.9 | 100 | DAS (nr) | 4 | BPc | .31 | .13 | 4 | - | - |
| Grewen et al. (2005) | 325; C Normal BP or mild hypertension; 43% African- American, 53% white |
38.5* | 51.7* | DAS (nr) | 4 | BPb | .18 | .05 | 4 | - | 0.09 |
| Holt-Lunstad, Birmingham, & Jones (2008) | 204; C, H | 31.2 | 49 | MAT (nr); DAS Satisfaction |
4 | BPa | .13 | .07 | 2 | - | 0.09 |
| Reeder (1956) | 300; C, H | nr | 0 | Burgess-Cottrell Marital Adjustment Scale short-form |
3.5 | BPd | −.12 | .06 | 0 | - | - |
| Tobe et al. (2005) | 248; C, H Canada |
54.6 | 50.8 | DAS Cohesion | 2.75 | BPa | .12 | .06 | 12 | - | - |
| Trevino et al. (1990) | 109; P/C Hypertension dx |
50.5 | 57.7 | DAS (106) |
4 | BPe | −.11 | .10 | 4 | - | - |
| Trief et al. (2006) | 134; P/C Diabetes patients; Subsample of Phase 1 telemedicine trial |
70.1 | 43 | DAS Cohesion & Satisfaction; Perceived Marital Stress Scale |
4 | BPd | .12 | .09 | 0 | - | - |
| Cardiovascular risk factors – structural markers | |||||||||||
| Baker et al. (1998) | 176; P/C Hypertension dx No other CVD Canada |
46 | 35.6 | DAS (nr) Areas of Change Q |
4 | Relative wall thickness; LVMI |
.00 | .08 | 16 | - | - |
| Gallo, Troxel, Kuller, Sutton-Tyrrell et al. (2003) | 200; C, H Subsample of Pittsburgh Healthy Women’s Study |
47.7 | 100 | SS: Marital satisfaction |
3 | Carotid IMT; Carotid plaque |
.16 | .07 | 3 | - | - |
| Smith, Uchino, Berg, & Florsheim (2012) | 308; C, H Older couples in Utah Health and Aging Study, with no CVD |
63.5 | 50 | Discordant vs. non discordant couplesf |
4 | Coronary artery calcification |
.16 | .06 | 12 | - | 0.03 |
| Other surrogate endpoints | |||||||||||
| Greene & Griffin (1998) | 17; P/C Parkinson’s disease |
72.2 | 12 | MAT (104.5) | 4 | Observed signs of orofacial hypokinesiag |
.16 | .26 | 0 | - | - |
| Sobal et al. (1995) | 1,980; R, NR National Survey of Personal Health Practices and Consequences |
nr | 60 | SS: Marital happiness and problems |
2.5 | BMI | −.02 | .02 | 0 | .04 | 0.11 |
| Trief et al. (2001) | 78; P/C Diabetes dx (56% Type 1) |
46 | 58 | DAS (nr) | 4 | HbA1c | .00 | .12 | 0 | - | - |
| Trief et al. (2006) | 134; P/C Subsample of Phase 1 telemedicine diabetes intervention trial |
70.1 | 43 | DAS Cohesion & Satisfaction; Perceived Marital Stress Scale |
4 | HbA1c | .15 | .09 | 0 | - | - |
| Whisman, Uebelacker, & Settles (2010) | 1,342; NR English Longitudinal Study of Ageing United Kingdom |
64 | 50 | SS: Self-reported supportive and negative interactions with spouse |
2.5 | Metabolic syndromeh |
.08 | .03 | 7 | .09i | 0.13 |
|
Longitudinal studies (length of follow-up intervals in parentheses under Outcome) | |||||||||||
| Baker, Paquette, Szalai, Driver, Perger, Helmers, O’Kelly et al. (2000) | 72; P/C Early hypertension dx Canada |
47.3 | 36 | DAS (108.4) | 4 | Δ LVMI (3 y) | .20 | .12 | 3 | - | - |
| Black (1988) | 26; P/C Obese patients undergoing weight loss program |
45.4 | 69 | Baseline MAT (109.6*) |
4 | Lbs lost (15 mo) | −.42 | .17 | 0 | - | - |
| Gallo, Troxel, Kuller, Sutton-Tyrrell et al. (2003) j | 200; C, H Subsample of Pittsburgh Healthy Women’s Study |
47.7 | 100 | SS: Marital satisfaction |
3 | Δ Carotid IMT and carotid plaque (3 y) |
.12 | .07 | 3 | - | - |
| Hafner et al. (1990) | 71; P/C Obese patients undergoing gastric restriction surgery |
nr | 100 | Marital Attitudes Evaluation Scale: Control and Include behavior subscales |
2.75 | Δ BMI (15 mo) |
.38 | .10 | 0 | - | - |
| Janicki et al. (2005) | 250; C, H Subsample of Pittsburgh Healthy Heart Project |
60.7 | 47.6 | DAS (111.9) | 4 | Δ Carotid IMT (3 y) |
−.07 | .06 | 2 | - | - |
| Phillips et al. (2006) | 66; C, H United Kingdom |
74.6 | 56.5 | MAT (nr) | 4 | Δ Influenza virus vaccine antibody titers (A/Panama strain; 1 mo) |
.20 | .12 | 1 | - | - |
| Tobe et al. (2007) | 229; C, H Canada |
53.7 | 50.8 | DAS Cohesion | 2.75 | Δ 24 h ambulatory BP (1 y) |
.10 | .07 | 13 | - | −0.005 |
| Trief et al. (2002) | 61; P/C Diabetes (56% Type 1) |
47 | 62 | DAS (nr) | 4 | ΔHbA1c (2 y) | .006 | .13 | 0 | - | - |
| Trief et al. (2006) | 134; P/C Subsample of Phase 1 telemedicine diabetes intervention trial |
70.1 | 43 | DAS Cohesion & Satisfaction; Perceived Marital Stress Scale |
4 | HbA1c (1 y) | −.03 | .09 | 8 | - | - |
| Troxel et al. (2005) | 413; C, H Subsample of Pittsburgh Healthy Women’s Study |
47.1 | 100 | SS: Marital satisfaction |
3 | Metabolic syndromeh (3 y) |
.29 | .05 | 3 | - | - |
| Wang et al. (2007) k | 69; P/C Myocardial infarction or unstable angina dx Sweden |
56 | 100 | SS: Marital stress | 3.25 | Δ coronary artery luminal diameter (3 y) |
.32 | .11 | 0 | - | - |
| Whisman & Uebelacker (2012) l | 432; NR English Longitudinal Study of Ageing United Kingdom |
62.4 | 50 | SS: Self-reported supportive and negative interactions with spouse rated by participant and partner |
2.5 | Metabolic syndromeh (4 y) |
.20 | .05 | 7 | - | 0.11 |
Note. Studies are organized by study design (cross-sectional or longitudinal), outcome, and are listed in alphabetical order by author. All study samples collected in the United States unless otherwise noted in the study description. Sample size refers to total number of individuals (as opposed to couples). Signs for all effect sizes were oriented to indicate that higher scores on marital quality are related to better health. For instance, if a reported effect size originally indicated that greater marital quality was related to lower ambulatory systolic blood pressure (r = −.16), and lower ambulatory systolic blood pressure is an indicator of better health, we changed the sign to r = + .16. Covariates only refer to number of variables, not terms in a regression (i.e., interactions). Gender differences were computed as women – men; thus, negative numbers indicate larger effects for women compared to men. Dashes indicate data are not available. For sample descriptions: C = community, dx = diagnosis, H = healthy, NR = nationally representative, P/C = patient/clinic sample + primary diagnosis of interest (if specified), R = random sample. For marital quality measures: SS = Study-specific measure; sample means for the DAS and MAT are reported in parentheses. Unless otherwise noted, Δ = change from baseline measures, nr = not reported, = inferred from other descriptive statistics in paper. CVD = cardiovascular disease; LVMI = left ventricular mass index; IMT = artery intima media thickness; Q = Questionnaire.
24 hour ambulatory BP.
ambulatory SBP and DBP during waking hours.
ambulatory SBP and DBP recorded at home for 15 hours.
Resting SBP and DBP or categories of SBP and DBP based on cutoffs.
Resting DBP – three most recent readings from medical record.
Grouping based on cluster analysis of behavioral and self-reported marital satisfaction data.
Rate of speech, rate and duration of eye blink during couple discussion.
Metabolic syndrome was indicated by presence of 3 or more of the following risk factors (based on established cutoffs): elevated fasting glucose or use of glucose-lowering medication, elevated triglyceride level, low high-density lipoprotein cholesterol level, high waist circumference, high systolic and/or diastolic blood pressure or use of antihypertensive medication.
An rmax model was only available for women, and not men in the sample. In the multilevel modeling analyses only the results for women are included.
Same sample as Troxel et al. (2005). Because of the smaller sample size relative to the Troxel paper, this paper was excluded from the meta-analyses of all longitudinal surrogate endpoint studies, and moderator and sensitivity analyses. The paper was only included in the meta-analyses for cross-sectional CVD surrogate endpoints, and longitudinal CV structural markers. Also same sample as Gallo, Troxel, Matthews, & Kuller (2003), which examined longitudinal associations with hematological markers of cardiovascular risk, including cholesterol, triglycerides, and fasting glucose levels. However, because no other studies examined levels of these markers, we included the Gallo et al. (2003) on atherosclerotic burden because other studies assessing structural markers of cardiovascular disease were available.
Same sample as Orth-Gomér et al. (2000), a longitudinal objective endpoint study. Subsample of Stockholm Female Coronary Risk study. Excluded from moderator analyses.
Same sample as Whisman, Uebelacker, & Settles (2010). Couples < 80 years old in intact marriages who completed the four-year follow-up. Because of the smaller sample size relative to the 2010 paper, this paper was excluded from analyses that combined cross-sectional and longitudinal studies.
Table 4.
Objective Clinical Endpoint Studies
| Study | Sample characteristics | Marital quality | Dependent measures and effect sizes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| N; Description | M age | % women |
Measure | Validity rating |
Outcome |
r
min |
SE r | Covariates | rmax | Gender d | |
| Cross-sectional | |||||||||||
| Fink et al. (1968) | 36; P/C Severely disabled women |
nr | 100 | SS composite a |
3.5 | Physician rating of physical mobility |
.05 | .17 | 0 | - | - |
| Kimmel et al. (2000) | 174; P/C End-stage renal disease patients (90.8% African-American) |
54* | 23 | DAS Satisfaction, Negativity |
4 | Rating of disease severity |
.06 | .08 | 0 | −0.06 | |
| Marcenes & Sheiham (1992) | 164; C Fathers of schoolchildren Brazil |
41.2 | 0 | SS: Marital quality |
2.75 | Count of decayed, missing, and filled tooth surfaces |
.41 | .07 | 0 | - | - |
| Marcenes & Sheiham (1996) b | 164; C Mothers of schoolchildren Brazil |
38.4 | 100 | SS: Marital quality |
2.75 | Dental caries and periodontal disease status based on clinical examination |
.25 | .05 | 0 | - | −0.09 |
| Longitudinal studies (length of follow-up intervals in parentheses under Outcome) | |||||||||||
| Ashmore, Emery, Hauck, & MacIntyre (2005) | 31; P/C Patients with diagnosis of COPD in pulmonary rehabilitation |
67.8 | 35.5 | DAS (111.7) | 4 | Δ 12 min walk test times (5 wk) |
.00 | .19 | 0 | - | - |
| Coyne, Rohrbaugh, Shoham et al. (2001) | 189; P/C Congestive heart failure patients |
53 | 26 | SS compositec | 2 | Mortality (4 years) |
.28 | .07 | 0 | .28 | 0.42 |
| Eaker, Sullivan, Kelley-Hayes, D’Agostino Sr., & Benjamin (2007) | 2,994; C Subsample of Framingham Offspring Study |
49 | 50 | SS: Spouse shows love. |
2.75 | Incidence of CHD (MI, coronary insufficiency and mortality), mortality (10 y) |
.00 | .02 | 7 | - | −0.0006 |
| Haynes, Feinleib, & Kannel (1980) | 1,764; R, C Subsample of Framingham Heart Study |
57.5 | 57 | SS: Conflict, satisfaction |
2.5 | CHD: Myocardial infarction; coronary insufficiency syndrome; angina pectoris; coronary heart disease, death. (8 y) |
.00 | .02 | 0 | - | - |
| Helgeson (1991) | 73; P/C Post myocardial infarction dx |
53.5* | 22 | SS: Disclosure | 2.25 | Rehospitalization for cardiac event (1 y) |
.60 | .08 | 5 | - | - |
| Hibbard & Pope (1993) | 2,157; C 5% sample of regional health maintenance organization members in Pacific Northwest |
41.5* | 54 | SS: Satisfaction |
3 | Diagnosis of stroke, ischemic HD, cancer malignancy, and mortality (15 y) |
.00 | .02 | 5 | - | −0.001 |
| Kiecolt-Glaser et al. (2005) | 84; C, H Married couples |
37 | 50 | Hostile behaviors (RMICS) |
3 | 90% wound healing after blister wound (12 days) |
.23 | .11 | 2 | - | - |
| Kimmel et al. (2000) d | 174; P/C End-stage renal disease patients (90.8% African-American) |
54* | 23 | DAS Satisfaction, Negativity |
4 | Mortality (median 36.8 mo) |
.20 | .07 | 5 | - | 0.29 |
| King & Reis (2012) | 181; P/C Coronary artery bypass surgery recipients |
60.6* | 76.9* | SS: Satisfaction item from MAT 1 y post- surgery |
3 | Mortality (15 y) | .30 | .07 | 0 | .31 | 0.32 |
| Kulik & Mahler (2006) | 296; P/C CABG patients |
64.2 | 24 | DAS (nr) | 4 | Length of stay after first-time CABG operation (5 – 7 days) |
.09 | .06 | 0 | - | 0.21 |
| Medalie et al. (1992) | 8,458; R, C Male civil service employees Israel |
51.8 | 0 | SS: Support (wife showing love) |
1.25 | Duodenal ulcer incidence (5 y) |
.13 | .01 | 6 | .14 | - |
| Orth-Gomér et al. (2000) | 187; P/C Patients previously hospitalized with acute MI; Stockholm Female Coronary Risk study Sweden |
55.8 | 100 | SS: Marital stress |
3.25 | Recurrent coronary events, including mortality (median 4.8 y) |
.19 | .07 | 1 | .19 | - |
| Vitaliano et al. (1993) | 77; P/C Alzheimer’s patients |
71.2 | 34 | Expressed emotion during caregiver interview |
2 | Mini-mental status score (15-18 mo) |
.00 | .12 | 0 | - | - |
| Yang & Schuler (2009) | 100; P/C Newly diagnosed, surgically treated breast cancer patients |
48.6 | 100 | DAS Satisfaction |
4 | Karnofsky Performance Status scale (5 y) |
.08 | .10 | 5 | - | - |
Note. Studies are organized by study design (cross-sectional or longitudinal) and are listed in alphabetical order by author. Sample size refers to total number of individuals (as opposed to couples). All study samples collected in the United States unless otherwise noted in the study description. Signs for all effect sizes were oriented to indicate that higher scores on marital quality are related to better health. Covariates only refer to number of variables, not terms in a regression (i.e., interactions). Gender differences were computed as women – men; thus, negative numbers indicate larger effects for women compared to men. For sample descriptions: C = community, dx = diagnosis, H = healthy, NR = nationally representative, P/C = patient/clinic sample + primary diagnosis of interest (if specified), R = random sampling. For marital quality measures: SS = Study-specific measure; sample means for the DAS and MAT are reported in parentheses. Unless otherwise noted, Δ = change from baseline measures, nr = not reported, = inferred from other descriptive statistics in paper. CABG = Coronary artery bypass graft; CHD = coronary heart disease; COPD = Chronic obstructive pulmonary disease; MI = myocardial infarction; RMICS = Rapid Marital Interaction Coding System.
Companionship, social status, power, understanding, affection, marital esteem, and sex in marriage.
Same sample as Marcenes and Sheiham (1992), only including data from mothers, but the paper provided separate estimates for mothers and fathers allowing for gender comparisons.
Self-reported marital satisfaction, marital routines, positive illness discussions, and observed positive behavior.
Same sample as Kimmel (2000), in cross-sectional subjective endpoints. Included in meta-analysis of cross-sectional studies, and moderator analyses.
To test for gender differences in the relationship between marital quality and health, when possible we extracted separate effect size estimates for men and women and/or statistical tests of the interaction between gender and marital quality on health outcomes. Relatively few studies provided separate effect size estimates for men and women (k = 25), and even fewer provided estimates of the interaction between gender and marital quality (k = 10). When separate effect sizes were available, we computed effect size rs for men and women within each study. We then compared correlation coefficients between men and women within each study by using the procedure developed by Fisher for comparing whether two correlation coefficients are equal, which yields a normally distributed z-statistic (J. Cohen & Cohen, 1983), which was converted to a Cohen’s d using the transform . For studies that reported estimates of the interaction between gender and marital quality, we computed an effect size d based on the test statistics (ts and Fs). We then performed a random effects meta-analysis on the available d-statistics describing differences in the relationship between marital quality and health for men compared to women (after accounting for duplicate samples, k = 34).
For gender inequality, we used the Gender Inequality Index (GII) developed by the United Nations Human Development Report Office (2011), which reflects the degree of disadvantage women face in health (maternal mortality ratio, adolescent fertility rate), empowerment (share of national parliamentary seats held by women, secondary and higher education attainment levels), and labor (workforce participation) in different countries. While this index does not reflect attitudes towards gender role equality (e.g., whether the populace has favorable attitudes towards gender equality), the GII does provide indicators of the real-world manifestations of such attitudes. The GII ranges from 0 (women and men fare equally) to 1 (women fare as poorly as possible in all dimensions). We selected scores from the 1995 report, which was the earliest available (ratings were highly stable across time, with an intraclass correlation of .98 for the 11 countries in this sample). Scores ranged from .08 (Sweden) to .52 (Brazil), with a mean of .21. The most represented country was the United States, GII = .28. Using this index allowed us to examine whether the degree of gender inequality in health, social, and labor between countries moderated the relationship between marital functioning and health, which may partially address the subordinate-reactivity hypothesis discussed in the introduction.
Methodology-related moderators
In addition to type of outcome (surrogate, subjective and objective clinical), we considered several methodology-related moderators: Study design (i.e., cross-sectional versus longitudinal), marital quality construct validity, and publication year.
Study design
Observational research on marital quality and health outcomes involves cross-sectional and prospective longitudinal designs. Cross-sectional studies cannot address the directionality of the relationship between physical health and marital satisfaction; only prospective studies can determine whether poor-quality marriages compromise physical health or whether poor physical health is a causal factor for subsequent marital dissatisfaction. In light of clear methodological differences between cross-sectional and prospective studies, we examined study design as a dichotomous moderator variable.
Marital quality construct validity
Marital quality is a multidimensional construct that can be measured with multiple instruments within multiple modalities, including self- or spouse-report and objective coding. The proliferation of marital quality measures in the literature makes generalizing findings across studies difficult, particularly studies with idiosyncratic measures. To examine construct validity as a potential moderator of the observed relationships between marital functioning and health, study authors independently rated the degree of construct validity of each marital quality measure, where: 0 = not representative, should not be considered for further inclusion in the meta-analysis; 1 = minimally representative of the evaluative and/or behavioral component of marital quality, with items or behaviors not used in traditional marital quality measures, representing only one dimension (positive or negative); 2 = somewhat representative of the evaluative and/or behavioral component of marital quality, with items or behaviors not used in traditional marital quality measures, both positive and negative dimensions represented; 3 = very representative of evaluative/behavioral components, most items shared with traditional marital quality measures, representing only one dimension; 4 = extremely representative, many shared items with traditional marital quality measures, both positive and negative dimensions represented. Measures of relationship satisfaction (e.g., MAT, DAS) and multidimensional measures (PREPARE, ENRICH inventories, Marital Satisfaction Inventory) recommended by Snyder, Heyman, and Haynes (2005) in their review of evidence-based assessments were rated with a 4. We averaged those ratings across the four raters to provide a single rating of marital quality measure construct validity for each study. The two-way random effects intraclass correlation for absolute agreement using the average of the raters was .86, 95% CI [.78, .92], indicating high reliability for the average construct validity ratings.
Publication year
Both marriage and public health have gone through considerable changes over the last half-century, which may influence the relationship between marital quality and health. To address these effects, we examined publication year as a moderator variable.
Covariates and confounders
All studies included were non-experimental, therefore third variables may have potentially confounded relationships between marital quality and health outcomes. One option for dealing with potential confounds is to include effect sizes from analyses that controlled for as many potential confounds as possible (which we called rmax). However, this may result in biased estimates of effect sizes (e.g., a given effect size reflects the relationship between marital quality and the health outcome after accounting for 4 covariates). At the same time, including effect sizes from bivariate analyses (without covariates) may not account for potential confounds. Furthermore, many studies either did not report analyses that included covariates, and others did not report bivariate analyses. We included unadjusted effect sizes (e.g., bivariate correlations) and for studies that did not report unadjusted effect sizes, we included the analysis with the fewest covariates possible (which we called rmin). To empirically determine whether adjusted models yielded different effect size estimates than unadjusted or minimally adjusted models (rmin ≠ rmax), we selected studies that reported effect sizes from both models. We then used multilevel modeling (PROC MIXED in SAS) to compare the within-study differences in effect sizes. Multilevel modeling allowed for nesting effect sizes within studies, and we modeled effect sizes (weighted by sample size) as a function of an intercept, and a dummy-coded variable where 0 was assigned rmin, and 1 was assigned to rmax.
Sensitivity analyses and publication bias
We conducted several analyses to determine whether our results were robust when comparing different study characteristics (Borenstein et al., 2009). Our analyses included whether effect sizes differed between small and large studies (generally, larger sample sizes should be related to smaller effect sizes), and if our estimates were robust when removing studies with significant sample size outliers over n = 5,000, and whether effect sizes differed between studies that used patient vs. nonpatient samples.
Publication bias was assessed by examining funnel plots of effect size and precision6. To aid in our interpretation of the funnel plots, we used Egger’s test, which uses the intercept term from a linear regression predicting the effect size divided by its standard error from the inverse of the standard error (precision) to quantify the degree of funnel plot asymmetry. Intercept terms that are significantly different from 0 at p < .10 suggest an asymmetrical funnel plot, and thus, publication bias in the direction of greater publication of positive results. We note that power for Egger’s test is significantly less for analyses with fewer than 10 studies (Higgins & Green, 2011). To determine whether the overall observed effects might be an artifact of publication bias, we computed Rosenthal’s fail-safe Nfs, which indicates the number of studies with an r = .00 required to make the cumulative effect size non-significant.
Results
Endpoint studies
The characteristics of the included studies are reported in Table 5, and the reported Ns indicate the number of individuals across studies, for a total N = 30,443 in cross-sectional studies, and N = 41,421 for longitudinal studies (total N across studies = 72,674). While large, epidemiological samples were included in each outcome and study design category, with the exception of longitudinal subjective clinical endpoint studies, median sample sizes were small (between 72 and 257). Mean age across samples was around middle-age, which reflects the midpoint of the wide age ranges within the larger studies. Included studies tended to have either equal or greater proportion of women to men. For longitudinal studies, follow-up intervals ranged from within a week to over a decade, with median follow-up around 2 – 5 years.
Table 5.
Descriptive Statistics for Endpoint Studies
| Outcome and study design | N | M age | % women | Follow-up interval (y) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| k | M | Mdn | Range | M | Range | M | Mdn | M | Mdn | Range | |
| Surrogate endpoints | |||||||||||
| Cross-sectional | 16 | 278 | 169 | 17 – 1,965 | 50.6 | 31.1 – 72.2 | 50 | 50 | |||
| Longitudinal | 12 | 169 | 103 | 26 – 432 | 55.6 | 45.4 – 74.6 | 67.9 | 59.3 | 2.13 | 2.5 | 0.083 - 4 |
| Subjective clinical endpoints | |||||||||||
| Cross-sectional | 58 | 513 | 154 | 29 – 7,156 | 49.6 | 26 - 77 | 57.1 | 52 | |||
| Longitudinal | 14 | 1,759 | 455 | 23 – 10,000 | 48.6a | 27.8 – 77 | 50.5 | 52 | 3.95 | 3.5 | 0.005 - 12 |
| Objective clinical endpoints | |||||||||||
| Cross-sectional | 4 | 176 | 169 | 36 - 328 | 45b | 39.8 - 54 | 50 | 50 | |||
| Longitudinal | 14 | 1,198 | 184 | 31 – 8,458 | 54.7 | 37 – 71.2 | 46.6 | 42.75 | 5.17 | 4.4 | −0.02 - 15 |
Note. Sample size refers to total number of individuals (as opposed to couples) aggregated within each category.
k = 13.
k = 3
Surrogate endpoints
Aggregate effect sizes are shown in the top portion of Figure 3, with individual studies in Table 2.7 Greater marital quality was significantly related to better physical health across all studies, r = .09, 95% CI [.04, .15], p = .001. Marital dissatisfaction was more consistently related to structural markers of cardiovascular disease (Baker et al., 1998; Gallo, Troxel, Kuller, Sutton-Tyrrell et al., 2003; Smith et al., 2012) compared to functional markers like blood pressure (Baker et al., 1999; Barnett, Steptoe, & Gareis, 2005; Carels, Sherwood, Szczepanski, & Blumenthal, 2000; Grewen, Girdler, & Light, 2005; Holt-Lunstad, Birmingham, & Jones, 2008; Reeder, 1956; Tobe et al., 2005; Trevino, Young, Groff, & Jono, 1990; Trief et al., 2006). Three studies examined the relationship between marital quality and glucose control in diabetes (Trief, Himes, Orendorff, & Weinstock, 2001; Trief et al., 2006; Trief, Wade, Britton, & Weinstock, 2002), and no study showed a significant relationship between marital quality and glucose control, k = 3, r = −.01, 95% CI [−.13, .11], p = .83. Other outcomes that were included in the overall category, but had insufficient number of studies to generate an aggregate effect size included weight gain (Black, 1988; Hafner, Rogers, & Watts, 1990), neurological signs in Parkinson’s Disease (e.g., rate of eye blink; Greene & Griffin, 1998) and antibody response to influenza vaccine (Phillips et al., 2006) .
Figure 3.
Aggregated effects of marital quality on health across studies and selected subsets of studies: Summary effect size, heterogeneity, and publication bias statistics, and forest plots. Positive correlation coefficients indicate that greater marital quality is related to better health. Diamond and box height is proportional to estimate precision – taller shapes are more precise. Width of the diamonds and error bars represents the 95% confidence interval. The number of studies (k) within an outcome/design category may not add up to the total k due to overlap of studies across categories (e.g., a study can contribute a pain disability and pain severity effect size) and overlap of studies across designs (e.g., a study can contribute a cross-sectional and longitudinal effect size). CV = cardiovascular. Nfs = fail-safe N.
* Significant publication bias by Egger’s test, p < .10
** Significant publication bias by Egger’s test, p < .05
Publication bias
We found no evidence of bias according to Egger’s test. Furthermore, Nfs was sufficiently large across studies (59 for cross-sectional studies compared to our 16 included studies; 84 for longitudinal studies compared to 12 included studies), suggesting that publication bias had little influence on our overall findings.
Subjective clinical endpoints
Aggregate effect sizes are shown in the middle portion of Figure 3, with individual studies in Table 3. Greater marital quality was related to better health, r = .14, 95% CI [.11, .17], p < .001; including better adherence, r = .21, p < .001; lower pain-related disability, r = .21, p = .009; and better self-rated health and/or lower self-rated symptoms, r = .16, p < .001. Marital quality was not related to pain severity, r = .02, p = .77. For functional impairment, marital quality showed a trend in cross-sectional studies, r = .09, p = .06, and no relationship in longitudinal studies, r = .03, p = .55.
Table 3.
Subjective Clinical Endpoint Studies
| Study | Sample characteristics | Marital quality | Dependent measures and effect sizes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| N; Description | M age | % women |
Measure | Validity rating |
Outcome | r min | SE r | Covariates | rmax | Gender d |
|
| Cross-sectional studies | |||||||||||
| Barnett, Davidson, & Marshall (1991) | 188; R Licensed practical nurses and social workers |
39.5 | 100 | SS: Partner role quality |
2 | Sx: Medical Symptom Checklist |
.18 | .07 | 4 | - | - |
| Barnett & Marshall (1993) | 294; R, C | 35 | 0 | SS: Marital role quality |
2.75 | Sx: Physical Symptom Checklist |
.07 | .06 | 8 | - | - |
| Basolo-Kunzer, Diamond, Maliszewski, et al. (1991) | 117; P/C Chronic headache |
40 | 65.8 | DAS Affection | 3 | Pain: SS | −.26 | .09 | 0 | - | - |
| Block & Boyer (1984) | 51; C Spouses of chronic low back pain patients |
41.6 | 50* | MAT (106) | 4 | FxPain: SS - Spouse reported limitations |
.55 | .10 | 0 | - | - |
| Bookwala (2005) | 693; R, NR National Survey of Midlife Development in the United States |
60.5 | 44.9 | SS: Marital quality |
4 | SRH and Sx. Fx: Chronic health problems in past year, ADL, IADLs. |
SRH: .14 Fx: .09 |
SRH: .04 Fx :.09 |
0 | - | - |
| Brown (1994) | 862; P/C Pregnant women |
26 | 50 | SS: Marital problems during pregnancy |
1 | Sx: Somatic symptoms (Health Responses Scale) |
.27 | .03 | 0 | - | 0.03 |
| Cano, Gills, Heinz et al. (2004) | 110; P/C Chronic musculoskeletal back/neck pain |
46.3 | 56 | MAT (108.5) | 4 | Pain: MPI Severity FxPain: SIP |
Pain: .02 FxPain: .12 |
Pain: .10 FxPain: .10 |
0 | - | - |
| Cano, Weisberg, & Gallagher (2000) | 165; P/C Chronic pain |
48.6 | 53 | MAT (113) | 4 | Pain: MPI severity |
.00 | .08 | 0 | - | 0.14 |
| Choi & Marks (2008) a | 1,832; NR National Survey of Families and Households |
44.5 | 54 | SS: Marital disagreement |
2.75 | Fx: SS (Year 1 data) |
.18 | .02 | 5 | - | - |
| Coughlin (1990) | 150; C, P/C PMS dx |
35 | 100 | Marital Satisfaction Inventory |
4 | Sx: Intensity of premenstrual syndrome symptoms |
.26 | .08 | 0 | - | - |
| Dunn, Lewis, Bonner, & Meize-Grochowski (1994) | 38; P/C Spouses of dialysis patients |
58 | 58 | DAS (nr) | 4 | SRH: Quality of Life Index health and functioning subscale |
.54 | .12 | 0 | - | - |
| Fisher et al. (2004) | 158; P/C Type 2 diabetes dx Chinese-American |
56.9 | 41 | SS: Marital satisfaction |
3.5 | SRH: SF-36 General Health |
.25 | .08 | 10 | - | - |
| Fitzpatrick (2009) | 257; C Recruited from community senior centers Canada |
77 | 100 | DAS (nr) | 4 | SRH(1) | −.02 | .06 | 8 | - | - |
| Goodwin (1997) | 126; P/C Chronic fatigue syndrome dx |
42.9 | 100 | DAS (nr) | 4 | Sx: De Groot Chronic Fatigue Syndrome Symptom Scale |
.18 | .09 | 0 | .50 | - |
| Hamilton, Pond, & Ryle (1962) | 146; C, H Parents of young children United Kingdom |
37 | 52 | SS: Objective ratings of whether needs of the couple were being met |
1.5 | Sx: CMI | .29 | .08 | 0 | - | 0.14 |
| Hodgson, Shields, & Rousseau (2003) | 84; C 20 wives with breast cancer, 22 wives with no major illness |
60.3 | 50 | 10 items from DAS Satisfaction |
4 | SRH: SF-36 General Health |
.14 | .11 | 0 | - | −0.15 |
| Kasle, Wilhelm, & Zautra (2008) | 148; P/C Rheumatoid arthritis |
56.6 | 77 | SS: Mutuality, defined as bidirectional disclosure |
1 | FxPain: multiple questionnairesb |
.34 | .07 | 0 | - | −0.02 |
| Kerns, Finn, & Haythornthwaite (1988) | 97; P/C Chronic pain |
50.7 | 17 | MAT (103.7) | 4 | Pain: Hourly ratings for 2 wks |
−.37 | .09 | 0 | - | - |
| Kerns, Haythornthwaite, Southwick, & Giller, Jr. (1990) | 106; P/C Chronic pain |
51.8 | 14 | MAT (102.6) | 4 | Pain: MPI Severity |
−.13 | .10 | 0 | - | - |
| Kerns & Turk (1984) | 30; P/C Chronic pain |
52.1 | 0 | MAT (93.6*) |
4 | Pain: MPQ severity and pain intensity during last week from Pain Screening Inventory |
.31 | .17 | 0 | - | - |
| Kimmel et al. (2000) c | 174; P/C End-stage renal disease patients (90.8% African- American) |
54* | 23 | DAS Satisfaction, Negativity |
4 | Adhobjective: Attendance at dialysis sessions |
.15 | .08 | 0 | - | 0.35 |
| Knoll, Burkert, Rosemeier et al. (2007) | 77; P/C Patients receiving laproscopic prostatectomy Germany |
61.2 | 0 | Spousal support 2 days postsurgeryd |
1 | Pain: 2 days post- surgery |
.004 | .12 | 0 | - | - |
| Ko et al. (2007) e | 287; C, H Utah Health and Aging Study |
54.2* | 50 | MAT (113.6*) | 4 | SRH(1) | .16 | .06 | 0 | - | 0.11 |
| Kool, Woertman, Prins et al. (2006) | 63; P/C Fibromyalgia The Netherlands |
39.3 | 100 | Relation Interaction Satisfaction Scale |
4 | Pain: Bodily pain | .27 | .12 | 0 | .47 | - |
| Kudel, Edwards, Raja et al. (2008) | 152; P/C Breast cancer post- mastectomy |
56.4 | 100 | SS: Marital satisfaction in context of cancer |
2 | FxPain: Pain Disability Index |
.41 | .07 | 4 | - | - |
| Kurpius, Nicpon, & Maresh (2001) | 136; C | 47 | 100 | DAS (107.4) | 4 | Sx: Menopausal symptoms from Women’s Health Questionnaire |
.31 | .08 | 0 | - | - |
| Leong, Cano, & Johansen (2011) | 78; P/C Chronic pain |
54.7 | 58 | Validation/invalid ation (SPAFF) |
1 | Pain: MPI Severity |
.02 | .12 | 0 | - | - |
| Levenson et al. (1993) | 156; R, C | 55* | 50 | Locke- Williamson; MAT (111.5*) |
4 | Sx: CMI Fx: SS |
Sx: .23 Fx: .00 |
Sx: .08 Fx :.08 |
0 | - | 0.36 |
| A. D. Mancini & Bonanno (2006) | 1,532; R, C Changing Lives of Older Couples study |
68.9 | 69 | DAS items | 4 | Fx: 4 items from Katz ADL Index |
−.02 | .03 | 0 | - | - |
| Masheb, Brondolo, & Kerns (2002) | 42; P/C Chronic vulvar pain |
43.9 | 100 | MAT | 4 | Pain: MPI Severity FxPain |
Pain: −.07 FxPain: .20 |
Pain: .16 FxPain: .15 |
0 | - | - |
| R. A. Matthews, Del Priore, Acitelli, & Barnes-Farrell (2006) | 226; R, C | 34.9 | 50 | SS: Relationship tension and satisfaction |
3.63 | Sxf | .29 | .06 | 0 | - | 0.17 |
| Meana, Binik, Khalife, & Cohen (1998) | 76; P/C Dyspareunic pain Canada |
40.18 | 100 | MAT (96.3) | 4 | Pain: MPQ severity |
.35 | .10 | 0 | .10 | - |
| Molloy, Perkins-Porras, Strike, & Steptoe (2008) | 144; P/C Acute coronary syndrome patients with partner United Kingdom |
60.6* | 23* | SS: Partner stress | 1 | SRH: SF-36 PCS Adhsubjective: Medication |
SRH: .10 Adh: .28 |
SRH: .08 Adh: .08 |
6 | - | - |
| Pence, Thorn, Jensen, & Romano (2008) | 64; P/C Chronic headache |
42.5 | 73.4 | MAT (108.33) | 4 | Pain: Wisconsin Pain Inventory FxPain: Wisconsin Pain Inventory |
Pain: −.07 FxPain: −.11 |
Pain: .13 FxPain: .13 |
0 | - | - |
| Raichle, Romano, & Jensen (2011) | 94; P/C Chronic musculoskeletal pain |
43.2 | 55 | DAS (112.9) | 4 | FxPain: SIP interference |
−.13 | .10 | 0 | - | - |
| Reese, Somers, Keefe et al. (2010) | 158; P/C Rheumatoid arthritis patients |
54.9 | 74.7 | MAT (112.7) | 4 | Pain: MPQ sensory and affective pain |
.27 | .08 | 0 | .12 | - |
| Ren (1997) | 7,156; R, NR National Survey of Families and Households |
37.95* | 58* | SS: Marital quality |
3.5 | SRH(1) | .09 | .01 | 4 | .09 | - |
| Romano, Turner, & Jensen (1997) | 50; P/C Chronic pain |
49 | 50 | DAS (112.06) |
4 | FxPain: SIP disability |
.17 | .14 | 0 | - | - |
| Ryan & Willits (2007) g | 534; C Cohort initially recruited from rural Pennsylvania high schools |
70.5* | nr | SS: Marital satisfaction |
3 | SRH: SS Fx: SS |
SRH: .07 Fx: .07 |
SRH: .07 Fx: .07 |
0 | - | - |
| Saarijärvi, Rytökoski, & Karppi (1990) | 63; P/C Chronic low back pain Finland |
47 | 51 | 14 DAS items; 6 Marital Communication Inventory items |
4 | FxPain | .23 | .12 | 0 | - | 0.46 |
| Sandberg, Miller, Harper, Robila, & Davey (2009) | 1,072; NR | 63.7* | 50 | SS: Latent variableh |
4 | SRH: Health problems and SRH(1) |
.12 | .03 | 4 | - | −0.03 |
| Schmoldt et al. (1989) i | 2,008; C 5% sample of regional health maintenance organization members in Pacific Northwest |
- | 50 | SS: Cohesion | 2.25 | SRH (1) | .13 | .02 | 0 | .13 | −0.02 |
| Shek (1995) | 1,501; R, C Multiple-stage cluster sample of public housing residents Hong Kong |
44.3* | 50.7* | Chinese DAS (nr); Chinese Kansas Marital Satisfaction Scale |
4 | SRH: Two items | .14 | .03 | 0 | - | 0.02 |
| Siegel (1986) | 130; P/C PMS patient selected for severe symptoms United States |
33 | 100 | Renne Index of Marital Satisfaction |
3.75 | Sx: Premenstrual symptoms |
.26 | .08 | 0 | - | - |
| Staland-Nyman et al. (2008) | 1062; C Employed women living in a specific county Sweden |
40.5 | 100 | SS: Domestic work equity and marital satisfaction |
2 | SRH: SF-36 physical health |
.12 | .03 | 0 | .05 | - |
| Strawbridge et al. (2004) j | 810; C Subsample of couples in Alameda County Study |
68.9* | 50 | SS: Marital happiness |
2.75 | Sx: Sleep problems |
.04 | .04 | 4 | - | 0.09 |
| Sullivan et al. (1994) | 49; P/C Tinnitus dx |
62.1 | 48 | DAS Cohesion | 4 | Fx: Tinnitus interference |
.34 | .13 | 4 | .00 | - |
| Trevino et al. (1990) | 109; P/C Hypertension dx |
50.5 | 57.7 | DAS (106) | 4 | Adhsubjective: Forgetting & stopping medications |
.25 | .09 | 4 | - | - |
| Trief et al. (2001) | 78; P/C Diabetes (56% Type 1) |
46 | 58 | DAS (nr) | 4 | SRH: SF-36 PCS | .00 | .12 | 2 | - | - |
| Troxel et al. (2009) | 1,938; C Study of Women’s Health Across the Nation |
45.8 | 100 | Single marital happiness item from DAS |
3.25 | Sx: Insomnia | .14 | .02 | 0 | .03 | - |
| Umberson et al. (2006) | 1,049; R, C Americans’ Changing Lives panel survey |
49.9 | 64 | SS: Positive and negative marital experience |
4 | SRH(1): Intercept model |
.06 | .03 | 11 | - | 0.07 |
| Waltz, Badura, Pfaff, & Schott (1988) | 400; P/C Verified first myocardial infarction Germany |
50* | 0 | SS: Marital problems and intimate attachment |
3.75 | SRH (1) | −.07 | .05 | 0 | - | - |
| Weiss & Aved (1978) | 208; C, H | 30 | 50 | MAT (112.3*) | 4 | Sx: CMI | .46 | .06 | 0 | .32 | −0.08 |
| Wickrama, Bryant, & Wickrama (2010) | 540; C African-American couples |
33.8 | 50 | SS: Spouse hostile behavior |
1.5 | SRH (1) Sx: Self-reported physical complaints |
.12 | .05 | 0 | .20 | 0.01 |
| Wickrama et al. (1997) | 364; C Rural Iowa counties |
40.59 | 50* | SS: marital quality |
3.38 | Sx (Intercept model) |
.16 | .05 | 5 | - | 0.02 |
| Willits & Crider (1988) | 1292; C Cohort from Ryan and Willits (2007) |
53* | 57 | SS: Marital satisfaction |
3 | SRH (1) | .08 | .03 | 0 | .07 | - |
| Yorgason et al. (2006) | 192; C Subsample of VA Normative Aging Study |
74 | 50 | 14-item DAS | 4 | Sx: SS and Wyler’s Seriousness of Illness Rating Scale |
−.08 | .07 | 0 | - | -0.15 |
| Zhou, Kim, Rasheed, et al. (2011) | 29; P/C Prostate cancer survivors |
71.9 | 0 | DAS Satisfaction (patient, spouse) |
4 | SRH: SF-36 physical health subscale |
.46 | .16 | 1 | - | - |
| Longitudinal studies (length of follow-up intervals in parentheses under Outcome) | |||||||||||
| Appelberg, Romanov, Heikkila, Honkasaol, & Koskenvuo (1996) | 2,195; C Nationwide sample of twins Finland |
44* | 50 | SS: Recent marital conflict |
2.25 | Fx: Work disability over 6 year interval or early retirement on medical grounds) (5 y) |
.01 | .02 | 3 | - | 0.03 |
| Baron et al. (2009) | 23; P/C Obstructive sleep apnea dx |
49.48 | 0 | Quality of Relationship Inventory support and conflict subscales |
3.75 | Adhobjective: Reports from CPAP device (3 mo) |
.24 | .21 | 0 | .17 | - |
| Choi & Marks (2008) a | 1,832; NR National Survey of Families and Households, sample with longitudinal data |
44.5 | 54 | SS: Marital disagreement |
2.75 | Fx: 4 instrumental ADL items (3 y) |
.11 | .02 | 5 | - | - |
| Guyll, Cutrona, Burzette, & Russell (2010) | 184; C Family and Community Health Study; African- American couples |
37.7 | 90 | Positive behavior at Wave 1 (IFIRS) |
3 | SRH: 5 SF-12 scales (4 y) |
−.04 | .07 | 0 | - | - |
| Hawkins & Booth (2005) | 1,147; NR Marital Instability Over the Life Course study |
35.46 | 62 | SS: Marital happiness and global satisfaction |
3 | SRH(1) (12 y) | .11 | .03 | 0 | - | - |
| Helgeson (1991) | 90; P/C Post myocardial infarction dx |
53.5* | 22 | SS: Marital disclosure |
2.25 | Sx: Severity of post-MI chest pain SRH(1) (1 y) |
.21 | .10 | 5 | - | 0.14 |
| Homish, Leonard, & Cornelius (2010) | 546; C | 27.8 | 50 | MAT at 7 y follow-up (103.9) |
4 | Adhsubjective: Nonmedical use of prescription drugs (9 years) |
.20 | .04 | 0 | .12 | 0.11 |
| Knoll, Burkert, Rosemeier et al. (2007) | 77; P/C Patients receiving laproscopic prostatectomy Germany |
61.2 | 0 | Spousal support prior to surgeryb |
1 | Pain: Severity at surgery site and other areas 2 days post-surgery |
−.05 | .12 | 0 | - | - |
| Levenstein et al. (1995) | 6,928; C Participants in the Alameda County Study |
nr | 54.4 | SS: Marital strain | 3.75 | Sx: Peptic ulcer incidence (8 - 9 y) |
.08 | .01 | 1 | .05 | 0.15 |
| Medalie et al. (1973) | 10,000; R, C Male civil service employees Israel |
51.8 | 0 | SS: Problems and conflicts in the family |
1.63 | Sx: Angina incidence (5 y) |
.22 | .01 | 1 | - | - |
| Prigerson et al. (1999) k | 927; NR Americans’ Changing Lives survey |
52.3 | 100 | SS: Marital satisfaction and harmony |
3.75 | Fx: ADLs (3 y) | −.07 | .03 | 4 | .05 | - |
| Rohrbaugh, Mehl, Shoham, Reilly, & Ewy (2008) | 120; P/C Heart failure dx |
67 | 50 | SS: Compositel | 3.75 | Δ SRH: SF-36 Δ Sx: Heart failure sxs (0.5 y) |
.40 | .08 | 3 | - | - |
| Trief et al. (2002) | 61; P/C Diabetes dx (56% Type 1) |
47 | 62 | DAS (nr) | 4 | SRH: SF-36 physical (2 y) |
.11 | .13 | 1 | - | - |
| Umberson et al. (2006) | 1,049; R, C Americans’ Changing Lives panel survey |
49.9 | 64 | SS: Positive and negative marital experience |
4 | SRH(1) (8 y, slope model) |
.07 | .03 | 11 | - | 0.04 |
| Wickrama et al. (1997) | 364; C Rural Iowa counties |
41.61 | 50* | SS: Marital quality |
3.38 | Self-reported symptoms (2 y – slope model) |
.37 | .05 | 4 | - | −0.43 |
Note. Studies are organized by study design (cross-sectional or longitudinal) and are listed in alphabetical order by author. All study samples collected in the United States unless otherwise noted in the study description. Sample size refers to total number of individuals (as opposed to couples). Signs for all effect sizes were oriented to indicate that higher scores on marital quality are related to better health. Covariates only refer to number of variables, not terms in a regression (i.e., interactions). Gender differences were computed as women – men; thus, negative numbers indicate larger effects for women compared to men. For sample descriptions: C = community, dx = diagnosis, H = healthy, NR = nationally representative, P/C = patient/clinic sample + primary diagnosis of interest (if specified), R = random sampling. For marital quality measures: SS = Study-specific measure; sample means for the DAS and MAT are reported in parentheses. Unless otherwise noted, Δ = change from baseline measures, nr = not reported, = inferred from other descriptive statistics in paper. Adh = adherence, with subjective or objective in subscript; ADL = Activities of Daily Living; CMI = Cornell Medical Index. Fx = Functional impairment; FxPain = Functional impairment due to pain; IADLS = Instrumental Activities of Daily Living; IFIRS = Iowa Family Interaction Rating Scale; MPI = West Haven-Yale Multidimensional Pain Inventory; MPQ = McGill Pain Questionnaire; PCS = Physical Component Score from SF-36; PMS = Premenstrual syndrome; SF-36 = Short Form – 36 Health Survey; SIP = Sickness Impact Profile; SPAFF = Specific Affect Coding System; SRH(1) = single item measure of self-rated health; Sx = symptoms.
Same sample as Ren (1997) in cross-sectional subjective endpoints. Because of the overlap in design, and smaller sample size relative to the Ren paper, this paper was excluded in the meta-analyses of all cross-sectional subjective endpoint studies and all cross-sectional studies, and was only included in the meta-analysis for all longitudinal subjective endpoint studies and all longitudinal studies.
Health Assessment Questionnaire – ADLs; Arthritis Impact Measurement-2 Short Form: arthritis impact on ADLs, work, social function.
Same sample as Kimmel (2000), in cross-sectional objective endpoints. Excluded from meta-analysis of cross-sectional studies, and moderator analyses.
Enacted spousal support - Berlin Social Support Scale; received social support (modified items from the Brief COPE).
Same sample as Smith et al. (2011), in cross-sectional surrogate endpoints. Excluded from meta-analysis of all cross-sectional studies and moderator analyses.
Frequency of trouble sleeping, feeling nervous and tense, stomach problems, and headaches.
Same sample as Willits and Crider (1988) in cross-sectional subjective endpoints. Because of the overlap in outcome and design, and smaller sample size relative to the Willits paper, this paper was excluded from meta-analyses of cross-sectional subjective endpoint studies or all cross-sectional studies, and was only included in the meta-analyses for cross-sectional functional impairment.
Latent variable measured by Global Distress Scale, Problem Solving Communication scale from Marital Satisfaction Inventory-Revised, Personal Assessment of Intimacy in Relationships.
Same sample as Hibbard and Pope (1993) in longitudinal objective endpoints. No overlap in outcome or design so this paper was not excluded from any analyses.
Same sample as Levenstein (1995), in longitudinal subjective endpoints. No overlap in outcome or design so this paper was not excluded from any analyses.
Same sample as Umberson et al., (2006) in longitudinal subjective endpoints. Because of the overlap in design, and smaller sample size relative to the Umberson paper, this paper was excluded from the meta-analyses of longitudinal subjective endpoint studies or all longitudinal studies, and only included in the meta-analyses for longitudinal functional impairment.
Standardized scores (patient and spouse) across Relationship Assessment Scale and Constructive Communication Scale.
Publication bias
The effect sizes for cross-sectional studies of self-rated health and symptoms showed significant publication bias based on Egger’s test, k = 33, regression intercept = 1.43, 95% CI [0.25, 2.61], p = .02. The funnel plot in Figure 4 suggested that studies finding positive associations between marital quality and self-rated health were more likely to be published, with only two published studies reporting negative associations between marital quality and self-rated health. Publication bias was not evident for the other cross-sectional outcomes. Longitudinal studies showed no evidence of publication bias using Egger’s test. For self-rated health, the cross-sectional Nfs = 2,703, and the longitudinal studies Nfs = 600, suggesting that despite publication bias in cross-sectional studies, the effect of marital quality on self-rated health was probably robust against publication bias.
Figure 4.
Funnel plot depicting the relationship between effect size and precision (publication bias) in cross-sectional studies of self-rated health and symptoms. The diamond depicts the mean effect size, and each circle depicts a single effect size. The solid horizontal line depicts no effect.
Objective clinical endpoints
Aggregate effect sizes are shown in the bottom portion of Figure 3, with individual studies in Table 4. Greater marital quality was related to better health, r = .15, 95% CI [.09, .21], p < .001. Cross-sectional studies examined the relationship between marital quality and physician rating of physical mobility in severely disabled women (Fink, Skipper, & Hallenbeck, 1968), oral health (Marcenes & Sheiham, 1992, 1996), and objective rating of end-stage renal disease severity (Kimmel et al., 2000), r = .21, p = .03. Longitudinal studies examined the relationship between marital quality and disease incidence (Eaker et al., 2007; Haynes, Feinleib, & Kannel, 1980; Hibbard & Pope, 1993; Medalie et al., 1992), cardiovascular disease-related events, including rehospitalization, myocardial infarction, days in the hospital following surgery, and mortality (Coyne et al., 2001; Eaker et al., 2007; Haynes et al., 1980; Helgeson, 1991; King & Reis, 2012; Kulik & Mahler, 2006; Orth-Gomér et al., 2000), objectively assessed physical (Ashmore et al., 2005; Yang & Schuler, 2009) and cognitive function (Vitaliano et al., 1993), mortality from end stage renal disease (Kimmel et al., 2000), all-cause mortality (Hibbard & Pope, 1993), and objectively assessed wound healing (Kiecolt-Glaser et al., 2005), r = .13, p < .001. Due to the small number of studies within each category, longitudinal studies involving cardiovascular disease outcomes, r = .19, did not show significantly larger effect sizes compared to studies that did not involve cardiovascular disease outcomes, r = .09, Q(1) = 1.88, p = .17. Greater marital quality was related to lower risk of early mortality, k = 7, r = .11, p = .003 (Coyne et al., 2001; Eaker et al., 2007; Haynes et al., 1980; Hibbard & Pope, 1993; Kimmel et al., 2000; King & Reis, 2012; Orth-Gomér et al., 2000). Of the seven studies examining mortality, two studies combined mortality with other cardiovascular disease-related clinical endpoints, and did not provide separate effect size estimates for mortality outcomes only (Haynes et al., 1980; Orth-Gomér et al., 2000). For example, being hospitalized for a heart attack (but not dying) and dying from a heart attack were counted as “events” in the analyses. After excluding both studies, greater marital quality remained significantly related to lower risk of early mortality, r = .19, 95% CI [.04, .33], p = .01, Nfs = 42.
Publication bias
We found no evidence of publication bias for cross-sectional or longitudinal studies based on Egger’s test. Further, the Nfs suggested that publication bias was small and had little influence on the findings. Egger’s test indicated publication bias for longitudinal studies of cardiovascular disease (k = 7, regression intercept = 5.05, 95% CI [2.94, 7.16], p = .002), and mortality (k = 7, regression intercept = 4.53, 95% CI [3.14, 5.92], p = .0004), suggesting that studies finding that greater marital quality was related to better cardiovascular disease outcomes and lower mortality risk were more likely to be published. However, Egger’s test has lower power to distinguish chance from true funnel plot asymmetry when k < 10 (Higgins & Green, 2011), and the Nfss were sufficiently large to mitigate concerns about publication bias.
Moderator analyses
Given the significant heterogeneity across studies, we conducted several analyses to determine whether theory-based moderators and methodology-related moderators explained systematic differences among studies. Unless noted otherwise, studies were combined across outcome type to increase available study sample size.
Theory-based moderators: Gender and gender inequality
To examine whether the relationship between marital quality and health outcomes differed between men and women, we first used meta-regression. Greater proportion of women in study samples was related to larger effect sizes, although this bordered statistical significance, k = 101, slope = 0.0009, p = .051.
Our second approach, testing whether effect sizes for the relationship between marital quality and health differed between men and women, drew from a subset of studies (k = 34) and yielded no significant gender difference, mean d = 0.04, SE = 0.02, 95% CI [−0.01, 0.09], p = .12. Looking specifically within each endpoint, there were no significant gender differences for objective clinical outcomes, k = 7, mean d = 0.03, SE = 0.09, 95% CI [−0.14, 0.19], p = .76, or subjective clinical outcomes, k = 21, mean d = 0.03, SE = 0.03, 95% CI [−0.03, 0.09], p = .36. However, the relationship between marital quality and surrogate endpoints was larger for women as compared to men, k = 6, mean d = 0.10, SE = 0.03, 95% CI [0.04, 0.16], p = .001. Notably, all the included surrogate endpoint studies involved cardiovascular disease-related surrogate endpoints, and the small Nfs = 5 and inspection of the funnel plot suggested that studies showing larger effects for women compared to men were overrepresented in the sample. Overall, of the 7 studies (out of 34) that showed statistically significant gender differences, two showed larger effects for men compared to women (Kimmel et al., 2000; Wickrama, Lorenz, Conger, & Elder, 1997), and five showed larger effects for women compared to men (Coyne et al., 2001; Kulik & Mahler, 2006; Levenson, Carstensen, & Gottman, 1993; Levenstein et al., 1995; Sobal et al., 1995; Whisman, Uebelacker, & Settles, 2010).
The observed gender differences were small, even in the surrogate endpoint category where significant gender differences were observed. Thus, we explored two possibilities: Studies were under-powered or the proportion of women in the study sample may have been systematically related to the magnitude of gender differences (i.e., studies with proportionally fewer women might have smaller effects). Regarding power, a given study would need at least n = 3,142 to detect the effect size d = 0.10 estimate from surrogate endpoint studies (two-tailed test, α = .05, power = .80). Only three of the 34 studies had sufficient sample size to detect such an effect. To detect the largest statistically significant gender differences (approximately ∣d∣ = .43; Coyne et al., 2001; Wickrama et al., 1997), a given study would need n = 172 using the same power assumptions. Most studies (26 out of 34) had sufficient sample sizes to detect the largest effect. A random effects meta-regression showed that proportion of women in the sample was not significantly related to gender difference effect size, slope = 0.002, p = .54.
For gender inequality, we conducted meta-regressions with the 1995 GII as a moderator. Greater gender inequality was related to larger effect size, slope = .40, p = .04. However, this was primarily accounted for by two papers from the same study in Brazil (Marcenes & Sheiham, 1992; 1996), a country > 2 SD from the sample GII mean. After removing the two papers, the relationship between gender inequality and effect sizes was not significant, slope = 0.17, p = .46.
Methodology-related moderators
We compared whether study design or outcome within each study design category was significantly related to effect sizes. There was no significant difference in effect sizes for cross-sectional compared to longitudinal studies across all studies, Q(1) = 0.69, p = .41, surrogate endpoints, Q(1) = 1.85, p = .17, subjective clinical endpoints, Q(1) = 0.18, p = .68, or objective clinical endpoints, Q(1) = 0.70, p = .40. For all longitudinal studies, longer follow-up intervals were related to smaller effect sizes, slope = −0.009, p = .02, shown in Figure 5. In terms of comparing outcomes, the difference in effect sizes for the three outcome categories was not significant Q(2) = 2.41, p = .30.
Figure 5.
Relationship between longer follow-up interval and smaller effect sizes in longitudinal studies. Each circle represents a single study (k = 36). Circle diameter is proportional to sample size (using random effects meta-regression).
Marital quality construct validity
To test whether our ratings of construct validity (Tables 2 - 4) were systematically related to effect sizes, we conducted a meta-regression with construct validity ratings as the independent variable. Greater marital quality construct validity rating was not related to effect size, k = 101, slope = −0.02, p = .19, even after excluding two longitudinal studies because of their extremely large sample sizes (slope = −.02, p = .22; Levenstein et al., 1995; Medalie et al., 1992). Construct validity ratings were negatively skewed, as over half (k = 52 out of 101) received a “4” rating. Removing studies receiving equal to 4 did not change the pattern of results, k = 49, slope = −0.02, p = .44. We explored the general lack of relationship between construct validity rating and effect sizes further, and noted that large studies had more study-specific measures of marital quality that were rated with lower construct validity8.
Publication year
Publication year was not significantly related to effect size, slope = 0.0004, p = .76). Similar results were obtained for cross-sectional, slope = 0.0001, p = .97 and longitudinal studies, slope = −0.0006, p = .93. For surrogate markers, more recent publications had larger effect sizes, slope = 0.005, p = .01. However, one study was more than 4 SD from the publication year mean (Reeder, 1956). After removing the study, there was no significant effect of publication year for surrogate markers, slope = 0.008, p = .10. For subjective and objective clinical outcomes, publication year was not related to effect size (ps > .16).
Covariates and cofounders
Other factors related to marital quality, notably demographic variables, health behaviors, or mental health status could explain links between marital quality and health. Of the studies reviewed in this paper, half included at least one covariate in their statistical analyses (data not shown). Demographic variables—particularly age—were controlled for in over half of the studies that included covariates. Psychological processes (e.g., negative affect), and health behaviors were rarely included as covariates. For example, only one or two out of every ten studies adjusted for health behaviors, with smoking the most consistently employed covariate.
To provide some inferences about whether controlling for such variables decreases the relationship between marital functioning and health, we identified 21 studies that reported effect sizes from more than one statistical model, and selected studies that reported an rmin and rmax. The word cloud in Figure 6 depicts the covariates adjusted for in these studies. Age, economic, and educational status were the most frequently appearing covariates. The range for rmin was −.07 - .46, and the range for rmax was .00 - .50. The average rmin (the intercept parameter in the mixed model) across studies was r = 0.16, p < .0001, a magnitude similar to the effect sizes observed across the larger set of studies included in this meta-analysis. Multilevel modeling indicated that the rmax did not significantly differ from rmin, parameter estimate = 0.005, SE = 0.01, p = .71. Thus, controlling for variables such as age and SES did not significantly change the relationship between marital functioning and health. However, these findings were based on a very small subsample of studies and should be interpreted with caution.
Figure 6.
Word cloud depicting covariate frequencies in studies with both minimal and maximal covariate adjustment. Font size is proportional to the number of studies (out of k = 21) including the covariate in rmax analyses. Numbers indicating the frequency of studies including the covariate are also shown.
Sensitivity Analyses
The following sensitivity analyses determined whether our results were robust to the assumptions made in our review (Borenstein et al., 2009).
Sample size and outliers
We compared studies with n ≤ 161 (the median across all studies) with studies with n > 161 within each outcome category, shown in Table 6. Across all outcomes, effect sizes were marginally greater for studies with small compared to large samples. Within each outcome, although the pattern was consistent with the expectation that smaller samples would have larger effect sizes, there were no significant differences between small and large studies. Regarding outliers, several studies had n > 5,000. We conducted the analyses excluding studies with sample sizes that were greater than 3 SD above the mean across all studies, and we obtained similar effect size estimates across all endpoints (data not shown).
Table 6.
Sensitivity Analyses for Endpoint Studies
| Comparison groups | k | Effect size r | Between-group Q | p-value |
|---|---|---|---|---|
| Sample size | ||||
| All studies | ||||
| n ≤ 161 | 51 | .18*** | 3.27 | .07 |
| n > 161 | 50 | .12*** | ||
| Surrogate endpoints | ||||
| n ≤ 161 | 11 | .12 | 0.28 | .60 |
| n > 161 | 13 | .08* | ||
| Subjective clinical endpoints | ||||
| n ≤ 161 | 31 | .18*** | 2.48 | .12 |
| n > 161 | 22 | .11*** | ||
| Objective clinical endpoints | ||||
| n ≤ 161 | 6 | .19 | 0.19 | .67 |
| n > 161 | 11 | .14*** | ||
| Patient vs. Heterogeneous samples | ||||
| Patient | 51 | .12*** | 0.51 | .48 |
| Heterogeneous | 50 | .15*** | ||
Note. P-values for statistical significance of effect size estimates are indicated with asterisks. Between-group heterogeneity statistics and p-values for statistical significance of the difference between groups of studies are shown in the last two columns.
p < .05,
p < .01,
p < .001
Patient samples vs. nonpatient samples
We compared effect sizes for studies that clearly identified their samples as medical patient samples (e.g., coronary patients, diabetes patients) and studies that did not identify their samples as exclusively composed of medical patients (Table 6). We note that inclusion of medically ill patients in nationally-representative samples is very likely, but that such samples were not composed of homogeneous patient samples, such as breast cancer patients. Effect sizes did not differ between patient and heterogeneous samples.
Biological mediator studies
The characteristics of the studies assessing cardiovascular reactivity, daily cortisol slopes, and cortisol reactivity are reported in Table 7. Individual cardiovascular reactivity studies are reported in Table 8, and cortisol response studies are reported in Table 9.
Table 7.
Descriptive Statistics for Biological Mediator Studies
| Outcome | k | N | M age | % women | ||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| M | Mdn | Range | M | Range | M | Mdn | ||
| Cardiovascular reactivity | 14 | 143.8 | 86 | 24 – 600 | 38.3 | 25 – 57.4 | 54 | 50 |
| Daily cortisol slopes | 6 | 83.5 | 86 | 20 - 144 | 43.4 | 34 - 55 | 64.4 | 50 |
| Cortisol reactivity | 4 | 121 | 121 | 82 – 180 | 40.6 | 25.7 – 66.8 | 50 | 50 |
Table 8.
Acute Cardiovascular Reactivity Studies
| Design, study | Sample characteristics | Marital quality | Dependent measures and effect sizes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| N; Description | M age | % women |
Measure | Validity rating |
Outcome (task) |
rmin | SE r | Covariates | Gender d | |
| Brown & Smith (1992) | 90; C Married couples |
26 | 50 | Behavior: Belittling, blaming (SASB) |
1 | Δ SBP (free talk) |
SBP -.22 | .10 | 0 | SBP: 0.25 |
| Carels, Szczepanski, Blumenthal, & Sherwood (1998) | 50; H,C Married, normotensive women |
33.9 | 100 | DAS (97.2*) |
4 | Δ HR, SBP, DBP (conflict recall) |
HR: −.16 SBP: −.18 DBP: −.24 |
HR, SBP, DBP: .14 |
4 | - |
| Carrere, Yoshimoto, Mittmann et al. (2005) | 108; H, C | 41.5 | 50 | Affect: Anger (SPAFF) |
2.5 | Average IBI (conflict discussion) |
HR: −.11 | .10 | 0 | HR: −0.10 |
| Ewart, Taylor, Kraemer, & Agras (1991) | 43; P/C Married hypertensive patients and partners |
57.4 | 56 | MAT patient, spouse average (109.9) |
4 | Δ SBP, DBP (conflict discussion) |
SBP: −.34 DBP: −.14 |
SBP: .14 DBP: .16 |
0 | SBP: −0.40 DBP: 0.009 |
| Fehm-Wolfsdorf, Groth, Kaiser, & Halweg (1999) | 160; H, C Germany |
38.6 | 50 | Behavior: Groups based on positive and negative behaviors (KPI) |
3.5 | Δ HR, SBP, DBP (conflict discussion) |
HR, SBP, DBP: −.05 |
HR, SBP, DBP: .08 |
6 | HR, SBP, DBP: 0.11 |
| Gottman & Levenson (1992) | 158; C | 30.4 | 50 | Behavior: Groups based on positive and negative behaviors (RCISS) |
4 | Average IBI (before and during conflict discussion) |
HR: −.14 | .08 | 2 | HR: −0.29 |
| Kiecolt-Glaser, Malarkey, Chee, et al. (1993) a | 180; H, C | 25.7 | 50 | Behavior: Negative (MICS) |
3 | Δ HR, SBP, DBP (conflict discussion) |
HR: −.06 SBP: −.16 DBP: −.26 |
HR: .08 SBP, DBP: .07 |
1 | HR, SBP, DBP: 0.10 |
| Levenson & Gottman (1983) | 60; C | nr | 50 | MAT (111.7) & Locke- Williamson |
4 | Average IBI (conflict discussion) |
HR: −.22 | .13 | 0 | 0.20 |
| Levenson, Carstensen, & Gottman (1994) | 312; H, C Older adult couples |
53.4 | 50 | Affect: Positive & negative (SPAFF) |
0.5 | Average IBI (events, conflict, pleasant topic discussions) |
HR: −.04 | .06 | 0 | HR: −0.03 |
| G. E. Miller, Dopp, Myers et al. (1999) | 82; H, C | 31.4 | 50 | Affect: Anger (SPAFF) |
2.5 | Δ HR, SBP, DBP |
HR: −.11 SBP: −.27, DBP: −.11 |
HR: .11 SBP: .10 DBP: .11 |
1 | HR: 0.00 SBP: 0.35 DBP: 0.00 |
| Menchaca & Dehle (2005 b | 64; C | 25 | 50 | DAS (112) | 4 | Δ HR | HR: .05 | .13 | 0 | −0.20 |
| Morell & Apple (1990) c | 24; H, C Married women |
46.5 | 100 | Marital Satisfaction Inventory – Global Distress |
4 | Δ HR, SBP | HR: .14 SBP: .14 |
HR: .21 | 0 | - |
| Newton & Sanford (2003) | 82; H, C | 33.1* | 50 | Behavior: Hostility/do minance (CIT) |
3 | Δ SBP, DBP | SBP: −.23 DBP: −.28 |
SBP, DBP: .11 |
2 | - |
| Smith, Uchino, Berg et al. (2009) | 600; H, C Older and middle- aged married couples |
54.4 | 50 | MAT (nr) | 4 | Δ HR | HR: −.15 | .04 | 1 | - |
Note. Studies are listed in alphabetical order by author. Sample size refers to total number of individuals (as opposed to couples). All study samples collected in the United States unless otherwise noted in the study description. Signs for all effect sizes were oriented to indicate that higher scores on marital quality were related to lower cardiovascular reactivity. For behavioral coding studies, the coding system is in described in parentheses. Sample means for the DAS and MAT are reported in parentheses. Greater interbeat interval (IBI) values indicate slower HR; accordingly, for studies that examined the direction of effect sizes was changed such that positive values indicate greater marital quality related to lower HR. Unless otherwise indicated, studies examining change in cardiovascular measures (denoted by the Δ symbol) computed change from baseline to during the discussion tasks. Gender differences were computed as women – men; thus, negative numbers indicate larger effects for women compared to men. For sample descriptions: C = community, dx = diagnosis, H = healthy, NR = nationally representative, P/C = patient/clinic sample + primary diagnosis of interest (if specified), R = random sampling. CIT = Checklist of Interpersonal Transactions; IBI = interbeat interval; KPI = Kategoriensystem für Partnerschaftliche Interaktion Interactional Coding System; MICS = Marital Interaction Coding System; RCISS = Rapid Couples Interaction Scoring System; SASB = Structural Analysis of Social Behavior; SPAFF = Specific Affect Coding System
Computed change from baseline to recordings after the discussion task.
Examined DAS scores as a dependent variable, with heart rate as the independent variable. However, similar to other studies in the table, the DAS was administered prior to cardiovascular data collection.
Computed change from baseline to during and after marital conflict discussion. Did not report adequate statistics to determine the direction of the non-significant effect. We estimated the non-significant effects as r = ∣.14∣, and conducted two separate meta-analyses with r = +.14 and r = −.14. The results did not differ between the two analyses.
Table 9.
Cortisol Response Studies
| Design, study | Sample characteristics | Marital quality | Dependent measures and effect sizes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| N; Description |
M age |
% women |
Measure | Validity rating |
Sample frequency |
rmin | SE r | Covariates | Gender d |
|
| Daily cortisol slopes | ||||||||||
| Adam & Gunnar (2001) | 70; C Mothers of toddlers |
34 | 100 | Satisfaction with partner relationship and support; and degree of stress from partner |
3 | 6x 2 days |
−.15 | .12 | 0 | - |
| Barnett, Steptoe, & Gareis (2005) | 105; C United Kingdom |
55 | 36.2 | Marital role quality – concerns |
3 | 5x 1 day |
−.26 | .09 | 6 | - |
| Ditzen, Hoppmann, & Klumb (2008) | 102; C Dual-earner couples Germany |
37 | 50 | Daily (6 days) duration of exchange of physical intimacy |
2 | 6x 6 days |
−.07 | .10 | 0 | - |
| Floyd & Riforgiate (2008) | 20; H,C | 40.3 | 50 | Affectionate Communication Scale |
2 | 4x 1 day |
−.12 | .24 | 0 | - |
| Saxbe, Repetti, & Nishina (2008) a | 60; C | 41 | 50 | MAT (111) | 4 | 4x 3 days |
−.30 | .12 | 5 | −0.37 |
| Vedhara, Tuinstra, Miles, et al. (2006) b | 144; H, P/C 85 breast cancer patients, 59 healthy controls Netherlands |
52.8 | 100 | Maudsley Marital Questionnaire |
3.5 | 8x 2 days |
patients .02 controls .31 |
patients .11 controls .12 |
0 | - |
| Cortisol reactivity to conflict discussions | ||||||||||
| Fehm-Wolfsdorf, Groth, Kaiser, & Hahlweg (1999) | 160; H, C Germany (KPI) |
38.6 | 50 | Behavior: Positive & negative groups |
3.5 | 5x | .16 | .08 | 6 | −0.20 |
| Kiecolt-Glaser, Glaser, Cacioppo, et al. (1997) | 62; H, C | 66.8 | 50 | Behavior: Negative escalation (MICS) |
3 | 5x | −.24 | .12 | 1 | - |
| Malarkey, Kiecolt-Glaser, Pearl, & Glaser (1994) | 180; H, C | 25.7 | 50 | Behavior: Negative (MICS) |
3 | 5x | −.05 | .08 | 4 | - |
| G. E. Miller, Dopp, Myers, et al. (1999) c | 82; H, C | 31.4 | 50 | Affect: Anger (SPAFF) |
2.5 | 2x | .07 | .11 | 1 | - |
Note. Studies are organized by cortisol metric (daily slopes or reactivity to conflict discussions) and are listed in alphabetical order by author. Sample size refers to total number of individuals (as opposed to couples). All study samples collected in the United States unless otherwise noted in the study description. For slopes, sampling frequency refers to the number of samples per day (e.g., 4x = 4 samples per day) and the number of sampling days. A positive coefficient indicates that greater marital quality is related to flatter slopes, and a negative coefficient indicates that greater marital quality is related to steeper slopes. For reactivity, all studies sampled cortisol at baseline and following discussions. Studies denoted with 5x obtained additional samples during the discussion. A positive coefficient indicates that greater marital quality is related to greater reactivity, and a negative coefficient indicates that greater marital quality is related to lower reactivity. Sample means for the DAS and MAT are reported in parentheses. Gender differences were computed as women – men; thus, negative numbers indicate larger effects for women compared to men. For sample descriptions: C = community, dx = diagnosis, H = healthy, NR = nationally representative, P/C = patient/clinic sample + primary diagnosis of interest (if specified), R = random sampling. EMA = ecological momentary assessment; KPI = Kategoriensystem für Partnerschaftliche Interaktion Interactional Coding System; MAT = Marital Adjustment Test; MICS = Marital Interaction Coding System; SPAFF = Specific Affect coding system.
While the direction of the d coefficient was negative, this reflects that the relationship between marital quality and cortisol slope was larger, and also negative for women (r = −.47) compared to men (r = −.12).
Reported separate effect sizes for women with breast cancer and healthy controls, and effect sizes were averaged together.
Cortisol measured in plasma; reflects biologically active and bound cortisol levels, compared to saliva, which reflects biologically active cortisol only.
Cardiovascular reactivity
Across studies, indicators of greater marital quality were related to lower cardiovascular reactivity during marital problem discussions as shown in the top portion of Figure 7, HR r = −.10, SBP r = −.18, DBP r = −.18. Notably, the degree of heterogeneity between studies was not statistically significant, likely due to the large within-study variances in many of the smaller studies. In addition, the low I2 values suggested that the observed variation between studies was likely spurious, and not due to systematic influences that might justify examining moderators. That said, we did examine the contribution of a theoretically and methodologically important feature across the studies, which was the modality of marital quality measurement (observed affect, observed behavior, or self-reported satisfaction). In these analyses, we averaged effect sizes within studies (e.g., if a study reported HR, SBP, and DBP, the effect sizes were averaged together). For marital quality measurement, the relationship between marital quality and reduced cardiovascular reactivity was significant for studies using self-report measures, k = 6, r = −.15, p < .001, and observed behavior measures, k = 5, r = −.15, p < .001, but not studies using observed affect measures, k = 3, r = −.08, p = .10. Finally, we found no evidence of bias for cardiovascular reactivity studies according to Egger’s test, and for individual cardiovascular measures between 20 – 40 studies with null effects would be necessary to bring the overall effect size to r = .00.
Figure 7.
Aggregated effects of marital quality on biological mediators across studies: Summary effect size, heterogeneity, and publication bias statistics, and forest plots. Diamonds indicate average effect size across cardiovascular reactivity measures. Squares indicate average effect sizes within an outcome category. Diamond and box height is proportional to estimate precision – taller shapes are more precise. Width of the diamonds and error bars represents the 95% confidence interval. Positive correlation coefficients indicate that greater marital quality is related to greater reactivity or flatter cortisol slope. For cardiovascular reactivity studies, not all 14 studies provided effect size estimates for HR, SBP, or DBP. HR = heart rate; SBP = systolic blood pressure; DBP = diastolic blood pressure.
Regarding gender differences, we extracted separate effect sizes estimates for men and women from 10 out of 14 studies, and used the same approach to testing differences in effect sizes between men and women described earlier in the paper. For HR, k = 8, d = −0.03, p = .64, SBP, k = 5, d = 0.13, p = .14, and DBP, k = 4, d = 0.08, p = .26, there were no significant gender differences in the relationship between marital quality and cardiovascular reactivity. Only three studies had p-values for the gender difference between men and women less than .20; two were in the direction of larger effects for women (Ewart et al., 1991; Gottman & Levenson, 1992), and one in the direction of larger effects for men (G. E. Miller et al., 1999).
HPA Axis function
As shown in the bottom portion of Figure 7, greater marital quality was not significantly related to cortisol slopes or reactivity. While there was significant heterogeneity across studies, the small number of studies precluded examining moderators. Only two studies provided adequate statistics on gender differences, showing that the relationship between marital quality and daily cortisol slope was larger for women compared to men (Saxbe et al., 2008), while the relationship between marital quality and cortisol responses to conflict was larger for men compared to women (Fehm-Wolfsdorf et al., 1999).
Discussion
Our meta-analysis of the links between marital quality and health aggregated findings from over 72,000 individuals across 126 published papers spanning a half-century of research, from samples obtained in Brazil, Canada, China, Finland, Germany, Hong Kong, Israel, Netherlands, Sweden, the United Kingdom, and the United States. Despite considerable heterogeneity across studies, we found that greater marital quality was related to better physical health, regardless of study design, marital quality measure, and publication year. Moreover, the consistent effects in longitudinal studies suggest that poor marital quality is a risk factor for poor health outcomes. In addition, we found clear evidence that greater marital quality was related to lower cardiovascular reactivity during marital conflict discussions. We did not find significant relationships between marital quality and HPA axis measures. Overall, our results should generalize to healthy individuals and individuals with chronic illness.
How “big” are these effects, and what is their practical importance?
Based on previously articulated conventions, the associations between marital quality and health endpoints were generally small in magnitude (less than r = .20; Ferguson, 2009a). In addition, some studies showed no effects of marital functioning on health, as indicated by small lower bound estimates of the 95% CI. At the same time, small effects may have considerable practical significance. Similar to health behaviors that occur on a daily basis, such as diet, exercise, and sedentary activity, the mechanisms that explain how marital functioning influences health (psychological, biological, and behavioral mediators) exert their effects on a daily basis. For example, the following effect sizes9, derived from meta-analytic reviews, are all considered small10 and have confidence intervals that border non-significance: Consumption of fruit and vegetables and risk of coronary heart disease, RR = 0.93, 95% CI [0.86, 1.00] (He, Nowson, Lucas, & MacGregor, 2007); exercise interventions for preventing declines in health-related quality of life, d = .11, r = .05 (Gillison, Skevington, Sato, Standage, & Evangelidou, 2009); and increased television viewing and risk for cardiovascular disease, RR = 1.15, 95% CI [1.06, 1.23] (Grøntved & Hu, 2011). Despite such small effect sizes, increasing consumption of fruits and vegetables and decreasing sedentary activity are considered important targets for improving public health (Katzmarzyk & Lee, 2012; United States Department of Health and Human Services, 2008; World Health Organization, 2004). Finally, besides operating on a daily basis in married couples, marital functioning shares an important feature with other health behaviors: The benefits of changing behavior may be conferred across multiple health outcomes over time.
The observed effect sizes were also small compared to associations between marital quality and mental health-related outcomes. In a meta-analysis of cross-sectional relationships between marital quality and depression and depressive symptoms (k = 26), the mean correlation was r = −.42 for women and r = −.37 for men (considered medium-size effects; Whisman, 2001). In addition, diagnosed depression was related to lower marital satisfaction, with large mean effect size ds ranging from 1.2 – 1.75 in cross-sectional studies (aggregated effect sizes were not available for longitudinal studies). In a meta-analysis of associations between marital quality and indicators of psychological well-being (which included depressive and/or anxiety symptoms, self-esteem, life satisfaction, happiness, other psychological symptoms), greater marital quality was related to greater psychological well-being with moderate effect sizes across cross-sectional, r = .37, k = 66, and longitudinal studies, r = .25, k = 27 (Proulx, Helms, & Buehler, 2007).
Thus, effect sizes for psychological well-being measures were larger than our observed effect sizes for subjective clinical endpoints (e.g., ranging from .15 - .17 for self-rated health). Self-rated health measures, despite being self-reported, reflect body sensations and symptoms that are related to disease pathology, and are clinically relevant in that they predict mortality after controlling for objective markers (Benyamini, 2011). Notably, effect sizes for subjective endpoints were similar in magnitude to surrogate and objective clinical endpoints, suggesting some convergence across health measures.
Overall, greater marital quality was associated with better subjective health ratings, including adherence, and better self-rated health and/or lower self-rated symptoms (excluding pain). Besides subjective outcomes, links between marital quality and health were strongest for objective clinical endpoints, including mortality, cardiovascular disease-related outcomes, ulcer incidence, and wound healing. For mortality, relationships were largest in studies of patients with chronic illnesses, particularly cardiovascular diseases and end-stage renal disease. Significant associations were also found between marital quality and structural markers of cardiovascular disease. Importantly, the association between marital quality and health held even after accounting for covariates. Studies with smaller samples showed a trend towards larger effects compared to studies with larger samples, and effect sizes held even after removing extremely large samples. In addition, effect sizes were statistically significant and retained their magnitude in both patient samples and more heterogeneous samples.
What outcomes were not related to marital quality?
Notably, self-reported functional impairment, including disruptions to self-care tasks and other activities of daily living, were not systematically related to marital quality. However, most studies included samples where the vast majority of participants were middle-aged and most likely highly functional. While a small number of studies contributed to a lack of significant effects for glucose control and weight, three studies found significant relationships between poor marital quality and metabolic syndrome, which includes a cluster of surrogate markers besides glucose control and weight (Troxel et al., 2005; Whisman & Uebelacker, 2012; Whisman, Uebelacker, & Settles, 2010). As we discuss later, marital quality was not related to cortisol slopes or laboratory reactivity. Finally, marital quality was not significantly related to pain severity, but was related to functional impairment in patients with chronic pain, confirming the conclusions in a previous narrative review on marital functioning and pain (Leonard et al., 2006). That review recommended that future research on marital functioning and pain severity should focus on longitudinal studies and pain-specific marital factors (which were related to pain severity in their review), particularly spouse responses to patients’ pain (Leonard & Cano, 2006).
Limitations of the meta-analysis
A notable limitation of our review was significant but unexplained heterogeneity. The I2 statistics suggested that most of the heterogeneity was “true” heterogeneity rather than noise, but our moderator variables were not significantly related to the observed heterogeneity. Much of the variability was likely due to observational designs, differences in study populations and measures, and unexamined moderators. We initially planned on including other sociodemographic variables and factors related to the marriage as potential moderators. Unfortunately, as we discuss later, the wide age range within studies limited our ability to use age as a moderator. In addition, numerous factors related to the marital quality, particularly marital duration, ethnicity, and SES were not consistently reported (if at all) across studies.
An additional limitation was that we excluded studies examining reverse causality, in which poor health contributes to poor marital quality. The vast majority of studies addressing that question were case-control designs comparing marital quality between patients with vs. without illness. Such designs provided no information about pre-illness marital functioning, which is key to understanding whether marital quality declines when health worsens. Studies in our meta-analysis that found significant associations between marital quality and health after controlling for baseline status all involved cardiovascular disease surrogate markers (Baker et al., 2000; Gallo et al., 2003) and clinical endpoints (Helgeson, 1991). Several studies did not find an association between marital quality and health outcomes after controlling for baseline health status (Appelberg et al., 1996; Hibbard & Pope, 1993; Prigerson, Maciejewski, & Rosenheck, 1997; Trief et al., 2002; Trief et al., 2006). However, as most studies did not test models with and without the inclusion of baseline status, we could not determine whether including baseline status weakened associations between health outcomes and marital quality, or whether such associations did not initially exist. For example, in one study, relationship satisfaction at baseline was not associated with baseline or change in glycemic control (Trief et al., 2006).
Theoretical implications
Conceptualizing health
We distinguished among surrogate, subjective clinical, and objective clinical endpoints. While these distinctions were not related to effect size magnitude, they provided a useful framework for classifying studies and refining theories of how marital quality impacts health. By distinguishing surrogate endpoints from other biomarkers, we could ascertain whether marital quality was associated with biological measures that are specific indicators of a disease process, such as atherosclerosis (e.g., Gallo, Troxel, Kuller, et al., 2003).
Mediating mechanisms
Although this meta-analysis provided evidence for links between marital quality and a variety of health outcomes, the specific mechanisms that may explain these links were rarely tested.
Social-cognitive/affective processes and marital distress-related psychopathology: Focusing on depression
Social-cognitive and affective processes, such as attributions or emotional expression, are potential mediators, but were not tested as such in the included studies. Instead, most papers examined measures of negative affect or depression as covariates or independent predictors. Among the 13 studies that included depressive symptoms or negative affectivity, two surrogate outcome studies demonstrated that the association between marital quality and health outcomes remained statistically significant after controlling for negative affect or depressive symptoms (Barnett, Steptoe, Gareis, 2005; Whisman, Uebelacker, & Settles, 2010). Other studies noted that depressive symptoms/negative affect and marital quality were independent predictors of sleep disturbance (Troxel et al., 2009), self-rated health (Molloy et al., 2008; Rohrbaugh et al., 2008), and heart failure symptoms (Rohrbaugh et al., 2008). In some cases, marital quality was a stronger predictor of these outcomes compared to distress (Helgeson, 1991; King & Reis, 2012; Meana et al., 1998; Rohrbaugh et al., 2008), while distress was a stronger predictor in other studies (Troxel et al., 2009). Two papers examined depression as a potential moderator, and found a combination of high depressive symptoms and poor marital quality were related to poorer health outcomes (Sullivan, Katon, Russo, Dobie, & Sakai, 1994; Yang & Schuler, 2009). Finally, depression was a partial mediator for self-reported physical health (Weiss & Aved, 1978), but did not mediate functional impairment (Choi & Marks, 2008). Instead, functional impairment mediated the relationship between marital conflict and later depressive symptoms (Choi & Marks, 2008).
Taken together, the relationship between marital quality and health outcomes remained even after controlling for depressive symptoms or negative affect. While these findings suggest that depression may not mediate the relationship between marital quality and health, they were based on a relatively small number of studies relative to the overall literature. Moreover, some studies suggested that the presence of marital dissatisfaction and depression could potentiate adverse physical health outcomes. Studies were mixed on whether depression/negative affect was an independent predictor of physical health and whether depression/negative affect mediated the relationship between marital quality and physical health. The discrepant results may be due in part to design (cross-sectional vs. longitudinal samples, variability in follow-up intervals) and measurement differences for both health outcomes and negative affect across studies.
Examining daily mood and accompanying social-cognitive and affective processes, rather than single occasion assessments of symptoms (with varying timeframes across studies) might help achieve some clarity. In daily diary studies, daily mood fluctuates along with perceived changes in relationship quality (Gable, Reis, & Downey, 2003), and members within a couple covary in mood across the day (Saxbe & Repetti, 2010). Given the known links between daily negative affect and poorer health (S. Cohen et al., 1995; Leventhal, Hansell, Diefenbach, Leventhal, & Glass, 1996; Marsland, Cohen, Rabin, & Manuck, 2001) and daily positive affect and better health (Steptoe, Gibson, Hamer, & Wardle, 2007), daily experienced affect, and contributing cognitive and affective processes are strong candidates as a mediating mechanisms.
Finally, the relationship between marital quality and physical health may not be due to specific features of depression but more broad categories of internalizing disorders. Given high comorbidity among psychological disorders, some have proposed and tested models that classify psychopathology into internalizing (anxious/fear and misery) and externalizing disorders rather than models that focus on specific Axis I diagnoses (e.g., Krueger, 1999). Thus, future research should consider a dimensional perspective on how broad classes of psychopathology may impact the relationship between poor marital quality and adverse physical health outcomes.
Health behaviors
Several mechanisms may explain how marital functioning influences health behaviors, including modeling, social control, stress-buffering, and effects on personal resources like self-efficacy or self regulation (DiMatteo, 2004; Lewis & Butterfield, 1997; Lewis & Rook, 1999). While this review could not directly address the role of these pathways, in the small number of studies (k = 12) that accounted for the potential relationship between marital quality and health behaviors (by treating health behaviors as covariates), eight reported significant associations between marital quality and health outcomes (Baker et al., 1999; Baker et al., 2000; Homish et al., 2010; King & Reis, 2012; Levenstein et al., 1995; Medalie et al., 1992; Tobe et al., 2005; Whisman et al., 2010). Four studies showed no significant associations between marital quality and health after controlling for health behaviors (Baker et al. 1998; Eaker, et al., 2007; Tobe et al., 2007; Trief et al., 2006).
In a stronger test of health behaviors as a potential confound or mediator, among the few studies that ran both unadjusted models and models that controlled for health behaviors, including health behaviors as a covariate slightly weakened (Levenstein et al., 1995; Whisman, Uebelacker, & Settles, 2010) or strengthened the association between marital quality and health (Medalie et al., 1992). None directly tested health behaviors as a mediator, and only one study (Trief et al., 2006) reported the association between marital quality and health behaviors, and found no correlation between smoking and marital satisfaction. Finally, most studies found that compared to health behaviors, marital quality was a stronger predictor of health outcomes. In the statistical models, 5 of 7 studies reported a stronger association for marital quality than for smoking, 3 of 5 for drinking, 1 of 1 for caffeine and for not eating breakfast, and 1 of 3 for exercise. However, the small number of studies accounting for health behaviors strongly suggests the need for including health behaviors as covariates, and particularly as mediators, in future research. More importantly, similar to research on marital functioning and pain, rather than focusing on documenting associations between marital quality and health behaviors, work in this area should focus on the specific pathways that may explain how marital functioning may influence attempts to initiate, change, and maintain health behaviors, such as social control.
In line with a previous meta-analysis on social support and medication adherence (DiMatteo, 2002), in a small number of studies we found a relationship between marital quality and adherence to medical recommendations. For example, in a study we could not include in the meta-analysis, greater marital quality predicted better self-reported adherence with diabetes self-care recommendations (Trief, Ploutz-Snyder, Britton, & Weinstock, 2004). Notably, two out of five studies used objective indicators of adherence (electronic reports from CPAP device, Baron et al., 2009; attendance at dialysis sessions, Kimmel et al., 2000). Nonadherence is a major problem, with estimates for medication adherence ranging from between 30 – 80%, with a mean of 50% (see Osterberg & Blaschke, 2005 for a review). Thus, documenting the role of marital functioning, particularly with respect to social control, buffering or exacerbating stress, and influences on personal resources like self-regulation, in adherence to medical recommendations is a promising avenue for future basic and couple-based intervention research.
Health behaviors that married couples frequently participate in together, such as eating and sleeping, are also promising directions for future research. Marriage is a natural context to study how psychological stress and diet work additively and interactively to influence health, through effects on eating behavior and biological mediators like inflammation (Kiecolt-Glaser, 2010). Moreover, marital discord is associated with unhealthy dieting behaviors in wives (Markey, Markey, & Birch, 2001). Besides eating together, most couples sleep together (61% in a 2005 National Sleep Foundation poll; National Sleep Foundation, 2005). Poor marital quality is correlated with poor sleep (Baron et al., 2009; Troxel et al., 2009), and sleep problems themselves are related to poorer marital quality (Troxel, Robles, Hall, & Buysse, 2007). Marital functioning may also influence sleep through the effects of shared stressful life events, particularly transitions to parenthood and chronic illness in the family.
Biological mediators
We found clear evidence that lower marital quality was related to greater cardiovascular reactivity to marital conflict. Such relationships were primarily found with self-reported marital quality and observed behavior. Future work may benefit from “unpacking” the sympathetic and parasympathetic nervous system contributions to cardiovascular reactivity (Smith et al., 2011). Interestingly, across studies there were no significant gender differences in the relationship between marital quality and cardiovascular reactivity, which runs counter to prevailing theoretical accounts (Kiecolt-Glaser & Newton, 2001; Gottman & Levenson, 1988). That said, of the three studies that found significant gender differences, two were in the direction of larger effects for women (Ewart et al., 1991; Gottman & Levenson, 1992), and one in the direction of larger effects for men (G. E. Miller et al., 1999). We discuss the issue of gender differences in further detail when addressing moderators.
Surprisingly, marital quality was not significantly related to daily cortisol slopes or cortisol reactivity. The findings for daily slopes were surprising, given that in several studies less satisfied couples showed flatter diurnal cortisol slopes during the day (Saxbe et al., 2008), lower waking cortisol levels (Floyd & Riforgiate, 2008; Saxbe et al., 2008), and higher total daily cortisol levels (Ditzen et al., 2008; cf. Vedhara et al., 2006). Most of the included studies sampled cortisol over 1 – 2 days, and more than 3 days may be needed to establish reliable slope estimates (Saxbe, 2008), suggesting a need for more sampling days in future work. Regarding cortisol reactivity, most studies focused exclusively on observed negative behaviors and emotions. However, other types of behaviors may interact with negative behaviors to predict HPA axis responses to conflict discussions. In two cortisol reactivity papers we could not include in the meta-analysis, a higher probability of husband’s withdrawal following wife’s negative behavior was associated with elevated wives’ cortisol levels (Kiecolt-Glaser et al., 1996), and high levels of supportive behavior were related to adrenocorticotropic hormone and cortisol declines, particularly during highly negative interactions (Robles, Shaffer, Malarkey, & Kiecolt-Glaser, 2006). Finally, beyond HPA and SAM pathways, other research in couples suggests exploring additional biological mechanisms, particularly oxytocin- and vasopressin-mediated pathways (Gouin et al., 2010; Grewen, Girdler, Amico, & Light, 2005; Light, Grewen, & Amico, 2005).
One theme that emerged over the past decade of biobehavioral research on marriage was increased attention to the marital support portion of the model in Figure 1. Constructively engaging in the resolution of disagreements may promote adaptive physiological responses (Robles et al., 2006). Naturalistic studies showed that high marital quality may buffer work stress-related elevations in cortisol (Ditzen et al., 2008; Saxbe et al., 2008). Little is known about the specific elements of marital quality that may moderate the effects of psychological states on physiology, but one possibility is marital disclosure—the extent to which people open up to their spouses about their thoughts and feelings. For example, wives lower in marital disclosure showed greater cortisol increases in response to worries about work compared to wives reporting high marital disclosure (Slatcher, Robles, Repetti, & Fellows, 2010).
While these studies hint at possible biological mechanisms involved in the links between marital quality and health, almost no studies have examined the links between marital quality, biological mediators and health outcomes in true mediational analyses that take into account temporal precedence. As we describe later, assessing health outcomes that can be observed over short intervals of time, like days or months, will be vital in determining whether physiological changes related to marital functioning explain later health problems.
Moderators: For whom do these effects matter?
Our current empirical understanding of factors that modify the relationship between marital quality and health is quite limited. The most plausible moderators (gender, age) were treated as covariates, and potential moderators in existing theory or needing consideration in future theory (e.g., hostility, SES, marital duration) were inconsistently reported and rarely tested. However, even if moderators like relational interdependence or SES were reported in a majority of studies, the likely limited variability between studies makes meta-analysis less ideal for testing moderation. Instead, we strongly suggest that sufficiently powered studies routinely test the moderators discussed below.
Gender
For health outcome studies, our two tests of gender moderation yielded different results. Greater proportion of women included in studies was related to larger effect sizes. In studies that directly tested gender moderation (or provided separate effect sizes for men and women), the gender difference was small and not significant, though in the direction of greater magnitude for women. Thus, while the first analyses suggested gender moderation, we did not find overwhelming evidence for the presence of gender moderation across health outcomes. We did find small but significant gender moderation for surrogate endpoints related to cardiovascular disease based on a small number of studies (k = 6). In general, our analyses of direct tests of gender moderation were underpowered, as we could only draw from one-third of the available literature. Moreover, few studies directly compared husbands and wives within the same dyad (although in studies of patients with chronic illness, partners may not be concordant on conditions like chronic pain or cardiovascular disease). While our failure to detect overall gender differences in the relationship between marital quality and health endpoints may appear counter to previous narrative reviews (Kiecolt-Glaser & Newton, 2001; Wanic & Kulik, 2011a), those prior reviews made suggestive, but not strong claims about the empirical status of gender differences, marital quality, and health outcomes11. Moreover, both the interpersonal-orientation and subordinate-reactivity hypothesis focus on “the pathway from negative marital conflict behaviors to physiological functioning [italics added]” (Kiecolt-Glaser & Newton, 2001, p. 493). However, many researchers (ourselves included) have generalized both hypotheses to sex differences in the associations among marital quality, marital status, and health outcomes.
We found no significant gender differences in the relationship between marital quality and cardiovascular reactivity or cortisol responses, counter to prior reviews (Kiecolt-Glaser & Newton, 2001; Wanic & Kulik, 2011a). Methodological differences between our meta-analysis and prior narrative reviews account for much of the difference. Our focus on marital quality as an independent variable prevented us from examining effect sizes that compared gender differences in biological responses to marital conflict (e.g., Ewart et al., 1991). Moreover, studies showing gender differences examined catecholamine levels (Kiecolt-Glaser et al., 1997; Malarkey et al., 1994) and daily plasma cortisol levels (Kiecolt-Glaser, Newton, Cacioppo, et al. 1996) were not included due to a small number of studies examining those outcomes.
Across endpoint studies and our biological mediators of interest, the observed gender differences were small, with mean effect size ds ≤ .10. Future studies would need large sample sizes (> 1500 of each gender) to detect such effects and most studies were underpowered (only 1 in 10 had adequate sample sizes). Heterogeneity between couples in key contexts such as SES and stressful life events may also limit power. One way to overcome heterogeneity between couples in future studies is to conduct within-dyad analyses comparing wives and husbands, which minimizes between-couple variability, and is most feasible in laboratory studies or descriptive studies that collect data from both members of the couple. That said, a surprising number of laboratory studies conducted between-group comparisons (men vs. women, rather than husbands vs. wives within dyads), or did not conduct explicit statistical tests (i.e., separate analyses by gender, rather than a gender x marital quality interaction).
The small observed gender differences, the enormous sample size requirements needed to detect them, and the multiple potential contributing factors to both marital quality and health outcomes that can increase “noise” highlights the need for a different approach to gender in marital functioning and health research: Measuring gender-related moderators (Kiecolt-Glaser & Newton, 2001; Wanic & Kulik, 2011a). Focusing on self-representations, traits, roles, relative power, and related constructs provides continuous, dimensional variables that reflect existing individual differences, and affords greater statistical power (Preacher, Rucker, MacCallum, & Nicewander, 2005). Our approach focused on country/society-wide indices of gender inequality, and the limited number of countries and overrepresentation by the United States in the sample likely contributed to our null findings.
Thus far, the best examples for the utility of examining gender-related moderators come from studying biological mediators, although the studies described below examined gender-related factors as independent variables instead of moderators. Spouses characterized as less powerful in the relationship (reporting higher levels of dependent love relative to their spouse) showed elevated HPA axis activity (elevated adrenocorticotropic hormone) during marital conflict (Loving, Heffner, Kiecolt-Glaser, et al., 2004). In dual-earner couples, spouses who devoted more time to housework upon returning home at the end of the workday had higher evening cortisol levels regardless of gender, although as a group husbands spent more time on leisure compared to housework (Saxbe, Repetti, & Graesch, 2011). Moreover, greater time spent on housework relative to the other spouse was related to elevated cortisol levels (Klumb, Hoppmann, & Staats, 2006; Saxbe et al., 2011). Finally, the best example of the importance of gender-related moderators comes from marital conflict discussions demonstrating that cardiovascular reactivity was greater among spouses who are in the position of making requests or demands from their partner, regardless of gender (Denton, Burleson, Hobbs, Von Stein, & Rodriguez, 2001; Newton & Sanford, 2003). While the interpersonal-orientation and subordinate-reactivity hypotheses might predict that women are generally in the position of making demands or requests, a potentially parsimonious explanation is that cardiovascular reactivity depends on which partner tends to make the most demands or requests in the relationship. Overall, dimensional measures of gender-related moderators must be considered as part of a wide array of contexts and individual difference variables that may impact the relationship between marital quality and physical health.
Age and cohort
The relationship between marital quality and health outcomes did not systematically vary by publication year, suggesting that such links have remained consistent despite profound changes in the institution of marriage and in public health over the last half-century. At the same time, this finding does not preclude the possibility of age or cohort effects. Publication year may potentially serve as a proxy for cohort effects (e.g., Baby Boomers vs. Generation X), but the vast majority of studies contained individuals from multiple birth cohorts and age brackets. At the same time, the variability in mean sample age was fairly restricted (around 50 years of age, with a standard deviation between 9 – 12 years), limiting our ability to compare younger vs. older samples. In general, age was treated as a covariate rather than a potential moderator, even in large epidemiological studies.
A more relevant question for future research is when in the life-course does marital quality most impact physical health? Umberson and colleagues showed that marital quality impacted self-rated health more strongly in older individuals (Umberson & Williams, 2005; Umberson et al., 2006). Age may also interact with gender and gender-related factors. Umberson and Williams (2005) found that while the trajectory of marital quality was relatively stable across age ranges for women, men’s marital quality fluctuated across age. In terms of physiology, older couples showed smaller cardiac reactivity to conflict compared to middle-aged couples, but showed larger blood pressure responses during a task involving working together to solve a problem, with effects particularly pronounced among older men (Smith et al., 2009). In the 21st century, the highest proportion of married individuals will be older adults, due to longer life expectancy and population aging, increased age of first marriages, and growth in rates of remarriage (often unreported in the studies we reviewed) and marriage without the expectation of childbirth (Cherlin, 2010). Thus, future work should consistently test and report interactions between marital quality and age.
Individual differences
Beyond gender-related moderators and age, individual differences in personality, such as trait hostility or neuroticism, are potential moderating factors. Further, personality traits may have a direct effect on psychological processes and health behaviors, or moderate the relationship between these variables and biological mediators. For example, as summarized by Kiecolt-Glaser and Newton (2001), trait hostility predicts poorer health outcomes (T. Q. Miller, Smith, Turner, Guijarro, & Hallet, 1996; Smith, Glazer, Ruiz, & Gallo, 2004), and is also associated with greater marital conflict and less supportive interpersonal relationships, greater physiological reactivity to interpersonal stress, negative health behaviors such as smoking and alcohol use, and depressive symptoms in married couples.
Only one study in our meta-analysis included negative affectivity as a covariate in analyses (Molloy et al., 2008) and the authors did not report on the unadjusted correlations, so we could not determine the extent to which including negative affectivity strengthened or weakened the associations. Moreover, future research on individual differences in the context of marital relationships and health should consider reports from both partners. In the Utah Health and Aging Study, self-reports of hostility and antagonism were not related to coronary artery calcification; instead, spouse reports of hostility and antagonism were related to greater coronary artery calcification, particularly among older couples (Smith et al., 2007).
Future directions in studying moderators
Across the studies we reviewed, theoretically important variables like gender, age, and individual differences were treated as covariates rather than moderators. Thus, the key question for future marriage and health research will be: For whom is marital quality especially beneficial or detrimental? Such research would posit and test individual difference variables that can strengthen or attenuate connections between marital quality and physical health, allowing for more targeted prevention and interventions. Beyond individual differences, numerous factors are well-established predictors of declines in marital satisfaction or marital dissolution/divorce. Significant predictors of poor marital satisfaction include depression history (Davila, Karney, Hall, & Bradbury, 2003; Whisman, 2001), stressful events both inside and outside of the marital domain (Neff & Karney, 2009; Randall & Bodenmann, 2009), and parental divorce and conflict (Story, Karney, Lawrence, & Bradbury, 2004). Generally, psychopathology, parental conflict and poor quality interactions characterized by high amounts of negative affect and behaviors and low amounts of positive affect and behaviors also predict divorce, as do demographic variables like premarital births and teenage marriage (Amato & DeBoer, 2001), younger age at marriage (Amato & Hohmann-Marriott, 2007), and lower SES (Birditt, Brown, Orbuch, & McIlvane, 2010). These phenomena should be incorporated into future research on marital quality and health.
Same-sex marriage
Given the increased prevalence of same-sex marriage, sexual orientation is a moderator that should be considered in future marital quality and health research. Same-sex couples share many similarities with opposite-sex couples, including initial levels and later declines in relationship satisfaction, and argument topics and frequency (Kurdek, 1998, 2004b). Thus, we might expect that the association between marital quality and physical health outcomes will be similar for heterosexual and same-sex marriages. At the same time, same-sex couples are more likely to engage in effective problem-solving, and avoid demand/withdraw behavior compared to heterosexual couples (Kurdek, 2004a).
Moreover, there are several key differences between same-sex and heterosexual couples. Same-sex marriage is not legal in many states and countries, limiting the institutional protections granted by marriage and the barriers to relationship dissolution for same-sex couples (Kurdek, 1998). Same-sex couples are also more likely to experience discrimination as a result of their sexual orientation in ways that contribute to mental health problems and relationship quality and stability (Peplau & Fingerhut, 2007). Thus, understanding how the lack of access to legal protections, coupled with experiencing discrimination, impacts same-sex couples’ relationship satisfaction and subsequent mental and physical health outcomes is a key direction for future research. Finally, traditional gender roles or gender distinctions are not as applicable in same-sex couples; for example, distribution of household labor in same-sex couples is more equitable compared to heterosexual couples, and same-sex couples are less likely to assign domestic responsibilities based upon gender roles (Kurdek, 2005). As a result, same-sex couples afford a unique opportunity to examine the moderating role of gender-linked factors (e.g., interpersonal orientation and domestic roles) without confounds related to gender and biological sex.
Methodological implications
Marital quality measurement
Unexpectedly, ratings of the construct validity of marital quality measures were not related to effect size magnitude. Similar results were observed when comparing effect sizes between “standard” marital quality measures like the MAT or DAS and non-standard marital quality measures. Lower construct validity ratings were partially confounded with smaller sample size, but even in smaller samples, standard marital quality measures had similar effect sizes as non-standard measures. On one hand, using a gold-standard marital quality measure may not be critical, and perhaps most measures that approximate our definition of marital quality as a global evaluation of the relationship sufficiently captured that definition (Fincham & Bradbury, 1987). On the other hand, sufficiently powered studies may be able to observe effects using measures with low construct validity.
For future work, current gold standard measures may not be ideally suited for deployment in social epidemiology studies given their length, as well as lingering questions about measuring the construct of marital quality (Bradbury, Fincham, & Beach, 2000; Fincham & Beach, 2010). For instance, most standard measures do not adequately differentiate between positive and negative aspects of marital functioning (Fincham & Linfield, 1997). We recommend that future large epidemiological studies consider a more recently developed, but brief 4-item Couples Satisfaction Inventory that was developed empirically based on item analyses of the most commonly-used marital quality measures (Funk & Rogge, 2007). Beyond brevity, the measure has greater precision in detecting differences in satisfaction between and within couples. In addition, future studies should include measures that assess and separately score positive and negative aspects of relationship functioning, and consider both facets in statistical analyses (Fincham & Beach, 2010; Fincham & Linfield, 1997). Finally, a continual challenge is obtaining samples with sufficient numbers of distressed couples to provide a reasonable range of marital quality that allows improved generalizability (recommendations for improvements are described in Karney, Davila, Cohan, Sullivan, Johnson, & Bradbury, 1995). Studies reporting DAS and MAT scores in Table 2 - 4, 8, and 9 clearly shows that most samples included predominantly highly satisfied couples (one exception is patients with chronic illness, such as chronic pain).
Study design
Longitudinal studies offer stronger evidence for determining whether marital quality is a risk factor, and potentially a causal risk factor (Kraemer et al., 1997), for future health problems. Moreover, relationships develop and change over time and contexts, making longitudinal studies particularly informative in understanding marital functioning (Bradbury, Cohan, & Karney, 1998; Karney & Bradbury, 1995). The fact that cross-sectional and longitudinal studies generally showed similar effect sizes suggests that future cross-sectional studies on the basic association between marital quality and health will not provide significant incremental contributions to the literature. However, one area where cross-sectional studies can still make an important contribution is research focused on the moderating factors described in this paper, and health endpoints that have received little to no empirical attention.
At the same time, our analyses suggest that prospective, longitudinal designs show observable effects over relatively short spans of time, and that longer follow-up intervals are related to smaller effect sizes. While Figure 4 suggests that more studies are needed with longer follow-up intervals, focusing on short-term outcomes that can be observed over days, weeks, and months, rather than years and decades, may be a fruitful direction for the field. Examples from this meta-analysis are wound healing, adherence, and length of hospital stay. We further suggest incorporating short-term, ubiquitous, yet clinically relevant health outcomes in future research, such as upper respiratory infections (Repetti, Robles, & Reynolds, 2011).
Implications for practice and policy
Prevention and promoting healthy marriages
Public policy has generally focused on promoting marriage and improving marital relationships through enhancing effective communication, especially among low-income couples due to concerns about health disparities and the contributions of low SES to marital discord. For example, the Supporting Healthy Marriage Project, a recent randomized relationship education intervention among low-income couples, demonstrated higher levels of relationship satisfaction, lower psychological abuse from partners, enhanced positive communication and reduced negative behaviors during marital conversations compared to a control intervention at 12 months (Hseuh et al., 2012). The small effect sizes from the relationship intervention mirror those reported for health-promoting behavioral interventions like exercise (Gillison et al., 2009) and diet (Thomson & Ravia, 2011).
At the same time, some have suggested that interventions for low-income couples need to recognize that these individuals often place a higher priority on marriage, face a higher number of contextual stressors like chronic health problems, and experience especially challenging marital problems (i.e., substance use, infidelity) compared to middle-class counterparts (Conger & Elder, 1994; Fincham & Beach, 2010; Karney & Bradbury, 2005). For instance, low SES is related to lower marital quality and less supportive marital interactions (Conger, Conger, & Martin, 2010; Cutrona et al., 2003; Cutrona, Wallace, & Wesner, 2006). Therefore, marital interventions developed in middle- to high-income couples may fail to recognize the increased severity of contextual stressors experienced by lower-income couples. At the same time, combined with our broader point below about screening for marital difficulties in health care delivery, the health care setting may actually be an ideal environment for delivering marital interventions to low-income couples, particularly given high rates of chronic illness and poorer health outcomes in lower socioeconomic strata (Adler & Rehkpof, 2008).
Clinical intervention and assessment
A natural follow-up question is whether the relationship between marital distress and health outcomes can be lessened or reversed with intervention. Such work, particularly in randomized controlled trials of marital interventions, would more clearly establish whether marital functioning is a causal risk factor for poor health (Kraemer et al., 1997), and is a promising direction for future research. As mentioned in the Introduction, marital interventions are effective for treating depression and substance use. Couple-focused interventions are effective for reducing pain symptoms and improving quality of life in patients with chronic illness (see Martire, Schulz, Helgeson, Small, & Saghafi, 2010 for a review), and are being extended to other patient populations, such as breast cancer (Baucom et al., 2009). As we described above, couple-focused interventions may have benefits for adherence. Moreover, couples-based interventions may also have direct biological effects. For example, a recent single-arm study examining the effects of relationship education on cortisol found that participation in a couples’ education intervention was related to lower cortisol responses to a conflict discussion post-intervention compared to pre-intervention, an effect partially mediated by changes in relationship quality (Ditzen, Hahlweg, Fehm-Wolfsdorf, & Baucom, 2011). In addition, a brief 4-week intervention involving spouses practicing providing warm touch techniques reduced 24-hour systolic blood pressure among husbands compared to a control intervention (Holt-Lunstad, Birmingham, & Light, 2008).
The association between marital quality and health outcomes has broader implications for patient care in medical settings, particularly given relationships between marital quality and mortality in patients with cardiovascular and end-stage renal disease. Brief measures of marital functioning (Funk & Rogge, 2007; Whisman, Snyder, & Beach, 2009) could be considered as part of screening in primary care and specialty settings if empirical data justify their use. Fostering greater understanding and awareness in health care providers of the relational context in which health problems often occur may eventually increase the development and dissemination of couples-based interventions.
Conclusion
The last half-century of research clearly suggests that low marital quality is a correlate and risk factor for poor health, whether assessed subjectively through self-rated health, or objectively through surrogate endpoint biomarkers or clinical endpoints, with small effects that may have important public health significance. Thus far, no study has fulfilled the stringent criteria that establish marital functioning as a causal risk factor for poor health (Kraemer et al., 1997), although studies from the last decade show movement towards that lofty aim. Along with evaluating the health impact of couples-based prevention and interventions, our meta-analytic review indicates that the questions of how and for whom marital quality impacts health remain surprisingly unanswered after a half-century and should be the key questions driving research on close relationships and health in the 21st century.
Acknowledgments
This research was supported by William T. Grant Foundation Research Grant 9333 and National Institutes of Health grant R21 AG032494 to the first author, T32 MH015750 and R01 HL114097 to the second author, and F31 AG034718 to the fourth author. The work of the fourth author was also supported by resources from the Department of Veterans Affairs Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, and the VA Puget Sound Health Care System, Seattle, Washington.
We thank the paper authors who sent us additional statistics to allow us to compute effect sizes; Blair Ibarra, Emily Kelleher, Jennifer Linchey, and Meera Parbhakar for collecting citations; Julianne Holt-Lunstad and Annemarie Cano for supportive consultation; and graduate students and postdoctoral trainees in the UCLA Relationships and Health Laboratory and Tom Bradbury for comments on earlier drafts of this paper.
Footnotes
We explored a meta-analysis of marital quality and immunity (Kiecolt-Glaser et al., 1987; Kiecolt-Glaser et al., 1988; Kiecolt-Glaser et al., 1993; Kiecolt-Glaser et al., 1997; Kiecolt-Glaser et al., 2005; Miller, Dopp, Myers, Stevens, & Fahey, 1999; Zautra et al., 1998; Whisman & Sbarra, 2012). However, for each subtype of immune outcome (e.g., EBV antibody titers) there was an insufficient number of studies from independent samples available for analysis (for a narrative review, see Robles & Kane, 2012).
A small number of studies from the same research group made the catecholamine outcomes unsuitable for our meta-analysis. Interestingly, in newlywed couples, elevated catecholamine levels during a marital conflict discussion were related to marital dissolution (divorce/separation) and lower marital satisfaction in intact couples 10 years later (Kiecolt-Glaser, Bane, Glaser, & Malarkey, 2003).
Our stringent inclusion and exclusion criteria led to excluding studies that were included in prior narrative reviews. The primary reasons for excluding studies cited in prior reviews were no direct statistical test of the relationship between marital quality and health, inadequate statistics for such tests, independent variables that did not meet our criteria for the definition of marital quality, and insufficient number of studies with similar dependent variables.
One strategy to adjust for dependence among effect sizes within a study involves computing a correction factor that increases the sample size estimate to account for such dependency, which increases precision and reduces Type II error (Cheung & Chan, 2004, 2008). This adjustment typically increases the sample size estimate for a given study to somewhere between the original sample size and the original sample size multiplied by the number of effect sizes that are averaged together. For example, a study with n = 150 that provides three effect sizes would have an nadjusted ranging between 150 and 450. The approach generates less biased estimates of heterogeneity compared to other correction methods that underestimate heterogeneity, and the large increase in n decreases the standard errors for those effect size estimates.
When a study contributed an effect size estimate for more than one endpoint, such as blood pressure and self-rated health, we selected the estimate based on the hierarchy: Objective clinical > surrogate endpoint > subjective clinical. When two papers from the same sample contributed an effect size for different endpoints, we used the same hierarchy. When more than one effect size was available from the same paper within an endpoint category (e.g., reporting blood pressure and glycemic control), we averaged the effect sizes between outcomes within a study.
A funnel plot is plotted with precision (e.g., sample size, variance, or standard error) on the X-axis, and effect size on the Y-axis (Borenstein et al., 2009). Larger studies (small standard errors, more precision), appear towards the right side of the plot, and smaller studies (large standard errors, less precision) appear towards the left side of the plot. Because smaller studies have greater sampling error, the pattern of scatter resembles a funnel (widest on the left, narrowing from left to right). If publication bias is limited, sampling error should be randomly distributed across studies, and scatter should be symmetrical around the mean effect size. Publication bias is evident when the scatter is asymmetrical, trending in one direction (e.g., positive effect sizes trending towards the top of the plot).
One study reported effect sizes for two surrogate endpoints (blood pressure and HbA1c; Trief et al., 2006), and we averaged the effect sizes between the two markers for these analyses. Conducting analyses with just one of the markers did not significantly alter the pattern of results.
Studies with non-standard marital quality measures had larger samples compared to studies with standard marital quality measures, mean difference = 968.85, t(51.3) = 3.06, p = .004. After restricting analyses to sample sizes that were less than the sample size median of 161, there were no differences between studies with non-standard marital quality measures (k = 18) and studies using standard marital quality measures (k = 33), Q(1) = 1.24, p = .27.
Risk ratios cannot be converted to effect size r. Thus, rather than directly comparing r-values between studies, we chose an approach based on conventions for small effects for risk ratios, where values between 1.0 – 2.0 (when the direction of the effect is predicting increased risk) are considered small and less likely to have practical value.
Other meta-analyses have compared observed effect sizes with risk estimates in the medical literature (odds ratios, risk ratios, etc.) that are typically converted to r’s. For example, Rosnow and Rosenthal (2003) famously noted that the effect size of taking aspirin to prevent heart attacks was r = .03. Ferguson (2009b) recently noted that comparisons between effect sizes in observational psychological research and effects from medical epidemiology or intervention research are not appropriate and should be avoided because the small effect sizes obtained from medical intervention research often factor in “hypothesis irrelevant” participants (e.g., patients who never take aspirin and never have a heart attack) which deflates effect sizes, due to very large sample sizes and low base rate phenomena.
Regarding objective health outcomes (the equivalent of surrogate and objective clinical endpoints in this meta-analysis, “…some studies…suggested sex differences…whereas others did not” (Kiecolt-Glaser & Newton, 2001, p. 477). Regarding subjective clinical endpoints, “…some studies revealed gender parity in marriage-health linkages…, whereas two suggested stronger links for women…none provided stronger evidence for men” (Kiecolt-Glaser & Newton, 2001, p. 480).
Contributor Information
Theodore F. Robles, Department of Psychology, University of California, Los Angeles
Richard B. Slatcher, Department of Psychology, Wayne State University
Joseph M. Trombello, Department of Psychology, University of California, Los Angeles
Meghan M. McGinn, Mental Illness Research, Education, and Clinical Care (MIRECC), VA Puget Sound Healthcare System
References
* Denotes study included in meta-analysis.
- Adler NE, Rehkopf DH. U.S. disparities in health: Description, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- *Adam EK, Gunnar MR. Relationship functioning and home and work demands predict individual differences in diurnal cortisol patterns in women. Psychoneuroendocrinology. 2001;26:189–208. doi: 10.1016/s0306-4530(00)00045-7. doi: 10.1016/S0306-4530(00)00045-7.
- Amato PR, DeBoer DD. The transmission of marital instability across generations: Relationship skills or commitment to marriage? Journal of Marriage and Family. 2001;63:1038–1051. doi: 10.1111/j.1741-3737.2001.01038.x. [Google Scholar]
- Amato PR, Hohmann-Marriott B. A comparison of high- and low-distress marriages that end in divorce. Journal of Marriage and Family. 2007;69:621–638. doi: 10.1111/j.1741-3737.2007.00396.x. [Google Scholar]
- *Appelberg K, Romanov K, Heikkila K, Honkasaol ML, Koskenvuo M. Interpersonal conflict as a predictor of work disability: A follow-up study of 15,348 Finnish employees. Journal of Psychosomatic Research. 1996;40:157–167. doi: 10.1016/0022-3999(95)00576-5. doi: 10.1016/0022-3999(95)00576-5.
- *Ashmore JA, Emery CF, Hauck ER, MacIntyre NR. Marital adjustment among patients with chronic obstructive pulmonary disease who are participating in pulmonary rehabilitation. Heart & Lung. 2005;34:270–278. doi: 10.1016/j.hrtlng.2004.12.005. doi: 10.1016/j.hrtlng.2004.12.005.
- *Baker B, Helmers K, O’Kelly B, Sakinofsky I, Abelsohn A, Tobe S. Marital cohesion and ambulatory blood pressure in early hypertension. American Journal of Hypertension. 1999;12:227–230. doi: 10.1016/s0895-7061(98)00184-8. doi: 10.1016/S0895-7061(98)00184-8.
- *Baker B, O’Kelly B, Szalai JP, Katic M, McKessock D, Ogilvie R. Determinants of left ventricular mass in early hypertension. American Journal of Hypertension. 1998;11:1248–1251. doi: 10.1016/s0895-7061(98)00132-0. doi: 10.1016/S0895-7061(98)00132-0.
- *Baker B, Paquette M, Szalai JP, Driver H, Perger T, Helmers K. The influence of marital adjustment on 3-year left ventricular mass and ambulatory blood pressure in mild hypertension. Archives of Internal Medicine. 2000;160:3453–3458. doi: 10.1001/archinte.160.22.3453. doi: 10.1001/archinte.160.22.3453.
- *Barnett RC, Davidson H, Marshall NL. Physical symptoms and the interplay of work and family roles. Health Psychology. 1991;10:94–101. doi: 10.1037//0278-6133.10.2.94. doi: 10.1037/0278-6133.10.2.94.
- *Barnett RC, Marshall NL. Men, family-role quality, job-role quality, and physical health. Health Psychology. 1993;12:48–55. doi: 10.1037//0278-6133.12.1.48. doi: 10.1037/0278-6133.12.1.48.
- Barnett PA, Spence D, Manuck SB, Jennings JR. Psychological stress and the progression of carotid artery disease. Journal of Hypertension. 1997;15:49–55. doi: 10.1097/00004872-199715010-00004. doi: 10.1097/00004872-199715010-00004. [DOI] [PubMed] [Google Scholar]
- *Barnett RC, Steptoe A, Gareis KC. Marital-role quality and stress-related psychobiological indicators. Annals of Behavioral Medicine. 2005;30:36–43. doi: 10.1207/s15324796abm3001_5. doi: 10.1207/s15324796abm3001_5.
- *Baron KG, Smith TW, Czajkowski LA, Gunn HE, Jones CR. Relationship quality and CPAP adherence in patients with obstructive sleep apnea. Behavioral Sleep Medicine. 2009;7:22–36. doi: 10.1080/15402000802577751. doi: 10.1080/15402000802577751.
- *Basolo-Kunzer M, Diamond S, Maliszewski M, Weyermann L, Reed J. Chronic headache patients’ marital and family adjustment. Issues in Mental Health Nursing. 1991;12:133–148. doi: 10.3109/01612849109040509.
- Baucom DH, Porter LS, Kirby JS, Gremore TM, Wiesenthal N, Aldridge W, Keefe FJ. A couple-based intervention for female breast cancer. Psychooncology. 2009;18:276–283. doi: 10.1002/pon.1395. doi: 10.1002/pon.1395. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Fincham FD, Katz J. Marital therapy in the treatment of depression: Toward a third generation of therapy and research. Clinical Psychology Review. 1998;18:635–661. doi: 10.1016/s0272-7358(98)00023-3. doi: 10.1016/S0272-7358(98)00023-3. [DOI] [PubMed] [Google Scholar]
- Benazon NR, Coyne JC. Living with a depressed spouse. Journal of Family Psychology. 2000;14:71–79. doi: 10.1037/0893-3200.14.1.71. [PubMed] [Google Scholar]
- Benyamini Y. Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychology and Health. 2011;26:1407–1413. doi: 10.1080/08870446.2011.621703. doi: 10.1080/08870446.2011.621703. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. doi: 10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Biomarker Definitions Working Group Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clinical Pharmacology and Therapeutics. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- Birditt KS, Brown E, Orbuch TL, McIlvane JM. Marital conflict behaviors and implications for divorce over 16 years. Journal of Marriage and Family. 2010;72:1188–1204. doi: 10.1111/j.1741-3737.2010.00758.x. doi: 10.1111/j.1741-3737.2010.00758.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Black DR. Weight changes in a couples program: Negative association of marital adjustment. Journal of Behavioral Therapy and Experimental Psychiatry. 1988;19:103–111. doi: 10.1016/0005-7916(88)90023-7. doi: 10.1016/0005-7916(88)90023-7.
- *Block AR, Boyer SL. The spouse’s adjustment to chronic pain: cognitive and emotional factors. Social Science & Medicine. 1984;19:1313–1317. doi: 10.1016/0277-9536(84)90018-2. doi: 10.1016/0277-9536(84)90018-2.
- *Bookwala J. The role of marital quality in physical health during the mature years. Journal of Aging and Health. 2005;17:85–104. doi: 10.1177/0898264304272794. doi: 10.1177/0898264304272794.
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Wiley; West Sussex, United Kingdom: 2009. [Google Scholar]
- Bradbury TN, Beach SRH, Fincham FD, Nelson GM. Attributions and behavior in functional and dysfunctional marriages. Journal of Consulting and Clinical Psychology. 1996;64:569–576. doi: 10.1037//0022-006x.64.3.569. doi: 10.1037/0022-006X.64.3.569. [DOI] [PubMed] [Google Scholar]
- Bradbury TN, Cohan CL, Karney BR. Optimizing longitudinal research for understanding and preventing marital dysfunction. In: Bradbury TN, editor. The developmental course of marital dysfunction. Cambridge University Press; New York: 1998. pp. 279–311. [Google Scholar]
- Bradbury TN, Fincham FD, Beach SRH. Research on the nature and determinants of marital satisfaction: A decade in review. Journal of Marriage and Family. 2000;62:964–980. doi: 10.1111/j.1741-3737.2000.00964.x. [Google Scholar]
- Brines J, Joyner K. The ties that bind: Principles of cohesion in cohabitation and marriage. American Sociological Review. 1999;3:333–355. doi: 10.2307/2657490. [Google Scholar]
- *Brown MA. Marital discord during pregnancy: A family systems approach. Family Systems Medicine. 1994;12:221–234. doi: 10.1037/h0089130.
- *Brown PC, Smith TW. Social influence, marriage, and the heart: Cardiovascular consequences of interpersonal control in husbands and wives. Health Psychology. 1992;11:88–96. doi: 10.1037//0278-6133.11.2.88. doi: 10.1037/0278-6133.11.2.88.
- Burman B, Margolin G. Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin. 1992;112:39–63. doi: 10.1037/0033-2909.112.1.39. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- *Cano A, Gillis M, Heinz W, Geisser M, Foran H. Marital functioning, chronic pain, and psychological distress. Pain. 2004;107:99–106. doi: 10.1016/j.pain.2003.10.003. doi: 10.1016/j.pain.2003.10.003.
- *Cano A, Weisberg JN, Gallagher RM. Marital satisfaction and pain severity mediate the association between negative spouse responses to pain and depressive symptoms in a chronic pain patient sample. Pain Medicine. 2000;1:35–43. doi: 10.1046/j.1526-4637.2000.99100.x. doi: 10.1046/j.1526-4637.2000.99100.x.
- *Carels RA, Sherwood A, Szczepanski R, Blumenthal JA. Ambulatory blood pressure and marital distress in employed women. Behavioral Medicine. 2000;26:80–85. doi: 10.1080/08964280009595755. doi: 10.1080/08964280009595755.
- *Carels RA, Szczepanski R, Blumenthal JA, Sherwood A. Blood pressure reactivity and marital distress in employed women. Psychosomatic Medicine. 1998;60:639–643. doi: 10.1097/00006842-199809000-00022.
- Carr D, Springer KW. Advances in families and health research in the 21st century. Journal of Marriage and Family. 2010;72:743–761. doi: 10.1111/j.0022-2445.2004.00088.x. [Google Scholar]
- *Carrere S, Yoshimoto D, Mittmann A, Woodin EM, Tabares A, Ullman J, Hawkins M. The roles of marriage and anger dysregulation in biobehavioral stress responses. Biological Research for Nursing. 2005;7:30–43. doi: 10.1177/1099800405275657. doi: 10.1177/1099800405275657.
- Cherlin AJ. The deinstitutionalization of American marriage. Journal of Marriage and Family. 2004;66:848–861. doi: 10.1111/j.0022-2445.2004.00058.x. [Google Scholar]
- Cherlin AJ. Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and Family. 2010;72:403–419. doi: 10.1111/j.1741-3737.2010.00710.x. doi: 10.1111/j.1741-3737.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung SF, Chan DKS. Dependent effect sizes in meta-analysis: Incorporating the degree of interdependence. Journal of Applied Psychology. 2004;89:780–791. doi: 10.1037/0021-9010.89.5.780. doi: 10.1037/0021-9010.89.5.780. [DOI] [PubMed] [Google Scholar]
- Cheung SF, Chan DKS. Dependent correlations in meta-analysis: The case of heterogeneous dependence. Educational and Psychological Measurement. 2008;68:760–777. doi: 10.1177/0013164408315263. [Google Scholar]
- *Choi H, Marks NF. Marital conflict, depressive symptoms, and functional impairment. Journal of Marriage and Family. 2008;70:377–390. doi: 10.1111/j.1741-3737.2008.00488.x. doi: 10.1111/j.1741-3737.2008.00488.x.
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Lawrence Erlbaum Associates Inc; Hillsdale, NJ: 1983. [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Fireman P, Gwaltney JM, Newsom JT. State and trait negative affect as predictors of objective and subjective symptoms of respiratory viral infections. Journal of Personality and Social Psychology. 1995;68:159–169. doi: 10.1037//0022-3514.68.1.159. doi: 10.1037/0022-3514.68.1.159. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [PubMed] [Google Scholar]
- Cohn JN, Quyyumi AA, Hollenberg NK, Jamerson KA. Surrogate markers for cardiovascular disease: Functional markers. Circulation. 2004;109:31–46. doi: 10.1161/01.CIR.0000133442.99186.39. doi: 10.1161/01.cir.0000133442.99186.39. [DOI] [PubMed] [Google Scholar]
- Comprehensive Meta-Analysis (Version 2) [Computer software] Biostat; Englewood, NJ: [Google Scholar]
- Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. Journal of Marriage and Family. 2010;72:685–704. doi: 10.1111/j.1741-3737.2010.00725.x. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Elder GH. Families in troubled times: Adapting to change in rural America. Aldine Transaction; New York: 1994. [Google Scholar]
- Cordova JV, Gee CB, Warren LZ. Emotional skillfulness in marriage: Intimacy as a mediator of the relationship between emotional skillfulness and marital satisfaction. Journal of Social and Clinical Psychology. 2005;24:218–235. doi: 10.1521/jscp.24.2.218.62270. [Google Scholar]
- *Coughlin PC. Premenstrual syndrome: How marital satisfaction and role choice affect symptom severity. Social Work. 1990;35:351–355.
- Coyne JC. Toward an interactional description of depression. Psychiatry. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- *Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA. Prognostic importance of marital quality for survival of congestive heart failure. American Journal of Cardiology. 2001;88:526–529. doi: 10.1016/s0002-9149(01)01731-3. doi: 10.1016/S0002-9149(01)01731-3.
- Cross SE, Madson L. Models of the self: Self-construals and gender. Psychological Bulletin. 1997;122:5–37. doi: 10.1037/0033-2909.122.1.5. doi: 10.1037/0033-2909.122.1.5. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Abraham WT, Gardner KA, Melby JN, Bryant C, Conger RD. Neighborhood context and financial strain as predictors of marital interaction and marital quality in African American couples. Personal Relationships. 2003;10:389–409. doi: 10.1111/1475-6811.00056. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Wallace G, Wesner KA. Neighborhood characteristics and depression. Current Directions in Psychological Science. 2006;16:188–192. doi: 10.1111/j.1467-8721.2006.00433.x. doi: 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley SE, Hammen C, Davila J, Burge D. Axis II symptomatology, depression, and life stress during the transition from adolescence to adulthood. Journal of Consulting and Clinical Psychology. 1998;66:595–603. doi: 10.1037//0022-006x.66.4.595. doi: 10.1037/0022-006X.66.4.595. [DOI] [PubMed] [Google Scholar]
- Davila J, Karney BR, Hall TW, Bradbury TN. Depressive symptoms and marital satisfaction: Within-subject associations and the moderating effects of gender and neuroticism. Journal of Family Psychology. 2003;17:557–570. doi: 10.1037/0893-3200.17.4.557. doi: 10.1037/0893-3200.17.4.557. [DOI] [PubMed] [Google Scholar]
- Denton WH, Burleson BR, Hobbs BV, Von Stein M, Rodriguez CP. Cardiovascular reactivity and initiate/avoid patterns of marital communication: A test of Gottman’s psychophysiologic model of marital interaction. Journal of Behavioral Medicine. 2001;24:401–421. doi: 10.1023/a:1012278209577. doi: 10.1023/A:1012278209577. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Ditzen B, Hahlweg K, Fehm-Wolfsdorf G, Baucom D. Assisting couples to develop healthy relationships: Effects of couples relationship education on cortisol. Psychoneuroendocrinology. 2011;36:597–607. doi: 10.1016/j.psyneuen.2010.07.019. doi: 10.1016/j.psyneuen.2010.07.019. [DOI] [PubMed] [Google Scholar]
- *Ditzen B, Hoppmann C, Klumb P. Positive couple interactions and daily cortisol: On the stress-protecting role of intimacy. Psychosomatic Medicine. 2008;70:883–889. doi: 10.1097/PSY.0b013e318185c4fc. doi: 10.1097/PSY.0b013e318185c4fc.
- *Dunn SA, Lewis SL, Bonner PN, Meize-Grochowski R. Quality of life for spouses of CAPD patients. ANNA J. 1994;21:237–246.
- Durtschi JA, Fincham FD, Cui M, Lorenz FO, Conger RD. Dyadic processes in early marriage: Attributions, behavior, and marital quality. Family Relations. 2011;60:421–434. doi: 10.1111/j.1741-3729.2011.00655.x. doi: 10.1111/j.1741-3729.2011.00655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Eaker ED, Sullivan LM, Kelley-Hayes M, D’Agostino RB, Sr., Benjamin EJ. Marital status, marital strain, and risk of coronary heart disease or total mortality: The Framingham Offspring Study. Psychosomatic Medicine. 2007;69:509–513. doi: 10.1097/PSY.0b013e3180f62357. doi: 10.1097/PSY.0b013e3180f62357.
- *Ewart CK, Taylor CB, Kraemer HC, Agras WS. High blood pressure and marital discord: Not being nasty matters more than being nice. Health Psychology. 1991;10:155–163. doi: 10.1037//0278-6133.10.3.155. doi: 10.1037/0278-6133.10.3.155.
- *Fehm-Wolfsdorf G, Groth T, Kaiser A, Hahlweg K. Cortisol responses to marital conflict depend on marital interaction quality. International Journal of Behavioral Medicine. 1999;6:207–227. doi: 10.1207/s15327558ijbm0603_1. doi: 10.1207/s15327558ijbm0603_1.
- Ferguson CJ. An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice. 2009a;40:532–538. doi: 10.1037/a0015808. [Google Scholar]
- Ferguson CJ. Is psychological research really as good as medical research? Effect size comparisons between psychology and medicine. Review of General Psychology. 2009b;13:130–136. doi: 10.1037/a0015103. [Google Scholar]
- Fincham FD, Beach SRH. Conflict in marriage: Implications for working with couples. Annual Review of Psychology. 1999;50:47–77. doi: 10.1146/annurev.psych.50.1.47. doi: 10.1146/annurev.psych.50.1.47. [DOI] [PubMed] [Google Scholar]
- Fincham FD, Beach SRH. Marriage in the new millennium: A decade in review. Journal of Marriage and Family. 2010;72:630–649. doi: 10.1111/j.1741-3737.2010.00722.x. [Google Scholar]
- Fincham FD, Beach SRH, Kemp-Fincham SI. Marital quality: A new theoretical perspective. In: Sternberg RJ, Hojjat M, editors. Satisfaction in close relationships. Guilford Press; New York, NY: 1997. pp. 275–304. [Google Scholar]
- Fincham FD, Bradbury TN. The assessment of marital quality: A reevaluation. Journal of Marriage and Family. 1987;49:797–809. doi: 10.2307/351973. [Google Scholar]
- Fincham FD, Linfield KJ. A new look at marital quality: Can spouses feel positive and negative about their marriage? Journal of Family Psychology. 1997;11:489–502. doi: 10.1037/0893-3200.11.4.489-502. [Google Scholar]
- *Fink SL, Skipper JK, Jr., Hallenbeck PN. Physical disability and problems in marriage. Journal of Marriage and Family. 1968;30:64–73. doi: 10.2307/350223.
- *Fisher L, Chesla CA, Chun KM, Skaff MM, Mullan JT, Kanter RA. Patient-appraised couple emotion management and disease management among Chinese American patients with type 2 diabetes. Journal of Family Psychology. 2004;18:302–310. doi: 10.1037/0893-3200.18.2.302. doi: 10.1037/0893-3200.18.2.302.
- *Fitzpatrick TR. The quality of dyadic relationships, leisure activities and health among older women. Health Care for Women International. 2009;30:1073–1092. doi: 10.1080/07399330903199367. doi: 10.1080/07399330903199367.
- *Floyd K, Riforgiate S. Affectionate communication received from spouses predicts stress hormone levels in healthy adults. Communication Monographs. 2008;75:351–368. doi: 10.1080/03637750802512371.
- Frattaroli J. Experimental disclosure and its moderators: A meta-analysis. Psychological Bulletin. 2006;132:823–865. doi: 10.1037/0033-2909.132.6.823. doi: 10.1037/0033-2909.132.6.823. [DOI] [PubMed] [Google Scholar]
- Funk JL, Rogge RD. Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology. 2007;21:572–583. doi: 10.1037/0893-3200.21.4.572. doi: 10.1037/0893-3200.21.4.572. [DOI] [PubMed] [Google Scholar]
- Gable SL, Reis HT, Downey G. He said, she said: A quasi-signal detection analysis of daily interactions between close relationship partners. Psychological Science. 2003;14:100–105. doi: 10.1111/1467-9280.t01-1-01426. doi: 10.1111/1467-9280.t01-1-01426. [DOI] [PubMed] [Google Scholar]
- *Gallo LC, Troxel WM, Kuller LH, Sutton-Tyrrell K, Edmundowicz D, Matthews KA. Marital status, marital quality, and atherosclerotic burden in postmenopausal women. Psychosomatic Medicine. 2003;65:952–962. doi: 10.1097/01.psy.0000097350.95305.fe. doi: 10.1097/01.Psy.0000097350.95305.
- Gallo LC, Troxel WM, Matthews KA, Kuller LH. Marital status and quality in middle-aged women: Associations with levels and trajectories of cardiovascular risk factors. Health Psychology. 2003;22:453–463. doi: 10.1037/0278-6133.22.5.453. doi: 10.1037/0278-6133.22.5.453. [DOI] [PubMed] [Google Scholar]
- Gerin W, Goyal TM, Mostofsky E, Shimbo D. The measurement of blood pressure in cardiovascular research. In: Luecken LJ, Gallo LC, editors. Handbook of physiological research methods in health psychology. Sage Publications; Thousand Oaks, CA: 2008. pp. 115–131. [Google Scholar]
- Gillison FB, Skevington SM, Sato A, Standage M, Evangelidou S. The effects of exercise interventions on quality of life in clinical and healthy populations: A meta-analysis. Social Science & Medicine. 2009;68:1700–1710. doi: 10.1016/j.socscimed.2009.02.028. doi: 10.1016/j.socscimed.2009.02.028. [DOI] [PubMed] [Google Scholar]
- *Goodwin SS. The marital relationship and health in women with chronic fatigue and immune dysfunction syndrome: Views of wives and husbands. Nursing Research. 1997;46:138–146. doi: 10.1097/00006199-199705000-00004. doi: 10.1097/00006199-199705000-00004.
- Gotlib IH, Joormann J. Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Levenson RW. The social psychophysiology of marriage. In: Noller P, Fitzpatrick MA, editors. Perspectives on marital interaction. Multilingual Matters; Clevedon, England: 1988. pp. 182–200. [Google Scholar]
- *Gottman JM, Levenson RW. Marital processes predictive of later dissolution - Behavior, physiology, and health. Journal of Personality and Social Psychology. 1992;63:221–233. doi: 10.1037//0022-3514.63.2.221. doi: 10.1037/0022-3514.63.2.221.
- Gottman JM, Krokoff LJ. Marital interaction and satisfaction: A longitudinal view. Journal of Consulting and Clinical Psychology. 1989;57:47–52. doi: 10.1037//0022-006x.57.1.47. doi: 10.1037/0022-006X.57.1.47. [DOI] [PubMed] [Google Scholar]
- Gouin JP, Carter CS, Pournajafi-Nazarloo H, Glaser R, Malarkey WB, Loving TJ, Stowell JR, Kiecolt-Glaser JK. Marital behavior, oxytocin, vasopressin, and wound healing. Psychoneuroendocrinology. 2010;35:1082–1090. doi: 10.1016/j.psyneuen.2010.01.009. doi: 10.1016/j.psyneuen.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Greene SM, Griffin WA. Symptom study in context: Effects of marital quality on signs of Parkinson’s disease during patient–spouse interaction. Psychiatry: Interpersonal and Biological Processes. 1998;61:35–45. doi: 10.1080/00332747.1998.11024817.
- Grewen KM, Girdler SS, Amico J, Light KC. Effects of partner support on resting oxytocin, cortisol, norepinephrine, and blood pressure before and after warm partner contact. Psychosomatic Medicine. 2005;67:531–538. doi: 10.1097/01.psy.0000170341.88395.47. doi: 10.1097/01.psy.0000170341.88395.47. [DOI] [PubMed] [Google Scholar]
- *Grewen KM, Girdler SS, Light KC. Relationship quality: Effects on ambulatory blood pressure and negative affect in a biracial sample of men and women. Blood Pressure Monitoring. 2005;10:117–124. doi: 10.1097/00126097-200506000-00002. doi: 10.1097/00126097-200506000-00002.
- Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality. JAMA: The Journal of the American Medical Association. 2011;305:2448–2455. doi: 10.1001/jama.2011.812. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Guyll M, Cutrona C, Burzette R, Russell D. Hostility, relationship quality, and health among African-American couples. Journal of Consulting and Clinical Psychology. 2010;78:646–654. doi: 10.1037/a0020436. doi: 10.1037/a0020436.
- *Hafner RJ, Rogers J, Watts JM. Psychological status before and after gastric restriction as predictors of weight loss in the morbidly obese. Journal of Psychosomatic Research. 1990;34:295–302. doi: 10.1016/0022-3999(90)90085-i. doi: 10.1016/0022-3999(90)90085-I.
- Hahlweg K. Development and validity of a new system to analyze interpersonal communication (KPI) In: Hahlweg K, Jacobson NS, editors. Marital interaction: Analysis and modification. Guilford press; New York: 1984. pp. 182–198. [Google Scholar]
- *Hamilton M, Pond DA, Ryle A. Relation of C.M.I. responses to some social and psychological factors. Journal of Psychosomatic Research. 1962;6:157–165. doi: 10.1016/0022-3999(62)90002-8. doi: 10.1016/0022-3999(62)90002-8.
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Interpersonal dysfunction in depressed women: Impairments independent of depressive symptoms. Journal of Affective Disorders. 2002;72:145–156. doi: 10.1016/s0165-0327(01)00455-4. doi: 10.1016/S0165-0327(01)00455-4. [DOI] [PubMed] [Google Scholar]
- Hammen CL, Shih JH. Stress generation and depression. In: Dobson KS, Dozois DJA, editors. Risk Factors in Depression. Elsevier; London: 2008. pp. 409–428. [Google Scholar]
- *Hawkins DN, Booth A. Unhappily ever after: Effects of long-term, low-quality marriages on well-being. Social Forces. 2005;84:451–471. doi: 10.1353/sof.2005.0103.
- *Haynes SG, Feinleib M, Kannel WB. The relationship of psychosocial factors to coronary heart disease in the Framingham study: III. Eight-year incidence of coronary heart disease. American Journal of Epidemiology. 1980;111:37–58. doi: 10.1093/oxfordjournals.aje.a112873.
- He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: Meta-analysis of cohort studies. Journal of Human Hypertension. 2007;21:717–728. doi: 10.1038/sj.jhh.1002212. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Wu J, Witkiewitz K, Epstein DH, Preston KL. Marriage and relationship closeness as predictors of cocaine and heroin use. Addictive Behaviors. 2009;34:258–263. doi: 10.1016/j.addbeh.2008.10.020. doi: 10.1037/0033-2909.118.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Helgeson VS. The effects of masculinity and social support on recovery from myocardial-infarction. Psychosomatic Medicine. 1991;53:621–633. doi: 10.1097/00006842-199111000-00004.
- Heuveline P, Timberlake JM. The role of cohabitation in family formation: The United States in comparative perspective. Journal of Marriage and Family. 2004;66:1214–1230. doi: 10.1111/j.0022-2445.2004.00088.x. doi: 10.1111/j.0022-2445.2004.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman RE. Observation of couple conflicts: Clinical assessment applications, stubborn truths, and shaky foundations. Psychological Assessment. 2001;13:5–35. doi: 10.1037//1040-3590.13.1.5. doi: 10.1037/1040-3590.13.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman RE, Weiss RL, Eddy JM. Marital Interaction Coding System: Revision and empirical evaluation. Behaviour Research and Therapy. 1995;33:737–746. doi: 10.1016/0005-7967(95)00003-g. doi: 10.1016/0005-7967(95)00003-G. [DOI] [PubMed] [Google Scholar]
- *Hibbard JH, Pope CR. The quality of social roles as predictors of morbidity and mortality. Social Science & Medicine. 1993;36:217–225. doi: 10.1016/0277-9536(93)90005-o. doi: 10.1016/0277-9536(93)90005-O.
- Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. 2011 Retrieved from www.cochrane-handbook.org.
- *Hodgson JH, Shields CG, Rousseau SL. Disengaging communication in later-life couples coping with breast cancer. Families, Systems Health. 2003;21:145–163. doi: 10.1037/1091-7527.21.2.145.
- *Holt-Lunstad J, Birmingham W, Jones BQ. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Annals of Behavioral Medicine. 2008;35:239–244. doi: 10.1007/s12160-008-9018-y. doi: 10.1007/s12160-008-9018-y.
- Holt-Lunstad J, Birmingham WA, Light KC. Influence of a “warm touch” support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosomatic Medicine. 2008;70:976–985. doi: 10.1097/PSY.0b013e318187aef7. doi: 10.1097/PSY.0b013e318187aef7. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homish GG, Leonard KE. Spousal influence on general health behaviors in a community sample. American Journal of Health Behavior. 2008;32:754–763. doi: 10.5555/ajhb.2008.32.6.754. doi: 10.5993/AJHB.32.6.19. [DOI] [PubMed] [Google Scholar]
- *Homish GG, Leonard KE, Cornelius JR. Individual, partner and relationship factors associated with non-medical use of prescription drugs. Addiction. 2010;105:1457–1465. doi: 10.1111/j.1360-0443.2010.02986.x. doi: 10.1111/j.1360-0443.2010.02986.x.
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hseuh JA, Alderson DP, Lundquist E, Michalopoulos C, Gubits D, Fein D, Knox V. The Supporting Healthy Marriage evaluation: Early impacts on low-income families. Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; Washington, DC: 2012. OPRE Report 2012-11. [Google Scholar]
- *Janicki DL, Kamarck TW, Shiffman S, Sutton-Tyrrell K, Gwaltney CJ. Frequency of spousal interaction and 3-year progression of carotid artery intima medial thickness: The Pittsburgh Healthy Heart Project. Psychosomatic Medicine. 2005;67:889–896. doi: 10.1097/01.psy.0000188476.87869.88. doi: 10.1097/01.psy.0000188476.87869.88.
- Janicki-Deverts D, Kamarck TW. Ambulatory blood pressure monitoring. In: Luecken LJ, Gallo LC, editors. Handbook of physiological research methods in health psychology. Sage Publications; Thousand Oaks, CA: 2008. pp. 159–182. [Google Scholar]
- Karney BR, Bradbury TN. The longitudinal course of marital quality and stability: A review of theory, method, and research. Psychological Bulletin. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- Karney BR, Bradbury TN. Contextual influences on marriage: Implications for policy and intervention. Current Directions in Psychological Science. 2005;14:171–174. doi: 10.1111/j.0963-7214.2005.00358.x. [Google Scholar]
- Karney BR, Davila J, Cohan CL, Sullivan KT, Johnson MD, Bradbury TN. An empirical investigation of sampling strategies in marital research. Journal of Marriage and Family. 1995;57:909–920. doi: 10.2307/353411. [Google Scholar]
- *Kasle S, Wilhelm MS, Zautra AJ. Rheumatoid arthritis patients’ perceptions of mutuality in conversations with spouses/partners and their links with psychological and physical health. Arthritis & Rheumatism-Arthritis Care & Research. 2008;59:921–928. doi: 10.1002/art.23821. doi: Doi 10.1002/Art.23821.
- Katzmarzyk PT, Lee I. Sedentary behaviour and life expectancy in the USA: A cause-deleted life table analysis. BMJ Open. 2012;2:e000828. doi: 10.1136/bmjopen-2012-000828. doi: 10.1136/bmjopen-2012-000828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kerns RD, Finn P, Haythornthwaite J. Self-monitored pain intensity: psychometric properties and clinical utility. Journal of Behavioral Medicine. 1988;11:71–82. doi: 10.1007/BF00846170. doi: 10.1007/BF00846170.
- *Kerns RD, Haythornthwaite J, Southwick S, Giller EL. The role of marital interaction in chronic pain and depressive symptom severity. Journal of Psychosomatic Research. 1990;34:401–408. doi: 10.1016/0022-3999(90)90063-a. doi: 10.1016/0022-3999(90)90063-a.
- *Kerns RD, Turk DC. Depression and chronic pain: The mediating role of the spouse. Journal of Marriage and Family. 1984;46:845–852. doi: 10.2307/352532.
- Kiecolt-Glaser JK. Stress, food, and inflammation: Psychoneuroimmunology and nutrition at the cutting edge. Psychosomatic Medicine. 2010;72:365–369. doi: 10.1097/PSY.0b013e3181dbf489. doi: 10.1097/PSY.0b013e3181dbf489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Bane C, Glaser R, Malarkey WB. Love, marriage, and divorce: Newlyweds’ stress hormones foreshadow relationships changes. Journal of Consulting and Clinical Psychology. 2003;71:176–188. doi: 10.1037//0022-006x.71.1.176. doi: 10.1037/0022-006X.71.1.176. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Cacioppo JT, Malarkey WB, Glaser R. Acute psychological stressors and short-term immune changes: What, why, for whom, and to what extent? Psychosomatic Medicine. 1992;54:680–685. doi: 10.1097/00006842-199211000-00008. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Fisher LD, Ogrocki P, Stout JC, Speicher CE, Glaser R. Marital quality, marital disruption, and immune function. Psychosomatic Medicine. 1987;49:13–34. doi: 10.1097/00006842-198701000-00002. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Glaser R, Cacioppo JT, MacCallum RC, Snydersmith M, Kim C, Malarkey WB. Marital conflict in older adults: Endocrinological and immunological correlates. Psychosomatic Medicine. 1997;59:339–349. doi: 10.1097/00006842-199707000-00001.
- Kiecolt-Glaser JK, Kennedy S, Malkoff S, Fischer L, Speicher CE, Glaser R. Marital discord and immunity in males. Psychosomatic Medicine. 1988;50:213–229. doi: 10.1097/00006842-198805000-00001. [DOI] [PubMed] [Google Scholar]
- *Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, Glaser R. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry. 2005;62:1377–1384. doi: 10.1001/archpsyc.62.12.1377. doi: 10.1001/archpsyc.62.12.1377.
- *Kiecolt-Glaser JK, Malarkey WB, Chee M, Newton T, Cacioppo JT, Mao H, Glaser R. Negative behavior during marital conflict is associated with immunological down-regulation. Psychosomatic Medicine. 1993;55:395–409. doi: 10.1097/00006842-199309000-00001.
- Kiecolt-Glaser JK, McGuire LM, Robles TF, Glaser R. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton T. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton T, Cacioppo JT, MacCallum RC, Glaser R, Malarkey WB. Marital conflict and endocrine function: Are men really more physiologically affected than women? Journal of Consulting and Clinical Psychology. 1996;64:324–332. doi: 10.1037//0022-006x.64.2.324. doi: 10.1037/0022-006X.64.2.324. [DOI] [PubMed] [Google Scholar]
- *Kimmel PL, Peterson RA, Weihs KL, Shidler N, Simmens SJ, Alleyne S, Phillips TM. Dyadic relationship conflict, gender, and mortality in urban hemodialysis patients. Journal of the American Society of Nephrology. 2000;11:1518–1525. doi: 10.1681/ASN.V1181518.
- *King KB, Reis HT. Marriage and long-term survival after coronary artery bypass grafting. Health Psychology. 2012;31:55–62. doi: 10.1037/a0025061. doi: 10.1037/a0025061.
- Klumb P, Hoppmann C, Staats M. Work hours affect spouse’s cortisol secretion--for better and for worse. Psychosomatic Medicine. 2006;68:742–746. doi: 10.1097/01.psy.0000233231.55482.ff. doi: 10.1097/01.psy.0000233231.55482.ff. [DOI] [PubMed] [Google Scholar]
- *Knoll N, Burkert S, Rosemeier HP, Roigas J, Gralla O. Predictors of spouses’ provided support for patients receiving laparoscopic radical prostatectomy peri-surgery. Psycho-Oncology. 2007;16:312–319. doi: 10.1002/pon.1061. doi: 10.1002/pon.1061.
- *Ko KJ, Berg CA, Butner J, Uchino BN, Smith TW. Profiles of successful aging in middle-aged and older adult married couples. Psychology and Aging. 2007;22:705–718. doi: 10.1037/0882-7974.22.4.705. doi: 10.1037/0892-7974.22.4.705.
- *Kool MB, Woertman L, Prins MA, Van Middendorp H, Geenen R. Low relationship satisfaction and high partner involvement predict sexual problems of women with fibromyalgia. Journal of Sex & Marital Therapy. 2006;32:409–423. doi: 10.1080/00926230600835403. doi: 10.1080/00926230600835403.
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;57:921–926. doi: 10.1001/archpsyc.56.10.921. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- *Kudel I, Edwards R, Raja S, Haythornthwaite J, Heinberg LJ. The association of perceived partner-related social support with self-reported outcomes in women post-mastectomy. Journal of Health Psychology. 2008;13:1030–1039. doi: 10.1177/1359105308097968. doi: 10.1177/1359105308097968.
- *Kulik JA, Mahler HIM. Marital quality predicts hospital stay following coronary artery bypass surgery for women but not men. Social Science & Medicine. 2006;63:2031–2040. doi: 10.1016/j.socscimed.2006.05.022. doi: 10.1016/j.socscimed.2006.05.022.
- Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: Findings from the Whitehall II Study. Journal of Clinical Endocrinology & Metabolism. 2011;96:1478–1485. doi: 10.1210/jc.2010-2137. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurdek LA. Relationship outcomes and their predictors: Longitudinal evidence from heterosexual married, gay cohabitating, and lesbian cohabitating couples. Journal of Marriage and Family. 1998;60:553–568. doi: 10.2307/353528. [Google Scholar]
- Kurdek LA. Are gay and lesbian cohabitating couples really different from heterosexual couples? Journal of Marriage and Family. 2004a:880–900. doi: 10.1111/j.0022-2445.2004.00060.x. [Google Scholar]
- Kurdek LA. Gay men and lesbians: The family context. In: Coleman M, Ganong LH, editors. Handbook of contemporary families: Considering the past, contemplating the future. Sage; Thousand Oaks, CA: 2004b. pp. 96–115. [Google Scholar]
- Kurdek LA. What do we know about gay and lesbian couples? Current Directions in Psychological Science. 2005;15:251–254. doi: 10.1111/j.0963-7214.2005.00375.x. [Google Scholar]
- *Kurpius SER, Nicpon MF, Maresh SE. Mood, marriage, and menopause. Journal of Counseling Psychology. 2001;48:77–84. doi: 10.1037/0022-0167.48.1.77.
- Laurenceau JP, Barrett LF, Rovine MJ. The interpersonal process model of intimacy in marriage: A daily-diary and multilevel modeling approach. Journal of Family Psychology. 2005;19:314–323. doi: 10.1037/0893-3200.19.2.314. doi: 10.1037/0893-3200.19.2.314. [DOI] [PubMed] [Google Scholar]
- Laurent HK, Powers SI. Social-cognitive predictors of hypothalamic-pituitary-adrenal reactivity to interpersonal conflict in emerging adult couples. Journal of Social and Personal Relationships. 2006;23:703–730. doi: 10.1177/0265407506065991. [Google Scholar]
- Lazarus RS. From psychological stress to the emotions: A history of changing outlooks. Annual Review of Psychology. 1993;44:1–22. doi: 10.1146/annurev.ps.44.020193.000245. doi: 10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- Lee GR, Payne KK. Changing marriage patterns since 1970: What’s going on, and why? Journal of Comparative Family Studies. 2010;41:537–555. [Google Scholar]
- Leonard MT, Cano A. Pain affects spouses too: Personal experience with pain and catastrophizing as correlates of spouse distress. Pain. 2006;126:139–146. doi: 10.1016/j.pain.2006.06.022. doi: 10/1016/j.pain.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: A review and integration of theoretical models and empirical evidence. Journal of Pain. 2006;7:377–390. doi: 10.1016/j.jpain.2006.01.442. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Leong LEM, Cano A, Johansen AB. Sequential and base rate analysis of emotional validation and invalidation in chronic pain couples: Patient gender matters. The Journal of Pain. 2011;12:1140–1148. doi: 10.1016/j.jpain.2011.04.004. doi: 10.1016/j.jpain.2011.04.004.
- *Levenson RW, Carstensen LL, Gottman JM. Long-term marriage - age, gender, and satisfaction. Psychology and Aging. 1993;8:301–313. doi: 10.1037//0882-7974.8.2.301. doi: 10.1037/0882-7974.8.2.301.
- *Levenson RW, Carstensen LL, Gottman JM. The influence of age and gender on affect, physiology, and their interrelations - a study of long-term marriages. Journal of Personality and Social Psychology. 1994;67:56–68. doi: 10.1037//0022-3514.67.1.56. doi: 10.1037//0022-3514.67.1.56.
- *Levenson RW, Gottman JM. Marital interaction: physiological linkage and affective exchange. Journal of Personality and Social Psychology. 1983;45:587–597. doi: 10.1037//0022-3514.45.3.587. doi: 10.1037/0022-3514.45.3.587.
- *Levenstein S, Kaplan GA, Smith M. Sociodemographic characteristics, life stressors, and peptic-ulcer - a prospective-study. Journal of Clinical Gastroenterology. 1995;21:185–192. doi: 10.1097/00004836-199510000-00004. doi: 10.1097/00004836-199510000-00004.
- Leventhal EA, Hansell S, Diefenbach M, Leventhal H, Glass DC. Negative affect and self-report of physical symptoms: Two longitudinal studies of older adults. Health Psychology. 1996;15:193–199. doi: 10.1037//0278-6133.15.3.193. doi: 10.1037/0278-6133.15.3.193. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Butterfield RM. Social control in marital relationships: Effect of one’s partner on health behaviors. Journal of Applied Social Psychology. 2007;37:298–319. doi: 10.1111/j.0021-9029.2007.00161.x. [Google Scholar]
- Lewis MA, Rook KS. Social control in personal relationships: Impact on health behaviors and psychological distress. Health Psychology. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. doi: 10.1037/0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- Light KC, Grewen KM, Amico JA. More frequent partner hugs and higher oxytocin levels are linked to lower blood pressure and heart rate in premenopausal women. Biological Psychology. 2005;69:5–21. doi: 10.1016/j.biopsycho.2004.11.002. doi: 10.1097/01.PSY.0000046076.93591.AD. [DOI] [PubMed] [Google Scholar]
- Linden W, Gerin W, Davidson K. Cardiovascular reactivity: Status quo and a research agenda for the new millennium. Psychosomatic Medicine. 2003;65:5–8. doi: 10.1097/01.psy.0000046076.93591.ad. doi: 10.1097/01.PSY.0000046076.93591.AD. [DOI] [PubMed] [Google Scholar]
- Liu H, Reczek C. Cohabitation and U.S. adult mortality: An examination by gender and race. Journal of Marriage and Family. 2012;74:794–811. doi: 10.1111/j.1741-3737.2012.00983.x. [Google Scholar]
- Liu H, Umberson DJ. The times they are a changin’: Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior. 2008;49:239–253. doi: 10.1177/002214650804900301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke HJ, Wallace KM. Short marital adjustment and prediction tests: Their reliability and validity. Marriage and Family Living. 1959;21:251–255. doi: 10.2307/348022. [Google Scholar]
- Loving TJ, Heffner KL, Kiecolt-Glaser JK, Glaser R, Malarkey WB. Stress hormone changes and marital conflict: Spouses’ relative power makes a difference. Journal of Marriage and Family. 2003;66:595–612. doi: 10.1111/j.0022-2445.2004.00040.x. [Google Scholar]
- *Malarkey WB, Kiecolt-Glaser JK, Pearl D, Glaser R. Hostile behavior during marital conflict alters pituitary and adrenal hormones. Psychosomatic Medicine. 1994;56:41–51. doi: 10.1097/00006842-199401000-00006.
- *Mancini AD, Bonanno GA. Marital closeness, functional disability, and adjustment in late life. Psychology and Aging. 2006;21:600–610. doi: 10.1037/0882-7974.21.3.600. doi: 10.1037/0882-7974.21.3.600.
- Mancini GBJ, Dahlof B, Diez J. Surrogate markers for cardiovascular disease: Structural markers. Circulation. 2004;109:IV22–30. doi: 10.1161/01.CIR.0000133443.77237.2f. doi: 0.1161/01.CIR.0000133443.77237.2f. [DOI] [PubMed] [Google Scholar]
- Manolio T. Novel risk markers and clinical practice. New England Journal of Medicine. 2003;349:1587–1589. doi: 10.1056/NEJMp038136. doi: 10.1056/NEJMp038136. [DOI] [PubMed] [Google Scholar]
- *Marcenes WS, Sheiham A. The relationship between work stress and oral health-status. Social Science & Medicine. 1992;35:1511–1520. doi: 10.1016/0277-9536(92)90054-t. doi: 10.1016/0277-9536(92)90054-T.
- *Marcenes WS, Sheiham A. The relationship between marital quality and oral health status. Psychology & Health. 1996;11:357–369. doi: 10.1080/08870449608400264.
- Markey CN, Markey PM, Birch LL. Interpersonal predictors of dieting practices among married couples. Journal of Family Psychology. 2001;15:464–475. doi: 10.1037//0893-3200.15.3.464. doi: 10.1037/0893-3200.15.3.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsland AL, Cohen S, Rabin BS, Manuck SB. Associations between stress, trait negative affect, acute immune reactivity, and antibody response to hepatitis B injection in healthy young adults. Health Psychology. 2001;20:4–11. doi: 10.1037/0278-6133.20.1.4. [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Masheb RM, Brondolo E, Kerns RD. A multidimensional, case-control study of women with self-identified chronic vulvar pain. Pain Medicine. 2002;3:253–259. doi: 10.1046/j.1526-4637.2002.02032.x. doi: 10.1046/j.1526-4637.2002.02032.x.
- Matthews KA, Schwartz J, Cohen S, Seeman T. Diurnal cortisol decline is related to coronary calcification: CARDIA study. Psychosomatic Medicine. 2006;68:657–661. doi: 10.1097/01.psy.0000244071.42939.0e. doi: 10.1097/01.psy.0000244071.42939.0e. [DOI] [PubMed] [Google Scholar]
- *Matthews RA, Del Priore RE, Acitelli LK, Barnes-Farrell JL. Work-to-relationship conflict: Crossover effects in dual-earner couples. Journal of Occupational Health Psychology. 2006;11:228–240. doi: 10.1037/1076-8998.11.3.228. doi: 10.1037/1076-8998.11.3.228.
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;388:171–179. doi: 10.1056/NEJM199801153380307. doi: 0.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- *Meana M, Binik I, Khalife S, Cohen D. Affect and marital adjustment in women’s rating of dyspareunic pain. Canadian Journal of Psychiatry. 1998;43:381–385. doi: 10.1177/070674379804300406.
- *Medalie JH, Snyder M, Groen JJ, Neufeld HN, Goldbourt U, Riss E. Angina pectoris among 10,000 men. 5 year incidence and univariate analysis. American Journal of Medicine. 1973;55:583–594. doi: 10.1016/0002-9343(73)90179-4. doi: 10.1016/0002-9343(73)90179-4.
- *Medalie JH, Stange KC, Zyzanski SJ, Goldbourt U. The importance of biopsychosocial factors in the development of duodenal ulcer in a cohort of middle-aged men. American Journal of Epidemiology. 1992;136:1280–1287. doi: 10.1093/oxfordjournals.aje.a116436.
- Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams textbook of endocrinology. 12th ed Saunders; Philadelphia, PA: 2011. [Google Scholar]
- *Menchaca D, Dehle C. Marital quality and physiological arousal: How do I love thee? Let my heartbeat count the ways. American Journal of Family Therapy. 2005;33:117–130. doi: Doi 10.1080/01926180590915897.
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science and Medicine. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Cole SW. Health psychology: Developing biologically plausible models linking the social world and physical health. Annual Review of Psychology. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- *Miller GE, Dopp JM, Myers HF, Stevens SY, Fahey JL. Psychosocial predictors of natural killer cell mobilization during marital conflict. Health Psychology. 1999;18:262–271. doi: 10.1037//0278-6133.18.3.262. doi: 10.1037/0278-6133.18.3.262.
- Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. Meta-analytic review of research on hostility and physical health. Psychological Bulletin. 1996;119:322–348. doi: 10.1037/0033-2909.119.2.322. doi: 10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- Mirgain SA, Cordova JV. Emotion skills and marital health: The association between observed and self-reported emotion skills, intimacy, and marital satisfaction. Journal of Social and Clinical Psychology. 2007;26:983–1009. doi: 10.1521/jscp.2007.26.9.983. [Google Scholar]
- *Molloy GJ, Perkins-Porras L, Strike PC, Steptoe A. Social networks and partner stress as predictors of adherence to medication, rehabilitation attendance, and quality of life following acute coronary syndrome. Health Psychology. 2008;27:52–58. doi: 10.1037/0278-6133.27.1.52. doi: 10.1037/0278-6133.27.1.52.
- *Morell MA, Apple RF. Affect expression, marital satisfaction, and stress reactivity among premenopausal women during a conflictual marital discussion. Psychology of Women Quarterly. 1990;14:387–402. doi: 10.1111/j.1471-6402.1990.tb00027.x.
- National Sleep Foundation 2005 Sleep in America poll. 2005 Mar; from http://www.sleepfoundation.org/sites/default/files/2005_summary_of_findings.pdf.
- Neff LA, Karney BR. Stress and reactivity to daily relationship experiences: How stress hinders adaptive processes in marriage. Journal of Personality and Social Psychology. 2009;97:435–450. doi: 10.1037/a0015663. doi: 10.1037/a0015663. [DOI] [PubMed] [Google Scholar]
- *Newton TL, Sanford JM. Conflict structure moderates associations between cardiovascular reactivity and negative marital interactions. Health Psychology. 2003;22:270–278. doi: 10.1037/0278-6133.22.3.270. doi: 10.1037/0278-6133.22.3.270.
- *Orth-Gomér K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA: Journal of the American Medical Association. 2000;284:3008–3014. doi: 10.1001/jama.284.23.3008. doi: 10.1001/jama.284.23.3008.
- Osterberg L, Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- *Pence LB, Thorn BE, Jensen MP, Romano JM. Examination of perceived spouse responses to patient well and pain behavior in patients with headache. Clinical Journal of Pain. 2008;24:654–661. doi: 10.1097/AJP.0b013e31817708ea. doi: 10.1097/AJP.0b013e31817708ea.
- Peplau LA, Fingerhut AW. The close relationships of lesbians and gay men. Annual Review of Psychology. 2007;58:405–424. doi: 10.1146/annurev.psych.58.110405.085701. doi: 10.1146/annurev.psych.58.110405.085701. [DOI] [PubMed] [Google Scholar]
- Peterson KM, Smith DA, Windle CR. Explication of interspousal criticality bias. Behaviour Research and Therapy. 2009;47:478–486. doi: 10.1016/j.brat.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. Journal of Applied Psychology. 2005;90:175–181. doi: 10.1037/0021-9010.90.1.175. doi: 10.1037/0021-9010.90.1.175. [DOI] [PubMed] [Google Scholar]
- Pew Research Center The decline of marriage and rise of new families. 2010 Retrieved from http://www.pewsocialtrends.org/files/2010/11/pew-social-trends-2010-families.pdf.
- *Phillips AC, Carroll D, Burns VE, Ring C, Macleod J, Drayson M. Bereavement and marriage are associated with antibody response to influenza vaccination in the elderly. Brain, Behavior Immunity. 2006;20:279–289. doi: 10.1016/j.bbi.2005.08.003. doi: 10.1016/j.bbi.2005.08.003.
- Prather AA, Marsland AL. Immunological functioning II: Field measures and viral challenge. In: Luecken LJ, Gallo LC, editors. Handbook of physiological research methods in health psychology. Sage Publications; Thousand Oaks, CA: 2008. pp. 235–245. [Google Scholar]
- Preacher KJ, Rucker DD, MacCallum RC, Nicewander WA. Use of the extreme groups approach: A critical reexamination and new recommendations. Psychological Methods. 2005;10:178–192. doi: 10.1037/1082-989X.10.2.178. doi: 10.1037/1082-989X.10.2.178. [DOI] [PubMed] [Google Scholar]
- *Prigerson HG, Maciejewski PK, Rosenheck RA. The effects of marital dissolution and marital quality on health and health service use among women. Medical Care. 1999;37:858–873. doi: 10.1097/00005650-199909000-00003. doi: 10.1097/00005650-199909000-00003.
- Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69:576–593. doi: 10.1111/j.1741-3737.2007.00393.x. [Google Scholar]
- Psaty BM, Weiss NS, Furberg CD, Koepsell TD, Siscovick DS, Rosendaal FR, Wagner EH. Surrogate end points, health outcomes, and the drug-approval process for the treatment of risk factors for cardiovascular disease. JAMA: Journal of the American Medical Association. 1999;282:786–790. doi: 10.1001/jama.282.8.786. doi: 10.1001/jama.282.8.786. [DOI] [PubMed] [Google Scholar]
- *Raichle KA, Romano JM, Jensen MP. Partner responses to patient pain and well behaviors and their relationship to patient pain behavior, functioning, and depression. Pain. 2011;152:82–88. doi: 10.1016/j.pain.2010.09.015. doi: 10.1016/j.pain.2010.09.015.
- Ramaker C, Marinus J, Stiggelbout AM, van Hilten BJ. Systematic evaluation of rating scales for impairment and disability in Parkinson’s disease. Movement Disorders. 2002;17:867–876. doi: 10.1002/mds.10248. doi: 10.1002/mds.10248. [DOI] [PubMed] [Google Scholar]
- Randall AK, Bodenmann G. The role of stress on close relationships and marital satisfaction. Clinical Psychology Review. 2009;29:105–115. doi: 10.1016/j.cpr.2008.10.004. doi: 10.1016/j.cpr.2008.10.004. [DOI] [PubMed] [Google Scholar]
- *Reeder LG. Social factors in heart disease: A preliminary research report on the relationship of certain social factors to blood pressure in males. Social Forces. 1956;34:367–371. doi: 10.2307/2573672.
- *Reese JB, Somers TJ, Keefe FJ, Mosley-Williams A, Lumley MA. Pain and functioning of rheumatoid arthritis patients based on marital status: Is a distressed marriage preferable to no marriage? The Journal of Pain. 2010;11(10):958–964. doi: 10.1016/j.jpain.2010.01.003. doi: 10.1016/j.jpain.2010.01.003.
- Rehman US, Gollan J, Mortimer AR. The marital context of depression: Research, limitations, and new directions. Clinical Psychology Review. 2008;28:179–198. doi: 10.1016/j.cpr.2007.04.007. doi: 10.1016/j.cpr.2007.04.007. [DOI] [PubMed] [Google Scholar]
- *Ren XS. Marital status and quality of relationships: The impact on health perception. Social Science & Medicine. 1997;44:241–249. doi: 10.1016/s0277-9536(96)00158-x. doi: 10.1016/S0277-9536(96)00158-X.
- Repetti RL, Robles TF, Reynolds B. Allostatic processes in the family. Development and Psychopathology. 2011;23:921–938. doi: 10.1017/S095457941100040X. doi: 10.1017/S095457941100040X. [DOI] [PubMed] [Google Scholar]
- Robles TF, Carroll JE. Restorative biological processes and health. Social and Personality Psychology Compass. 2011;5:518–537. doi: 10.1111/j.1751-9004.2011.00368.x. doi: 10.1111/j.1751-9004.2011.00368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles TF, Glaser R, Kiecolt-Glaser JK. Out of balance: A new look at chronic stress, depression, and immunity. Current Directions in Psychological Science. 2005;14:111–115. doi: 10.1111/j.0963-7214.2005.00345.x. [Google Scholar]
- Robles TF, Kane HS. Marriage and immunity. In: Segerstrom SC, editor. The Oxford Handbook of Psychoneuroimmunology. Oxford University Press; New York: 2012. pp. 197–213. [Google Scholar]
- Robles TF, Kiecolt-Glaser JK. The physiology of marriage: Pathways to health. Physiology and Behavior. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. doi: 10.1016/S0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Robles TF, Shaffer VA, Malarkey WB, Kiecolt-Glaser JK. Positive behaviors during marital conflict: Influences on stress hormones. Journal of Social and Personal Relationships. 2006;23:305–325. doi: 10.1177/0265407506062482. [Google Scholar]
- *Rohrbaugh MJ, Mehl MR, Shoham V, Reilly ES, Ewy GA. Prognostic significance of spouse we talk in couples coping with heart failure. Journal of Consulting and Clinical Psychology. 2008;76:781–789. doi: 10.1037/a0013238. doi: 10.1037/A0013238.
- Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. American Journal of Cardiology. 2006;98:1069–1072. doi: 10.1016/j.amjcard.2006.05.034. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- *Romano JM, Turner JA, Jensen MP. The family environment in chronic pain patients: Comparison to controls and relationship to patient functioning. Journal of Clinical Psychology in Medical Settings. 1997;4:383–395. doi: 10.1023/A:1026253418543.
- Rosnow RL, Rosenthal R. Effect sizes for experimenting psychologists. Canadian Journal of Experimental Psychology. 2003;57:221–237. doi: 10.1037/h0087427. doi: 10.1037/h0087427. [DOI] [PubMed] [Google Scholar]
- *Ryan AK, Willits FK. Family ties, physical health, and psychological well-being. Journal of Aging and Health. 2007;19:907–920. doi: 10.1177/0898264307308340. doi: 10.1177/0898264307308340.
- Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, Nathan DM. Executive summary: Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clinical Chemistry. 2011;57:793–798. doi: 10.1373/clinchem.2011.163634. doi: 10.1373/clinchem.2011.163634. [DOI] [PubMed] [Google Scholar]
- *Sandberg JG, Miller RB, Harper JM, Robila M, Davey A. The impact of marital conflict on health and health care utilization in older couples. Journal of Health Psychology. 2009;14:9–17. doi: 10.1177/1359105308097938. doi: 10.1177/1359105308097938.
- *Saarijärvi S, Rytokoski U, Karppi S. Marital satisfaction and distress in chronic low-back pain patients and their spouses. The Clinical Journal of Pain. 1990;6:148–152. doi: 10.1097/00002508-199006000-00014.
- Saxbe DE. A field (researcher’s) guide to cortisol: Tracking the HPA axis in everyday life. Health Psychology Review. 2008;2:163–190. doi: 10.1080/17437190802530812. [Google Scholar]
- Saxbe DE, Repetti RL. For better or worse? Coregulation of couples’ cortisol levels and mood states. Journal of Personality and Social Psychology. 2010;98:92–103. doi: 10.1037/a0016959. doi: 10.1037/a0016959. [DOI] [PubMed] [Google Scholar]
- Saxbe DE, Repetti RL, Graesch AP. Time spent in housework and leisure: Links with parents’ physiological recovery from work. Journal of Family Psychology. 2011;25:271–281. doi: 10.1037/a0023048. doi: 10.1037/a0023048. [DOI] [PubMed] [Google Scholar]
- *Saxbe DE, Repetti RL, Nishina A. Marital satisfaction, recovery from work, and diurnal cortisol among men and women. Health Psychology. 2008;27:15–25. doi: 10.1037/0278-6133.27.1.15. doi: 10.1037/0278-6133.27.1.15.
- Sbarra DA, Law RW, Portley RM. Divorce and death: A meta-analysis and research agenda for clinical, social, and health psychology. Perspectives on Psychological Science. 2011;6:454–474. doi: 10.1177/1745691611414724. doi: 10.1177/1745691611414724. [DOI] [PubMed] [Google Scholar]
- *Schmoldt RA, Pope CR, Hibbard JH. Marital interaction and the health and well-being of spouses. Women & Health. 1989;15:35–56. doi: 10.1300/J013v15n01_04. doi: 10.1300/J013v15n01_04.
- Schwartz P, Young L. Sexual satisfaction in committed relationships. Sexuality Research and Social Policy. 2009;6:1–17. [Google Scholar]
- *Shek DTL. Marital quality and psychological well-being of married adults in a Chinese context. Journal of Genetic Psychology. 1995;156:45–56. doi: 10.1080/00221325.1995.9914805.
- *Siegel JP. Marital dynamics of women with premenstrual tension syndrome. Family Systems Medicine. 1986;4:358–366. doi: 10.1037/h0089694.
- Slatcher RB. Marital functioning and physical health: Implications for social and personality psychology. Social and Personality Psychology Compass. 2010;4:455–469. doi: 10.1111/j.1751-9004.2010.00273.x. [Google Scholar]
- Slatcher RB, Robles TF, Repetti RL, Fellows MD. Momentary work worries, marital disclosure and salivary cortisol among parents of young children. Psychosomatic Medicine. 2010;72:887–896. doi: 10.1097/PSY.0b013e3181f60fcc. doi: 10.1097/PSY.0b013e3181f60fcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, O’Donovan A, Epel ES, Kemeny ME. Black sheep get the blues: A psychobiological model of social rejection and depression. Neuroscience and Biobehavioral Reviews. 2010;35:39–45. doi: 10.1016/j.neubiorev.2010.01.003. doi: 10.1016/j.neubiorev.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DA, Peterson KM. Overperception of spousal criticism in dysphoria and marital discord. Behavior Therapy. 2008;39:300–312. doi: 10.1016/j.beth.2007.09.002. doi: 10.1016/j.beth.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Smith TW, Brown PC. Cynical hostility, attempts to exert social control, and cardiovascular reactivity in married couples. Journal of Behavioral Medicine. 1991;14:581–592. doi: 10.1007/BF00867172. doi: 10.1007/BF00867172. [DOI] [PubMed] [Google Scholar]
- Smith TW, Cribbet MR, Nealey-Moore JB, Uchino BN, Williams PG, MacKenzie J, Thayer JF. Matters of the variable heart: Respiratory sinus arrhythmia response to marital interaction and associations with marital quality. Journal of Personality and Social Psychology. 2011;100:103–119. doi: 10.1037/a0021136. doi: 10.1037/a0021136. [DOI] [PubMed] [Google Scholar]
- Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. Journal of Personality. 2004;72:1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x. doi: 10.1111/j.1467-6494.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- *Smith TW, Uchino BN, Berg CA, Florsheim P. Marital discord and coronary artery disease: A comparison of behaviorally defined discrete groups. Journal of Consulting and Clinical Psychology. 2012;80:87–92. doi: 10.1037/a0026561. doi: 10.1037/a0026561.
- Smith TW, Uchino BN, Berg CA, Florsheim P, Pearce G, Hawkins M, Yoon HC. Hostile personality traits and coronary artery calcification in middle-aged and older married couples: Different effects for self-reports versus spouse ratings. Psychosomatic Medicine. 2007;69:441–448. doi: 10.1097/PSY.0b013e3180600a65. doi: 10.1097/PSY.0b013e3180600a65. [DOI] [PubMed] [Google Scholar]
- Smith TW, Uchino BN, Berg CA, Florsheim P, Pearce G, Hawkins M, Olsen-Cerny C. Conflict and collaboration in middle-aged and older couples: II. Cardiovascular reactivity during marital interaction. Psychology and Aging. 2009;24:274–286. doi: 10.1037/a0016067. doi: 10.1037/a0016067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth JM. Written emotional expression: Effect sizes, outcome types, and moderating variables. Journal of Consulting and Clinical Psychology. 1998;66:174–184. doi: 10.1037//0022-006x.66.1.174. doi: 10.1037/0022-0006X.66.1.174. [DOI] [PubMed] [Google Scholar]
- Snyder DK, Heyman RE, Haynes SN. Evidence-based approaches to assessing couple distress. Psychological Assessment. 2005;17:288–307. doi: 10.1037/1040-3590.17.3.288. doi: 10.1037/1040-3590.17.3.288. [DOI] [PubMed] [Google Scholar]
- Snyder DK, Simpson JA, Hughes JN, editors. Emotion regulation in couples and families: Pathways to dysfunction and health. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- *Sobal J, Rauschenbach BS, Frongillo EA. Obesity and marital quality - analysis of weight, marital unhappiness, and marital problems in a US national sample. Journal of Family Issues. 1995;16:746–764. doi: 10.1177/019251395016006004.
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family. 1976;38:15–28. doi: 10.2307/350547. [Google Scholar]
- *Staland-Nyman C, Alexanderson K, Hensing G. Associations between strain in domestic work and self-rated health: A study of employed women in Sweden. Scandinavian Journal of Public Health. 2008;36:21–27. doi: 10.1177/1403494807085307. doi: 10.1177/1403494807085307.
- Steptoe A, Gibson EL, Hamer M, Wardle J. Neuroendocrine and cardiovascular correlates of positive affect measured by ecological momentary assessment and by questionnaire. Psychoneuroendocrinology. 2007;32:56–64. doi: 10.1016/j.psyneuen.2006.10.001. doi: 10.1016/j.psyneuen.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Story LB, Karney BR, Lawrence E, Bradbury TN. Interpersonal mediators in the intergenerational transmission of marital dysfunction. Journal of Family Psychology. 2004;18:519–529. doi: 10.1037/0893-3200.18.3.519. doi: 10.1037/0893-3200.18.3.519. [DOI] [PubMed] [Google Scholar]
- *Strawbridge WJ, Shema SJ, Roberts RE. Impact of spouses’ sleep problems on partners. Sleep. 2004;27:527–531. doi: 10.1093/sleep/27.3.527.
- Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. The Lancet. 2007;370:1960–1973. doi: 10.1016/S0140-6736(07)61816-9. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- *Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. General Hospital Psychiatry. 1994;16:259–266. doi: 10.1016/0163-8343(94)90005-1. doi: 10.1016/0163-8343(94)90005-1.
- Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin. 2005;131:260–300. doi: 10.1037/0033-2909.131.2.260. doi: 10.1016/S0191-8869(98)00064-6. [DOI] [PubMed] [Google Scholar]
- Temple R. Are surrogate markers adequate to assess cardiovascular disease drugs? JAMA: The Journal of the American Medical Association. 1999;282:790–795. doi: 10.1001/jama.282.8.790. doi: 10.1001/jama.282.8.790. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52:145–161. doi: 10.1177/0022146510395592. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Thomson CA, Ravia J. A systematic review of behavioral interventions to promote intake of fruit and vegetables. Journal of the American Dietetic Association. 2011;111:1523–1535. doi: 10.1016/j.jada.2011.07.013. doi: 10.1016/j.jada.2011.07.013. [DOI] [PubMed] [Google Scholar]
- *Tobe SW, Kiss A, Sainsbury S, Lesin M, Geerts R, Baker B. The impact of job strain and marital cohesion on ambulatory blood pressure during 1 year: The double exposure study. American Journal of Hypertension. 2007;20:148–153. doi: 10.1016/j.amjhyper.2006.07.011.
- *Tobe SW, Kiss A, Szalai JP, Perkins N, Tsigoulis M, Baker B. Impact of job and marital strain on ambulatory blood pressure results from the double exposure study. American Journal of Hypertension. 2005;18:1046–1051. doi: 10.1016/j.amjhyper.2005.03.734. doi: 10.1016/j.amjhyper.2005.03.734.
- *Trevino DB, Young EH, Groff J, Jono RT. The association between marital adjustment and compliance with antihypertension regimens. Journal of the American Board of Family Practice. 1990;3:17–25.
- Trieber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosomatic Medicine. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- *Trief PM, Himes CL, Orendorff R, Weinstock RS. The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care. 2001;24:1384–1389. doi: 10.2337/diacare.24.8.1384. doi: 10.2337/diacare.24.8.1384.
- *Trief PM, Morin PC, Izquierdo R, Teresi J, Starren J, Shea S, Weinstock RS. Marital quality and diabetes outcomes: The IDEATel Project. Families, Systems Health. 2006;24:318–331. doi: 10.1037/1091-7527.24.3.318.
- Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine. 2004;27:148–154. doi: 10.1207/s15324796abm2703_2. doi: 10.1207/s15324796abm2703_2. [DOI] [PubMed] [Google Scholar]
- *Trief PM, Wade MJ, Britton KD, Weinstock RS. A prospective analysis of marital relationship factors and quality of life in diabetes. Diabetes Care. 2002;25:1154–1158. doi: 10.2337/diacare.25.7.1154. doi: 10.2337/diacare.25.7.1154.
- *Troxel WM, Buysse DJ, Hall M, Matthews KA. Marital happiness and sleep disturbances in a multi-ethnic sample of middle-aged women. Behavioral Sleep Medicine. 2009;7:2–19. doi: 10.1080/15402000802577736. doi: 10.1080/15402000802577736.
- *Troxel WM, Matthews KA, Gallo LC, Kuller LH. Marital quality and occurrence of the metabolic syndrome in women. Archives of Internal Medicine. 2005;165:1022–1027. doi: 10.1001/archinte.165.9.1022. doi: 10.1001/archinte.165.9.1022.
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS. Health-related social control within older adults’ relationships. Journal of Gerontology: Psychological Sciences. 2002;57B:P387–P395. doi: 10.1093/geronb/57.5.p387. doi: 10.1093/geronb/57.5.P387. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Social support and physical health: Understanding the health consequences of relationships. Yale University Press; New Haven, CT: 2004. [Google Scholar]
- Uchino BN. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science. 2009;4:236–255. doi: 10.1111/j.1745-6924.2009.01122.x. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- Umberson D, Williams K. Marital quality, health, and aging: Gender equity? Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60:109–113. doi: 10.1093/geronb/60.special_issue_2.s109. doi: 10.1093/geronb/60.Special_Issue_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. doi: 10.1177/002214650604700101.
- United States Census Bureau American Community Survey 1-year estimates: S1201 – Marital status. 2010 [Data set and interactive table]. Retrieved from http://www.census.gov/acs/www/
- United States Department of Health and Human Services . 2008 Physical activity guidelines for Americans. author; Washington, DC: 2008. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division World Marriage Data 2008: Ever married women and men. 2009 [Data file]. Retrieved from http://www.un.org/esa/population/publications/WMD2008/WP_WMD_2008/Data.html.
- United Nations Human Development Report Office Gender Inequality Index (GII) Trend (1995-2011) 2011 [Data file]. Retrieved from http://hdr.undp.org/en/statistics/gii/
- *Vedhara K, Tuinstra J, Miles JNV, Sanderman R, Ranchor AV. Psychosocial factors associated with indices of cortisol production in women with breast cancer and controls. Psychoneuroendocrinology. 2006;31:299–311. doi: 10.1016/j.psyneuen.2005.08.006. doi: 10.1016/j.psyneuen.2005.08.006.
- *Vitaliano PP, Young HM, Russo J, Romano JM, Magana-Amato A. Does expressed emotion in spouses predict subsequent problems among care recipients with Alzheimer’s disease? Journal of Gerontology. 1993;48:P202–P209. doi: 10.1093/geronj/48.4.p202. doi: 10.1093/geronj/48.4.P202.
- *Waltz M, Badura B, Pfaff H, Schott T. Marriage and the psychological consequences of a heart attack: A longitudinal study of adaptation to chronic illness after 3 years. Social Science & Medicine. 1988;27:149–158. doi: 10.1016/0277-9536(88)90323-1. doi: 10.1016/0277-9536(88)90323-1.
- Wanic RA, Kulik J. Toward an understanding of gender differences in the impact of marital conflict on health. Sex Roles. 2011a;5:297–302. doi: 10.1007/s11199-011-9968-6. [Google Scholar]
- Wanic RA, Kulik J. Embracing complexity and seeking simplicity in interpersonal relationships: A defense of the subordination-reactivity hypothesis. Sex Roles. 2011b;5-6:327–331. doi: 10.1007/s11199-011-0026-1. [Google Scholar]
- *Wang HX, Leineweber C, Kirkeeide R, Svane B, Schenck-Gustafsson K, Theorell T. Psychosocial stress and atherosclerosis: Family and work stress accelerate progression of coronary disease in women. The Stockholm Female Coronary Angiography Study. Journal of Internal Medicine. 2007;261:245–254. doi: 10.1111/j.1365-2796.2006.01759.x. doi: 10.1111/j.1365-2796.2006.01759.x.
- Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 Health Survey. QualityMetric, Inc.; Lincoln, RI: 2000. [Google Scholar]
- *Weiss RL, Aved BM. Marital satisfaction and depression as predictors of physical health status. Journal of Consulting and Clinical Psychology. 1978;46:1379–1384. doi: 10.1037/0022-006X.46.6.1379.
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. American Psychological Association; Washington, DC: 2001. pp. 3–24. [Google Scholar]
- Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clinical Child and Family Psychology Review. 2012;15:4–13. doi: 10.1007/s10567-011-0107-2. doi: 10.1007/s10567-011-0107-2. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Sbarra DA. Marital adjustment and interleukin-6 (IL-6) Journal of Family Psychology. 2012;26:290–295. doi: 10.1037/a0026902. doi: 10.1037/a0026902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA, Snyder DK, Beach SRH. Screening for marital and relationship discord. Journal of Family Psychology. 2009;23:247–254. doi: 10.1037/a0014476. doi: 10.1037/a0014476. [DOI] [PubMed] [Google Scholar]
- *Whisman MA, Uebelacker LA. A longitudinal investigation of marital adjustment as a risk factor for metabolic syndrome. Health Psychology. 2012;31:80–86. doi: 10.1037/a0025671. doi: 10.1037/a0025671.
- Whisman MA, Uebelacker LA, Bruce ML. Longitudinal association between marital dissatisfaction and alcohol use disorders in a community sample. Journal of Family Psychology. 2006;20:164–167. doi: 10.1037/0893-3200.20.1.164. doi: 10.1037/0893-3200.20.1.164. [DOI] [PubMed] [Google Scholar]
- *Whisman MA, Uebelacker LA, Settles TD. Marital distress and the metabolic syndrome: Linking social functioning with physical health. Journal of Family Psychology. 2010;24:367–370. doi: 10.1037/a0019547. doi: 10.1037/a0019547.
- *Wickrama KAS, Bryant CM, Wickrama TKA. Perceived community disorder, hostile marital interactions, and self-reported health of African American couples: An interdyadic process. Personal Relationships. 2010;17:515–531. doi: 10.1111/j.1475-6811.2010.01299.x.
- *Wickrama KAS, Lorenz FO, Conger RD, Elder GH. Marital quality and physical illness: A latent growth curve analysis. Journal of Marriage and Family. 1997;59:143–155. doi: 10.2307/353668.
- *Willits FK, Crider DM. Health rating and life satisfaction in the later middle years. Journals of Gerontology. 1988;43:S172–S176.
- Wood W, Eagly AH. A cross-cultural analysis of the behavior of women and men: Implications for the origins of sex differences. Psychological Bulletin. 2002;128:699–727. doi: 10.1037/0033-2909.128.5.699. doi: 10.1037/0033-2909.128.5.699. [DOI] [PubMed] [Google Scholar]
- World Health Organization Fruit and vegetables for health: Report of a joint FAO/WHO workshop; Kobe, Japan. 1-3 September 2004; Geneva, Switzerland: Author; 2004. [Google Scholar]
- *Yang HC, Schuler TA. Marital quality and survivorship: Slowed recovery for breast cancer patients in distressed relationships. Cancer. 2009;115:217–228. doi: 10.1002/cncr.23964. doi: 10.1002/cncr.23964.
- *Yorgason J, Almeida D, Neupert SD, Spiro A, Hoffman L. A dyadic examination of daily health symptoms and emotional well-being in late-life couples. Family Relations. 2006;55:613–624. doi: 10.1111/j.1741-3729.2006.00430.x.
- Zautra AJ, Hoffman JM, Matt KS, Yocum D, Potter PT, Castro WL, Roth S. An examination of individual differences in the relationship between interpersonal stress and disease activity among women with rheumatoid arthritis. Arthritis Care and Research. 1998;11:271–279. doi: 10.1002/art.1790110408. doi: 10.1002/art.1790110408. [DOI] [PubMed] [Google Scholar]
- *Zhou ES, Kim Y, Rasheed M, Benedict C, Bustillo NE, Soloway M, Penedo FJ. Marital satisfaction of advanced prostate cancer survivors and their spousal caregivers: The dyadic effects of physical and mental health. Psychooncology. 2011;20:1353–1357. doi: 10.1002/pon.1855. doi: 10.1002/pon.1855.