Abstract
Angle kappa is the difference between the pupillary and visual axis. This measurement is of paramount consideration in refractive surgery, as proper centration is required for optimal results. Angle kappa may contribute to MFIOL decentration and its resultant photic phenomena. Adjusting placement of MFIOLs for angle kappa is not supported by the literature but is likely to help reduce glare and haloes. Centering LASIK in angle kappa patients over the corneal light reflex is safe, efficacious, and recommended. Centering in-between the corneal reflex and the entrance pupil is also safe and efficacious. The literature regarding PRK in patients with an angle kappa is sparse but centering on the corneal reflex is assumed to be similar to centering LASIK on the corneal reflex. Thus, centration of MFIOLs, LASIK, and PRK should be focused on the corneal reflex for patients with a large angle kappa. More research is needed to guide surgeons’ approach to angle kappa.
Keywords: Angle Kappa, Visual Axis, Pupillary Axis, LASIK, PRK, Multi focal Intra ocular lenses
Introduction
With recent advancements in the precision of refractive surgery angle kappa stands as an important consideration in improving visual outcomes. Angle kappa is defined as the angle between the visual axis (line connecting the fixation point with the fovea) and the pupillary axis (line that perpendicularly passes through the entrance pupil and the center of curvature of the cornea).[1] It can be identified clinically by the nasal displacement of the corneal light reflex from the pupil center,[2] and it represents a misalignment of light passing through the refractive surface of the cornea and the bundle of light formed by the pupil. Figure 1 depicts a coronal view of angle kappa as well as the surgeon's view when seen through the microscope.
Figure 1.
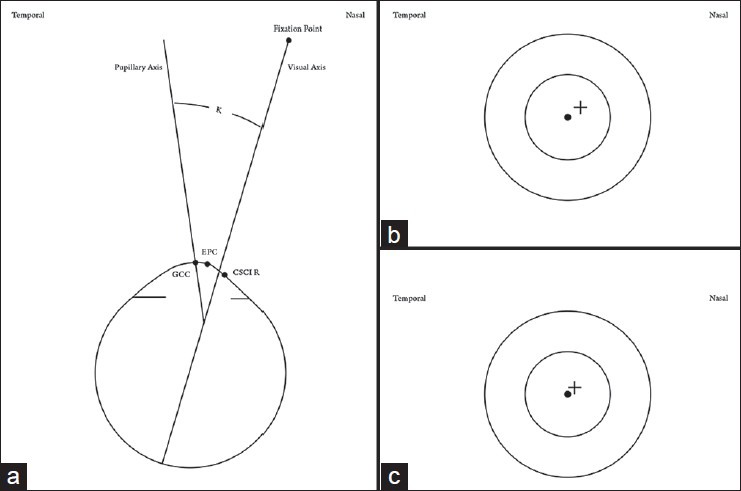
(a) Depicting angle κ, geometric center of the cornea (GCC), entrance pupil center (EPC), and coaxially sighted corneal light reflex (CSCLR) as identified by Pande and Hillman,[4] (b) Surgeon's view of a large angle kappa, (c) Surgeon's view of a normal but small positive angle kappa. (•) = EPC (+) = CSCLR
A large angle kappa is clinically significant as it may lead to alignment errors during photo ablation in laser refractive surgery,[3] as well lens decentration in intraocular refractive surgery. The decentration of ablation zones can lead to under correction[4] and irregular astigmatism.[3] Decentration of intraocular lenses may cause photic phenomenon[5] and decreased lens effectiveness.[6] This issue is most important in hyperopic patients, who tend to have larger angle kappa values.[3,7]
A Pubmed literature review was conducted for several terms related to angle kappa and refractive surgery. Relevant manuscripts were compiled into this review to summarize the current literature on the role of angle kappa in refractive surgery, specifically as it relates to PRK, LASIK, and placement of multifocal intraocular lenses (MFIOLs).
Materials and Methods
A thorough PubMed search was conducted using various combinations of the following terms: Angle Kappa, LASIK, PRK, Intraocular lenses, Capsulorrhexis, Centration, Refractive Surgery, Cataract Surgery, Pupillary Axis, Visual Axis, Coaxial Axis, Pupil Tracking, and Hyperopia. The search was limited to articles of the following types: Reviews, systematic reviews, randomized controlled trial, practice guidelines, meta-analysis, journal article, guideline, clinical trial, and case reports. The initial literature review resulted in 66 articles. From the initial inquiry articles were chosen based on their relevance to Angle kappa, MFIOLs, LASIK, PRK and Hyperopia. In total 40 articles were selected, reviewed for relevant content, and compiled into this review.
Angle kappa in the general population
As the fovea lies slightly temporal to the point at which the pupillary axis intersects with the posterior pole of the globe, the normal angle kappa is slightly positive.[3] The high prevalence of small positive angle kappa values in the non-hyperopic population was reported in 2005 by Srivannaboon and Chotikavanich. In 408/420 (97%) eyes undergoing refractive surgery for correction of myopia, a positive angle kappa of 0.5 mm or less was observed.[8]
Several studies have been conducted to determine the population's mean value of a positive angle kappa. The results of these studies are summarized in Table 1. Based on current literature the mean value of angle kappa in a normal population of emmetropes lies between 2.78 ± 0.12° in right eyes and 3.32 ± 0.13° in left eyes when measured by the Syntophore corneal topography system (Clement Clarke International Ltd, London, UK).[3,9] The value lies between 5.55 ± 0.13° and 5.62 ± 0.10° in right and left eyes respectively when measured by the Orbscan II corneal topographer (Bausch and Lomb, USA).[3] The range may slightly differ (4.97 ± 1.24°) if measured with the Orbscan IIz (Bausch and Lomb, USA).[10]
Table 1.
Summary of studies reporting normative angle kappa values
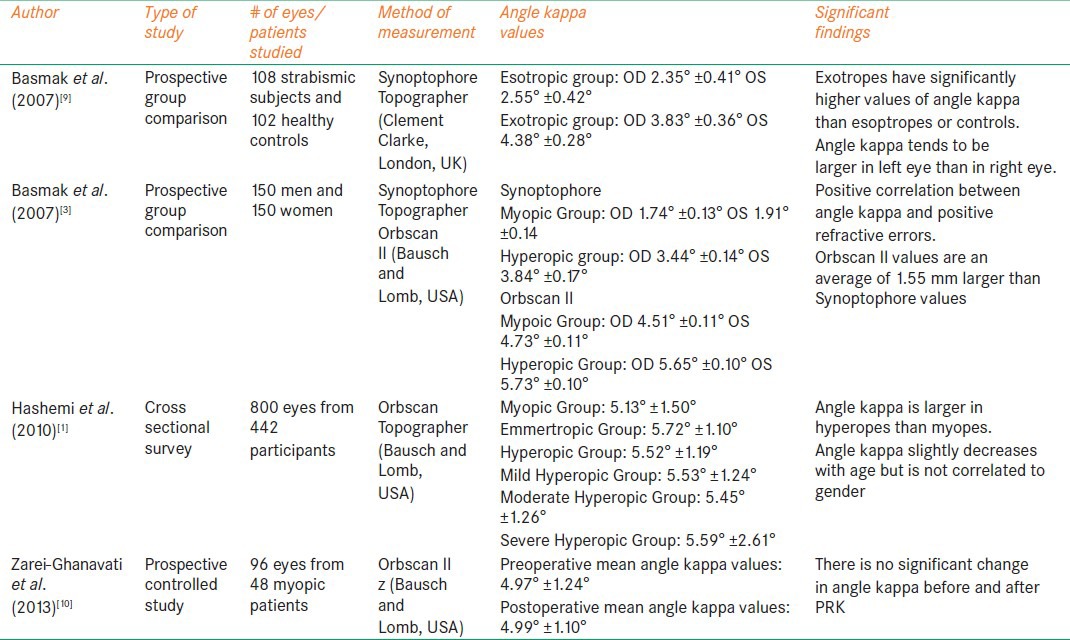
The significance of eye dominance as well as the machine used to measure angle kappa is not fully understood however, these are two variables that should likely be considered when contemplating issues related to angle kappa. Additionally gender does not appear to be correlated with angle kappa.[1] While angle kappa tends to decrease with age,[1] the change in direction or magnitude is not significant.[11]
Angle kappa and multifocal intra ocular lenses
Multi-focal intraocular lenses (MFIOLs) are designed with concentric apodization to provide functional vision at distance as well as near. With this design distance and intermediate visual acuity are adversely affected if the lens is decentered.[6] The etiology of this is not fully understood. Decentration can also cause photic phenomenon[5] and is one of the main indications for MFIOL exchange.[12] A large angle kappa could contribute to functional decentration if the MFIOL is centered on one axis, (pupillary or visual axis) and is not aligned with the other.
In 2011 Prakash et al reported that larger preoperative angle kappa values in MFIOL placement were correlated with patient complaints of glare (R2= 0.26, P= 0.033). They also reported that perceived severity of haloes were correlated to angle kappa and postoperative uncorrected distance visual acuity (UCVA) (R2 = 0.26, P = 0.029).[5] While positive angle kappa may play a role in contributing to glare and haloes, dissatisfaction with MFIOLs is truly multifactorial. Blurry vision of various etiologies,[13] other forms of photic phenomenon,[14] and unsatisfactory postoperative distance UCVA[5] are more common patient complaints after receiving MFIOLs.
A large angle kappa may contribute to functional decentration of MFIOLs, but the effect of this decentration is not clear. In 2010, Rosales et al used simulated aberration models generated from the anatomical, Purkinje, and Sheimpflug data of 21 eyes to show that the tilt and decentration of IOLs have only a minor effect on higher order aberrations.[15] However, it has been reported that decentration of MFIOLs greater than 0.7 mm substantially impairs distance visual acuity.[6]
If the lens is significantly decentered because of failure to accommodate for angle kappa, then central light rays may miss the central optical zone and pass through one of the multifocal rings, leading to glare. In 2012, Berdahl suggested that MFIOLs are unacceptable for use if the angle kappa is greater than half of the diameter of the central optical zone for the respective lens. For the ReSTOR lens (Alcon TX, USA) this would be an angle kappa greater than 0.4mm and for the Tecnis lens (Abbott Illinois, USA) this would be a value greater than 0.5 mm.[16]
One proposed method for compensating for large angle kappa in MFIOLs is to purposely decenter the lens toward the visual axis. Due to contraction of the capsule, memory of the haptics, and IOL rotation, it is uncertain if the lens would stay in the decentered position.[5] Gluing a single haptic of the IOL to align its position with the visual axis has also been suggested.[5] Solomon and Donnefield have reported performing post-operative pupilloplasty with argon laser to center the pupil, and move the pupillary axis closer to the visual axis in MFIOL cases with a large angle kappa.[17] Melki and Harissi-Dagher described a method for centering the capsulorrhexis on the coaxially sighted intraocular lens reflex instead of the corneal reflex as a way to accommodate for angle kappa.[18] These methods may be effective but have not been validated in large studies. More research is needed to determine their clinical relevance.
Based on the current literature, a large angle kappa may contribute to decentration of MFIOLs potentially resulting in glare and decreased visual acuity. However, the clinical significance of lens decentration as a direct result of angle kappa is not fully understood. There is no evidence to show that altering centration of MFIOLs is detrimental or dangerous for the patient. Thus we recommend centering these lenses on the corneal reflex in eyes with angle kappa values greater than the normative values discussed earlier as per eye and per topography system used.
Angle kappa in laser guided refractive surgery: the debate over where to center ablation profiles
There are four main methods for centration of laser refractive surgery that have been suggested in the literature:
Center of the pupil: In 1987, Uozato and Guyton suggested using the center of the pupil[19] as it has been shown that photoreceptors actively orient themselves toward the pupillary center.[20] Mandell seconded this suggestions with the rationale that the pupil defines the bundle of light that passes through the eye and forms the retinal image.[21]
Coaxially Sighted Corneal Light Reflex: In 1993, Pande and Hillman concluded that the coaxially sighted corneal light reflex (CSCLR) should be used for centration as it was the closest measurable point to the visual axis.[4] Additionally, they noted that the center of the pupil changes position with changes in the size of the pupil,[22] and thus should not be used for centration.[4]
Corneal Vertex Normal: In 2006, De Ortueta et al centered ablation zones on the corneal vertex normal,[23] which is the point of maximum elevation in corneal topography.[2] This was combined with videokeratoscopy/pupil tracking which allowed the ablation zone to shift a fixed amount in relation to the center of the pupil as it changed with differing light conditions.[23] The results of this study are summarized in Table 2.
Between the pupillary and visual axis: In 2009 Kermani et al centered on a distance halfway between the center of the pupil (line of sight) and the corneal light reflex (visual axis) in patients with a large angle kappa.[24]
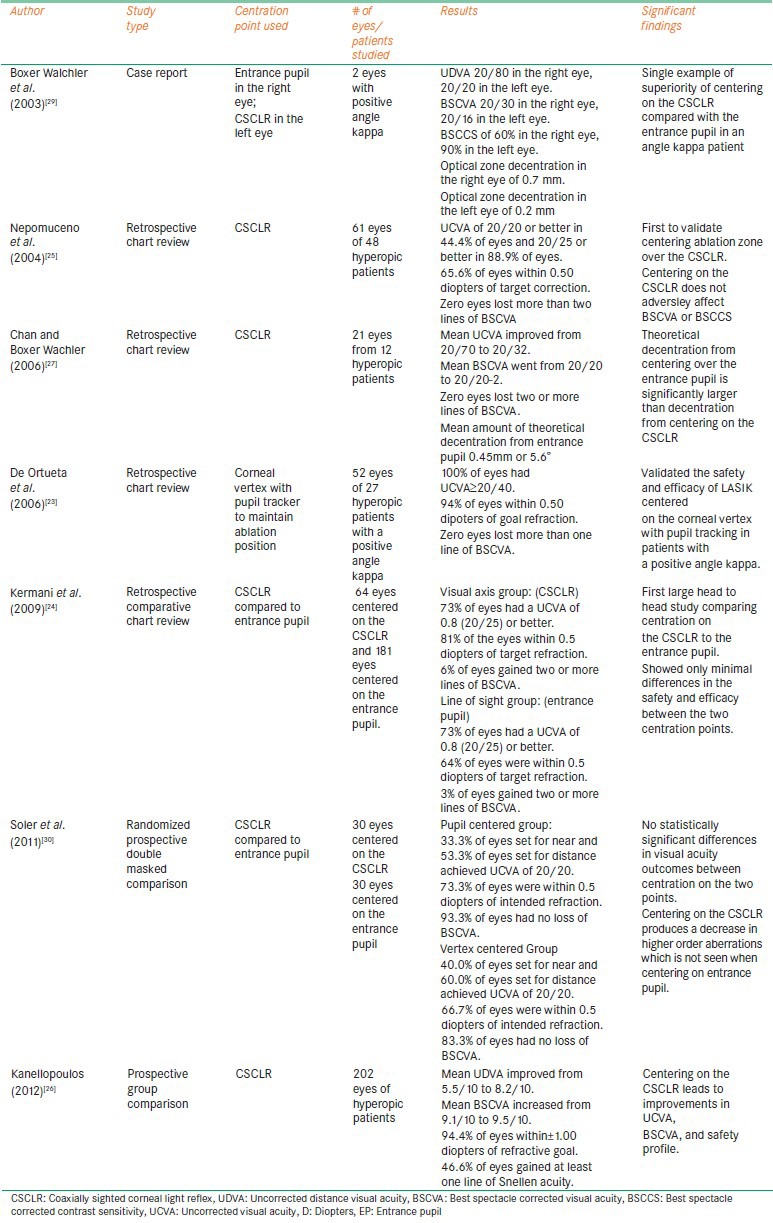
Table 2.
Summary of articles relating angle kappa to LASIK
These four methods of centration have not simultaneously been compared in head to head trials. The following will discuss what has been accomplished in the literature specifically as it relates centering in patients with a large angle kappa.
Angle kappa and hyperopic laser assisted in situ keratomileusis (LASIK)
Several studies are found in the literature that demonstrate the benefits of moving centration for hyperopic LASIK to the CSCLR to adjust for a large angle kappa. This review focused on hyperopic LASIK as hyperopes are more likely to have a large angle kappa. These studies are summarized in Table 2.
Nepomuceno et al was the first to validate this method in 2004 with patients who underwent hyperopic LASIK correction using the LADARVision 4000 excimer laser (Alcon, TX, USA). They reported an increased safety profile which they attributed to this centration technique because the same surgeon did not have equivalently good results when using other centration sites. The authors stressed the importance of centering over the CSCLR for hyperopes due to a large angle kappa, and also because hyperopes have smaller functional optical zones and less tolerance of decentration.[25] Several years later, Kanellopoulos also reported a good safety profile when centering on the CSCLR to accommodate for angle kappa. In addition, he reported a significant postoperative improvement in uncorrected visual acuity and an increase in best spectacle corrected visual acuity (BSCVA).[26]
Chan and Boxer Wachler measured the amount of post-operative decentration of ablation zones centered on the CSCLR in patients with a large angle kappa. This value was added to the pre-operative angle kappa to represent the amount of decentration that would have occurred if the ablation had been centered on the entrance pupil. The theoretical decentration from entrance pupil centration was significantly larger than the decentration that actually occurred when centering on the corneal reflex.[27]
Kermani reported a case of a patient with a large angle kappa who underwent LASIK with ablation centered on the entrance pupil. Postoperatively he had lost two lines of BSCVA, his hyperopia was under corrected, and astigmatic error was introduced. The patient later had a repeat procedure centered on the CSCLR. The refractive error was corrected and the BSCVA was restored.[28]
The above reviewed studies helped establish the safety and efficacy of centering ablation profiles on or near the visual axis in patients with a large angle kappa. In 2003, a case report of a patient with bilateral large angle kappa provided the first direct comparison of centering on the entrance pupil versus centering on the CSCLR. He had LASIK centered on the entrance pupil in the right eye, and over the CSCLR in the left eye. The left eye demonstrated significantly better visual acuity, smaller refractive error, and a smaller amount of post-operative decentration.[29]
While this case report was intriguing, it was not until 2009 that a larger study comparing the two methods was published. Kermani et al conducted a retrospective review of LASIK centered on the pupil versus centration focused on the CSCLR in eyes with a positive angle kappa. Based on their previous experience the researchers centered the CSCLR group on a point midway between the line of sight and the corneal reflex. They reported only minimal differences in safety and efficacy between the two centration points. However, they did report a decrease in total higher order aberrations in the CSCLR group; this effect was not seen in the pupil centered group.[24]
In 2011, Soler et al published the only randomized double masked comparison of pupil centered vs. corneal reflex centered hyperopic LASIK. This study concluded that there were no statistical differences in terms of safety, efficacy, or accuracy between the two different centration points[30] However, this study was limited by a small sample size and by a patient population of mild to moderate hyperopes. The smaller angle kappa values associated with lower degrees of hyperopia may have masked prominent differences between the two centration options.
From the current literature, several conclusions can be drawn. Angle kappa generally is larger in hyperopic patients.[3] A larger angle kappa increases the risk for decentration of the optical zone from the visual axis if ablation is centered over the entrance pupil. Such decentration can cause many optical problems, induce astigmatism,[26] and leave the patient's visual deficits uncorrected. Thus, centering over the corneal reflex may decrease higher order aberrations which the patient is likely to appreciate.[30]
We recommend using the corneal reflex when performing LASIK on hyperopes, especially when they have a large angle kappa. Centering over a point half of the distance between the CSCLR and the pupil center may also be an effective method in angle kappa patients.[24] Using the entrance pupil when performing LASIK on myopes or mild hyperopes with a small angle kappa is safe and efficacious as the entrance pupil and CSCLR will nearly align. A large double masked head to head trial comparing the various centration techniques is needed to further guide this debate. This study would be most helpful if it had a large array of hyperopes with multiple ranges of angle kappa values that could be individually analysed.
Angle kappa and photorefractive keratectomy (PRK)
There have been very few studies conducted concerning angle kappa and PRK. Many of these studies only indirectly address angle kappa by touching on principles of decentration in myopes or principles applied to hyperopic surgery where angle kappa is more prevalent. The results of these studies are summarized in Table 3.
Table 3.
Summary of articles relating angle kappa to PRK
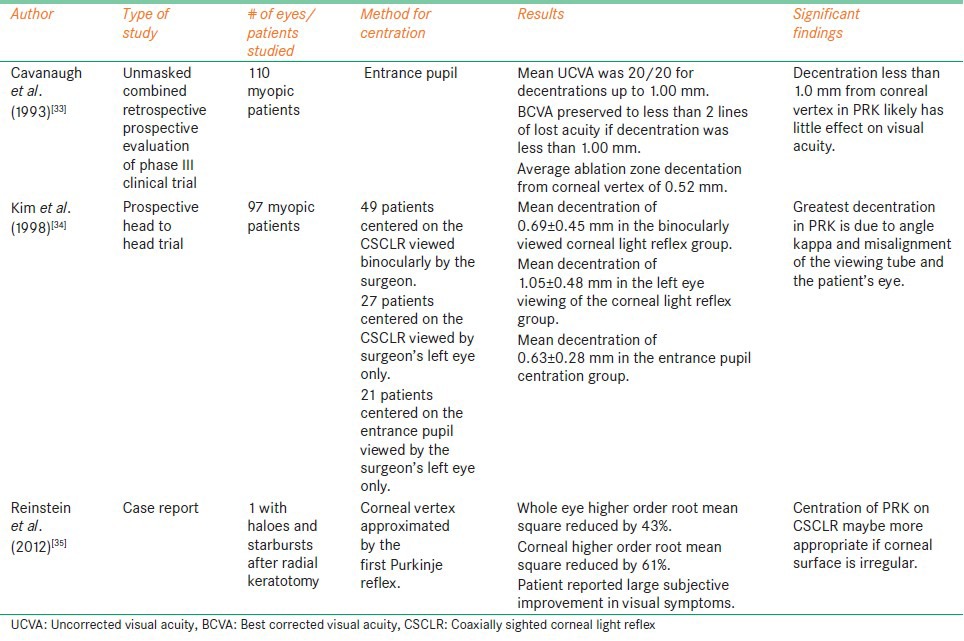
In 1993, Cavanaugh et al noted that angle lambda, the angle between the pupillary axis and the line of sight, could contribute to decentration error when performing PRK.[31] Angle kappa and angle lambda are nearly identical at distance fixation.[32] This study emphasized centering ablation zones for PRK over the entrance pupil as crucial to the success of the procedure.[31] However, it should be noted that this study was conducted on myopes, who are not as likely as hyperopes to have a large angle kappa.[3]
In 1993, Cavanaugh et al published a separate study on PRK centered over the entrance pupil, which measured the average amount of decentration from the corneal vertex that occurs and resultant effects on visual acuity. They reported a positive correlation between preserved UCVA and BCVA in patients whose decentration was less than 1.0 mm.[33] This would suggest that if PRK is centered on the entrance pupil in a patient with a large angle kappa, decentration may be insignificant if it is less than 1.0 mm. However, the relevance of this measurement is hard to extrapolate as the authors centered their procedures over the entrance pupil but then measured decentration from the corneal vertex.
In 1998, Kim et al measured and compared the post-operative decentration of ablation zones in PRK using three different methods: 1) ablation zones centered on the corneal light reflex as viewed by both eyes of the surgeon, 2) ablation zones centered on the corneal reflex viewed with only the surgeon's left eye, and 3) ablation zones centered on the entrance pupil viewed with only the surgeon's left eye. The smallest amount of decentration was seen in the group which was centered on the entrance pupil viewed by the surgeons left eye. The largest decentration was seen when centered on the corneal reflex viewed by the surgeons left eye only. They attributed this result partly to a large angle kappa and misalignment, but mainly thought it to be a product misalignment of the fixation tube when viewing the patient's right eye with the surgeon's left eye.[34]
In 2012, Reinstein et al reported a case of PRK centered on the corneal vertex in a patient with a large vertical angle kappa. The patient had significant night vision disturbances after having radial keratotomy. The authors speculated that wave front guided profiles centered on his pupil would have been inappropriate for the irregular surface of his cornea and potentially could have made his symptoms worse. The corneal topography ablation profile centered on his corneal reflex addressed these irregularities and was better suited to fix his problem. PRK was performed using the profile centered on the corneal light reflex. The patient had improved visual results and a subjective reduction in his night vision disturbances.[35]
While investigating decentration patterns in myopic patients that underwent PRK, Lin et al reported moving the ablation zone to a point half of the distance between the pupil center and the corneal reflex when the discrepancy between them (angle kappa) was more than 0.2 mm. This represented an undisclosed percentage of the study population and they did not perform sub group analysis. However, they did report that moving the ablation zone such a small distance was tolerable for the patients.[36]
Although centering PRK over the entrance pupil has not been specifically tested in patients with a large angle kappa, it has been tested in hyperopes which tend to have larger angle kappa values.[3] Dausch et al reported standard PRK with a 7.0 mm ablation zone centered over the entrance pupil to be efficient and relatively safe for correction of hyperopia up to 7.5 diopters.[37] They also reported that PRK with a 9.0 mm ablation zone centered over the entrance pupil is safe and efficient in treating hyperopia up to 8.25 diopters.[38]
The data regarding angle kappa and PRK is very limited, and no specific conclusions can be drawn. This is likely to be due to the limited number of publications on the topic of angle kappa combined with the nationwide trend to perform LASIK more frequently than PRK. Although the limited data suggest that centering on the entrance pupil is safe and effective, this data comes largely from studies which only indirectly addressed the issue of angle kappa. Centering on the entrance pupil may be safe if the ablation zone is made large enough to cover the misalignment induced by angle kappa. The optical and refractive principles of PRK very closely mimic those used in LASIK. Given this similarity and the body of evidence which supports LASIK centration over the corneal reflex, we recommend centering PRK over the corneal reflex in patients with a large angle kappa.
Angle kappa and myopic LASIK
It may also necessary to consider angle kappa in centration for treatment in myopic patients. It has been suggested by Okamoto et al that approximately 30% of myopic refractive surgery candidates have an angle kappa large enough to warrant centering closer to the visual axis.[39] However, other authors have suggested that angle kappa in myopia is usually negligible.[19,25] A full discussion of the centration techniques in myopia is beyond the scope of this article but two studies deserve mention. Arbelaez et al compared LASIK centered over the pupil to LASIK centered over the corneal vertex in 52 myopic patients with a moderate to large angle kappa. The corneal vertex centered treatments performed better in terms of induced ocular aberrations and asphericity, but there was no difference in photopic visual acuity.[40] In 2009 Okamoto et al compared myopic LASIK centered on the CSCLR with centration on the entrance pupil in 556 eyes with unknown angle kappa values. LASIK centered on the CSCLR was significantly safer, more effective, and had lower induction of coma and total higher order aberrations than LASIK treatments centered on the pupil.[39]
Conclusions
Angle kappa is of great importance in refractive surgery, particularly when treating hyperopes, who tend have large angle kappa values. In some instances, this may also be important for myopes. Angle kappa may play a role in MFIOL decentration, possibly leading to increased glare and haloes. This decentration may be clinically insignificant; however, centering the MFIOLs on the corneal reflex will likely decrease this risk. In hyperopic LASIK or PRK, centration should be focused on either the corneal reflex or the distance half way between pupillary center and the corneal reflex, especially in patients with a large angle kappa. Further studies are needed to fully establish the difference between the various centration methods used in refractive surgery and their effects on eyes with a large angle kappa.
Acknowledgement
Special thanks to Cody Hockin, Graphic Designer, BFA Visual Communication, for his assistance in generation of Figure 1. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Hashemi H, Khabazkhoob M, Yazdani K, Mehravaran S, Jafarzadejpur E, Fotouhi A. Distribution of angle kappa measurements with Orbscan II in a population-based survey. J Refract Surg. 2010;26:966–71. doi: 10.3928/1081597X-20100114-06. [DOI] [PubMed] [Google Scholar]
- 2.Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol. 2012;23:269–75. doi: 10.1097/ICU.0b013e3283543c41. [DOI] [PubMed] [Google Scholar]
- 3.Basmak H, Sahin A, Yildirim N, Papakostas TD, Kanellopoulos JA. Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg. 2007;23:456–60. doi: 10.3928/1081-597X-20070501-06. [DOI] [PubMed] [Google Scholar]
- 4.Pande M, Hillman JS. Optical zone centration in keratorefractive surgery. Entrance pupil center, visual axis, coaxially sighted corneal reflex, or geometric corneal center? Ophthalmology. 1993;100:1230–7. [PubMed] [Google Scholar]
- 5.Prakash G, Prakash DR, Agarwal A, Kumar DA, Agarwal A, Jacob S. Predictive factor and kappa angle analysis for visual satisfactions in patients with multifocal IOL implantation. Eye (Lond) 2011;25:1187–93. doi: 10.1038/eye.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayashi K, Hayashi H, Nakao F, Hayashi F. Correlation between pupillary size and intraocular lens decentration and visual acuity of a zonal-progressive multifocal lens and a monofocal lens. Ophthalmology. 2001;108:2011–7. doi: 10.1016/s0161-6420(01)00756-4. [DOI] [PubMed] [Google Scholar]
- 7.Kermani O, Schmeidt K, Oberheide U, Gerten Gl. Hyperopic laser in situ keratomileusis with 5.5-, 6.5-, and 7.0-mm optical zones. J Refract Surg. 2005;21:52–8. doi: 10.3928/1081-597X-20050101-11. [DOI] [PubMed] [Google Scholar]
- 8.Srivannaboon S, Chotikavanich S. Corneal characteristics in myopic patients. J Med Assoc Thai. 2005;88:1222–7. [PubMed] [Google Scholar]
- 9.Basmak H, Sahin A, Yildirim N, Saricicek T, Yurdakul S. The angle kappa in strabismic individuals. Strabismus. 2007;15:193–6. doi: 10.1080/09273970701631926. [DOI] [PubMed] [Google Scholar]
- 10.Zarei-Ghanavati S, Gharaee H, Eslampour A, Abrishami M, Ghasemi-Moghadam S. Angle kappa changes after photorefractive keratectomy for myopia. Int Ophthalmol. 2013 doi: 10.1007/s10792-013-9775-x. In press. [DOI] [PubMed] [Google Scholar]
- 11.Berrio E, Tabernero J, Artal P. Optical aberrations and alignment of the eye with age. J Vis. 2010;10:34. doi: 10.1167/10.14.34. [DOI] [PubMed] [Google Scholar]
- 12.Leysen I, Bartholomeeusen E, Coeckelbergh T, Tassignon MJ. Surgical outcomes of intraocular lens exchange: Five-year study. J Cataract Refract Surg. 2009;35:1013–8. doi: 10.1016/j.jcrs.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 13.Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35:992–7. doi: 10.1016/j.jcrs.2009.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Vries NE, Webers CA, Touwslager WR, Bauer NJ, De Branbander J, Berendschot TT, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37:859–65. doi: 10.1016/j.jcrs.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 15.Rosales P, De Castro A, Jiménez-alfaro I, Marcos S. Intraocular lens alignment from purkinje and Scheimpflug imaging. Clin Exp Optom. 2010;93:400–8. doi: 10.1111/j.1444-0938.2010.00514.x. [DOI] [PubMed] [Google Scholar]
- 16.Berdahl JP, Waring GO. Match right lens to patient needs: 10 objective measurements can improve multifocal IOL implantation outcomes [monograph on the internet] Ophthalmology Times. 2012. [Last cited 2013 Oct 4]. pp. 28–9. Available from: http://digital.healthcaregroup.advanstar.com .
- 17.Solomon R, Donnenfeld ED, Perry HD, Stein JJ, Su MY, Holladay JT. New Orleans, LA: Poster presented at: The AAO Annual Meeting; 2007. Nov 12, Argon laser iridoplasty to improve visual function following multifocal IOL implantation. [Google Scholar]
- 18.Melki SA, Harissi-dagher M. Coaxially sighted intraocular lens light reflex for centration of the multifocal single piece intraocular lens. Can J Ophthalmol. 2011;46:319–21. doi: 10.1016/j.jcjo.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Uozato H, Guyton DL. Centering corneal surgical procedures. Am J Ophthalmol. 1987;103:264–75. [PubMed] [Google Scholar]
- 20.Enoch JM, Laties AM. An analysis of retinal receptor orientation. II. Predictions for psychophysical tests. Invest Ophthalmol. 1971;10:959–70. [PubMed] [Google Scholar]
- 21.Mandell RB. Apparent pupil displacement in videokeratography. CLAO J. 1994;20:123–7. [PubMed] [Google Scholar]
- 22.Fay AM, Trokel SL, Myers JA. Pupil diameter and the principal ray. J Cataract Refract Surg. 1992;18:348–51. doi: 10.1016/s0886-3350(13)80069-7. [DOI] [PubMed] [Google Scholar]
- 23.De Ortueta D, Schreyger FD. Centration on the cornea vertex normal during hyperopic refractive photoablation using videokeratoscopy. J Refract Surg. 2007;23:198–200. doi: 10.3928/1081-597X-20070201-13. [DOI] [PubMed] [Google Scholar]
- 24.Kermani O, Oberheide U, Schmiedt K, Gerten G, Bains HS. Outcomes of hyperopic LASIK with the NIDEK NAVEX platform centered on the visual axis or line of sight. J Refract Surg. 2009;25(Suppl 1):S98–103. doi: 10.3928/1081597X-20090115-04. [DOI] [PubMed] [Google Scholar]
- 25.Nepomuceno RL, Boxer Wachler BS, Kim JM, Scruggs R, Sato Ml. Laser in situ keratomileusis for hyperopia with the LADAR Vision 4000 with centration on the coaxially sighted corneal light reflex. J Cataract Refract Surg. 2004;30:1281–6. doi: 10.1016/j.jcrs.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 26.Kanellopoulos AJ. Topography-guided hyperopic and hyperopic astigmatism femtosecond laser-assisted LASIK: Long-term experience with the 400 Hz eye-Q excimer platform. Clin Ophthalmol. 2012;6:895–901. doi: 10.2147/OPTH.S23573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan CC, Boxer Wachler BS. Centration analysis of ablation over the coaxial corneal light reflex for hyperopic LASIK. J Refract Surg. 2006;22:467–71. doi: 10.3928/1081-597X-20060501-08. [DOI] [PubMed] [Google Scholar]
- 28.Kermani O. Alignment in customized laser in situ keratomileusis. J Refract Surg. 2004;20(Suppl 5):S651–8. doi: 10.3928/1081-597X-20040903-03. [DOI] [PubMed] [Google Scholar]
- 29.Wachler BS, Korn TS, Chandra NS, Michel FK. Decentration of the optical zone: centering on the pupil versus the coaxially sighted corneal light reflex in LASIK for hyperopia. J Refract Surg. 2003;19:464–5. doi: 10.3928/1081-597X-20030701-17. [DOI] [PubMed] [Google Scholar]
- 30.Soler V, Benito A, Soler P, Triozon C, Arné JL, Madariaga V, et al. A randomized comparison of pupil-centered versus vertex-centered ablation in LASIK correction of hyperopia. Am J Ophthalmol. 2011;152:591–9.e2. doi: 10.1016/j.ajo.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 31.Cavanaugh TB, Durrie DS, Riedel SM, Hunkeler JD, Lesher MP. Centration of excimer laser photorefractive keratectomy relative to the pupil. J Cataract Refract Surg. 1993;19(Suppl):S144–8. doi: 10.1016/s0886-3350(13)80398-7. [DOI] [PubMed] [Google Scholar]
- 32.Legrand Y, El Hage SG. Springer series in optical sciences. Berlin, Germany: Springer; 1980. Physiologic optics; p. 72. [Google Scholar]
- 33.Cavanaugh TB, Durrie DS, Riedel SM, Hunkeler JD, Lesher MP. Topographical analysis of the centration of excimer laser photorefractive keratectomy. J Cataract Refract Surg. 1993;19(Suppl):136–43. doi: 10.1016/s0886-3350(13)80397-5. [DOI] [PubMed] [Google Scholar]
- 34.Kim EK, Jang JW, Lee JB, Hong SB, Lee YG, Kim HB. Comparison of corneal centering in photorefractive keratectomy. Yonsei Med J. 1998;39:317–21. doi: 10.3349/ymj.1998.39.4.317. [DOI] [PubMed] [Google Scholar]
- 35.Reinstein DZ, Archer TJ, Gobbe M. Is topography-guided ablation profile centered on the corneal vertex better than wavefront-guided ablation profile centered on the entrance pupil? J Refract Surg. 2012;28:139–43. doi: 10.3928/1081597X-20111115-01. [DOI] [PubMed] [Google Scholar]
- 36.Lin DT, Sutton HF, Berman M. Corneal topography following excimer photorefractive keratectomy for myopia. J Cataract Refract Surg. 1993;19(Suppl):149–54. doi: 10.1016/s0886-3350(13)80399-9. [DOI] [PubMed] [Google Scholar]
- 37.Dausch D, Klein R, Schröder E. Excimer laser photorefractive keratectomy for hyperopia. Refract Corneal Surg. 1993;9:20–8. [PubMed] [Google Scholar]
- 38.Dausch D, Smecka Z, Klein R, Schröder E, Kirchner Sl. Excimer laser photorefractive keratectomy for hyperopia. J Cataract Refract Surg. 1997;23:169–76. doi: 10.1016/s0886-3350(97)80338-0. [DOI] [PubMed] [Google Scholar]
- 39.Okamoto S, Kimura K, Funakura M, Ikeda N, Hiramatsu H, Bains HS. Comparison of myopic LASIK centered on the coaxially sighted corneal light reflex or line of sight. J Refract Surg. 2009;25(Suppl 10):S944–50. doi: 10.3928/1081597X-20090915-09. [DOI] [PubMed] [Google Scholar]
- 40.Arbelaez MC, Vidal C, Arba-mosquera S. Clinical outcomes of corneal vertex versus central pupil references with aberration-free ablation strategies and LASIK. Invest Ophthalmol Vis Sci. 2008;49:5287–94. doi: 10.1167/iovs.08-2176. [DOI] [PubMed] [Google Scholar]


