Abstract
The Diagnosis and classification of periodontal diseases has remained a dilemma since long. Two distinct concepts have been used to define diseases: Essentialism and Nominalism. Essentialistic concept implies the real existence of disease whereas; nominalistic concept states that the names of diseases are the convenient way of stating concisely the endpoint of a diagnostic process. It generally advances from assessment of symptoms and signs toward knowledge of causation and gives a feasible option to name the disease for which etiology is either unknown or it is too complex to access in routine clinical practice. Various classifications have been proposed by the American Academy of Periodontology (AAP) in 1986, 1989 and 1999. The AAP 1999 classification is among the most widely used classification. But this classification also has demerits which provide impediment for its use in day to day practice. Hence a classification and diagnostic system is required which can help the clinician to access the patient's need and provide a suitable treatment which is in harmony with the diagnosis for that particular case. Here is an attempt to propose a practicable classification and diagnostic system of periodontal diseases for better treatment outcome.
Keywords: Classification, periodontal disease, practicable classification
INTRODUCTION
Historically, Periodontal Diseases were named based upon the cluster of symptoms. As the clinical descriptions became more sophisticated, there started classification of diseases into separate groups, and from this came new insight into disease etiology.[1] Various forms of periodontal and mucogingival diseases have been diagnosed and discussed in the past with varying explanations.
Two distinct concepts have been used to define diseases: Essentialism and Nominalism. The essentialistic concept implies the real existence of a disease. But the concept is deceptive for quite a few fine reasons, like many diseases remain of unknown origin and if the origin is known it could either be of diverse type or complex type with the interplay of several factors, e.g. Aggressive periodontitis is the interplay of genetic and systemic factors. Nominalism, the counterpart of essentialism implies that a disease name is just a name given to a group of subjects who share a group of well-defined signs and symptoms. Ideally, a nominalistic disease definition describes a set of criteria that is fulfilled by all the persons said to have the disease, but not fulfilled by the person that are considered free from the disease.[2] Scadding et al. supported the nominalistic concept and stated that the name of diseases are a convenient way of stating concisely the endpoint of a diagnostic process that advances from assessment of symptoms and signs towards the knowledge of causation.
Naming the periodontal disease on the basis of essentialistic concept is intricate because of the fact that the periodontal diseases are of multiple origin caused due to interplay of complex genetic, local, systemic and environmental factors. Microbiologic factors have been proposed to be associated with different periodontal conditions, but studies are still needed to answer many questions like why same bacteria causes destruction at one site and no or minimum destruction at the other site. So it is difficult to diagnose periodontal diseases on the etiological basis. It is evident that diagnosing various conditions and classifying them on the basis of sound knowledge is of prime importance, merely assembling the facts is insufficient. But the present knowledge of the periodontal disease seems insufficient to satisfactorily explain the terminology used to define different periodontal conditions.[3]
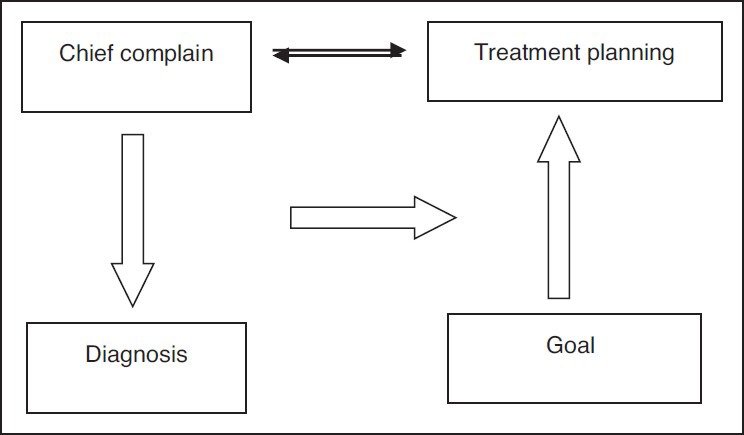
The purpose of the diagnosis is screening of the disease in an asymptomatic individual, classify a disease category, treatment planning, monitoring of treatment efficacy and disease recurrence.[4] However, the design of the previous classifications and diagnostic system is such that it creates a state of dilemma in which either chief complaint, goal of the therapy, diagnosis or treatment plan is overlooked or ignored. Generally, the diagnosis is made in response to the overall status of the periodontium and treatment is planned accordingly without considering the patient's complaint and goal of the therapy.
The Purpose of the present classification is to build a diagnostic system that is in harmony with the goal of the periodontal therapy with special emphasis on:
Eliminating the unknown and complex factors from the classification which are either complex or difficult to access in day to day practice.
Develop a harmonious relationship between chief complaint, diagnosis, treatment plan and goal of the therapy.
To avoid over exaggerated examination, which in turn decreases the trauma to inflamed periodontal tissue during initial periodontal therapy.
Origin of classification systems and their demerits
Fauchard in 1723 coined the term “Scurvy” that was for the periodontal diseases of the gums.[5] Gottlieb for the first time in 1920 classified the periodontal diseases into 4 groups Schmutz-pyorrhoae, alveolar atrophy or diffuse atrophy, paradental-pyorrhoae and occlusal trauma.[6] Schmutz-pyorrhoae is somewhat similar to the present day mild periodontitis characterized by shallow pockets and abundant local factors. Paradental-pyorrhoae depicts moderate to severe periodontitis consisting of irregular distribution of deep to moderate pockets. Alveolar atrophy comes closer to present day aggressive periodontitis and occlusal trauma is somewhat similar to present day's “trauma from occlusion” (TFO).
McCall and Box introduced the term “periodontitis” to inflammatory diseases in which all three components of the Periodontium, i.e. The gingiva, bone, and periodontal ligament were affected.[7] Orban and Weinmann coined term “periodontosis” to designate non-inflammatory disease.[8] “Periodontosis” was considered as a separate disease entity, distinctly different from periodontitis, which was considered as a sequel of gingivitis of the deeper periodontal structures, and therefore, of inflammatory origin. Butler introduced the name “Juvenile Periodontitis” instead of “periodontosis” when describing the periodontal condition of young individuals with severe periodontal bone loss.[9]
Page and Schroeder divided periodontal diseases into Pre-pubertal, Juvenile, Rapidly progressive, Adult periodontitis and Acute necrotizing ulcerative gingivo-periodontitis (ANUG/P).[10] It is important to note that with the exception of ANUG/P, the age of onset was of decisive importance. This notion was adopted in almost all subsequent classifications; moreover, there were no definite criteria behind dividing the disease except the age limitation.
American Academy of Periodontology (AAP) 1986 classification, classified periodontal diseases into juvenile periodontitis, pre-pubertal, local juvenile, generalized juvenile, adult periodontitis, ANUG/P and refractory periodontitis.[11] This classification also followed same criteria to divide them according to age limits but was complicated by adding the pre-pubertal under the juvenile periodontitis category.
AAP 1989 classification added a new category of periodontitis associated with systemic diseases and organized the early onset periodontitis into pre-pubertal, juvenile and rapidly progressing.[12] However, the author haven’t given any consistent basis for classification except for the age criteria used in the previous classification. Other disadvantages of this classification included extensive overlap between the different diagnostic categories. The quality of treatment provided previously and the patient response to therapy was required.
The first European Workshop 1993 accepted the fact that there is insufficient knowledge to separate truly different diseases (disease heterogeneity) from differences in the presentation/severity of the same disease (phenotypic variation) and stated that the existing classifications are unsatisfactory.[13] The 1993 classification proposed a simple classification distinguishing between 1. Early onset periodontitis, 2. Adult periodontitis, 3. Necrotizing periodontitis. However, there was a need to use additional secondary descriptors for defining the clinical situation. These include: Distribution within the dentition, rate of progression, response to treatment, relation to systemic diseases, microbiological, ethnic group characteristics, and other factors. But the change in the classification system has still not solved the purpose behind as there was considerable uncertainty about arbitrarily setting an upper age limit for patients with so-called early onset periodontitis. e.g., what if 21 year male has typical incisor molar pattern, so the age was of decisive importance. Further the rate of progression in the past and response to the therapy was also required for secondary description.
AAP 1999 classification, proposed a new classification and was widely accepted for many reasons such as an improvement with regard to the category of gingival diseases.[14] Adult periodontitis was renamed as “chronic periodontitis” on the basis of speculation that slowly progressive disease could be present at any age, i.e. in adults as well as in adolescents. There was the elimination of separate disease category for “refractory periodontitis.” The elucidation of the designation “periodontitis as a manifestation of systemic disease” was given. A list of diseases which are commonly manifested in the oral cavity was given. There was the addition of new categories like abscess, endodontic-periodontic lesion, development and acquired deformity which were not explained in the previous classifications. But this classification also falls short to answer many issues. The term “chronic” and “aggressive” periodontitis arose the need for the rate of progression of the disease and how much severe disease could be categorized as “aggressive periodontitis.” Primary criteria given by Lang for aggressive periodontitis need a detailed systemic investigation, familial history and rate of progression, which are difficult to access in clinical practices.
Further, the studies related to the rate of disease progression seem to be insufficient. There are many questions, which remain unanswered like why Diabetes mellitus has not been given place for the systemic condition modifying the periodontal disease. There is no description about environmental factors affecting the periodontitis and gingivitis, when there are so many proven studies available for them, e.g., smoking. Moreover, the entities like “color of gingiva” and “gingival enlargements” are included in periodontal disease category. There is no description about what degree of increase in size of gingiva could be designated as gingival enlargement?
In case of multiple diagnoses, as is the case most of the times, which diagnosis is to be put first? Patient may not come with the complaint which actually requires the treatment before the present complaint, so a disparity develop between the chief complain, diagnosis and treatment plan. Further there are situations, where the etiology of a disease is unknown; in those conditions the relation between diagnosis and the treatment plan creates a state of perplexity.
After the review of the previous classifications, it can be concluded that none of the classification comes near to the idealistic classification. AAP 1999 classification is the most widely accepted classification and used for most of research and academic purposes. Vander valden 2005 classification made an attempt to simplify the terminology but failed to reach the realistic goal, the classification still deals with same problems, which were existing in the previous classification systems. Armitage comment,[3] “The present knowledge of the periodontal disease seems to be insufficient to classify them on the basis of host/infection paradigm” still stands true. Despite of latest advancements in the research, our treatment modalities are based on the conventional concepts, so sometimes a state of confusion arises between the patient's chief complaint, diagnosis and the treatment plan.
Development of new classification system
It is of utmost importance to understand that for a successful treatment, there should be a harmonious relationship between the patient's chief complaint, diagnosis, goal of therapy and treatment plan. Goal of therapy should be realistic; an overenthusiastic goal is bound to be a failure.
Concept of primary and secondary diagnosis
Diagnosis is the basic foundation for the treatment plan. However, the present classification gives a long list of periodontal diseases, which is difficult to apply in day to day practice. A state of confusion arises when there are multiple diagnosis for a case as which one to be put first? There are situations when etiology of the complaint remains obscure, in those cases a disharmony develops between diagnosis and treatment. e.g., A patient come with a complain of pain in upper right first molar, but the clinician does not find any relevant cause for the pain, in those cases most times the diagnosis is based on the overall status of periodontal tissue rather than the complaint of the patient and hence a disparity develops between the complaint of the patient and treatment plan. So the concept of primary and secondary diagnosis comes into the picture.
Primary diagnosis
It is a diagnosis made in response to the patient's chief complaint to justify patient's immediate complaint and suggests the treatment plan to achieve the immediate goal of the therapy [Figure 1].
Figure 1.
Sequence of Periodontal Treatment
Secondary diagnosis
It is a diagnosis which reveals the patients actual periodontal health status irrespective of patient's chief complaint and suggests a treatment plan to achieve the ultimate, ideal or pragmatic goal.
It is important to note here that both the primary and secondary diagnosis can be same, when the patient's chief complaint reflects the overall status of the oral cavity. There can be more than one diagnosis in each category. There may not be any primary diagnosis if patients complaint is vague or if the main etiology is obscure, in that case secondary diagnosis will be the only diagnosis but cannot be called as the primary diagnosis.
Depending upon the goal of the therapy either of the diagnosis can be used and fulfilled.
Goals of the periodontal therapy
The goal of treatment should be pre decided based on the patient's expectation and prognosis for the case.
Immediate goal
The immediate goal of therapy is to prevent, arrest, control, or eliminate the periodontal disease.
Ideal goal: The ideal goal aims to promote healing through regeneration of the lost form, function, esthetics, and comfort.
Pragmatic goal: When the ideal goal cannot be achieved, the pragmatic goal of therapy would be to repair the damage resulting from the disease.
Ultimate goal: Finally, the ultimate goal of therapy is to sustain the masticatory apparatus-especially teeth, or their analogues, in the state of health.[15]
How to start clinical examination
Assessment of gingival status
A gingival examination should begin with the assessment of the gingival inflammation. The Color of the gingiva, edema, suppuration and bleeding on probing (BOP) are the parameters which help in the assessment of the gingival inflammation. Color of the gingiva has the least positive predictive value and BOP has the highest positive predictive value.[16]
Assessment of periodontal status
Periodontal destruction should be assessed by probing depth, clinical attachment loss (CAL) and radiographs. BOP can be used as a parameter to access the activity or inactivity of the disease. Finding the etiology should be a secondary requisite which can be achieved by mean of microbial culture, biochemical methods and immunological assays.
At this stage, probing depth is inaccurate because the measurements are recorded on the inflamed tissue. The Accurate scores can be obtained only after the reduction of inflammation. So probing should be done grossly, to assess the periodontal attachment loss or in contrary radiographs can be used. Measurement of the CAL at this level should not be tried.
Presence of any abscess or sinus opening, carious lesion, wasting disease, root stumps and mobility should be accessed. Radiological investigation: Intraoral periapical (IOPA) and Orthopantogram OPG (if required) and routine blood investigation: Clotting time, bleeding time, hemoglobin percentage and blood sugar etc. should be carried out as and when needed.
After scaling and root planning: (base line examination) measurement of recession, mobility (re-evaluate), CAL, Pocket depth, and Edema should be performed. There may be a need for the reassessment of radiological, hematological and microbiological test. At this stage, one should make secondary diagnosis and treatment plan accordingly.
List of diagnosis
Gingival diseases
Gingival diseases are mostly chronic and generalized in nature so rather than calling them as chronic gingivitis the term plaque induced gingival disease is more appropriate as it describes the nature of the disease as well. Further, if the conditions which modify the gingival disease [Table 1] are also present, they have to be mentioned in the diagnosis. Gingival conditions, which are not primarily induced by plaque or are a manifestation of the systemic conditions should be put in the category of non-plaque induced gingival disease [Table 2]. In this way, gingival conditions can be put under either of the under mentioned categories
Table 1.
Systemic conditions affecting the gingivitis
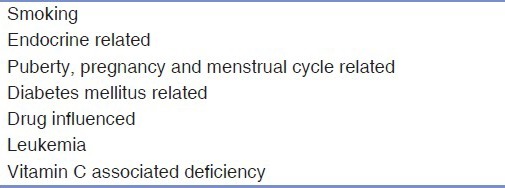
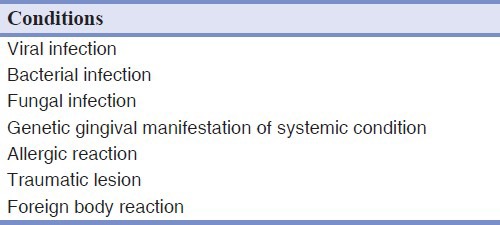
Table 2.
Non-plaque induced gingival destruction
Plaque induced gingival disease.
Plaque induced gingival disease modified by systemic factors.
Non-plaque induced gingival disease
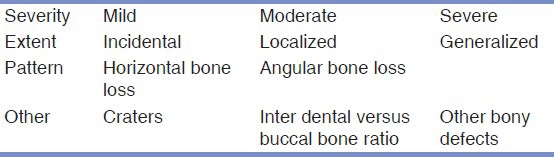
Periodontal diseases
The disease under the term “chronic periodontitis” is put under the category of “Plaque induced periodontal destruction” with secondary description [Table 3] to explain extent, pattern and other characteristics. Severity of the periodontal disease can be divided into mild (bone loss less than 1/3rd of the root surface), moderate (bone loss more than 1/3rd and less than 2/3rd of the root surface), sever (bone loss more than 2/3rd of the root surface). Extent of the disease can be incidental (1 tooth affected), localized (2-7 teeth affected), generalized (More than 7 teeth affected) The periods of activity/inactivity of the periodontal diseases should be accessed on the basis of signs of inflammation. CAL over a period of time should be used as a parameter to monitor the periodontal tissue stability in the maintenance phase.[17]
Table 3.
Secondary description for periodontal disease
Systemic diseases and conditions like diabetes mellitus, bruxism/environmental factors like smoking, stress affecting periodontal destruction, if present have to be mentioned in a separate category “Plaque induced periodontal destruction influenced by systemic disease/condition/environmental factor.” A separate disease category should be assigned for the disease causing periodontal destruction irrespective of the presence or absence of plaque. Such disease should be put under the category of periodontal destruction as a manifestation of systemic disease [Table 4]. In most of the older classifications recession is considered as a finding rather than diagnosis. But we consider recession as a separate entity with a definite line of treatment. Further two variants of recession can be separated based on the etiology, one which is due to inflammation and starts at the Interdental area and the other one which starts on the facial and lingual surface due to tooth brush trauma. Post-scaling sensitivity, which is a common phenomenon and renders the patient to move from one dentist to other, such a problem should be put under a category “Iatrogenic cemental tear” although the term Iatrogenic mimic as if there is a part of dentist in it but from the past evidences it is clear that some amount of cemental tear is always associated with scaling and root planning and hence justify the terminology. Halitosis is a very common problem with varying etiology, so a list of factors associated with halitosis is mentioned [Table 5]. So the diagnosis of halitosis can be written as follows: Halitosis associated with suppurative periodontitis, halitosis associated with tooth related factors, halitosis associated with diabetes, halitosis of Idiopathic factors. Periodontal destruction due to ongoing orthodontic treatment or faulty prosthesis/endodontic treatment comes under a category named as “compromised periodontium of iatrogenic origin.”
Table 4.
Systemic factors manifested in the oral cavity
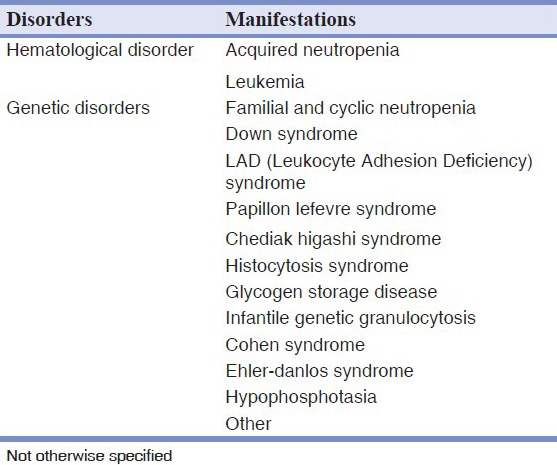
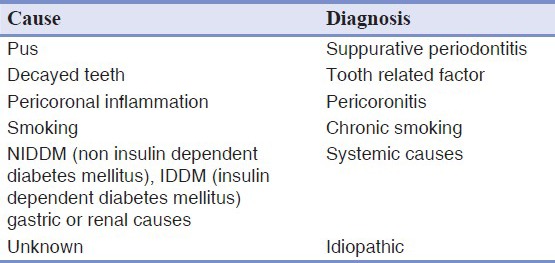
Table 5.
Descriptions for halitosis
None of the previous classification has discussed about implant related problems. This classification provides a simple yet effective classification for implant related problems also. The problems related to implant can be divided into 3 categories: “Ailing implant,” which has soft tissue problems around the implant without any marked mobility/loss of function. “Failing implant,” which has the increasing mobility over a period of time, but implant being still in function. “Failed implant” is that, having a marked mobility and loss of function.
Etiology and diagnosis of the aggressive periodontitis is complex and provide diagnostic problems in clinical setup, moreover, there are cases which neither set in the category of chronic periodontitis nor in aggressive periodontitis, so a special category of “periodontal disease of complex idiopathic factors” is introduced, where patients are having periodontal disease of undiagnosed syndrome/familial/genetic/immunological/systemic variation. Necrotizing periodontal disease. Disease categories such as abscesses of periodontium, periodontal disease associated with endodontic lesions, mucogingival, acquired or developmental disorders, TFO kept same as in AAP 1999 classification.
In this way, periodontal diseases can be put under either of the under mentioned categories.
Plaque induced periodontal destruction
Plaque induced periodontal destruction influenced by systemic disease/condition/environmental factor.
Periodontal destruction as a manifestation of systemic disease.
Necrotizing periodontal disease.
Abscesses of Periodontium.
Periodontal disease associated with endodontic lesions
-
Recession
-
a)Inflammatory (which begins in the Interdental area)
-
b)Non-inflammatory (from tooth brush trauma, mostly facial surface is affected).
-
a)
Mucogingival problem (inadequate width/volume of attached gingiva, aberrant frenum, shallow vestibule and gingival color).
Iatrogenic cemental tear
Acquired or developmental disorders.
-
TFO: Primary TFO
Secondary TFO
Compromised Periodontium of iatrogenic origin (due to orthodontic therapy).
Halitosis (secondary description).
Implant related problems: Ailing implant, Failing implant, Failed implant
Endodontic or prosthodontic need with respective area.
Periodontal disease of complex idiopathic factors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Temple LK, McLeod RS, Gallinger S, Wright JG. Essays on science and society. Defining disease in the genomics era. Science. 2001;293:807–8. doi: 10.1126/science.1062938. [DOI] [PubMed] [Google Scholar]
- 2.Wulff HR, Gotzsche PC. Evidence-based Clinical Decision Making. 3rd ed. Oxford: Blackwell Science; 2000. The disease classification. Rational Diagnosis and Treatment; pp. 39–62. [Google Scholar]
- 3.van der Velden U. Purpose and problems of periodontal disease classification. Periodontol 2000. 2005;39:13–21. doi: 10.1111/j.1600-0757.2005.00127.x. [DOI] [PubMed] [Google Scholar]
- 4.Mombelli A. Critical issues in periodontal diagnosis. Periodontol 2000. 2005;39:9–12. doi: 10.1111/j.1600-0757.2005.00126.x. [DOI] [PubMed] [Google Scholar]
- 5.Gold SI. Periodontics. The past. Part (I). Early sources. J Clin Periodontol. 1985;12:79–97. doi: 10.1111/j.1600-051x.1985.tb01367.x. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb B. The formation of the pocket: Diffuse atrophy of alveolar bone. J Am Dent Assoc. 1928;15:462–76. [Google Scholar]
- 7.McCall JO, Box HK. The pathology and diagnosis of the basic lesions of chronic periodontitis. J Am Dent Assoc. 1925;12:1300–9. [Google Scholar]
- 8.Orban B, Weinmann JP. Diffuse atrophy of the alveolar bone. J Periodontol. 1942;13:31–45. [Google Scholar]
- 9.Butler JH. A familial pattern of juvenile periodontitis (periodontosis) J Periodontol. 1969;40:115–8. doi: 10.1902/jop.1969.40.2.115. [DOI] [PubMed] [Google Scholar]
- 10.Page RC, Schroeder HE. Basel: Karger; 1982. Periodontitis in Man and Other Animals. A Comparative Review. [Google Scholar]
- 11.Chicago: The American Academy of Periodontology; 1989. The American Academy of Periodontology. Proceedings of the World Workshop in Clinical Periodontics; pp. I/23–4. [Google Scholar]
- 12.Princeton NJ. Periodontal diagnosis and diagnostic aids. Proceedings of the world workshop in clinical periodontics. Consensus report, discussion section I. Am Acad Periodontol. 1989;2:13–20. [Google Scholar]
- 13.Tonetti MS. Etiology and pathogenesis. In: Lang NP, Karring T, editors. Proceedings of the 1st European Workshop on Periodontology. Chicago: Quintessence Books; 1994. pp. 54–89. [Google Scholar]
- 14.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 15.Consensus Report Discussion Section 11, Proceedings of the World Workshop in Clinical Periodontics. 1989;11:13–20. [Google Scholar]
- 16.Armitage GC. Periodontal diseases: Diagnosis. J Periodontol Ann. 1996;1:37–215. doi: 10.1902/annals.1996.1.1.37. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Periodontology. Parameter on aggressive periodontitis. J Periodontol. 2000;71:767–9. doi: 10.1902/jop.2000.71.5-S.867. [DOI] [PubMed] [Google Scholar]


