Abstract
Background:
The success of combined periodontal and orthodontic approach in the treatment of aggressive periodontitis patients with the pathologic extruded anterior teeth is a main concern and stability of the treatment results is an important factor to evaluate the treatment. The present study investigated the periodontal parameters at the end of the orthodontic treatment in patients with the aggressive periodontitis.
Materials and Methods:
Eight patients with an aggressive periodontal disease, extruded maxillary incisors, infrabony defects and probing depth of ≥5 mm were enrolled in this clinical trial (before, after). After periodontal therapy, orthodontic treatment was carried out for intrusion and alignment of teeth. Plaque index (PI), probing pocket depth (PPD), distance between incisal edge and interdental papilla, root length (RL), and defect dimensions (depth and width) were examined at the end of treatment and three as well as 6 months afterward. The data were subjected to repeated measure ANOVA test. P < 0.05 was considered as significant.
Results:
There was statistically significant decrease in PPD, PI, and depth of the defects during T0, T3 and T6 (P < 0.05). No significant differences were observed in the RL and distance between incisal edge and interdental papilla (P = 0.95). Furthermore, width of the defects demonstrated significant decrease up to T3 (P = 0.042) while no significant changes from 3 months to 6 months were noted (P = 0.59).
Conclusion:
The results showed that combined periodontal and orthodontic approach would be a successful treatment with acceptable stability in the case of regular follow-up visits and controlled oral hygiene habits.
Keywords: Aggressive periodontitis, orthodontic treatment, periodontal defect
INTRODUCTION
Today, more demands have been observed to receive orthodontic treatments among different age groups in all societies.[1] The efficiency and success of orthodontic treatment depends upon the response of the host periodontal tissues. Orthodontic tooth movement involves reconstruction of the alveolar bone while the movement is associated with the physiological processes of cell activity in the periodontal connective tissue and osteoclast-osteoblast activity in the alveolar bone. Due to the complexity of esthetic and functional rehabilitations, the adjunction of periodontal and orthodontic treatments is necessitated to achieve the treatment goals.[2]
Orthodontic therapy using fixed or removable appliances can result in the different side effects such as plaque formation or caries incidence.[3,4] Furthermore, the bacterial population increases in the plaque-retentive sites impairing the mechanical plaque removal. These changes can cause a qualitative bacterial shift, with a higher incidence of periodontal pathogens such as Actinobacilus actinomycetemcomitans and Porphyromonas gingivalis.[5] Orthodontic treatment affects the periodontium by facilitating plaque-associated gingivitis, contributing to gingival enlargement, an increase in the pocket probing depth (PPD), and bleeding on probing.[6] All the aforementioned ideas call for a strict oral hygiene during the orthodontic treatments as well as in the years following the treatment.
Due to the risk of permanent tissue injuries and decreased periodontal support, orthodontic tooth movement in patients with untreated periodontal disease is contraindicated. Periodontal treatments such as scaling, root planing, and the removal of deep pockets must be performed before starting orthodontic treatment, as deep pockets can transmit microbial plaque from supragingival to the subgingival locations as well as attachment loss and angular bone defect developments.[7,8]
Localized aggressive periodontitis, a form of severe periodontal disease, is associated with the connective tissue attachment loss as well as infrabony pockets and vertical bone defects in some specific areas of the dental arch, e.g., first molars and incisors, in the earlier ages.[9,10]
In 30-50% of the patients infected with the moderate-severe forms of the disease, pathologic migration occurs with the attachment loss and severe bone resorptions, clinically apparent as the elongation, diastema, rotation and labial inclination of the central teeth.[11,12]
Regenerative treatments are successfully used to manage the vertical bone defects; however, in the case of tooth migration from its original location, ideal esthetics along with the interdental papillae (IPD) reconstructions doesn’t achieve even with the successful regenerative approaches requiring adjunctive orthodontic treatments.[13]
The combined periodontal treatments and intrusion of the anterior elongated and translated teeth together with the controlled oral hygiene is the best treatment plan for the correction of the teeth relationships in the aggressive periodontitis.[14]
Furthermore, tooth orthodontic vertical movement can resolve some bony defects in the periodontal patients while this movement eliminates the need to bone respective surgeries.[2]
Because of the importance of the stability of periodontal therapies, predetermined maintenance follow-up visits are required in patients.[15] Oral hygiene instructions and 3-6 month visits as well as assessment of the sulcus depth, tooth mobility, gingival recession, bone surface examinations and root planning by the dental hygienist are recommended for these purposes.
The present study investigated the periodontal parameters at the end of orthodontic treatment in patients with aggressive periodontitis.
MATERIALS AND METHODS
This non control before-after clinical trial was approved by the Ethics Committee of Tehran University of Medical Sciences, Dental School. The examinations were performed with the understanding and written consent of each patient. The subjects consisted of eight patients (seven female and one male with the mean age of 30 years old) who had been referred for the treatment of the aggressive periodontitis with the history of teeth extrusion and orthodontic treatment. All patients presented the probing depth of ≥5 mm, infrabony defects, 1 mm or more extrusion compared to the similar tooth in the dental arch, while they were all cooperative with the follow-up examinations (Plaque index [PI] of less than 15%). In the case of the systemic disease involvement, drug consumption in the past 3 months, smoking habits, inability to afford orthodontic treatment expense, or not participating in the follow-up examinations, the patients were excluded from the study.
All patients showed clinical and radiographic manifestations of the aggressive periodontitis. They were all received scaling and root planning in regular timings as well as open full-thickness flap was made by a sulcular incision to remove the inner pocket walls and inflammation in consequent. The patients received oral hygiene instructions before orthodontic treatments beginning while they were asked to brush their teeth twice a day.
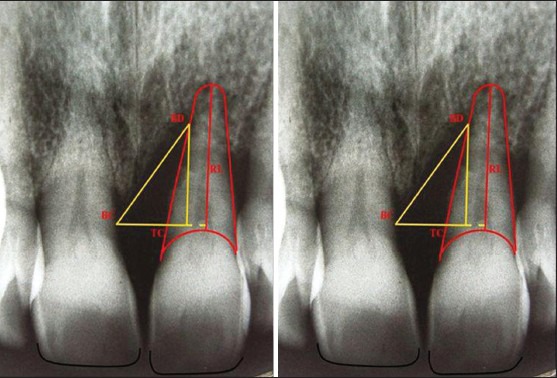
After stability of the periodontal status and reduction of the PI to 15% or less, when the patients were all satisfied to cooperate with the follow-up examinations, the fixed orthodontic treatment was started using full arch approach, intrusion step up wire technique and realignment of the central teeth. The loads were applied equally to 10-15 g in each tooth (checked up with Correx™ measuring device, HAAG-STREIT Holding AG) regarding their specific periodontal situations. For preventing the anchorage loss we extend the posterior anchorage to full arch approach, serving from transpalatal arch and the appliances were adjusted once in each 4 weeks. The surface root planning and repeated oral hygiene instructions were done once in each 3 months. The complete orthodontic treatment lasted from 10 months to 2 years specific to each patient [Figure 1]. Afterward, the patients entered retention phase of the treatment. At the treatment end, the fixed appliances were removed and the fixed retainers (Braided stainless steel, 0/38 mm, Dentaflex®, Germany) were used in the maxillae and mandibles. The patients received oral hygiene instructions again.
Figure 1.

(a, b) Frontal and lateral view of extruded right maxillary central related to bone loss in a patient affected by localized aggressive periodontitis (pathologic movement) after periodontal treatment and just before starting of orthodontic force, (c, d) 6 month after fixed orthodontic treatment utilizing full arch technique and step up wire intended for intrusion of anterior extruded tooth, (e) end of the orthodontic force treatment
The O’Leary PI was calculated using the disclosing tablets on the mesial, distal, buccal and lingual surfaces.
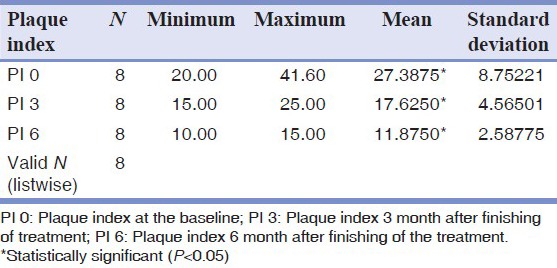
PPD was also determined on the six points of Distolingual (DL), Linqual (L), Mesio Linqual (ML), Distobuccal (DB), Buccal (B) and MesioBuaccal (MB) by the William's probe in mm. Furthermore, the distance between the papillary tips to the incisal edge of the teeth was measured to indicate the papillary height compared to the adjacent teeth using a graduated probe in mm. Then, periapical radiographies were obtained by a long cone parallel approach. In order to achieve a correct film position, adequate reliability and prevention of the higher exposures, a film holder of the putty silicone index was fabricated for each patient from his/her own occlusal position. The film was located parallel to the teeth long axis and perpendicular to the beam with the dose of 40 Kvp. On the radiographic image, a line was drawn perpendicular to the root (Tooth Crest point;TC) from the most upper area of the Bone Crest (BC) using a pencil and Negatoscope. The distance between TC and BC suggested the Defect Width (DW). Again, a line was drawn from BC to the most extreme area of the bone defect. The distance between TC and Bone Defect (BD) showed the Defect Depth (DD). For the measurement of the Root Length (RL), a line was traced from the lowest regions of the root to the lowest regions of Cementoenamel Junction (CEJ) [Figure 2].
Figure 2.
The most upper area of the Bone Crest determined as BC) point. The point that created from a line that was drawn perpendicular to the root from BC point determined as Tooth Crest or (TC) point. The point that created from a line that was drawn from the BC point to the most extreme area of the Bone Defect determined as BD point. The measurement from the lowest regions of the root to the lowest regions of cementoenamel junctionCEJ of tooth determined as root length
The measurements were repeated on the three and 6 months after the end of the orthodontic treatments while the data were statistically analyzed using the repeated measure ANOVA and Bonferroni post hoc tests on 0, 3 and 6 months following orthodontic treatments. P < 0.05 was considered as significant.
RESULTS
The mean and standard deviation of PI scores was 27.39 ± 8.75% at the end of the orthodontic treatment (T0) decreasing to 17.63 ± 4.57% at the 3rd month (T3) and 11.88 ± 2.59% at the 6th month following the treatment (T6). The changes of plaque scores were statistically significant during the studied time. Furthermore, the PI changes found between the end of the treatment (T0) compared to the 3rd (P = 0.032) and 6th month after the treatment, was also significant (P = 0.022). The differences found between the 3rd month and 6th month were also statistically significant (P = 0.022) [Table 1].
Table 1.
Mean and standard deviation of plaque index
The mean and standard deviation of PPD were also 1.93 ± 0.9 mm, 1.79 ± 0.87 mm and 1.7 ± 0.85 mm at T0, T3, and T6 respectively with overall significant changes. Statistically, significant differences were also found between PPD measured at T0 and T3 (P = 0.042), T0 and T6 (P = 0.039), and T3 and T6 (P = 0.047) [Table 2].
Table 2.
Mean and standard deviation of probing depth (in mm)
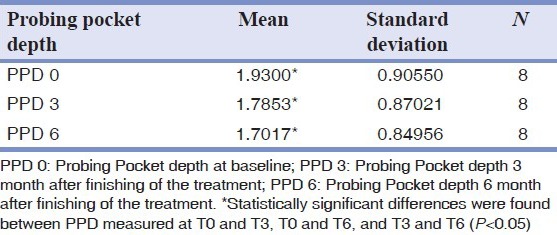
The mean distance of the incisal edge to the IPD was 5.97 ± 0.44 mm at T0, 5.99 ± 0.42 mm at T3 and 5.97 ± 0.33 mm at T6 with no statistically significant differences (P = 0.932) [Table 3].
Table 3.
Mean and standard deviation of the distance between top of the papilla and incisal edge (in mm)
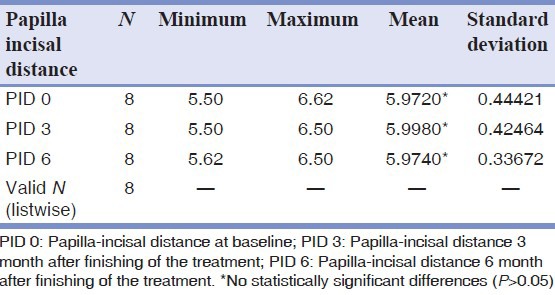
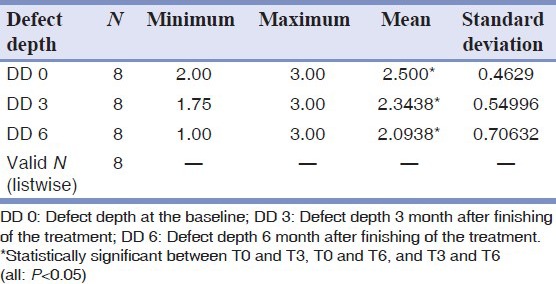
Furthermore, the mean DD in the patients was 2.5 ± 0.46 mm at T0, 2.34 ± 0.54 mm at T3 and 2.09 ± 0.7 mm at T6. The decrease measured in the DD was statistically significant between T0 and T3 (P = 0.0432), T0 and T6 (P = 0.039), and T3 and T6 (P = 0.035) [Table 4].
Table 4.
Mean and standard deviation of the defect depth (in mm)
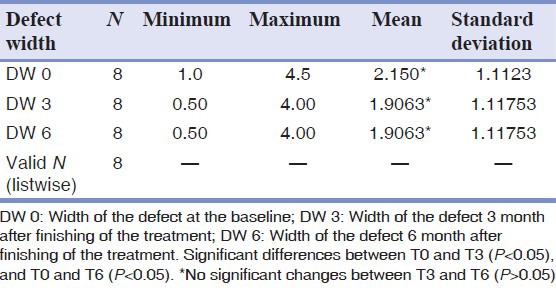
There was also significant differences between T0 and T3 (P = 0.042), and T0 and T6 (P = 0.039) regarding the infrabony DW (2.15 ± 1.11 mm, 1.9 ± 1.11 mm and 1.9 ± 1.11 mm respectively) while no significant changes were observed between T3 and T6 (P = 0.59) [Table 5].
Table 5.
Mean and standard deviation of the defect width (in mm)
The RL was remained constant during the 6 months and no statistically significant differences were found between the times patients examined in this regard (P = 0.95).
DISCUSSION
Regenerative treatments have been used in the aggressive periodontitis patients involved with infrabony defects experiencing tooth pathologic migrations. As mere periodontal therapy is unable to improve destructions occurred because of the pathologic occlusion, especially those resulted for the interdental papillary elimination, and orthodontic therapies are recommended for the intrusion and alignment of the involved teeth.[2,11,13] The stability of the treatment results are also important due to the severe bone destructions in these patient while most studies did not consider the issue in their short or long term assessments.[16,17,22] Furthermore, patients may consider the appliance removal as the treatment final step without any attempt to cooperate with the maintenance phase. In the present study, periodontal parameters were examined at the maintenance phase of the treatment and reorganization of periodontal ligaments after the removal of orthodontic appliances.
Some studies reported adverse consequences for the orthodontic treatment of aggressive periodontitis patients with the history of anterior teeth extrusion such as inability to adequate mechanical plaque control after the treatment,[18] the possible conversion of supra-gingival plaque to sub-gingival plaque 8), destruction of the periodontal tissues following orthodontic treatment,[16,19] and increased tissue destructions in the orthodontic patients.[20] Hence, excellent plaque control with the regular follow-up visits of 3-6 months and use of simply applied light and continuous orthodontic forces are suggested for the successful treatment of the patients with the vertical periodontal defects.
In the present study, fixed orthodontic retainers were used for the patients, which have been previously shown to result in the controlled movements in three plans enabling light and continuous loads application, necessary to achieve bone regenerations.[20] These retainers make physiologic tooth movements possible and lead to the improved periodontal health and bone remodeling by controlling the unnecessary movements.[21] Furthermore, the device does not require patient's cooperation being ideal for their easiness and esthetic demands.[20,22,23] Some case, reports showed the decreased probing depth, improved defect dimensions, bone gain, acceptable C/R ratio, good periodontal health, good esthetics, and function following combination therapies for aggressive periodontitis patients.[24] As the treatment comprises both orthodontic and periodontal approaches, the maintenance and stability of both treatments must be taken into consideration. Although, some investigations stressed the importance of the treatment stability and maintenance phase, no study examined the treatment success in the long term as far as the authors know.
PI of the patients decreased constantly during the 6 month period, which may be due to the simplified oral hygiene habits after appliance removal and teeth realignment. These findings are similarly reported by Re, et al.,[25] Prior to the appliance removal, the efficacy of oral hygiene habits is limited,[16,20] which justify the great differences of PI between T0 and T3 and T6. Furthermore, the decreased plaque accumulation between T3 and T6 can be related to the use of modified bass technique in tooth brushing, which is the most effective mechanical method in the plaque removal.[5,26] It is obvious that patients will be motivated observing the orthodontic treatment results with a great effort to maintain these results.
The significantly decreased probing depth during T0, T3, and T4 was also associated with the appliance removal or the use of new modified brushing method; both leading to the simplified oral hygiene habits, effective plaque removal, decreased pathogen population or gingival inflammation improvements.[26] Direct relationships between PI and probing depth coincides with the studies reporting decreased probing depth and attachment gain after the reduced PI and inflammation.[27]
Significant reductions in the probing depth were also reported when routine treatment modalities of the surgery or antibiotic therapies have been used for aggressive periodontitis patients.[28] These studies showed reductions of the inflammation or pathogen populations as a prerequisite for the decreased probing depth as observed in the present study. Zhu, et al., showed all under-40-aged aggressive periodontitis patients experienced probing depth reductions after receiving intrusion treatment,[29] although, pocket depth remained stable between treatment end time and 1 year afterwards as shown by Re, et al.,[25] According to Melsen, et al., the decreased probing depth is a result of new connective tissue formation after increased periodontal ligament cellular activity and closure of the formative cells to the tooth surface.[30] Passanzaei interpreted the increased new connective tissue formation after successful root planning in the orthodontic/periodontic combination therapy of aggressive periodontitis as a result of the roots’ tendency to the mesenchymal cells compared to the epithelium cells.[31] However, some reports denied the role of new connective tissue after orthodontic treatments stating long junction epithelium as a reason for the decreased probing depth.[32]
Although, showing the probing depth to be reduced, our results failed to discriminate between new connective tissue and long junctional epithelium as histopathological specimens were required for this purpose, which was not possible in the studied subjects (However, considering the results reported by Passanzaei and decreased radiographic dimensions of the bone defects; new connective tissue possibly had been formed.[31]
No significant differences were observed regarding the distance between tooth incisal edge to the interdental gingival margins during T0, T3, and T6 time intervals. The tooth stable relationships with the adjacent teeth, the stable orthodontic treatment results and no recessions in the interdental gingival tissue may be responsible in this regards. As IPD adheres to the underlying bone surface, the stable periodontal tissue and underlying bone prognosis is made as there is no recession in the interdental gingival tissues.[33] Orthodontic treatments were effective to reconstruct IPD calling for a way to preserve the results in the long term period.[20] Similar to our findings, Re, et al., concluded no gingival recession, no appearance change as well as periodontal improvements after 1-years follow-up in aggressive periodontitis patients underwent intrusion therapy and bonded retainers.[25] However, Levin, et al., regarded fixed retainers as a cause for gingival recessions due to the limited oral hygiene control and 50% failures were reported for the fixed retainers during 4-40 month post-treatment observations.[34]
The RLs were remained stable at T0, T3, and T6 as determined by the radiographic images suggesting lack of any root recession and availability of the standardized radiographic images. It has declared no root recession when intruding the tooth toward the infrabony defects being correlated with the applying light and continuous loads similarly to our results.[20] Intrusion apparently focuses loads in the apex, PDL region and surrounding bone, although, with the lower values applying toward a bony defect; ischemic necrosis risk would be reduced, PDL cells be affected and their turn over would be increased.[20] On the contrary, some investigations reported signs of root recessions during the orthodontic active phase as a natural mechanism of intrusive forces which are related to the conical characteristic of the anterior teeth and force concentration in the apex. Ischemic necrosis of PDL and miner eliminations in the precementum, cementoblasts, and dentinoclasts’ colonization are the consequences of the mentioned mechanism.[35]
In the present study, significant reductions were found between the paired follow-up times after the treatment concerning DD and width; although, the width differences were insignificant between T3 and T6. The increased bone formation following orthodontic tooth movements toward infrabony defects are justified by different mechanisms such as PDL tissue tension and its role as a natural barrier against epithelial cells penetration into the defect (Guided Bone Regeneration (GBR) imitation),[20] the increased bone formations by the periodontal ligament cells,[22,36,37] the effect of orthodontic mechanical forces as the first messenger as well as its effect on the bone coupling[37] jiggling,[38] reactivation of the bone formation and osteogenic properties of the remaining soft tissue in the primary defect location.[30] The defect dimensions was examined when the orthodontic treatment had been finished in which bone complete mineralization did not occur yet, in turn, the reduced defect dimensions may be related to the gradual mineralization of the bone during orthodontic treatment phase as shown by the radiographic imagine.[20] Furthermore, prevention of the jiggling phenomenon,[38] followed by the tooth splint with the fixed retainer could reduce inflammation and pathogen agents that is important in the formation and remineralization of the new bone. In addition, orthodontic forces may result in the increased width of periodontal ligament space with the reduced bone remodeling. After the orthodontic treatment and force elimination, PDL returns to its normal values gradually. Therefore, the decreased radiographic dimensions of the defects are influenced by the changes occurred in periodontal ligament spaces.[39,40]
The stable radiographic width of the defects at T3 and T6 time intervals can be interpreted in terms of completed bone mineralization at T3, so that, as shown by radiographic images, PDL would have returned to its normal values at T3.
However, the authors believe; further studies are necessary to measure clinical parameters with a constant reference point in a larger sample size to facilitate a more accurate long-term evaluation of gingival changes.
CONCLUSION
With the limitations of this study, the stable treatment results can be obtained with the regular follow-up visits and controlled oral hygiene habits in patient with aggressive peridontitis that are treated with a combination of periodontal and orthodontic treatment option.
ACKNOWLEDGMENTS
This study was partly supported by the Dental Research Center, Tehran University of Medical Sciences. The authors would like to thanks Dr. Mohammad Javad Kharazifard for statistical testing and for his contributions to the study.
Footnotes
Source of Support: Dental Research Center, Tehran University of Medical Sciences,
Conflict of Interest: None declared.
REFERENCES
- 1.Scott P, Fleming P, DiBiase A. An update in adult orthodontics. (431-4).Dent Update. 2007;34:427–8. doi: 10.12968/denu.2007.34.7.427. 436. [DOI] [PubMed] [Google Scholar]
- 2.Newmann MG, Takei HH, Klokkevold PR, Carranza FA. Clinical Periodontology. 10th ed. Ch. 57. St. Louis: WB Saunders Co; 2006. pp. 856–71. [Google Scholar]
- 3.Ogaard B. Prevalence of white spot lesions in 19-year-olds: A study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–7. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 4.Hägg U, Kaveewatcharanont P, Samaranayake YH, Samaranayake LP. The effect of fixed orthodontic appliances on the oral carriage of Candida species and Enterobacteriaceae. Eur J Orthod. 2004;26:623–9. doi: 10.1093/ejo/26.6.623. [DOI] [PubMed] [Google Scholar]
- 5.Paolantonio M, Pedrazzoli V, di Murro C, di Placido G, Picciani C, Catamo G, et al. Clinical significance of Actinobacillus actinomycetemcomitans in young individuals during orthodontic treatment. A 3-year longitudinal study. J Clin Periodontol. 1997;24:610–7. doi: 10.1111/j.1600-051x.1997.tb00237.x. [DOI] [PubMed] [Google Scholar]
- 6.Ong MM, Wang HL. Periodontic and orthodontic treatment in adults. Am J Orthod Dentofacial Orthop. 2002;122:420–8. doi: 10.1067/mod.2002.126597. [DOI] [PubMed] [Google Scholar]
- 7.Boyd RL, Leggott PJ, Quinn RS, Eakle WS, Chambers D. Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. Am J Orthod Dentofacial Orthop. 1989;96:191–8. doi: 10.1016/0889-5406(89)90455-1. [DOI] [PubMed] [Google Scholar]
- 8.Behfarnia P, Birang R, Andalib AR, Asadi S. Comparative evaluation of IFNγ, IL4 and IL17 cytokines in healthy gingiva and moderate to advanced chronic periodontitis. Dent Res J (Isfahan) 2010;7:45–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Chopra R, Patil SR, Mathur S. Comparison of cardiovascular disease risk in two main forms of periodontitis. Dent Res J (Isfahan) 2012;9:74–9. doi: 10.4103/1735-3327.92953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newmann MG, Takei HH, Klokkevold PR, Carranza FA. 10th ed. Ch. 33. St. Louis: WB Saunders Co; 2006. Clinical Periodontology; pp. 506–13. [Google Scholar]
- 11.Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol. 1997;68:967–72. doi: 10.1902/jop.1997.68.10.967. [DOI] [PubMed] [Google Scholar]
- 12.Martinez-Canut P, Carrasquer A, Magán R, Lorca A. A study on factors associated with pathologic tooth migration. J Clin Periodontol. 1997;24:492–7. doi: 10.1111/j.1600-051x.1997.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 13.Tonetti MS, Cortellini P. Case selection and treatment considerations of guided tissue regeneration in deep intrabony defects. Curr Opin Periodontol. 1997;4:82–8. [PubMed] [Google Scholar]
- 14.Musich DR. Assessment and description of the treatment needs of adult patients evaluated for orthodontic therapy. II. Characteristics of the dual provider group. Int J Adult Orthodon Orthognath Surg. 1986;1:101–17. [PubMed] [Google Scholar]
- 15.Proffit WR, Field HW, Sarver DM. 14th ed. Ch. 18. Canada: Mosby Co; 2007. Contemporary Orthodontics; pp. 635–86. [Google Scholar]
- 16.Folio J, Rams TE, Keyes PH. Orthodontic therapy in patients with juvenile periodontitis: Clinical and microbiologic effects. Am J Orthod. 1985;87:421–31. doi: 10.1016/0002-9416(85)90202-7. [DOI] [PubMed] [Google Scholar]
- 17.Rabie AB, Deng YM, Jin LJ. Adjunctive orthodontic treatment of periodontally involved teeth: Case reports. Quintessence Int. 1998;29:13–9. [PubMed] [Google Scholar]
- 18.Genco RJ, Cianciola LJ, Roseling BG. Treatment of localized juvenile periodontitis. J Dent Res. 1981;60:870–80. [Google Scholar]
- 19.Kipioti A, Gusberti F, Lang NP. Microbiological and clinical effects on orthodontic bands in children. J Dent Res. 1983;62:209–12. [Google Scholar]
- 20.Lindhe J, Karring T, Lang N. 4th ed. Ch. 31. United Kingdom: Blackwell; 2003. Clinical Periodontology and Implant Dentistry; pp. 744–76. [Google Scholar]
- 21.Nyman S, Karring T, Bergenholtz G. Bone regeneration in alveolar bone dehiscences produced by jiggling forces. J Periodontal Res. 1982;17:316–22. doi: 10.1111/j.1600-0765.1982.tb01159.x. [DOI] [PubMed] [Google Scholar]
- 22.Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93:143–8. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]
- 23.Gazit E, Lieberman M. Occlusal and orthodontic considerations in the periodontally involved dentition. Angle Orthod. 1980;50:346–9. doi: 10.1043/0003-3219(1980)050<0346:OAOCIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.McLain JB, Proffit WR, Davenport RH. Adjunctive orthodontic therapy in the treatment of juvenile periodontitis: Report of a case and review of the literature. Am J Orthod. 1983;83:290–8. doi: 10.1016/0002-9416(83)90224-5. [DOI] [PubMed] [Google Scholar]
- 25.Re S, Cardaropoli D, Abundo R, Corrente G. Reduction of gingival recession following orthodontic intrusion in periodontally compromised patients. Orthod Craniofac Res. 2004;7:35–9. doi: 10.1111/j.1601-6343.2004.00277.x. [DOI] [PubMed] [Google Scholar]
- 26.Zhang JH, Sha YQ, Cao CF. Comparative study of the effects of removing plaque by two toothbrushing methods. Beijing Da Xue Xue Bao. 2005;37:542–4. [PubMed] [Google Scholar]
- 27.Cobb CM. Nonsurgical pocket therapy: Mechanical. Ann Periodontol. 1996;1:443–50. doi: 10.1902/annals.1996.1.1.443. [DOI] [PubMed] [Google Scholar]
- 28.Buchmann R, Nunn ME, Van Dyke TE, Lange DE. Aggressive periodontitis: 5-year follow-up of treatment. J Periodontol. 2002;73:675–83. doi: 10.1902/jop.2002.73.6.675. [DOI] [PubMed] [Google Scholar]
- 29.Zhu BL, Guo YH, Zhou HA, Fu XH. The clinical results of combined periodontal-orthodontic treatment on patients with periodontitis and labial displacement of incisors. Shanghai Kou Qiang Yi Xue. 2005;14:431–3. [PubMed] [Google Scholar]
- 30.Melsen B, Agerbaek N, Eriksen J, Terp S. New attachment through periodontal treatment and orthodontic intrusion. Am J Orthod Dentofacial Orthop. 1988;94:104–16. doi: 10.1016/0889-5406(88)90358-7. [DOI] [PubMed] [Google Scholar]
- 31.Passanzaei D. Interdisciplinary treatment of a localized juvenile periodontitis, a new prospective to an old one. Am J Orthod Dentofacial Orthop. 2007;13:271–80. doi: 10.1016/j.ajodo.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 32.Rabie AB, Dan Z, Samman N. Ultrastructural identification of cells involved in the healing of intramembranous and endochondral bones. Int J Oral Maxillofac Surg. 1996;25:383–8. doi: 10.1016/s0901-5027(06)80038-x. [DOI] [PubMed] [Google Scholar]
- 33.Lindhe J, Karring T, Lang N. 4th ed. Ch. 44. United Kingdom: Blackwell; 2003. Clinical Periodontology and Implant Dentistry; pp. 1014–24. [Google Scholar]
- 34.Levin L, Samorodnitzky-Naveh GR, Machtei EE. The association of orthodontic treatment and fixed retainers with gingival health. J Periodontol. 2008;79:2087–92. doi: 10.1902/jop.2008.080128. [DOI] [PubMed] [Google Scholar]
- 35.Beck BW, Harris EF. Apical root resorption in orthodontically treated subjects: Analysis of edgewise and light wire mechanics. Am J Orthod Dentofacial Orthop. 1994;105:350–61. doi: 10.1016/S0889-5406(94)70129-6. [DOI] [PubMed] [Google Scholar]
- 36.Nemcovsky CE, Beny L, Shanberger S, Feldman-Herman S, Vardimon A. Bone apposition in surgical bony defects following orthodontic movement: A comparative histomorphometric study between root- and periodontal ligament-damaged and periodontally intact rat molars. J Periodontol. 2004;75:1013–9. doi: 10.1902/jop.2004.75.7.1013. [DOI] [PubMed] [Google Scholar]
- 37.Vardimon AD, Nemcovsky CE, Dre E. Orthodontic tooth movement enhances bone healing of surgical bony defects in rats. J Periodontol. 2001;72:858–64. doi: 10.1902/jop.2001.72.7.858. [DOI] [PubMed] [Google Scholar]
- 38.Nyman S, Karring T, Bergenholtz G. Bone regeneration in alveolar bone dehiscences produced by jiggling forces. J Periodontal Res. 1982;17:316–22. doi: 10.1111/j.1600-0765.1982.tb01159.x. [DOI] [PubMed] [Google Scholar]
- 39.Verna C, Melsen B. Tissue reaction to orthodontic tooth movement in different bone turnover conditions. Orthod Craniofac Res. 2003;6:155–63. doi: 10.1034/j.1600-0544.2003.03262.x. [DOI] [PubMed] [Google Scholar]
- 40.Seifi M, Ghoraishian SA. Determination of orthodontic tooth movement and tissue reaction following demineralized freeze-dried bone allograft grafting intervention. Dent Res J (Isfahan) 2012;9:203–8. doi: 10.4103/1735-3327.95237. [DOI] [PMC free article] [PubMed] [Google Scholar]


