Abstract
Background:
Cavernous sinus tuberculomas are extremely rare, but the increasing incidence worldwide of central nervous system (CNS) tuberculosis, mostly due to human immunodeficiency virus and poor sanitary conditions, and the ability of tuberculomas to mimic a brain neoplasm makes cavernous sinus tuberculomas a suspicious pathologic finding in the differential diagnosis of a brain space-occupying lesion.
Case Description:
We present an immunocompetent patient with no signs of systemic tuberculosis and an isolated right cavernous sinus space-occupying lesion. A skull base approach was performed and tumor resection achieved. The postoperative course was uneventful. Pathologic findings consisted of a tuberculoma and antituberculous treatment was immediately begun with total tumor regression after a 12-month regimen. After reviewing the literature, we propose suggestions to orient the diagnosis and a treatment algorithm for tuberculomas in rare locations.
Conclusion:
Tuberculomas in rare locations, as the cavernous sinus, are a challenging pathology as they have the ability to mimic a brain neoplasm. Although first line treatment are antituberculous therapy (4 drugs for at least 12 months) and adjuvant steroids, in inconclusive cases, surgical biopsy or excision is recommended for histopathologic confirmation and to reduce the mass effect, always following with antituberculous therapy and adjuvant steroids.
Keywords: Brain tumor, cavernous sinus, meningioma, skull base, tuberculoma, tuberculosis
INTRODUCTION
Tuberculosis (TB) has reemerged as a public health problem worldwide, mostly due to human immunodeficiency virus (HIV) and poor sanitary conditions. Central nervous system (CNS) involvement with TB ranges from 0.5% to 10%, most commonly affecting immunodeficient patients and developing countries.[8,12,21,23] Meningoencefalitis is the most frequent CNS manifestation of TB, while tuberculomas represent only 10-30% of cases, being mostly hemispheric.[3,6] Unusual reported locations are the hypothalamic region, Meckel's cave, sellar and suprasellar regions, cerebellopontine angle, and intraventricular spaces.[7,9,11,15,18] Cavernous sinus (CS) tuberculomas are extremely rare, with only eight[2,4,5,8,13,14,16,23] cases published. Furthermore, isolated CNS tuberculomas without systemic TB, as our case, are exceptional and commonly misdiagnosed. Current treatment of tuberculomas in rare locations, as CS, is controversial.
We present a case of an isolated right CS tuberculoma with no signs of systemic TB operated on with a skull base approach, review the literature to propose suggestions to orient diagnosis, and provide a treatment algorithm for tuberculomas in rare locations.
CLINICAL CASE
History and examination
A 42-year-old immunocompetent female patient presented with a 6-month history of severe intermittent right hemicraneal headaches. Four months later she developed a right eye ptosis and ophtalmoplegy. She had benign medical and epidemiologic histories. A neurologic examination revealed gaze limitations in all directions, ptosis of the right eye and right hemifacial hypoesthesia, with no signs of meningeal irritation. The general examination, routine hematologic examination, and chest radiography were normal with no history of fever or respiratory tract infections. Orbital computed tomographic scans and magnetic resonance imaging (MRI) were normal. Brain MRI revealed a right CS tumor [Figure 1a]. Erythrosedimentation, HIV serology, VDRL, C3, C4, ANA, ANCA, thyroid profile, and PCR for Epstein–Barr virus and TB all yielded negative results. Cerebrospinal fluid (CSF) testing was normal.
Figure 1.
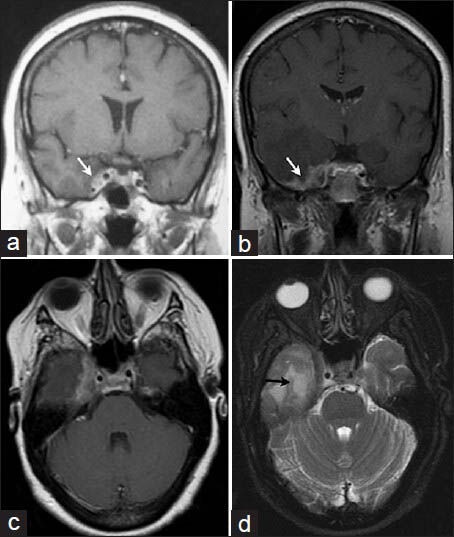
First T1-weighted coronal magnetic resonance images (a) with contrast enhancement of a right cavernous sinus tumor (white arrow). Six months later, preoperative T1-weighted coronal (b) and axial (c) MRI with gadolinium showing progression of the tumor involving the right cavernous sinus with dura-arachnoid thickening and intense pachymeningeal enhancement with mesial temporal infiltration (white arrow); T2-weighted axial MRI (d) showing temporal lobe edema (black arrow)
The patient was empirically treated with steroids suspecting a granulomatous disease with partial clinical improvement; however, she did not take the medications regularly and missed physician follow-up evaluations. Five months later she was readmitted with a clinical relapse and a new cerebral MRI revealed marked tumoral progression with adjacent right mesial temporal involvement [Figure 1b–d].
With no definitive diagnosis and tumoral progression, the patient was referred to our Neurosurgery Department and a surgical excisional procedure was recommended.
Operation
We considered it an inconclusive case and with the suspicion of a brain neoplasm, under general anesthesia, a right craneo-orbito-zygomatic with extended middle fossa approach was performed. The extradural anterior clinoidectomy and the CS and middle fossa peeling, allowed to identify both dural layers (dura propia and dura periostica). The inner layer of the lateral wall of the CS was not infiltrated by the tumor. The basal temporal and CS dura propia with an infiltrative tumoral mass, invading the mesial temporal lobe, was resected. The tumor had a firm, white appearance [Figure 2]. Subtotal tumor resection was achieved as the intraoperative pathologic impression was of an inflammatory disease. The CS was not opened. Dural closure was achieved with fascia lata.
Figure 2.
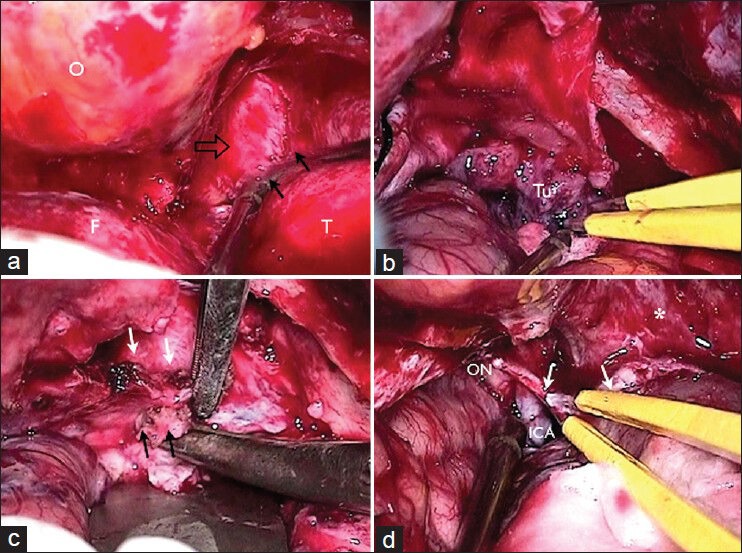
Intraoperative photos. (a) Right craneo-orbito-zygomatic with extended middle fossa approach, exposing the orbit (o), frontal (f), and temporal (t) lobes extradurally. Peeling of the lateral wall of the cavernous sinus and middle fossa floor identifying both dural layers (dura propia [black arrows] and dura periostica [open arrows]); (b and c) resection of tumor (Tu) with cavernous sinus and basal temporal dura propia infiltration (black arrows). Inner layer of cavernous sinus lateral wall without tumoral involvement (white arrows); (d) subtotal resection showing the optic nerve (ON), internal carotid artery (ICA), and dura mater (white arrows)
Pathologic findings
Microscopy revealed a caseous necrotic centre surrounded by a granulomatous reaction that included Langhans giant cells, epithelioid cells, and lymphocytes. In addition, there was abundant fibrosis [Figure 3c and d]. Immunological test were performed and definitive pathologic findings consisted of a tuberculoma, although Ziehl Neelsen and PAS stains did not demonstrate acid-fast bacilli and bacteriologic cultures were negative.
Figure 3.
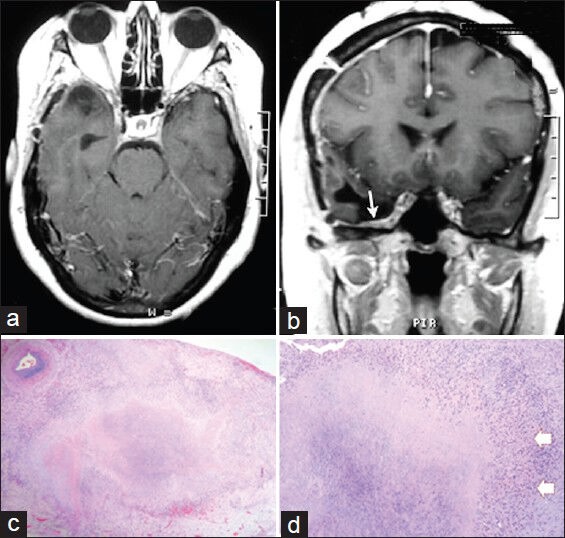
(a and b) Postoperative T1-weighted axial (a) and coronal (b) MRI with contrast injection showing the dural closure with fascia lata (white arrow). c and d: Photomicrograph H and E. (c) (original magnification ×100): Fibrosis and thickening of the dura with granulomatous inflammation and caseous necrosis; (d) (original magnification ×200): Granuloma with Langhans cells (arrows)
Postoperative course
Antituberculous treatment was immediately begun with a four drug (rifampin, isoniazid, ethambutol, and pyrazinamide) 2-month regimen followed by a two drug (rifampin and isoniazid) regimen for 10 months, and dexamethasone for the first 8 weeks.
The postoperative course was uneventful with no surgical morbidity and clinical improvement in the weeks thereafter. The 1-year postoperative follow-up MRI showed complete regression of the lesion [Figure 3a and b] and complete resolution of the symptoms.
DISCUSSION
CNS Mycobacterium tuberculosis disemination is hematogenous, generally from a primary lung infection, developing subpial, subependymal, or subcortical foci. The time from primary lung infection to CNS tuberculoma is age- and immune-dependent,[12] and the tuberculoma may lie latent for years with activation from Rich's focus.[5]
Tuberculomas represent 10-30% of cases of CNS TB, and in developing and endemic countries nearly 20% of brain masses have a tuberculous origin.[8] CS infections are extremely rare. We performed a PubMed search and found only eight cases of CS tuberculomas published.[2,4,5,8,13,14,16,23]
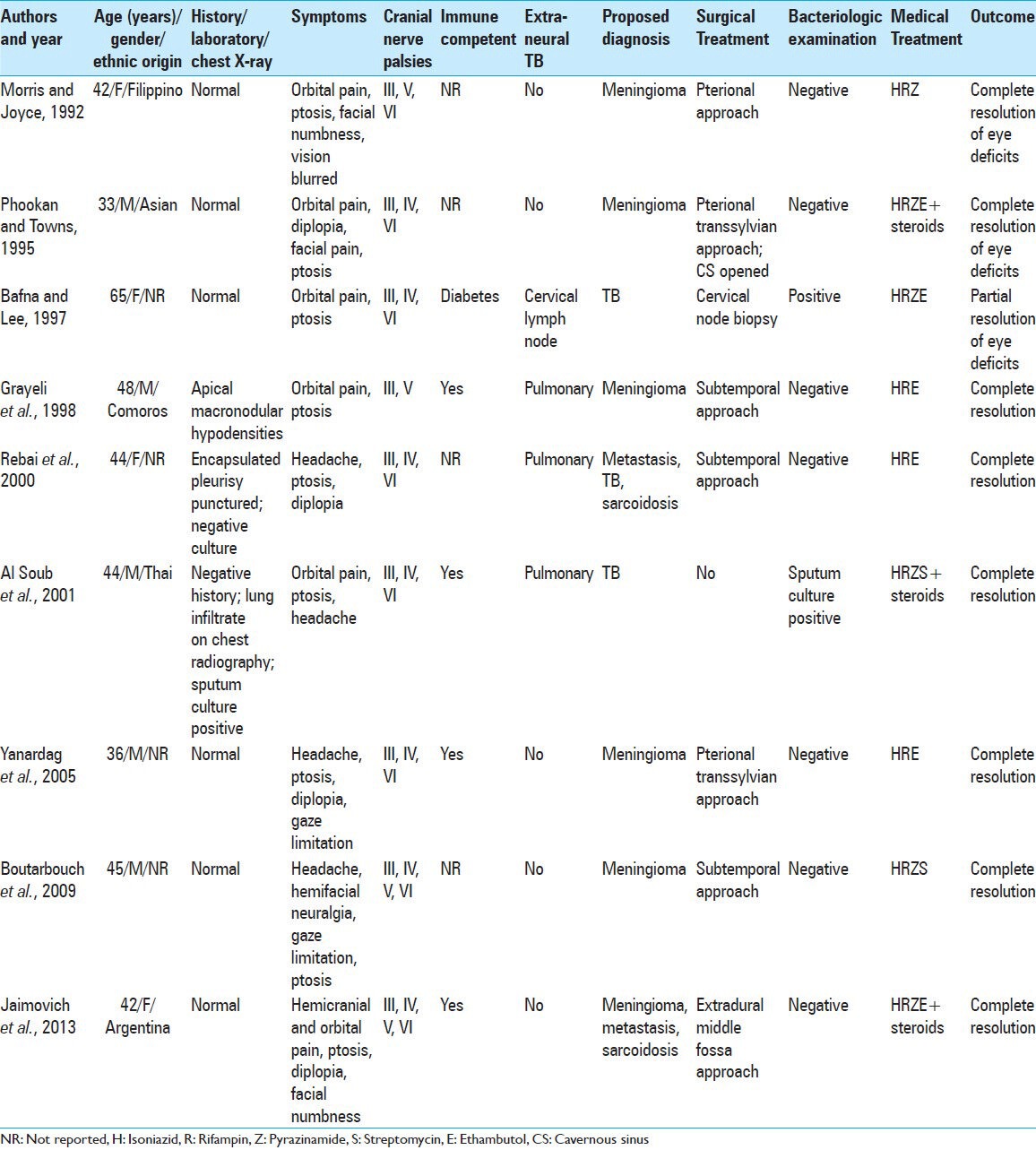
Most cases of CS tuberculomas presented with variable degrees of CS syndrome, no history of TB, and nonspecific laboratory and chest radiographic findings, thus, not considering this diagnosis. Four reported patients presented with extra-neural TB.[2,4,8,16] The proposed diagnosis was meningioma in five cases[5,8,13,14,23] and an intradural transsylvian or subtemporal approach was performed. In all cases, tuberculous bacilli were absent in the CSF, and cultures from the excised mass were negative. Medical treatment was empiric in two cases[2,4] with satisfactory resolution. All patients received a three or four drug regimen for a 12-month period; only two patients[2,14] were administered steroids. Resolution was achieved in all patients [Table 1].
Table 1.
Summary of CS tuberculoma cases reported
CNS tuberculomas have the ability to mimic a brain neoplasm and can develop in any region of the CNS, including extremely rare locations, such as the CS. Can even occur in immunocompetent patients with no history of TB (Gonzalez Ericsson P, Álvarez C, Nobili C, Jaimovich SG, Figurelli S: TB and CNS. Our Experience. Poster presented at the 44th Argentinean Congress of Pathology, Buenos Aires, Argentina, November 15-17, 2012). Brain imaging is not characteristic and clinical manifestations are consistent with a CS syndrome, making the diagnosis a difficult task, and thus the importance of surgical biopsy of the lesion to obtain anatomopathologic confirmation of the tuberculoma so to immediately initiate antituberculous chemotherapy.[12,23]
Unusual locations, reported in the literature, are the hypothalamic region, Meckel's cave, sellar, suprasellar and CS regions, cerebellopontine angle, intraventricular spaces.[7,9,11,15,18]
After reviewing the literature we propose suggestions to orient the diagnosis:[3,6,12,17,20,21,22]
Extensive epidemiologic and medical history interrogatory;
Infectious disease serologic testing;
Erythrosedimentation (generally elevated);
Blood and CSF tests;
TB PCR;
Chest X-rays;
Mantoux tuberculin skin test (not specific in endemic areas);
Search for extra-CNS TB (adenitis, pulmonary infection, bone, joint or kidney infections);
Brain MRI (high sensitivity, but low specificity); and
Rule out other differential diagnoses. For CS location rule out meningiomas, lymphomas, metastases, giant cell tumors, or inflammatory diseases (sarcoidosis, Tolosa Hunt syndrome, Wegener granulomatosis, aspergillomas, and mucormycotic lesions)
Clinical manifestations are of a CS syndrome, presenting with varying degrees of headaches, periorbital pain, ophtalmoplegy, ptosis, and hemifacial hypoesthesia
Systemic infections and usual laboratory parameters may be absent. Even tuberculous bacilli are not always present in the CSF.[17,23]
MRI is highly sensitive, but has low specificity for the diagnosis of tuberculomas. T1-weighted images show an area of hypo- or iso-intensity, revealing dural thickening and pachymeningeal contrast enhancement involving the CS, and T2-weighted images show a hypo- or iso-intense tumor with perilesional hyperintensity (edema).[5,6,22] Currently, proton MR spectroscopy can help orient diagnosis. Tuberculomas are characterized by a prominent decrease in NAA/Cr and a slight decrease in NAA/Cho, with lipid–lactate peaks usually elevated.[5]
For a definitive diagnosis, a tissue sample is mandatory for bacteriologic and histopathologic evaluations. However, according to the literature, bacteriologic examinations are positive in only 25% of CSF samples and 35% of tuberculoma tissue samples, and results may take between 10 days and 8 weeks. Consequently, negative bacteriologic samples do not eliminate a diagnosis of tuberculomas.[17,22] In our case, as in all the cases reported, tuberculous bacilli were absent and cultures from the excised mass were negative.[5,8,13,14,16,23]
Histopathologic evaluation confirms the diagnosis presenting as caseous necrosis, Langhans giant cells, and epithelioid cells, with or without tuberculous bacilli.[17]
Treatment of tuberculomas in rare locations, as CS, is controversial.[2,4,5,8,12,13,14,16,23]
In the presented case, with the suspected diagnosis of a neoplasm without the suspicion of a tuberculoma, we performed an extended extradural middle fossa approach. Although the postoperative course was uneventful, we think that this pathology has to be always considered in inconclusive cases and, as antituberculous therapy is the treatment of choice, a surgical biopsy for histopathologic confirmation via the most minimally invasive approach possible has to be performed. In cases of symptomatic mass effect, the approach may allow partial tumor resection to achieved neural decompression
Thus, after reviewing the literature, we suggest the following treatment algorithm [Figure 4].
Figure 4.
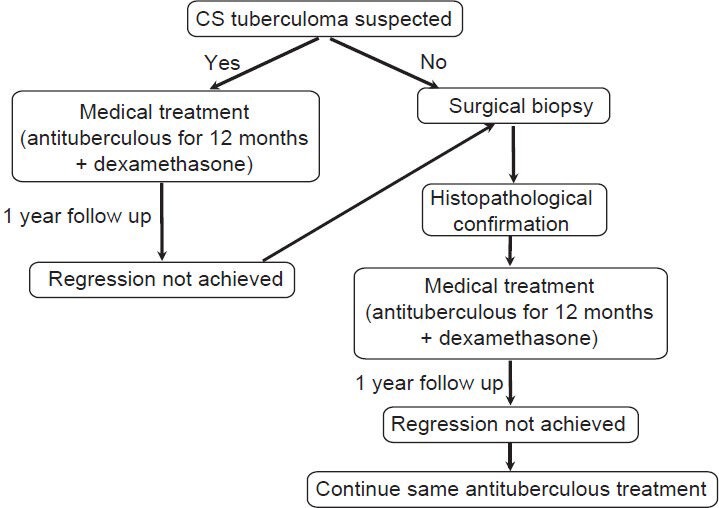
Treatment algorithm suggested (refer to text for details)
When tuberculoma is strongly suspected, empiric antituberculous treatment may be recommended. Regimen should consists of four drugs (rifampin, isoniazid, ethambutol, and pyrazinamide) for a 2-month period, followed by two drugs (rifampin and isoniazid) for a minimum of 10 months, and dexamethasone (0.4 mg/kg/day for 6-8 weeks).[21] Close follow-up is recommended until complete lesion regression on MRI. If regression is not achieved after 12 months of conservative treatment, lesion biopsy is suggested to obtain histopathologic confirmation
When the diagnosis is not conclusive, a tissue biopsy is recommended to rule out other differential diagnoses (most often meningiomas, lymphomas, metastases, and inflammatory diseases, for CS location). Different approaches are possible according to the involvement of the lesion.[2,4,5,8,12,13,14,16,23] However, the most minimally invasive approach possible has to be performed. Always initiate antituberculous treatment immediately with four drugs (rifampin, isoniazid, ethambutol, and pyrazinamide) for a 2-month period, followed by two drugs (rifampin and isoniazid) for a minimum of 10 months, and dexamethasone (0.4 mg/kg/day for 6-8 weeks).[21] In cases in which complete regression on MRI in not achieved after a 12-month period, the same regimen must be used for 18 months or until complete regression.
Although there is a lack of prospective and randomized studies on steroid benefits for tuberculomas, it use has been recommended in association with antituberculous treatment to reduce intracranial pressure, prevent paradoxic tuberculoma expansion during treatment and to achieve better outcomes.[2,10,17,19,21]
Follow-up must be close and for a long-term with MRI, considering the likelihood of recurrence and that the lesion can take more than 18 months to resolve with antituberculous treatment as a function of size. In this situation, the indication is to continue same treatment.[1,17]
In conclusion, the increasing incidence of CNS TB and the ability of tuberculomas to mimic a brain neoplasm makes tuberculomas an always suspected in the differential diagnosis. In inconclusive cases, surgical biopsy or excision is recommended for histopathologic confirmation and to reduce the mass effect. First line treatment are antituberculous therapy (4 drugs for at least 12 months) and adjuvant steroids, with a long-term follow-up.
ACKNOWLEDGMENTS
Silvina Figurelli, M.D.: Division of Anatomopathology, Juan A. Fernandez General Hospital, Buenos Aires City, Argentina Sebastián Lescano, M.D.: Division of Neuroradiology, Juan A. Fernandez General Hospital, Buenos Aires City, Argentina.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/158/123203
Contributor Information
Sebastián G. Jaimovich, Email: sebastianjaimovich@gmail.com.
Victor Castillo Thea, Email: vmcastillothea@yahoo.com.ar.
Martin Guevara, Email: martinguevara2@gmail.com.
Javier L. Gardella, Email: javiergardella@arnet.com.ar.
REFERENCES
- 1.Afghani B, Liebermann JM. Paradoxical enlargement or development of intracranial tuberculomas during therapy: Case report and review. Clin Infect Dis. 1994;19:1092–9. doi: 10.1093/clinids/19.6.1092. [DOI] [PubMed] [Google Scholar]
- 2.Al Soub H, Al Alousi F, Al Khal A. Tuberculoma of the cavernous sinus. Scand J Infect Dis. 2001;33:868–70. doi: 10.1080/00365540110027268. [DOI] [PubMed] [Google Scholar]
- 3.Arvind C, Korath MP, Raveendranadhan K, Jagadeesan K. A retropective study of 1247 cases of intracranial tuberculomata diagnosed by computerized tomography. J Assoc Physicians India. 1993;41:559–61. [PubMed] [Google Scholar]
- 4.Bafna S, Lee GA. Presumed tuberculosis presenting as a cavernous sinus syndrome. J Neuroophtalmol. 1997;17:207–8. [PubMed] [Google Scholar]
- 5.Boutarbouch M, Arkha Y, Gana R, El Maquili MR, Bellakhdar F. Tuberculoma of the cavernous sinus mimicking a meningioma: Case report and review of the literature. J Neurol Sci. 2009;278:123–6. doi: 10.1016/j.jns.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 6.De Castro CC, de Barros NG, Campos ZM, Cerri GG. CT scans of cranial tuberculosis. Radiol Clin North Am. 1995;33:753–69. [PubMed] [Google Scholar]
- 7.Flannery MT, Pattani S, Wallach PM, Warner E. Hypothalamic tuberculoma associated with secondary panhypopituitarism: Case report. Am J Med Sci. 1993;306:101–3. doi: 10.1097/00000441-199308000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Grayeli AB, Redondo A, Salama J, Rey A. Tuberculoma of the Cavernous Sinus: Case Report. Neurosurgery. 1998;42:179–82. doi: 10.1097/00006123-199801000-00040. [DOI] [PubMed] [Google Scholar]
- 9.Goel A, Nadkarni T, Desai AP. Tuberculoma in the Meckel's cave: A case report. Neurol India. 1999;47:238–40. [PubMed] [Google Scholar]
- 10.Gropper MR, Schulder M, Sharan AD, Cho ES. Central nervous system tuberculosis: Medical management and surgical indications. Surg Neurol. 1995;44:378–85. doi: 10.1016/0090-3019(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 11.Gücüyener K, Baykaner MK, Keskil IS, Hasanoglu A, Ilgit E, Beyazova U. Tuberculoma in the suprasellar cistern: Possible CT-misinterprataion as aneurysm. Pediatr Radiol. 1993;21:153–4. doi: 10.1007/BF02012415. [DOI] [PubMed] [Google Scholar]
- 12.Jaimovich SG, Driollet Laspiur S, Figurelli S, Guevara M, Gardela JL. Tuberculoma mimicking intracerebral neoplasm. Diagnostic and therapeutic tips. Neurol Arg. 2013;5:30–3. [Google Scholar]
- 13.Morris JT, Joyce MP. Central nervous system tumour presenting as a cavernous sinus tumour. Clin Infect Dis. 1992;15:181–2. doi: 10.1093/clinids/15.1.181. [DOI] [PubMed] [Google Scholar]
- 14.Phoohan G, Towns MG. Tuberculoma of the cavernous sinus: A case report. Br J Neurosurg. 1995;9:205–7. doi: 10.1080/02688699550041566. [DOI] [PubMed] [Google Scholar]
- 15.Povedano Rodriguez V, Mellado Rubio R, Jurado Ramos A, Seco Piñero I, López Villarejo P. Tuberculoma as expansive process of the cerebellopontine angle. Case report and bibliographical survey. An Otorrinolaringol Ibero Am. 1993;20:55–60. [PubMed] [Google Scholar]
- 16.Rebai R, Boudawara MZ, Bahloul K, Chabchoub I, Chaari S, Boudawara T, et al. Cavernous sinus tuberculoma: Diagnostic difficulties in a personal case. Surg Neurol. 2001;55:372–5. doi: 10.1016/s0090-3019(01)00474-8. [DOI] [PubMed] [Google Scholar]
- 17.Santosh IP, Vedantam R. Rate of resolution of histologically verified intracranial tuberculomas. Neurosurgery. 2003;53:873–9. doi: 10.1227/01.neu.0000083553.25421.6f. [DOI] [PubMed] [Google Scholar]
- 18.Sharma MC, Arora R, Mahapatra AK, Sarat-Chandra P, Gaikwad SB, Sarkar C. Intrasellar tuberculoma-an enigmatic pituitary infection: A series of 18 cases. Clin Neurol Neurosurg. 2000;102:72–7. doi: 10.1016/s0303-8467(00)00063-9. [DOI] [PubMed] [Google Scholar]
- 19.Sunil KP. Conservative treatment of intracranial tuberculomas. Neurol India. 1982;30:30–6. [Google Scholar]
- 20.Sutlas PN, Unal A, Forta H, Senol S, Kırbas D. Tuberculous meningitis in adults: Review of 61 cases. Infection. 2003;31:387–91. doi: 10.1007/s15010-003-3179-1. [DOI] [PubMed] [Google Scholar]
- 21.Thwaites G, Fisher M, Hemingway C, Scott G, Solomon T, Innes J. British Infection Society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. J Infect. 2009;59:167–87. doi: 10.1016/j.jinf.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 22.Unala A, Sutlas PN. Clinical and radiological features of symptomatic central nervous system tuberculomas. Eur J Neurol. 2005;12:797–804. doi: 10.1111/j.1468-1331.2005.01067.x. [DOI] [PubMed] [Google Scholar]
- 23.Yanardag H, Uygun S, Yumuk V, Caner M, Canbaz B. Cerebral tuberculosis mimicking intracranial tumour. Singapore Med J. 2005;46:731–3. [PubMed] [Google Scholar]


