Abstract
Background and Objectives:
Growth parameters are important indicators of a child's overall health, and they are influenced by factors like blood glucose control in diabetic children. Data on growth parameters of Indian diabetic children is scarce. This retrospective, cross-sectional, case control study was conducted at diabetes clinic for children at a tertiary care center at Pune, to study growth parameters of diabetic children in comparison with age-gender matched healthy controls and evaluate effect of different insulin regimes and age at diagnosis of diabetes on growth.
Materials and Methods:
One twenty five diabetic children (boys: 50) and age gender matched healthy controls were enrolled. All subjects underwent anthropometric measurements (standing height and weight). Mean height (HAZ), weight (WAZ) and body mass index (BAZ) for age Z scores were calculated. Diabetes control was evaluated by measuring glycosylated hemoglobin (HbA1C). Statistical analysis was done by SPSS version 12.
Results:
Mean age of diabetic children and age gender matched controls was 9.7 ± 4.4 years. Diabetic children were shorter (128.3 ± 24.3 cm vs. 133.6 ± 24.7 cm) and lighter (29.2 kg ± 15.3 vs. 31.3 ± 15.4 kg). HAZ (−1.1 ± 1.2 vs. −0.2 ± 0.8) and WAZ (−1.2 ± 1.3 vs. −0.7 ± 1.3) were significantly lower in diabetic children (P < 0.05). Children on both insulin regimes (intensive and conventional) were shorter than controls (HAZ-intensive −1.0 ± 1.0, conventional −1.3 ± 1.3, control −0.2 ± 0.8, P < 0.05). HAZ of children who were diagnosed at <3 years of age was the least (−1.6 ± 1) amongst all diabetic children while those diagnosed after puberty (>14 years) were comparable to healthy controls.
Conclusions:
Growth was compromised in diabetic children in comparison to controls. Children diagnosed at younger age need more attention to optimize growth.
Keywords: Age at diagnosis, growth, India, insulin regimens, type 1 diabetes
INTRODUCTION
Type 1 Diabetes Mellitus (T1DM) is one of the most common chronic endocrine disorders of childhood and adolescence.[1] Impaired growth is a well-documented complication of diabetes; studies suggest that good metabolic control is crucial for normal growth.[2] There is evidence to suggest that there are abnormalities in the hypothalamic-pituitary-growth hormone axis in patients with diabetes and these are more common in subjects with poor glucose control and longer duration of the disorder. Hence, evaluating growth in children and adolescents with diabetes together with metabolic control is important.
Studies also suggest that growth velocity is affected in accordance with the age of the patient, as well as the age at diagnosis. Growth of children in pre-pubertal years has been reported to be affected by diabetes. It has been noted that poor relative growth is associated with younger age at onset.[3] Thus, assessing growth of diabetic children with respect to age at diagnosis and duration of disease is crucial.
Reports suggest that the impact of T1DM on growth is no longer of major relevance in developed countries because of more physiological insulin substitutions and self-monitoring.[4] However, in developing countries such as India, there are constraints of finances (cost of insulin and blood glucose monitoring) and knowledge, which make the management of diabetes difficult. Conventional regimes are suitable for and in use by a vast majority of patients in India. As a result, it is likely that under-insulinization may be associated with poor growth in these situations.[5] However, data on growth parameters of Indian children with T1DM on conventional insulin versus intensive insulin therapy are very scarce.
Thus, the objectives of our retrospective observational study were: (1) To assess growth parameters (height, weight and body mass index [BMI]) in diabetic children in comparison with age-gender matched healthy controls. (2) To study the impact of insulin regime (conventional versus intensive) on growth parameters. (3) To study the impact of age at diagnosis and duration of diabetes on growth parameters.
MATERIALS AND METHODS
Subjects
All patients visiting the type 1 diabetes clinic at a tertiary care center at Pune were approached for the study and those children who gave assent and whose parents gave consent were enrolled in the study. Ethical approval was granted by the institutional ethics committee. Patients on any other medication but insulin for blood glucose control, with known co-morbidities like celiac disease, untreated hypothyroidism and eating disorders were excluded from the study.
A clinical examination was performed by a pediatrician for evaluating health status. Tanner staging for sexual maturity was performed by a pediatric endocrinologist.[6,7] In all, 125 children, 9.7 ± 4.4 years (boys: 50; girls: 75) meeting the selection criteria were enrolled in the study between May 2011 and April 2012. Age-gender matched healthy controls were recruited in the study from private schools with their assent and parents’ consent.
Data on age at diagnosis, duration of diabetes and insulin regimen were gathered by a standardized questionnaire and cross-checked from patient records. Medical history of all patients was also verified from hospital medical records.
Anthropometry
Standing height was measured to the nearest millimeter using a portable stadiometer (Leicester Height Meter, Child Growth Foundation, UK), and weight was measured using an electronic scale to the nearest 100 g. BMI was calculated by the formula weight/height in meter square. The height, weight and BMI were converted to Z scores using contemporary Indian references.[8]
Biochemical measurements
Diabetes control was evaluated by measuring glycosylated hemoglobin (HbA1C). A fasting blood sample (5 ml) was collected between 7 am and 9 am by a trained pediatric nurse. HbA1C was measured by High performance liquid chromatography (HPLC) (BIO-RAD, Germany). Fasting and post prandial blood glucose were measured using the glucose oxidase-peroxidase method (GOD-POD).
Statistical methods
All statistical analysis was carried out using the SPSS for Windows software program, version 12 (SPSS, Chicago, IL, USA). All outcome variables were tested for normality before performing any statistical analysis. Differences in means were tested using Student's t-test. One way ANOVA with post-hoc Tuckey's test was used to compare the effect of insulin regime on growth parameters in diabetic children. A P < 0.05 was considered significant.
Insulin dosage
The insulin requirement was calculated according to standard protocol,[9] the age and pubertal stage of the child (Pre-puberty 0.7 U/kg/day, Mid puberty 1 U/kg/day, Late Puberty 1.2 U/kg/day). Children were either on a conventional or an intensive (basal-bolus) regime. The conventional (split-mix) regime included either two or three injections per day of pre-mixed insulin and regular insulin, whereas children on the intensive regime took four injections per day, which included three analogs or short acting doses and one of basal insulin.
RESULTS
Growth parameters of the diabetic children (mean age 9.7 ± 4.4 years) and age-gender matched controls have been summarized in Table 1. The mean height of diabetic boys was 129 ± 25.7 (HAZ −0.9 ± 1.3) and that of girls was 127.4 ± 23.3 (HAZ −1.3 ± 1.3). The mean height for age Z scores (HAZ) as well as the weight for age Z score (WAZ) of the diabetic children were significantly lower than that of controls (P < 0.05). The mean BMI for age Z scores (BAZ) were comparable in both groups [Table 2]. Total percentage of diabetic children who had their HAZ score <−2 SD was 27.1% and that for WAZ was 10.9% and for BAZ was 13.2%. No children had complications of DM such as retinopathy, nephropathy and neuropathy.
Table 1.
Comparison of anthropometric parameters between boys and girls in diabetic and control children
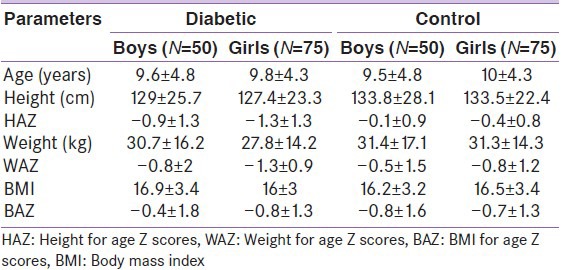
Table 2.
Comparison of growth parameters between diabetic children according to insulin regimen and control children
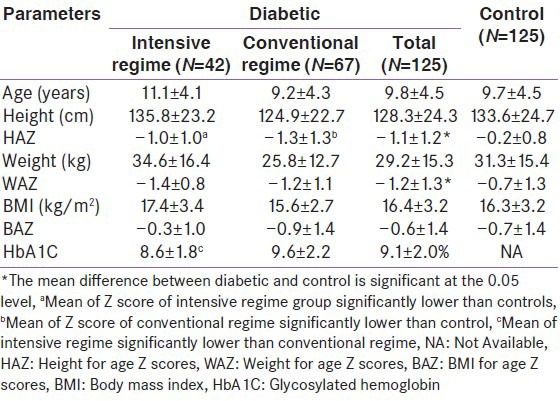
To further study the possible impact of different insulin regimes, children were divided as per the insulin received (conventional or intensive) and growth parameters were compared with those of controls [Table 2]. There were no significant differences in the HAZ scores of children on the two insulin regime; however, both groups were significantly shorter than the healthy controls (P < 0.05). For the WAZ scores and BAZ scores there were no significant differences between children on intensive or conventional insulin regimes and healthy controls. Children who received intensive insulin therapy were taller than those on the conventional regime; however, the difference was not statistically significant. (HAZ −1.0 ± 1.0 vs. −1.3 ± 1.3).
Blood glucose control was evaluated by measuring HbA1C. The mean HbA1C of the diabetic children was 9.1 ± 2.0%. HbA1C did not show any correlation with HAZ. When the HbA1C level was divided into tertiles to compare the lowest and the highest group representing good control to poor control over blood sugar, there were no significant differences in the growth parameters of both the groups. The HbA1C level of children on the two different insulin regimes was, however, significantly different. (Intensive regime −8.6 ± 1.8%, conventional regime −9.6 ± 2.2%, P = 0.040) however, there was no difference in their growth parameters.
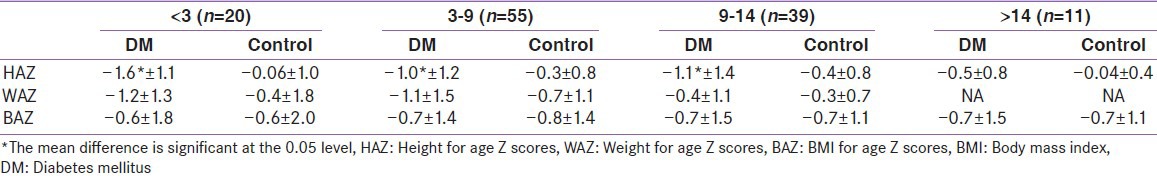
Apart from poor metabolic control one of the other factors which may affect growth is the age at diagnosis. Children were divided into four groups according to their age at diagnosis of diabetes as: <3 years, 3-9 years, 9-14 years and >14 years [Table 3]. Children who were diagnosed <3 years of age were shortest (HAZ −1.6 ± 1.1), while those diagnosed after 14 years were not different from controls (HAZ −0.5 ± 0.7). Most children diagnosed around 14 years were growing at time of diagnosis. However, overall, a total of 16 children above the age of 14 years had completed puberty when study was performed. To evaluate the impact of duration of diabetes on growth, years since children had diabetes (2.3 ± 2.8 years) was divided into tertiles and HAZ was compared across tertiles. No significant difference was found in HAZ across tertiles.
Table 3.
Comparison of height, weight and body mass index Z scores according to age at diagnosis
The mean insulin dose was 1 ± 0.3 units/kg. Children who were prepubertal, as well as those who were in puberty received insulin within the recommended dose.[9] To assess the impact of insulin dose on growth, children were divided into two groups according to the median of insulin dose per kg per day into high dose and low dose. There was no significant difference between both the groups for the HAZ scores.
DISCUSSION
Our results indicate that our study children with T1DM were shorter than age matched controls; children who received intensive insulin therapy were less affected than those in the conventional regime, although the difference was not statistically significant. Diabetic children were also lighter than the controls. Children who were diagnosed before 3 years of age were the shortest, while height was least affected in those diagnosed after 14 years of age.
There is conflicting literature on anthropometric parameters in children with diabetes. While it is generally agreed that there are perturbations in stature in diabetic children, some studies report that these are related to metabolic control[10,11,12] while others have reported that differences in height cannot be attributed to metabolic control alone.[4,13,14] In line with results of the latter studies, we also found that growth impairment was not associated with metabolic control as judged by HbA1c, suggesting other possible mechanisms for the short stature.
Several longitudinal studies have demonstrated weight gain was more prominent amongst girls during the pubertal years.[4,15] Ours being a cross-sectional study we could not study the weight gain amongst our study population. However, there were no differences noted amongst diabetic children and controls for weight and BMI.
Although reasons for reduced stature in diabetics are still debatable, some studies on growth in diabetic children report that stature is most affected when diabetes is diagnosed prepubertally.[11,13,14] The opposite has been concluded in another study where prepubertal boys were taller than normal children at the time of diagnosis but such differences were not seen in pubertal children.[16] In our study population, children diagnosed after 14 years were comparable with normal healthy children while children diagnosed before 3 years were the most affected.
The shortcomings of using conventional insulin regimes have been described by several studies.[12,17] Use of intensive therapy in children who were on conventional therapy has been shown to improve growth.[18] Our children were on both conventional and intensive therapy. Children on intensive therapy had a higher HAZ score than the children on conventional therapy though the HAZ was not significantly different. Also the control of diabetes by measuring HbA1C in both the groups suggested that the intensive regime group had a lower HbA1C. Due to high cost of intensive regime, mandatory glucose monitoring and higher number of injections involved, intensive insulin therapy is still not acceptable by many children and families[5] and hence a large number of children in our study were on conventional regime (52%).
Further investigations are needed to understand growth parameters of Indian diabetic children. Longitudinal data is needed to understand how these growth parameters are affected over a period of time.
In summary, our results indicate that in Indian type 1 diabetics, particularly those diagnosed at a younger age, growth is likely to be affected. Intensive insulin therapy may improve growth of these children over a period of time. Hence, close monitoring of growth in all children with T1DM, with special reference to children diagnosed in preschool years is essential.
ACKNOWLEDGMENT
Lavanya S Parthasarathy thanks University Grants Commission, Government of India for the funding. Our sincere thanks to Mr. S. Pancharatnam from Panchsheel, Chinchwad, Pune.
Footnotes
Source of Support: Mr. S. Pancharatnam from Panchsheel, Chinchwad, Pune
Conflict of Interest: None declared
REFERENCES
- 1.Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 2.Wise JE, Kolb EL, Sauder SE. Effect of glycemic control on growth velocity in children with IDDM. Diabetes Care. 1992;15:826–30. doi: 10.2337/diacare.15.7.826. [DOI] [PubMed] [Google Scholar]
- 3.Danne T, Kordonouri O, Enders I, Weber B. Factors influencing height and weight development in children with diabetes. Results of the Berlin Retinopathy Study. Diabetes Care. 1997;20:281–5. doi: 10.2337/diacare.20.3.281. [DOI] [PubMed] [Google Scholar]
- 4.Lebl J, Schober E, Zidek T, Baldis S, Rami B, Pruhova S, et al. Growth data in large series of 587 children and adolescents with type 1 diabetes mellitus. Endocr Regul. 2003;37:153–61. [PubMed] [Google Scholar]
- 5.Bhatia E, Aggarwal A. Insulin therapy for patients with type 1 diabetes. J Assoc Physicians India. 2007;55:29. [PubMed] [Google Scholar]
- 6.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45:13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khadilkar VV, Khadilkar AV, Cole TJ, Sayyad MG. Crosssectional growth curves for height, weight and body mass index for affluent Indian children, 2007. Indian Pediatr. 2009;46:477–89. [PubMed] [Google Scholar]
- 9.Bangstad HJ, Danne T, Deeb L, Jarosz-Chobot P, Urakami T, Hanas R. Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes. 2009;12:82–99. doi: 10.1111/j.1399-5448.2009.00578.x. [DOI] [PubMed] [Google Scholar]
- 10.Demir K, Altıncık A, Abacı A, Büyükgebiz A, Böber E. Growth of children with type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol. 2010;2:72–7. doi: 10.4274/jcrpe.v2i2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holl RW, Grabert M, Heinze E, Sorgo W, Debatin KM. Age at onset and long-term metabolic control affect height in type-1 diabetes mellitus. Eur J Pediatr. 1998;157:972–7. doi: 10.1007/s004310050980. [DOI] [PubMed] [Google Scholar]
- 12.Gunczler P, Lanes R, Esaa S, Paoli M. Effect of glycemic control on the growth velocity and several metabolic parameters of conventionally treated children with insulin dependent diabetes mellitus. J Pediatr Endocrinol Metab. 1996;9:569–75. doi: 10.1515/jpem.1996.9.6.569. [DOI] [PubMed] [Google Scholar]
- 13.Stipancić G, La Grasta Sabolić L, Jurcić Z. Growth disorders in children with type 1 diabetes mellitus. Coll Antropol. 2006;30:297–304. [PubMed] [Google Scholar]
- 14.Kanumakala S, Dabadghao P, Carlin JB, Vidmar S, Cameron FJ. Linear growth and height outcomes in children with early onset type 1 diabetes mellitus– A 10-yr longitudinal study. Pediatr Diabetes. 2002;3:189–93. doi: 10.1034/j.1399-5448.2002.30404.x. [DOI] [PubMed] [Google Scholar]
- 15.Wong GW, Cheng PS, Leung TF. Sex differences in the growth of diabetic children. Diabetes Res Clin Pract. 2000;50:187–93. doi: 10.1016/s0168-8227(00)00192-3. [DOI] [PubMed] [Google Scholar]
- 16.Scheffer-Marinus PD, Links TP, Reitsma WD, Drayer NM. Increased height in diabetes mellitus corresponds to the predicted and the adult height. Acta Paediatr. 1999;88:384–8. doi: 10.1080/08035259950169738. [DOI] [PubMed] [Google Scholar]
- 17.Majaliwa ES, Munubhi E, Ramaiya K, Mpembeni R, Sanyiwa A, Mohn A, et al. Survey on acute and chronic complications in children and adolescents with type 1 diabetes at Muhimbili National Hospital in Dar es Salaam, Tanzania. Diabetes Care. 2007;30:2187–92. doi: 10.2337/dc07-0594. [DOI] [PubMed] [Google Scholar]
- 18.Rudolf MC, Sherwin RS, Markowitz R, Bates SE, Genel M, Hochstadt J, et al. Effect of intensive insulin treatment on linear growth in the young diabetic patient. J Pediatr. 1982;101:333–9. doi: 10.1016/s0022-3476(82)80054-1. [DOI] [PubMed] [Google Scholar]


