 |
Daniel Beard is a Professor in the Department of Molecular and Integrative Physiology and School of Medicine Collegiate Professor at the University of Michigan. He received a B.S. in Biomedical Engineering from Boston University in 1993 and an M.S. in Applied Mathematics and Ph.D. in Bioengineering from the University of Washington in 1997. Dr Beard is the Director of the Virtual Physiological Rat (VPR) project, an NIH National Center for Systems Biology, working to analyse, interpret, simulate, and ultimately predict physiological function in health and disease. Eric Feigl MD graduated from the University of Minnesota and had postdoctoral training in Sweden and NIH. He is a Professor of Physiology in the Medical School of the University of Washington and his honours include The Katz Prize from the American Heart Association, the Outstanding Research Award of the International Society for Heart Research, the Wiggers Award and the Berne Award of the American Physiological Society. Dr Feigl has taught cardiovascular medicine to medical students for several decades without using the confusing Guyton model.
The thesis of this essay is that Guyton's model of the systemic circulation has been so misinterpreted by Guyton and others that it generates more confusion than insight.
Because of the capacitance of arteries and veins, blood pressure will attain a finite value if blood flow is quickly stopped without a change in vascular tone. This static pressure is called the ‘mean systemic pressure’PMS. Guyton devised an experimental preparation in open chest dogs where an external artificial pump drew blood from the right atrium and delivered it to the pulmonary artery.
The output flow rate of the pump was manually adjusted by raising and lowering a collapsible tube (Starling resistor) at the inlet (right atrial) side of the pump. In this way the steady state cardiac output flow of the left ventricle was set as the independent experimental variable. In other words, the artificial pump opened the circuit of the circulation and haemodynamically isolated the right atrium from the heart so that the systemic circulation could be studied in quasi-isolation. As will be explained, the confusion over Guyton's results and associated model can be traced to the mistaken interpretation of the measured right atrial pressure as an independent causal variable governing the behaviour of the system.
Using the preparation with a Starling resistor, Guyton made steady state measurements of right atrial pressure at different pump output levels, including mean systemic pressure when pump output was zero (Guyton, 1955, 1959). An example of Guyton's original data is shown in Fig. 1A. Remember that these are steady state measurements where venous return equals cardiac output by definition.
Figure 1.
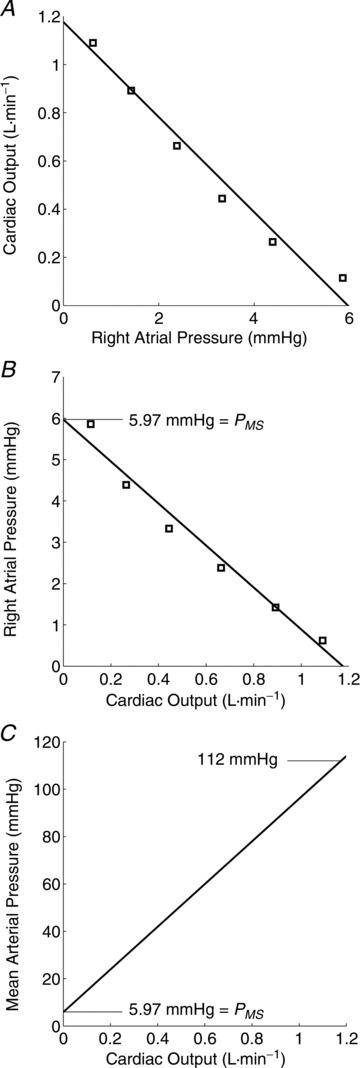
A, data from Guyton et al. (1959) are plotted showing the steady state relation between flow (F= cardiac output = venous return) and right atrial pressure (PRA) measured when flow was altered by limiting the inflow to an artificial pump with a collapsible tube. B, the data from A are replotted with flow plotted on the abscissa correctly indicating that cardiac output is the independent variable. The intercept on the ordinate is the right atrial pressure (equal to the mean systemic pressure) when flow (cardiac output) is zero. C, the calculated arterial pressure according to Guyton's model, with constant systemic vascular resistance, when flow is varied over the range defined in A and B. See Beard & Feigl (2011) for details. Figure reproduced, with permission, from the American Journal of Physiology Heart – Heart and Circulatory Physiology.
Guyton's first misinterpretation was to assume that the independent (causal) variable in his experiment was the right atrial pressure because it was determined by manually adjusting the elevation of the Starling resistor. However, adjusting the height of the collapsible tube was just a means of changing the pump output, which was the true independent variable. This point is verified by the observations of Grodins et al. (1960) and Levy (1979), who used the same external pump right heart bypass preparation without a Starling resistor so the pump just connected the right atrium to the pulmonary artery. Grodins et al. and Levy obtained very similar results to Guyton when the pump rate was manually dialled up or down, thus eliminating confusion about the independent variable; clearly it is the pump (cardiac) output.
Guyton's second major misconception was the assertion that the driving pressure for steady state cardiac output (‘venous return’) is mean systemic pressure minus right atrial pressure (PMS–PRA).
This interpretation has no physical or physiological basis. The static mean systemic pressure only exists when cardiac output flow is zero. When there is flow, the mean systemic pressure exists only as an abstraction of a mathematical model. It is possible to define a resistance, RVR, relating the flow (F) and the mean systemic pressure minus right atrial pressure. This is Guyton's famous venous return equation.
| (1) |
RVR is an equivalent resistance (Guyton's ‘resistance to venous return’) that is simply a consequence of this equation, and does not represent an actual physical structure or mechanism. It is misleading to think of PMS as a driving force for flow through a resistor. PMS is solely a function of the magnitude of blood volume and systemic vascular capacitance. In steady state, PMS is not a function of flow, and flow is not a function of PMS. However, right atrial pressure is a function of flow in the Guyton model as emphasized by Beard & Feigl (2011). Another way of stating it is: the mean systemic pressure (only manifest when flow is zero) is the transmural pressure distending the vasculature, but this pressure cannot generate flow along the vascular tree because pressure is equal everywhere in the systemic circulation when flow is zero.
A third misinterpretation, not made by Guyton but by those who followed him using his model, is that vascular capacitance provides a driving force for venous return. A passive elastic element can store pressure energy and smooth pulsations from beat to beat but cannot generate pressure to overcome resistive losses during steady state (see Discussion in Beard & Feigl (2011)).
These major misconceptions are promoted by how the relationship between flow and right atrial pressure is presented in textbooks. Guyton's model, (usually in graphic form) has been used to explain the relation between cardiac output (venous return) and right atrial pressure as shown in Fig. 1A. This is misleading because right atrial pressure is graphed on the x-axis abscissa implying that right atrial pressure is the independent, causative variable. In Guyton's model right atrial pressure is determined by the flow through the systemic circulation. Therefore the graph shown in Fig. 1B where cardiac output is the independent variable plotted on the x-axis is less misleading. The flow determines the right atrial pressure. The right atrial pressure does not represent a ‘back pressure’ limiting venous return.
Why does the Guyton model predict a decrease in right atrial pressure as cardiac output increases? This is because the model assumes a constant total systemic vascular resistance, and thus predicts that the arterial pressure increases as cardiac output increases as shown in Fig. 1C. An increase in arterial pressure results in increased filling of the arterial capacitance in the model. Since systemic blood volume is constant in the model definition, volume is shifted from the venous capacitance to the arterial capacitance in the model. The decreased filling of the venous capacitance is reflected in the diminished venous pressure and right atrial pressure as cardiac output is augmented. However, what actually happens in the circulation is more complicated than indicated by the simple constant-coefficient lumped Guyton model. What really occurs during physiological adjustments is that vascular resistance changes (reflexes, local metabolic control, etc.) and the distribution of cardiac output changes to the various organs in parallel (skeletal muscle, skin, kidney, gut, etc.), each with its own separate resistance and capacitance.
The three misinterpretations described above have potential clinical consequences. For example, in a condition when right atrial pressure is low a clinician might withhold giving needed fluids under the misguided thought that increasing right atrial pressure will decrease the gradient for ‘venous return’ (PMS–PRA) and cardiac output. Furthermore, the simple series Guyton model with only single arterial and venous compartments and a fixed total vascular resistance is not sufficient to describe what happens in exercise, fever, postural changes, shock, heart failure, etc.
Numerous critical analyses, discussions, and letters to the editor have exposed the misinterpretations of Guyton's venous return curves: Grodins et al. (1960), Levy (1979), Brengelmann (2003), Brengelmann (2006), Beard & Feigl (2011). Nevertheless, confused interpretations of the Guyton model continue to be presented in textbooks that bewilder students and mislead clinicians. The Guyton model and, critically, Guyton's misinterpretation of the model generates more confusion than clarity and should be discarded.
Sometimes it is possible to get a correct answer for the wrong reasons. However, the hazard is that one is likely to get other answers that are incorrect if one starts with a faulty premise. Guyton's idea, that venous return (equal to cardiac output) is determined by the pressure difference between mean systemic pressure and right atrial pressure (PMS–PRA) is physically and physiologically wrong. This idea should not be taught because it results in confused thinking about the cardiovascular system.
Call for comments
Readers are invited to give their views on this and the accompanying CrossTalk articles in this issue by submitting a brief comment. Comments may be posted up to 6 weeks after publication of the article, at which point the discussion will close and authors will be invited to submit a ‘final word'. To submit a comment, go to http://jp.physoc.org/letters/submit/jphysiol;591/23/5795
References
- Beard DA, Feigl EO. Understanding Guyton's venous return curves. Am J Physiol Heart Circ Physiol. 2011;301:H629–H633. doi: 10.1152/ajpheart.00228.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brengelmann GL. A critical analysis of the view that right atrial pressure determines venous return. J Appl Physiol. 2003;94:849–859. doi: 10.1152/japplphysiol.00868.2002. [DOI] [PubMed] [Google Scholar]
- Brengelmann GL. Counterpoint: the classical Guyton view that mean systemic pressure, right atrial pressure, and venous resistance govern venous return is not correct. J Appl Physiol. 2006;101:1525–1526. doi: 10.1152/japplphysiol.00698a.2006. (Discussion pp. 1526–1527) [DOI] [PubMed] [Google Scholar]
- Grodins FS, Stuart WH, Veenstra RL. Performance characteristics of the right heart bypass preparation. Am J Physiol. 1960;198:552–560. doi: 10.1152/ajplegacy.1960.198.3.552. [DOI] [PubMed] [Google Scholar]
- Guyton AC. Determination of cardiac output by equating venous return curves with cardiac response curves. Physiol Rev. 1955;35:123–129. doi: 10.1152/physrev.1955.35.1.123. [DOI] [PubMed] [Google Scholar]
- Guyton AC, Abernathy B, Langston JB, Kaufmann BN, Fairchild HM. Relative importance of venous and arterial resistances in controlling venous return and cardiac output. Am J Physiol. 1959;196:1008–1014. doi: 10.1152/ajplegacy.1959.196.5.1008. [DOI] [PubMed] [Google Scholar]
- Levy MN. The cardiac and vascular factors that determine systemic blood flow. Circ Res. 1979;44:739–747. doi: 10.1161/01.res.44.6.739. [DOI] [PubMed] [Google Scholar]


