Abstract
The outcomes of both dental implants and endodontically treated teeth have been extensively studied. However, there is still a great controversy over when to keep a natural tooth and when to extract it for a dental implant. This article reviews the benefits and disadvantages of both treatment options and discusses success vs. survival outcomes, as well as the impact of technical advances for modern endodontics and endodontic microsurgery on the long-term prognosis of tooth retention.
Keywords: dental implants, endodontic therapy, oral health, outcome, systematic review, treatment planning
Introduction
Helping people to keep their dentition is the ultimate goal of dentistry. A challenging dilemma faced by clinicians—and one that has been hotly debated—is when teeth should be condemned and implants used instead (Ruskin et al., 2005; John et al., 2007; Torabinejad et al., 2007). A tendency exists toward a simplified approach of ‘extraction and implant’, but this is not always simple or ethical. Particularly, endodontically treated teeth have been regarded as inferior to implants in terms of long-term stability and retention (Ruskin et al., 2005).
Endodontics includes primary and secondary endodontic treatment and periradicular surgery, all of which are applied to save teeth with prognostic value that can be restored. Dental implants extend the dentition when teeth are missing or cannot be maintained with reasonable effort. However, teeth need not be replaced prematurely, since the overall goal in dentistry is the patient’s long-term health and benefit. Endodontics and implantology should complement each other and not compete. Unfortunately, because of misinformation, great confusion exists regarding the long-term outcome of implants and endodontics. The following essential issues will be addressed in this review: retention vs. replacement, misconceptions associated with endodontic therapy and implants, and current strategies for endodontic treatment planning relating to long-term success and tooth retention.
Modern dentistry should follow an evidence-based approach. However, the question of retention or extraction of a tooth has not been satisfactorily answered at a high level of evidence (Iqbal and Kim, 2007). The decision-making process between tooth retention and extraction is difficult to investigate. A tooth may be functioning; however, multi-factorial risks may lead to extraction upon endodontic or restorative treatment attempts (Wolcott and Meyers, 2006). This is complicated by countless natural or pathological variations, different treatment planning options, a clinician’s attitude and/or skillfulness, and patient preferences. Altogether, limitations in study design become apparent.
In spite of the existence of good evidence, many myths regarding endodontic treatment have spread, including the notion to connect “failing” endodontic cases and reported endodontic outcome rates with general tooth retention to support the need for implants (Ruskin et al., 2005). This has been done repeatedly and falsely without addressing the failures, longevity, and, particularly, complications associated with implants (Lundgren et al., 2008). Nevertheless, evidence exists that the loss rate of implants is higher than that of natural teeth in clinically well-maintained patients (Tomasi et al., 2008).
Benefits of Implants
In the past, clinicians used various now-obsolete implant designs that healed by fibro-osseous integration. Modern dental implantology began with the introduction of screw-type, root-form implants healing by osseointegration, with direct apposition of vital bone to titanium surfaces (Albrektsson et al., 1986). These implants added great benefit for patients with fully or partially edentulous situations. Modern dental implants are among the greatest advancements in dentistry; however, can this benefit all clinical situations? Posterior edentulism would be the perfect situation, making partial dentures unnecessary. For single teeth requiring treatment, however, general options include restoration, extraction without replacement, replacement by fixed partial dentures (FPD) on natural teeth, or implants.
Fixed partial dentures are less well-regarded today, since their use requires preparation of adjacent teeth and the sacrifice of healthy tooth structure. Although historically very successful, survival rates of FDPs are inferior to single-unit implants (Torabinejad et al., 2007), particularly when abutment teeth were endodontically treated (De Backer et al., 2008). Thus, proper use of dental implants provides benefits that could not be imagined in the past.
Success vs. Survival; Implants and Endodontics
The term ‘survival’ never entered endodontic outcome assessment until implants arrived. Essentially, the resolution of apical periodontitis, together with asymptomatic responses, is considered endodontic success (Strindberg, 1956; Ørstavik et al., 1996). For implants, osseointegration of an implant, with or without peri-implantitis, or loss of bone is considered survival, not success. Thus, comparing implants and endodontically treated teeth on the basis of endodontic outcome is a difficult endeavor. Strindberg’s and Ørstavik’s criteria (PAI index) are almost ubiquitously accepted for non-surgical endodontics. Surgical outcome is commonly assessed by Rud et al.’s (1972) or Molven et al.’s (1987) criteria. The implant field lacks a singular definition of success. The latest guidelines of the Academy of Osseointegration describe “the desired outcome of successful implant therapy” as “not only the achievement of the therapeutic goal but the maintenance of a stable, functional and esthetically acceptable tooth replacement for the patient” (Academy of Osseointegration, 2010) and list only “variations from the desired outcome of implant placement” in lieu of defined outcome criteria. These variations may include implant mobility or loss, inability to restore the implant, persistent pain, neuropathy and/or loss of function, persistent peri-implant radiolucency, progressive bone loss, increased probing depths, persistent uncontrolled inflammation and/or infection, prosthesis instability, fractured or loosened occlusal materials or prosthetic components, and implant fractures. This derives from many historic outcome criteria (Albrektsson et al., 1986; Smith and Zarb, 1989; Buser et al., 1991). Probably the most widely used are Albrektsson’s criteria, their revision by Smith and Zarb, and Buser’s criteria. Whereas endodontic success criteria are generally rather strict, implant criteria offer much greater variety for the definition of success. According to Albrektsson, success is defined as the absence of mobility, no evidence of peri-implant radiolucency, less than 0.2 mm of bone loss annually after the first year of service, and the absence of persistent and/or irreversible signs and symptoms such as pain, infection, neuropathies, paresthesia, or any violation of the mandibular canal. Buser includes no mobility, absence of persistent subjective complaints (including pain, foreign body sensations, and/or dysesthesia), but differs from Albrektsson in describing the absence of a continuous radiolucency around the implant as a positive outcome. In other words, the bony attachment of the implant should be maximal according to Albrektsson, but may be almost completely lost according to Buser to be successful, thus making this marginally different from survival. Implant survival has frequently been documented as an outcome measure (Iqbal and Kim, 2007). For example, a meta-analysis of implant outcome included studies using either Albrektsson’s or Smith and Zarb’s criteria “as a useful yardstick”, or that “sufficiently described criteria for failure or survival” (Lindh et al., 1998). A systematic review and qualitative analysis of implant studies spanning 20 years found the majority of studies using survival over success assessment (Bhatavadekar, 2010). This is significant because a distinct difference exists between outcome rates obtained from success vs. survival analysis. For 1,022 implants observed over 7 years, cumulative survival was 92.2%, but cumulative success was only 83.4% (Brocard et al., 2000). Cumulative implant survival/success rates of 95.6% [survival]/75.6% [success] were found for implants supporting single-tooth prostheses, of 94.4%/76.3% for cantilever fixed-partial prostheses, of 96.1%/73.8% for fixed-partial prostheses, of 100%/63.8% for fixed complete prostheses, of 90.6%/70.6% for implant-/tooth-supported prostheses, and of 95.7%/78.6% for overdentures (Romeo et al., 2004).
Thus, it is difficult, if not prohibitive, to compare endodontic outcome studies with strictly defined success criteria with implant outcome data based on survival. If a positive outcome for teeth was defined as retention without symptoms, regardless of the periapical status, the survival of endodontically treated teeth is as high as that of implants. If survival is used as the measure (Iqbal and Kim, 2007; Ng et al., 2011), it provides a unit-to-unit, tooth-to-implant comparison, rather than a comparison of a functional unit with healing of an inflammatory process. Based on data from a health insurance carrier, 1,462,936 teeth with primary endodontic treatment were followed over 8 years (Salehrabi and Rotstein, 2004). Of these teeth, 97.0% were retained with the primary endodontic treatment still in place, and 3.0% received surgical or non-surgical re-treatment or were extracted. Similarly, 1,557,547 endodontically treated teeth were followed for 5 years, with a 92.9% survival rate. In a meta-analysis, no significant difference was found between restored single-unit implants (95%) and endodontically treated teeth (94%) over 6 years (Iqbal and Kim, 2007) (Fig. 1).
Figure 1.
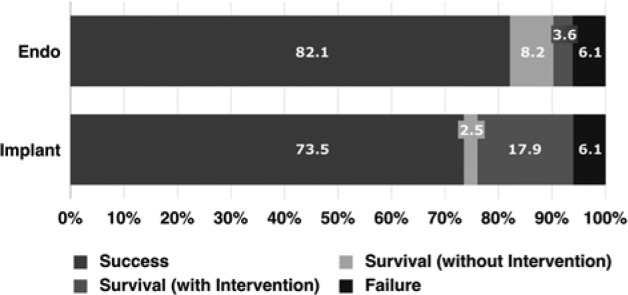
Overall reported cumulative survival rates for restored single-unit implants and endodontically treated teeth. Modified from Iqbal and Kim, 2007.
Prognosis of Implants
Implant studies frequently reported outcome rates exceeding 95%. Meta-analyses found success rates of 96.7% to 97.5% for single-unit restorations and 92.5% to 93.6% for fixed partial restorations over 6 to 7 years (Lindh et al., 1998). A large-scale study described cumulative survival rates of 92% for 13,049 two-stage implants over 15 years and 85% for 5,515 one-stage surgery implants over 10 years, including early failures (Boioli et al., 2001). Again, it has to be made very clear that “success” may frequently address “survival” (Listgarten, 1997), and that sometimes, even “ailing” or “failing” implants were deemed successful (Zitzmann et al., 2009). den Hartog and co-workers reported a survival rate of 95.5% after 1 year of follow-up; however, these authors also noted that esthetic outcome, soft-tissue aspects, and patient satisfaction were less likely mentioned (den Hartog et al., 2008).
Complications remain frequently unaddressed in dental implantology. Peri-implantitis was associated with 9.7% of single-unit implants, bone loss exceeded 2 mm in 6.3%, and prosthetic or abutment screws loosened on 12.7% of implants after only 5 years (Salinas and Eckert, 2010). Within a relatively short-term 5-year follow-up, the frequency of peri-implantitis and severe bone loss challenges long-term stability. Consistent with these data, 16% to 28% of implants were found to be afflicted by peri-implantitis, with an increasing percentage in situations with multiple implants (Lundgren et al., 2008). Peri-implantitis is a form of late failure (Quirynen et al., 2007). In advanced stages, it may present with pain or bleeding on probing (Heitz-Mayfield, 2008). Although, clinically, peri-implantitis is comparable with progressive periodontal disease on a tooth, a tooth will become mobile, whereas an implant with remaining areas of osseointegrated surface will not. When an implant must be removed, it may be a traumatic intervention with significant bone loss. A second or even third “replacement” implant will have to be placed under much more difficult circumstances. Implants may need replacement over a patient’s lifetime. Natural teeth exceed the life expectancy of implants at ten-year observation points, including endodontically treated or periodontally compromised teeth (Holm-Pedersen et al., 2007).
Although good follow-up data exist for implants, the question of true long-term success and/or survival still needs to be answered. However, a recent study provided 20-year data on implants with a rough, microporous surface in partially edentulous situations, with 72 of 145 original implants remaining for follow-up after the exclusion of deceased patients and those lost to follow-up (Chappuis et al., 2013). Of these implants, 68% had been without technical complications. The success/survival rate was 75.8%/89.5%. Still, these long-term data are scarce. Even after the completion of craniofacial development, implant placement in young adults may therefore be viewed with caution, since restorability options in areas where implants were previously lost have yet to be explored on a higher evidence level.
Based on the critical evaluation of published data and methods used in clinical studies, reported outcome rates for implants may be greatly inflated. Furthermore, implant companies have supported a majority of outcome studies, begging possible bias (Bhatavadekar, 2010; Popelut et al., 2010). A systematic review of industry-sponsored implant trials revealed that 63% of studies did not disclose funding, 66% of trials had a risk of bias, and trials with unknown funding or industry sponsorship had lower annual failure rates compared with those of non-industry-associated trials (Popelut et al., 2010).
Strict inclusion/exclusion criteria are common for implant trial participants (Listgarten, 1997), effectively excluding patients seen in an average clinical setting, particularly those who suffer from diseases or habits that have a clinically negative effect on implants. This refers to patients who smoke (Mundt et al., 2006), regularly consume alcohol (Galindo-Moreno et al., 2005), and have poor oral hygiene (Schou et al., 2002), Type IV bone, or other para-functions and/or bruxism (Misch and Wang, 2003). In particular, bruxism may be a primary force for early implant failure. In contrast to clenching, where only vertical forces are exerted, bruxism also creates lateral forces that may be less favorable. The data from a highly selected patient pool may not represent true outcome values in the general population (Tomasi et al., 2008).
Which implants are actually being evaluated must be reviewed carefully. Implants included in survival analyses should already be osseointegrated and functionally loaded (Smith and Zarb, 1989). Non-restorable and “sleeping” implants, or implants having caused iatrogenic damage to surrounding tissues, including the mandibular alveolar nerve, sinus or nasal cavities, or adjacent teeth, would not be accounted for or reported as successful (Smith and Zarb, 1989). Early failures during the osseointegration period should also not count as failures (Smith and Zarb, 1989). In fact, most survival studies counted implants after successful loading. However, a great many implant failures occur prior to osseointegration (Quirynen et al., 2007), and most losses occur between the placement of the fixture and that of the suprastructure (Tomasi et al., 2008). In a comparison of evaluation immediately after placement vs. after loading, the survival rate of single implants dropped 5.8% in the posterior mandible and 10.3% in partially or completely edentulous jaws (Morris and Ochi, 2000a). In summary, promoting to the general population success or survival rates of > 95% for implants is based on erroneous information, because these values stem from ideal situations. The outcome in the general population would be significantly lower.
Matched pairs of endodontically treated teeth and single-unit implants were compared at the University of Minnesota (Doyle et al., 2006). This university-based study, without industry support, provided more objective and non-biased information. After 7 to 9 years, the positive outcome was 74% for implants and 84% for endodontically treated teeth (Fig. 2). The rate of complications and necessary interventions was significantly higher in the implant group, and it took longer for patients to adjust to the implant restoration. However, similar satisfaction levels with implants or endodontically treated teeth were also reported (Gatten et al., 2011). The survival of restored endodontically treated teeth (83.34%) and implants (80.8%) in the same arch showed no significant difference after 8 years (Vozza et al., 2011). All reported success/survival rates, however, did not guarantee a favorable prognosis, given individual clinical circumstances (John et al., 2007). The decision for tooth or implant should not be made based on outcome analysis (Iqbal and Kim, 2007).
Figure 2.
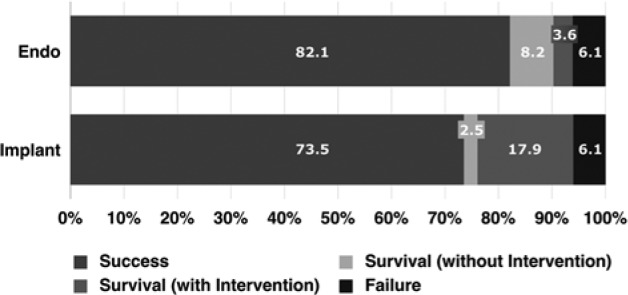
Long-term outcome of restored single-unit implants and endodontically treated teeth in a non-selected patient population. Modified from Doyle et al., 2006.
Prognosis of Endodontically Treated Teeth
Strindberg’s criteria (Strindberg, 1956) and the PAI index (Ørstavik et al., 1996) were introduced above as primary assessment tools for endodontic outcome. These criteria are generally more strict than those for implants (Iqbal and Kim, 2007). A systematic review and meta-analysis of primary endodontic treatment found cumulative success rates of 68% to 85% for the decades between 1950 and 2000, ranging from 69.6% to 81.4% for teeth with and 82.1% to 90.1% without apical radiolucency (Ng et al., 2007). However, many datasets derived from treatments by pre-doctoral students who lacked experience. Some studies had only 6-month follow-ups. Short-term follow-ups may not reflect true endodontic outcomes. Endodontic healing may take up to 4 years (Ørstavik et al., 1996), and even later long-term healing has been reported (Molven et al., 2002).
Old and New Techniques in Endodontics and Implantology
Twenty-first Century endodontics enjoys many modern instruments and new equipment, previously unknown and gradually introduced since the 1990s. Many studies that were included in meta-analyses used techniques that are now outdated and obsolete. A recent randomized clinical trial comparing one- vs. two-visit treatments of teeth with apical periodontitis applied modern techniques and found a mean 92.9% success according to the PAI index after 2 years of follow-up (Paredes-Vieyra and Jimenez Enriquez, 2012). Key to this outcome may have been the use of the dental microscope and biologically adequate instrumentation for larger sizes with activated irrigation. Modern implementation in endodontics includes electrometric length measurement devices for accurate and objective canal length determination, the microscope for better visualization and identification of canals (Fig. 3), rotary nickel-titanium instruments to prepare canals more easily and safely, ultrasonic preparation, improved disinfection protocols, and, most recently, cone beam computed tomography.
Figure 3.
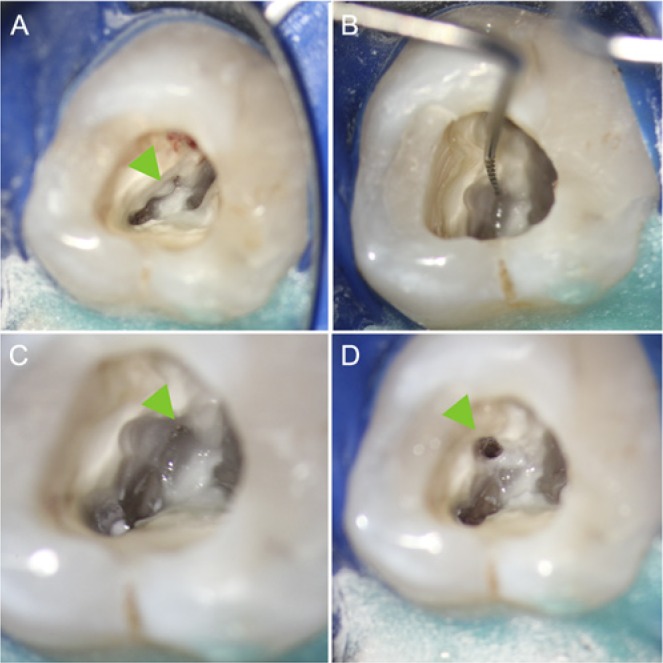
Modern microendodontic procedure: identification and instrumentation of a calcified second mesiobuccal canal (MB2) in a first maxillary molar. (A) Overview after access cavity was prepared. Overhanging dentin covers MB2 (arrow)(10x magnification). (B) Identification of MB2 orifice with micro-instrument after ultrasonic removal of obstructing dentin (10x). (C) Initial preparation of MB2 (arrow) to allow for straight-line access (16x). (D) Fully instrumented MB2 canal prior to root filling (10x). Note mesial relocation of the orifice after complete debridement and instrumentation (arrow). Endodontic treatment by first author.
The inclusion of data ranging over more than 5 or 6 decades for outcome analysis is problematic. Ng et al. (2007, 2008) calculated cumulative success using studies dating back as far as 1922 for primary endodontic treatment and back to 1961 for non-surgical retreatment. For better illustration, this may include studies prior to ISO standardization, modern disinfectants, and intra-canal medications (e.g., sodium hypochlorite and calcium hydroxide) or obturation techniques such as silver points or Kloroperka fillings. This would be comparable with calculating cumulative success rates for dental implants with the inclusion of blade implants or other designs that heal by fibro-osseous integration. Rather, the focus should be on the modern advances and techniques in either field.
Implants with rough topographies, such as acid-etched or sand-blasted surfaces, are seen as a significant advancement in implantology. However, these are technically still implants that heal by osseointegration. Rough-surfaced implants have demonstrated excellent survival rates of 97% to 98% (Kotsovilis et al., 2009). Although the increase in surface roughness was reported to facilitate biofilm formation (Subramani et al., 2009), controversial reports exist on whether rough-surfaced implants were more susceptible to peri-implantitis than were machine-surfaced implants (Wennström et al., 2004). Given the generally excellent outcomes of osseointegration with modern techniques, however, the focus in implantology has shifted away from general implant survival or success to marginal bone level changes, which have been reported to range between 0.24 (± 0.10) mm and 0.75 (± 0.05) mm with modern implant systems (Laurell and Lundgren, 2011).
In regard to endodontically treated teeth, the focus should shift to the overall picture of tooth retention, including the advances not only in primary endodontic therapy, but also in modern endodontic re-treatment, if necessary.
Endodontic Microsurgery -Ultimate Endodontic Procedure to Save Teeth
Failure of primary endodontic treatment leaves 3 choices: extraction and surgical or non-surgical re-treatment. For non-surgical re-treatment, only data with historical techniques exist. A weighted pooled success rate of 77.2% has been reported with data from 1961 to 2005 (Ng et al., 2008). Re-treatment of failed endodontic cases with apical periodontitis and altered canal morphology such as transportation demonstrated only 40% success (Gorni and Gagliani, 2004). For these situations, or when disassembly of the existing restoration could lead to non-restorability, surgical re-treatment may be advised as a less invasive option, although non-surgical re-treatment is generally preferred (Karabucak and Setzer, 2007).
A systematic review of surgical endodontic outcome found success rates from 37% to 91%; however, these included historical data with traditional techniques as well as modern studies (Friedman, 2005). Traditional root-end surgery, apicoectomy, essentially used a bur attached to a straight handpiece, a beveled resection, root-end preparation at an inadequate angle, and a retrograde amalgam filling. The success rate of traditional apicoectomy was reported to be 59.0% (Setzer et al., 2010). Modern microsurgical techniques include ultrasonic instruments for root-end preparation along the long axis of the root and an operating microscope to identify the complexity of the canal anatomy on the resected root surface at high magnification (12-24x) (Kim and Kratchman, 2006). Biocompatible root-end filling materials such as mineral trioxide aggregates (MTA) have demonstrated favorable healing (Baek et al., 2005). Two meta-analyses (Setzer et al., 2010) that focused on contemporary microsurgical techniques on teeth with only endodontic pathology but good periodontal supports, using ultrasonic root-end preparation and modern root-end filling materials, found cumulative success rates of 91.4% to 93.5% after at least one year of follow-up.
Practitioner-specific Treatment Planning and Perception
It has been argued that even restorable teeth with apical periodontitis (Greenstein et al., 2007) or needing non-surgical re-treatment (Dechouniotis et al., 2010) should be extracted in favor of implants. This trend is increasingly observed as individual specialization leads to narrower views of other fields of dentistry. This may lead to a tendency to pursue the one well-known treatment concept (Avila et al., 2009). More than 300 dentists who graduated over the past 30 years were surveyed to evaluate the perceived success rates of endodontic treatment and implant therapy (Stockhausen et al., 2011). Of these, 49% were not aware that different criteria existed for implants and endodontic therapy. A further 30% believed that root canal treatment of teeth with necrotic pulps had a higher success rate than with implants; however, overall, they perceived a superior outcome with implants.
Periodontal and Restorative Aspects
Today, too many teeth are extracted in favor of implants, since extraction is perceived as easier and more lucrative than saving a natural tooth, which may require more knowledge for proper periodontal and restorative treatment planning (Ricci et al., 2011). Extraction and implant placement have been recommended for periodontally compromised teeth, in esthetically challenging situations, with the presence of apical periodontitis, or when re-treatment is needed (Greenstein et al., 2007). However, periodontal therapy per se has proven to be highly favorable (König et al., 2002). In fact, teeth with moderate vertical bone loss, even with furcation involvement, have a good prognosis if proper periodontal treatment is rendered.
Dental restorations on teeth have a good long-term prognosis. Restorations on implant fixtures have a lower life expectancy over 5 to 10 years than the implant itself (Pjetursson et al., 2004) and are more susceptible to biological and technical complications (Goodacre et al., 2003). Implant loss may pose significant difficulties, in particular in extensive restorations that combine several units, potentially causing irreversible damage. Problems related to conventional restorations are easier to correct in a majority of situations.
Esthetically, the anterior maxilla is the most challenging and complicated to restore. Satisfactory esthetics and gingival architecture are significantly more difficult to achieve with implants, in particular with a high smile line, greater distances between inter-proximal contact point and alveolar bone, or a thin, scalloped periodontal biotype. The distance from contact point to alveolar bone should not exceed 4 mm in patients with a thin, scalloped periodontal biotype to restore the papilla between tooth and implant. The super-eruption of natural teeth, even in patients with otherwise complete craniofacial growth, may lead to esthetically displeasing horizontal steps at the incisor line and the gingival margins between implants and teeth (Bernard et al., 2004). Because of increasing esthetic concerns, more clinicians resort to tooth preservation in demanding situations.
Factors such as periodontal and endodontic status, prosthodontic issues, including the anatomical crown-root ratio, crown or root fractures, and the remaining tooth structure will have a decisive impact on whether a tooth can and/or should be preserved, including the need for 4 to 5 mm of supra-osseous hard tissue structure with 3 mm of biological width and 1 to 2 mm of ferrule. The latter may be achieved by crown-lengthening or orthodontic extrusion. However, tooth preservation must fit the overall treatment plan and meet the patient’s expectations and financial abilities.
Conclusion
Market strategies and economic forces have resulted in an ongoing commercialization of clinical practice. If dental education becomes dominated by companies rather than by educators or experienced clinicians, or if fewer cases are handled by specialists, we must not be surprised when the number of implant and/or endodontic complications and/or failures will increase. The survival of implants placed by inexperienced practitioners was 73.0% compared with 95.5% by implant specialists (Morris and Ochi, 2000a,b). A comparison of tooth survival rates after endodontic treatment by endodontic specialists vs. general practitioners, in a multi-center study consisting of 350 teeth that met the inclusion criteria, showed a difference of only 98.1% vs. 89.7% (Alley et al., 2004).
Both implants and endodontically treated teeth demonstrate significant outcome rates if the treatments are appropriately chosen and rendered. However, a missing tooth is irreversibly gone, and a tooth should be removed only after worthwhile deliberation. There is no lifetime guarantee for either a natural tooth or an implant. Both options should be seen as complementing each other, not as competing, and should serve the overall goal in dentistry, the long-term health and benefit of the patient, being least invasive and incorporating function, comfort, and esthetics. To achieve these goals, it is important for clinicians to be fully aware of true long-term outcomes of both implants and endodontically treated teeth.
Footnotes
The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Academy of Osseointegration (2010). Guidelines of the Academy of Osseointegration for the provision of dental implants and associated patient care. Int J Oral Maxillofac Implants 25:620-627 [PubMed] [Google Scholar]
- Albrektsson T, Zarb GA, Worthington P, Eriksson AR. (1986). The long-term efficacy of currently used dental implants: a review and proposed criteria of success. J Oral Maxillofac Implants 1:11-25 [PubMed] [Google Scholar]
- Alley BS, Kitchens GG, Alley LW, Eleazer PD. (2004). A comparison of survival of teeth following endodontic treatment performed by general dentists or by specialists. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98:115-118 [DOI] [PubMed] [Google Scholar]
- Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. (2009). A novel decision-making process for tooth retention or extraction. J Periodontol 80:476-491 [DOI] [PubMed] [Google Scholar]
- Baek SH, Plenk H, Jr, Kim S. (2005). Periapical tissue responses and cementum regeneration with amalgam, super-EBA and MTA as root-end filling materials. J Endod 31:444-449 [DOI] [PubMed] [Google Scholar]
- Bernard JP, Schatz JP, Christou P, Belser U, Kiliaridis S. (2004). Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults. A retrospective study. J Clin Periodontol 31:1024-1028 [DOI] [PubMed] [Google Scholar]
- Bhatavadekar N. (2010). Helping the clinician make evidence-based implant selections. A systematic review and qualitative analysis of dental implant studies over a 20 year period. Int Dent J 60:359-369 [PubMed] [Google Scholar]
- Boioli LT, Penaud J, Miller N. (2001). A meta-analytic, quantitative assessment of osseointegration establishment and evolution of submerged and non-submerged endosseous titanium oral implants. Clin Oral Implants Res 12:579-588 [DOI] [PubMed] [Google Scholar]
- Brocard D, Barthet P, Baysse E, Duffort JF, Eller P, Justumus P, et al. (2000). A multicenter report on 1,022 consecutively placed ITI implants: a 7-year longitudinal study. Int J Oral Maxillofac Implants 15:691-700 [PubMed] [Google Scholar]
- Buser D, Weber HP, Brägger U, Balsiger C. (1991). Tissue integration of one-stage ITI implants: 3-year results of a longitudinal study with hollow-cylinder and hollow-screw implants. Int J Oral Maxillofac Implants 6:405-412 [PubMed] [Google Scholar]
- Chappuis V, Buser R, Brägger U, Bornstein MM, Salvi GE, Buser D. (2013). Long-term outcomes of dental implants with a titanium plasma-sprayed surface: a 20-year prospective case series study in partially edentulous patients. Clin Implant Dent Relat Res [Epub ahead of print 3/18/2013] (in press). [DOI] [PubMed] [Google Scholar]
- De Backer H, Van Maele G, De Moor N, Van den Berghe L. (2008). Long-term results of short-span versus long-span fixed dental prostheses: an up to 20-year retrospective study. Int J Prosthodont 21:75-85 [PubMed] [Google Scholar]
- Dechouniotis G, Petridis XM, Georgopoulou MK. (2010). Influence of specialty training and experience on endodontic decision making. J Endod 36:1130-1134 [DOI] [PubMed] [Google Scholar]
- den Hartog L, Slater JJ, Vissink A, Meijer HJ, Raghoebar GM. (2008). Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol 35:1073-1086 [DOI] [PubMed] [Google Scholar]
- Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR. (2006). Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod 32:822-827 [DOI] [PubMed] [Google Scholar]
- Friedman S. (2005). The prognosis and expected outcome of apical surgery. Endod Topics 11:219-262 [Google Scholar]
- Galindo-Moreno P, Fauri M, Avila-Ortiz G, Fernández-Barbero JE, Cabrera-León A, Sánchez-Fernández E. (2005). Influence of alcohol and tobacco habits on peri-implant marginal bone loss: a prospective study. Clin Oral Implants Res 16:579-586 [DOI] [PubMed] [Google Scholar]
- Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N. (2011). Quality of life of endodontically treated versus implant treated patients: a university-based qualitative research study. J Endod 37:903-909 [DOI] [PubMed] [Google Scholar]
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. (2003). Clinical complications with implants and implant prostheses. J Prosthet Dent 90:121-132 [DOI] [PubMed] [Google Scholar]
- Gorni FG, Gagliani MM. (2004). The outcome of endodontic re-treatment: a 2-yr follow-up. J Endod 30:1-4 [DOI] [PubMed] [Google Scholar]
- Greenstein G, Greenstein B, Cavallaro J. (2007). Prerequisite for treatment planning implant dentistry: periodontal prognostication of compromised teeth. Compend Contin Educ Dent 28:436-446 [PubMed] [Google Scholar]
- Heitz-Mayfield LJ. (2008). Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35(8 Suppl):292S-304S [DOI] [PubMed] [Google Scholar]
- Holm-Pedersen P, Lang N, Müller F. (2007). What are longevities of teeth and oral implants? J Clin Oral Implant Res 18(Suppl 3):15-19 [DOI] [PubMed] [Google Scholar]
- Iqbal MK, Kim S. (2007). For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants 22(Suppl):96-116 [PubMed] [Google Scholar]
- John V, Chen S, Parashos P. (2007). Implant or the natural tooth—a contemporary treatment planning dilemma? Aust Dent J 52(1 Suppl):138-150 [DOI] [PubMed] [Google Scholar]
- Karabucak B, Setzer F. (2007). Criteria for the ideal treatment option for failed endodontics: surgical or nonsurgical? Compend Contin Educ Dent 28:391-397 [PubMed] [Google Scholar]
- Kim S, Kratchman S. (2006). Modern endodontic surgery concepts and practice: a review. J Endod 32:601-623 [DOI] [PubMed] [Google Scholar]
- König J, Plagmann HC, Rühling A, Kocher T. (2002). Tooth loss and pocket probing depths in compliant periodontally treated patients: a retrospective analysis. J Clin Periodontol 29:1092-1100 [DOI] [PubMed] [Google Scholar]
- Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. (2009). A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol 80:1700-1718 [DOI] [PubMed] [Google Scholar]
- Laurell L, Lundgren D. (2011). Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res 13:19-28 [DOI] [PubMed] [Google Scholar]
- Lindh T, Gunne J, Tillberg A, Molin M. (1998). A meta-analysis of implants in partial edentulism. Clin Oral Implants Res 9:80-90 [DOI] [PubMed] [Google Scholar]
- Listgarten MA. (1997). Clinical trials of endosseous implants: issues in analysis and interpretation. Ann Periodontol 2:299-313 [DOI] [PubMed] [Google Scholar]
- Lundgren D, Rylander H, Laurell L. (2008). To save or extract, that is the question. Natural teeth or dental implants in periodontitis-susceptible patients: clinical decision-making and treatment strategies exemplified with patient case presentations. Periodontol 2000. 47:27-50 [DOI] [PubMed] [Google Scholar]
- Misch CE, Wang HL. (2003). Immediate occlusal loading for fixed prostheses in implant dentistry. Dent Today 22:50-56 [PubMed] [Google Scholar]
- Molven O, Halse A, Fristad I, MacDonald-Jankowski D. (2002). Periapical changes following root-canal treatment observed 20-27 years postoperatively. Int Endod J 35:784-790 [DOI] [PubMed] [Google Scholar]
- Molven O, Halse A, Grung B. (1987). Observer strategy and the radiographic classification of healing after endodontic surgery. Int J Oral Maxillofac Surg 16: 432-439 [DOI] [PubMed] [Google Scholar]
- Morris HF, Ochi S. (2000a). Influence of two different approaches to reporting implant survival outcomes for five different prosthodontic applications. Ann Periodontol 5:90-100 [DOI] [PubMed] [Google Scholar]
- Morris HF, Ochi S. (2000b). Influence of research center on overall survival outcomes at each phase of treatment. Ann Periodontol 5:129-136 [DOI] [PubMed] [Google Scholar]
- Mundt T, Mack F, Schwahn C, Biffar R. (2006). Private practice results of screw-type tapered implants: survival and evaluation of risk factors. Int J Oral Maxillofac Implants 21:607-614 [PubMed] [Google Scholar]
- Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. (2007). Outcome of primary root canal treatment: systematic review of the literature - part 1. Effects of study characteristics on probability of success. Int Endod J 40:921-939 [DOI] [PubMed] [Google Scholar]
- Ng YL, Mann V, Gulabivala K. (2008). Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J 41:1026-1046 [DOI] [PubMed] [Google Scholar]
- Ng YL, Mann V, Gulabivala K. (2011). A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J 44:610-625 [DOI] [PubMed] [Google Scholar]
- Ørstavik D, Kerekes K, Eriksen HM. (1986). The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 2:20-34 [DOI] [PubMed] [Google Scholar]
- Paredes-Vieyra J, Jimenez Enriquez FJ. (2012). Success rate of single versus two-visit root canal treatment of teeth with apical periodontitis: a randomized controlled trial. J Endod 38:1164-1169 [DOI] [PubMed] [Google Scholar]
- Pjetursson BE, Tan K, Lang NP, Brägger U, Egger M, Zwahlén M. (2004). A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 15:625-642 [DOI] [PubMed] [Google Scholar]
- Popelut A, Valet F, Fromentin O, Thomas A, Bouchard P. (2010). Relationship between sponsorship and failure rate of dental implants: a systematic approach. PLoS One 5:e10274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quirynen M, Abarca M, Van Assche N, Nevins M, van Steenberghe D. (2007). Impact of supportive periodontal therapy and implant surface roughness on implant outcome in patients with a history of periodontitis. J Clin Periodontol 34:805-815 [DOI] [PubMed] [Google Scholar]
- Ricci G, Ricci A, Ricci C. (2011). Save the natural tooth or place an implant? Three periodontal decisional criteria to perform a correct therapy. Int J Periodontics Restorative Dent 31:29-37 [PubMed] [Google Scholar]
- Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G. (2004). Long-term survival and success of oral implants in the treatment of full and partial arches: a 7-year prospective study with the ITI Dental Implant System. Int J Oral Maxillofac Implants 19:247-259 [PubMed] [Google Scholar]
- Rud J, Andreasen JO, Jensen JE. (1972). Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg 1:195-214 [DOI] [PubMed] [Google Scholar]
- Ruskin JD, Morton D, Karayazgan B, Amir J. (2005). Failed root canals: the case for extraction and immediate implant placement. J Oral Maxillofac Surg 63:829-831 [DOI] [PubMed] [Google Scholar]
- Salehrabi R, Rotstein I. (2004). Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod 30:846-850 [DOI] [PubMed] [Google Scholar]
- Salinas T, Eckert S. (2010). Implant-supported single crowns predictably survive to five years with limited complications. J Evid Based Dent Pract 10:56-57 [DOI] [PubMed] [Google Scholar]
- Schou S, Holmstrup P, Stoltze K, Hjørting-Hansen E, Fiehn NE, Skovgaard LT. (2002). Probing around implants and teeth with healthy or inflamed peri-implant mucosa/gingiva. A histologic comparison in cynomolgus monkeys (Macaca fascicularis). Clin Oral Implants Res 13:113-126 [DOI] [PubMed] [Google Scholar]
- Setzer FC, Shah S, Kohli M, Karabucak B, Kim S. (2010). Outcome of endodontic surgery: a meta- analysis of the literature—part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod 36:1757-1765 [DOI] [PubMed] [Google Scholar]
- Smith DE, Zarb GA. (1989). Criteria for success of osseointegrated endosseous implants. J Prosthet Dent 62:567-572 [DOI] [PubMed] [Google Scholar]
- Stockhausen R, Aseltine R, Jr, Matthews JG, Kaufman B. (2011). The perceived prognosis of endodontic treatment and implant therapy among dental practitioners. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:e42-e47 [DOI] [PubMed] [Google Scholar]
- Strindberg LZ. (1956). The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical follow-up examinations. Acta Odontol Scand 14(Suppl 21):1-175 [Google Scholar]
- Subramani K, Jung RE, Molenberg A, Hämmerle CH. (2009). Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants 24:616-626 [PubMed] [Google Scholar]
- Tomasi C, Wennström JL, Berglundh T. (2008). Longevity of teeth and implants – a systematic review. J Oral Rehabil 35(Suppl 1):23-32 [DOI] [PubMed] [Google Scholar]
- Torabinejad M, Anderson P, Bader J, Brown LJ, Chen LH, Goodacre CJ, et al. (2007). Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent 98:285-311 [DOI] [PubMed] [Google Scholar]
- Vozza I, Barone A, Quaranta M, De Paolis G, Covani U, Quaranta A. (2011). A comparison between endodontics and implantology: an 8-year retrospective study. Clin Implant Dent Relat Res 15:29-36 [DOI] [PubMed] [Google Scholar]
- Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J. (2004). Oral rehabilitation with implant-supported fixed partial dentures in periodontitis-susceptible subjects: a 5-year prospective study. J Clin Periodontol 31:713-724 [DOI] [PubMed] [Google Scholar]
- Wolcott J, Meyers J. (2006). Endodontic re-treatment or implants: a contemporary conundrum. Compend Contin Educ Dent 27:104-110 [PubMed] [Google Scholar]
- Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. (2009). Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J 42:757-774 [DOI] [PubMed] [Google Scholar]


