Abstract
Background
Preventing anatomic failure after rotator cuff repair (RCR) remains a challenge. Augmentation with a surgical mesh may permanently reinforce the repair and decrease failure rates. The purpose of this study is to assess the postoperative outcomes of open RCR augmented with a novel reticulated polycarbonate polyurethane patch.
Materials and methods
Ten patients with supraspinatus tendon tears underwent open RCR augmented with a polycarbonate polyurethane patch secured in a 6-point fixation construct placed over the repaired tendon. Patients were evaluated with preoperative and postoperative outcome measures, including the Simple Shoulder Test, visual analog pain scale, American Shoulder and Elbow Surgeons shoulder score, Cumulative Activities of Daily Living score, and University of California, Los Angeles shoulder scale, as well as range of motion. Postoperative magnetic resonance imaging was used to evaluate repair status.
Results
Patients showed significant improvements in visual analog pain scale, Simple Shoulder Test, and American Shoulder and Elbow Surgeons shoulder scores at both 6 and 12 months postoperatively (P <.05 and P < .01, respectively). The University of California, Los Angeles postoperative score was good to excellent in 7 patients at 6 months and in 8 patients at 12 months. Range of motion in forward flexion, abduction, internal rotation, and external rotation was significantly improved at both 6 and 12 months postoperatively (P < .05 and P < .01, respectively). Magnetic resonance imaging at 12 months showed healing in 90%; one patient had a definitive persistent tear. We found no adverse events associated with the patch, including the absence of fibrosis, mechanical symptoms, or visible subacromial adhesions.
Discussion
The polycarbonate polyurethane patch was designed to support tissue in growth and enhance healing as shown by preclinical animal studies. Clinically, the patch is well tolerated and shows promising efficacy, with a 10% retear rate at the 12-month time point.
Level of evidence
Level IV, Case Series, Treatment Study.
Keywords: Rotator cuff, rotator cuff augmentation, surgical mesh, polyurethane scaffold, outcome
Outcomes after rotator cuff repairs vary widely in the literature and are dependent on factors such as age,4,9,14,19 tear size,4,9,19,26 muscle atrophy,16 and chronicity.10 Despite improved understanding of rotator cuff pathology, surgical repair techniques, and instrumentation, a certain percentage of rotator cuff repairs still go on to failure.
Historically, studies have shown that despite repair failure, patients generally maintain a high level of satisfaction.16,19,24 However, critical examination of patient outcomes and recent long-term data has shown that healing and anatomic integrity of the rotator cuff repair site produce better outcomes.4,9,11,14,19,46 This knowledge has generated a trend among shoulder surgeons to place more emphasis on reducing anatomic failure rates in rotator cuff surgery.
Anatomic failure after rotator cuff repair is generally reported to occur in 20% to 40% of primary rotator cuff repairs,4,9,11,14,24,42 and the inability to attain high healing rates has fueled the investigation of a variety of biologic and bioengineered adjuncts to rotator cuff repair. Augmentation strategies including the use of Gore-Tex,20 freeze-dried rotator cuff,32,33 periosteal patches,7 extracellular matrices,1,3,5,6,21,25,34,38,39,41 polyglycolide co-polymers,2,13,30,35,47 polytetrafluoroethylene felt,23 and chitosan-based hyaluronan polymers15 have all been investigated for augmentation scaffolding in rotator cuff tendon repair and regeneration; however, clinical data to support the use of these various devices are limited.
Reduced material properties of the rotator cuff muscle–tendon unit after a tear10,27,40,43 have significant effects on the repair and may ultimately be the driving force behind anatomic failure.4 Therefore, a possibility exists that the addition of a nonresorbable scaffold may provide permanent structural support to strengthen repairs and decrease anatomic failure rates.
The purpose of this study was to assess 6- and 12-month postoperative outcomes after mini-open rotator cuff repair augmented with a novel nonresorbable reticulated polycarbonate polyurethane patch (Biomerix, Fremont, CA).
Materials and methods
Study design
Before the initiation of this study, approval was given by the human subjects review board at the institution providing subject care (National Institute for Rehabilitation, Mexico City, Mexico) (09/08). Informed consent was obtained before enrollment into the study. A series of 10 female patients with full-thickness rotator cuff tears were identified by either ultrasound or magnetic resonance imaging (MRI). The criteria for inclusion were the presence of a full-thickness tear of either the supraspinatus or infraspinatus tendon and intact insertions of the subscapularis. All patients underwent preoperative assessment with the Simple Shoulder Test (SST), visual analog pain scale (VAS), American Shoulder and Elbow Surgeons (ASES) shoulder score, Cumulative Activities of Daily Living score, and University of California, Los Angeles (UCLA) shoulder scale. Ten open repairs with augmentation were performed by the senior surgeon (I.E.-D.). Evaluation of tendon healing and cuff integrity was performed at 6 and 12 months after surgery with the use of MRI and ultrasound. Postoperative evaluation of patients was performed at 2 weeks, 4 weeks, 3 months, 6 months, and 12 months by use of validated scoring questionnaires and physical examination.
Patient population
Before surgery, all patients underwent a 6-month trial of conservative management consisting of physical therapy and anti-inflammatory medications. The mean patient age was 56.2 years (range, 44–65 years), and the mean duration of symptoms before surgery was 16.2 months. There were 9 right shoulders and 1 left shoulder, which corresponded to 8 dominant and 2 nondominant arms. Preoperative tear width was measured anterior to posterior and averaged 20 mm (range, 10–40 mm), and tear retraction averaged 21 mm (range, 10–35 mm).
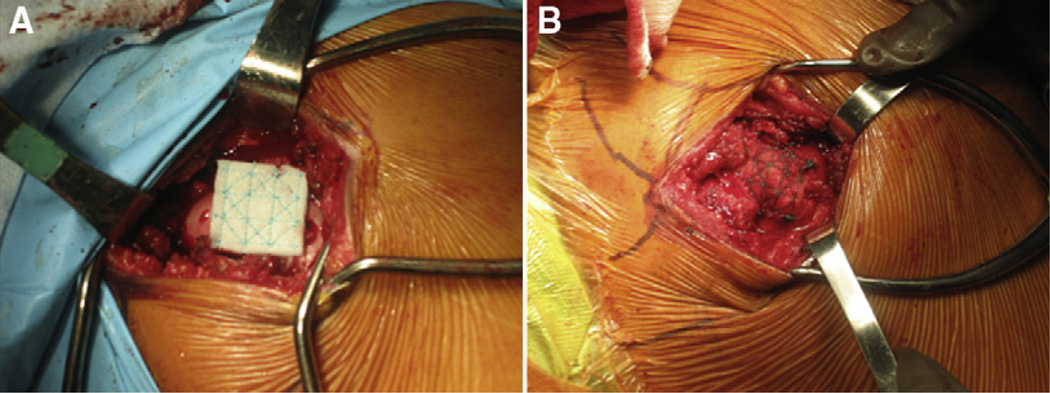
Surgical technique
All patients were positioned in the beach-chair position under regional anesthesia. A 5-cm anterolateral approach was used. A small portion of the anterior and lateral fibers of the deltoid was detached from the acromion. The subacromial space was cleared of adhesions, and a subacromial decompression and partial bursectomy were performed exposing the underlying rotator cuff tear. The size of the tear was then measured with a ruler in the anterior-to-posterior and medial-to-lateral planes. Adhesions were then released to ensure adequate cuff mobility. The supraspinatus footprint was prepared with a rasp. Five-millimeter metallic anchors with double-loaded nonabsorbable sutures were then placed in the middle of the footprint without tension. Mason-Allen knot configurations were placed into the rotator cuff tendons approximately 10 mm from the free edge of the tendon. Once the repair was completed, the repair site was then reinforced with the augmentation patch. The patch was placed over the repair site on top of the tendon, and No. 2 polyester braided sutures were used to secure the patch with 6 points of fixation along the medial and lateral borders (Fig. 1). Concomitant biceps tenotomies were performed in all cases because of fraying and inflammation of the biceps tendon.
Figure 1.
A and B, Intraoperative photographs showing 6-point suture repair configuration.
The postoperative regimen consisted of sling use for 4 weeks, after which patients commenced passive movement exercises under the supervision of a physiotherapist. Active movement exercises were commenced at 6 weeks. A cuff-strengthening exercise program was then followed, beginning at 8 weeks postoperatively.
Postoperative evaluation
Patients were evaluated postoperatively at 2 weeks, 4 weeks, 3 months, 6 months, and 12 months with validated scoring questionnaires, including the SST, VAS, ASES shoulder score, and Cumulative Activities of Daily Living score. The UCLA shoulder scale was used to evaluate patients at 6 and 12 months. Physical examination measured range of motion (ROM) for forward flexion, abduction, external rotation with the arm at the patient’s side, and internal rotation. All patients had MRI and ultrasound at 12 months postoperatively to evaluate repair site integrity.
Statistical analysis was performed with paired t tests to compare preoperative scores with 6-month and 12-month postoperative scores. The significance level was set at .05. Statistical analysis was performed with GraphPad Prism 5.0 (GraphPad Software, San Diego, CA).
Results
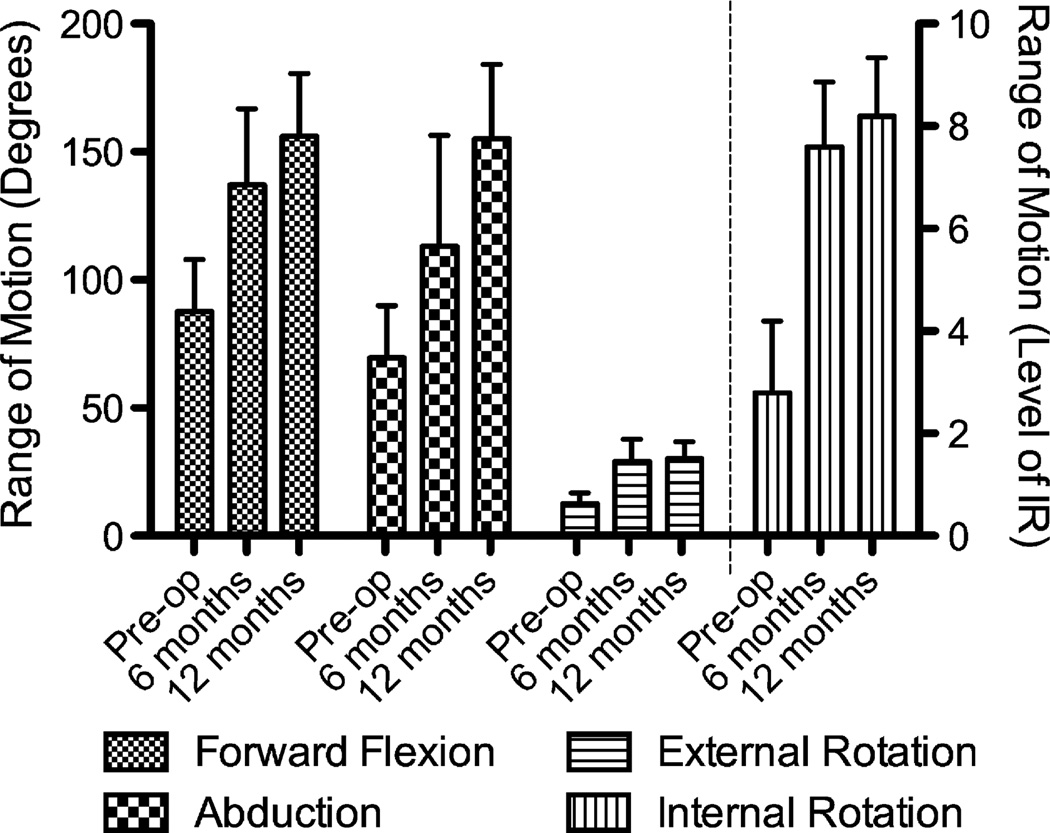
Patients showed significant improvements in VAS, SST, and ASES scores at both 6 and 12 months postoperatively (P < .05 and P < .01, respectively). The UCLA postoperative score was good to excellent in 7 of 10 patients at 6 months and good to excellent in 8 of 10 patients at 12 months. The Cumulative Activities of Daily Living score was significantly improved (P < .01) at 12 months (Table I). ROM in forward flexion, abduction, internal rotation, and external rotation was significantly improved at both 6 and 12 months postoperatively (P < .05 and P < .01, respectively) (Fig. 2).
Table I.
Subjective shoulder surveys
| Preoperatively | 6 mo postoperatively |
P value: Preoperatively vs 6 mo postoperatively |
12 mo postoperatively |
P value: Preoperatively vs 12 mo postoperatively |
|
|---|---|---|---|---|---|
| VAS (maximum 10) | 5.7 | 3.8 | .009 | 2.6 | <.001 |
| SST (maximum 12) | 3.6 | 6.5 | .022 | 7.7 | .004 |
| ASES (maximum 100) | 44.0 | 61.3 | .008 | 73.3 | <.001 |
| CADL (maximum 20) | 10.5 | 14.5 | .054 | 16.6 | .002 |
| UCLA | N/A | 27.8 | N/A | 29.2 | N/A |
| SF-P | 35.6 | 42.5 | .027 | 40.4 | .130 |
| SF-M | 45.5 | 53.1 | .099 | 51.1 | .318 |
CADL, Constant Activities of Daily Living; N/A, not applicable; SF-P, Short Form 12—Physical; SF-M, Short Form 12—Mental.
Figure 2.
ROM. Forward flexion, abduction, and external rotation in degrees. Internal rotation values correspond to the level of internal rotation: dorsum of hand to interscapular region (T7) or higher (10), dorsum of hand to twelfth dorsal vertebrae (8), dorsum of hand to waist (L3) (6), dorsum of hand to lumbosacral junction (4), dorsum of hand to buttock (2), and dorsum of hand to lateral thigh or less (0). All 4 motions showed significant improvement from preoperatively to 6 months as well as preoperatively to 12 months (P < .05).
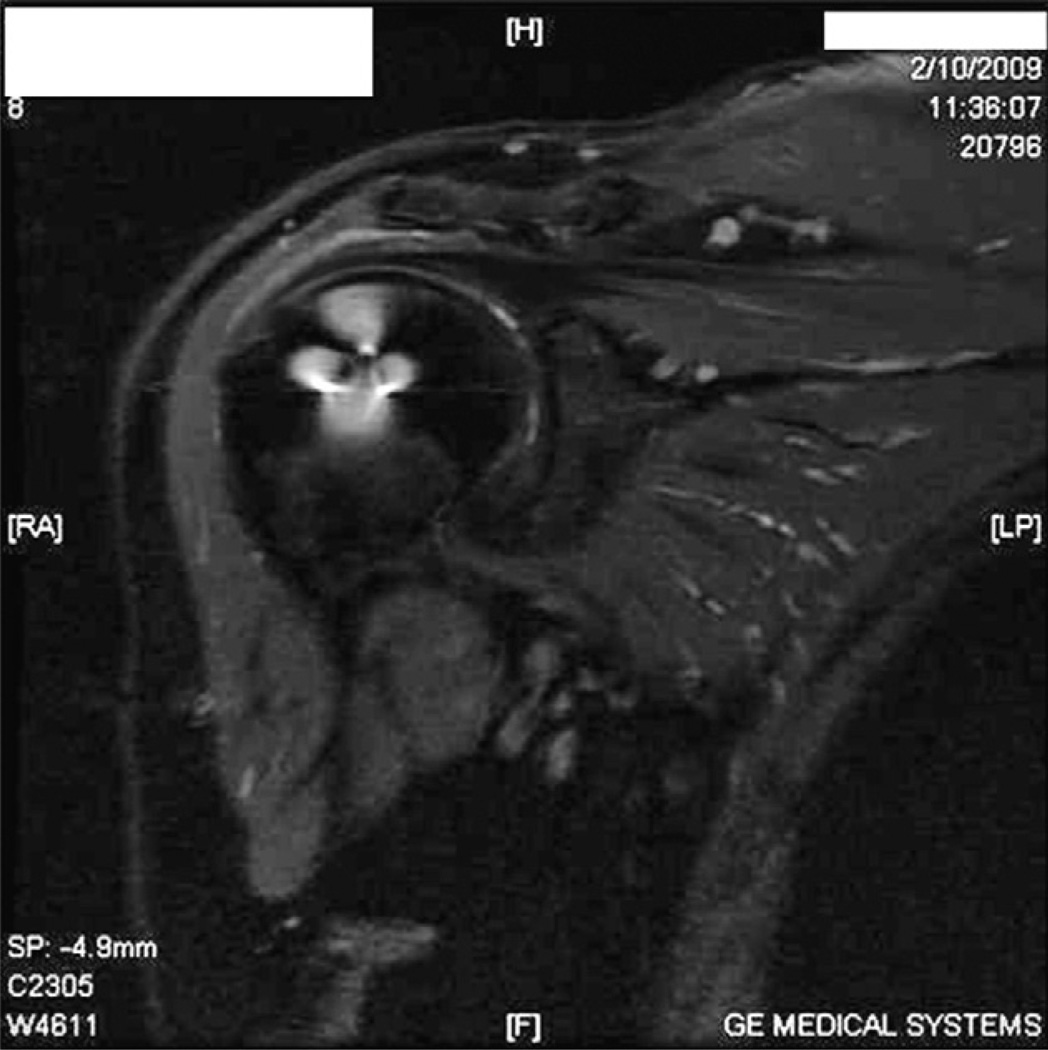
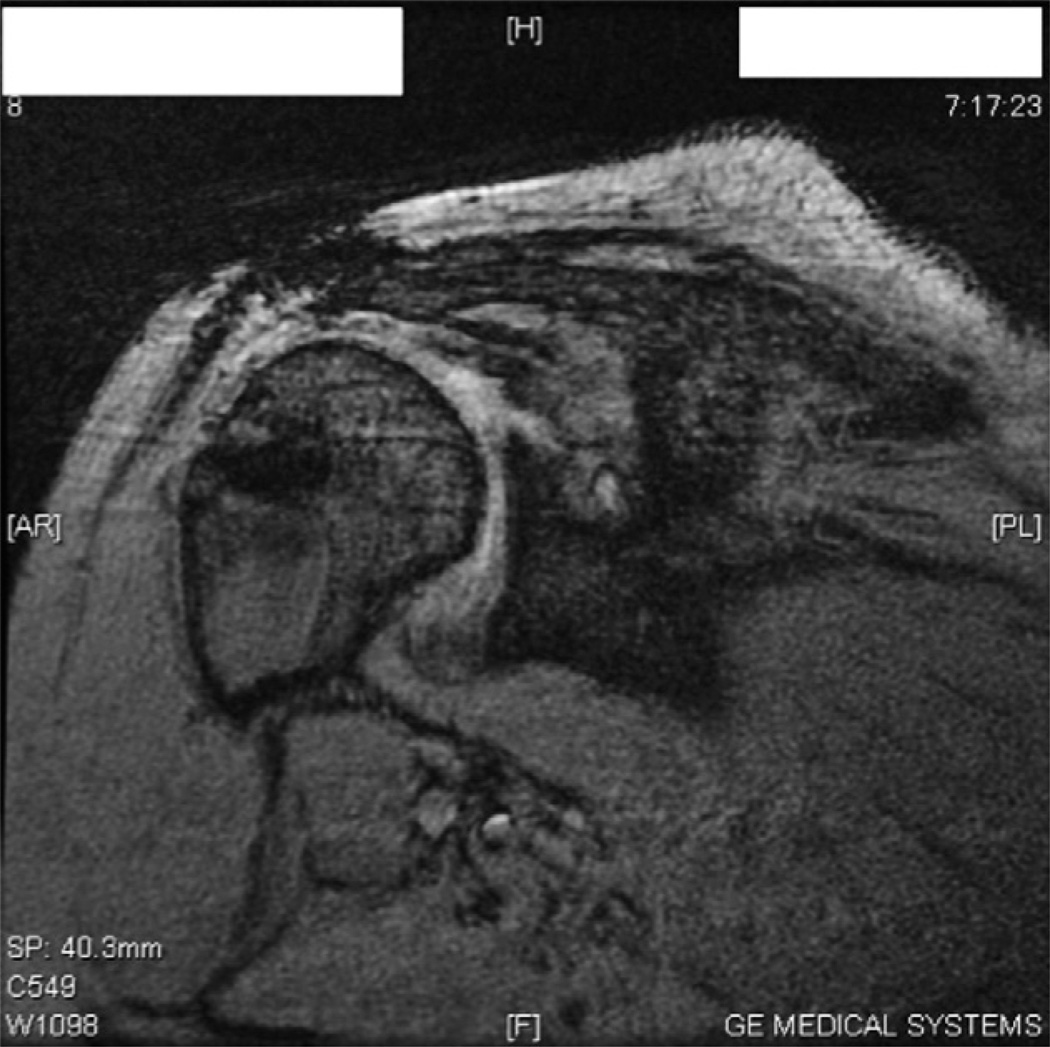
MRI and ultrasound at 12 months showed healing in 90% (9 of 10 patients) (Fig. 3); 1 patient showed a definitive retear (Fig. 4). No adverse events were found associated with the patch including the absence of fibrosis, mechanical symptoms, or visible subacromial adhesions. A summary of patient results is shown in Table II.
Figure 3.
Postoperative MRI scan showing intact rotator cuff augmented with patch.
Figure 4.
MRI scan at 12 months postoperatively showing retear of supraspinatus tendon.
Table II.
Summary of patient data, including demographic information; preoperative and 12-month postoperative data for VAS, SST, and ASES; and postoperative MRI
| Patient No. |
Sex | Age (y) | Tear size (cm2) |
VAS | Postoperatively | SST | ASES | Postoperative MRI |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Preoperatively | Preoperatively | Postoperatively | Preoperatively | Postoperatively | ||||||
| 1 | F | 65 | 20 | 2 | 0 | 5 | 7 | 73.3 | 83.3 | Intact |
| 2 | F | 51 | 62 | 7 | 4 | 7 | 12 | 36.7 | 75.0 | Intact |
| 3 | F | 59 | 20 | 5 | 4 | 4 | 2 | 36.7 | 53.3 | Intact |
| 4 | F | 52 | 40 | 5 | 1 | 1 | 9 | 40.0 | 81.7 | Intact |
| 5 | F | 51 | 70 | 8 | 3 | 3 | 7 | 26.7 | 73.3 | Intact |
| 6 | F | 44 | 40 | 4 | 1 | 6 | 7 | 56.7 | 86.7 | Intact |
| 7 | F | 64 | 80 | 4 | 3 | 3 | 6 | 53.3 | 61.7 | Intact |
| 8 | F | 53 | 50 | 8 | 3 | 6 | 10 | 41.7 | 71.7 | Retear |
| 9 | F | 61 | 30 | 7 | 4 | 1 | 8 | 51.7 | 68.3 | Intact |
| 10 | F | 62 | 15 | 7 | 3 | 0 | 9 | 23.3 | 78.3 | Intact |
Discussion
High failure rates of rotator cuff repair result from a combination of reduced tissue quality10,27,29,36,43 after chronic injury and high stress seen at the tendon-bone interface.17,18 To address these problems, many researchers have investigated the use of augmentation devices secured over the repair site to buffer physiologic demands on the tendon and enhance mechanical properties of the repair. Many types of biologic devices have been described for augmentation. Our goal was to examine the efficacy of a new biocompatible nonresorbable synthetic device applied to provide long-term structural support to rotator cuff repairs.
Biologic extracellular matrix patches are composed of a collagenous matrix derived from xenogeneic or allogeneic tissue depending on the manufacturer. Human sources include processed human dermal tissue, whereas xenografts are generally derived from porcine dermis or small intestine submucosa. Although these patches are marketed as acellular, it has been shown that these grafts maintain DNA,12 which may potentially incite inflammatory reactions after certain types of graft use.28,44,45,49 Malcarney et al28 described an overt inflammatory reaction in 4 of 25 patients who underwent rotator cuff augmentation with porcine small intestine submucosal implants. In an animal model, Valentin et al44 used histologic sampling to show inflammatory cellular responses in human dermal and porcine small intestine submucosal tissue grafts retrieved from Sprague-Dawley rats.
Our study used a synthetic device composed of biocompatible polycarbonate polyurethane-urea (Biomerix). Polyurethane has been found to be an innocuous polymer for soft-tissue applications in a variety of studies.8,22,31,37,48 The biologic response to supraspinatus tendon repairs augmented with a polycarbonate polyurethane patch in Sprague-Dawley rats has been examined previously, showing no inflammatory reaction on histologic sectioning and tissue in growth of 79.9%.8 Although histologic response was not examined in our study, we were unable to identify local inflammatory or adverse events associated with the polycarbonate polyurethane, consistent with previous investigations on the material.8
To shift the paradigm away from biologic resorbable augmentation, we used a synthetic nonresorbable reticulated polycarbonate polyurethane patch (Biomerix). It is difficult to compare the results of our study population with previous augmentation studies primarily because we performed augmentation on small and medium tears rather than large and massive rotator cuff tears, for which augmentation has typically been used. However, our premise was not to introduce a method of reconstructing larger cuff defects but was to address the more basic principle of anatomic failure after full-thickness tears, which is generally reported to occur in 20% to 40% of cases.4,9,11,14,24,42 In this study, we achieved a 90% healing rate at 12 months and significant improvements in postoperative clinical scoring and ROM by augmenting tears ranging from 1 to 4 cm with this device.
This study is not without limitations. The study population consisted of a small number of young female patients with only 12 months’ follow-up. The mean tear width represents small- to medium-sized tears rather than large or massive tears, which would more often necessitate augmented repair. Furthermore, without a control group, it is difficult to assess all evaluation measures, including the healing rate. However, there is very little literature currently available on the clinical performance of synthetic nonabsorbable devices, and we have shown that a polycarbonate polyurethane patch can be safely implanted and may enhance rotator cuff repair integrity and improve patient outcomes.
Conclusion
Despite improvements in rotator cuff repair techniques, anatomic failure rates after rotator cuff repair still remain high. Augmentation of the repair site with a nonresorbable scaffold may provide permanent structural support to strengthen repairs and decrease anatomic failure rates. The purpose of this study was to assess 6- and 12-month postoperative outcomes after rotator cuff repair augmented with a novel reticulated polycarbonate polyurethane patch (Biomerix) using subjective and objective outcome measurements including MRI. Clinically, the patch shows promising efficacy with a 10% retear rate at the 12-month time point. This augmentation device was well tolerated and did not show any adverse events at 12 months. This may provide a rationale for providing a permanent structural scaffold to enhance repairs and dissipate forces seen at the tendon-bone interface after rotator cuff repair.
Acknowledgments
Disclaimer
Ivan Encalada-Diaz receives research support from Biomerix. Brian J. Cole and John D. MacGillivray are Biomerix clinical advisors and hold stock options in the company. All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
This study was supported by National Institutes of Health grant T32 AR052272 (N.A.F).
References
- 1.Adams JE, Zobitz ME, Reach JS, Jr, An KN, Steinmann SP. Rotator cuff repair using an acellular dermal matrix graft: an in vivo study in a canine model. Arthroscopy. 2006;22:700–709. doi: 10.1016/j.arthro.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Aoki M, Miyamoto S, Okamura K, Yamashita T, Ikada Y, Matsuda S. Tensile properties and biological response of poly(L-lactic acid) felt graft: an experimental trial for rotator-cuff reconstruction. J Biomed Mater Res B Appl Biomater. 2004;71:252–259. doi: 10.1002/jbm.b.30084. [DOI] [PubMed] [Google Scholar]
- 3.Badhe SP, Lawrence TM, Smith FD, Lunn PG. An assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elbow Surg. 2008;17(Suppl):35S–39S. doi: 10.1016/j.jse.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 5.Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a Graft-Jacket allograft: technique and preliminary results. Arthroscopy. 2008;24:403.e1–409.e1. doi: 10.1016/j.arthro.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 6.Burkhead WZ, Schiffern SC, Krishnan SG. Use of graft jacket as an augmentation for massive rotator cuff tears. Semin Arthroplasty. 2007;18:11–18. [Google Scholar]
- 7.Chang CH, Chen CH, Su CY, Liu HT, Yu CM. Rotator cuff repair with periosteum for enhancing tendon-bone healing: a biomechanical and histological study in rabbits. Knee Surg Sports Traumatol Arthrosc. 2009;17:1447–1453. doi: 10.1007/s00167-009-0809-x. [DOI] [PubMed] [Google Scholar]
- 8.Cole BJ, Gomoll AH, Yanke A, Pylawka T, Lewis P, Macgillivray JD, et al. Biocompatibility of a polymer patch for rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2007;15:632–637. doi: 10.1007/s00167-006-0187-6. [DOI] [PubMed] [Google Scholar]
- 9.Cole BJ, McCarty LP, III, Kang RW, Alford W, Lewis PB, Hayden JK. Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elbow Surg. 2007;16:579–585. doi: 10.1016/j.jse.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Coleman SH, Fealy S, Ehteshami JR, MacGillivray JD, Altchek DW, Warren RF, et al. Chronic rotator cuff injury and repair model in sheep. J Bone Joint Surg Am. 2003;85:2391–2402. doi: 10.2106/00004623-200312000-00018. [DOI] [PubMed] [Google Scholar]
- 11.DeFranco MJ, Bershadsky B, Ciccone J, Yum JK, Iannotti JP. Functional outcome of arthroscopic rotator cuff repairs: a correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16:759–765. doi: 10.1016/j.jse.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Derwin KA, Baker AR, Spragg RK, Leigh DR, Iannotti JP. Commercial extracellular matrix scaffolds for rotator cuff tendon repair. Biomechanical, biochemical, and cellular properties. J Bone Joint Surg Am. 2006;88:2665–2672. doi: 10.2106/JBJS.E.01307. [DOI] [PubMed] [Google Scholar]
- 13.Derwin KA, Codsi MJ, Milks RA, Baker AR, McCarron JA, Iannotti JP. Rotator cuff repair augmentation in a canine model with use of a woven poly-L-lactide device. J Bone Joint Surg Am. 2009;91:1159–1171. doi: 10.2106/JBJS.H.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flurin PH, Landreau P, Gregory T, Boileau P, Brassart N, Courage O, et al. Arthroscopic repair of full-thickness cuff tears: a multicentric retrospective study of 576 cases with anatomical assessment [in French] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:31–42. doi: 10.1016/s0035-1040(05)84503-9. [DOI] [PubMed] [Google Scholar]
- 15.Funakoshi T, Majima T, Iwasaki N, Suenaga N, Sawaguchi N, Shimode K, et al. Application of tissue engineering techniques for rotator cuff regeneration using a chitosan-based hyaluronan hybrid fiber scaffold. Am J Sports Med. 2005;33:1193–1201. doi: 10.1177/0363546504272689. [DOI] [PubMed] [Google Scholar]
- 16.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am. 1999;81:1281–1290. doi: 10.2106/00004623-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Gimbel JA, Van Kleunen JP, Lake SP, Williams GR, Soslowsky LJ. The role of repair tension on tendon to bone healing in an animal model of chronic rotator cuff tears. J Biomech. 2007;40:561–568. doi: 10.1016/j.jbiomech.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Harryman DT, II, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., III Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- 20.Hirooka A, Yoneda M, Wakaitani S, Isaka Y, Hayashida K, Fukushima S, et al. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J Orthop Sci. 2002;7:451–456. doi: 10.1007/s007760200078. [DOI] [PubMed] [Google Scholar]
- 21.Iannotti JP, Codsi MJ, Kwon YW, Derwin K, Ciccone J, Brems JJ. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:1238–1244. doi: 10.2106/JBJS.E.00524. [DOI] [PubMed] [Google Scholar]
- 22.Jayabalan M, Rathinam K. Effects of biostability and morphology on host response of polyurethane-based soft tissue implants. Clin Mater. 1992;11:179–191. doi: 10.1007/978-94-011-1872-9_24. [DOI] [PubMed] [Google Scholar]
- 23.Kimura A, Aoki M, Fukushima S, Ishii S, Yamakoshi K. Reconstruction of a defect of the rotator cuff with polytetrafluoroethylene felt graft. Recovery of tensile strength and histocompatibility in an animal model. J Bone Joint Surg Br. 2003;85:282–287. doi: 10.1302/0301-620x.85b2.12823. [DOI] [PubMed] [Google Scholar]
- 24.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, et al. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. doi: 10.1177/0363546504265262. [DOI] [PubMed] [Google Scholar]
- 25.Kovacevic D, Rodeo SA. Biological augmentation of rotator cuff tendon repair. Clin Orthop Relat Res. 2008;466:622–633. doi: 10.1007/s11999-007-0112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu SH, Baker CL. Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy. 1994;10:54–60. doi: 10.1016/s0749-8063(05)80293-2. [DOI] [PubMed] [Google Scholar]
- 27.Longo UG, Franceschi F, Ruzzini L, Rabitti C, Morini S, Maffulli N, et al. Histopathology of the supraspinatus tendon in rotator cuff tears. Am J Sports Med. 2008;36:533–538. doi: 10.1177/0363546507308549. [DOI] [PubMed] [Google Scholar]
- 28.Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: a report of 4 cases. Am J Sports Med. 2005;33:907–911. doi: 10.1177/0363546504271500. [DOI] [PubMed] [Google Scholar]
- 29.Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–495. doi: 10.1302/0301-620X.88B4.16845. [DOI] [PubMed] [Google Scholar]
- 30.Moffat KL, Kwei AS, Spalazzi JP, Doty SB, Levine WN, Lu HH. Novel nanofiber-based scaffold for rotator cuff repair and augmentation. Tissue Eng Part A. 2009;15:115–126. doi: 10.1089/ten.tea.2008.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nair PD, Mohanty M, Rathinam K, Jayabalan M, Krishnamurthy VN. Studies on the effect of degree of hydrophilicity on tissue response of polyurethane interpenetrating polymer networks. Biomaterials. 1992;13:537–542. doi: 10.1016/0142-9612(92)90105-w. [DOI] [PubMed] [Google Scholar]
- 32.Nasca RJ. The use of freeze-dried allografts in the management of global rotator cuff tears. Clin Orthop Relat Res. 1988;218–26 [PubMed] [Google Scholar]
- 33.Neviaser JS, Neviaser RJ, Neviaser TJ. The repair of chronic massive ruptures of the rotator cuff of the shoulder by use of a freeze-dried rotator cuff. J Bone Joint Surg Am. 1978;60:681–684. [PubMed] [Google Scholar]
- 34.Nicholson GP, Breur GJ, Van Sickle D, Yao JQ, Kim J, Blanchard CR. Evaluation of a cross-linked acellular porcine dermal patch for rotator cuff repair augmentation in an ovine model. J Shoulder Elbow Surg. 2007;16(Suppl):S184–S190. doi: 10.1016/j.jse.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 35.Post M. Rotator cuff repair with carbon filament. A preliminary report of five cases. Clin Orthop Relat Res. 1985:154–158. [PubMed] [Google Scholar]
- 36.Rokito AS, Zuckerman JD, Gallagher MA, Cuomo F. Strength after surgical repair of the rotator cuff. J Shoulder Elbow Surg. 1996;5:12–17. doi: 10.1016/s1058-2746(96)80025-5. [DOI] [PubMed] [Google Scholar]
- 37.Sanders JE, Bale SD, Neumann T. Tissue response to microfibers of different polymers: polyester, polyethylene, polylactic acid, and polyurethane. J Biomed Mater Res. 2002;62:222–227. doi: 10.1002/jbm.10285. [DOI] [PubMed] [Google Scholar]
- 38.Schlegel TF, Hawkins RJ, Lewis CW, Motta T, Turner AS. The effects of augmentation with Swine small intestine submucosa on tendon healing under tension: histologic and mechanical evaluations in sheep. Am J Sports Med. 2006;34:275–280. doi: 10.1177/0363546505279912. [DOI] [PubMed] [Google Scholar]
- 39.Sclamberg SG, Tibone JE, Itamura JM, Kasraeian S. Six-month magnetic resonance imaging follow-up of large and massive rotator cuff repairs reinforced with porcine small intestinal submucosa. J Shoulder Elbow Surg. 2004;13:538–541. doi: 10.1016/j.jse.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 40.Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008;17(Suppl):1S–7S. doi: 10.1016/j.jse.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 41.Soler JA, Gidwani S, Curtis MJ. Early complications from the use of porcine dermal collagen implants (Permacol) as bridging constructs in the repair of massive rotator cuff tears. A report of 4 cases. Acta Orthop Belg. 2007;73:432–436. [PubMed] [Google Scholar]
- 42.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 43.Thomopoulos S, Hattersley G, Rosen V, Mertens M, Galatz L, Williams GR, et al. The localized expression of extracellular matrix components in healing tendon insertion sites: an in situ hybridization study. J Orthop Res. 2002;20:454–463. doi: 10.1016/S0736-0266(01)00144-9. [DOI] [PubMed] [Google Scholar]
- 44.Valentin JE, Badylak JS, McCabe GP, Badylak SF. Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J Bone Joint Surg Am. 2006;88:2673–2686. doi: 10.2106/JBJS.E.01008. [DOI] [PubMed] [Google Scholar]
- 45.Walton JR, Bowman NK, Khatib Y, Linklater J, Murrell GA. Restore orthobiologic implant: not recommended for augmentation of rotator cuff repairs. J Bone Joint Surg Am. 2007;89:786–791. doi: 10.2106/JBJS.F.00315. [DOI] [PubMed] [Google Scholar]
- 46.Wilson F, Hinov V, Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff 2- to 14-year follow-up. Arthroscopy. 2002;18:136–144. doi: 10.1053/jars.2002.30443. [DOI] [PubMed] [Google Scholar]
- 47.Yokoya S, Mochizuki Y, Nagata Y, Deie M, Ochi M. Tendon-bone insertion repair and regeneration using polyglycolic acid sheet in the rabbit rotator cuff injury model. Am J Sports Med. 2008;36:1298–1309. doi: 10.1177/0363546508314416. [DOI] [PubMed] [Google Scholar]
- 48.Zhang YZ, Bjursten LM, Freij-Larsson C, Kober M, Wesslen B. Tissue response to commercial silicone and polyurethane elastomers after different sterilization procedures. Biomaterials. 1996;17:2265–2272. doi: 10.1016/0142-9612(96)00055-5. [DOI] [PubMed] [Google Scholar]
- 49.Zheng MH, Chen J, Kirilak Y, Willers C, Xu J, Wood D. Porcine small intestine submucosa (SIS) is not an acellular collagenous matrix and contains porcine DNA: possible implications in human implantation. J Biomed Mater Res B Appl Biomater. 2005;73:61–67. doi: 10.1002/jbm.b.30170. [DOI] [PubMed] [Google Scholar]