Abstract
Purpose
This study was performed to evaluate the general anatomy and morphology of the nasopalatine canal using cone-beam computed tomography (CBCT) and to determine the human anatomic variability of the nasopalatine canal in relation to age and gender.
Materials and Methods
The study included 100 subjects aged between 20 and 86 years who were divided into the following 3 groups: 1) 20-34 years old; 2) 35-49 years old; 3) ≥50 years old. The subjects were equally distributed between the genders. CBCT was performed using a standard exposure and patient positioning protocol. The data of the CBCT images were sliced in three dimensions. Image planes on the three axes (X, Y, and Z) were sequentially analyzed for the location, morphology and dimensions of the nasopalatine canal by two independent observers. The correlation of age and gender with all the variables was evaluated.
Results
The present study did not reveal statistically significant differences in the number of openings at the nasal fossa; diameter of the nasal fossa openings; diameter of the incisive fossa; shape, curvature, and angulation of the canal as viewed in the sagittal sections; antero-posterior dimensions and length of the canal in the sagittal sections; or the level of division of the canal in the coronal plane by age. However, males and females showed significant differences in the length of the canal in the sagittal sections and level of the division of the canal in the coronal plane.
Conclusion
The present study highlighted important variability observed in the anatomy and morphology of the nasopalatine canal.
Keywords: Cone-Beam Computed Tomography, Anatomy, Nasopalatine Canal
Introduction
The nasopalatine canal (NPC), also known as the incisive canal or anterior palatine canal, is a long slender passage present in the midline of the anterior maxilla that connects the palate to the floor of the nasal cavity. The canal continues in the oral cavity as a single incisive foramen posterior to the central incisor teeth and in the nasal cavity as the foramina of Stenson, which are usually two in number. Through each of them passes the terminal branch of the descending palatine artery and the nasopalatine nerve, to communicate with the posterior septal branch of the spheno-palatine artery and greater palatine nerve, respectively. Thorough knowledge of the anatomical appearances and variation of the NPC is essential prior to surgical procedures like implant placement and local anesthesia in the anterior maxilla. Difficulties and anatomic limitations regarding the location of the nasopalatine canal in relation to the maxillary central incisor implants have been reported.1 Complications of implant rehabilitation include non-osseointegration of the implant due to contact with nervous tissue or sensory dysfunction.2 Recent studies have also shown that implants in the nasopalatine canal may be a viable treatment approach for the rehabilitation of the severely atrophied maxilla.3-5 Augmentation in the proximity of the incisive foramen to allow for reliable placement of implants has also been reported.6 The characteristic description of the nasopalatine canal and the knowledge of its contents and variable appearance are crucial to optimizing surgical planning and avoiding complications during implant placement in this anesthetically demanding region.
The nasopalatine duct cyst occurs in the nasopalatine or incisive canal, and it may be difficult to decide on a radiograph whether radiolucency in that area is a cyst or a large incisive foramen. Several authors have reported different dimensions of radiolucency as diagnostic of the cyst. According to Shear and Speight,7 a radiographic shadow with antero-posterior dimensions of as much as 10 mm in the incisive fossa region may be within the normal limit. However, Bodin et al8 proposed that if the radiolucency had a width exceeding 8 mm, was pronounced, and had a thin cortical border on the periphery, exploratory surgery should be considered, especially if the lesion was asymmetrically bulging; and that radiolucencies exceeding 14 mm in diameter were always cysts. Much of this uncertainty has arisen because of two-dimensional (2D) representation of the three-dimensional (3D) anatomy of the NPC on radiograph. The introduction of the 3D imaging modality CBCT and its potential for 3D CT-based surgical planning and measurements have been advantageous for evaluating the nasopalatine canal.
The aim of this study was to identify the anatomic characteristics of the nasopalatine canal in terms of its morphology, dimensions, and relation to the central incisors; to determine the occurrence of anatomical variation; and to look for any correlations of these variables with age and gender.
Materials and Methods
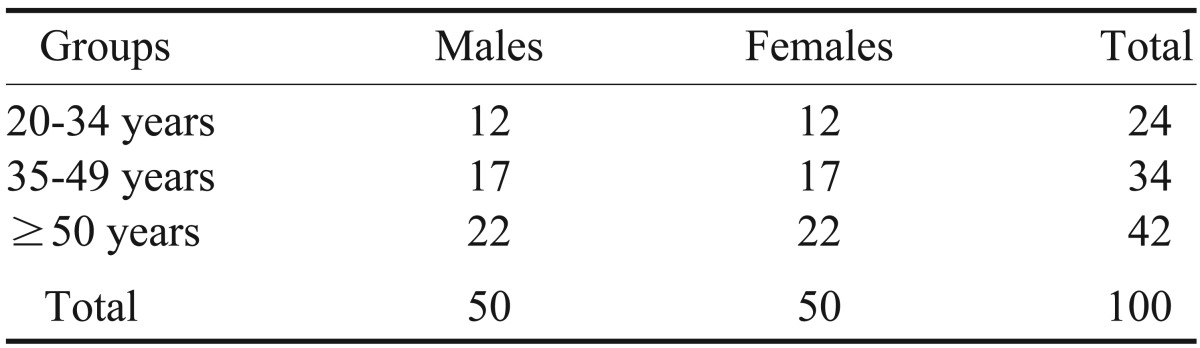
The main source of data for the study was patients reporting to the Department of Oral Medicine and Radiology between April and October 2010. The study material included 100 CBCT images that included the entire NPC in all three planes. The CBCT had been advised for evaluation of teeth in the anterior maxilla for various diagnostic purposes. The CBCT scans from the patients with nasopalatine canal pathology or impacted teeth in the region were excluded from the present study. The patients were informed about the rationale for the study and the methods applied, and informed consent was obtained. Among the 100 patients with an age range of 20 to 86 years, 50 were males and 50 were females. The patients were divided into 3 groups, details of which are given in Table 1.
Table 1.
Distribution of the patients included in the study by age and sex
The CBCT examinations were made using a Kodak 9000 3D digital imaging system (Carestream Dental LLC, Atlanta, GA, USA). The occlusal plane was positioned horizontally to the scan plane. The mid-sagittal plane was centered. The images were obtained at 70 to 74 kV, 10 mA, and 10.8 s with a voxel size of 76.5 µm3. The field of view (FOV) size was 50 mm×37 mm with a 200-µm image resolution. The acquired volumes were reformatted to images of a thickness of 200 µm.
For evaluation of the CBCT images, a 19-inch LCD monitor (HP L1910, Hewlett-Packard Development Co., Palo Alto, CA, USA) with 1280×1024 pixel resolution and a 800 : 1 contrast ratio was used. The Kodak Dental Imaging Software 6.8 Windows edition (Carestream Health Inc., St. Rochester, NY, USA) was used. The data of the CBCT images were sliced in three dimensions. Planes on the three axes (X, Y, and Z) of the CBCT images were sequentially analyzed. Two specialists in oral and maxillofacial radiology with experience of 12 years independently analyzed all of the images for NPC morphology, canal dimension, and relation to the central incisors. In case of disagreement, the observers had to reach consensus. The parameters analyzed in the study are detailed in Table 2.
Table 2.
Description of the parameters analyzed in the study
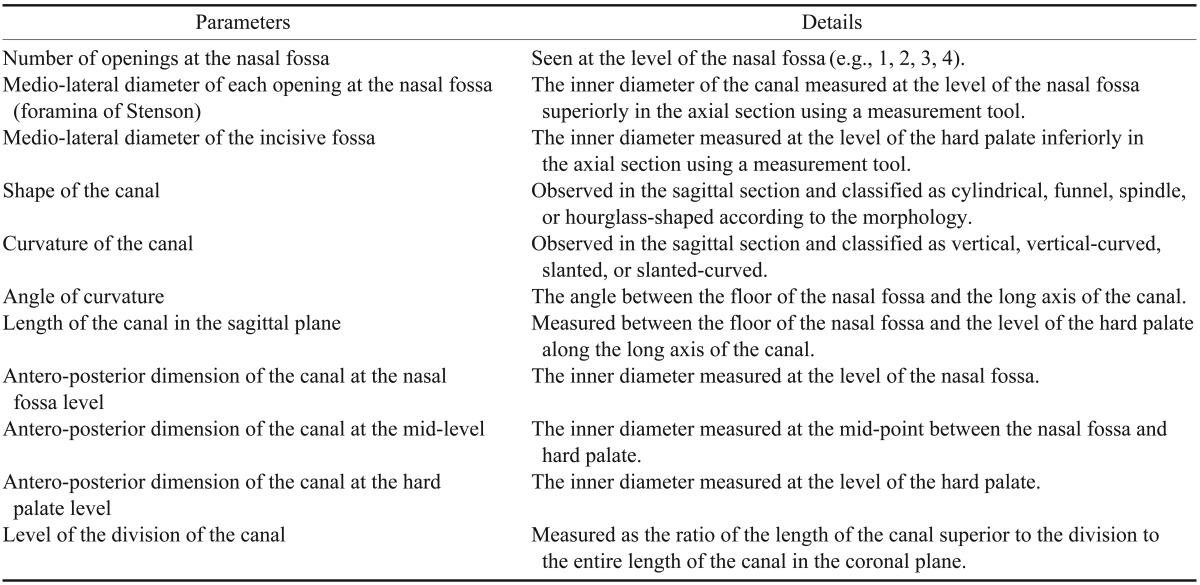
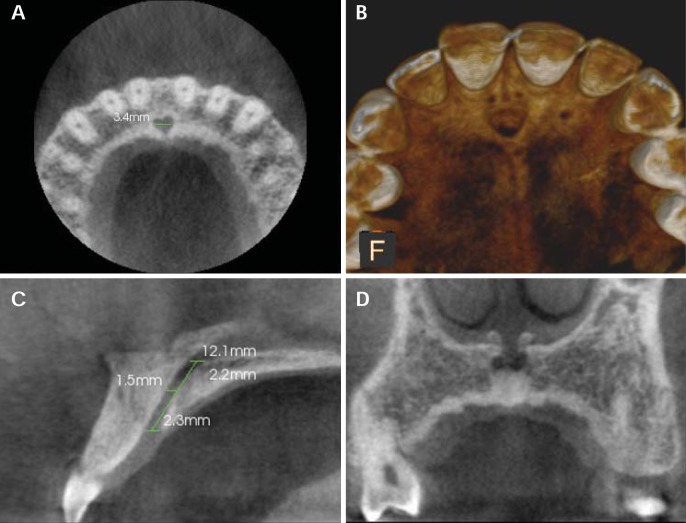
The medio-lateral diameter of the incisive fossa and foramen of Stenson and the number of openings at the nasal fossa were evaluated in the axial sections, while the shape of the canal, curvature of the canal, angle of curvature, length of the canal, and antero-posterior diameters were assessed in the sagittal slices. The level of division of the canal superior-inferiorly was evaluated in the coronal plane (Fig. 1).
Fig. 1.
The nasopalatine canal on CBCT images. A. An axial section at the level of the incisive fossa shows the medio-lateral diameter of the incisive fossa. B. A three-dimensional reconstructed image of the nasopalatine canal. C. A sagittal section shows the measurements of the length of the nasopalatine canal and the antero-posterior diameter of the canal at the nasal fossa, mid-level, and hard palate. D. A coronal section shows two openings of Stenson's foramina.
Results
Foramina of Stenson (Number of openings at the nasal fossa)
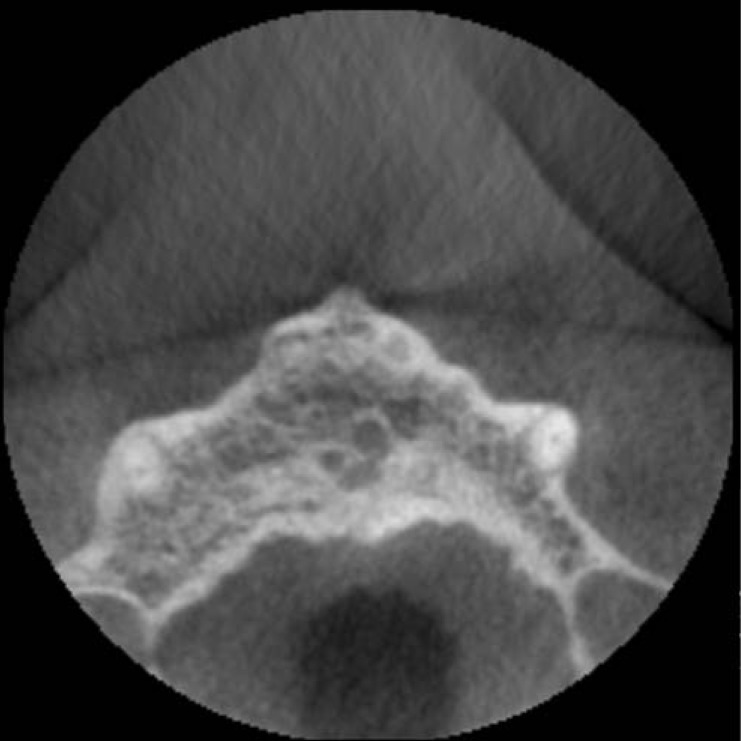
In the present study, it was observed that most subjects (81%) had 2 openings, or foramina of Stenson, at the nasal fossa (Fig. 2). Thirteen percent of the patients had 3 openings, while 4% had a single opening, and only 2% had 4 openings. The distribution of the number of openings at the nasal fossa by age and gender is shown in Figure 3. Pearson's correlation test for comparison of all of the parameters between the two genders is shown in Table 3. Pearson's correlation test for comparison of all of the parameters according to age distribution is shown in Table 4. The mean medio-lateral diameter at the foramen of Stenson was 1.75 (±0.77). The diameter ranged from 0.50 mm to 5.60 mm. The greatest diameter was observed in the canals with a single opening at the nasal fossa. Statistically significant differences among males and females and the different age groups with respect to the number of openings or average medio-lateral diameter of the foramen of Stenson were not observed in the present study.
Fig. 2.
A CBCT image shows 3 openings of the nasopalatine canal.
Fig. 3.
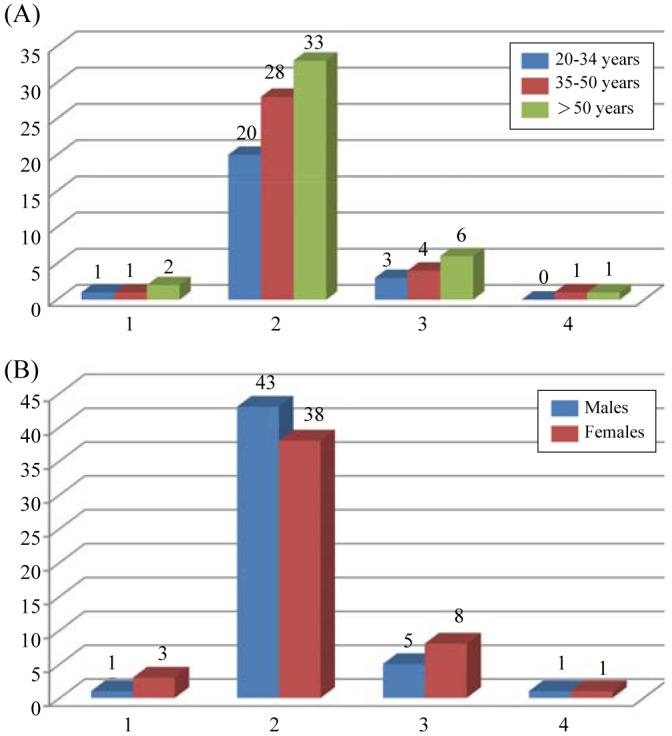
Bar diagrams show the distribution of the number of openings at the nasal fossa. A. An age-wise distribution of the number of openings at the nasal fossa. B. A gender-wise distribution of the number of openings at the nasal fossa.
Table 3.
Karl Pearson's correlation test for comparison of all parameters between males and females
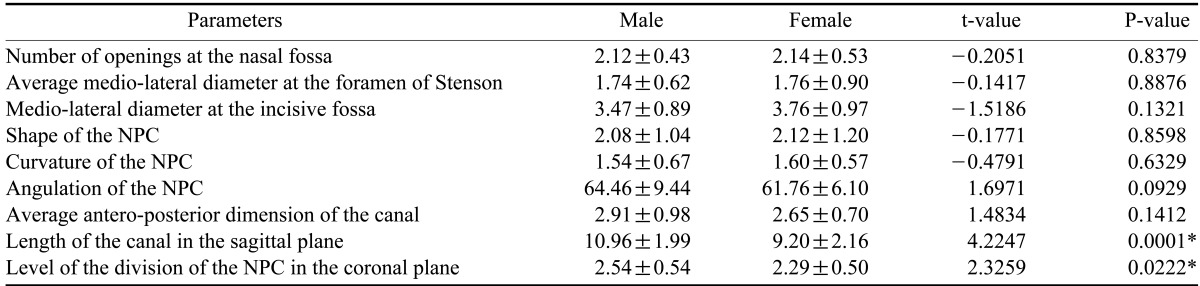
Table 4.
Pearson's correlation test for comparison of all parameters according to age distribution
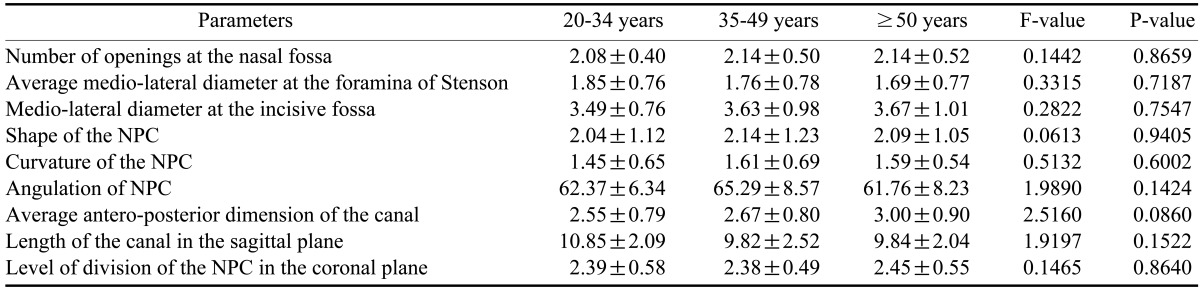
NPC: nasopalatine canal
Incisive foramen
The incisive foramen is located at the midline posterior to the root of the central incisors. The planes of the incisive foramen were generally oval-shaped and faced the postero-inferior side, though round and heart-shaped openings were also found in our study. The mean medio-lateral diameter of the incisive foramen, as seen on axial sections, was 3.62 (±0.94) and ranged from 1.40 mm to 5.90 mm. The mean diameter did not show statistically significant differences between males and females or among different age groups.
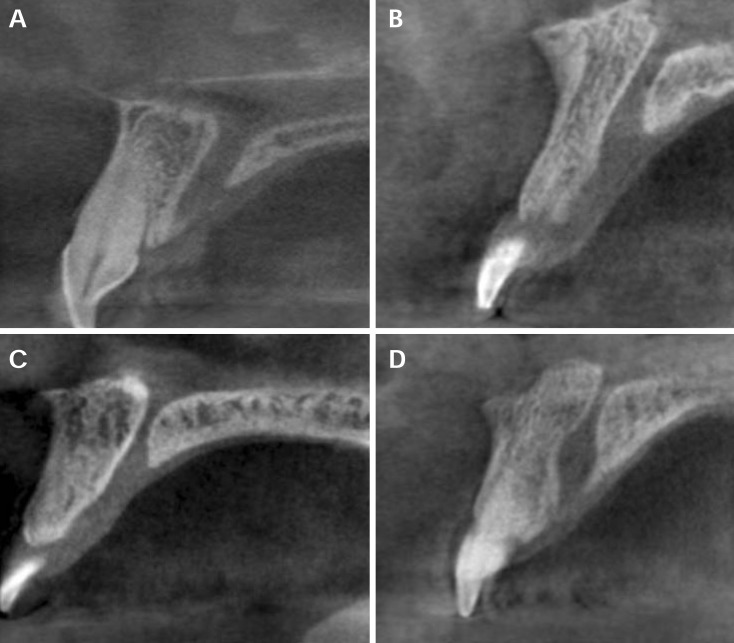
Classification of the NPC according to its shape, direction, and course
The shape, direction, and course of the NPC differed among cases in the sagittal view. The NPCs were thus classified into 4 categories according to their shape viewed on the sagittal sections: cylindrical, funnel, spindle, or hourglass (Fig. 4). The most commonly encountered shape was the cylindrical shape, which was seen in 38 subjects, and the least common was the spindle shape, seen in 11 subjects. The distribution of the subjects by age and gender according to the shape of the canal is shown in Figure 5. Statistically significant differences between the genders and between the different age groups with respect to the shape of the NPC were not observed.
Fig. 4.
CBCT images show the four shapes of the nasopalatine canal as seen on sagittal planes based on the labial and palatal walls of the nasopalatine canal. A. A cylindrical shape formed by parallel labial and palatal walls of the nasopalatine canal. B. A funnel shape formed by an increasing antero-posterior dimension of the nasopalatine canal from the nasal fossa to the hard palate. C. An hourglass shape in which the narrowest antero-posterior dimension of the NPC was at the mid-level compared to the dimensions at the nasal fossa and hard palate levels. D. A spindle shape in which the widest antero-posterior dimension of the nasopalatine canal was at the mid-level compared to the dimensions at the nasal fossa and hard palate levels.
Fig. 5.
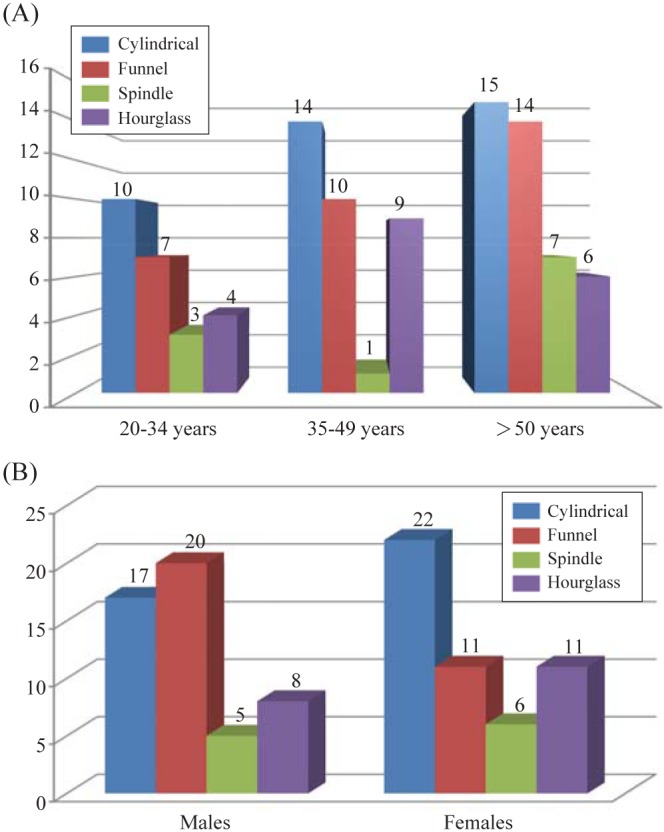
Bar diagrams show the distribution of the subjects according to the shape of the canal. A. An age-wise distribution of the subjects according to the shape of the canal. B. A gender-wise distribution of the subjects according to the shape of the canal.
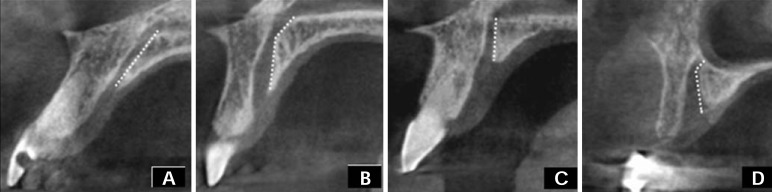
The NPCs were further classified according to their direction and course. The nasal floor was regarded as the "horizontal" plane. The 3D reconstructions were reoriented with reference to that plane. Based on the line perpendicular to the horizontal plane, the NPCs whose course changed by >10° from the vertical were regarded to be "slanted," and those whose course changed by <10° from vertical were regarded as "vertical" (Fig. 6). Whether the course of the NPC was straight or curved was also noted based on the curvature of the palatal wall of the canal. Therefore, four types of NPCs based on curvature were noted: vertical, vertical-curved, slanted, and slanted-curved (Fig. 7). Most commonly, the NPC was found to be slanted (51%), and only one subject was found to have a vertical-curved canal. Figure 8 shows the distribution of subjects by age and gender according to the curvature of the canal. Statistically significant differences between the genders and between the different age groups with respect to the shape of the NPC were not observed.
Fig. 6.
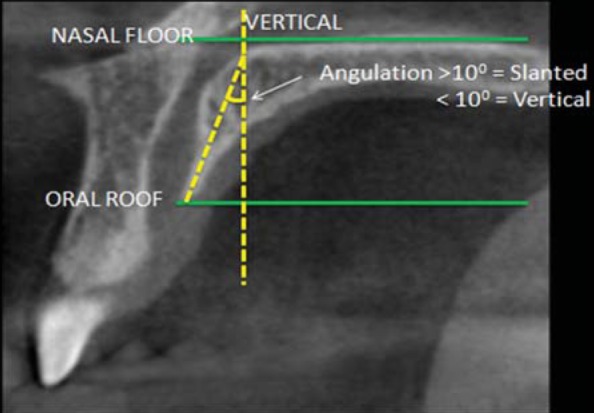
A CBCT image in the sagittal plane shows the method of measurement for vertical and slanted nasopalatine canals.
Fig. 7.
CBCT images show the curvature of the nasopalatine canal as viewed in the sagittal plane. A. A slanted nasopalatine canal. B. A slanted-curved nasopalatine canal. C. A vertical nasopalatine canal. D. A vertical-curved nasopalatine canal.
Fig. 8.
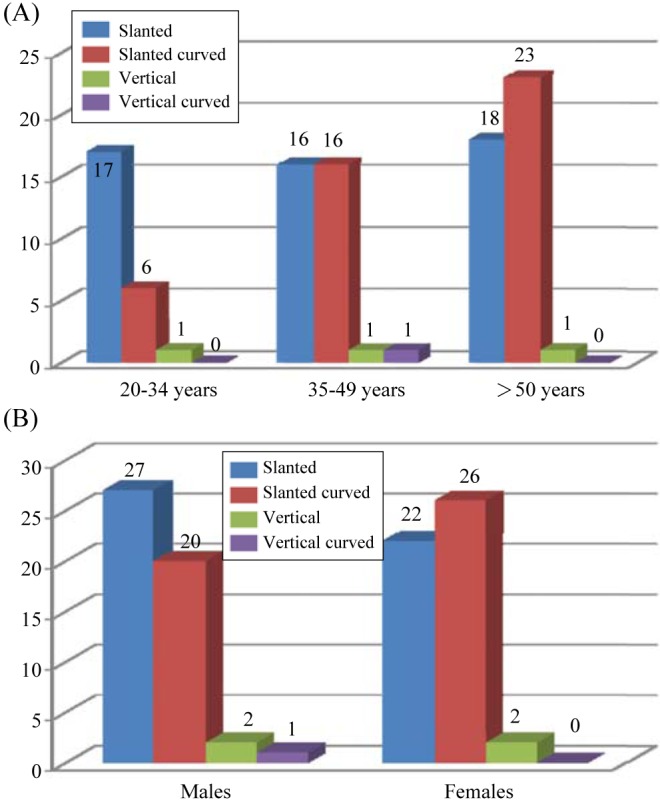
Bar diagrams show the distribution of the subjects according to the curvature of the canal. A. An age-wise distribution of the subjects according to the curvature of the canal. B. A gender-wise distribution of the subjects according to the curvature of the canal.
Angulation of the NPC
The slanting angle of the NPC was the angle measured between the floor of the nasal fossa and long axis of the NPC, which was considered to be the line joining the midpoint of the antero-posterior diameter at the nasal fossa level and the midpoint of the antero-posterior diameter at the level of the hard palate (Fig. 9).
Fig. 9.
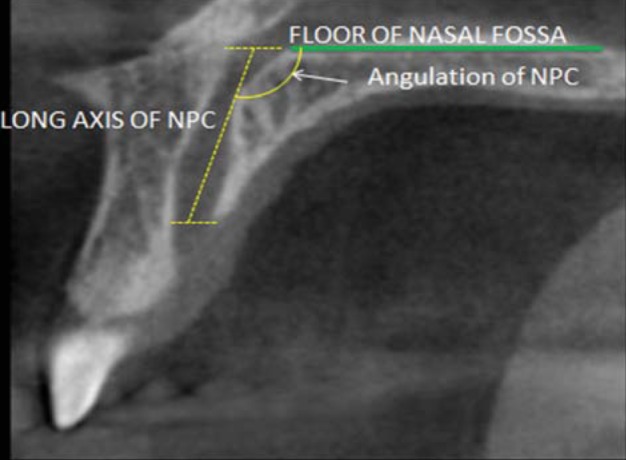
A CBCT image in the sagittal plane shows the method of measurement for the angulation of the nasopalatine canal.
Overall, the slanting angle of the NPC ranged from 46° to 99° in reference to the "horizontal" plane. The mean was 63° (±8.03). None of the subjects demonstrated negative values, which means that in all cases, the incisive foramen was located anterior to the nasopalatine foramina. Statistical analysis failed to show the correlation of the slanting angle of the NPC with age or gender.
Length of the NPC
As viewed on the sagittal plane, the length of the NPC was measured between the level of the nasal fossa and the level of the hard palate along the long axis of the canal (Fig. 1). It ranged from 4.60 mm to 15.70 mm, and the mean was 10.08mm(±2.25). Among different age groups, statistically significant differences in the length of the NPC were not observed. However, there was a statistically significant difference (p=0.0001) in the length of the canal between males (mean 10.96 mm) and females (mean 9.20 mm).
Antero-posterior diameter of the canal
The mean antero-posterior diameter of the NPC as viewed in sagittal plane was 2.78 (±0.85). The average antero-posterior diameter at the nasal fossa level was 2.86 mm, at mid-level was 2.32 mm, and at the palatal level was 3.15 mm. The differences in the values between males and females and among the different age groups were not found to be statistically significant.
Division of the NPC
The level of division of the canal in the coronal plane was assessed. Based on the coronal ratio, which was the ratio of the length of the canal superior to the division to the entire length of the canal in the coronal plane, the NPCs were divided into 3 categories: a coronal ratio of 1-0.65 (division of the canal at a level up to one-third from the inferior margin), a coronal ratio of 0.66-0.33 (division of the canal at a level in the middle-third from the inferior margin), coronal ratio <0.33 (division of the canal at a level in the farthest one-third from the inferior margin). Most commonly, the NPC division was in the middlethird level (51%), followed by the top one-third level (47%). Only on 2 occasions was the division found to be in the lowest third level. The level of the division of the NPC showed a statistically significant difference (p=0.0222) between males and females. However, the same could not be observed among different age groups.
Discussion
Several previous reports have dealt with the pathology of the nasopalatine canal region. The anatomical variations in the dimensions and morphology of this canal remain poorly documented. The present study indicated that the nasopalatine canal showed a great deal of variability with regard to its dimensions as well as to its morphological appearance.
The present study found up to four foramina at the level of the nasal floor. This was in accordance with the previous studies by Mraiwa et al9 and Liang et al2 who also reported observing up to four foramina at the level of the nasal floor. Sicher10 reported that there could be up to six separate foramina. The additional foramina have been labeled the foramina of Scarpa. However, Song et al11 and Jacob et al12 observed only two foramina in their respective studies and questioned the existence of the term "foramina of Scarpa" as real additional nasopalatine foramina at the level of the nasal floor. This variability in results could be due to sample differences and the various imaging techniques used in different studies. The average diameter of the foramen of Stenson in the present study was 1.75 mm, as compared to 2.2 mm reported by Mraiwa et al.9
The mean inner diameter of the incisive foramen in the present study was 3.61 (±0.94). These values were lower than those reported in the previous study by Mraiwa et al9 (4.6 mm) but comparable to those reported by Liang et al2 (3.4 mm). The diameter of the incisive foramen is usually considered to be below 6 mm; when it exceeds 10 mm, pathological conditions should be considered.9 In the present study, the diameter of the incisive fossa ranged from 1.40 mm to 5.90 mm, in accordance to previously accepted values.
Previous studies have reported that a cylindrically shaped NPC was most commonly observed.1,2 In accordance with this, in our study, the cylindrical shape was found in most of the subjects. In contrast to Song et al11 who reported the predominance of the vertical type of NPC in their study, in our study, slanted canals were more commonly observed than vertical ones. Liang et al2 have previously reported the mean angulation of the NPC from the horizontal as 77.4° (±8.9°). Our subjects showed a mean angulation of 63° (±8.03) from the horizontal.
Song et al11 have reported the length of the NPC to be 12.0 mm (8.4-15.8 mm) in dentulous maxillae, Mraiwa et al9 have reported a mean length of 8.1 (±3.4) mm, and Liang et al2 in their study assessed the length of the NPC as 9.9 (±2.6) mm. In the present study, the mean length of the NPC was found to be 10.08 mm (±2.25). It has been previously reported that the dividing point of the NPC in the coronal plane was at about the level of the upper fifth of the incisive canal.11 However, in our subjects, this was not the case. Most commonly, the NPC was divided within the middle-third level (51%), followed by division in the upper third level (47%).
In this study, statistically significant differences in the assessed parameters could not be observed among the different age groups. This could be attributed to the dentate population chosen for this study. It is likely that the increase in the size of the NPC, as observed in other studies,1,2 could be more likely due to the edentulous status of the patient rather than a purely age-related change, because in the other studies, the samples included some edentulous patients.
Among the males and females, the length of the canal and the level of the division in the coronal plane showed statistically significant differences. The greater length of the NPC in the males could be ascribed to the relatively larger cranio-caudal dimension of the face observed in the males as compared to the females and the differences in the size of the NPC could be relative to the facial dimensions rather than absolute. Similar findings have been previously reported by Liang et al.2
In conclusion, this study highlighted the anatomic variability of the NPC in relation to several parameters. The difference observed from the previously reported studies could be due to population variation or variability in the imaging techniques used to assess the NPC. Nevertheless, the anatomic variations in terms of dimensional and morphological parameters were significant, emphasizing the role of 3D imaging and assessment of this anatomical landmark in treatment planning of this area for implant placement or assessment of pathologies in this region or in preventing inadvertent complications while operating in the anterior maxillary region. The shape, curvature, and angulation of the canal and its antero-posterior dimensions are the most significant parameters for placement of implants in the maxillary incisor region. Additionally, the number of openings, medio-lateral dimensions, length of the canal, and level of its division may prove important when implants within the nasopalatine canal are being considered.
References
- 1.Mardinger O, Namani-Sadan N, Chaushu G, Schwartz-Arad D. Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae. J Periodontol. 2008;79:1659–1662. doi: 10.1902/jop.2008.080043. [DOI] [PubMed] [Google Scholar]
- 2.Liang X, Jacobs R, Martens W, Hu Y, Adriaensens P, Quirynen M, et al. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol. 2009;36:598–603. doi: 10.1111/j.1600-051X.2009.01429.x. [DOI] [PubMed] [Google Scholar]
- 3.Kraut RA, Boyden DK. Location of incisive canal in relation to central incisor implants. Implant Dent. 1998;7:221–225. doi: 10.1097/00008505-199807030-00010. [DOI] [PubMed] [Google Scholar]
- 4.Cavalcanti MG, Yang J, Ruprecht A, Vannier MW. Accurate linear measurements in the anterior maxilla using orthoradially reformatted spiral computed tomography. Dentomaxillofac Radiol. 1999;28:137–140. doi: 10.1038/sj/dmfr/4600426. [DOI] [PubMed] [Google Scholar]
- 5.Artzi Z, Nemcovsky CE, Bitlitum I, Segal P. Displacement of the incisive foramen in conjunction with implant placement in the anterior maxilla without jeopardizing vitality of nasopalatine nerve and vessels: a novel surgical approach. Clin Oral Implants Res. 2000;11:505–510. doi: 10.1034/j.1600-0501.2000.011005505.x. [DOI] [PubMed] [Google Scholar]
- 6.Raghoebar GM, den Hartog L, Vissink A. Augmentation in proximity to the incisive foramen to allow placement of endosseous implants: a case series. J Oral Maxillofac Surg. 2010;68:2267–2271. doi: 10.1016/j.joms.2010.02.047. [DOI] [PubMed] [Google Scholar]
- 7.Shear M, Speight P. Cysts of the oral and maxillofacial regions. 4th ed. Oxford: Blackwell; 2007. pp. 108–118. [Google Scholar]
- 8.Bodin I, Isacsson G, Julin P. Cysts of the nasopalatine duct. Int J Oral Maxillofac Surg. 1986;15:696–706. doi: 10.1016/s0300-9785(86)80110-7. [DOI] [PubMed] [Google Scholar]
- 9.Mraiwa N, Jacobs R, Van Cleynenbreugel J, Sanderink G, Schutyser F, Suetens P, et al. The nasopalatine canal revisited using 2D and 3D CT imaging. Dentomaxillofac Radiol. 2004;33:396–402. doi: 10.1259/dmfr/53801969. [DOI] [PubMed] [Google Scholar]
- 10.Sicher H. Anatomy and oral pathology. Oral Surg Oral Med Oral Pathol. 1962;15:1264–1269. doi: 10.1016/0030-4220(62)90163-9. [DOI] [PubMed] [Google Scholar]
- 11.Song WC, Jo DI, Lee JY, Kim JN, Hur MS, Hu KS, et al. Microanatomy of the incisive canal using three-dimensional reconstruction of microCT images: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:583–590. doi: 10.1016/j.tripleo.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 12.Jacob S, Zelano B, Gungor A, Abbott D, Naclerio R, McClintock MK. Location and gross morphology of the nasopalatine duct in human adults. Arch Otolaryngol Head Neck Surg. 2000;126:741–748. doi: 10.1001/archotol.126.6.741. [DOI] [PubMed] [Google Scholar]