Abstract
Despite government efforts to increase health care insurance and access in China, many individuals, regardless of insurance status, continue to engage in high levels of self-medication. To understand the factors influencing common self-medication behaviour in a community of food market venders in Fuzhou China, a total of 30 market venders were randomly recruited from six food markets in 2007. In-depth interviews were conducted with each participant at their market stalls by trained interviewers using a semi-structured open-ended interview protocol. Participants were asked broad questions about their health-seeking behaviours as well as their past experiences with self-medication and hospital care. ATLAS.ti was used to manage and analyze the interview data. The results showed that hospital-based health care services were perceived as better quality. However, self-medication was viewed as more affordable in terms of money and time. Other factors prompting self-medication included confidence in understanding the health problem, the easy accessibility of local pharmacies, and the influences of friends/peers and advertising. Three broad domains, attitude, cost, and effectiveness, were all seen to determine past decisions and experiences with self-medication. Interestingly, the effective management of self-medication via pharmacy resources raised particular concern because of perceived variation in quality. In conclusion, self-medication was found to be an important and common health-seeking behaviour driven by multiple factors. A sound and comprehensive public health system should systematically attend to these behaviours and the pharmacies where much of the behaviour occurs.
Keywords: Self-Medication, Qualitative Research, Health-Seeking Behaviour, Community Pharmacies
Introduction
Self-medication is defined as the selection and use of medicines by individuals to treat self-identified illnesses or symptoms (Anonymous 1998). Although self-medication has been reported to have several benefits (Hughes et al. 2001), it has also been associated with many risks, including the lack of appropriate instruction from physicians, increased risk of adverse drug events and drug resistance, and, most distressing, accidental death (Anonymous 2009a, Ouedraogo et al. 2008, Awad and Eltayeb 2007, Al-Azzam et al. 2007, Berzanskyte et al. 2006, Sihavong et al. 2006).
As China’s economy has grown rapidly over the past 30 years, the country’s health care system also experienced an enormous transition from a national centrally-controlled system to more market based (Ho and Gostin 2009, Yip and Hsiao 2008, Ma et al. 2008, Dong and Phillips 2008). Although great improvements have been made in the areas of infant mortality, infectious disease control, and life expectancy (Dong and Phillips 2008, Liu et al. 2008), the nature of its fee-for-service has placed a large financial burden on Chinese people, particularly those without health insurance (Peng et al. 2010, Ma et al. 2008, Liu et al. 2008, Yip and Hsiao 2008, Blumenthal and Hsiao 2005, Lindelow M 2005). One recent study found that 94% of migrant workers in Beijing, China’s capital city, didn’t have any insurance coverage (Peng et al. 2010). Consequently, to avoid the high cost of health care, many Chinese people, especially the uninsured, choose self-medication as their first option when they encounter a need for health care—even for serious infectious diseases like STDs (Peng et al. 2010, Mou et al. 2009, Zhao et al. 2008, Wong et al. 2006, Lieber et al. 2006, Ma et al. 2005, Detels et al. 2003, Wong and Yilin 2003).
In 2009, in order to increase access to and the equality of health care, China unveiled its health care reform plan which included increasing insurance coverage as one of the highest priorities (Anonymous 2009b, Yip et al. 2009). However, recent studies report that even with higher rates of insurance coverage, outpatient medical service utilization rates remain far below desirable levels (Yu et al. 2010, Mou et al. 2009). Further, there were no significant differences found between insured and uninsured groups in terms of hospital-based care utilization rates (Yu et al. 2010). Other research has suggested that, age, education, geographic region, disease severity, and self-medication experiences may play an important role in determining these health seeking behaviours (Yinhuan et al. 2008, Yinhuan and Hao 2008, Dong 2003, Bi et al. 2000). However, the majority of this work has involved the use of quantitative research methods which limit the possible range of findings in understanding these behaviours. Through the use of qualitative methods, this study aimed to identify and explore a broader range of the factors influencing self-medication behaviour and provide a more comprehensive picture of the behaviours and circumstances in which they occur.
Method
Study site and participants
This study was conducted between July and December, 2007 in Fuzhou city, Fujian Province. The capital city of the province, Fuzhou is located on China’s south-east coast and has a population of 6.8 million—which accounts for about 19% of the total province population. Being one of the major cities in the coast area, Fuzhou is best known for its travel industry and has a large rural to urban migrant population.
The data for this study come from the National Institute of Mental Health (NIMH) Collaborative HIV/STD Prevention Trial conducted in five countries with populations at risk for HIV and STDs: China, India, Peru, Russia and Zimbabwe (National Institue of Mental Health Collaborative HIV/STD Prevention Trial 2007a). In China, market venders were selected as the target population for the main trial due to several characteristics seen as favourable for the randomized controlled trial. These characteristics included available base rate information on STDs, relative population stability over time, a sufficient number of venues, stable social groups, and sufficient distance between the venues (National Institue of Mental Health Collaborative HIV/STD Prevention Trial 2007b). A two-stage sampling strategy was used to select potential participants for this sub-study. Firstly, six food markets were randomly selected by using a simple random sampling method from among the 40 food markets participating in the main trial (Detels et al. 2003). Prior to the second sampling stage, flyers recruiting participants for a ‘Community Health Study’ were posted in the selected food markets to inform potential market vender participants about the study. Study staff then randomly approached potential participants at each market to screen for eligibility and recruit eligible candidates until they reached the designated sample size for each market.
Eligibility criteria included: a) age—18 years or older; b) self-report of having visited a pharmacy at least once in the past 3 months; c) absence of any condition or disability that would make it difficult to communicate—ex. deafness or serious psychological problem; and d) willingness and ability to provide informed consent. After full explanation and disclosure of this study, eligible participants were asked to complete all required informed consent procedures. Ultimately, the sample size was determined by budget, time, and staffing constraints. A total of 30 market venders, five from each selected market, were finally recruited in this study. Participants were compensated 20 RMB (approximately US$2.50) in cash for their participation. The study was approved by the internal review boards for the protection of human subjects (IRBs) at the University of California, Los Angeles and Chinese Center for Disease Control and Prevention.
Data collection
The in-depth interviews were conducted with each participant by trained interviewers based on a semi-structured open-ended interview protocol. Each interview lasted between one to two hours and, for convenience, was conducted at the participant’s market stall. Interviews were usually conducted during the lunchtime hours when the subjects were less busy with customers. Interviewers were trained and instructed to seek quality and depth in the information they would be collecting. As such, while the full protocol was systematically covered in each interview, the format was intentionally flexible to allow more time for depth of discussion and the expansion into new areas of content as they were revealed during the interview. Participants provided demographic information and were asked, in broad terms, about their health-seeking behaviours when experiencing health problems and their attitude towards self-medication. All interviews were audio recorded for the purpose of data analysis and quality control. After interviews were completed, the recordings were transcribed by field research staff. Each interview was transcribed by one transcriber and was double checked by a second transcriber. The procedures of cross-checking and confirmations of the transcription were conducted to assure quality of work was maintained. All qualitative data were recorded and transcribed in Chinese.
Analysis
ATLAS.ti (Muhr 1997), a qualitative data analysis software package, was used to manage and analyze the interview data. Two coders were involved in excerpting, coding, and analyzing the qualitative data. The code system that was ultimately applied was developed in an iterative manner. Initially, the code system was outlined based on a conceptual framework consisting of factors known, or believed, to influence self-medication and a few concepts emerging from a preliminary reading of interview transcripts. At the outset, each of the team members coded three interview transcripts independently for the purpose of evaluating the comprehensiveness and usefulness of the system and for guiding a revision of these system and concept framework. The coding system and concept framework were revised as a need for new topics, dimensions, or relationships among key factors emerged from the interview transcripts. This iterative process continued until the code system stabilized and no new data were encountered that suggested a need for further revisions. To establish acceptable levels of inter-coder reliability among the research team members, each coder independently coded a set of transcripts and then compared the results for relative consistency. Where coding discrepancies were found, further discussions were held and the definitions and application criteria for each code were fine-turned until each code could be independently applied with acceptable consistency.
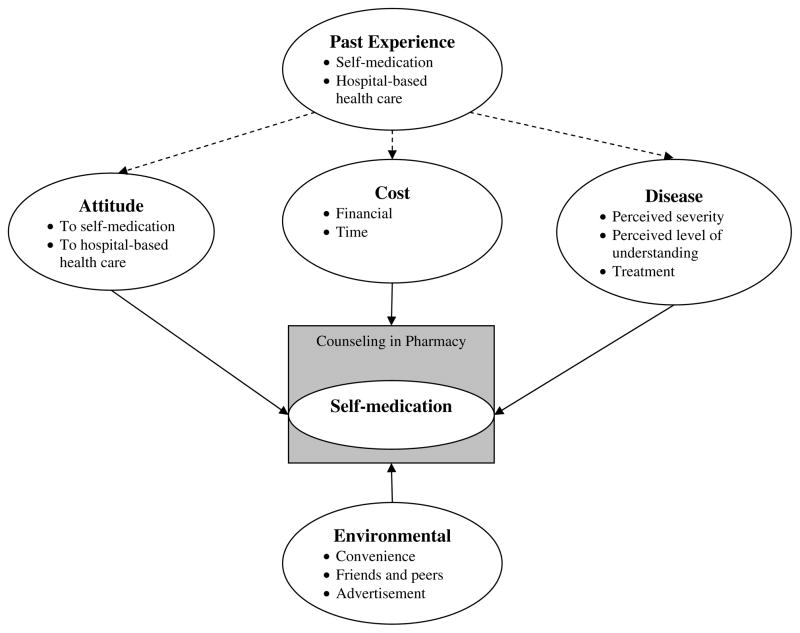
Following a series of revisions, the conceptual framework for understanding the factors influencing self-medication behaviour (see Figure 1) and the code system for use in this study (see Table 1) were finalized. As shown in Figure 1, variation in self-medication was considered from five domains of possible influence: attitude, cost, disease, environmental, and past experience. Moreover, pharmacy-based self-medication counselling was also included as an intervening factor in understanding self-medication decisions and management. Accordingly, six code families were identified under the framework including a total of 14 codes (see Table 1). Each aspect of the model was used to organize and communicate the themes and content extracted from the interview data. All coding and analysis were completed in Chinese with the results being summarized and translated into English for presentation here.
Figure 1.
Conceptual model of factors influencing self-medication
Table 1.
Code System Structure
| Code Family | Code | Definition |
|---|---|---|
| Attitude | Attitude towards self-medication | Respondents’ subjective attitudes towards self-medication in terms of the service quality and effectiveness. |
| Attitude towards hospital based health care | Respondents’ subjective attitudes towards hospital based healthcare in terms of the service quality and effectiveness. | |
| Cost | Financial | Financial burden associated with hospital-based health care or financial advantages associated with self-medication. |
| Time | Concerns about health care time consumption. | |
| Disease | Perceived severity | Respondents’ perceived severity/controllability of the disease or condition. |
| Perceived understanding | Respondents’ perceived level of understanding the disease or condition—the extent to which the individual believes their understanding of the disease or condition is accurate. | |
| Treatment | Whether respondents know how to treat the disease or condition. | |
| Environmental | Convenience | Pharmacy’s convenience advantage in terms of accessibility. |
| Advertisement | Self-medication was prompted by advertisement. | |
| Friends & Peers | Influences of friends and peers. | |
| Past experience | Past experience - attitude | Attitude about previous hospital visits in terms of the service quality. |
| Past experience - cost | Feelings about previous hospital visits in terms of cost—both in terms of time and money. | |
| Past experience – disease | Knowledge gained from previous hospital visits related to treatment information. | |
| Counseling | Counseling | Self-medication counseling from a pharmacy. |
Results
Demographic information
A total of 30 subjects were interviewed. The full sample age range spanned from 28 to 57 years with half being between 30 and 39 years of age. All participants reported being married, slightly more than half were female (57%), and regarding education level attained, 10% reported less than middle school, 67% middle school, and 23% high school (see Table 2).
Table 2.
Age, gender, education and marital status of study participants (n=30)
| Number | Percentage | |
|---|---|---|
| Age | ||
| 20~29 | 1 | 3% |
| 30~39 | 15 | 50% |
| 40~49 | 9 | 30% |
| 50~59 | 5 | 17% |
| Gender | ||
| Male | 13 | 43% |
| Female | 17 | 57% |
| Education | ||
| Illiterate | 1 | 3% |
| Primary School | 2 | 7% |
| Middle School | 20 | 67% |
| High School | 7 | 23% |
| Marital Status | ||
| Married | 30 | 100% |
Theme One: Hospital-based health care was perceived as having better service quality
Attitude was the only domain about which participants reported a unanimous belief that hospital-based health care was most preferred because of better quality services. The most frequently mentioned advantages of hospital included more qualified and better-trained doctors, better medical equipment and diagnosis, and higher quality medications. On the other hand, attitude concerns regarding self-medication included treatment delay, inappropriate diagnosis, and improper or inadequate treatment. Given these reported beliefs, it is clear that hospitals are more trusted by the study population. The follow quotes illustrate respondents’ attitudes toward self-medication and hospital-based health care as related to the quality of service.
Attitude towards self-medication
There were many pharmacies in the community. Some of them sold fake drugs and they had no effects at all. (Male, 50 years old)
There were too many medicines in the market and you don’t know them. If you bought it by yourself, you might have misdiagnosed your need. (Male, 36 years old)
It was not good to buy medicines from a pharmacy. First, you might get fake ones. Second, there was no instruction from a doctor. The selling staff was just some young girls and you might not use the medicine appropriately. (Female, 39 years old)
Attitude towards hospital based care
It (hospital) was different from the pharmacies. It has very comprehensive, skillful and professional doctors. It was better than a pharmacy for sure. What’s more, it also had good equipments. (Male, 40 years old)
I felt safe while visiting a hospital. You should go to a big hospital for health checkup. All the services were secured. (Female, 28 years old)
I would feel safe while seeking health care in hospital. About the medicine, they would not sell fake or expired drugs to us. (Male, 40 years old)
Theme Two: Self-medication was perceived as a way to save money and time
As market venders, respondents had to spend most of their time at their businesses in order to support their families and, accordingly, earning money was reported as an important part of their daily life. As a result, losing time was thought of as losing business. Not surprisingly, saving money and time is seen as a high priority when seeking health care. This priority becomes even stronger when you consider the general lack of insurance in the sample population. As a result, concerns about the cost of health care, both money and time, leads individuals to avoid hospitals whenever possible.
Our businesses are very small. It is quite common to cost several hundred Yuan for just one visit to a hospital. Even for a simple cold, it will cost you one or two hundred. What do you think a vender like me can earn everyday? We have to support the whole family, it is not easy. We have to save wherever we can. (Female, 37 years old)
It costs time to wait to see a doctor in line. It takes half a day to visit a hospital. We don’t have such time leaving our business unattended. (Female, 45 years old)
Reasons? Our biggest concern is we are not covered by insurance. No one shares our costs. A minor problem would cost hundreds of Yuan. By what means could I make a claim? How much you think I earn every month? If we are recruited by a company and have insurance, I would take every minor problem as a big one. (Male, 51 years old)
Accordingly, as compared with hospital-based health care, self-medication was reported to help save time and money and so its use is fully aligned with the study population’s more immediate concerns.
The first advantage of pharmacy is it being cheaper and the second is time savings. Spending a little time can solve some small problems. (Male, 40 years old)
If I get a cold today, I would get cured with several Yuan in pharmacy. But it could cost me a half day--much too long—and one to two hundred Yuan in hospital for the same problem. (Male, 50 years old)
You will save 20 to 30 Yuan for the same medicine of the same brand in pharmacy. (Female, 37 years old)
Theme Three: Role of perceived understanding of the disease
When facing a health problem, it was quite common for the respondents to perform a symptom based self-evaluation of the disease or condition. This evaluation includes severity, cause, and possible treatment options before deciding where to seek health care. The results of the self-evaluation were found to play a key role in health-seeking behaviour. For those diseases believed to be relatively minor, well understood, or of common treatment options, self-medication would be more preferred. On the other hand, if the disease was thought severe, unfamiliar, not responsive to self-medication, or confusing as to how to treat, study respondents would much more likely select hospitals as the first option for seeking health care.
Well understood diseases
Any minor problem, say cold, sore throat or excess internal heat [an expression used in Chinese medication], for which I have confidence to deal with by getting some medicines by myself. (Female, 37 years old)
It depends on the specific situation. Why bother visiting a hospital for a minor problem like abdomen pain or diarrhea? Self-purchased medicines would work for such minor problems. (Female, 42 years old)
For those situations I could figure out what illness I am suffering from and what medicines would help, I would go to buy the medicines by myself. (Male, 38 years old)
Poorly understood diseases
(Chuckle): I definitely won’t go to a hospital unless I have serious illness. (Female, 47 years old)
For those situations that could not be managed by my own efforts or that I could not understand, I would then visit a doctor. (Male, 38 years old)
For those I’ve never experienced or that I don’t understand, I would go to a hospital directly. Regardless how serious my problem is, for those I don’t understand, I would ask for help from a doctor. (Male, 40 years old)
Theme Four: Role of environmental factors
Three environmental factors that promoted the use of self-medication were identified in this study: convenience, friend/peer influence, and advertisement. Related to issues of time savings, convenience was one of the most frequently mentioned self-medication advantages because of the convenient access to local pharmacies versus that of hospital-based health care. Visiting a hospital was thought of as troublesome in terms of longer distances and more complication in receiving care. Further, as self-medication was reported as a common health-seeking behaviour in respondent communities, the influences of friends and/or peers was also noted as playing an important role in encouraging the behaviour. Finally, commercial advertisements were also found to positively promote self-medication behaviour.
Convenience
It is convenient. No registration, no line and no card [a computer system for information management] required. (Male, 33 years old)
The pharmacy is very close. You can get there in a minute. If you go to hospital, you would have to walk for a while. (Female, 31 years old)
It is really troublesome if you want to go to a hospital. It is quite far from here and you would have to wait in line. You also need to have a card. It is too troublesome. (Female, 34 years old)
Friend/peer influence
People like us in the market would always buy medicine by ourselves when we have some small problems. If I get a cold, my friend would suggest to me which medicine I should buy from which pharmacy and I would just follow his suggestions. (Male, 57 years old)
The reason [for buying a medicine] is that I have heard about this medicine from my friend. He said, ‘this medicine was good for colds at an early stage.’ I tried it and it worked pretty well. That’s it. (Female, 42 years old)
All my friends in the community would buy medicines from local pharmacies when they get colds. (Female 46 years old)
Commercial Advertisement
I don’t really understand [the medicine I am going to buy]. As an example, I purchased the throat medicine last time because of its advertisement. (Female, 45 years old)
I would generally follow TV commercials. I would not go for those medicines I’ve never heard of. (Male, 31 years old)
Yes, I would always buy those brands that I have seen them in the commercial advertisement. I don’t like those less known and inferior brands. (Female, 45 years old)
Theme Five: Role of past experience
The effects of past experiences on self-medication behaviour were mediated by and acted on mainly as a function of issues related to attitude, cost, and disease. Respondents reported both positive and negative reactions to previous health care seeking experiences. These real life experiences provided direct and detailed evidence about their health care options and, as such, played an important role in their future health care seeking behaviour. Consistent with the above analysis, respondents’ experiences with hospital-based health care were largely satisfying with regard to the quality of service and longer-term prognosis of their health problems. However, the relatively high cost, complication, and time demands associated with accessing hospital-based health care remained a deterrent to seeking health care at hospitals. Accordingly, participants reported trying to combine the advantages of both hospital-based and self-medication health care. Essentially, individuals worked to develop an informed self-guided self-medication approach which was based on their earlier treatment experiences. That is, the first time they experienced a health problem, they sought care at a hospital. In the future, to the extent that they believed they were experiencing similar problems, they would choose to treat by self-medication.
Positive experiences
The experience was really good. You got the right diagnosis and treatment, so the prognosis was good. (Male, 50 years old)
My problem was cured in the hospital. You will get a comprehensive exam and treatment in hospitals. Right now, I don’t have any pain at all. (Male, 33 years old)
The hospital’s service quality was quite good. You should get treatment early if you had a problem for sure. If it was delayed and the tumour getting bigger, you would be finished. (Female, 37 years old)
Negative experiences
The experience was not good. It took me too much time. Waiting in the line took me a long time. The price of medicines was also much higher in hospitals. (Male, 40 years old)
It was very crowded. You had to get up very early for registration. Then I came out to take care of my business and came back again one or two hours later. That hospital was very crowded. Every morning, there was a long line there. Many people were waiting there. (Female, 37 years old)
You always need to stay in lines in hospitals—too troublesome. It would take you at least half day. There was a line for casher, a line for pharmacy. Lines were everywhere. It was impossible if you went there by yourself. I always go with my husband. I would never go there by myself (smile). I felt very bad! (Female, 45 years old)
Self-guided self-medication
I would visit a doctor when I have an illness for the first time. Among the prescribed medicines I would choose the most effective ones for similar illness in the future. I would visit a pharmacy of good reputation, certainly. (Male, 38 years old)
I would definitely visit a doctor the first time I got sick due an illness. (Interviewer: Could you give me a reason?) If the medicine prescribed by the doctor works for the first time, I would make purchases by myself the next time I got sick for the same reason. (Male, 51 years old)
I would visit a hospital when I had a problem for the first time, otherwise, you would not know which medicine worked for you. But I would not always do that. With the prescription, I could buy the same medicine from pharmacy next time. (Female, 37 years old)
Theme Six: Self-medication counselling in pharmacy
Although some respondents expressed a willingness to receive self-medication counselling from pharmacy workers before purchasing a medicine, they also expressed some concerns about the quality of the counselling. Most respondents expressed their worries about the purpose of counselling services in pharmacies. Profit motives are thought of as the primary goal of such counselling services, therefore, respondents believe that guidance on which drug to recommend was based more on profit than on patients’ needs. Accordingly, individuals believe that the drugs being recommended in the pharmacies were not the best ones, but the most expensive or fake ones.
Most of the time, I would not consult them, because their recommendations were usually very expensive. (Male, 33 years old)
I would worry about the quality of the drugs they recommended. The drugs might be fake ones and pharmacy worker wanted to cheat you. (Male, 38 years old)
Well, I think the more strongly they recommended the worse the drug would be. Last time I got back pain and I bought two pieces of plaster they recommended, but it didn’t work at all. I would trust myself next time. (Female, 45 years old)
I think their recommendations were not good (interviewer: why, because it was expensive?) Not this. They all looked like the salesmen of the drug company. What they recommended were usually their products. (Female, 28 years old)
Discussion
Self-medication remains a common health care seeking behaviour in many developing Countries (Fuentes Albarran and Villa Zapata 2008, Yousef et al. 2008, Berzanskyte et al. 2006, Awad et al. 2006). While several studies employing quantitative methods had identified important factors associated with self-medication (e.g., age, income, education, and gender) (Al-Azzam et al. 2007, Awad and Eltayeb 2007, Awad et al. 2006, Awad et al. 2005), this study’s qualitative approach provided for a broader perspective on these behaviours. Findings here were consistent with other works that had identified minimal ailment or disease severity as a common factor contributing to decisions about self-medication (Suleman et al. 2009, Afolabi 2008, Fuentes Albarran and Villa Zapata 2008, Wazaify et al. 2008, Yousef et al. 2008). Beyond severity, respondents’ beliefs about how well they understood the health problem and its treatment were also identified in this study as issues related to self-medication decisions. However, both the perceived severity and beliefs about level of understanding of a health problem were based on the symptoms being experienced. Common symptoms, such as colds, sore throat, and abdominal pain were usually thought to be associated with minor problems. Although the accuracy of common symptom-based self-evaluation was not assessed in this study, given its influential role on health-seeking behaviour, it would be appropriate to assume that self-medication behaviour may be problematic if the accuracy of this symptom based self-diagnosis is poor.
Also, based on data from the larger trial that this study has drawn from, Yin and colleagues reported that the overall accuracy of physician’s symptom-based assessment was only 10% in diagnosing the five most common STIs among over 4000 market venders (Yin et al. 2008). Such a low accuracy rate shown by even those well trained physicians raises serious concerns about the potential dangers of study participants continuing symptom-based self-diagnosis and self-medication. Moreover, given the complexity of many diseases and that many different diseases share common and relatively mild early-stage symptoms, inappropriate symptom-based self-medication can potentially threaten public health when considering highly infectious diseases, such as H1N1 influenza, tuberculosis, and STDs/HIV. Many infectious diseases start with flu-like symptoms, increases the likelihood of misdiagnosis and, subsequently, inappropriate self-medication. This pattern of response can lead to the possible spreading of an epidemic which could threaten the broader community and society. Moreover, studies have shown that inappropriate self-treatment can lead to adverse drug events, drug resistance, potential drug interaction, and even accidental death (Anonymous 2009a, Ajuoga et al. 2008, Ouedraogo et al. 2008, Indermitte et al. 2007). Taken together, inappropriate self-diagnosis and medication may raise serious concerns related to the health of individuals and the broader community.
Consistent with previous studies, lower cost was one of the key reasons for self-medication behaviour. Cost was understood by study participants to include both the direct monetary expense of hospital medical services and medication as well as many indirect costs (e.g., time and the loss of business opportunity). The issue of cost has an important historical context. Prior to the early 1980s, the Chinese health care system was almost completely based on centrally planned economies where health care was a part of comprehensive social welfare system provided by the state (Bloom and Xingyuan 1997, Hsiao 1995). The people of China had nearly universal access to primary and hospital care as well as pharmaceuticals at little or no cost (Yip and Hsiao 2001). As a result of economic reforms in late 1970s, the institutional and economic foundations of China’s health system weakened (Ramesh and Wu 2009). This weakening included a decrease in government oversight (Wang 2004) and an increase in hospital-based medical care. Providers prescribed expensive, and often unnecessary, drugs, diagnostics, and procedures for profit purpose (Liu and Hsiao 1995). These increasing costs placed a significant burden on the Chinese population, particularly those in lower income levels and rapidly rising health care spending became a grave public concern throughout China (Ramesh and Wu 2009). Clearly a reform of the health system with the aim of increasing direct government funding and expanding insurance coverage is necessary and, fortunately, the planning of such reform is in development (Anonymous 2009b). From 2009 to 2011, the central government and all lower levels of government aim to invest 850 billion RMB (approximately 127 billion US dollars) in the health system with the intention of reforming and expanding basic universal health insurance to cover 90% of the population by 2011 (Anonymous 2009c).
As far as environmental factors, the relative convenience of access to local pharmacies was a major force that encouraged self-medication behaviour in the study population. While it is clearly impractical in terms of logistics and cost to widely increase the numbers of hospitals to provide easier access to quality health care, the potential value of pharmacies in a tiered health care system should not be overlooked. Well monitored and proper managed self-medication could be of great benefit in terms of efficiency and effectiveness (Hughes 2003). One key to achieving this goal would be to strengthen or modify the role of the pharmacy. In one of our previous studies, we have argued that in the area of STD/HIV prevention and control, pharmacies should play a more active role in providing consultation and referral services rather than a specific emphasis on selling medication (Wen et al. 2009). This argument would remain valid even under the broader circumstances considered here. The roles of pharmacies to public health have been recognized in most developed counties and recently by many developing countries (Thanh et al. 2010, Kamat and Nyato 2010, Anderson 2007). As an indispensable component of health care system, pharmacies should not consider commercial profits as their only interest. Besides that, they should be required to take more responsibility for self-medication management and monitoring and referral services (Naves Jde et al. 2010). However, such a system is yet to develop. Pharmacy’s roles in public health were still overlooked in the currently system. Most current existing regulations for pharmacies focused on the management procedures for pharmaceuticals, including the procedures of purchase, storage, and sales, rather than a broader view of the role pharmacies could play in the public health care system. To promote this development, formal policies and regulations, including staff training, referral systems between pharmacies and hospitals, and regular monitoring would be required. Should such efforts be made, the role of pharmacies could evolve from that of simple commercial businesses to an increasingly important aspect of the public health system.
As a relatively small scale study, the main limitation is likely the limited transferability of findings. The source population, total number of participant in this study and the random selection of participants might have resulted in less variability in the sample population. For example, the sample did not include any unmarried venders which restricted a possible exploration of how marital status may have influenced behaviour. In the future, a purposive, stratified, or quota sampling method would be helpful to ensure representation from all important sub-groups. In addition, all participants came from one city in Fujian, a population with relative low socio-economic levels, and, as such the views of people from other socio-economic groups may not have been captured in the data. Finally, since interviews were conducted at the venders’ stalls, interviews might be interrupted or disturbed by some distraction presenting in the area. Nevertheless, while concerns about transferring the findings here are valid, it is important to point out that this sample is similar to a significant demographic throughout China and a great deal can be learned from this work about the more common beliefs and practices of individuals living in similar circumstances.
In conclusion, decisions about self-medication behaviour are determined by multiple factors. Many of the advantages associated with self-medication will likely ensure that this will remain an important and common health seeking behaviour. However, the potential dangers to individual and public health are clear if self-medication behaviour continues without the appropriate guidance and management from qualified professionals. Accordingly, a sound and comprehensive health care system should accept the notion that individuals will engage in self-diagnosis and treatment and give special attention to the management and guidance of this behaviour and the role of pharmacies where much of this behaviour occurs.
What is known about this topic
Self-medication has been reported to have both benefits and risks.
Many Chinese people choose self-medication as their first option when they encounter a health problem to avoid the high cost of healthcare.
Even with higher insurance coverage, hospital-based medical service utilization rates in China remain far below desirable levels.
What this paper adds
Self-medication is a behaviour affected by factors from the domains of attitude, cost, disease, environment and past experience.
The only reported advantage associated with hospital-based care is its better service quality.
Health care system should give special attention to the management of self-medication and community pharmacies where much of this behaviour occurs.
Acknowledgments
This study was funded by National Institute of Mental Health grant number U10MH61513, a five-country Cooperative Agreement being conducted in China, India, Peru, Russia, and Zimbabwe. We thank team members in Fuzhou, China for their support and contributions to this study.
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- AFOLABI AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7:120–7. doi: 10.4103/1596-3519.55666. [DOI] [PubMed] [Google Scholar]
- AJUOGA E, SANSGIRY SS, NGO C, YEH RF. Use/misuse of over-the-counter medications and associated adverse drug events among HIV-infected patients. Res Social Adm Pharm. 2008;4:292–301. doi: 10.1016/j.sapharm.2007.08.001. [DOI] [PubMed] [Google Scholar]
- AL-AZZAM SI, AL-HUSEIN BA, ALZOUBI F, MASADEH MM, AL-HORANI MA. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20:373–80. doi: 10.2478/v10001-007-0038-9. [DOI] [PubMed] [Google Scholar]
- ANDERSON S. Community pharmacy and public health in Great Britain, 1936 to 2006: how a phoenix rose from the ashes. J Epidemiol Community Health. 2007;61:844–8. doi: 10.1136/jech.2006.055442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous. Report of the 4th WHO Consultative Group on the Role of the Pharmacist. World Health Organization; Geneva: 1998. The role of the pharmacist in self-care and self-medication. [Google Scholar]
- ANONYMOUS. At-home medication mistakes causing more accidental deaths. Mayo Clin Womens Healthsource. 2009a;13:3. [PubMed] [Google Scholar]
- Anonymous. The Details of the Medical Reform [Online] Chinese Government Net; 2009b. [Accessed Jun. 26 2009]. Available: http://www.gov.cn/test/2009-04/08/content_1280218.htm. [Google Scholar]
- Anonymous. The standing conference of State Council of China adopted Guidelines for Furthering the Reform of Health-care System in Principle [Online] Ministry of Health of China; 2009c. [Accessed Augest 4 2010]. Available: http://www.moh.gov.cn/publicfiles/business/htmlfiles/mohbgt/s3582/200901/38889.htm. [Google Scholar]
- AWAD A, ELTAYEB I, MATOWE L, THALIB L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- AWAD AI, ELTAYEB IB. Self-medication practices with antibiotics and antimalarials among Sudanese undergraduate university students. Ann Pharmacother. 2007;41:1249–55. doi: 10.1345/aph.1K068. [DOI] [PubMed] [Google Scholar]
- AWAD AI, ELTAYEB IB, CAPPS PA. Self-medication practices in Khartoum State, Sudan. Eur J Clin Pharmacol. 2006;62:317–24. doi: 10.1007/s00228-006-0107-1. [DOI] [PubMed] [Google Scholar]
- BERZANSKYTE A, VALINTELIENE R, HAAIJER-RUSKAMP FM, GUREVICIUS R, GRIGORYAN L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19:246–53. doi: 10.2478/v10001-006-0030-9. [DOI] [PubMed] [Google Scholar]
- BI P, TONG S, PARTON KA. Family self-medication and antibiotics abuse for children and juveniles in a Chinese city. Soc Sci Med. 2000;50:1445–50. doi: 10.1016/s0277-9536(99)00304-4. [DOI] [PubMed] [Google Scholar]
- BLOOM G, XINGYUAN G. Health sector reform: lessons from China. Soc Sci Med. 1997;45:351–60. doi: 10.1016/s0277-9536(96)00350-4. [DOI] [PubMed] [Google Scholar]
- BLUMENTHAL D, HSIAO W. Privatization and its discontents--the evolving Chinese health care system. N Engl J Med. 2005;353:1165–70. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- DETELS R, WU Z, ROTHERAM MJ, LI L, GUAN J, YIN Y, LIANG G, LEE M, HU L. Sexually transmitted disease prevalence and characteristics of market vendors in eastern China. Sex Transm Dis. 2003;30:803–8. doi: 10.1097/01.OLQ.0000086607.82667.CF. [DOI] [PubMed] [Google Scholar]
- DONG H. Health financing policies: patient care-seeking behaviour in rural China. Int J Technol Assess Health Care. 2003;19:526–32. doi: 10.1017/s0266462303000461. [DOI] [PubMed] [Google Scholar]
- DONG Z, PHILLIPS MR. Evolution of China’s health-care system. Lancet. 2008;372:1715–6. doi: 10.1016/S0140-6736(08)61351-3. [DOI] [PubMed] [Google Scholar]
- FUENTES ALBARRAN K, VILLA ZAPATA L. Analysis and quantification of self-medication patterns of customers in community pharmacies in southern Chile. Pharm World Sci. 2008;30:863–8. doi: 10.1007/s11096-008-9241-4. [DOI] [PubMed] [Google Scholar]
- HO CS, GOSTIN LO. The social face of economic growth: China’s health system in transition. JAMA. 2009;301:1809–11. doi: 10.1001/jama.2009.555. [DOI] [PubMed] [Google Scholar]
- HSIAO WC. The Chinese health care system: lessons for other nations. Soc Sci Med. 1995;41:1047–55. doi: 10.1016/0277-9536(94)00421-o. [DOI] [PubMed] [Google Scholar]
- HUGHES CM. Monitoring self-medication. Expert Opin Drug Saf. 2003;2:1–5. doi: 10.1517/14740338.2.1.1. [DOI] [PubMed] [Google Scholar]
- HUGHES CM, MCELNAY JC, FLEMING GF. Benefits and risks of self medication. Drug Saf. 2001;24:1027–37. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- INDERMITTE J, REBER D, BEUTLER M, BRUPPACHER R, HERSBERGER KE. Prevalence and patient awareness of selected potential drug interactions with self-medication. J Clin Pharm Ther. 2007;32:149–59. doi: 10.1111/j.1365-2710.2007.00809.x. [DOI] [PubMed] [Google Scholar]
- KAMAT VR, NYATO DJ. Soft targets or partners in health? Retail pharmacies and their role in Tanzania’s malaria control program. Soc Sci Med. 2010;71:626–33. doi: 10.1016/j.socscimed.2010.04.016. [DOI] [PubMed] [Google Scholar]
- LIEBER E, LI L, WU Z, ROTHERAM-BORUS MJ, GUAN J. HIV/STD stigmatization fears as health-seeking barriers in China. AIDS Behav. 2006;10:463–71. doi: 10.1007/s10461-005-9047-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LINDELOW MWA. China’s Health Sector – Why Reform is Needed? Washington, DC: World Bank; 2005. [Google Scholar]
- LIU X, HSIAO WC. The cost escalation of social health insurance plans in China: its implication for public policy. Soc Sci Med. 1995;41:1095–101. doi: 10.1016/0277-9536(94)00423-q. [DOI] [PubMed] [Google Scholar]
- LIU Y, RAO K, WU J, GAKIDOU E. China’s health system performance. Lancet. 2008;372:1914–23. doi: 10.1016/S0140-6736(08)61362-8. [DOI] [PubMed] [Google Scholar]
- MA J, LU M, QUAN H. From a national, centrally planned health system to a system based on the market: lessons from China. Health Aff (Millwood) 2008;27:937–48. doi: 10.1377/hlthaff.27.4.937. [DOI] [PubMed] [Google Scholar]
- MA JM, LIU N, CHEN AP, YANG GH. Study on knowledge, attitudes and behaviours regarding infectious diseases among Chinese people in 2002. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:389–93. [PubMed] [Google Scholar]
- MOU J, CHENG J, ZHANG D, JIANG H, LIN L, GRIFFITHS SM. Health care utilisation amongst Shenzhen migrant workers: does being insured make a difference? BMC Health Serv Res. 2009;9:214. doi: 10.1186/1472-6963-9-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MUHR T. Atlas TI Berlin: Scientific Software Development. 1997. [Google Scholar]
- NAVES JDEO, CASTRO LL, CARVALHO CM, MERCHAN-HAMANN E. Self-medication: a qualitative approach of its motivations. Cien Saude Colet. 2010;15(Suppl 1):1751–62. doi: 10.1590/s1413-81232010000700087. [DOI] [PubMed] [Google Scholar]
- NIMH COLLABORATIVE HIV/STD PREVENTION TRIAL. Methodological overview of a five-country community-level HIV/sexually transmitted disease prevention trial. AIDS. 2007a;21(Suppl 2):S3–18. doi: 10.1097/01.aids.0000266453.18644.27. [DOI] [PubMed] [Google Scholar]
- NIMH COLLABORATIVE HIV/STD PREVENTION TRIAL. Selection of populations represented in the NIMH Collaborative HIV/STD Prevention Trial. AIDS. 2007b;21(Suppl 2):S19–28. doi: 10.1097/01.aids.0000266454.26268.90. [DOI] [PubMed] [Google Scholar]
- OUEDRAOGO LT, SOME IT, DIARRA M, GUISSOU IP. Self-medication in the treatment of acute malaria: study based on users of private health drug stores in Ouagadougou, Burkina Faso. Bull Soc Pathol Exot. 2008;101:124–7. [PubMed] [Google Scholar]
- PENG Y, CHANG W, ZHOU H, HU H, LIANG W. Factors associated with health-seeking behaviour among migrant workers in Beijing, China. BMC Health Serv Res. 2010;10:69. doi: 10.1186/1472-6963-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAMESH M, WU X. Health policy reform in China: lessons from Asia. Soc Sci Med. 2009;68:2256–62. doi: 10.1016/j.socscimed.2009.03.038. [DOI] [PubMed] [Google Scholar]
- SIHAVONG A, LUNDBORG CS, SYHAKHANG L, AKKHAVONG K, TOMSON G, WAHLSTROM R. Antimicrobial self medication for reproductive tract infections in two provinces in Lao People’s Democratic Republic. Sex Transm Infect. 2006;82:182–6. doi: 10.1136/sti.2005.016352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SULEMAN S, KETSELA A, MEKONNEN Z. Assessment of self-medication practices in Assendabo town, Jimma zone, southwestern Ethiopia. Res Social Adm Pharm. 2009;5:76–81. doi: 10.1016/j.sapharm.2008.04.002. [DOI] [PubMed] [Google Scholar]
- THANH NX, LOFGREN C, PHUC HD, CHUC NT, LINDHOLM L. An assessment of the implementation of the Health Care Funds for the Poor policy in rural Vietnam. Health Policy. 2010 doi: 10.1016/j.healthpol.2010.05.005. [DOI] [PubMed] [Google Scholar]
- WANG S. China’s health system: from crisis to opportunity. Yale-China Health Journal. 2004;3:5–49. [Google Scholar]
- WAZAIFY M, AL-BSOUL-YOUNES A, ABU-GHARBIEH E, TAHAINEH L. Societal perspectives on the role of community pharmacists and over-the-counter drugs in Jordan. Pharm World Sci. 2008;30:884–91. doi: 10.1007/s11096-008-9244-1. [DOI] [PubMed] [Google Scholar]
- WEN Y, GUAN J, WU Z, LI L, ROTHERAM-BORUS MJ, LIN C, DETELS R. Pharmacy workers’ sexually transmitted diseases/human immunodeficiency virus knowledge in Fuzhou, China: implications for human immunodeficiency virus testing, treatment, and prevention strategies. Sex Transm Dis. 2009;36:221–6. doi: 10.1097/OLQ.0b013e3181901ca2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WONG WC, YILIN W. A qualitative study on HIV risk behaviours and medical needs of sex workers in a China/Myanmar border town. AIDS Patient Care STDS. 2003;17:417–22. doi: 10.1089/108729103322277439. [DOI] [PubMed] [Google Scholar]
- WONG WC, ZHANG J, WU SC, KONG TS, LING DC. The HIV related risks among men having sex with men in rural Yunnan, China: a qualitative study. Sex Transm Infect. 2006;82:127–30. doi: 10.1136/sti.2005.016790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YIN YP, WU Z, LIN C, GUAN J, WEN Y, LI L, DETELS R, ROTHERAM-BORUS MJ. Syndromic and laboratory diagnosis of sexually transmitted infection: a comparative study in China. Int J STD AIDS. 2008;19:381–4. doi: 10.1258/ijsa.2007.007273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YINHUAN H, HAO C. Investigation on attitude towards self-medication in Chinese urban residents. Chinese Public Health. 2008:24. [Google Scholar]
- YINHUAN H, HAO C, DIFEI W. Investigation on the Self-medication Need of Chinese Urban Residents. Medicine and Society. 2008:21. [Google Scholar]
- YIP W, HSIAO WC. The Chinese health system at a crossroads. Health Aff (Millwood) 2008;27:460–8. doi: 10.1377/hlthaff.27.2.460. [DOI] [PubMed] [Google Scholar]
- YIP W, HSIAO WCL. Economic transition and urban health care in China: impacts and prospects. conference on financial sector reform in China; China: Harvard University; 2001. [Google Scholar]
- YIP W, WAGSTAFF A, HSIAO WC. Economic analysis of China’s health care system: turning a new page. Health Econ. 2009;18(Suppl 2):S3–6. doi: 10.1002/hec.1525. [DOI] [PubMed] [Google Scholar]
- YOUSEF AM, AL-BAKRI AG, BUSTANJI Y, WAZAIFY M. Self-medication patterns in Amman, Jordan. Pharm World Sci. 2008;30:24–30. doi: 10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]
- YU B, MENG Q, COLLINS C, TOLHURST R, TANG S, YAN F, BOGG L, LIU X. How does the New Cooperative Medical Scheme influence health service utilization? A study in two provinces in rural China. BMC Health Serv Res. 2010;10:116. doi: 10.1186/1472-6963-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ZHAO G, DETELS R, GU F, LI D, LI X, LI Y, LI K. The distribution of people seeking STD services in the various types of health care facilities in Chao Yang District, Beijing, China. Sex Transm Dis. 2008;35:65–7. doi: 10.1097/OLQ.0b013e318148b4dc. [DOI] [PMC free article] [PubMed] [Google Scholar]