Abstract
Isolated oculomotor nerve palsy (ONP) attributable to mild closed head trauma is a distinct rarity. Its diagnosis places high demands on the radiologist and the clinician. The authors describe this condition in a 36-year-old woman who slipped while walking and struck her face. Initial computed tomography did not reveal any causative cerebral and vascular lesions or orbital and cranial fractures. Enhancement and swelling of the cisternal segment of the oculomotor nerve was seen during the subacute phase on thin-sectioned contrast-enhanced magnetic resonance images. The current case received corticosteroid therapy, and then recovered fully in 13 months after injury. Possible mechanism of ONP from minor head injury is proposed and previous reports in the literature are reviewed.
Keywords: Computed tomography, Head injury, Magnetic resonance imaging, Oculomotor nerve, Oculomotor nerve palsy
INTRODUCTION
Cranial nerve lesions often accompany head trauma. Injury of the cranial nerve is the result of important kinetic forces to the brain and cranium. The trauma required to damage the oculomotor nerve (ON) usually is severe and associated with other neurologic deficits, basilar skull fracture, orbital injury or subarachnoid hemorrhage14,16). However, in rare instances, minor blunt head trauma can cause isolated oculomotor nerve palsy (ONP) without other cranial nerve palsy. Nevertheless, only a few reports have described the clinical feature of these patients, and mechanisms and imaging studies of nerve damage have not been discussed in depth2,8).
The authors herein present a case of previously healthy woman who developed acute isolated ONP caused by mild frontal blow that insufficient to cause fractured skull or loss of consciousness. To our knowledge, this is the first reported case in which the diagnosis of traumatic isolated ONP was rightly made by high-quality three-dimensional (3D) reconstructed magnetic resonance images (MRIs). The authors also discuss the current knowledge of the relevant neuroanatomy, the proposed mechanism of nerve injury, and treatment of solitary ONP associated with minor head trauma.
CASE REPORT
A 36-year-old woman with no past medical history was admitted to hospital after slipping on the ice. The patient did not lose consciousness, but she immediately noted drooping of her right eyelid and double vision when she elevated the lid. There was a 3 cm laceration wound on the chin and some abrasions over the neck and the central region of her face (Fig. 1A).
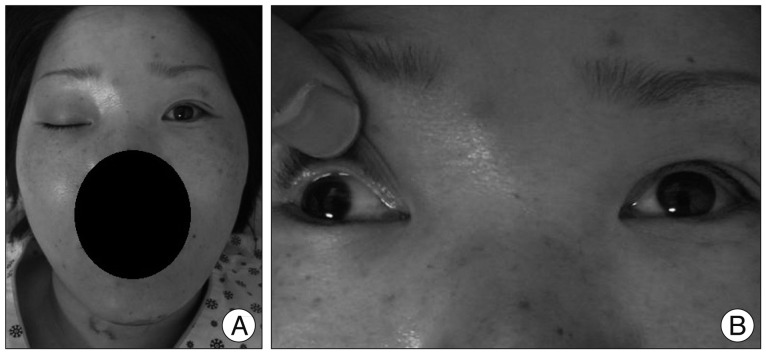
Fig. 1.
Appearance and examination of ocular movement and pupil size on initial presentation. Note bruises on the face and the right side of her neck. The patient can't elevate the right upper eyelid which is completely drooped (A). The right eye has limited motion in up, down, and medial gazes with lateral deviation (B).
The right pupil was fixed and dilated, and there was complete right ptosis. The patient could not elevate, depress, or adduct the right eye, but the eye intorted on attempted downgaze (Fig. 1B). The right pupil measured 5 mm in diameter and was sluggish reactive to light. Ophthalmologic tests of vision and intraocular pressure were within normal ranges in both eyes. Further physical and neurological examinations were normal. Skull X-rays and orbital computed tomography (CT) scans immediately after the accident failed to show fractures. MRI and MR angiography of the brain did not reveal any pathology on admission (Fig. 2). Contrast-enhanced spoiled gradient-recalled (SPGR) MR sequences with multiplanar reconstruction (MPR) was subsequently performed to produce high-resolution images of the cisternal portions of the cranial nerves. The 3D MR studies indicated a slightly rough-shaped ON near the the posterior petroclinoid ligament (PCL), but no nerve enhancement (Fig. 3A). The patient's history, along with the ophthalmologic symptoms and the radiologic findings strongly suggested the diagnosis of an isolated lesion in the course of the ON without further damage in the right oculomotor nucleus.
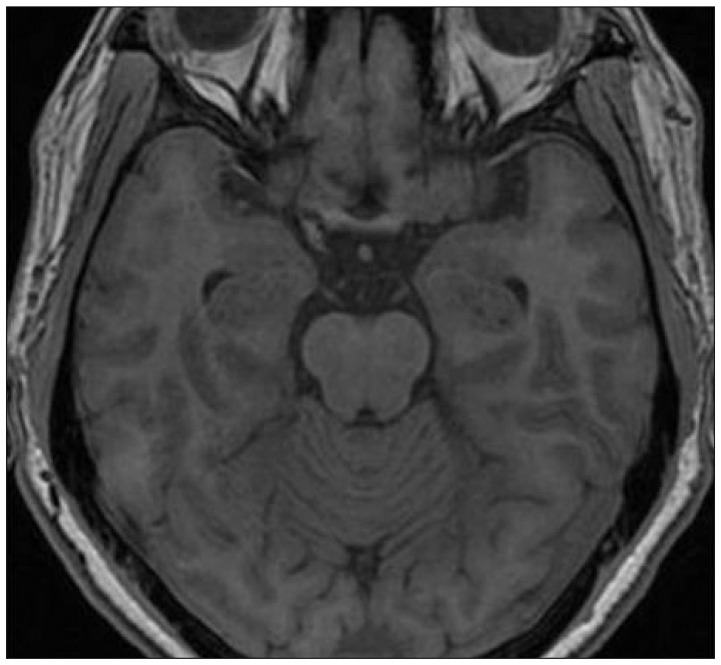
Fig. 2.
Axial T1-weighted magnetic resonance image reveals no abnormalities in the third nerve and the midbrain.
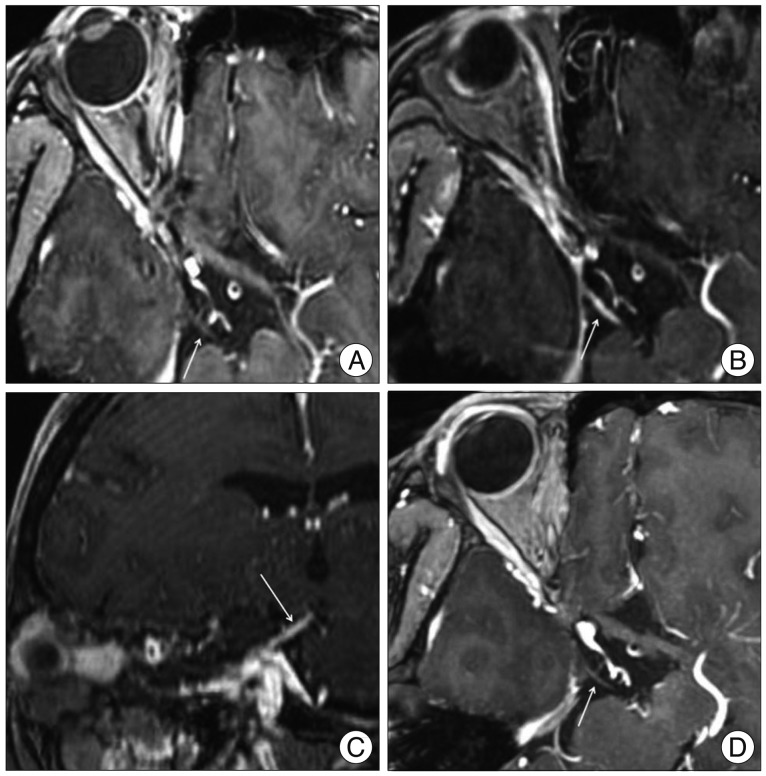
Fig. 3.
Multiplanar reconstruction magnetic resonance images using contrast-enhanced spoiled gradient-recalled sequences clearly depict the oculomotor nerves (ONs) (arrows) in head trauma patient. A : Initial image shows focal swelling of the right ON at the posterior petroclinoid ligament, but no gadolinium enhancement. B and C : Axial and sagittal reconstruction images obtained 16 days after the injury reveal diffuse thickening and enhancement of the cisternal portion of the right ON. D : Follow-up study confirms virtually complete resolution of the enhancement of the nerve itself.
She was then treated with oral prednisone in a tapering dose over several weeks. MPR of contrast-enhanced 3D MRI taken 2 weeks after the event clearly demonstrated strong enhancement and enlargement over the whole length of the right ON (Fig. 3B, C). At the time of follow-up two months after trauma, her ptosis slightly improved. Three months later, ptosis was completely resolved, and there was some restoration of ocular motion in the direction of adduction. Follow-up MRI 6 months post-injury showed complete resolution of the enhancement and swelling of the right ON (Fig. 3D). Nine months after the injury, the patient still suffered from symptomatic glare and blurred vision for near objects, although complete recovery of diplopia was seen. Four months later, spontaneous improvement of pupillary dilatation was observed, and ophthalmology examination also revealed no paralysis of accommodation.
DISCUSSION
Because traumatic ONP is highly associated with skull or cervical spine fracture and intracranial injury, all possible causes and additional injuries should be ruled out with clinical examination and imaging investigation10). Brain CT and CT angiography is recommended in acutely traumatized patients with ONP to rapidly evaluate blood, bone, supratentorial structure, and vascular anomaly. Cerebral MRI is also indicated because CT scans may fail to detect abnormalities in the midbrain and the ON itself. On admission of our patient, the absence of other neurological signs and normal brain MRI suggested the lesion was most likely within the subarachnoid space, as the other important structures near the ON, such as the brainstem, cavernous sinus and orbit, were undamaged.
Experimental and postmortem examinations illustrated types of damage to the cranial nerve following head trauma : 1) lesion involves nucleus or nuclear complex, 2) rootlets avulsion at their exit from the brainstem, 3) focal softening in the subarachnoid portion of the nerve, and 4) cellular edema and intraneural hemorrhage at the sites of fixation3,4). However, the actual mechanisms of isolated ONP from minor head trauma are still not apparent. It has been reported that most patients with traumatic ONP had suffered a blow to the central frontal region of the head like the present case5,9). With frontal blows to the head, a violent linear accelerated force in the rostro-caudal plane is generated, which runs parallel to the course of the ON11). Anatomically, the ON crosses the posterior PCL, at which point it is thought to be susceptible to damage as the brainstem moves downward. During impact to head, therefore, the ON fascicule is focally stretched and contused at the posterior PCL act as a fulcrum. This appears to be the accepted mechanism for patients of complete ONP seen after minor trauma without identifiable lesions like this case.
The high-resolution multipositional MRI is helpful to define the number of affected extraocular muscles and the nature of the nerve damages in patients with ophthalmoplegia due to various causes12,17). This report on traumatic ONP confirmed an intrinsic transient enhancement limited to the ON was the only anatomical abnormality on MRI with MPR. Indeed, the similarity with enhancement of the facial nerve seen in patients with Bell's palsy which is considered a form of viral neuritis is striking7). Most ophthalmoplegic patients in whom ocular motor nerves were abnormally enhanced, due to ischemia, inflammatory or demyelinating conditions appeared recovered in 1-6 months, with diminishing nerve enhancement13,17). In these patients, the fact that enhancement disappears within several weeks as the patient's symptoms resolve after treatment with steroids is a strong indication that the clinical presentations and the radiologic abnormality are related6,15). Therefore, follow-up contrast-enhanced 3D MRI might be useful for predicting the treatment results and clinical course.
The rate of recovery for ONP caused by trauma is slow and prolonged18). Follow-up of this case showed that after five months, there was partial recovery of the ONP, which was similarly reported in a few case series2,7,12,15). In one study on ONP with mild head injury10), the prognoses of patients with ptosis, external ophthalmoplegia and internal ophthalmoplegia were evaluated separately. Recovery rates were 100%, 60%, and 50% respectively. However, the individual prognosis of traumatic ONP is unpredictable. The authors treated the patient with a 6-week course of corticosteroids, although this is not reported in the literature. Nevertheless, the authors thought it might be useful with regard to the cellular edema described in histopathologic examinations. Generally speaking, after a traumatic ONP, 6-12 months is usually allowed for spontaneous recovery before surgical intervention is considered1). During this observational period, temporary treatment options can be tried to overcome disabling diplopia, including occlusion of an eye with pads, wearing prism lenses or injection of botulinum toxin into the lateral rectus muscle in certain patients8). Strabismus surgery is proposed when there is no further improvement. The pupil in traumatic ONP shows denervation hypersensitivity and constricts in response to low-dose pilocarpine drops16). Using this solution counters glare and may help in the strengthening of fusion in downgaze in the less seriously injured subgroup.
CONCLUSION
The authors illustrate an interesting case of purely isolated ONP that occurred as a consequence of a minor head injury. High-resolution and multi-axial enhanced MRI can be helpful in the diagnosis and monitoring of patients with this rare phenomenon, accurately depicting a transient internal abnormality in the cisternal portion of the ON at the posterior PCL.
References
- 1.Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007;27:257–268. doi: 10.1055/s-2007-979681. [DOI] [PubMed] [Google Scholar]
- 2.Chen CC, Pai YM, Wang RF, Wang TL, Chong CF. Isolated oculomotor nerve palsy from minor head trauma. Br J Sports Med. 2005;39:e34. doi: 10.1136/bjsm.2004.016311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhaliwal A, West AL, Trobe JD, Musch DC. Third, fourth, and sixth cranial nerve palsies following closed head injury. J Neuroophthalmol. 2006;26:4–10. doi: 10.1097/01.wno.0000204661.48806.1d. [DOI] [PubMed] [Google Scholar]
- 4.Elston JS. Traumatic third nerve palsy. Br J Ophthalmol. 1984;68:538–543. doi: 10.1136/bjo.68.8.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eyster EF, Hoyt WF, Wilson CB. Oculomotor palsy from minor head trauma. An initial sign of basal intracranial tumor. JAMA. 1972;220:1083–1086. [PubMed] [Google Scholar]
- 6.Hosoya T, Adachi M, Yamaguchi K, Yamaguchi K, Kato T, Sugai Y. Abducens nerve enhancement demonstrated by multiplanar reconstruction of contrast-enhanced three-dimensional MRI. Neuroradiology. 2001;43:295–301. doi: 10.1007/s002340000338. [DOI] [PubMed] [Google Scholar]
- 7.Janssen K, Wojciechowski M, Poot S, De Keyser K, Ceulemans B. Isolated abducens nerve palsy after closed head trauma : a pediatric case report. Pediatr Emerg Care. 2008;24:621–623. doi: 10.1097/PEC.0b013e3181850c5c. [DOI] [PubMed] [Google Scholar]
- 8.Kaido T, Tanaka Y, Kanemoto Y, Katsuragi Y, Okura H. Traumatic oculomotor nerve palsy. J Clin Neurosci. 2006;13:852–855. doi: 10.1016/j.jocn.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 9.Kruger M, Noel P, Ectors P. Bilateral primary traumatic oculomotor nerve palsy. J Trauma. 1986;26:1151–1153. doi: 10.1097/00005373-198612000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Kuo LT, Huang AP, Yang CC, Tsai SY, Tu YK, Huang SJ. Clinical outcome of mild head injury with isolated oculomotor nerve palsy. J Neurotrauma. 2010;27:1959–1964. doi: 10.1089/neu.2010.1407. [DOI] [PubMed] [Google Scholar]
- 11.Levy RL, Geist CE, Miller NR. Isolated oculomotor palsy following minor head trauma. Neurology. 2005;65:169. doi: 10.1212/01.wnl.0000167288.10702.03. [DOI] [PubMed] [Google Scholar]
- 12.Liu YT, Lee YC, Liu HC. Isolated oculomotor nerve palsy due to head injury. J Chin Med Assoc. 2004;67:149–151. [PubMed] [Google Scholar]
- 13.Mark AS, Casselman J, Brown D, Sanchez J, Kolsky M, Larsen TC, 3rd, et al. Ophthalmoplegic migraine : reversible enhancement and thickening of the cisternal segment of the oculomotor nerve on contrast-enhanced MR images. AJNR Am J Neuroradiol. 1998;19:1887–1891. [PMC free article] [PubMed] [Google Scholar]
- 14.Memon MY, Paine KW. Direct injury of the oculomotor nerve in craniocerebral trauma. J Neurosurg. 1971;35:461–464. doi: 10.3171/jns.1971.35.4.0461. [DOI] [PubMed] [Google Scholar]
- 15.Muthu P, Pritty P. Mild head injury with isolated third nerve palsy. Emerg Med J. 2001;18:310–311. doi: 10.1136/emj.18.4.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagaseki Y, Shimizu T, Kakizawa T, Fukamachi A, Nukui H. Primary internal ophthalmoplegia due to head injury. Acta Neurochir (Wien) 1989;97:117–122. doi: 10.1007/BF01772821. [DOI] [PubMed] [Google Scholar]
- 17.Quisling SV, Shah VA, Lee HK, Policeni B, Smoker WR, Martin C, et al. Magnetic resonance imaging of third cranial nerve palsy and trigeminal sensory loss caused by herpes zoster. J Neuroophthalmol. 2006;26:47–48. doi: 10.1097/01.wno.0000204660.41183.1b. [DOI] [PubMed] [Google Scholar]
- 18.Walter KA, Newman NJ, Lessell S. Oculomotor palsy from minor head trauma : initial sign of intracranial aneurysm. Neurology. 1994;44:148–150. doi: 10.1212/wnl.44.1.148. [DOI] [PubMed] [Google Scholar]