Abstract
Introduction
horax injuries are to be found in approximately 78% amongst all accident victims. Moreover, they implicate an increase in mortality rate. Consequently, an adequate contemporary treatment has to begin preclinically, even if the conditions are less comfortable than in a clinical setting. Emergency doctors need to be familiar with the placement of chest tubes.
Materials and Methods
From January 1, 2007 to December 31, 2010, emergency doctors of the rescue helicopter site Christoph 20 had to place chest tubes directly at the scene of an accident in 49 patients. These patients were now reidentified, and their clinical course was reevaluated. By means of apparative diagnostics, it was possible to analyze the location of the tubes tip. Following a comparison of the patient, outcome versus the quality of preclinical thoracic discharge could be made.
Results
The preclinical placement of a chest tube became necessary mainly because of a blunt thoracic trauma. This was predominantly related to victims of traffic accidents, whereas male victims clearly dominated. Forty-two of those patients received further treatment at the Klinikum Bayreuth hospital, enabling an analysis of the tubes location by CAT (computed axial tomography) scan. Six patients had been discharged on both sides, contributing to 48 tube tips that could be examined concerning their location. Of the 48 chest tubes, 46 had been placed from a lateral approach. The ventral access by Monaldi had only been chosen in two cases. Altogether, nine incorrect placements, mainly within the right interlobe gap, had been detected.
Conclusions
The study collective showed a significant preference to the lateral approach when placing a chest tube at the emergency scene of an accident. In total, a prevalence of 19% incorrect placements could be revealed, meaning the chest tube had either been placed within the lung parenchyma, the interlobe gap, or extrathoracically. Concerning the patient outcome, no statistically significant difference regarding the clinical course after incorrect chest tube placement could be identified.
Keywords: air rescue, chest tube, pneumothorax, preclinical application of a thoracic drain, thoracic trauma
Introduction
As part of the air rescue and related preclinical emergency doctoral practice, treating blunt thorax traumas is an important field of action. Isolated thorax traumas are rather rare. They often occur in combination in polytraumatized patients. Between 40% and 66% of polytraumatized patients show a blunt injury of the thorax, especially in Europe [1]. In comparison to other injuries, multiple casualties show thorax traumas nearly as often as cranium brain traumas (40%–60%) or severe injuries of the extremities (42%–67%) [2, 3].
The incidence of a pneumothorax as the most common thoracic injury is indicated with 9%–41% [4–7]. However, only 17%–25% of patients with a secured chest trauma show a relevant pneumothorax requiring treatment [8]. Besides the isolated pneumothorax, one has to add the hemothorax, the combined hemopneumothorax, rib fractures, and especially lung contusions as frequently occurring consequences of blunt force on the thorax. Kshettry and Bolmann [24] found in a study of polytraumatized traffic accident victims that more than half the patients had a thorax trauma. Through the predominant accident mechanism of a high speed trauma and the severe energy impact, a high injury gravity has to be ascertained. Paramedics arriving at the scene of accident first often have to recognize drastic breathing or lung dysfunctions and treat them. Depending on the injury pattern and condition of the patient’s vital functions, various emergency medical interventions can become necessary (securing the respiratory passages and cardiovascular function, etc.). The preclinical assessment of the severity of a thorax trauma is often impeded by the lack of equipment. Therefore, the assessment of the severity of the thorax trauma has to be made on the basis of the accident, several symptoms, and examination findings. Ominous signs of a severe chest trauma are, for example, decreased breathing sounds, hyper sonorous percussion, circulatory insufficiency with congested neck veins, or a rising pressure of respiration after intubation. Aufmkolk et al. demonstrated in their evaluation of the polytrauma database of the German Society of Trauma Surgery that, in only 49% of cases, a proper preclinical assessment of the severity of chest injury was existent [3]. A misjudgement on site poses the risk of omission of necessary measures as well as the risk of additional harm to the patient through unnecessary invasive procedures or an extension of the preclinical treatment time. The aim of this essay is to give a descriptive analysis of the preclinical placed thorax drainages with patients’ outcome analysis through the rescue helicopter team “Christoph 20.”
Materials and Methods
Between January 1, 2007 and December 31, 2010, emergency doctors of the rescue helicopter Christoph 20 stationed at Klinikum Bayreuth Hospital placed a preclinical thorax drainage with a total of 49 patients. It was followed by the identification of these patients and monitoring the course of injury at Klinikum Bayreuth Hospital. Since the majority of patients with a preclinical thorax drainage received a trauma scan in line with the polytrauma algorithm upon hospital admission, it was possible to access appropriate images for verification of the chest tube system. A comparison of the course of injury after failed malposition was to provide information on the risk benefit ratio in a preclinical drainage system.
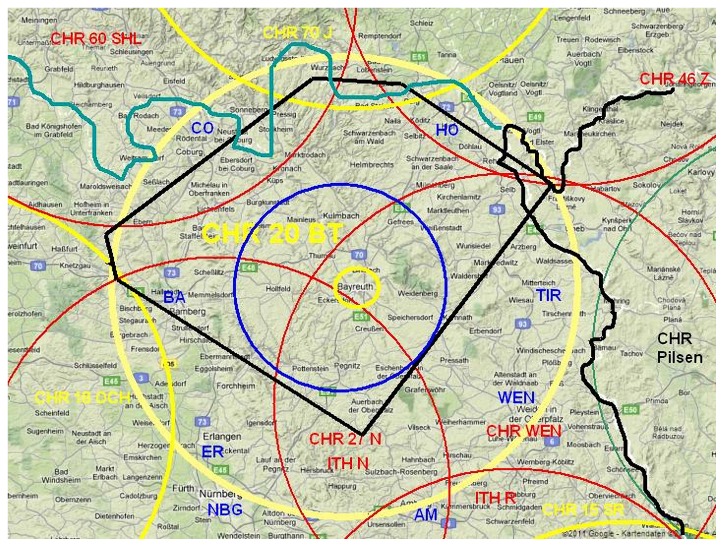
Enclosed criteria
The analysis was based on the medical use of data from the rescue helicopter Christoph 20. The operation radius of Christoph 20 is 60–70 km and includes the city of Klinikum Bayreuth and district with neighboring counties (see Fig. 1). The operating time is from sunrise (earliest from 7 am) until sunset. The alarm is sent via the Rescue Coordination Centre of Klinikum Bayreuth. Since the foundation in 1984, the crew consists of a pilot, a paramedic assistant of the Bavarian Red Cross of the Klinikum Bayreuth district, and a member of medical staff, mainly from the Trauma Clinic at Klinikum Bayreuth Hospital. The latest type of helicopter is an EC (Eurocopter) 135, which is equipped with facilities in accordance with the requirements for a primary rescue helicopter and can transport one patient. The data collection covers the period from January 1, 2007 to December 31, 2010. In accordance with the question, only patients and their operational protocols with chest trauma and preclinical facility of a chest drain were included. Since a majority of the patients were polytraumatized and because a polytrauma scan was conducted according to guidelines, a CAT (computed axial tomography) of the thorax was carried out for almost all patients so that the images which are digitally stored on the PACS (picture archiving and communication system) could be evaluated again retrospectively. Forty-nine patients with preclinical thorax drainage were followed up. Two patients died before the radiological thorax test could be carried out; in one case, there were only conventional X-rays available, and four patients could not be followed up primarily because of relocation to another hospital from where the data acquisition was not possible due to protection provisions. In total, 42 preclinically applied thorax drainages could be tested through thoracic computed tomography (CT) for correct position.
Fig. 1.
Operation radius of the rescue helicopter Christoph 20
Assessment
Through the trauma scan of the thorax, the position of the thoracic drainage was assessed retrospectively in collaboration with an experienced radiologist. According to the standard classification (see Table I), the following estimates were made [9, 10].
Table I.
Classification of thoracic drainage system [9, 10]
| Correct position | Top of the thoracic drainage lies in the pleural cavity dorsal or ventral to the adjacent parietal pleura |
| Interlobar position | Top of the thoracic drainage lies in the interlobar gap |
| Parenchymatous position |
Top lies in the area of the lung parenchyma |
| Extrathoracic position | Top lies outside the pleural cavity, i.e. in the soft tissue or abdomen |
Results
During the documented four-year period, the rescue helicopter Christoph 20 was alerted in 6168 emergency cases of which 703 (11.4%) had been traffic accidents. According to the estimation in the emergency operation protocol, the majority of these patients had at least a serious thorax trauma (AIS >3). The Abbreviated Injury Scale (AIS) is an anatomically based consensus-derived global severity scoring system that classifies each injury in every body region according to its relative severity on a six point ordinal scale: 1 minor, 2 moderate, 3 serious, 4 severe, 5 critical, and 6 maximal (currently untreatable).
About 8.8% (49 of 554) of these at least serious thorax traumatized patients required the installation of a preclinical thoracic drainage (see Table II).
Table II.
Emergency overview Christoph 20
| 2007 | 2008 | 2009 | 2010 | Sum | |
|---|---|---|---|---|---|
| Emergencies (overall) | 1483 | 1554 | 1558 | 1573 | 6168 |
| Traffic accidents | 199 | 169 | 184 | 151 | 703 |
| Thoracic drainages | 12 | 11 | 13 | 13 | 49 |
| Thorax trauma | 124 | 137 | 127 | 121 | 554 |
Patient population
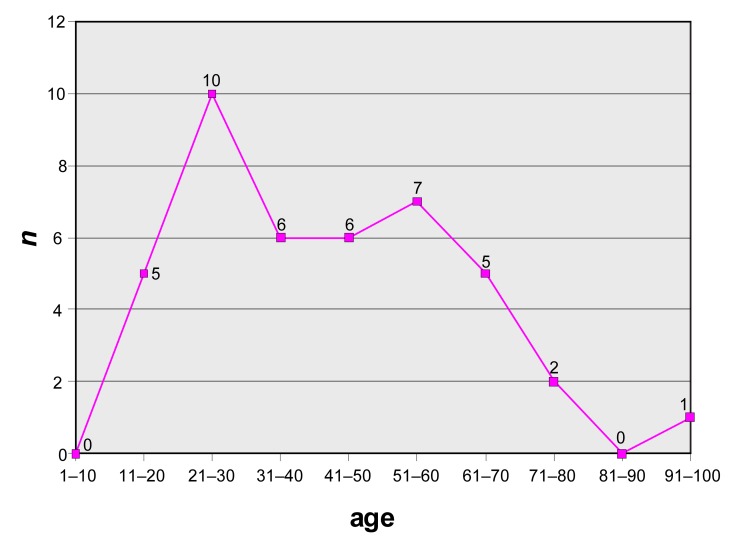
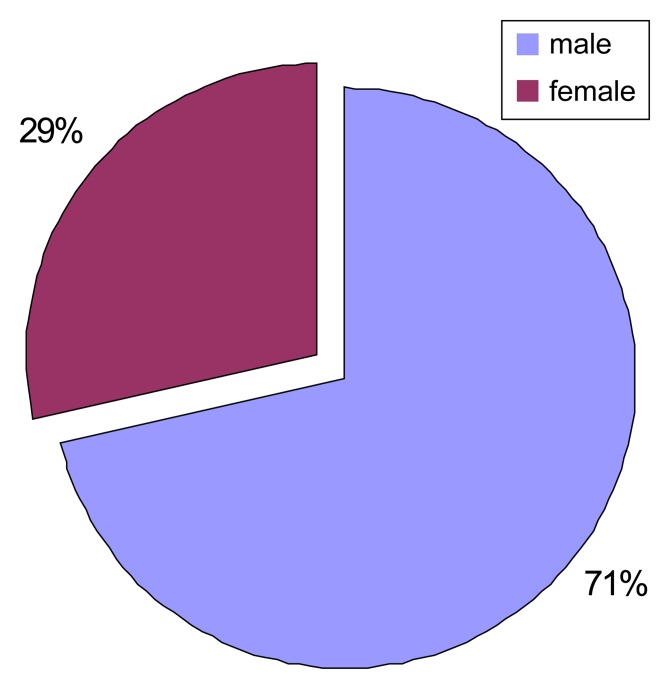
The average age of the study population was 42.3 ± 14.1 years. This resulted in a twin-peaked distribution. The first summit was in the age decade from 21 to 30 years. The second summit was around age 50 (see Fig. 2). Of the 42 patients enrolled in the study, 30 were male and 12 were female (see Fig. 3).
Fig. 2.
Age distribution
Fig. 3.
Gender ratio
In contrast to studies from the regions of North America or Africa where mainly penetrating thorax injuries predominate, in this test, a large number of patients (95.2%) suffered the injury as part of a blunt thorax trauma. The average NACA (National Advisory Committee for Aeronautics) score was 4.3 ± 0.2. The Glasgow Coma Scale (GCS) at the scene of accident was very heterogeneous, and averaged 9.6 ± 4.9. Twenty patients (47.6%) were already intubated at the scene of accident by the emergency doctor, another eight patients upon arrival in the reanimation room. The overall mortality in the study, defined as death during hospitalization, was 33.3%. The total length of stay in acute care hospital was 32.4 ± 21.1 days (see Table III).
Table III.
Characteristics of the study population
| Parameter | Average value |
|---|---|
| Age | 42.3 ± 14.1 years |
| Trauma mechanization | 95.2% blunt trauma |
| NACA | 4.3 ± 0.2 |
| Preclinical intubation rate | 47.6% |
| GCS at scene of accident | 9.6 ± 4.9 |
| Mortality | 33.3% |
| Hospital days | 32.3 ± 21.1 days |
| GCS, Glasgow Coma Scale; NACA, National Advisory Committee for Aeronautics. Scoring system of the severity in injuries was developed for accidents in aviation: NACA 0, no injury; NACA I, minor disturbance; NACA II, moderate disturbance; NACA III, Moderate not life-threatening disorder; NACA IV, serious incident where rapid development into a life-threatening condition cannot be excluded, NACA V, acute danger, NACA VI, respiratory or cardiac arrest; NACA VII, death | |
Of the 42 patients included in the study, 36 were provided with a drainage and 6 had already needed a preclinical bilateral drainage system. Both thorax sides were affected in approximate equal frequency. Only two drainages were placed conspicuously above the ventral approach according to Monaldi. Forty-six drainages were placed laterally. The height of the in-between intercostal space through which the thoracic drainage was inserted corresponded mainly to the standard height, that is, with the ventrally placed, the second ICR was chosen and, with the laterally placed, the third to the sixth ICR was used as entry point (see Table IV).
Table IV.
Side distribution after location of the thoracic drainage
| Side | Ventral | Lateral |
|---|---|---|
| Right side | 2 | 24 |
| Left side | 0 | 22 |
Malpositions could be detected in nine cases through CT scan. Five of nine radiological misplaced drainages were in the interlobar gap. This was the most frequent malposition. Of the four remaining malpositions, three drainage tops were located in the lung parenchyma and one, extrathoracically. Here, the pleura was not penetrated, so the drainage top was outside the thorax in the soft tissue. In cases of drainages of the right thoracic, half there prevailed an interlobar malposition (see Table V).
Table V.
Malpositions
| Right | Left | |
|---|---|---|
| II Interlobar | 4 | 1 |
| III Parenchymatous | 1 | 2 |
| IV Extra thoracic | 0 | 1 |
When viewing the subpopulation of the patients with radiological malposition, the average age was 40.2 ± 20.5 years. The trauma mechanism was 100% blunt. The NACA score of 4.6 ± 0.3 was significantly higher than in the whole population. Even the intubation ratio of 88.8% and the Glasgow Coma Scale with 7.3 indicate that, by trend in the group of patients with malposition, there were more severely injured patients than in the group without malposition.
Discussion
Indication of the thoracic drainage
Compared to other established measures in the preclinical emergency medical aid, the application of a thoracic drainage is rarely necessary and, therefore, possibly not so familiar to every emergency doctor. However, it is required that all actively practicing emergency doctors are certain in putting up the indication as well as performing a preclinical placed thoracic drainage. An untreated tension pneumothorax, which potentially can develop out of every pneumothorax, is acutely life-threatening and calls for immediate medical action. A study on a pig model showed that a tension pneumothorax can quickly lead to a heart-circulation insufficiency. By placing a thoracic drainage and relieving the tension pneumothorax, the heart and circulatory situation could be stabilized rapidly [11]. Therefore, in the case of a tension pneumothorax, it is vital to perform immediate that is usual preclinical relief. Implementing a thoracic drainage does not require special adjuvants. In their review, Waydhas and Sauerland classified the immediate relief of a tension pneumothorax with a high grade of recommendation [12]. Besides the tension pneumothorax, there is a range of other indications for placing a thoracic drainage preclinically. An aerodermectasia occurring in respirated patients for example represents an urgent indication. An aerodermectasia is evidence of intrapleural excess pressure, so that, in a respirated patient, a thoracic drainage has to be placed on an emergency basis [1, 13]. The prophylactical appliance of a thoracic drainage in an artificial respirated patient is recommended in the case of serial rib fractures because of the high risk of pneumothorax. Especially in the field of air rescue, interventions during the flight are difficult due to lack of space. Therefore, a bountiful indication of a thorax decompression is put up. The generally purely prophylactic application in multi-injured and artificially respirated patients is however controversial. The preclinical application in favor of a shorter patient-centered care time should be relinquished in awake and spontaneously breathing patients with stable respiratory parameters, even in the clinical case of a pneumothorax.
Excluding other causes, high ventilation pressures without clinical explanation constitute an urgent indication for the preclinical application of a thoracic drainage. [4]. Only for occult pneumothorax in patients not artificially respirated, the preclinical application of a thoracic drainage is not necessary if there is enough control on the side of the emergency doctor. Vitally stable patients neither benefit from the preclinical intubation nor from the prophylactic application of a thoracic drainage. Of course, respiratory function and cardiovascular parameters must be monitored closely.
Access route
Only two of 48 placed thoracic drainages were placed ventrally. This tendency to the lateral approach is reflected in newer articles. In 1995, Baldt et al. already showed in 70% of cases the preference for the lateral approach, and Waksman showed in 1999 that out of 43 placed drainages, 42 were placed laterally [14]. The opinions on which access route offers more advantages are very heterogeneous. British Thoracic Surgeons [15] seem to prefer an apical positioning according to Monaldi, while in compliance with the ATLS® guidelines, the lateral access route is given preference. In the teaching manual under the section of skills, the so-called “Triangle of Safety” is defined as a secure access area [16].
The main arguments for the lateral access route are less risk of bleeding, less muscle and soft tissue damage, and a greater acceptance by the patient at cosmetically less disturbing cicatrice.
The main argument for the ventral approach is that, in a supine patient, air accumulates especially ventrally in the pleural cavity and is easier and more efficient to drain through the ventral entry [17, 18].
The complications with the lateral access are rather intra-abdominal malpositions, in part also with organ injuries. Especially in cases of high speed traumas, there is a possibility of diaphragmatic rupture which more frequently on the left side can also lead to a shift of intra-abdominal organs.
The access according to Monaldi poses mainly the danger of injury to the mediastinal vessels or also the heart due to the anatomical location.
For both the ventral and lateral access way, there are described extensive complications not only when laying the patient but also during the course, i.e., malposition or subcutaneous emphysema abscess formation [7, 19]. The main complication here is the misplacement of a drainage. Numerous studies have shown that misplacements of thoracic drainages are accompanied by an increased risk for persistent pneumothorax and hematothorax as well as late complications such as abscesses and empyema [9, 20]. Even the possibility of developing a tension pneumothorax through a misplaced drainage is described [21].
Malpositions
Stark et al. were able to show that patients with an insufficient drainage have longer stays in hospital. Given the results, the question whether priority should be given to a preclinical thoracic drainage system contrary to a clinical one is of vital importance. In no case should an urgent life-threatening state be overlooked nor out of false ambition a complete preclinical care tried to be provided, because applying a thoracic drainage has undoubtedly better circumstances within the clinical situation. The frequently studied differentiation of the various access routes ventral/lateral is of less interest. However, there are numerous studies on the topic of thoracic drainages which neglect trauma patients or do not go into a preclinical placed system. In addition, the radiological malpositions are often tested only in conventional X-ray, and therefore, the position of the drainage tip is not broken down further. In 1995, Baldt et al. reported 26% malpositions in a total of 77 placed drainages at the scene of the accident. As a suitable diagnostic method, a thoracic CT is mentioned. In addition, it was shown that lateral drainages show malpositions more frequently than ventral ones [9]. David et al. [23] describe five malpositions in 44 thoracic drainages, placed at the scene of accident. One drainage was even positioned extrathoracically in the liver parenchyma. However, the review of the drainage facility only took place partly with X-rays. Malpositions of thoracic drainages placed in the hospital are also being investigated. Mirvis et al. reported 15% malpositions in polytrauma patients [22].
Considering this, the position of preclinical placed thoracic drainages is the main focus of this study. As a by-product, differences between ventral and lateral access route should be looked into regarding the rate of misplacements. However, probably due to the ATLS® training, a ventral access route was used only twice.
Study collective
The sociodemographic characteristics can be compared well with other studies. The proportion of male patients among the traumatized patients with severe thoracic trauma is considerably higher than the proportion of female patients. Deneuville predominantly found 86% to be male patients. Barton also saw this gender coherence, and Duponselle even investigated only male victims. Even in nontraumatic caused pneumothoraces, a predominant proportion of 4 : 1 of male to female patients is reported. In total, there is a strong preference for the lateral approach.
Operating conditions
All evaluated drainages in this study were placed by the emergency doctor of the rescue helicopter Christoph 20 under emergency conditions. In this respect, the study differs largely from the literature. On the one hand, this is because doctor-staffed emergency resources occur mainly in the European language area, and therefore, often, only preclinical interventions can be performed. In the Anglo-American language area, the preclinical treatment is influenced mainly by so-called paramedics, not medical personnel. On an emergency basis, nonmedical rescue workers prefer the needle decompression. Thoracic drainages are usually only placed under so-called “save conditions” in hospital. Many other studies on thoracic drainages also incorporate nontraumatic, so-called spontaneous pneumothoraces. Here, the thoracic drainages are generally placed in hospital after safe diagnosis under optimal conditions. This means that the patient can be prepared and placed optimally. There is no time pressure, and usually, there are enough helpers available.
Limitations paragraph
Despite 4 years of data collection, the weakness of this study is the low case number. Therefore, in the results section, the study disclaims analysis of significance. It is very difficult gaining comparable data in the field of preclinical patient care. Often, the documentation is sketchy and only rudimentary. A validation of the preclinical invasive activities carried out is not the rule, be it even only placing a permanent venous catheter. We have, therefore, decided to examine data from the air rescue, because on the one hand, only here, there are a limited number of emergency doctors, and on the other, there exists a largely complete documentation in the “LIKS” (air rescue, information, and communication system) by the German AA. This documentation system has been developed continually every year since 1994 on basis of Lotus Notes and has to be filled in obligatory on every operation. With regard to the position control of the thoracic drainage, only cases until 2006 could be considered, as from then on, the CT trauma scan was carried out as a standard at Klinikum Bayreuth Hospital in line with the polytraumatic algorithm.
Conclusions
Even if the results are comparable with the numerous studies cited here, for statistically meaningful results, a higher number of cases should be observed. In order to increase the validity of the data in line with a further study and simultaneously take as basis the rate of malpositions of thoracic drainages from this study, one would have to study at least 200 placed thoracic drainages. All patients of all rescue helicopter stations would have to be included in a corresponding study. However, the difficulty then is the further documentation of the destination hospital, as preliminary studies of our study showed a large documentation or diagnostic deficit in the resuscitation room management. It was very difficult finding complete older records. Another limitation of our study is the large number of participating doctors. Currently, 20 emergency doctors from the Surgical Clinic occupy the Christoph 20, however, with heterogeneous education level. All physicians have the proof of expertise in emergency medicine and at least 3 years of experience in ground-based emergency ambulance service. Nevertheless, for example, surgeons experienced in thoracic surgery as well as anesthesia assistant doctors take part. For this reason, the assumption is allowed that a certain differing level of training influences the quality and any complications. It is, therefore, imperative that all emergency physicians ask themselves whether they have sufficient knowledge specifically in the technique of “placing drainages” and if they perceive a deficit if necessary to take part in training for preclinical skills. Although the transport time in Germany from the scene of accident to a hospital usually should not exceed 15 min, placing a thoracic drainage during this time of preclinical care can be lifesaving.
Looking at the subpopulation of drainage malposition shows that there existed apparently more serious injuries (Table VI). Both the NACA score and the GCS point to more serious injuries. The higher intubation rate also seems to be an indication for this. In purely statistical terms, reviewing the medical records showed a shortened hospital stay. However, this can be explained due to the small number of cases and the fact that this subpopulation included the more severely injured victims, some of whom died in the emergency department. From a purely descriptive view, the records showed no reference to complications from malposition because it was usually corrected within the first hour at the hospital. The omission of a subscripted preclinical thoracic drainage system certainly represented a bigger loss with more far-reaching consequences than the malposition.
Table VI.
Characteristics of the subpopulation with drainage malposition
| Parameter | Average value |
|---|---|
| Age | 40.2 ± 20.5 years |
| Trauma mechanism | 100% blunt trauma |
| NACA | 4.6 ± 0.3 |
| Preclinical intubation rate | 88.8% |
| GCS at scene of accident | 7.3 ± 3.9 |
| Mortality | 37.5% |
| Hospital days | 25.1 ± 19.2 |
Funding Statement
Funding sources: None.
Footnotes
Conflict of interest: None.
Contributor Information
Rupert Schupfner, Klinikum Bayreuth, Bayreuth, Germany.
Walter Wagner, Klinikum Bayreuth, Bayreuth, Germany.
Angelika Schneller, Klinikum Bayreuth, Bayreuth, Germany.
References
- 1.Aul A, Klose R. Präklinische Thoraxdrainage – Indikationen und Technik. Notf Rettungsmed. 2005;8:49–56. doi: 10.1007/s00101-004-0766-1. [DOI] [PubMed] [Google Scholar]
- 2.Schlechtriemen T, Schaefer S, Stolpe E, Altemeyer KH. [Preclinical care of trauma patients in air rescue. Results of the medical quality management for patients with severe head injury and polytrauma in the years 2000 and 2001] Unfallchirurg. 2002 Nov;105(11):974–985. doi: 10.1007/s00113-002-0515-3. [DOI] [PubMed] [Google Scholar]
- 3.Aufmkolk M, Ruchholtz S, Hering M, Waydhas C, Nast-Kolb D. [The value of subjective estimation of the severity of thoracic injuries by the emergency surgeon] Unfallchirurg. 2003 Sep;106(9):746–753. doi: 10.1007/s00113-003-0640-7. [DOI] [PubMed] [Google Scholar]
- 4.Bardenheuer M, Obertacke U, Waydhas C, Nast-Kolb D. [Epidemiology of the severely injured patient. A prospective assessment of preclinical and clinical management. AG Polytrauma of DGU] Unfallchirurg. 2000 May;103(5):355–363. doi: 10.1007/s001130050550. [DOI] [PubMed] [Google Scholar]
- 5.Demartines N, Kiener A, Scheidegger D, Harder F. [Thoracic drainage at the accident site] Helv Chir Acta. 1990 Oct;57(2):273–277. [PubMed] [Google Scholar]
- 6.Di Bartolomeo S, Sanson G, Nardi G, Scian F, Michelutto V, Lattuada L. A population-based study on pneumothorax in severely traumatized patients. J Trauma. 2001 Oct;51(4):677–682. doi: 10.1097/00005373-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Gaillard M, Hervé C, Mandin L, Raynaud P. Mortality prognostic factors in chest injury. J Trauma. 1990 Jan;30(1):93–96. doi: 10.1097/00005373-199001000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Waydhas C, Sauerland S. Thoraxtrauma und Thoraxdrainage: Diagnostik und Therapie – Ein systematisches Review. Notf Rettungsmed. 2003;6:627–639. [Google Scholar]
- 9.Baldt MM, Bankier AA, Germann PS, Pöschl GP, Skrbensky GT, Herold CJ. Complications after emergency tube thoracostomy: assessment with CT. Radiology. 1995 May;195(2):539–543. doi: 10.1148/radiology.195.2.7724780. [DOI] [PubMed] [Google Scholar]
- 10.Cameron EW, Mirvis SE, Shanmuganathan K, White CS, Miller BH. Computed tomography of malpositioned thoracostomy drains: a pictorial essay. Clin Radiol. 1997 Mar;52(3):187–193. doi: 10.1016/s0009-9260(97)80271-1. [DOI] [PubMed] [Google Scholar]
- 11.Barton ED. Tension pneumothorax. Curr Opin Pulm Med. 1999 Jul;5(4):269–274. doi: 10.1097/00063198-199907000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Waydhas C, Sauerland S. Thoraxtrauma und Thoraxdrainage: Diagnostik und Therapie – Ein systematisches Review. Notf Rettungsmed. 2003;6:541–548. [Google Scholar]
- 13.Trupka A, Nast-Kolb D, Schweiberer L. Blunt chest trauma. [Thoracic trauma] Unfallchirurg. 1998 Apr;101(4):244–258. doi: 10.1007/s001130050265. [DOI] [PubMed] [Google Scholar]
- 14.Waksman I, Bickel A, Szabo A, Weiss M, Eitan A. Use of endoscopic trocar-cannula for chest drain insertion in trauma patients and others. J Trauma. 1999 May;46(5):941–943. doi: 10.1097/00005373-199905000-00028. [DOI] [PubMed] [Google Scholar]
- 15.Tang A, Hooper T, Hasan R. A regional survey of chest drains: evidence-based practice? Postgrad Med J. 1999 Aug;75(886):471–474. doi: 10.1136/pgmj.75.886.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Surgeons. ATLS®, Advanced Trauma Life Support for Doctors. 8. Chicago, IL: American College of Surgeons; 2008. [Google Scholar]
- 17.Laws D, Neville E, Duffy J. BTS guidelines for the insertion of a chest drain. Thorax. 2003 May;58(Suppl 2):ii53–ii59. doi: 10.1136/thorax.58.suppl_2.ii53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomlinson MA, Treasure T. Insertion of a chest drain: how to do it. Br J Hosp Med. 1997 Sep-30;58(6):248–252. [PubMed] [Google Scholar]
- 19.Hyde J, Sykes T, Graham T. Reducing morbidity from chest drains. BMJ. 1997 Mar 29;314(7085):914–915. doi: 10.1136/bmj.314.7085.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stark DD, Federle MP, Goodman PC. CT and radiographic assessment of tube thoracostomy. AJR Am J Roentgenol. 1983 Aug;141(2):253–258. doi: 10.2214/ajr.141.2.253. [DOI] [PubMed] [Google Scholar]
- 21.Lim KE, Tai SC, Chan CY, Hsu YY, Hsu WC, Lin BC, Lee KT. Diagnosis of malpositioned chest tubes after emergency tube thoracostomy: is computed tomography more accurate than chest radiograph? Clin Imaging. 2005 Nov-Dec;29(6):401–405. doi: 10.1016/j.clinimag.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 22.Mirvis SE, Tobin KD, Kostrubiak I, Belzberg H. Thoracic CT in detecting occult disease in critically ill patients. AJR Am J Roentgenol. 1987 Apr;148(4):685–689. doi: 10.2214/ajr.148.4.685. [DOI] [PubMed] [Google Scholar]
- 23.David A, Eitenmüller J, Muhr G. Präklinische Versorgung von Thoraxverletzungen – Möglichkeiten und Grenzen. Hefte Unfallheilkunde. 1992:223–224. [Google Scholar]
- 24.Kshettry VR, Bolman RM., 3rd Chest trauma. Assessment, diagnosis, and management. Clin Chest Med. 1994 Mar;15(1):137–146. [PubMed] [Google Scholar]