Abstract
Background
Child maltreatment is a potent risk factor for psychopathology. Although the developmental timing of first exposure to maltreatment is considered important in shaping risk of future psychopathology, no consensus exists on whether earlier or later exposures are more deleterious. This study examines whether age at first exposure to abuse is associated with subsequent depression and suicidal ideation.
Methods
Data were drawn from the National Longitudinal Study on Adolescent Health (n=15,701). Timing of first maltreatment exposure was classified using: (1) a crude measure capturing early childhood (0–5), middle childhood (6–10), or adolescence (11–17); and (2) a refined measure capturing infancy (0–2), preschool (3–5), latency (6–8), prepubertal (9–10), pubertal (11–13), or adolescence (14–17). We examined whether timing of first exposure was associated with depression and suicidal ideation in early adulthood in the entire sample and among those exposed to maltreatment.
Results
Respondents exposed to physical abuse at any age had a higher odds of depression and suicidal ideation in young adulthood than non-maltreated respondents. Among maltreated respondents, exposure during early childhood (0–5), particularly pre-school (3–5), was most strongly associated with depression. Respondents first exposed to physical abuse during preschool had a 77% increase in the odds of depression and those first exposed to sexual abuse during early childhood had a 146% increase in the odds of suicidal ideation compared to respondents maltreated as adolescents.
Conclusions
Developmental timing of first exposure to maltreatment influences risk for depression and suicidal ideation. Whether these findings are evidence for biologically-based sensitive periods requires further study.
Keywords: developmental timing, sensitive period, child maltreatment, depression, suicidal
Introduction
Depression and suicidality (i.e., suicidal ideation, suicide attempts) are serious public health problems among youth, currently estimated in cross-sectional studies to affect 11.7% (Merikangas et al., 2011) and 14.5% of adolescents, respectively 1. Exposure to childhood adversity, particularly physical and sexual abuse, is a potent risk factor for all types of psychopathology across the lifespan, including depression and suicidality 2; 3. These findings are concerning given that more than a third of adults in the United States report having been exposed to physical or sexual abuse as children 4.
The developmental timing of exposure to child maltreatment is considered an important dimension of the maltreatment experience that may be related to subsequent psychopathology risk 5; 6. However, there is little consensus on whether earlier or later exposure is associated with worse outcomes. On one hand, early maltreatment might be more deleterious than later maltreatment because it can compromise a child’s ability to successfully master stage-salient developmental tasks (e.g., self-regulation, secure attachments); failure to meet earlier developmental milestones can, in turn, interfere with the child’s ability to successfully accomplish future developmental tasks, consistent with developmental psychopathology theories 7. From the perspective of developmental neuroscience, early life adversities may also be more deleterious because they occur when the foundation of brain architecture and neurobiological systems involved in regulating arousal, emotion, stress responses, and reward processing are being wired. Exposure to maltreatment early in life can disrupt the development of neural circuits that interfere with typical patterns of brain development, heightening vulnerability to a host of mental health problems 8–11. On the other hand, later exposures, such as those occurring during adolescence, might be more harmful because adolescents have developed the cognitive skills to conceptualize experiences of abuse 12; 13. Moreover, physiological stress response systems undergo substantial change during adolescence (Stroud et al, 2009), potentially magnifying the detrimental impact of maltreatment on mental health.
Identification of age periods during which an exposure might be accompanied by heightened risk for subsequent adverse outcomes may help identify “sensitive periods” in development, or windows of time when the developing brain is particularly sensitive to environmental influence 14; 15. Although the existence of sensitive periods has been established for the visual 16, and auditory systems 17, knowledge about the existence of sensitive periods for social and emotional development is limited. Identification of sensitive periods in child social and emotional development could have profound implications, yielding novel insights into developmentally-relevant biological pathways, and points in development during which interventions could be most efficacious in minimizing the effects of maltreatment and reducing children’s risk for psychopathology.
To date, few studies have examined the effect of developmental timing of exposure to maltreatment on the subsequent development of psychopathology. Existing studies have reported mixed findings regarding the age period associated with most harm. In two prospective studies, individuals with maltreatment prior to age 5 had higher levels of internalizing symptoms in childhood 18 and depressive symptoms in adulthood 19 compared to those exposed during later stages. However, others have found that exposure to maltreatment occurring in adolescence was associated more strongly with adolescent depressive symptoms than maltreatment prior to age 12 20. Another study found evidence that both early and late onsets were harmful, with childhood-limited maltreatment being significantly associated with higher levels of both depression and suicidality and adolescent maltreatment being associated with suicidality 21. Two studies found no effect of developmental timing of maltreatment in relation to internalizing symptoms 22; 23. Although these studies suggest that developmental timing of maltreatment exposure may matter for later risk of depression or suicidality, these studies are limited by a predominant focus on children prior to adolescence, a lack of attention to suicidality and potential gender differences, and reliance on small community-based samples.
We address these limitations by using data from a large nationally representative sample of young adults to examine whether there are developmental timing differences in the associations of child maltreatment with depression and suicidal ideation. We examined developmental timing differences, separately for physical and sexual abuse, using a relatively crude and a more refined measure of age at first abuse. We used these two coding schemes to evaluate whether greater insights could be gained by using a more nuanced approach. Based on extensive prior literature, we expected that respondents exposed to either physical or sexual abuse at any age would have higher risk for depression and suicidal ideation relative to those who were unexposed. We also hypothesized that respondents first exposed to maltreatment during the early childhood period would have higher risk for depression and suicidal ideation than those first exposed at later time points. Finally, because previous studies have shown that exposure to child maltreatment, depression, and suicidal ideation differ by gender 2; 24; 25, we tested for potential gender differences in these associations.
Methods
Sample and Procedures
Data came from the National Longitudinal Study of Adolescent Health (Add Health), a nationally representative longitudinal survey of adolescents and young adults. Add Health recruited a school-based sample of adolescents in grades 7 through 12 in 1994 and has followed respondents into young adulthood. To date, there have been 4 waves of data collection. This study used data from the Wave 1, 3 and 4 interviews. Wave 1 (1994–1995) utilized a multi-stage sampling design to enroll adolescents. A systematic random sample of high schools along with feeder schools (i.e., middle schools whose students matriculate at the selected high school) was selected. A total of 134 schools (79%) participated. An in-school survey was completed by 90,118 students, and 20,745 students participated in a more detailed in-home interview (75.6% and 79.5% of eligible students, respectively). Wave 3 (2001–2002) interviewed 15,197 in-home Wave 1 respondents (aged 18–26), and Wave 4 (2008–2009) follow-up interviews were completed with 15,701 of these respondents (aged 24–32; 77.4% and 80.3% of eligible respondents, respectively). Additional information about the sample and sampling procedures is available elsewhere 26.
Measures
Predictors: Exposure to Physical and Sexual Abuse
At Wave 4, respondents completed items assessing exposure to physical and sexual abuse. Physical abuse was ascertained by the question: “Before your 18th birthday, how often did a parent or adult caregiver hit you with a fist, kick you, or throw you down on the floor, into a wall, or down stairs?” Sexual abuse was ascertained with the item: “How often did a parent or other adult caregiver touch you in a sexual way, force you to touch him or her in a sexual way, or force you to have sexual relations?” For both questions, respondents reported how old they were the first time the event happened. We created two different coding schemes for exposure timing, consistent with prior research 19. The first was a crude, three category variable denoting first exposure during early childhood (0–5), middle childhood (6–10), or adolescence (11–17). The second was a refined six category variable denoting first exposure during infancy (0–2), preschool (3–5), latency (6–8), prepubertal (9–10), pubertal (11–13), or adolescence (14–17).
Psychopathology
We examined the association of child maltreatment with Wave 3 depression and suicidal ideation. Although these outcomes were assessed in prior waves, we focused on responses from Wave 3 because this was the first wave when all respondents in the sample were older than age 17 and therefore outside the exposure time period.
Depression
Depression was measured using a 9-item version of the Center for Epidemiological Studies of Depression Scale (CES-D) 27. Respondents indicated the frequency of depressive symptoms in the past week on a scale ranging from “never or rarely” to “most/all of the time.” The scale has sound psychometric properties 27; 28. The short form of the CES-D used in the Add Health survey has demonstrated adequate reliability (Cronbach’s alpha=0.79) and has been utilized in numerous studies examining the correlates and consequences of adolescent depression 29; 30. A total score for each respondent was calculated. To facilitate interpretation, and address the skew towards lower values in the sample, we dichotomized responses into the top quartile (depressed), which corresponded to a score of 7 or higher on the total score, and bottom three quartiles (not depressed). Previous studies have used comparable thresholds to define depression 31.
Suicidal ideation
Suicidal ideation was measured with the item: “During the past 12 months, have you ever seriously thought about committing suicide.” This item was taken from the Youth Risk Behavior Surveillance system and has been shown to have good test-retest reliability 32 as well as convergent and discriminant validity 33.
Covariates
All models contained controls for sex, age (continuous), parental education (highest level attained by either mother or father; 1=less than high school; 2=GED or high school diploma; 3=business, trade, or vocational school post-high school; 4=some college; 5=college; 6=more than college; 7=missing) and parental occupation (1=professional/manager; 2=technical, officer worker, or sales; 3=industry, construction, transportation, or military; 4=missing) as measures of socioeconomic status, and self-reported race/ethnicity (1=white; 2=black; 3=Asian; 4=Hispanic; 5=native American; 6=other; 7=multi-racial). All of these covariates were taken from the Wave 1 interview.
Data Analyses
We fit a series of logistic regression models that examined the associations between timing of first maltreatment exposure and both depression and suicidal ideation using our crude and refined measures. We conducted these analyses first in the total sample (with respondents who never experienced maltreatment as the referent) and in the sample of respondents exposed to maltreatment (where first onset of exposure in adolescence was the referent). We used survey procedures in SAS 9.2 to adjust for survey design, sample weights, and non-response. We tested for multiplicative interactions between gender and both physical and sexual abuse in predicting depression and suicidal ideation in the total sample.
Results
Table 1 presents descriptive statistics on the total analytic sample and the respondents who reported high levels of depressive symptoms and suicidal ideation. In Add Health, 24.49% of respondents experienced depressive symptoms exceeding the cut-point and 6.61% reported past-year suicidal ideation. Additionally, 17.43% reported having been exposed to physical abuse and 4.84% to sexual abuse by age 17 (Figure 1). A total of 19.83% experienced at least one of these exposures and 2.36% experienced both. The mean age at first onset of exposure to physical abuse (mean=10.68; se=0.12) was older than the mean age at first onset of exposure to sexual abuse (mean=8.07; se=0.21). In the models described below, no statistically significant interactions between gender and physical or sexual abuse emerged, using either the crude or refined categories or the total sample or exposed-only sample. Therefore, we present results for males and females combined.
Table 1.
Demographic characteristics of the National Longitudinal Study of Adolescent Health (AddHealth) analytic sample
| Age (continuous) | Total Sample (n=14,322) | High Depressive Symptoms (n=3,686) | High Suicidal Ideation (n=845) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| M | SD | M | SD | M | SD | |
|
| ||||||
| 15.95 | 0.12 | 15.90 | 0.13 | 15.60 | 0.16 | |
|
| ||||||
| % | n | % | n | % | n | |
|
| ||||||
| Sex | ||||||
| Female | 49.15 | 7555 | 55.50 | 2187 | 51.86 | 464 |
| Male | 50.85 | 6767 | 44.49 | 1499 | 48.14 | 381 |
| Race/Ethnicity | ||||||
| White, non Hispanic | 65.09 | 7436 | 57.36 | 1637 | 70.26 | 489 |
| Black, non Hispanic | 15.07 | 2844 | 18.17 | 828 | 8.83 | 120 |
| Asian | 3.36 | 965 | 4.67 | 322 | 2.78 | 53 |
| Hispanic/Latino | 10.93 | 2139 | 13.26 | 625 | 10.69 | 117 |
| Native American | 0.47 | 79 | 0.75 | 25 | 1.17 | 13 |
| Other | 0.75 | 108 | 0.84 | 27 | 0.64 | 5 |
| Multi-Racial | 4.35 | 751 | 4.95 | 222 | 5.64 | 48 |
| Parent Education | ||||||
| Less than high school | 10.85 | 1632 | 15.32 | 546 | 9.69 | 80 |
| High school diploma/GED | 30.28 | 4028 | 31.81 | 1081 | 35.47 | 220 |
| Business/trade/vocational post-high school | 6.97 | 932 | 7.68 | 246 | 9.09 | 62 |
| Some college | 13.04 | 1914 | 10.79 | 462 | 13.77 | 120 |
| College Graduate | 21.84 | 3246 | 18.84 | 748 | 23.18 | 188 |
| More than college | 10.85 | 1765 | 7.93 | 345 | 12.25 | 124 |
| Missing | 6.18 | 805 | 7.62 | 258 | 6.56 | 51 |
| Parent Occupation | ||||||
| Service industry/construction/transportation/military | 35.07 | 4904 | 40.45 | 1414 | 35.60 | 293 |
| Technical/office worker/sales | 24.81 | 3437 | 22.49 | 845 | 24.73 | 200 |
| Professional/Manager | 31.80 | 4795 | 26.40 | 1044 | 32.35 | 282 |
| Missing | 8.32 | 1186 | 10.67 | 383 | 7.32 | 70 |
| Exposure to Physical Abuse | ||||||
| Unexposed | 83.55 | 9976 | 77.63 | 2344 | 70.07 | 505 |
| Infancy (0–2) | 0.56 | 55 | 0.53 | 17 | 1.06 | 6 |
| Preschool (3–5) | 2.22 | 288 | 3.68 | 107 | 4.80 | 47 |
| Latency (6–8) | 2.97 | 368 | 4.10 | 127 | 4.61 | 30 |
| Pre-pubertal (9–10) | 1.74 | 247 | 2.52 | 83 | 2.89 | 24 |
| Pubertal (11–13) | 3.54 | 404 | 5.02 | 135 | 6.85 | 46 |
| Adolescent (14–17) | 5.42 | 668 | 6.53 | 221 | 9.71 | 70 |
| Exposure to Sexual Abuse | ||||||
| Unexposed | 95.29 | 11578 | 92.48 | 2861 | 90.60 | 671 |
| Infancy (0–2) | 0.33 | 37 | 0.60 | 17 | 1.30 | 8 |
| Preschool (3–5) | 1.28 | 153 | 1.97 | 59 | 3.83 | 28 |
| Latency (6–8) | 1.11 | 146 | 1.99 | 59 | 1.42 | 13 |
| Pre-pubertal (9–10) | 0.62 | 74 | 0.63 | 21 | 0.80 | 5 |
| Pubertal (11–13) | 0.72 | 91 | 1.28 | 40 | 1.36 | 11 |
| Adolescent (14–17) | 0.65 | 81 | 1.07 | 31 | 0.70 | 6 |
Percents include adjustments for clustering and sampling weights; N’s reflect unweighted data.
Columns may not sum to total sample size or 100% due to missing data or rounding.
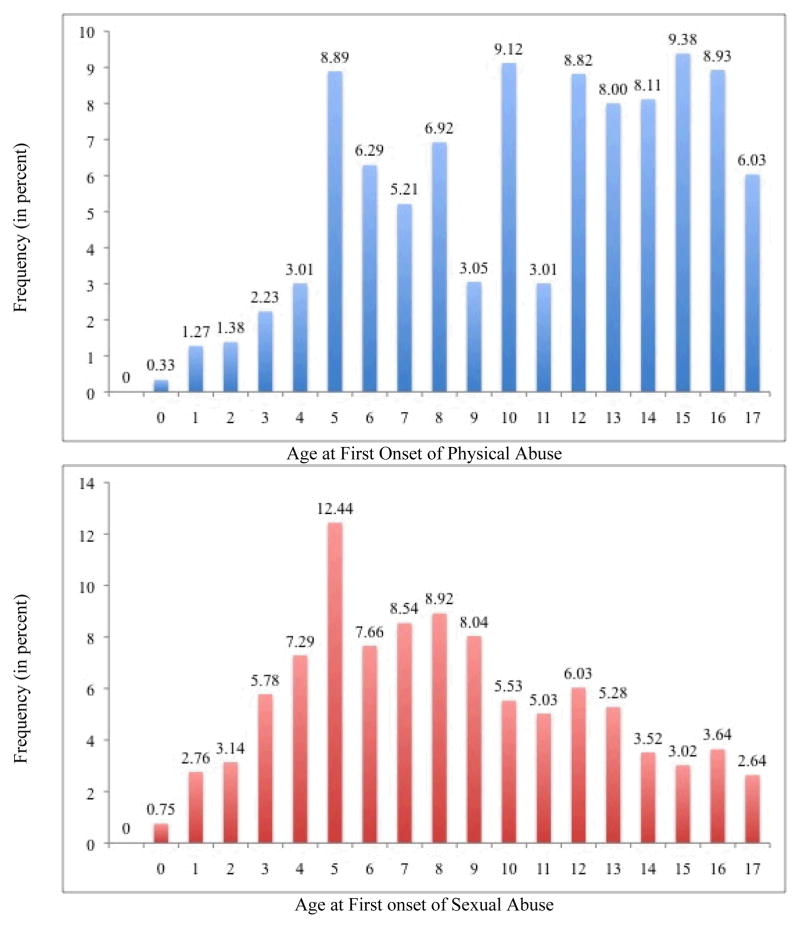
Figure 1.
Distribution of age at first onset of exposure to physical and sexual abuse in AddHealth
With respect to physical abuse, 3.38% were exposed during infancy (age 0–2), 13.5% during preschool (age 3–5), 18.05% during latency (age 6–8), 10.60% during the pre-pubertal period (age 9–10), 21.52% during the pubertal period, and 32.94% during the adolescent period (age 14–17). With respect to sexual abuse, 6.97% were exposed during infancy, 27.11% during preschool, 23.59% during latency, 13.17 during pre-pubertal period, 15.31% during the pubertal period, and 13.86% during the adolescent period.
Child Maltreatment, Depression, and Suicidal ideation
Respondents who reported exposure to child maltreatment at any age had higher odds of subsequent depression and suicidal ideation than non-maltreated respondents. Respondents exposed to physical abuse had 1.62 times the odds of experiencing depression (p<0.0001) and 2.41 times the odds of having suicidal ideation (p<0.0001) compared to unexposed respondents. Those exposed to sexual abuse had 1.77 times the odds of experiencing depression (p<0.0001) and 2.31 times the odds of having suicidal ideation (p<0.0001) when compared to non-maltreated respondents.
Developmental Timing of Exposure to Adversity, Depression, and Suicidal ideation in Total Sample
Age at onset of exposure to child maltreatment (both crude and refined), influenced the association between maltreatment and depression, and suicidal ideation (Table 2). Compared to unexposed respondents, those exposed to physical or sexual abuse had higher odds of experiencing depression, regardless of the age of exposure, in the crude analysis (odds ratios range from 1.47 to 1.90). However, in the refined analysis, there were some exceptions: respondents first exposed to physical abuse during the infancy period (OR=1.04; p=0.9317) or sexual abuse during the pre-pubertal period (OR=0.92; p=0.8220) were no more likely to develop depression than the unexposed group. The largest increase in odds of depression was observed for first exposure to physical abuse during the pre-school period (OR=2.28; p<0.0001) and first exposure to sexual abuse during the infancy period (OR=2.73; p=0.0175).
Table 2.
Adjusted association between age at onset of child maltreatment and subsequent depression and suicidal ideation in the total sample
| Depression | Suicidal Ideation | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
|
| ||||||
| Physical Abuse | ||||||
| Unexposed | ref | ref | ref | ref | ref | ref |
| Crude abuse age at onset | ||||||
| Early childhood (0–5) | 1.99 | <0.0001 | 1.43, 2.76 | 2.76 | <0.0001 | 1.68, 4.52 |
| Middle childhood (6–10) | 1.73 | <0.0001 | 1.36, 2.19 | 2.11 | 0.0004 | 1.40, 3.19 |
| Adolescence (11–17) | 1.47 | <0.0001 | 1.21, 1.78 | 2.46 | <0.0001 | 1.82. 3.33 |
| Refined abuse age at onset | ||||||
| Infancy (0–2) | 1.04 | 0.9317 | 0.41, 2.64 | 2.58 | 0.0854 | 0.88, 7.57 |
| Preschool (3–5) | 2.28 | <0.0001 | 1.63, 3.21 | 2.80 | <0.0001 | 1.73, 4.56 |
| Latency (6–8) | 1.71 | 0.0008 | 1.25. 2.33 | 2.02 | 0.0110 | 1.18, 3.46 |
| Pre-pubertal (9–10) | 1.77 | 0.0045 | 1.19, 2.62 | 2.28 | 0.0052 | 1.28, 4.05 |
| Pubertal (11–13) | 1.69 | 0.0003 | 1.27, 2.24 | 2.62 | <0.0001 | 1.78, 3.86 |
| Adolescent (14–17) | 1.33 | 0.0208 | 1.05, 1.70 | 2.36 | <0.0001 | 1.62, 3.42 |
| Sexual Abuse | ||||||
| Unexposed | ref | ref | ref | ref | ref | ref |
| Crude abuse age at onset | ||||||
| Early childhood (0–5) | 1.90 | 0.0022 | 1.26, 2.87 | 3.94 | <0.0001 | 2.21, 7.04 |
| Middle childhood (6–10) | 1.60 | 0.0149 | 1.10, 2.33 | 1.48 | 0.2825 | 0.73, 3.01 |
| Adolescence (11–17) | 1.96 | 0.0007 | 1.33. 2.90 | 1.69 | 0.1294 | 0.86. 3.35 |
| Refined abuse age at onset | ||||||
| Infancy (0–2) | 2.73 | 0.0175 | 1.19, 6.27 | 5.17 | 0.0032 | 1.74, 15.40 |
| Preschool (3–5) | 1.73 | 0.0187 | 1.10, 2.74 | 3.64 | <.0001 | 1.96, 6.78 |
| Latency (6–8) | 2.09 | 0.0017 | 1.32, 3.31 | 1.51 | 0.3172 | 0.67, 3.37 |
| Pre-pubertal (9–10) | 0.92 | 0.8220 | 0.44. 1.91 | 1.42 | 0.5078 | 0.50, 4.06 |
| Pubertal (11–13) | 2.06 | 0.0104 | 1.19, 3.57 | 2.04 | 0.1220 | 0.83, 5.01 |
| Adolescent (14–17) | 1.85 | 0.0358 | 1.04, 3.30 | 1.28 | 0.6572 | 0.43, 3.76 |
Cell entries are adjusted exponentiated beta coefficients (OR), p-values, and 95% confidence intervals.
For suicidal ideation, exposure to physical abuse was associated with elevated odds in all time periods except infancy, whether age at onset was coded as crude or refined. The largest increase in odds was found for first exposure to physical abuse during preschool (OR=2.80; p<0.0001). For sexual abuse, only early childhood exposures (OR=3.94; p<0.0001), including exposure during infancy (OR=5.17; p=0.0032) or the preschool period (OR=3.64; p<0.0001) were significantly associated with suicidal ideation.
Developmental Timing of Exposure to Adversity, Depression, and Suicidal ideation in Maltreated Respondents
Among the sample of respondents with a maltreatment history, age at onset of maltreatment exposure was associated with some measures of subsequent psychopathology but not others (Table 3). First exposure to physical abuse during the preschool period was associated with an elevated odds of depression when compared to first exposure during the adolescent period (OR=1.77; p=0.0042). For the crude age at exposure onset, there was a trend for early childhood exposure to be associated with increased odds of depression (OR=1.40; p=0.0709). No significant differences were found for depression across age-at-exposure groups for sexual abuse.
Table 3.
Adjusted association between age at onset of child maltreatment and subsequent depression and suicidal ideation among exposed group
| Depression | Suicidal Ideation | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
|
| ||||||
| Physical Abuse | ||||||
| Crude abuse age at onset | ||||||
| Early childhood (0–5) | 1.40 | 0.0709 | 0.97, 2.00 | 1.16 | 0.5956 | 0.67, 2.02 |
| Middle childhood (6–10) | 1.22 | 0.2029 | 0.90, 1.65 | 0.86 | 0.5303 | 0.54, 1.37 |
| Adolescence (11–17) | ref | ref | ref | ref | ref | ref |
| Refined abuse age at onset | ||||||
| Infancy (0–2) | 0.82 | 0.687 | 0.30, 2.20 | 1.20 | 0.7576 | 0.38, 3.78 |
| Preschool (3–5) | 1.77 | 0.0042 | 1.20, 2.62 | 1.23 | 0.4964 | 0.68, 2.24 |
| Latency (6–8) | 1.32 | 0.1862 | 0.87, 2.00 | 0.85 | 0.6115 | 0.46, 1.59 |
| Pre-pubertal (9–10) | 1.40 | 0.1714 | 0.87, 2.26 | 1.02 | 0.9660 | 0.49, 2.09 |
| Pubertal (11–13) | 1.28 | 0.1823 | 0.89, 1.85 | 1.14 | 0.5830 | 0.71, 1.84 |
| Adolescent (14–17) | ref | ref | ref | ref | ref | ref |
| Sexual Abuse | ||||||
| Crude abuse age at onset | ||||||
| Early childhood (0–5) | 1.00 | 0.9943 | 0.57, 1.75 | 2.46 | 0.0313 | 1.08, 5.59 |
| Middle childhood (6–10) | 0.87 | 0.6282 | 0.48, 1.55 | 0.92 | 0.8717 | 0.32, 2.62 |
| Adolescence (11–17) | ref | ref | ref | ref | ref | ref |
| Refined abuse age at onset | ||||||
| Infancy (0–2) | 1.32 | 0.5947 | 0.47, 3.72 | 3.91 | 0.1184 | 0.71, 21.70 |
| Preschool (3–5) | 1.04 | 0.9179 | 0.52, 2.09 | 3.20 | 0.0829 | 0.86, 11.92 |
| Latency (6–8) | 1.27 | 0.5355 | 0.60, 2.66 | 1.26 | 0.7496 | 0.30, 5.34 |
| Pre-pubertal (9–10) | 0.53 | 0.1674 | 0.22, 1.30 | 1.22 | 0.8049 | 0.25, 6.00 |
| Pubertal (11–13) | 1.18 | 0.6975 | 0.52, 2.64 | 1.68 | 0.4940 | 0.38, 7.35 |
| Adolescent (14–17) | ref | ref | ref | ref | ref | ref |
Cell entries adjusted exponentiated beta coefficients (OR), p-values, and 95% confidence intervals.
Considering suicidal ideation, no significant differences emerged across age-at-onset groups for physical abuse. However, respondents first exposed to sexual abuse during early childhood had increased odds of suicidal ideation (OR=2.46; p=0.0313), although the association was attenuated in the refined analysis.
As a final step, we evaluated models using alternative reference categories in the exposed-only analysis. Using the crude categorization, individuals first exposed to sexual abuse during early childhood had a higher odds of suicidal ideation relative to those first exposed during middle childhood (OR=2.69; p=0.0299). Using the refined categorization, individuals first exposed to sexual abuse during the pre-school (OR=1.94; p-value=0.10) and latency period (OR=2.37; p=0.0706) had higher odds of depression than those first exposed during the pre-pubertal period. Respondents first exposed to sexual abuse during the pre-school period had marginally elevated odds of suicidal ideation compared those first exposed during the latency period (OR=2.53; p=0.0682).
Discussion
Child maltreatment is among the most potent determinants of subsequent psychopathology, not only in children and adolescents, but also in adults 2; 3. Consistent with this prior work, we find that respondents exposed to physical and sexual abuse were more likely to have high levels of depression and to experience suicidal ideation in young adulthood relative to those with no maltreatment exposure. Importantly, our findings additionally suggest that the risk for future mental health problems among individuals exposed to maltreatment is shaped, in part, by the developmental timing of maltreatment exposure. Among those who experienced maltreatment, first exposure during the early childhood period (ages 0–5), particularly during pre-school (ages 3–5), was most deleterious. Specifically, respondents first exposed to physical abuse during preschool had a 77% increase in the odds of depression compared to those first maltreated as adolescents. Similarly, respondents first exposed to sexual abuse during early childhood had a 146% increase in the odds of suicidal ideation relative to those maltreated during adolescence. These findings are consistent with several previous studies showing that earlier onsets of maltreatment (prior to age 5) 18; 19; 21 are associated with depression, suicidal ideation, and other mental outcomes.
A more complicated story regarding developmental timing emerged for sexual abuse in our analyses comparing exposed respondents to unexposed respondents. Here, we found that child sexual abuse was associated with an elevated risk of depression across all age groups when using our crude measure. However, in the refined analysis we found no elevation in depression among those first maltreated during the pre-pubertal period (ages 9–10). Given the lower prevalence of sexual abuse than physical abuse, this finding may reflect insufficient power to detect differences in our refined analysis. Moreover, compared to unexposed respondents, first exposure to sexual abuse after the pre-school period was not associated with an elevated risk of suicidal ideation. One possibility is that a greater proportion of unwanted sexual experiences occurring later in development are perpetrated by peers, rather than family members or other adults, which could have implications for long-term impact on mental health. Collectively, findings for both physical and sexual abuse illustrate the importance of examining developmental timing using a refined approach, as collapsing into crude categories obscured important developmental differences.
We also did not identify any significant interactions between gender and exposure to either physical or sexual abuse. These results were somewhat surprising given that depression, in particular, is much more prevalent in females compared to males 24; 34. However, recent research has found that gender differences in depression are partly explained by females’ higher likelihood of experiencing interpersonal violence; it is not explained by females’ differential susceptibility to depression following exposure to violence 2.
Why might maltreatment during early childhood be so harmful? Several factors could explain these findings. It is well-known that child maltreatment impacts core developmental processes that are linked to psychopathology risk, including attachment, emotion regulation, stress response, executive functioning, and arousal see for example 35; 36. Although not well studied empirically, extant theory suggests that early childhood is the time when there is the greatest capacity to develop and refine these processes 37. Therefore, maltreatment occurring during the first five years of life could be more deleterious than maltreatment occurring later in life because it coincides with the window of vulnerability (or sensitive period) for typical developmental processes. Early childhood is also a period of rapid brain development, including synapse formation and pruning 37. According to stress neurobiology research, exposure to maltreatment at this stage has a greater potential to become literally wired into the brains of developing children 38; 39.
The finding that first onset of maltreatment during early childhood was associated with higher odds of depression and suicidal ideation in young adulthood has important implications for theory, practice, and policy. It extends current thinking regarding possible sensitive periods in social-emotional developmental processes by providing empirical data to support this knowledge-base and theory around sensitive periods. These findings also suggest that interventions and policies designed to protect children exposed to maltreatment from developing long-term mental health problems should be targeted as early in development as possible. This is a significant challenge, given that the highest rates of victimization are among younger children, with almost one third of the estimated 772,000 children in the United States with substantiated cases of child abuse or neglect were maltreated prior to age 4 40. Delivering psychosocial interventions to young children can be challenging, but evidence-based approaches for young children and their caregivers that both improve mental health outcomes and prevent future maltreatment incidents exist, including Parent Child Interaction Therapy 41 and Parent Infant Psychotherapy 42. Greater dissemination and implementation of these interventions may be one effective approach to reducing the long-term mental health consequences of child maltreatment at the societal level.
Several limitations should be considered in interpreting results of this study. First, our information about maltreatment experience is relatively limited in that these measures lack specific details about the characteristics of abuse (e.g., severity, chronicity, duration, and relationship of the perpetrator to the respondent). In particular, our measure of physical abuse does not include information about injuries caused by abuse (e.g., bruising, bleeding, and broken bones). Furthermore, our measure of sexual abuse combines different types of sexual abuse experiences that could vary in their degree of trauma (e.g., touching vs. forced rape). Moreover, although we found evidence that early maltreatments appears more deleterious than later maltreatment, earlier exposures may also be more chronic than later experiences. Future studies will need to incorporate detailed measures of multiple dimensions of the maltreatment experience so that the effects of developmental timing can be teased apart from other characteristics of the abuse. Second, our outcome measures were based on symptoms of depression during the past week and a single item of suicidal ideation, rather than a diagnostic interview or depression over a longer period of time. However, both measures have been widely used in epidemiological studies and have demonstrated good reliability and validity 27; 32; 33. Future research should examine timing of maltreatment in relation to mental disorder onsets and chronicity. Third, exposure to physical and sexual abuse was obtained retrospectively, which may provide a less reliable and valid measure than prospective reports as a result of memory issues or lack of willingness to disclose private matters. However, recent studies have found retrospective and prospective measures of maltreatment produce similar estimates of effect, including for depression 43. In addition, recalling age at first exposure may introduce recall bias and it is difficult to gauge the validity of reports occurring during infancy. Prospective research is needed to replicate these findings. Finally, we focused on two outcomes – depression and suicidal ideation – that are most likely distally related to exposure to maltreatment. While not a limitation per se, examination of more proximal processes, for example, brain structure and function, is needed to complement epidemiological studies and provide more conclusive evidence regarding the points in development when maltreatment is most likely to be deleterious. Moreover, inclusion of information regarding mental health services received following exposure to maltreatment is also important and should be included in future studies. This type of information could be important in helping to better disentangle the consequences of exposure to maltreatment and identify factors that could mitigate risk for future psychopathology.
Conclusion
Using data from a large nationally-representative sample, we find that early maltreatment is more strongly associated with risk for depression and suicidal ideation than maltreatment beginning at later developmental periods. These findings underscore the need to incorporate developmentally-specific measures of maltreatment exposure into future studies.
Acknowledgments
This work was supported by National Institute of Health grant K24MH094614 (JWS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
References
- 1.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Cheyen D, et al. Morbidity and Mortality Weekly: Surveillance Summaries. 2008. Youth Risk Behavior Surveillance - United States, 2007. [PubMed] [Google Scholar]
- 2.Dunn EC, Gilman SE, Slopen N, Willett JB, Molnar BE. The impact of exposure to interpersonal violence on gender differences in adolescent-onset major depression: Results from the National Comorbidity Survey Replication (NCS-R) Depression and Anxiety. 2012;29:392–399. doi: 10.1002/da.21916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication II: Associations with persistence of DSM-IV disorders. Archives of General Psychiatry. 2010;67(2):124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koenen KC, Roberts A, Stone D, Dunn EC. The epidemiology of early childhood trauma. In: Lanius R, Vermetten E, editors. The hidden epidemic: The impact of early life trauma on health and disease. New York, NY: Oxford University; 2010. pp. 13–24. [Google Scholar]
- 5.Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Child abuse, child development, and social policy. Norwood, NJ: Ablex; 1993. pp. 7–73. [Google Scholar]
- 6.English DJ, Graham JC, Litrownik AJ, Everson M, Bangdiwala SI. Defining maltreatment chronicity: Are there differences in child outcomes. Child Abuse and Neglect. 2005;29:575–595. doi: 10.1016/j.chiabu.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Cicchetti D, Toth SL. A developmental psychopathology perspective on child abuse and neglect. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:541–565. doi: 10.1097/00004583-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 8.McLaughlin KA, Fox NA, Zeanah CH, Nelson CA. Adverse rearing environments and neural development in children: The development of frontal electroencephalogram asymmetry. Biological Psychiatry. 2011;70:1008–1015. doi: 10.1016/j.biopsych.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fox SE, Levitt P, Nelson CA. How the timing and quality of early experiences influence the development of brain architecture. Child Development. 2010;81(1):28–40. doi: 10.1111/j.1467-8624.2009.01380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLaughlin KA, Fox NA, Zeanah CH, Sheridan MA, Marshall P, Nelson CA. Delayed maturation in brain electrical activity partially explains the association between early environmental deprivation and symptoms of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2010;68:329–336. doi: 10.1016/j.biopsych.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheridan MA, Fox NA, Zeanah CH, McLaughlin KA, Nelson CA. Variation in neural development as a result of exposure to institutionalization early in childhood. Proceedings of the National Academy of Science. 109(32):12927–12932. doi: 10.1073/pnas.1200041109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garbarino J. Troubled youth, troubled families: The dynamics of adolescent maltreatment. In: Cicchetti D, Carlson V, editors. Child maltreatment: theory and research on the causes and consequences of child abuse and neglect. New York, NY: Cambridge University Press; 1989. pp. 685–706. [Google Scholar]
- 13.Maccoby EE. Social-emotional development and response to stressors. In: Rutter M, Garmezy N, editors. Stress, coping, and development in children. New York, NY: McGraw-Hill; 1983. pp. 217–234. [Google Scholar]
- 14.Knudsen E. Sensitive periods in the development of the brain and behavior. Journal of Cognitive Neuroscience. 2004;16:1412–1425. doi: 10.1162/0898929042304796. [DOI] [PubMed] [Google Scholar]
- 15.Bailey DB, Bruer JT, Symons FJ, Lichtman JW, editors. Critical thinking about critical periods. Baltimore, MD: Paul H. Brookes Publishing Company; 2001. [Google Scholar]
- 16.Hensch TK. Critical period regulation. Annual Review of Neuroscience. 2004;27:549–579. doi: 10.1146/annurev.neuro.27.070203.144327. [DOI] [PubMed] [Google Scholar]
- 17.McMahon E, Wintermark P, Lahav A. Auditory brain development in premature infants: the importance of early experience. Annals of the New York Academy of Sciences. 2012;1252:17–24. doi: 10.1111/j.1749-6632.2012.06445.x. [DOI] [PubMed] [Google Scholar]
- 18.Keiley MK, Howe TR, Dodge KA, Bates JE, Pettit GS. The timing of child physical maltreatment: A cross-domain growth analysis of impact on adolescent externalizing and internalizing problems. Development and Psychopathology. 2001;13:891–912. [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116(1):176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- 20.Thornberry TP, Ireland TO, Smith CA. The importance of timing: The varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Development and Psychopathology. 2001;13:957–979. [PubMed] [Google Scholar]
- 21.Thornberry TP, Henry KL, Ireland TO, Smith CA. The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. Journal of Adolescent Health. 2010;46:359–365. doi: 10.1016/j.jadohealth.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jaffee SR, Maikovich-Fong AK. Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. Journal of Child Psychology and Psychiatry. 2011;52(2):184–194. doi: 10.1111/j.1469-7610.2010.02304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manly JT, Kim JE, Rogosch FA, Cicchetti D. Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology. 2001;13:759–782. [PubMed] [Google Scholar]
- 24.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KA. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10 year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–141. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 25.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. Journal of the American Medical Association. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 28.Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Fletcher JM. Child mistreatment and adolescent and young adult depression. Social Science and Medicine. 2009;68:799–806. doi: 10.1016/j.socscimed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Gerard JM, Buehler C. Cumulative environmental risk and youth maladjustment: The role of youth attributes. Child Development. 2004;75:1832–1849. doi: 10.1111/j.1467-8624.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 31.Primack BA, Swanier B, Georgiopoulos AM, Land SR, Fine MJ. Association between media use in adolescence and depression in young adulthood: A longitudinal study. Archives of General Psychiatry. 2009;66(2):181–188. doi: 10.1001/archgenpsychiatry.2008.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brener NC, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 Youth Risk Behavior Survey Questionnaire. Journal of Adolescent Health. 2002;31:336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 33.May A, Klonsky ED. Validity of suicidality items from the Youth Risk Behavior Survey in a high school sample. Assessment. 2010;18(3):379–381. doi: 10.1177/1073191110374285. [DOI] [PubMed] [Google Scholar]
- 34.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115(3):424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 35.Pollak SD, Vardi S, Putzer Bechner A, Curtin JJ. Physically abused children’s regulation of attention in response to hostility. Child Development. 2005;76(5):968–977. doi: 10.1111/j.1467-8624.2005.00890.x. [DOI] [PubMed] [Google Scholar]
- 36.McCrory E, DeBrito SA, Viding E. Research Review: The neurobiology and genetics of maltreatment and adversity. Journal of Child Psychology and Psychiatry. 2010;51(10):1079–1095. doi: 10.1111/j.1469-7610.2010.02271.x. [DOI] [PubMed] [Google Scholar]
- 37.Shonkoff JP, Phillips DA. From neurons to neighborhoods: The science of early childhood development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 38.DeBellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- 39.Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services, Administration on Children Youth and Families. Child Maltreatment 2008. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- 41.Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, Jackson S, Lensgraf J, Bonner BL. Parent-child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology. 2004;72(3):500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- 42.Lieberman AF, Van Horn P, Ippen CG. Toward evidence-based treatment: Child-parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(12):1241–1248. doi: 10.1097/01.chi.0000181047.59702.58. [DOI] [PubMed] [Google Scholar]
- 43.Scott KM, McLaughlin KA, Smith DAR, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: Comparison of prospective and retrospective findings. British Journal of Psychiatry. 2012;200:469–475. doi: 10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]