Abstract
Purpose
The purpose of this study was to evaluate glenoid labral heights before injury and after repair with 2 suture anchors: (1) traditional suture anchor secured with knots and (2) knotless suture anchor.
Methods
Ten matched pairs of human cadaveric glenoids were examined. In each specimen the labrum was detached from the 3-o’clock position to the 6:30 clock position on the anteroinferior glenoid, and labral repair was performed with either (1) traditional Bio-SutureTak suture anchors (n = 10) (Arthrex, Naples, FL) or (2) knotless PushLock suture anchors (n = 10, contralateral side) (Arthrex). By use of a 3-dimensional digitizer, the labral height, measured from the deepest point of the glenoid articular surface to the highest tip of the labrum, was measured in all specimens before injury and after repair at the 3:30, 4:30, and 5:30 clock positions. The degree of labral height increase was computed as a percent increase in labral height from before injury to after repair.
Results
Labral height increased significantly for all specimens from before injury (5.35 mm) to after repair (8.05 mm) (159.1% ± 13.7%, P < .0001). Increases in labral height from before injury to after repair were similar (P > .05) for Bio-SutureTak suture anchors (164.6% ± 18.7%, P < .0001) and PushLock suture anchors (153.6% ± 5.8%, P < .0001). The amount of labral height increase did not vary by anatomic location (157.0% ± 50.2%, 168.9% ± 51.0%, and 150.4% ± 35.2% at 3:30, 4:30, and 5:30, respectively; P = .46).
Conclusions
An increase in labral height can be achieved to create a significant height increase from before injury to after labral repair. The difference in labral height afforded by a traditional suture anchor and a knotless anchor is not statistically significant.
Clinical Relevance
Both traditional and knotless suture anchor constructs provide a reliable restoration of labral height in an acute Bankart model.
The glenoid labrum is a fibrocartilaginous rim attached to the periphery of the glenoid cavity and is a critical component in maintaining stability of the glenohumeral joint. The labrum functions to increase the height and surface area of the glenoid, thus enhancing the compression/concavity stabilizing function1 by centering the humeral head in the glenoid.2 A cadaveric study by Lazarus et al.,3 which created a Bankart lesion reducing the labral height by 80%, showed that the resultant stability of the glenohumeral joint was decreased by 60%. Furthermore, restoration of this labral height was paramount in restoring stability to the glenohumeral joint.3 Therefore the glenoid labrum becomes important in stabilization of the joint, acting as a restraint for humeral head translation within the glenoid cavity.
The “essential” lesion in an acute Bankart lesion is a tearing of the anterior-inferior labrum off of the glenoid resulting in laxity of the anterior inferior glenohumeral ligament (AIGHL).4,5 The surgical goal in an acute Bankart lesion is anatomic restoration of the labral complex to restore tension in the AIGHL and stability to the glenohumeral joint to prevent further dislocation or subluxation events.
Proper positioning of the labrum is necessary for successful arthroscopic treatment of instability. Most frequently, 1 of 2 types of anchors are used to facilitate this repair: traditional suture anchors secured with knots or knotless suture anchors. Many surgeons prefer using traditional suture anchors secured with knots because this technique facilitates anchor placement and optimal tensioning of the capsulolabral tissue. Both traditional and knotless suture anchors have been shown to provide a robust anchor construct that withstands cyclic mechanical loading in vitro.6
The objectives of this study are (1) to quantify the increase in labral height after repair with contemporary suture anchors and (2) to compare the labral heights after capsulolabral complex restoration with a traditional suture anchor secured with knots (3.0-mm Bio-SutureTak [BST]; Arthrex, Naples, FL) compared with knotless suture anchors (2.9-mm PushLock [PL]; Arthrex).
Because 1 goal of anterior labral repair is to increase the height of the labrum, we hypothesize that the labrum height will increase from before repair to after repair with either suture anchor construct. In addition, we hypothesize that there is no difference in the resulting repair height of the labrum using either PL or BST anchors.
METHODS
In this study 10 matched pairs (mean age, 63 ± 12 years; 5 male and 5 female) of cadaveric shoulders (scapula with glenoid) were dissected and potted to allow consistent alignment of the specimens for testing. All specimens were free of pre-existing pathology such as labral tears, Hill-Sachs lesions, cartilage damage, or osteoarthritis. The glenoid surface and labrum of all specimens were then marked for measurement of labral heights at clock positions of 3:30, 4:30, and 5:30 (for a right shoulder) by use of a standardized template. For simplicity, only the position on the right glenoid (3:30, 4:30, and 5:30) will be referred to throughout the rest of the article. During testing, the specimens were kept moist by use of a saline solution spray.
A 3-dimensional (3D) digitizer (Microscribe MX; Immersion, San Jose, CA) (accuracy, 0.051 mm) allowed for the glenoid and labrum surfaces to be mapped with a number of points. First, the coordinates were determined at the deepest point of the glenoid articular surface. The 3D digitizer then measured several coordinate positions by tracing the shape of the labrum, from medial to lateral labrum, at each of the 3:30, 4:30, and 5:30 clock positions. Digital tracking was performed by 2 independent observers.
By use of a custom-written Matlab code (The MathWorks, Natick, MA), the coordinate data from the 3D digitizer were graphically mapped. The z-coordinate at the deepest point of the glenoid articular surface and the highest tip of the labrum were determined. The increase in labral height was calculated as the shortest z-coordinate distance from a tangential line drawn through the deepest point of the glenoid articular surface to the tip of the labrum at each of the clock positions (Fig 1). The percent change in labral height was determined as the post-repair height divided by the preinjury height.
Figure 1.
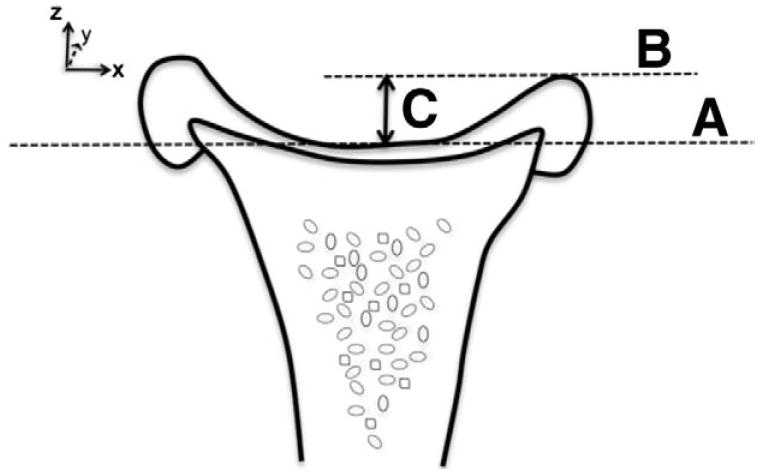
(C) Labral height was determined as the shortest z-coordinate distance from a tangential line drawn through (A) the deepest point of the glenoid articular surface to (B) the tip of the labrum at each of the clock positions.
Labral detachment was then performed, in which the labrum was separated from the underlying bone from the 3-o’clock position to the 6:30 clock position (9-o’clock position to 5:30 clock position on the left glenoid) to a depth of 1.0 cm with an arthroscopic elevator.
For each glenoid pair, 1 side was randomly selected to receive 1 of 2 different Bankart reconstructive procedures, with the contralateral side receiving the other: (1) 3 traditional 3.0-mm BSTs with No. 2 FiberWire anchors (Arthrex) secured with knots or (2) 3 knotless 2.9-mm PL suture anchors with No. 2 FiberWire. In brief, for each repair group, 3 anchors were placed on the glenoid rim at the 3-, 4-, and 5-o’clock positions by use of the aforementioned clock template. For the BST anchor placement, a hole was drilled to the standard depth at the glenoid articular margin/glenoid rim at a 45° angle to the glenoid, after which the anchor was tapped in to the recommended depth according to the manufacturer’s guidelines. To ensure that a standardized bite of tissue was obtained, a digital caliper was used to measure the distance from the simulated labral tear to a distance of 1 cm anteroinferiorly from the anchor placement for all 3 anchors. The bite was taken anteroinferiorly to simulate capsular laxity so that the labrum would be pulled superiorly to retension the AIGHL. An arthroscopic suture-relaying technique (SutureLasso; Arthrex) was used to shuttle 1 limb of the sutures beneath the labrum, creating a simple knot configuration. The 2 limbs were then tied by use of 6 alternating half-hitches with alternating posts (surgeon’s knot) as described by Lo et al.7 to secure the labrum to the glenoid. For labral repair with the PL anchors, after drilling of the glenoid at a 45° angle to the rim, the same procedure was used except that 1 of the limbs of a No. 2 FiberWire was passed through the capsulolabral tissue (by use of the standardized 1.0-cm anteroinferior bite of tissue) to shuttle the suture through the tissue before anchor insertion. Both ends of the suture were passed through the PL eyelet, inserted into the predrilled hole, and impacted to the depth recommended by the manufacturer. These steps were repeated for each of the anchor positions (Fig 2).
Figure 2.
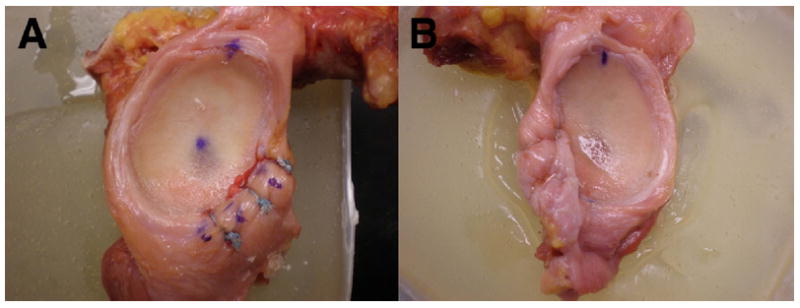
(A) Labral repair with BSTs at 3-, 4-, and 5-o’clock positions of a right glenoid. (B) Labral repair with PL anchors at 8-, 7-, and 6-o’clock positions of a left glenoid.
The post-repair labral height was again measured with the 3D digitizer and Matlab for each position, as described previously. The percent change in labral height from before injury to after repair was determined as the post-repair height divided by the preinjury height.
Statistical analyses were performed with paired t tests to compare preinjury and post-repair labral heights, independent t tests to compare BST and PL, and 1-way analysis of variance to determine the effect of clock position. A significance value of P = .05 was used for all analyses.
RESULTS
An increase in labral height was achieved for all specimens, with mean labral height increasing from 5.35 mm to 8.05 mm (Table 1). This corresponded to a 159% ± 13.7% increase from before injury to after repair. The increase in labral height from before injury to after repair for specimens repaired by BST and PL was 164.0% ± 18.7% (P < .0001) and 153.0% ± 5.8% (P < .0001), respectively (Figs 3 and 4).
Table 1.
Labral Heights of Specimens Before Injury and After Repair With BST and PL Anchors, Measured at Each Position
| Preinjury Labral Height (mm) | Post-Repair Labral Height (mm) | P Value | Preinjury Height/Post-Repair Height (%) | |
|---|---|---|---|---|
| BST | ||||
| 3:30 | 4.85 | 7.63 | < .01 | 171.04 |
| 4:30 | 5.08 | 8.09 | < .01 | 171.80 |
| 5:30 | 5.30 | 7.77 | < .01 | 150.75 |
| PL | ||||
| 3:30 | 5.64 | 7.88 | < .01 | 144.43 |
| 4:30 | 5.50 | 8.82 | < .01 | 166.27 |
| 5:30 | 5.65 | 8.05 | < .01 | 150.12 |
Figure 3.
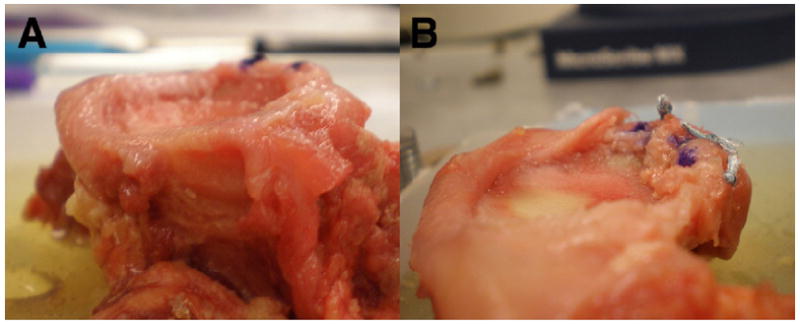
(A) Glenoid labrum before injury. The intact labrum is seen on the far right. (B) Glenoid labrum after repair with BSTs.
Figure 4.
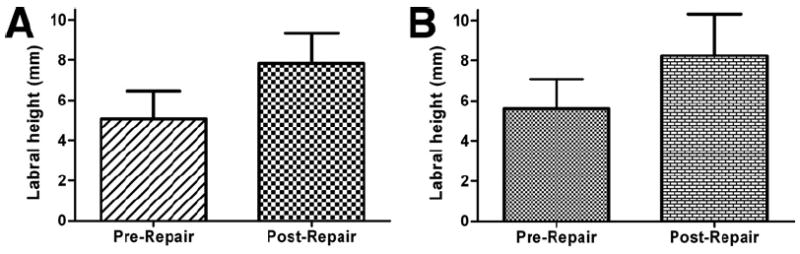
(A) Labral heights (in millimeters) before injury and after repair for specimens repaired with traditional suture anchors (BSTs). (B) Labral heights (in millimeters) before injury and after repair for specimens repaired with knotless suture anchors (PLs). Labral heights were significantly increased from before injury to after repair for both BSTs (P < .0001) and PLs (P < .0001).
BST anchors and PL anchors were compared at each of the clock positions. At 3:30, the increase in labral height was 171% ± 63.1% and 144% ± 33.5% for BST and PL repairs, respectively. At 4:30, the increase in labral height was 171% ± 59.9% and 166% ± 44.7% for BST and PL repairs, respectively. At 5:30, the increase in labral height was 151% ± 29.2% and 150% ± 41.5% for BST and PL repairs, respectively. There were no significant differences in labral height for specimens prepared with BST or PL repairs at clock positions of 3:30 (P = .260), 4:30 (P = .818), and 5:30 (P = .971) (Fig 5).
Figure 5.
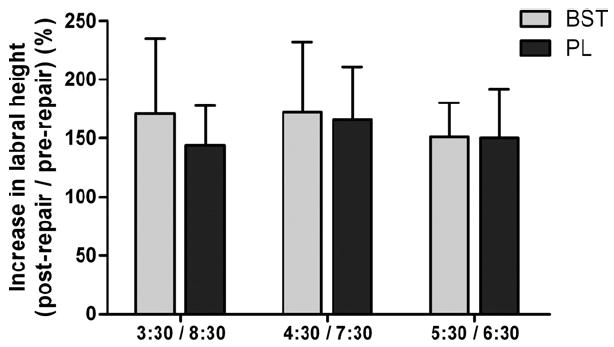
Comparison of BST and PL repairs at each clock position along labrum. No significant differences were observed between BSTs and PLs at any of the 3 positions (P = .260 at 3:30, P = .818 at 4:30, and P = .971 at 5:30).
Furthermore, for a given repair technique, labral height was similar (P = .64 for BST and P = .46 for PL) among the 3 anatomic positions examined.
DISCUSSION
Proper positioning of the labrum, as well as proper tensioning of the AIGHL, is necessary for successful arthroscopic treatment of instability in acute Bankart lesions. Failure to re-establish the proper ligamentous restraints in patients has been shown to lead to increased failure rates after arthroscopic stabilization.8 Therefore current techniques repair the labrum anatomically, shifting the labrum superiorly and laterally up onto the glenoid rim near the articular margin, resulting in tightening of the AIGHL.
When the capsule is taken together with the labrum, the resulting labrum plus capsule serves 2 purposes. First, it restores the natural tension in the capsular ligaments, resulting in less translation in positions of vulnerability.9 Second, this complex increases the depth of concavity of the glenoid. By re-establishing this concavity, the labrum plus capsule helps to restore normal loads across the glenoid in positions vulnerable to dislocation.10
To our knowledge, this is the first study to analyze the measurement and change of capsulolabral height with contemporary suture anchor techniques. One purpose of the study was to determine the extent of increase in labral height that occurs with capsular augmentation. Several studies have shown that loss of labral height leads to increased instability of the glenohumeral joint in either the anterior or posterior direction.3,11 Re-creation of labral height has been shown by Lazarus et al.3 to not only normalize the stability of the glenohumeral joint but also to help restore the concavity. Therefore in an acute Bankart lesion restoration of the labral height is necessary to restore several of the key stabilizers of glenohumeral function. Our results show that both suture anchor constructs used in this study effectively restore the labral height and even increase the labral height in reference to the center of the glenoid. Capsular augmentation of the labrum resulted in a mean increase in labral height of 150% at the 3:30 clock position, which is typically the most important anchor to anatomically reattach the AIGHL.11 The resulting restoration of labral tissue height can improve glenohumeral stability, center the humeral head, and restore the concavity/compression function of the labrum as previously shown by Lazarus et al.
The secondary goal was to determine the differences between traditional suture anchors secured with knots and second-generation knotless suture anchors regarding the ability to re-create the labrum. One disadvantage of the early knotless anchors was the inability to select the amount of tissue to be used in the labral repair. If too large of a bite is taken, the knotless anchor would not insert properly because of high tension on the loop construct. Conversely, if too small of a bite is taken, there would be insufficient tension, resulting in laxity in the AIGHL and recurrent instability. However, it has been hypothesized that second-generation knotless anchors allow any amount of tissue and tension to be obtained. This concept is evident by the creation of increased labral height with a “1-cm bite” of capsular tissue. If the knotless anchor was not able to tension the capsular tissue appropriately, the tissue would be lax and not brought up to the labrum as with traditional suture anchors, resulting in a shorter labral height. However, this study showed no differences in labral augmentation between BSTs and PLs at any of the positions along the glenoid labrum, suggesting that knotless suture anchors may work just as well as traditional suture anchors secured with knots in restoring labral height.
This study only looked at the re-creation of the labrum and its resultant height differences before and after repair with the use of 2 suture anchor constructs in an open manner at time 0. Assessments of strength, stability, or changes in the repair height over time were not attempted because of the design of the study. Limitations include lack of preinjury and post-repair translational studies showing a decrease in the ability to translate the shoulder anteroinferiorly after repair. Further studies should examine the differences in height of the labrum and changes in translational forces needed to dislocate the shoulder. Another disadvantage of this study is that the cadavers had an intact AIGHL before the creation of a simulated Bankart lesion. Speer et al.12 have documented that instability of the glenohumeral joint involves some stretching of the AIGHL in addition to the Bankart lesion. The lack of capsular laxity in our specimens may have led to an artificial inflation of the labral height because stretching of the capsular ligament would possibly lead to a smaller amount of tissue taken. Furthermore, in this model an open restoration of labral height was performed, and extrapolation of these results to an arthroscopic model might not be warranted. Arthroscopically, it is difficult to place anchors at a 45° angle to the glenoid, as has been shown previously, which can affect the stability of the glenohumeral joint.13,14
CONCLUSIONS
An increase in labral height can be achieved to create a significant height increase from before injury to after labral repair. The difference in labral height afforded by a traditional suture anchor and a knotless anchor is not statistically significant.
Supplementary Material
Acknowledgments
The authors thank Alejandro Espinoza, Ph.D., for assistance with data analysis.
All of the researchers received funding from Arthrex, Naples, Florida. Supported by National Institutes of Health grant T32 AR052272.
References
- 1.Robinson G, Ho Y, Finlay K, Friedman L, Harish S. Normal anatomy and common labral lesions at MR arthrography of the shoulder. Clin Radiol. 2006;61:805–821. doi: 10.1016/j.crad.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Fehringer EV, Schmidt GR, Boorman RS, et al. The anteroinferior labrum helps center the humeral head on the glenoid. J Shoulder Elbow Surg. 2003;12:53–58. doi: 10.1067/mse.2003.128196. [DOI] [PubMed] [Google Scholar]
- 3.Lazarus MD, Sidles JA, Harryman DT, II, Matsen FA., III Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am. 1996;78:94–102. doi: 10.2106/00004623-199601000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Baker CL, Uribe JW, Whitman C. Arthroscopic evaluation of acute initial anterior shoulder dislocations. Am J Sports Med. 1990;18:25–28. doi: 10.1177/036354659001800104. [DOI] [PubMed] [Google Scholar]
- 5.Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–1217. [PubMed] [Google Scholar]
- 6.Barber FA, Coons DA, Ruiz-Suarez M. Cyclic load testing and ultimate failure strength of biodegradable glenoid anchors. Arthroscopy. 2008;24:224–228. doi: 10.1016/j.arthro.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Lo IK, Burkhart SS, Chan KC, Athanasiou K. Arthroscopic knots: Determining the optimal balance of loop security and knot security. Arthroscopy. 2004;20:489–502. doi: 10.1016/j.arthro.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 9.Metcalf MH, Pon JD, Harryman DT, II, Loutzenheiser T, Sidles JA. Capsulolabral augmentation increases glenohumeral stability in the cadaver shoulder. J Shoulder Elbow Surg. 2001;10:532–538. doi: 10.1067/mse.2001.118411. [DOI] [PubMed] [Google Scholar]
- 10.Halder AM, Kuhl SG, Zobitz ME, Larson D, An KN. Effects of the glenoid labrum and glenohumeral abduction on stability of the shoulder joint through concavity-compression: An in vitro study. J Bone Joint Surg Am. 2001;83:1062–1069. doi: 10.2106/00004623-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Kim SH, Noh KC, Park JS, Ryu BD, Oh I. Loss of chondrolabral containment of the glenohumeral joint in atraumatic posteroinferior multidirectional instability. J Bone Joint Surg Am. 2005;87:92–98. doi: 10.2106/JBJS.C.01448. [DOI] [PubMed] [Google Scholar]
- 12.Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76:1819–1826. doi: 10.2106/00004623-199412000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Davidson PA, Tibone JE. Anterior-inferior (5 o’clock) portal for shoulder arthroscopy. Arthroscopy. 1995;11:519–525. doi: 10.1016/0749-8063(95)90126-4. [DOI] [PubMed] [Google Scholar]
- 14.Ilahi OA, Al-Fahl T, Bahrani H, Luo ZP. Glenoid suture anchor fixation strength: Effect of insertion angle. Arthroscopy. 2004;20:609–613. doi: 10.1016/j.arthro.2004.04.063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


