Abstract
Older women may have chronic or age-related conditions that increase the risk of falls or that limit their ability to remain active. It is unclear if a water-based exercise program provides a safe and effective alternative to land-based exercise. The purpose of this study was to evaluate the impact of a water-based exercise program method on land-based functional activities of daily living (ADL) for women 60 years and older. This study used a quasi- experimental, nonequivalent control group design. Sixty-six women (60-89 yr of age) self- selected to a water exercise (WEX) group (n = 48) or control (C) group (n = 18). The training consisted of a 16-week (45 min·day-1, 3 d·wk-1) supervised WEX program that included 10 min of warm-up and warm down/stretching and 35 min training using the S.W.E.A.T.™ method in shallow water 1.0-1.2 m, with water temperature approximately 28-29°C. Participants were required to attendat least 94% of the sessions. Assessments for participants included ADL functional field tests. In comparison to the C group, WEX participantsimproved (p < 0.05) flexibility (8%), sit- to-stand (31%), walking speed (16%) and stride length (10%), agility (20%), stair climb (22%), arm curl (39%), and static (42-48%) balance, but not dynamic balance. Results indicate that the S.W.E.A.T.™ method applied to this water exercise program provides a well-rounded, safe, and effective exercise program where older women can improve functional ADL and static balance.
Key Points.
Older women with a variety of health conditions participated in 16 weeks of exercise (92% adherence) with no injuries.
The S.W.E.A.T.™ method applied to this water-based program was found to significantly improve several aspects of physical function, including postural balance.
This shallow water program provided a well-rounded, safe and effective activity for women to improve functional ADL on land.
Key words: Functional ADL, water/aquatic exercise, older women
Introduction
Physical activity can decrease the risk of disability and increase mobility among older adults (Hirvensalo et al., 2000). Mobility also impacts balance and activities of daily living (ADL) yet some women aged 50 and older may have chronic or age-related conditions that limit their ability to perform exercises or physical activity on land. Upright water exercise performed in shallow water (WEX) has become increasingly popular among older adults. Water immersion reduces the fear and risk of falling and therefore may provide a safe, comfortable and effective alternative to land-based training for improving health and mobility. It has been reported that WEX elicits significant improvements in cardiorespiratory fitness, muscular strength, body fat and total cholesterol among women age 50 and older (Bocalini et al., 2008; Campbell et al., 2003; Colado et al., 2009; Devereux et al., 2005; Meredith-Jones et al., 2009, 2011; Nagle et al., 2013; Takeshima et al., 2002; Tsourlou et al., 2006). Some studies have found significant improvements in several functional tests after WEX (Bento et al., 2012; Colado et al., 2009; Katsura et al., 2010; Takeshima et al., 2002; Tsourlou et al., 2006). However, sample size in each of these studies was small or medium (n<30) for the experimental groups. Additionally a few studies have shown that WEX improves dynamic balance and posture (Katsura et al., 2010; Simmons and Hansen, 1996). One study (n = 50) investigated the effect of WEX on dynamic balance and found improvements in repeated up and down stair stepping (Devereux et al., 2005). However, static balance was not measured in any of these studies. Thus, it is important to clarify the effects of WEX in a larger sample and in both static and dynamic balance assessments.
Training designs for water-based studies have varied widely. The S.W.E.A.T.™ method has been found to be an effective training method in shallow and deep water, resulting in improved cardiovascular and muscular endurances for a middle-aged woman (43 years), for a young woman, a woman diagnosed with muscular dystrophy, and one with severe physical disabilities (Escobar et al. , 2013; Nagle et al., 2013; Sanders, 1993; Sanders and Escobar, 2010). The S.W.E.A.T.™ acronym describes a method of cues that coach participants to changes in speed, surface area, impact, range of motion, planes of movement and travel through water. Each variable when applied changes how the properties of water are engaged against the body for varied and interval-based training.
Several factors were used to design the cuing method including the effects of buoyancy and drag resistance. Buoyancy is a force that leads to resistance downward, assistance upward, and the degree of lower body impact which varies based on an individual’s body density, the water depth, and movement speed (Harrison et al., 1987; 1992; Becker, 1997). The higher density of water (compared to air) along with drag forces, results in loading that occurs during all movements and varies with speed and surface area (Cassady and Nielsen, 1992; Colado and Triplett, 2009; Rafaelli et al., 2010; Wilder et al., 1993). Eddies, wakes and drag forces provide water turbulence for overload and body stabilization challenges as the arms and legs move in different planes and is enhanced further as the body travels through the water (Campbell et al., 2003; Colado and Triplett, 2009; Colado et al., 2009; Pöyhönen, 2002; Skinner and Thompson, 1989). Based on these findings, the S.W.E.A.T.™ method variables were designed to include the following cues:
S. = Changes in Surface area and Speed.
W. = Changes in impact by using the Working positions of rebound (jumping), neutral (chest submerged, feet touch lightly), suspended (buoyant work performed without feet touching bottom), and extended (standing tall, feet grounded on the bottom).
E. =Enlarge the movement (extending to fuller range of motion).
A. = Work Around the body or joint by changing planes (sagital, transverse and multiplaner).
T. = Traveling through water forward, backwards and on diagonal.
The purpose of the current study was to evaluate the impact of the S.W.E.A.T.™ method as an instructional method during a water-based exercise program targeting functional activities of daily living (ADL) for women 60 years and older.
Methods
Participants
Seventy-seven participants were recruited from the community through a newspaper, community bulletins, and via a television talk show aired to explain the study and recruitment criteria. In order to be accepted into the study, participants had to be women, 60 years of age or older, living a sedentary or relatively inactive lifestyle (less than 150 minutes of exercise per week). In addition they needed to be available to attend 16 weeks of exercise, plus pre/post-testing sessions. In addition they had to be cleared by their physician for independent community-based water exercise and be able to use a poolside ladder to enter and exit the pool with only minor assistance. After the first meeting, 72 participants were invited to return with their physician’s approval to enroll. During the second meeting, 71 participants completed consent forms and scheduled assessments. During the assessments, five were excluded due to conditions that included frozen shoulder (limited range of motion for poolentry/exit), illness, or inability to commit to the scheduled sessions. (Figure 1) The remaining 66 volunteers (60-89 yr of age) were included in the study which was approved by the Human Research Protection Board, University of Nevada.
Figure 1.
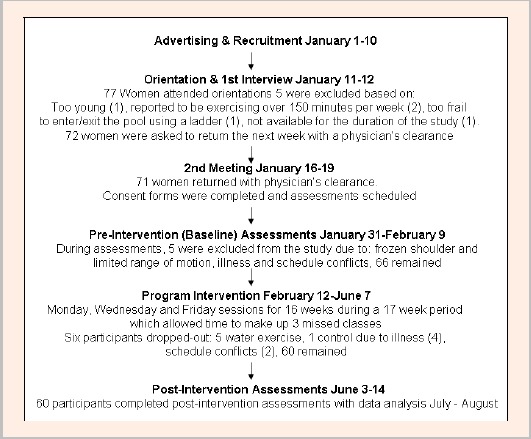
Study process flow chart.
Following baseline measurements of height (centimeters) and weight (kilograms), the participants completed nine functional ADL assessments and self-selected into one of two groups: a training (WEX) group (n = 48) or a non-exercise control (C) group (n = 18). A limitation of this approach is the lack of randomization of subjects to the intervention group. Thus, this study used a quasi-experimental, nonequivalent control group design. This design is reported to be an acceptable alternative to an experimental design when randomization is not possible. Most participants who attended the study orientation meetings wanted to participate in the WEX and only reluctantly agreed to participate as a control after the WEX was filled. Sixty-six participants were selected from initial screening. All participants provided written consent forms from physicians and signed an informed consent form in accordance with the university Human Subjects Review Committee Guidelines.
Although the number of exercisers and controls were significantly different, the groups were found to be homogeneous with respect to physical characteristics for age, height and weight (Table 1). Participant co-morbidities in both groups were similar. Reported co- morbidities included: hypertension controlled with medication (31% WEX, 44% C), smoking (5% for both WEX and C), history of heart attack (4% WEX, 5% C), family history of heart disease (54% WEX, 22% C), arthritis symptoms (73% WEX, 72% C), and back pain primarily associated with arthritis (19% WEX, 16% C). Over 60% of the WEX group claimed to be former smokers compared to 22% of C group. Two participants in each group had knee replacements and some participants in both groups reportedly had knee pain (6% WEX, 11% C). One participant in each group reported poor balance, to the extent that they required a cane to assist with walking long distances. The WEX group participated in a 16-wk water exercise program. The control group was instructed to continue their normal physical activities, without adding new ones. All participants were asked not to change their nutrition practices during the duration of the study. After 16 weeks, all measurements for height, weight, and ADL were repeated.
Table 1.
Participant descriptive characteristics Pre-Intervention vs. Post-Intervention, mean (standard deviation).
| Pre-Intervention | Pre-Intervention | |||
|---|---|---|---|---|
| Exercise group (n=48) |
Control group (n=18) |
Exercise group (n=43) |
Control group (n=17) |
|
| Age (years) | 73.6 (13.5) | 72.8 (27.4) | ||
| Height (m) | 1.62 (.07) | 1.58 (.07) | 1.61 (.07) | 1.57 (.06) |
| Weight (kg) | 71.1 (14.0) | 66.2 (10.2) | 70.6 (14.1) * | 65.8 (10.8) |
* p < 0.05 compared to baseline.
Functional ADL testing protocols
Participants were instructed to come to the testing site fully rested (no exercise for 24 hours before). There were no dietary restrictions. Nine functional tests assessed static and dynamic balance (Johnson and Nelson, 1986); agility, walking speed and stride length (steps per walk), lower body strength, upper body strength and stair climbing using the AAHPERD Functional Fitness Protocols for older adults (Corbin and Metal-Corbin, 1984) and lower body flexibility (Golding et al., 1989). Studies conducted on assessments for agility, biceps (arm) curl, dynamic balance, and sit and reach yielded test-retest reliabilities ranging from .82 to .99 for women aged 60 to 81 years (Bravo et al., 1997; Osness, et al., 1996; Shaulis et al., 1994).
Static balance for the right and left legs was measured while the participant stood on one leg with eyes open and hands on hips. A perfect score was 60 seconds with time recorded to the nearest hundredth (Johnson and Nelson, 1986). Static balance assessments were conducted for both the right and left legs independently, repeated two times on each leg and were recorded as separate variables. The best score was recorded.
Dynamic balance measured the ability of participants to maintain balance while shifting their weight when walking. Participants were directed to step within the boundaries of circles arranged in a pattern that included both forward and diagonal stepping. In addition, they were directed to balance briefly for four seconds, if possible, on one leg after each step. Four points were awarded for stepping in the center of each of the seven circles plus four possible points were awarded for each second that participants held the static balance position in each circle and a numerical score was awarded based on points earned for each step completed within the circle and time to balance (Johnson and Nelson, 1986). A perfect score for dynamic balance was 56 points. The test was performed twice with the best score recorded for performance.
The sit-and-reach measured lower body flexibility. Shoes were removed and participants sat with both legs extended forward. A yardstick was positioned between their legs with the 0 inch mark on the yardstick facing the body. The participant then reached forward while keeping the knees straight as they tried to touch their toes. The score recorded to the nearest one-quarter inch, the most distant point reached on the yardstick with the fingertips (Golding et al., 1989). The test was performed twice with the best score recorded for performance.
Sit-to- stand was used to determine lower body muscular strength/endurance. The assessment began with the participant fully seated in a chair with back straight and feet flat on the floor. Arms were crossed and held against the chest. Participants were asked to rise to a full standing position and then sit back down, as quickly as possible. Each full hip extension (stand) counted as a stand. If participants ended the 30 seconds midway between hip extension and flexion, they were awarded a .5 for the partial stand. The number of stands participants completed (full and partial) within 30 seconds was recorded (Corbin and Metal-Corbin, 1984). The test was performed twice with the best score recorded for performance.
Walking speed was measured by how fast participants walked a distance of 50 feet. Participants were instructed to stand still, feet together, toes at the starting line. They then were cued to walk a quick, but safe pace, crossing the finish line while keeping the pace. Time in seconds to complete the distance was measured with a stopwatch and recorded to the nearest hundredth second by one researcher. Stride length was also measured during the 50-foot speed walking assessment. Participants stepped first on their right foot and the number of right-legged steps taken to complete the distance was counted. Each time the right foot stepped forward it was counted as one (a complete gait cycle). If participants completed the distance with the left leg forward, the step counted as .5. The number of steps required to cover the distance was recorded by another researcher responsible for counting steps only (Corbin and Metal-Corbin, 1984). The test was performed twice with the bestscore recorded for performance.
Agility and dynamic balance were evaluated using the up-and-go assessment which began with participants fully seated in a chair and on a signal they were directed to rise from the chair, turn right and walk as quickly as possible using a pattern that crossed behind the back of a cone placed to the right and slightly behind the chair. The participant then returned to the chair assuming a seated position. They then immediately stood up to repeat the pattern to the left side without hesitation. The circuit was repeated twice and time was recorded in seconds to the nearest hundredth with the best time used for analysis (Corbin and Metal-Corbin, 1984). The test was performed twice with the best score recorded for performance.
Stair climb assessed both descending and ascending speed. Participants were directed to stand at the top of a flight of stairs and walk down the flight of stairs, turn around, and walk back up the stairs. They were instructed to step off the bottom step with both feet to turn around before ascending. Participants completed two test trials and the time was recorded in seconds to the nearest hundredth (Corbin and Metal-Corbin, 1984). The best time recorded was used for analysis.
Biceps (arm) curl measured upper body muscular strength and endurance. While seated in a chair, the participant held a five-pound dumbbell in the dominant hand using the “handshake grip” with the elbow extended. On the signal, the participant gradually turned the palms up while curling the arm through full range of motion and then returned to the fully extended position in a controlled manner. Each curl was counted as one when the elbow was fully flexed. A partial count of .5 was awarded when the assessment ended with the participant’s elbow positioned midway between full flexion and extension. The score represented the total number of curls (full and partial) completed correctly within 30 seconds (Corbin and Metal-Corbin, 1984). The test was performed twice with the best score recorded for performance.
Exercise- training protocol
The WEX group participated in a 16-week program, 3 sessions·wk- 1 and progressed from 20-45 min per session. Each session was lead by trained fitness instructors and supervised by researchers. Training was performed on 3 different days of the week with at least 1 day of rest between sessions. Generally, Monday’s session focused on learning new skills and modifications as needed by the individual. Wednesday’s targeted skills review with drills designed to practice progression (S.W.E.A.T.™ system applied). Fridays were dedicated to application of the skills and drills learned previously with the focus on training. Fridays were the only day music was used during week 1-7. Starting at week 8, music was also added to Wednesday sessions after the skills and drills were practiced. The water level was at xiphoid level 1.0 to1.2 m with an average water temperature of approximately 28 to 29 °C. To be included in the final analysis, participants were required to attend 94% of the training sessions (45 out of a possible 48 sessions) over 16 weeks. Participant-to-instructor ratio was nine to one.
The pool program consisted of 10 minutes of warm-up and warm down/stretching (5 minutes for each), and 10-35 minutes of training. Training exercises varied based on the daily objectives but generally included: functional ADL progressions (10-20 minutes), cardiovascular endurance (10-15 minutes) and muscular endurance training (5-10 minutes) (Table 2). All progressions began by first having participants demonstrate good posture, stabilizing the body in an upright stationary position using a flat sculling technique with hands. Lycra webbed gloves (MIZUNO® Corp., Osaka, Japan) were used to increase the surface area of the hands for enhanced stability and to help “grip” the water during movements. During cardiorespiratory exercises, one of the six basic movements; walk, jog, rock, kick, jump and scissors, were varied by applying a method of cues defined by the acronym S.W.E.A.T.™ method. Each letter represents a cue that is applied to a basic exercise every 15-30 seconds. These movement variations created progressions that encourage participants to increase or decrease intensity and/or complexity. Instructors applied the cues based on how the students generally were responding to the exercise. For comfort and safety, each participant was taught to use parts of the S.W.E.A.T.™ method including slowing speed, decreasing the size, and to find a stabilized position for recovery, to modify their own intensity as needed during the workout. The program is described completely in a 75 minute DVD entitled: The Golden Waves® Program, Functional Water Training for Older Adults (Sanders and Maloney-Hills, 2008; www. dswfitness.com or www.HealthyLearning.com).
Table 2.
Program design.
| Wk (CT in min) | Objective | Basic Move(s) | Intensity Rating of Perceived Exertion (RPE) |
Intervals Format* | S.W.E.A.T.TMCues (Variations) |
|---|---|---|---|---|---|
|
1 (20-30) |
Learn, modify and practice basic skills and walking | En tr y/exit skills Adjustment to water depth Recover to stand Sculling practice with gloves Posture practice Walking | Easy | Walking with SWEAT variations changed every 15- 30 sec | E (50% to full ROM) A W (Extended) T tr avel forward, back and sideways |
|
2 (20-30) |
Learn, modify and practice jog, walk, balance | Walk, jog 1 legged stands | Easy/Moderate | SWEAT variations changed every 15- 30 sec | S. W. E. A. T. |
| 3 (30-45) | Learn, modify, practice & train Walk, jog Upper body muscular endurance |
Walk, jog Biceps/ tr iceps with gloves (open or closed hand) |
Cardio: Easy to moderate Muscular: Moderate to somewhat hard |
Cardio: SWEAT variations changed every 15- 30 sec Muscular: 8 repetitions X 2 sets |
Cardio: S. W. E. A. T. Muscular: S. |
|
4 (45) |
Repeat wk 3, and add: Kick Trapezius |
Walk, jog, kick Biceps/ triceps and trapezius with gloves (open or closed) |
Cardio: Moderate to somewhat hard Muscular: Moderate to somewhat hard |
Cardio: SWEAT variations changed every 15- 30 seconds Muscular: 8 repetitions, 3 sets |
Cardio: S. W. E. A. T. Muscular: S. T. |
|
5 (45) |
Repeat wk 4 and add: Rock Pectorals |
Walk, jog, kick, rock cardio intervals Pectorals, tr apezius, biceps/ triceps |
Cardio: 15 sec somewhat hard to hard, recover easy Muscular: Somewhat hard to hard Aquaflex® paddles used to increase surface area overload |
Cardio: SWEAT variations using 15 sec intervals (speed variations) Muscular: 8-15 repetitions, 3 sets (gloves or paddles) |
Cardio: S. W. E. A. T. Muscular: S. T. |
| 6 (45) | Repeat wk 5 and add: Jump Deltoids, Rhomboids |
Walk, jog, kick, rock, jump Deltoids, rhomboids |
Cardio: Repeat wk 5 Muscular: Repeat wk 5 |
Cardio: Repeat wk 5 Muscular: Repeat wk 5 |
Cardio: S. W. E. A. T. Muscular: S. T. |
| 7 (45) | Repeat wk 6 and add: Scissors Abdominals, Hip ad/ab -ductors |
Walk, jog, kick, rock, jump, scissors Abdominals, Hip ad/ab -ductors |
Cardio: Repeat wk 6 Muscular: Repeat wk 6 |
Cardio: Repeat wk 6 Muscular: Repeat wk 6 |
Cardio: S. W. E. A. T. Muscular: S. T. |
| 8-16 (45) | Add ADL targeted progressions each wk (50 exercises total**) to basic moves and muscular exercises Progress intensity and complexity |
ADL patterned exercises are developed from basic moves to target tasks Step work and resistance bands are added to muscular, cardio and balance exercises |
Repeat previous wks, add new ADL exercises each wk Cardio: Moderate to hard/very hard Muscular: Hard to very hard |
Integrate learned exercises into ADL patterned progressions | ADL: S. W. E. A. T. Cardio: S. W. E. A. T. Muscular: S. T. |
CT = class time
* Interval Formats:
- Variations of a basic move using S.W.E.A.T. cues are applied every 15- 30 seconds.
-
Timed Cardio Interval Variations (15:15:15) are applied to a basic move using each S.W.E.A.T. cue:
-
▪15 seconds preparation for a posture check using the “I surrender” or “Hands up” cue to set the shoulders over hips, to stabilize the body in buoyancy, then practice pattern of the move to develop full range of motion (Easy/Moderate)
-
▪15 seconds work (Somewhat Hard/Hard)
-
▪15 seconds active recovery and/or stretch (Easy)
-
▪
** The Golden Waves Functional Water Fitness Program for Older Adults is available on DVD through Desert Southwest Fitness, www.DSWFitness.com or through Healthy Leaning at www.HealthyLearning.com
During all of the 50 functionally designed ADL exercises, the S.W.E.A.T.™ method was applied to each basic pattern of movement that targeted and challenged activities such as: stair climb (step on and off a step), sit-to-stand (squat jumps), agility and dynamic balance (walk or jog with changes in speed, interrupted by cues to “freeze frame” on one leg for balance), or fall and recovery to a stand. During the 15- 30 second work phases participants were encouraged to work vigorously to achieve an RPE of 13-14, (Somewhat Hard) and if able to maximize effort by working at an RPE 15 (Hard) on the Borg scale 6-20 (Borg, 1998).
For example, during a 3 minute jogging set, the S.W.E.A.T.™ method would be applied as follows:
Objective: Cardiovascular Endurance: Begin with an easy jog, knees forward. Hands scull using webbed open gloves on the surface (15-30 seconds). Check posture and water depth for lower body impact comfort. Jog and -
S. = Speed up (15-30 seconds)
S. = Slow down (15-30 seconds, recovery)
E= Enlarge range of motion (15-30 seconds)
S. = Speed up using large range of motion of the legs (15-30 seconds)
S. = Slow down, make the move smaller (15-30 seconds, recovery)
W. = Change the Working positions, jog in rebound (pressing off the bottom) (15 seconds), Slowdown and submerge the chest to neutral position (15 seconds), then lift the feet to suspended position (buoyant jog for 15 seconds), then stand up to extended position (standing tall, feet grounded on the bottom, slow down and recover 15-30 seconds).
E. A. = Work Around the body by rotating the hips, wide leg jog to engage different muscle groups (15-30 seconds), then Enlarge (15-30 Seconds) and Speed up (15-30 seconds), then Slow down, stabilize and then
T. =Travel through water, using open webbed gloves to increase Surface area and to assist: forward, backwards and on diagonal. To challenge balance, participants would be surprised to “Freeze and stand on one leg, hands up!” during the set.
Participants progressed at their own rate by adding surface area equipment (e.g., Aqua Flex® paddles) and by webbing open the gloves more frequently to increase surface area to reach the goal RPE for each exercise as stated by the instructor (Table 2). Surface area was added as needed by the participant to achieve RPE targets. In addition, medium weight Thera-Band® elastic resistance bands (Hygenic Corp., Akron OH), were used 1-2 times a week starting at week 6, for 3-5 minutes of eccentric, concentric and isometric postural/upper body exercises that were coordinated with walking, jogging, jumping, kicking or scissors basic moves. Stretching exercises included buoyancy-assisted range of motion moves such as leaping and reaching. Catching drag force resistance against the webbed gloves enhanced upper body stretches as participants walked forward.
Statistical analysis
Data analysis was completed using the statistical software program SPSS for MAC (V.19.0, SPSS Inc., Chicago, IL). Absolute values were used for statistical analysis. However, when discussing outcome measures, relative change was used to provide a clearer translation for the purpose of comparisons between measures with different units. Data were screened for outliers, and assumptions of normality and homoscedasticity. To reduce the potential influence of outliers on the statistical analysis, box-and-whiskers plots were used to identify outliers, which were subsequently eliminated prior to analysis. Each parameter was examined for normality using the Kolomogorov-Smirnov test. Assumptions of homogeneity of variance and sphericity were evaluated. Baseline group mean comparisons were performed using two-tailed independent t-tests. Comparisons between groups over time were evaluated using a two-way multivariate ANOVA with repeated measures. (ANOVA, Wilk’s criterion). Group (WEX and C) served asthe between-subject factor, while Time (pre- and post-test) served as the within-subject factor. Percent changes from pre to post were calculated from the differences in scores. A probability value of less than 0.05 was considered statistically significant.
Results
No significant differences at baseline were present between the WEX group and C in age, height and weight (Table 1). Nor were there any differences in functional ADL measures between groups at baseline (Table 3).
Table 3.
Effects of water exercise on functional ADL (n=61).
| Before | After | Change | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | (%) | ||
| Sit & reach (cm) | Exercise | 25.59 | 6.47 | 27.66 * | 6.90 | 8.4 |
| Control | 21.92 | 6.81 | 21.90 | 5.53 | ||
| Sit to stand (Number) | Exercise | 10.77 | 3.06 | 14.06 *** | 3.95 | 30.5 |
| Control | 12.03 | 2.77 | 12.18 | 1.44 | ||
| Walk Speed(seconds) | Exercise | 10.72 | 2.60 | 9.00 *** | 2.39 | -16.0 |
| Control | 10.92 | 2.34 | 10.16 | 1.87 | ||
| Walk Steps (Number) | Exercise | 11.92 | 1.78 | 10.65 *** | 1.78 | -10.5 |
| Control | 12.18 | 1.96 | 11.59 * | 1.83 | -4.8 | |
| Agility (seconds) | Exercise | 35.3 | 10.68 | 28.12 *** | 9.59 | -20.0 |
| Control | 32.08 | 7.06 | 31.7 | 6.74 | ||
| Stair Climb (seconds) | Exercise | 16.64 | 7.94 | 12.94 *** | 4.73 | -22.5 |
| Control | 18.26 | 7.28 | 16.56 * | 6.64 | -9.3 | |
| Arm curl (Number) | Exercise | 14.01 | 3.77 | 19.53 *** | 5.03 | 30.8 |
| Control | 14.38 | 3.53 | 14.35 | 4.10 | ||
|
Static Balance (seconds) |
Exercise Right | 15.43 | 17.91 | 21.98 * | 18.51 | 42.4 |
| Exercise Left | 14.37 | 14.75 | 21.34 * | 19.72 | 48.0 | |
| ControlRight | 16.79 | 19.82 | 15.34 | 17.92 | ||
| ControlLeft | 14.86 | 16.38 | 11.59 | 16.97 | ||
| Dynamic Balance | Exercise | 45.39 | 9.20 | 50.02 *** | 7.16 | 10.2 |
| Perfect score=54 | Control | 39.88 | 13.46 | 43.65 | 11.21 | |
* p < 0.05,
*** p < 0.001 compared with before
Participants continued the WEX through the full length of the study without any injuries, however due to conflict in scheduling, illness and required surgery, five participants (5WEX, 1C) dropped the program resulting in n = 60 (Figure 1). No injuries were reported during the exercise program and adherence was 92%.
The WEX group significantly improved all functional ADL assessments when compared to the C group (Table 3). The most impressive gains made in static balance (43% right leg and 48% left leg), sit-to-stand and arm curl (31% and 39%, respectively). Walking speed increased for the WEX group (16%) and they also took 10% fewer steps. Agility and stair climb speed, agility, and flexibility (20%, 22%, 8%, respectively) also increased for the WEX. No significant changes were noted in dynamic balance measures for the WEX group, or in any of the measured variables in the C group after the intervention period.
Discussion
Aging is associated with a gradual decrease in muscle mass, strength and power. Water exercise may help to decrease immobility, while increasing power for functional skills (Takeshima et al., 2002). Mobility, the ability to move without assistance, is critical for maintaining independence with limitations including difficulty walking 400 meters (.25 miles), climbing stairs or rising from a chair (Reid et al., 2012). Many studies suggest that muscle strength is a predictor for functional performance however muscle power (force and velocity) may better predict ADL performance (Reid and Fielding, 2012). Timed measures such as sit-to-stand, standing balance, walking speed have been validated as an objective measure of ADL that require muscle power output (Reid and Fielding, 2012).
The S.W.E.A.T.™ method applied to this program was found to be effective for improving sit-to-stand performed by 31%; faster walking speed 16%; fewer steps taken to cover distance 10%, sit-and-reach 8%; agility (20%), speed to climb stairs 22%, arm curl (39%), and static balance (42% right leg and 48% left leg). Participants stated they were more active as a result of the program and could catch themselves now if they stumbled. As reported in their personal journals, improvements by the WEX group in arm curls performed for speed lead to greater ability to lift and move things around.
These results are in accordance with other studies (Bento et al., 2012; Colado et al., 2009; Katsura et al., 2010; Takeshima et al., 2002; Tsourlou et al., 2006). Bento et al., 2012 analyzed the effects of 12 weeks of combined aerobic and strength training in 24 elderly subjects, with 3 sessions per week in shallow water at xiphoid depth. They found significant improvement in functional tests: sit and reach, 8-ft up and go and 6-min walk, and no significant changes were found in the control group (n = 14). In the study of Colado et al., 2009, 15 sedentary postmenopausal women performed 24 weeks of resistance training in shallow water in progression, from 2 to 3 sessions per week. The experimental group improved significantly in all functional tests: sit and reach, knee push-ups, sixty second squats and abdominal crunch, whereas the control group (n = 10) did not show significant changes. Another study (Katsura et al., 2010) found significant improvements in sit and reach, up and go and 5-mwalking speed tests. The subjects who improved these functional tests were 12 healthy older individuals performing 8 weeks of combined aerobic, strength and flexibility training in shallow water with water resistance equipment. Similarly, Takeshima et al., 2002 analyzed the effects of 12 weeks of combined aerobic, strength and stretching training in xiphoid-level water in 15 older women, performing 3 sessions per week. They found significant improvement in the side stepping agility test and no changes were found in the control group (n = 15). Tsourlou et al., 2006 also found significant improvements in sit and reach and timed up and go tests after 24 weeks of combined aerobic and strength training in 12 healthy older women, and no significant changes were found in control group.
Devereux et al., 2005 randomized 50 community-dwelling women (mean age = 73.3 years) diagnosed with oeteopenia or osteoporosis into a shallow-water exercise or non-exercising control group. The 10-week water exercise program was conducted two times a week for 60 minutes a session. Water exercises included 50 minutes of stretches, aerobics and balance. Similar to the current study, participants walked with long strides and performed exercises that stimulated recovery from a fall. Lower body strengthening for hip flexors, quadriceps and ankles were emphasized and land-based tai chi movements were transferred to water. The water exercisers improved stair climbing ability (20%) as measured by a test that required repeated stepping up and down from a step.
Dynamic and static balances are critical for walking with direction changes, stopping, standing and recovery from a stumble. Participants in our study were assessed for both dynamic/static and static balance skills. Static balance was measured during a single-legged stand. Participants in our study improved static balance on both the right and left legs (42 and 48%, respectively). Dynamic balance was measured on a flat surface, and included a combination of multidirectional walking and single-legged static balance. Both the WEX group and C group demonstrated similar changes of approximately 10% between pre- and post-intervention testing. Although scores on the agility test, which requires dynamic balance, improved in the WEX group, we were unable to show an improvement on a specific dynamic balance test during this study. A possible reason for this is the test itself which was developed for use with school-aged children and may not be appropriate for use with older adults. Future studies shouldutilize a test of dynamic balance which is designed specifically for this population.
A limitation of this study is the lack of randomization which resulted in unequal intervention and comparison group sizes. Although this is appropriate and acceptable for a quasi-experimental design, a stronger defense of the intervention would be made with a truly randomized approach. Another potential limitation is the test used to evaluate dynamic balance specifically. It is possible that the test used in the current study, which was designed for evaluating balance in children, was not sensitive enough to detect changes in older adults or that the training stimulus was insufficient to promote improvement.
Conclusion
These results indicate that this S.W.E.A.T.™ method applied to this water-based exercise program elicits significant improvements in ADL and static balance. Therefore, water exercise appears to be a safe and effective mode of exercise that can be performed to improve ADL and balance in older women.
Acknowledgements
Special thanks to the Sanford Center for the Aging, School of Medicine, University of Nevada, Reno and to Mizuno Corp, Osaka, Japan for grant funding support.
To the Golden Waves® program team for data collection, exercise design and instruction: Cathy-Maloney-Hill, RPT, aquatic physical therapist, Courage Center, Eden Prairie, Minnesota, Mary C.V. Curry, Woodbury, Minnesota, Nora L. Constantino, PhD, FACSM, Professor, School of Community Health Sciences, University of Nevada, Reno, Nicki E. Rippee, PhD, Professor Emeritus, Abilene Christian University, Abilene, Texas and John Hseih, PhD, Professor Emeritus, School of Community Health Sciences, University of Nevada, Reno for statistical analysis.
Biographies

Mary E. SANDERS
Employment
Clinical exercise physiologist/Associate Professor School of Medicine, Adjunct Professor, College of Community Health Sciences, University of Nevada, Reno and Director of WaterFit®.
Degree
PhD
Research interests
Water exercise.
E-mail: msanders@medicine.nevada.edu
Nobou TAKESHIMA
Employment
Professor, National Institute of Fitness and Sports, Kanoya, Japan.
Degree
PhD
Research interests
The physiological responses to a wide variety of exercise program types and modes, including water and land-based interventions for older adults.
E-mail: takeshima@nifs-k.ac.jp

Michael E. ROGERS
Employment
Chair of the Department of Human Performance Studies, professor of Exercise Science, and Director for the WSU Center for Physical Activity and Aging Wichita State University, Wichita, Kansas.
Degree
PhD
Research interests
Balance and strength training to reduce fall risk and to improve function in older adults.
E-mail: michael.rogers@wichita.edu
Juan C. Colado
Employment
Laboratory Coordinator of Physical Activity and Health and Director of the research group in Sport and Health. University of Valencia, Spain.
Degree
PhD
Research interests
Aquatic exercise, core, resistance exercise with elastic bands, unstable surfaces and EMG.
E-mail: juan.colado@uv.es

University of Valencia.
Employment
Degree
PhD
Research interests
Aquatic exercise, core training, the role of unstable surfaces for training and EMG.
E-mail: sborreani@yahoo.es
References
- Becker B.E.(1997). Aquatic physics In: Aquatic Rehabilitation. : Ruoti R., Morris P., Cole A.Philadelphia: Lippincott; 15-23 [Google Scholar]
- Bento P.C.B., Pereira G., Ugrinowitsch C., Rodacki A.L.F.(2012). The effects of a water-based exercise program on strength and functionality of older adults. Journal of Aging and Physical Activity 20, 469-483 [DOI] [PubMed] [Google Scholar]
- Bocalini D.S., Serra A., Murad N., Levy R.F.(2008). Water-versus land-based exercise effects on physical fitness in older women. Geriatrics and Gerontology International 8, 265-271 [DOI] [PubMed] [Google Scholar]
- Borg G.(1998). Borg’s perceived exertion and pain scales. Champaign, IL: Human Kinetics [Google Scholar]
- Bravo G., Gauthier P., Roy P.M., Payette H., Gaulin P.(1997). A weight bearing, water-based exercise program for osteopenic women: It’s impact on bone, functional fitness, and well being. Archives of Physical Medicine and Rehabilitation 78, 1375-1380 [DOI] [PubMed] [Google Scholar]
- Cassidy S.L., Nielsen D.H.(1992). Cardiorespiratory responses of healthy subjects to calisthenics performed on land versus in water. Physical Therapy 72, 532-538 [DOI] [PubMed] [Google Scholar]
- Campbell D.T., Stanley J.C.(1963). Experimental and quasi-experimental designs for research on teaching. In: Handbook of Research on Teaching. : Gage N.L.Chicago: Rand McNally; 445-632 [Google Scholar]
- Campbell J.A., D’Acquisto L.J., D’Acquisto D.M., Cline M.G.(2003). Metabolic and cardiovascular response to shallow water exercise in young and older women. Medicine & Science in Sports & Exercise 35, 675-681 [DOI] [PubMed] [Google Scholar]
- Colado J.C., Triplett N.T.(2009). Monitoring the intensity of aquatic resistance exercises with devices that increase the drag force: An update. Journal of Strength & Conditioning Research 31(3), 94-99 [DOI] [PubMed] [Google Scholar]
- Colado J.C., Triplett N.T., Tella V., Saucedo P., Abellán J.(2009). Effects of aquatic resistance training on health and fitness in postmenopausal women. European Journal of Applied Physiology 106, 113-122 [DOI] [PubMed] [Google Scholar]
- Corbin D.E., Metal-Corbin. J.(1984). Reach for it! A handbook of health, exercise and dance activities for older adults. 2nd edition Reston, VA: American Alliance for Health Physical Education recreation & Dance (AAHPERD). [Google Scholar]
- Devereux K., Robertson D., Briffa N.K.(2005). Effects of a water-based program on women 65 years and over:a randomized controlled trial. Australian Journal of Physiotherapy 51, 102-108 [DOI] [PubMed] [Google Scholar]
- Escobar Torres L., Sanders M.E., Lawson D., Belenguer Benítez C.(2013). A case study: Mobility and health impact of an aquatic fitness program for a woman with intellectual and physical disabilities. International Journal on Aquatic Research and Education 7, 147-153 [Google Scholar]
- Golding L.A., Myers C.R., Sinning W.E.(1989). Y’s Way to Physical Fitness. Champaign, IL: Human Kinetics for the YMCA of the USA [Google Scholar]
- Harrison R., Bulstrode S.(1987). Percentage weight bearing during partial immersion in hydrotherapy pool. Physiotherapy Practice 3, 60-63 [Google Scholar]
- Harrison R.A., Hillman M., Bulstrode S.(1992). Loading of the lower limb while walking partially immersed: Implications for clinical practice. Physiotherapy 78,164-166 [Google Scholar]
- Hirvensalo M., Rantanen T., Heikkinen E.(2000). Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. Journal of the American Geriatrics Society 48, 493-498 [DOI] [PubMed] [Google Scholar]
- Johnson B.L., Nelson J.K.(1986). Practical measurements for evaluation in physical education. 4th editionEdina, MN: Burgess Publishing [Google Scholar]
- Katsura Y., Yoshikawa T., Ueda S.Y., Usui T., Sotobayashi D., Nakao H., Sakamoto H., Okumoto T., Fujimoto S.(2010). Effects of aquatic exercise training using water-resistance equipment in elderly. European Journal of Applied Physiology 108, 957-964 [DOI] [PubMed] [Google Scholar]
- Kenny D.A.(1975). A quasi-experimental approach to assessing treatment effects in the nonequivalent control group design. Psychological Bulletin 82, 345-362 [Google Scholar]
- Meredith-Jones K., Waters D., Legge M., Jones L.(2011). Upright water-based exercise to improve cardiovascular and metabolic health: A qualitative review. Complementary Therapies in Medicine 19, 93-103 [DOI] [PubMed] [Google Scholar]
- Meredith-Jones K., Jones L.M., Legge M.(2009). Circuit-based deep water running improves cardiovascular fitness, strength and abdominal obesity in older, overweight women. Medicine and Sport 13, 5-12 [Google Scholar]
- Nagle E.F., Sanders M.E., Shafer A., Gibbs B.B., Nagle J.A., Deldin A.R., Franklin B.A., Robertson R.J.(2013). Energy expenditure, cardiorespiratory and perceptual responses to shallow-water aquatic exercise in young adult women. The Physician and Sports Medicine 41(3), 67-76 [DOI] [PubMed] [Google Scholar]
- Osness W.H., Arian M., Clark B., Hoeger W., Raab D., Wiswell B.(1996). Functional fitness assessment for adults over 60 years. 2nd edition Dubuque, IA: Kendall/Hunt [Google Scholar]
- Pöyhönen T., Sipilä S., Keskinen K.L., Hautala A., Savolainen J., Mälkiä E.(2002). Effects of aquatic resistance training on neuromuscular performance in healthy women. Medicine and Science in Sports and Exercise 34, 2103-2109 [DOI] [PubMed] [Google Scholar]
- Raffaelli C., Lanza M., Zannolla L., Zamparo P.(2010). Exercise intensity of head-out water-based activities (water fitness). European Journal of Applied Physiology 109, 829-838 [DOI] [PubMed] [Google Scholar]
- Reid K.F., Fielding R.(2012). Skeletal muscle power: A critical determinant of physical functioning in older adults. Exercise and Sport Sciences Review 40, 4-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders M., Escobar Torres L.(2010). Aquatic exercise for Muscular Dystrophy: The story of Laura Sos, Castellon, Spain. ACSM’s Health & Fitness Journal 14(6), 35-41 [Google Scholar]
- Sanders M., Maloney-Hills(2008). The Golden Waves Functional Water Training for Health Program and The Golden Waves, Functional Water Training for Health, Leadership Program videos. Sanford Center for Aging: University of Nevada, Reno and WaterFit, Reno, Nevada. [Google Scholar]
- Sanders M.E.(1993). Selected physiological responses to a water exercise program called wave aerobics. Unpublished masters thesis. University of Nevada, Reno [Google Scholar]
- Shaulis D., Golding L.A., Tandy R.D.(1994). Reliability of the AAHPERD functional fitness assessment across multiple practice sessions in older men and women. Journal of Aging and Physical Activity 2, 273-279 [Google Scholar]
- Skinner A.R., Thompson A.M.(1989). Duffield’s Exercise in Water, 3rd edition Philadelphia: Bailliere Tindall; 4-46 [Google Scholar]
- Simmons V., Hansen P.(1996). Effectiveness of water exercise on postural mobility in the well elderly: an experimental study on balance enhancement. Journal of Gerontology: Medical Sciences 51A, M233-M238 [DOI] [PubMed] [Google Scholar]
- Takeshima N., Rogers M.E., Wantanebe E., Brechue W. F., Okada A., Yamada T., Islam M.M., Hayano J.(2002). Water-based exercise improves health-related aspects of fitness in older women Medicine and Science in Sports and Exercise 33, 544-551 [DOI] [PubMed] [Google Scholar]
- Tsourlou T., Benik A., Dipla K., Zafeiridis A., Kellis S.(2006). The effects of a twenty-four week aquatic training program on muscular strength performance in healthy elderly women, Journal of Strength and Conditioning Research 20, 811-818 [DOI] [PubMed] [Google Scholar]
- Wilder R.D., Brennan D.K., Schotte D.(1993). A standard measure for exercise prescription for aqua running . American Journal of Sports Medicine 21, 45-48 [DOI] [PubMed] [Google Scholar]


