Abstract
Bacillus anthracis is surrounded by an antiphagocytic polypeptide capsule composed of poly γ-d-glutamic acid (γDPGA). γDPGA has been identified recently as a potential target for vaccine development. Studies of the role of γDPGA in disease have been hampered by the poor Ab response to this antigen and the lack of immunochemical reagents. As a consequence, neither the extent of γDPGA production during anthrax nor the protective activity of γDPGA Abs in inhalation anthrax are known. Here we report production of IgG Abs to γDPGA in mice following an immunization regimen using γDPGA in combination with agonist mAbs to CD40. mAbs were produced that are specific for γDPGA. Passive immunization with γDPGA mAbs protected >90% of mice in a pulmonary model of anthrax that was lethal in control mice (P < 0.0001). Use of γDPGA mAb in an antigen detection immunoassay found that the appearance of γDPGA in serum coincided with the emergence of bacteremia. These studies identify CD40 stimulation as a means for production of Ab and generation of mAbs against a weakly immunogenic antigen and demonstrate that the capsule is an effective target for immunoprotection and for antigen detection in the diagnosis of anthrax.
Inhalation anthrax occurs in several discrete steps (1). Endo-spores of Bacillus anthracis are taken up by macrophages at the site of initial infection and may be transported to regional lymph nodes (2). The spores germinate inside the phagolysosome to become vegetative bacteria that escape from the phagolysosome and replicate within the cytoplasm (3, 4). Vegetative cells are released into the extracellular milieu and enter the circulation, where the vegetative cells grow extracellularly to levels as high as 108 bacteria per ml of blood. In this environment, the vegetative bacteria respond to physiological body temperature and CO2 levels to transcriptionally activate genes responsible for capsule formation and toxin synthesis (5). Finally, massive edema and organ failure are produced as a consequence of toxin formation. Experience with the 2001 bioterrorism incident found that, once the disease reaches the phase during which patients show evidence of significant toxin production, treatment with antibiotics can do little to prevent a fatal outcome (6). Similar results were reported in animal models (7). As a consequence, early diagnosis and intervention before toxin production are essential to patient survival.
B. anthracis is surrounded by an antiphagocytic capsule composed of poly γ-d-glutamic acid (γDPGA). Recent studies highlighted the γDPGA capsule as a potential target for vaccine development (8, 9). γDPGA is poorly immunogenic and shares many properties with T cell-independent polysaccharides, e.g., high molecular weight, repeating epitopes, resistance to degradation in vivo, and enhanced immunogenicity when complexed to protein. Two recent reports demonstrated that protein conjugates of γDPGA are immunogenic in mice (8, 9). However, the ability of anti-γDPGA to prevent anthrax in vivo has not been reported.
Studies of γDPGA production during infection and an assessment of protection by anti-γDPGA have been hampered by the poor immunogenicity of this antigen, the inherent difficulty in generating mAbs to weakly immunogenic antigens, and the consequent lack of immunochemical reagents. An alternative approach to protein conjugates or whole bacteria for induction of an IgG Ab response to T cell-independent antigens is the use of CD40 agonist mAb to enhance the immune response (10). Here we report production of anti-γDPGA IgG in mice using an immunization regimen of γDPGA in combination with agonist CD40 mAb, the generation of mAbs reactive with γDPGA, protection by anti-γDPGA in a murine model of pulmonary anthrax, and the use of γDPGA mAbs for detection of γDPGA in serum of infected mice. These results indicate that the γDPGA capsule can be targeted for active and passive immunization and for antigen detection in diagnosis of inhalation anthrax.
Experimental Procedures
Bacterial Strains, Bacterial Culture, and Isolation of γDPGA. Bacillus licheniformis strain 9945 was obtained from the American Type Culture Collection. B. anthracis Pasteur strain is maintained by the Nevada State Health Laboratory (Reno) and was originally obtained from the Centers for Disease Control and Prevention (Atlanta). The B. anthracis Ames strain was obtained from the U.S. Army Medical Research Institute of Infectious Diseases (Frederick, MD).
B. licheniformis was grown for 60 h on a gyratory shaker (250 rpm) at 37°C on Medium E that contained 2 mM MnCl2·4 H2O to stimulate maximal production of γPGA in the D isoform (11, 12). Sodium acetate crystals and glacial acetic acid were added to final concentrations of 10% and 1%, respectively. The bacterial cells were removed by centrifugation followed by filtration, and the PGA was precipitated from the medium with two volumes of ethanol. The precipitate was resolubilized in sodium acetate buffer (10% sodium acetate crystals and 1% glacial acetic acid) and reprecipitated with ethanol. The precipitate was washed with absolute ethanol and acetone and dried. Amino acid analysis showed the presence of only glutamic acid. A phenol-sulfuric acid test for carbohydrate (13) was negative. An acid hydrolysate exhibited a specific optical rotation (-25.2°) indicating that ≈84% of the glutamic acid was the D isomer.
B. licheniformis was also grown as described above in Medium E that contained 0.15 μM MnCl2·4 H2O to maximize production of PGA in the L isoform. Capsulated bacteria grown in this manner were used to assess mAb binding to cells having capsules of predominantly γLPGA.
B. anthracis γDPGA was isolated from cultures of the Pasteur strain that were grown on a dialysate of brain heart infusion broth (Difco) for 24 h on a gyratory shaker (175 rpm) at 37°C in 15% CO2. Formaldehyde was added to a final concentration of 2% for 24 h at 23°C. Nonviability of the culture was confirmed by plating on nutrient agar (Difco). γDPGA was isolated from the supernatant fluid of B. anthracis broth cultures as described above for γDPGA from B. licheniformis.
Immunization of Mice and Production of γDPGA mAbs. Preliminary dose-response experiments established that optimal serum levels of anti-γDPGA IgG were produced when BALB/c mice (Charles River Laboratories) were immunized i.p. with 0.5 μg of γDPGA from B. licheniformis in combination with 400 μg of mAb FGK115, an agonist rat IgG2a anti-mouse CD40 (14). Sera were collected at various times after immunization, and Ab levels were assessed by ELISA in which γDPGA from B. licheniformis was coated onto microtiter plates.
For hybridoma formation, spleens were obtained from mice 8-29 days after immunization with γDPGA in combination with CD40 mAb. In some cases, mice were given an i.v. booster injection of 0.5 or 1.0 μg of γDPGA in PBS 4 days before collection of spleens. Hybridomas were produced by fusion with the X63-Ag8.653 cell line using standard techniques. Cell lines were grown in tissue culture with a Tecnomouse hollow fiber culture system or an Integra CL 1000 culture flask (Integra Biosciences), and mAbs were isolated by affinity chromatography on protein A (Pierce). An irrelevant IgG3 mAb (mAb M600) reactive with the capsular polysaccharide of Cryptococcus neoformans serotypes A and D was used as an isotype control.
Immunoassay for Anti-γDPGA. An ELISA for detection of anti-γDPGA was adapted from a procedure for detection of Ab to meningococcal polysaccharide (15). The procedure is exactly as described for the detection of IgG Abs to cryptococcal glucuronoxylomannan (16), with the exception that plates were coated with B. licheniformis γDPGA. The ELISA was adapted for detection of Ab class and subclass by use of horseradish peroxidase-labeled class- and subclass-specific second Abs (Southern Biotechnology Associates).
Binding of γDPGA mAbs to the B. anthracis capsule was assessed by direct immunofluorescence and by the quellung reaction. The quellung reaction was determined by differential interference contrast microscopy. Direct immunofluorescence used γDPGA mAb F26G3 that had been labeled with Alexa Fluor 488 (Molecular Probes). Microscopy was done with a Nikon Confocal Microscope C1 that was fitted to a Nikon Eclipse E800 microscope. Precipitin formation by soluble γDPGA and mAb F26G3 was assessed by double immunodiffusion in agar (17).
Antigen Capture Immunoassay for γDPGA. Microtiter plates were coated overnight with γDPGA mAb F26G3 in PBS (0.75 μg/ml), washed with PBS-Tween (PBS containing 0.05% Tween 20), and blocked by incubation for an additional 90 min with PBS-Tween. Serial dilutions of γDPGA or sera from infected mice were prepared in PBS-Tween and incubated for 90 min at room temperature with the Ab-coated wells. The wells were washed with PBS-Tween, incubated for 90 min with horseradish peroxidase-labeled (Pierce) γDPGA mAb F26G3 (0.2 μg/ml), washed, and incubated with tetramethylbenzidine substrate (Kirkegaard & Perry Laboratories). The data are reported as picograms of γDPGA per milliliter using B. licheniformis γDPGA as a standard. An OD450 of 0.5 was used as the limit of assay sensitivity.
Murine Model of Pulmonary Anthrax. For preparation of a spore inoculum, a starter culture was prepared by inoculating phage assay broth (4) with a colony of B. anthracis (Ames strain) from a blood agar plate and incubated overnight at 37°C on a shaker at 350 rpm. Large-scale culture was prepared by inoculating fresh phage assay broth with a portion of the starter culture (1:40 ratio) and incubated for 24 h at 37°C on a shaker at 350 rpm. Sterile distilled water was added, and the incubation was continued for an additional 40-80 h. After 40 h of incubation, the cultures were examined periodically by phase contrast microscopy to confirm complete sporulation and the absence of vegetative cells. The spore preparation was then heated at 68°C for 40 min to eliminate trace contamination with vegetative forms. Aliquots of the spore suspension were frozen at -80°C, and the titer of the spore stock was determined by quantitative culture on blood agar plates.
BALB/c mice (Harlan) were used for pulmonary anthrax studies. To challenge the mice, frozen spore stocks were thawed and diluted in sterile PBS to the appropriate concentration for intratracheal delivery. Mice were anesthetized with avertin, and a 50-μl inoculum containing 5 LD50 (≈5,000 spores) was instilled into the lungs via the intratracheal route. Mice were observed twice daily for moribundity or death.
Quantitative culture of spleen was used as an indicator for bacteremia. Mice were killed, spleens were harvested and homogenized in 1 ml of PBS, and quantitative plate cultures were prepared from 50 μl of splenic homogenate or a serial dilution of homogenate. The sensitivity limit for determination of splenic colony-forming units (CFU) was ≈20 CFU per spleen.
Statistics. Survival curves were analyzed by use of Kaplan-Meier estimators, survival curves were compared by using the log-rank test, and pairwise multiple comparisons were done with P values adjusted for these multiple comparisons by the Bonferroni method. Correlation coefficients were determined by the Spearman rank correlation coefficient.
Results
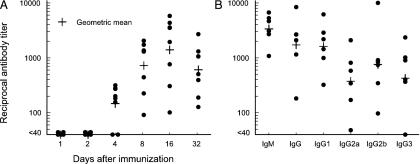
Immunization of Mice and Production of γDPGA mAbs. As shown by others (8, 9), preliminary studies found little or no Ab response after immunization with γDPGA alone. As a consequence, we attempted immunization of BALB/c mice with B. licheniformis γDPGA in combination with CD40 agonist mAb. Most mice had detectable anti-γDPGA IgG 4 days after immunization, and all mice were positive after 8 days (Fig. 1A). Examination of the IgG subclass of anti-γDPGA showed an IgG isotype-switched response 7 days after immunization (Fig. 1B). These results demonstrate that CD40 stimulation with an agonist mAb facilitates production of a serum Ab response to weak antigens.
Fig. 1.
(A) Kinetics for production of anti-γDPGA IgG after immunization with B. licheniformis γDPGA in combination with CD40 agonist mAb. (B) Levels of γDPGA Abs of different isotypes 7 days after immunization with γDPGA in combination with CD40 agonist mAb. Data shown are γDPGA Ab titers for individual mice as well as the geometric mean titers.
Results from study of hybridomas generated from four mice showed few hybridomas secreting anti-γDPGA from mice immunized with γDPGA plus CD40 mAb alone (Table 1). However, the number of Ab-secreting hybridomas was increased >100-fold if mice were given a booster immunization 4 days before the collection of spleens. Five cell lines that secrete anti-γDPGA were cloned by limiting dilution. Notably, four of the five cell lines secreted anti-γDPGA IgG3. One hybridoma that produced mAb F26G3 was selected for further study. This hybridoma was chosen because the cell line adapted well to large-scale Ab production in high concentrations in vitro.
Table 1. Hybridoma formation from spleens of mice immunized with γDPGA in combination with CD40 agonist mAb.
| Fusion no.* | Immunization protocol | IgM-secreting wells/total wells† | IgG-secreting wells/total wells† | Cell lines produced and cloned by limiting dilution |
|---|---|---|---|---|
| 21 | γDPGA + CD40 mAb (IP)‡ | Not tested | 1/192 | 21BL (IgG1) |
| 25 | γDPGA + CD40 mAb (IP)§ | 0/192 | 0/192 | None |
| 24 | γDPGA + CD40 mAb (IP) + PGA IV boost¶ | 157/192 | 184/192 | F24G7 (IgG3), F24F2 (IgG3) |
| 26 | γDPGA + CD40 mAb (IP) + PGA IV boost∥ | 33/192 | 20/192 | F26G4 (IgG3), F26G3 (IgG3) |
Each fusion represents a mouse immunized by use of the indicated immunization protocol.
After fusion, cells were distributed into 192 wells. The results indicate the number of wells containing colonies that secrete anti-γDPGA IgM or IgG.
Spleens were harvested for hybridoma production 8 days after immunization with γDPGA plus CD40 mAb.
Spleens were harvested 29 days after immunization with γDPGA plus CD40 mAb.
Mice were given an i.v. booster immunization with 0.5 μg of γDPGA 25 days after the initial immunization with PGA plus CD40 mAb; spleens were harvested 4 days later.
Mice were given an i.v. booster immunization with 1.0 μg of γDPGA 17 days after the initial immunization with PGA plus CD40 mAb; spleens were harvested 4 days later.
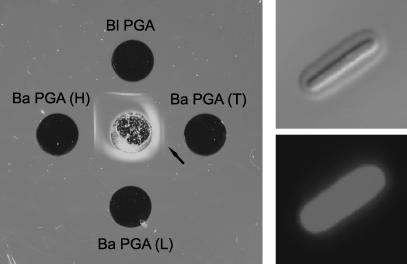
Reactivity of mAb F26G3 with soluble γDPGA and capsulated B. anthracis was determined by double immunodiffusion in agar and differential interference contrast and direct immunofluorescence microscopy, respectively (Fig. 2). The precipitin line produced with γDPGA from B. licheniformis was sharp and slightly concave toward the antigen well. γDPGA from B. anthracis produced two precipitin lines, a broad diffuse band that was concave toward the Ab well and a weak line that was straight (Fig. 2, arrow), suggesting the presence of two species of γDPGA of different molecular sizes. The high and low molecular weight forms were separated by resolubilizing the total γDPGA in sodium acetate buffer, and the high molecular weight γDPGA was precipitated by addition of one volume of ethanol. The low molecular weight γDPGA precipitated upon addition of two more volumes of ethanol. Analysis of the high and low molecular weight precipitates by immunodiffusion showed that the two forms had been separated by this differential precipitation (Fig. 2).
Fig. 2.
(Left) Double immunodiffusion showing reactivity of mAb F26G3 with γDPGA from B. licheniformis (Bl PGA), total γDPGA isolated from B. anthracis [Ba PGA (T)], the low molecular weight fraction of γDPGA isolated from B. anthracis [Ba PGA (L)], and the high molecular weight fraction of γDPGA isolated from B. anthracis [Ba PGA (H)]. The arrow identifies a weak precipitin line produced by a high molecular weight component of the total γDPGA. (Right) Binding of Alexa 488 mAb F26G3 (50 μg/ml) to B. anthracis when viewed by differential interference contrast microscopy to show quellung reaction (Upper) or by confocal microscopy (Lower).
Examination of the binding of mAb F26G3 to capsulated B. anthracis by differential interference contrast microscopy showed a quellung type capsular reaction. Similarly, direct immunofluorescence showed uniform binding of the Ab to the capsule of all cells. An examination by immunofluorescence of binding of mAb F26G3 to cells of B. licheniformis that were grown to stimulate production of γLPGA found that only a small portion (<20%) of the cells bound detectable Ab (data not shown). The failure of mAb to bind to the majority of B. licheniformis grown for production of γLPGA was not because of an absence of capsule formation, because all cells in the population exhibited prominent capsules when viewed by india ink negative stain.
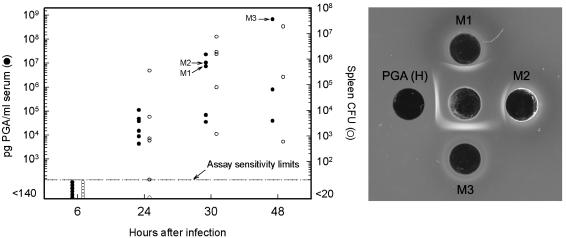
Production of Soluble γDPGA During Pulmonary Anthrax. An antigen capture ELISA was constructed with mAb F26G3 in the capture phase and a horseradish peroxidase conjugate of mAb F26G3 as the indicator. Assessment of assay sensitivity using γDPGA from B. licheniformis demonstrated that the assay could detect γDPGA at concentrations as low as 100-140 pg/ml.
Mice were infected via the intratracheal route with 5 LD50 of B. anthracis spores (Ames strain). Mice were killed 6, 24, 30, or 48 h after challenge. Spleens were harvested for quantitative organ culture, and serum was prepared for analysis of γDPGA content (Fig. 3). At 24 h after challenge, antigenemia was detected in all animals; culture of spleen was positive for five of six mice. An additional result shown in Fig. 3 is the high level of antigenemia that occurs in disseminated anthrax. One mouse showed a γDPGA titer of 1/5,000,000. Such a titer corresponds to ≈600 μg/ml γDPGA.
Fig. 3.
(Left) Detection of γDPGA antigenemia and B. anthracis bacteremia as shown by splenic CFU after intratracheal challenge with 5 LD50 B. anthracis spores. Animals were killed at the indicated times after infection. Serum antigen levels (•) are reported as pg/ml γDPGA using purified γDPGA from B. licheniformis as a standard (left axis). Results from quantitative organ culture (○) are shown as total CFU per spleen (right axis). (Right) Double immunodiffusion showing reactivity of mAb F26G3 with undiluted serum from infected mice (M1, M2, and M3 having concentrations of 7.3, 11, and 670 μg/ml γDPGA, respectively) or the high molecular weight fraction of B. anthracis γDPGA [PGA (H)].
Antigenemia produced during pulmonary anthrax is also demonstrated in Fig. 3, where sera from three infected mice were examined by double immunodiffusion. Prominent precipitin lines were produced. The position of the lines reflects the γDPGA concentration in each of the sera. The shape of the precipitin lines is similar to the high molecular weight γDPGA isolated from B. anthracis grown in vitro (Fig. 2); precipitin lines consistent with the low molecular weight γDPGA were not observed.
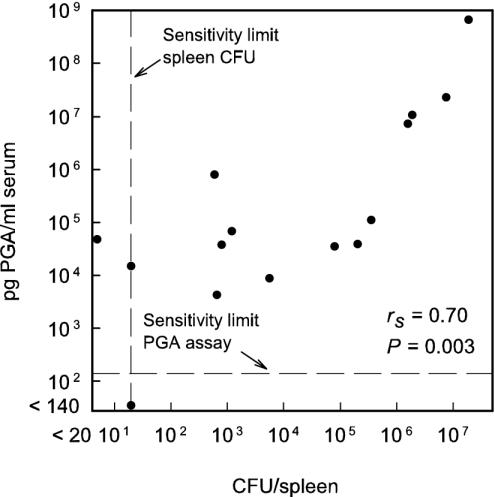
Results from all mice in Fig. 3 that had a positive test for either bacteremia (positive spleen culture) or antigenemia (OD450 ≥ 0.5) are shown in Fig. 4. Antigen concentration in serum is plotted as a function of CFU in spleen for each mouse. The results showed a correlation (rs = 0.70; P = 0.003) between results from the two assays. Despite the correlation for the group of mice, there were several instances in which bacteremia levels exceeded antigenemia levels in individual mice or vice versa. In particular, there were two mice that showed considerable antigenemia, but the spleen cultures were at or below the level of detection.
Fig. 4.
Correlation between levels of antigenemia (pg of γDPGA per ml of serum) and bacteremia (spleen CFU) for individual mice. Results are presented from all mice shown in Fig. 3 regardless of the time after infection at which the samples were taken. Correlation was determined by the Spearman rank correlation coefficient.
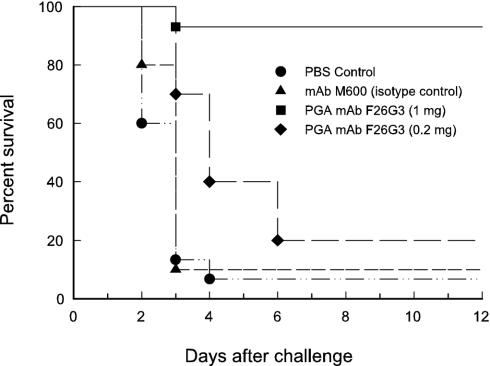
Immunoprotection by γDPGA mAb. Mice were treated by i.p. injection of 1 mg or 200 μg of the IgG3 γDPGA mAb F26G3. Controls were PBS or an irrelevant IgG3 mAb that is reactive with the capsular polysaccharide of C. neoformans (mAb M600). Mice were challenged 18 h after mAb treatment by intratracheal instillation of ≈5 LD50 of spores from the Ames strain of B. anthracis. The results showed that ≥90% of control mice died rapidly, within 3 or 4 days after challenge (Fig. 5). More than 90% of mice given 1 mg of the γDPGA mAb survived (P < 0.0001 vs. control mice). Partial protection was observed in mice passively immunized with 200 μg of the γDPGA mAb where a significant extension of survival time was observed relative to control mice (P < 0.05).
Fig. 5.
Effect of passive immunization on survival of mice after intratracheal challenge with ≈5LD50 of B. anthracis spores. Results shown are the combined data from two independent experiments. Mice were treated 18 h before challenge by i.p. injection of PBS (5 mice in Exp. 1 and 10 mice in Exp. 2), 1 mg irrelevant isotype control (IgG3) mAb M600 (10 mice in Exp. 2), 0.2 mg of γDPGA mAb F26G3 (10 mice in Exp. 2; P < 0.05 vs. control mice), or 1 mg of γDPGA mAb F26G3 (4 mice in Exp. 1 and 10 mice in Exp. 2; P < 0.0001 vs. control mice).
Discussion
Our study of anti-γDPGA has three primary findings. First, use of CD40 agonist mAb was an effective means to make Abs to a polymeric antigen alone, without the need for a protein conjugate. Second, use of γDPGA mAbs in an immunoassay for γDPGA in sera of infected mice found that detectable antigenemia coincided with the emergence of bacteremia. Finally, Abs to γDPGA were protective in a murine pulmonary anthrax model.
Studies of the role of γDPGA in the pathogenesis of anthrax and as a target for active or passive immunization have been hampered by poor immunogenicity. Protein conjugates of γDPGA were recently found to induce high levels of anti-γDPGA in mice. In the present study, we report that a single immunization with γDPGA in combination with CD40 agonist mAb leads to production of specific IgG Abs as early as 4 days after immunization. Use of CD40 agonist mAbs to enhance T cell-independent responses was first reported for Streptococcus pneumoniae capsular polysaccharide (10). Our results extend the enhancing effect of CD40 mAb to a capsular polypeptide and demonstrate that splenic lymphocytes from mice immunized in this manner produce Ab-secreting hybridomas when coupled with a booster immunization shortly before harvesting of spleen cells.
γDPGA for immunization was obtained from B. licheniformis that was grown under conditions that stimulated production of PGA with the D isomer. A mAb that was generated from mice immunized in this manner was reactive with B. anthracis γDPGA as shown by (i) precipitation in double immunodiffusion, (ii) a distinct quellung reaction and binding of fluorescently labeled mAb to whole bacterial cells, (iii) detection of γDPGA in sera of infected mice, and (iv) protection against pulmonary anthrax infection. The absence of binding of mAb to most cells of B. licheniformis grown for production of γLPGA indicates that the Ab is specific for the D isoform. Our observation that the mAb binds to a small portion of the cells grown for production of γLPGA is consistent with studies by Thorne and Leonard (11) that found that PGA isolated from culture filtrates of Bacillus subtilis grown under conditions of limiting Mn2+ produced a mixture of PGA in the D and L forms, with a predominance of γLPGA. Our results extend these findings to suggest that synthesis of the D or L isoform is determined at the level of individual cells.
A difference between γDPGA isolated from B. licheniformis and B. anthracis was the appearance of the antigens in double immunodiffusion. B. licheniformis γDPGA produced a single precipitin line with a shape that was consistent with having a high molecular weight. B. anthracis γDPGA produced two precipitin lines; the shape of one line was consistent with the antigen having a low molecular weight, and the other was consistent with a high molecular weight. The presence of low and high molecular weight γDPGA in culture filtrates of B. anthracis was previously reported by Uchida et al. (18), who attributed the low molecular weight fraction to depolymerization of high molecular weight γDPGA by a depolymerase that is produced by B. anthracis. Analysis of sera from infected mice by double immunodiffusion showed only the high molecular weight form of γDPGA. Absence of the low molecular weight form in serum could be due to a failure to depolymerize the high molecular weight form in vivo. Alternatively, the low molecular weight form could be cleared rapidly from serum.
Little is known about production of soluble γDPGA during anthrax. We used γDPGA mAb F26G3 for construction of an antigen capture immunoassay for detection of soluble antigen. The assay had a detection limit of ≈100 pg/ml. Use of the immunoassay for analysis of sera from infected mice showed that antigen appears at a time after infection that coincides with the appearance of bacteremia as shown by splenic CFU. As the infection progressed, assay for antigenemia closely paralleled the results of splenic culture, suggesting that immunoassay for γDPGA is a useful surrogate for blood culture in the assessment of B. anthracis infection. Finally, in the latter stages of infection, high levels of serum γDPGA were observed, reaching concentrations of >500 μg/ml.
Evaluation of factors influencing patient outcome in the 2001 anthrax attack showed that early recognition of infection and prompt administration of antibiotics were closely associated with patient survival (19). A report of two patients who died of bioterrorism-related inhalation anthrax emphasized the need for specific diagnostic tools that can be used in the clinical setting where infection is likely to be encountered (20). Immunoassay for bacterial capsular antigens in body fluids is a proven technology. Such assays can be inexpensive, sensitive, rapid, and easy to perform by untrained personnel. The finding of readily measurable levels of γDPGA early in infection at the time of emergence of bacteremia suggests that γDPGA detection is a means for early diagnosis of inhalation anthrax.
Finally, the high level of protection afforded by passive immunization with a γDPGA mAb identifies γDPGA as a target for active or passive immunization. The current anthrax vaccine adsorbed is aimed at anthrax toxins. The extent to which a toxin-based immunity alone can protect against the potential large inoculum that might occur in a bioterrorism attack is not known. One approach to an improved vaccine formulation is a conjugate vaccine that targets both the antiphagocytic capsule and the toxin (8, 9). Our results provide strong proof of concept for targeting γDPGA in a vaccine formulation and suggest efficacy of passive immunization in individuals who have not been immunized (21). These data urge clinical evaluation of active immunization with a conjugate vaccine and passive immunization that targets γDPGA.
Acknowledgments
We thank G. Cutter and I. Aban for consultation on the statistical analysis and the staff at the Nevada State Health Laboratory for providing formalin-killed broth cultures of the B. anthracis Pasteur strain. We also thank Lucy Berliba and Kristin Garrison for their technical expertise. This work was supported by Public Health Service Grants AI-14209, CA-99572, and CA-72669 and Defense Advanced Research Program Agency Grant N00178-01-C-3069.
Abbreviations: γDPGA, poly γ-d-glutamic acid; CFU, colony-forming unit.
References
- 1.Dixon, T. C., Meselson, M., Guillemin, J. & Hanna, P. C. (1999) N. Engl. J. Med. 341, 815-826. [DOI] [PubMed] [Google Scholar]
- 2.Ross, J. M. (1957) J. Pathol. Bacteriol. 73, 485-494. [Google Scholar]
- 3.Guidi-Rontani, C., Weber-Levy, M., Labruyère, E. & Mock, M. (1999) Mol. Microbiol. 31, 9-17. [DOI] [PubMed] [Google Scholar]
- 4.Dixon, T. C., Fadl, A. A., Koehler, T. M., Swanson, J. A. & Hanna, P. C. (2000) Cell. Microbiol. 2, 453-463. [DOI] [PubMed] [Google Scholar]
- 5.Koehler, T. M., Dai, Z. & Kaufman-Yarbray, M. (1994) J. Bacteriol. 176, 586-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inglesby, T. V., O'Toole, T., Henderson, D. A., Bartlett, J. G., Ascher, M. S., Eitzen, E., Friedlander, A. M., Gerberding, J., Hauer, J., Hughes, J., et al. (2002) J. Am. Med. Assoc. 287, 2236-2252. [DOI] [PubMed] [Google Scholar]
- 7.Kalns, J., Morris, J., Eggers, J. & Kiel, J. (2002) Biochem. Biophys. Res. Commun. 297, 506-509. [DOI] [PubMed] [Google Scholar]
- 8.Schneerson, R., Kubler-Kielb, J., Liu, T.-Y., Dai, Z. D., Leppla, S. H., Yergey, A., Backlund, P., Shiloach, J., Majadly, F. & Robbins, J. B. (2003) Proc. Natl. Acad. Sci. USA 100, 8945-8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhie, G. E., Roehrl, M. H., Mourez, M., Collier, R. J., Mekalanos, J. J. & Wang, J. Y. (2003) Proc. Natl. Acad. Sci. USA 100, 10925-10930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dullforce, P., Sutton, D. C. & Heath, A. W. (1998) Nat. Med. 4, 88-91. [DOI] [PubMed] [Google Scholar]
- 11.Thorne, C. B. & Leonard, C. G. (1958) J. Biol. Chem. 233, 1109-1112. [PubMed] [Google Scholar]
- 12.Leonard, C. G., Housewright, R. D. & Thorne, C. B. (1958) J. Bacteriol. 76, 499-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubois, M., Gilles, K. A., Hamilton, J. K., Rebers, P. A. & Smith, F. (1956) Anal. Chem. 28, 350-356. [Google Scholar]
- 14.Hixon, J. A., Blazar, B. R., Anver, M. R., Wiltrout, R. H. & Murphy, W. J. (2001) Biol. Blood Marrow Transplant. 7, 136-143. [DOI] [PubMed] [Google Scholar]
- 15.Leinonen, M. & Frasch, C. E. (1982) Infect. Immun. 38, 1203-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brandt, S., Thorkildson, P. & Kozel, T. R. (2003) Clin. Diagn. Lab. Immunol. 10, 903-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ouchterlony, Ö. (1948) Acta Pathol. Microbiol. Scand. 25, 186-191. [DOI] [PubMed] [Google Scholar]
- 18.Uchida, I., Makino, S., Sasakawa, C., Yoshikawa, M., Sugimoto, C. & Terakado, N. (1993) Mol. Microbiol. 9, 487-496. [DOI] [PubMed] [Google Scholar]
- 19.Jernigan, J. A., Stephens, D. S., Ashford, D. A., Omenaca, C., Topiel, M. S., Galbraith, M., Tapper, M., Fisk, T. L., Zaki, S., Popovic, T., et al. (2001) Emerg. Infect. Dis. 7, 933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borio, L., Frank, D., Mani, V., Chiriboga, C., Pollanen, M., Ripple, M., Ali, S., DiAngelo, C., Lee, J., Arden, J., et al. (2001) J. Am. Med. Assoc. 286, 2554-2559. [DOI] [PubMed] [Google Scholar]
- 21.Casadevall, A. (2002) Nat. Biotechnol. 20, 114. [DOI] [PubMed] [Google Scholar]