Abstract
Background:
Dietary supplements are used by one-third of children. We examined motivations for supplement use in children, the types of products used by motivations, and the role of physicians and health care practitioners in guiding choices about supplements.
Methods:
We examined motivations for dietary supplement use reported for children (from birth to 19 y of age; n = 8,245) using the National Health and Nutrition Examination Survey 2007–2010.
Results:
Dietary supplements were used by 31% of children; many different reasons were given as follows: to “improve overall health” (41%), to “maintain health” (37%), for “supplementing the diet” (23%), to “prevent health problems” (20%), and to “boost immunity” (14%). Most children (~90%) who use dietary supplements use a multivitamin–mineral or multivitamin product. Supplement users tend to be non-Hispanic white, have higher family incomes, report more physical activity, and have health insurance. Only a small group of supplements used by children (15%) were based on the recommendation of a physician or other health care provider.
Conclusion:
Most supplements used by children are not under the recommendation of a health care provider. The most common reasons for use of supplements in children are for health promotion, yet little scientific data support this notion in nutrient-replete children.
The use of dietary supplements has increased in the last 30 y in the United States (1,2). Parents who use dietary supplements are more likely to have children who use them (3). Approximately one-third of infants, children, and adolescents (from birth to 19 y of age, henceforth referred to as children) in the United States are reported to use dietary supplements (4,5). However, the actual motivations for use of dietary supplements among children remain unclear. The purpose of this analysis was to examine motivations for use of dietary supplements by children, to characterize the types of products that are commonly used, and to update previous estimates of dietary supplement use among children using the National Health and Nutrition Examination Survey (NHANES), 2007–2010.
Results
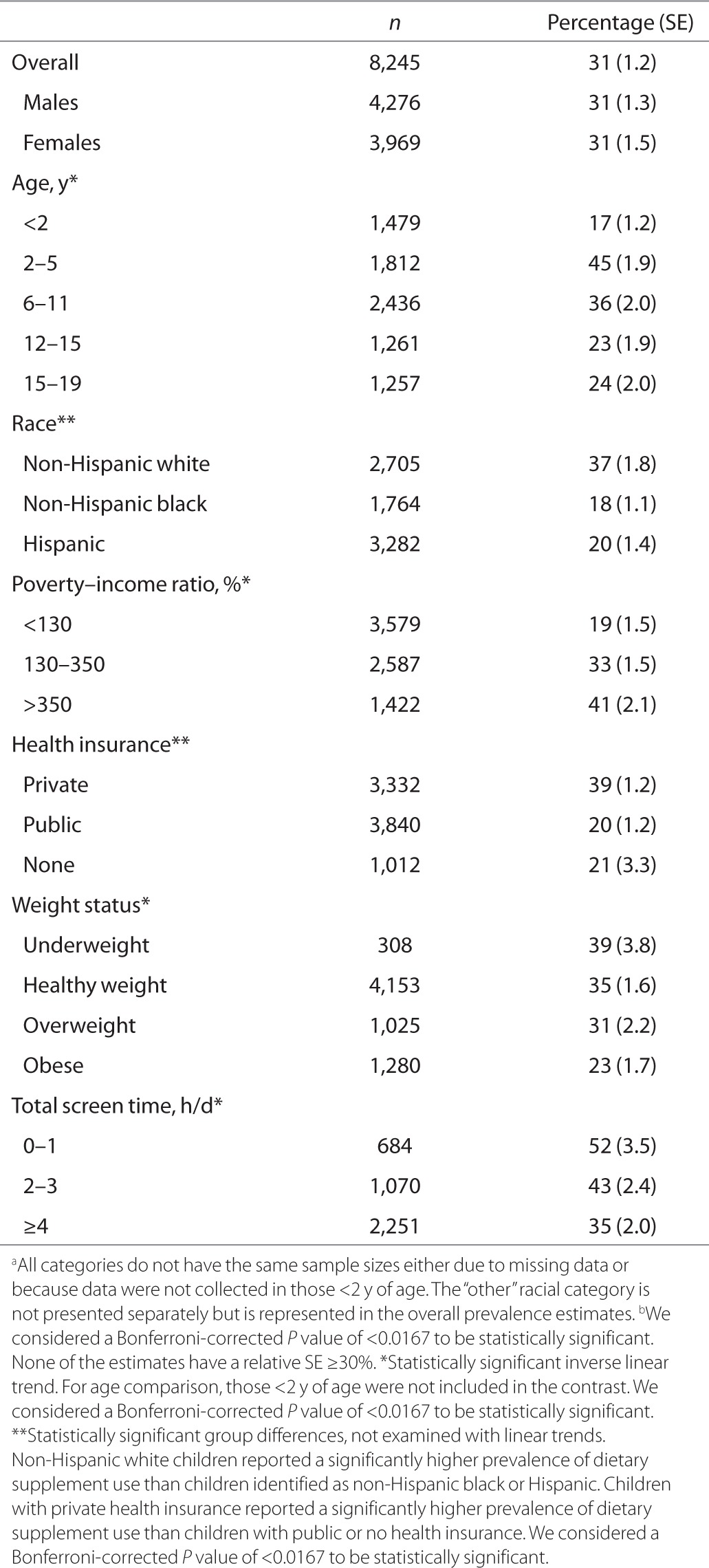
In the period 2007–2010, 31% of children reported the use of dietary supplements in the past month, with no differences by sex. When children <2 y of age were excluded, there was a significant inverse trend toward lower dietary supplement use with increasing age (Table 1). Dietary supplements were more frequently used by non-Hispanic white children than by non-Hispanic black or Hispanic children. Children with private health insurance were more likely to report using dietary supplements than those with public or no health insurance. Weight status, poverty–income ratio, and time spent in front of a computer, television, or video game screen were all inversely related to dietary supplement use. The vast majority of children took one (86%, SE = 1) or two (10%, SE = 1) dietary supplements (data not shown) in the past 30 d.
Table 1. Prevalence (percentage (SE)) of use of dietary supplements among children (≤19 y of age) in the United States by demographic and lifestyle characteristics, 2007–2010a,b.
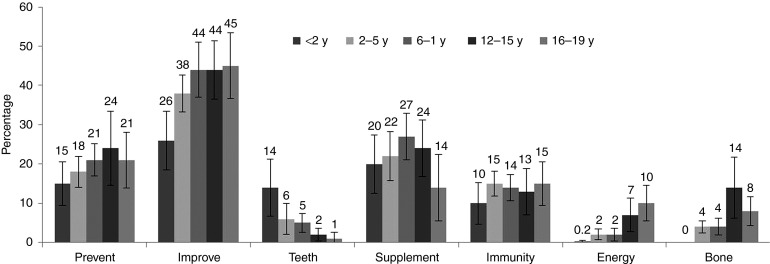
Among children who took dietary supplements, 41% reported using supplements to “improve overall health”, 37% to “maintain health”, 23% for “supplementing the diet”, 20% to “prevent health problems”, and 14% to “boost immunity” (Table 2). There were no significant differences by sex in motivations for use of dietary supplements. The youngest children, <2 y of age, were more likely to use supplements for “tooth health and cavity prevention” (14%, SE = 3.7); whereas the oldest children, 16–19 y of age, were more likely to report using products “to get more energy” (10%, SE = 2.3; Figure 1). Less than 1% of children were reported to use dietary supplements for specific health conditions (e.g., diabetes, weight loss, and allergies), to improve well-being (e.g., enhance sleep and reduce stress), or for organ site–specific health reasons (e.g., heart, eye, joints, respiratory problems, thyroid imbalance, or liver detoxification; data not shown).
Table 2. Prevalence (%(SE)) of reported motivations for use of dietary supplements among children (≤19 y of age) who reported dietary supplement use in the past 30 d in the United States, 2007–2010.
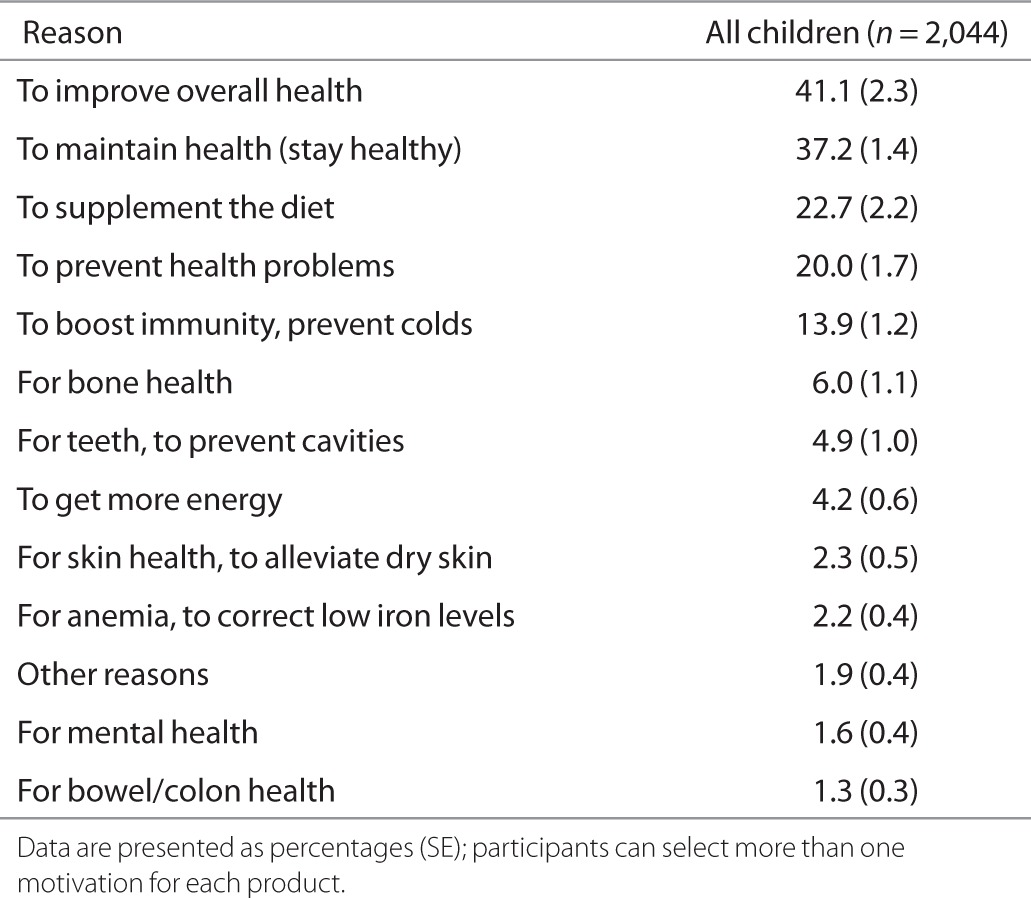
Figure 1.
Prevalence of selected motivations for dietary supplement use by age group among children (≤19 y of age) in the United States, 2007–2010.
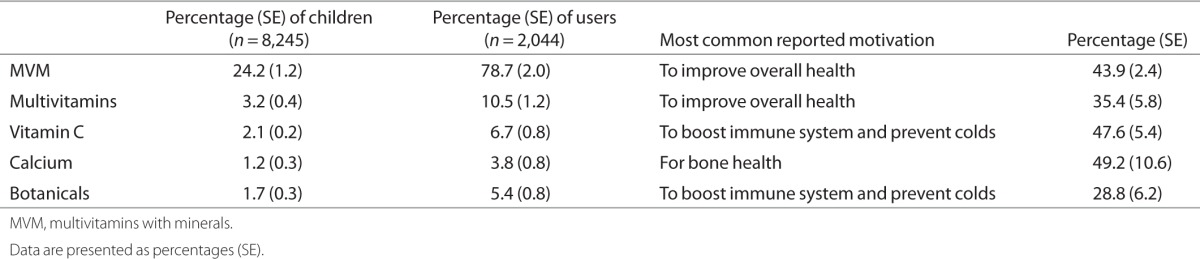
Multivitamins with minerals (MVMs) were the most frequently reported supplement products used by children, followed by multivitamins (without minerals), vitamin C, calcium, and botanicals (Table 3). All other product classes were reported to be used by <1% of children and are not shown. The most frequent motivation among children for using MVMs, multivitamins, and botanicals was to “improve overall health.” Vitamin C was used most commonly to “boost the immune system and prevent colds,” whereas calcium was used most often for improving “bone health.” Because very few children used vitamins A, E, B12, B6, and folic acid; iron; magnesium; and joint-health, sports-nutrition, or “other” dietary supplements, an analysis of motivations for using these products was not possible.
Table 3. Prevalence (percentage (SE)) of specific types of dietary supplements and the most frequently reported motivation for use of each product type in children (≤19 y of age) in the United States, 2007–2010.
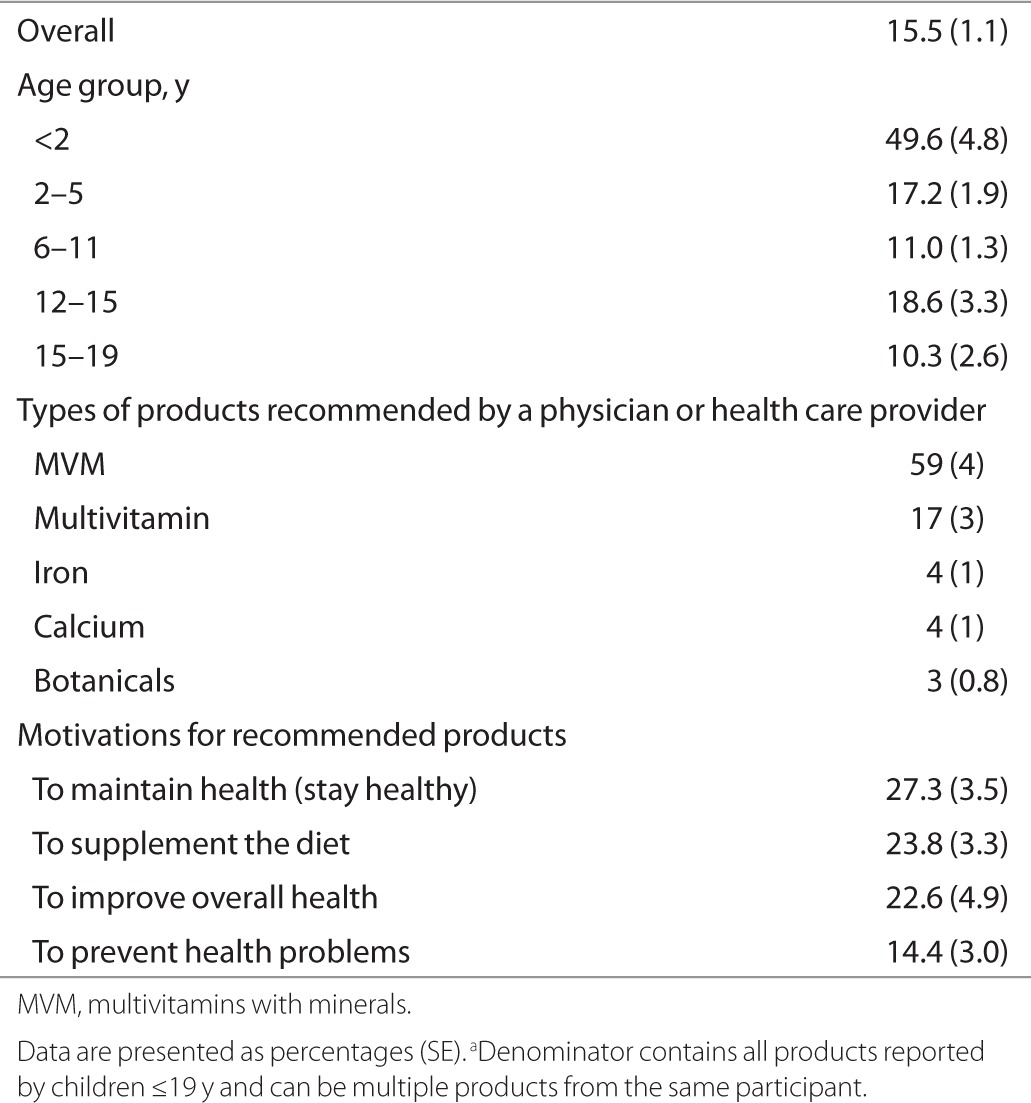
Overall, 15.5% of the products reported to be used by children were based on the advice or recommendation of a physician or other health care professional (Table 4). This was much more common among children ≤2 y of age, with ~50% of the products reported to be used by this group being on the basis of the recommendation of a physician or other health care professional. Only 10% of the products reported to be used by 15–19 y olds were based on the recommendations of health care providers. Nearly 60% of the products used on the basis of the recommendations of health care providers were MVM products. These dietary supplement products were recommended by the health care providers primarily to “maintain health or stay healthy” (Table 4).
Table 4. The proportion (percentage (SE)) of products used by US children (≤ 19 y) that were recommended by a physician or health care provider, 2007–2010 (n = 2,269)a.
Discussion
The results of our analysis indicate that children's primary reasons for using dietary supplements were to improve or maintain health. These motivations did not differ by sex and were consistent across all age groups. However, younger children were more likely to use products to promote dental health (i.e., prevent cavities), whereas teenagers used supplements “to enhance energy.” The use of supplements to treat or prevent specific health conditions was very low. Only about one-quarter of children used dietary supplements to enhance nutrient intake from food.
Nearly 90% of child dietary supplement users use MVM or multivitamin products and they use these products primarily to improve their health. Vitamin C, calcium, and botanicals/herbals as stand-alone products were used by ~1–2% of children; however, these may also be ingredients within MVM or multivitamin products. Patterns of dietary supplement use among children have been fairly consistent over the past decade, with ~30% reporting the use of some supplement product in the previous 30 d (4,5). The sociodemographic characteristics of supplement users are similar in children and adults; in both age groups, the use of dietary supplements is higher in people who are non-Hispanic white, have a higher family income, and have health insurance (2,5). Screen time in children and physical activity among adults are positively associated with higher dietary supplement use (6). However, in adults, the use of dietary supplements by BMI categories does not have the same positive linear relationship as it does in children; normal weight adults most frequently reported the use of dietary supplements (53%), followed by overweight adults (49%), obese adults (46%), and underweight adults (44%). Our analysis also confirms previous findings that supplement use in children is more common in those aged 2–5 y than in other age groups and that infants and young toddlers (<2 y of age) have the lowest use of supplements (10%, SE = 2, in those <1 y of age, data not shown) (5).
In our study, weight status and screen time were inversely related to supplement use. This finding is consistent with previous reports (5), supporting the notion that children who use supplements are perhaps more physically active than those who do not use them. Two previous studies found that teenage supplement users were more likely to express intentions to make healthy food choices (7) and engage in physical activity practices than nonusers (8). Our finding that the use of nutrient-containing supplements is low in adolescents is paradoxical, because nutrient intake from food sources among teenagers is likely to be inadequate to achieve some of the Dietary Reference Intake targets. By contrast, children aged 2–8 y, who more frequently use dietary supplements, are more likely to meet the nutrient recommendations from foods alone than are older children (9).
In this report, we classified products into mutually exclusive groups. Previously, we examined the use of micronutrients from dietary supplements regardless of the type of the product (4,5). For example, in this analysis, 1.2% of children specifically used a calcium product, whereas we previously reported (NHANES 2003–2006) that 18–30% of children use any type of product that contains calcium (i.e., could come from an MVM or any other product). Therefore, the estimates for specific types of products identified in this analysis are not directly comparable with those of previous NHANES data for specific micronutrients. However, the overall prevalence estimates and the estimates of MVM and multivitamin use can be compared because they have been classified similarly across previous NHANES studies (4,5).
The most common MVM products used by children provide >50% of the daily value for vitamins (A, C, D, E, B1, B2, B3, B6, B12; folic acid, pantothenic acid) and minerals (iron, iodine, zinc, and copper), with the exception of calcium. Of note, a recent study indicates that calcium and vitamin D intakes remain low in children (2–18 y of age), even among those who use dietary supplements (9). However, among children who used dietary supplements, excess nutrient intake was also observed for folic acid (49%), zinc (52%), and vitamin A (45%) (9).
Approximately 15% the of products reported to be used by children were based on the recommendations from a physician or health care provider; stated differently, 85% of the supplements used by US children are based on either self-selection or decisions made by parents, caregivers, or others who may or may not be qualified to guide the choice of when and how much to supplement a diet. Health care providers were more likely to recommend dietary supplements to children <2 y of age than to other age groups. This is a diverse age group: those <1 y of age may be exclusively breast or bottle fed, whereas some infants are being introduced to food at 4–6 mo of age. The American Academy of Pediatrics recommends vitamin D and iron (after 4 mo of age) supplements to exclusively breastfed children, and the American Dental Association Council on Scientific Affairs recommends fluoride to children at high risk of developing dental caries and whose primary source of drinking water is deficient in fluoride; however, no other formal guidelines exist on the use of dietary supplements in healthy children in any other age groups.
The 24-h dietary recall has been shown to be a less-biased estimator of calories and protein from foods in adults than a frequency-based questionnaire (10). However, no such comparisons are available for dietary supplements. In NHANES 2007–2010, information on dietary supplement use was collected by both the Dietary Supplement Questionnaire (DSQ) and the 24-h dietary recalls. We have previously examined the prevalence of use from the DSQ in comparison with the 24-h recalls in NHANES and found that there is a higher prevalence of dietary supplement use when the DSQ is used compared with the 24-h recall data. This was an expected finding because some supplements may be taken episodically (i.e., vitamin C for a cold), whereas others are taken habitually (i.e., calcium for bone health), and the 30-d time frame is more likely to accurately capture dietary supplement use (11). The other strength of the DSQ is that it is administered in the home interview where NHANES staff view the product labels to ensure the most accurate information. A limitation of this analysis is that the NHANES is a cross-sectional study and thus these motivations are assessed at only one point in time.
In conclusion, nearly one-third of the children in the United States use dietary supplements, most often one product. Patterns of use of supplements have been consistent across time in the United States. Most children who use dietary supplements use an MVM or a multivitamin product. This report is the first to characterize motivations for use of dietary supplements among children using the NHANES data. Only a small percentage of supplements used by children were based on the recommendation of a physician or other health care provider. Both adults and children primarily report using dietary supplements to improve or maintain overall health (6). Due to the lack of scientific evidence (and very limited scientific inquiry) for the role of dietary supplements in promoting health in nutrient-replete children, knowledge of the reasons for supplement use may help in guiding physicians and health care providers to tailor anticipatory guidance to children and their caregivers.
Methods
The NHANES is a nationally representative, cross-sectional survey that collects data on a sample of noninstitutionalized, civilian US residents using a complex, stratified, multistage probability cluster sampling design (12). The National Center for Health Statistics of the Centers for Disease Control and Prevention collects the NHANES data. Participants complete an in-home interview and a physical examination after the home interview. We combined data from NHANES participants aged ≤19 y of age from the NHANES 2007–2008 and 2009–2010 (n = 8,534) waves and excluded data on age-eligible participants with missing information on dietary supplement use (n = 5) or physical examination results (n = 284); the final analytical sample size was 8,245. A proxy informant provided information for survey participants who were <16 y and individuals who could not answer the questions themselves. Participants aged ≥16 y and emancipated minors were interviewed directly. Written informed consent was obtained from all participants either by parental consent (for those who were ≤6 y of age) or parent consent and child assent for those aged ≥7 y. The survey protocol was approved by the National Center for Health Statistics Research Ethics Review Board.
Demographic data, including age, sex, and race/ethnicity, were collected through a computer-assisted personal interview. The NHANES sampling framework includes the following age groups for children: 0–5, 6–11, and 12–19 y of age; we chose to further break down the age groups to 0–2, 2–5, 6–11, 12–15, and 16–19 y of age. Self-reported race/ethnic groups as defined in the NHANES were non-Hispanic white, non-Hispanic black, Hispanic (including Mexican American), and other races (including multiracial). Following the recommendations of the National Center for Health Statistics, the “other” race group was only used in the estimates for the total sample. We constructed three categories of the family poverty–income ratio—the ratio of household income to the poverty threshold—after adjustments for inflation and family size, as follows: <130, 130–350, and >350%. A poverty–income ratio <130% is the eligibility criterion for participation in the Supplemental Nutrition Assistance Program (i.e., the former Food Stamps Program) and these cutoff points have been previously used in the NHANES analyses of children during these survey years (13). We calculated screen time as the sum of the total time spent looking at a television, computer, and/or videogame screen per day for those aged ≥2 y (n = 4,006) using the Physical Activity Questionnaire. Health insurance was categorized as none, private, or public health insurance (14).
The NHANES study uses the DSQ to collect detailed information on each participant's use of any dietary supplement during the past 30 d (15). Participants are also asked to show the survey personnel the containers of each reported supplement. Supplement containers were seen 75% of the time. The NHANES interviewers also assessed motivations for each reported supplement using a card that lists possible reasons for taking each supplement; participants could choose >1 reason. Participants were also able to provide their own reasons if it was not found on the hand card as one of the response categories.
All supplements were categorized into broad, mutually exclusive supplement categories based on their nutrient content and/or characteristics that many mentioned in describing these products. The categories reported for use in children in this study were as follows: (i): multivitamin: MVM, defined as a single product containing three or more vitamins and at least one mineral; (ii) botanicals and herbals; (iii) multivitamins (without minerals); (iv) calcium-containing supplements (in combination with vitamin D or other nutrients); and (v) single-nutrient supplements, such as supplements containing only vitamin C or only iron. A calcium-containing supplement has calcium as the primary ingredient, with or without other minerals or vitamins, and is not part of an MVM. Complete details of the categorization scheme are published elsewhere (6).
The NHANES personnel measured weight and height during the physical examination. Percentiles of BMI, which are calculated as weight in kilograms divided by height in meters squared, were used to categorize each participant's weight status as underweight (<5th percentile), healthy weight (5th–85th percentiles), overweight (85th–95th percentiles), and obese (≥95th percentile) based on the growth charts of the Centers for Disease Control and Prevention (2000); the SAS programs used to calculate BMI percentiles in children are publicly available (16). Children <2 y of age were not included in the study.
Statistical Analysis
All data were analyzed using SAS, version 9.3 (SAS Institute, Cary, NC) and SUDAAN, version 10.0 (RTI International, Research Triangle Park, NC) statistical software programs to incorporate the physical examination survey weights that account for unequal probabilities of selection, nonresponse, and oversampling. Motivations for use of dietary supplements are presented only for users of supplements (n = 2,044); a user was defined as an individual who reported using any dietary supplement on the DSQ (i.e., within the past 30 d). We conducted linear trend tests using four age categories (constructed based on recommendations, poverty–income ratio, BMI, and screen time). We used individual t-tests for testing the differences in race/ethnicity, sex, and health insurance groups. We examined the statistical reliability of estimates using the relative standard error as recommended by the National Center for Health Statistics. Estimates with a relative standard error >30% may be statistically unreliable and are shown in tables. We considered a Bonferroni-corrected P value of <0.0167 to be statistically significant.
Statement of Financial Support
This work was supported in part by resources from the Office of Dietary Supplements at the National Institutes of Health.
References
- Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004;24:401–31. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999-2000. Am J Epidemiol. 2004;160:339–49. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- Dwyer J, Nahin RL, Rogers GT, et al. Prevalence and predictors of children's dietary supplement use: the 2007 National Health Interview Survey. Am J Clin Nutr. 2013;97:1331–7. doi: 10.3945/ajcn.112.052373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey RL, Gahche JJ, Lentino CV, et al. Dietary supplement use in the United States, 2003-2006. J Nutr. 2011;141:261–6. doi: 10.3945/jn.110.133025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picciano MF, Dwyer JT, Radimer KL, et al. Dietary supplement use among infants, children, and adolescents in the United States, 1999-2002. Arch Pediatr Adolesc Med. 2007;161:978–85. doi: 10.1001/archpedi.161.10.978. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Gahche JJ, Miller PE, Thomas PR, Dwyer JT. Why US adults use dietary supplements. JAMA Intern Med. 2013;173:355–61. doi: 10.1001/jamainternmed.2013.2299. [DOI] [PubMed] [Google Scholar]
- Dwyer JT, Garcea AO, Evans M, et al. Do adolescent vitamin-mineral supplement users have better nutrient intakes than nonusers? Observations from the CATCH tracking study. J Am Diet Assoc. 2001;101:1340–6. doi: 10.1016/s0002-8223(01)00321-2. [DOI] [PubMed] [Google Scholar]
- George GC, Springer AE, Forman MR, Hoelscher DM. Associations among dietary supplement use and dietary and activity behaviors by sex and race/ethnicity in a representative multiethnic sample of 11th-grade students in Texas. J Am Diet Assoc. 2011;111:385–93. doi: 10.1016/j.jada.2010.11.019. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Fulgoni VL, 3rd, Keast DR, Lentino CV, Dwyer JT. Do dietary supplements improve micronutrient sufficiency in children and adolescents. J Pediatr. 2012;161:837–42. doi: 10.1016/j.jpeds.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subar AF, Kipnis V, Troiano RP, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol. 2003;158:1–13. doi: 10.1093/aje/kwg092. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Gahche JJ, Dodd KW, Dwyer JT.Changes in the dietary supplement collection system in NHANES 2007–2008: implications for researchers. FASEB J 20112529.220826543 [Google Scholar]
- National Center for Health Statistics. About the National Health and Nutrition Examination Survey.http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.) Accessed 27 March 2013.
- Fakhouri TH, Hughes JP, Brody DJ, Kit BK, Ogden CL. Physical activity and screen-time viewing among elementary school-aged children in the United States from 2009 to 2010. JAMA Pediatr. 2013;167:223–9. doi: 10.1001/2013.jamapediatrics.122. [DOI] [PubMed] [Google Scholar]
- Schober SE, Makuc DM, Zhang C, Kennedy-Stephenson J, Burt V.Health insurance affects diagnosis and control of hypercholesterolemia and hypertension among adults aged 20–64: United States, 2005–2008.NCHS Data Brief 1–8. [PubMed]
- National Center for Health Statistics. National Health and Nutrition Examination Survey. Household Interview Questionnaires.http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.) Accessed 1 September 2010.
- Centers for Disease Control and Prevention. A SAS Program for the Growth Charts. http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.) Accessed 15 November 2012.